Abstract
Treatment-resistant depression (TRD) occurs in many patients and causes high morbidity and mortality. Because TRD subjects are particularly difficult to study especially longitudinally, biological data remain very limited. In a preliminary study to judge feasibility and power, 25 TRD patients were referred from specialty psychiatric practices. All were severely and chronically depressed and mostly had comorbid psychiatric disorders as is typical in TRD. Nine patients were able to complete all required components of the protocol that included diagnostic interview; rating scales; clinical magnetic resonance imaging; medication washout; treatment with maximally tolerated olanzapine-fluoxetine combination for 8 weeks; and pre- and post-treatment fluorodeoxyglucose positron emission tomography. This drug combination is an accepted standard of treatment for TRD. Dropouts arose from worsening depression, insomnia, and anxiety. One patient remitted; three responded. A priori regions of interest included the amygdala and subgenual cingulate cortex (sgACC; Brodmann area BA25). Responders showed decreased metabolism with treatment in the right amygdala that correlated with clinical response; no significant changes in BA25; better response to treatment the higher the baseline BA25 metabolism; and decreased right ventromedial prefrontal metabolism (VMPFC; broader than BA25) with treatment which did not correlate with depression scores. The baseline metabolism of all individuals showed heterogeneous patterns when compared to a normative metabolic database. Although preliminary given the sample size, this study highlights several issues important for future work: marked dropout rate in this study design; need for large sample size for adequate power; baseline metabolic heterogeneity of TRD requiring careful subject characterization for future studies of interventions; relationship of amygdala activity decreases with response; and the relationship between baseline sgACC and VMPFC activity with response. Successful treatment of TRD with olanzapine-fluoxetine combination shows changes in cerebral metabolism like those seen in treatment-responsive major depression.
Introduction
Treatment-resistant depression (TRD) is often operationally defined as a major depressive episode that fails to remit after treatment with at least two antidepressants of different classes at therapeutic doses for an adequate treatment period [1–8]. More extensive staging criteria for TRD have been proposed as well [1]. TRD must be distinguished from inadequately treated depression resulting from numerous factors such as patient non-compliance, intolerance to side effects, misdiagnosis (e.g., thyroid disease), low dosage, etc. [2]. It is unclear if TRD is a particularly malignant form of depression with its own pathophysiology, or if treatment-related changes in brain metabolism are different than those found in treatment-responsive depression [3]. Patients with TRD are at increased risk of relapse [4]. Also, most TRD patients have numerous psychiatric comorbidities inherently raising potential confounds with diagnosis [5–8].
The STAR*D trial documents TRD is a frequent occurrence and a serious problem in psychiatry afflicting about 30% of patients [4]. In terms of disease burden, it is second only to back pain in terms of life-years of disability [9]. The high significance of TRD has prompted an aggressive search for novel, more effective treatments including new classes of antidepressants (e.g., glutamatergic receptor antagonists, neuroactive steroids), add-on treatments (drug combinations, boosters such as lithium or liothyronine, atypical neuroleptics, mood stabilizers), and devices for neuromodulation (e.g., transcranial magnetic stimulation, TMS; vagus nerve stimulation, VNS; deep brain stimulation, DBS, direct current stimulation, DCS).
Despite the clinical importance of TRD, few studies have examined its biology and treatment. Several challenges have hindered such research. The recruitment of TRD patients is difficult. These patients are likely heterogenous in pathology, have numerous comorbidities, and are quite ill with significant risk for suicide. Their cross-sectional physiology may be confounded by the many previous treatment trials. At best, the medley of ineffective medications needs wash out, but this may lead to potential withdrawal symptoms or symptom worsening. Encouragement to undergo yet another treatment after so many failed trials becomes paramount. These patients need frequent follow-up and clinician availability. Despite these impediments, some work has been done using 18F-fluorodeoxyglucose positron emission tomography (FDG PET) in those with TRD [10–18]. However, not only does the biology of TRD, if homogeneous, remain unclear, but also no biomarkers predicting treatment resistance have reached clinical utility for this group of patients.
Past neuroimaging studies of treatment-responsive depression have highlighted the amygdala and subgenual anterior cingulate cortex (sgACC) as key nodes of depression-related circuity showing reduction in activity with successful treatment (see reviews [19–21]), although there are exceptions (e.g., no sg ACC change [22]; no amygdala change [23]). Studies have suggested several features may characterize TRD such as sgACC hyperactivity, amygdala hyperactivity, prefrontal/thalamic dysconnectivity, habenular connectivity, prefrontal hypoactivity, and hippocampal subfield volumes [10, 13, 14, 24–26]; however, consensus is yet to be achieved.
To our knowledge, there are no prior studies of brain metabolism in TRD patients with drug washout to establish a baseline examined both before and after a full trial of a combination antidepressant drug and atypical neuroleptic. Yet, the combination of antidepressant and atypical neuroleptic is being used increasingly throughout the world to treat TRD. The present study is of necessity preliminary, as no prior data existed with which to power the sample size or even to determine its feasibility.
The focus of this work rests on the amygdala and sgACC regions based on extensive prior literature. For example, unmedicated depressed patients have hypermetabolic amygdalae at rest [20]; decreased amygdala volume that correlates with depression severity [27, 28]; increased amygdala reactivity to sensory stimuli even without conscious awareness [29, 30]; amygdala reactivity prognostic of response to cognitive therapy [31]; sustained amygdala responses to negative words [32]; and disrupted functional connectivity[33–36].
The amygdala is densely connected both anatomically and functionally to the sgACC [37–39]. Depressed patients can show focal atrophy in the sgACC [21, 40–42]. Both hyperactivity and hypoactivity in the sgACC of depressed patients at rest have been reported [10, 21, 40]. Several antidepressant treatments decrease activity in the sgACC (e.g., SSRI, [23]; antidepressant placebo response [43]; DBS [10]; electroconvulsive therapy, ECT [44]; and VNS [17, 18]. DBS of tracts to the amygdala are neurosurgical targets for the treatment of refractory depression [45]. Greater efficacy of transcranial magnetic stimulation was associated with anticorrelated activity between the dorsolateral prefrontal cortex and sgACC [46]. Of note, healthy subjects’ ratings of negative affectivity during the prior month correlated with activity in the sgACC [47].
Given these a priori targets, this cohort observational study sought to test feasibility and to characterize regional brain metabolism in TRD before and after adequate treatment with a combination of an atypical neuroleptic (olanzapine) and fluoxetine (O/F), a selective serotonin reuptake inhibitor (SSRI) antidepressant. Use of these drugs in combination will be referred to hereafter as O/F.
This drug combination was the first drug approved by the USA Food and Drug Administration in 2009 specifically for the indication of TRD [48]. There have been several clinical trials, reviews, and meta-analyses examining the efficacy of O/F for TRD; that discussion is beyond the scope of this study [49–56]. Originally, use of O/F was based on preclinical work. Neurobiological changes associated with O/F dosing in rats include increased prefrontal monoamine levels [57, 58] and suppression of limbic immediate-early gene expression [59] relative to olanzapine or fluoxetine alone. No differential effects on limbic neurogenesis were found using O/F, whereas the individual drugs are associated with neurogenesis [60]. Whereas higher doses of O/F increased levels of neurotrophin-3 selectively in rat prefrontal cortex, low O/F doses or higher doses of olanzapine or fluoxetine administered individually did not [61]. These animal findings suggest some unique effects of O/F therapy not accounted for by the actions of the individual drugs.
The aim of the present work was not to assess efficacy or health outcomes in a clinical trial, as this has been reported previously (see above). Rather, the project’s purpose was to use imaging to bear on the question of mechanisms. Whether such combination treatments for TRD follow similar metabolic effects to other antidepressants in treatment-responsive depression is unknown. In addition, the individual TRD patient’s deviation from a normative database indicate for the first time the potential changes in regional brain metabolism in an individual, unmedicated, TRD patient. Such data could address preliminarily whether sgACC hypermetabolism or other biomarker is characteristic of TRD, a key issue in patient selection for future treatment trials of TRD.
Materials and methods
Participants
Twenty-five participants with severe TRD were enrolled. They had many psychotherapy and medication trials, some even failing convulsive therapy. They all had a longstanding chronic illness lasting many years. Most had comorbid psychiatric disorders. They were recruited and enrolled through referral from physicians’ outpatient clinics known to specialize in the treatment of TRD (co-authors: DA, BR, FSA). The principal inclusion criterion was severe, refractory major unipolar depressive disorder (Scheduled Clinical Interview for Diagnostic and Statistical Manual-IV; SCID [62]) as the primary diagnosis. Exclusion criteria included a lifetime history of cognitive impairment, psychosis, bipolar disorder, drug dependence, pregnancy, as well as any clinically significant findings on magnetic resonance imaging. All subjects provided written informed consent as approved by the VA Institutional Review Board (IRB) and the Radioactive Drug Research Committee (RDRC) approved by the FDA.
Treatment
Patients’ polypharmacy was tapered with washout for two weeks before the baseline measurement of glucose uptake using FDG PET as described previously [63]. They were then titrated to the maximal tolerated dose of fluoxetine (≤ 60 mg) and olanzapine (≤ 30 mg). The use of the combination of an SSRI such as fluoxetine and an atypical neuroleptic such as olanzapine is a standard of care in the management of patients with TRD. The maximal tolerated dose was held constant for eight weeks except for rescue medication of low dose benzodiazepine or short acting hypnotics for severe anxiety or insomnia. Given the seriousness of the illness, risk for suicide, and focus on mechanisms rather than efficacy, the study had no placebo control medication. Patients were seen either weekly or every two weeks (depending on stability) during wash out and treatment. Compliance was checked by counting pills every 1–2 weeks. Side effects were evaluated with open-ended questions without checklists typical of clinical trials. After treatment with O/F for eight weeks and PET imaging, they were returned to their referring psychiatrist for continued assessment and follow-up.
Clinical assessments
All subjects were assessed by their referring physician as having TRD as their primary diagnosis. Medical records were reviewed to ensure all subjects had at least two trials of antidepressants from different classes with adequate doses and duration of treatment (at least stage III TRD [1]). All subjects underwent structured diagnostic interviews using the SCID-1, Clinician Version [64]. The primary outcome measure was the change in Montgomery-Asberg Depression Rating Scale (MADRS [65]) score after eight weeks of treatment. The MADRS has good psychometric properties. The inter-rater reliability (concordance in score between a pair of independent raters) as measured by the intraclass correlation is 0.86 [66]. The internal consistency reliability (i.e., intra-observer reliability) using test/re-test method (clinical status between tests considered constant; i.e., stability over time) had an intraclass correlation of 0.78 [67]. As is standard for assessing responses to antidepressant interventions [68], a clinical response was defined a priori as a greater than or equal to 50% drop in depression score, while a remission was defined a priori as a MADRS of less than or equal to 8. Anxiety was scored with the Hamilton Anxiety Scale (HAMA [69]). Additional testing not directly pertinent to the present study included Clinical Global Impression Scale (CGI [70]), Mini-Mental Status Exam (MMSE [71]), Shipley Institute of Living Scale [72], Edinburgh Handedness Inventory [73], Profile of Mood States (POMS) [74], and Positive Affect Negative Affect Scale (PANAS [75]).
Positron emission tomography
Patients were scanned after washout (pre-treatment or baseline) and after completion of the eight weeks of treatment at maximal tolerated dose (post-treatment). Participants fasted for at least six hours before imaging; blood glucose was checked immediately before scanning. The relative regional glucose uptake was measured by injecting intravenously a bolus of 18F-FDG in saline at a dose of 185 MBq (5 mCi)/70 kg. They rested for 50 minutes during tracer uptake with eyes closed and ears open in a dimly lit, quiet room while being monitoring for wakefulness. The scanner was a Siemens (Knoxville, TN, USA) ECAT EXACT 47 operated in 2-D mode with septae extended. After measured attenuation, counts were collected during an emission scan lasting 20 minutes. Data were corrected for scatter, decay, randoms, and electronic deadtime. Images were reconstructed using filtered backprojection to a resolution of approximately 12 mm full width at half maximum.
Image analysis
Image analysis followed routine procedures including normalization for whole-brain activity, intersubject non-linear stereotactic averaging, subtraction of pre- from post-treatment activity, and statistical parametric mapping with regression for age using Neurostat software [76]. Parametric maps were overlaid on a template MRI blurred to a similar resolution as the PET scan. In-house software (iiV, http://james.psych.umn.edu/iiV/) was used to display results on a standard MRI template [77]. To explore individual TRD patient’s baseline metabolism, each patient was contrasted with our normative database (N = 30) [63]. For the purposes of display, the individually warped t images used an uncorrected magnitude threshold of P = .05.
Regions of interest
Two ROIs were examined based upon existing, extensive literature: amygdala and sgACC (see Introduction and Fig 1). The amygdala ROI (Fig 1A) consisted of a sphere of 13 mm diameter center on each amygdala in the atlas of Talairach and Tournoux at coordinates (±23, -4, -16) [78]. Mean counts were collected for each ROI from the pre- and post- treatment scans for each patient. The percent change in MADRS score was regressed linearly against the mean amygdala activity. Paired t-tests were used to compare mean amygdala counts before and after treatment for the group and for responders vs. non-responders separately. A threshold of P < .05 was used for the ROI analysis.
Fig 1. Regions of interest.
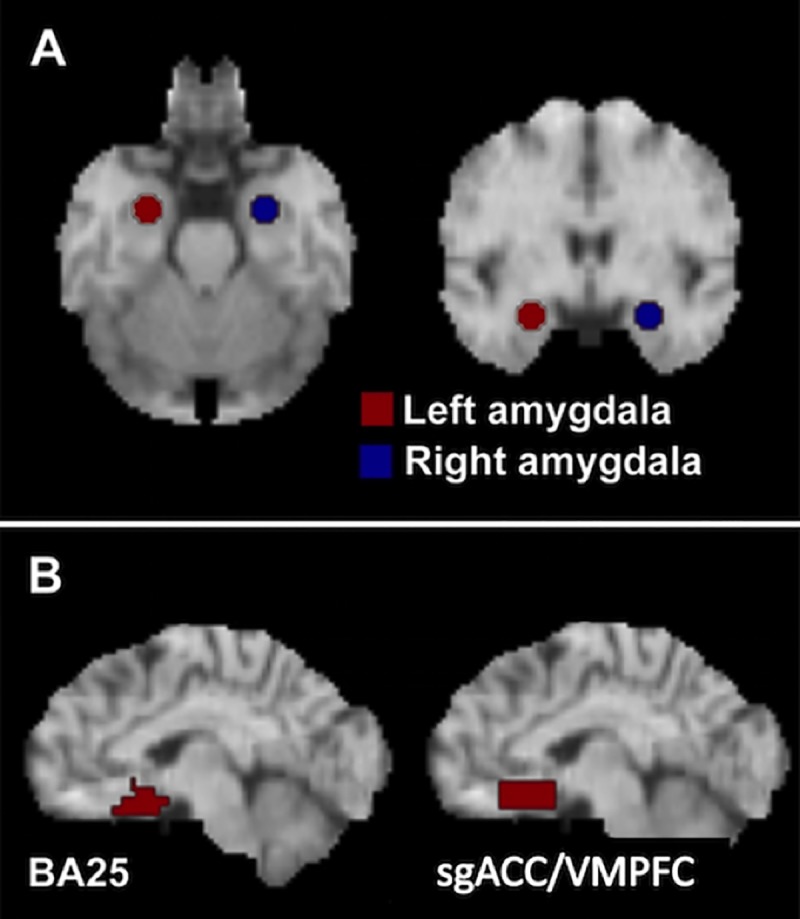
(A) Amygdala. (B) sgACC/VMPFC.
Based upon an a priori focus on the sgACC, we defined two additional subregions within sgACC for this analysis. Previous studies point to changes in subgenual metabolism that are not restricted to the sgACC of Brodmann area 25 (BA25) but extend along the ventromedial cingulate cortex [10, 17, 18, 40, 44, 46, 79]. So, a region including only those voxels labeled as BA25 by the atlas of Talairach and Tournoux [78] was created using the Talairach Daemon (http://ric.uthscsa.edu/projects/talairachdaemon.html) [80]. A second, less specific region was drawn as a cuboid on each hemisphere with the following extents measured from the anterior commissure: x, ±1–12 mm; y, 10–25 mm; z, -5 to -16 mm [78]. This approximated the region of hypometabolism associated with antidepressant treatment reported previously by our laboratory [18]. The region encompasses BA25, as well as portions of BA32 and BA33 and will be referred to as subgenual/VMPFC (Fig 1B).
One additional unplanned ROI was included post hoc because of its proximity to the amygdala, involvement in depression, and similar response to treatment in published work [22]. A 13 mm diameter spherical ROI was centered on the hippocampus at the following Talairach coordinates: x, ±27 mm, y, -23 mm; z, -9 mm or MNI (±27, -22, -0) http://sprout022.sprout.yale.edu/mni2tal/mni2tal.html.
Statistical analyses
Clinical changes before and after treatment were assessed with paired t-tests. First for image analysis, whole-brain voxel-wise changes in metabolism were measured with statistical parametric mapping using Neurostat software with a statistical threshold of Z = 3.3 as described previously to account for multiple testing [81]. Second, mean counts from each ROI were described pre- and post- treatment for responders and non-responders using paired t-tests. Percent-change in mean ROI metabolism was linearly regressed against percent-change in MADRS across all subjects. Third, a repeated measures ANOVA was performed on the amygdala, VMPFC, and head of the hippocampus ROIs as defined above. Extensive prior literature highlights these regions as important in affective illness. The BA25 region was not included as no change in activity occurred with treatment (see below). The dependent measure was glucose uptake (PET counts). Repeated measures included TIME (Pre-treatment, Post- treatment), ROI (amygdala, hippocampus, and VMPFC), and SIDE (right hemisphere, left hemisphere). Fourth, the correlation matrix for glucose uptake across amygdala, VMPFC, and hippocampus was calculated for exploratory purposes only (S2 Table).
Results
Clinical response
Of the 25 enrolled subjects, 16 were withdrawn because of failure to meet inclusion/exclusion criteria on further investigation or inability to complete the full study. Drug wash out led frequently to increased insomnia, anxiety, and depression. Six specific reasons that arose for a consensus by both patient and clinician to terminate included the following: adverse event probably related to olanzapine (lower extremity edema); adverse event probably related to olanzapine (severe sedation); spontaneous remission during washout with patient deciding to not restart medications; severe hyperlipidemia that could be aggravated by olanzapine; lack of any response with patient deciding to discontinue trial; and severe back discomfort during first PET scan related to previous musculoskeletal injury. Side effects from O/F observed reflected those commonly seen with this drug combination [49]. There were no suicide attempts during the study. Nine participants completed the entire protocol (clinical MRI; drug washout; O/F treatment; Pre- and Post-treatment PET scans). Clinical data for completers are shown in Table 1 which includes demographics, gender, family history of depression, illness onset, comorbidities (both current and lifetime), failed treatments, and response designation. The HAMA and MADRS scores as well as weights before and after treatment are displayed in S1 Table and S1 Data. The average tolerated dose was 39 mg (range 30–45 mg) of fluoxetine and 12 mg (range 10–12 mg) of olanzapine. Their weight increased significantly during treatment (S1 Table; S1 Fig); there was no interaction between time (pre vs post) and response (P = .20). The average baseline MADRS score was 31 (SD 5; range 24–38); no significant differences arose in baseline MADRS score between responders vs. non-responders (P = .63; not shown). Completers showed a decrease in MADRS score following eight weeks of treatment (Mean, 12; SD, 5; S1 Table). The baseline HAMA did not differ between responders vs. non-responders (P = .72). The HAMA declined significantly also after treatment (t(8) = 4.7; P = .002) with the significance driven by the non-responders (P = .006; responders, P = .13). Four patients responded; one of these remitted. Of note, responders tended to have fewer comorbidities and earlier onset than non-responders.
Table 1. Patient demographics and outcomes.
| Age ID # |
Sex | Family History of MDD | Life time Comorbidity | Current Comorbidity | Failed medications | Baseline MADRS | % Change | Response |
|---|---|---|---|---|---|---|---|---|
| 47 pL0009 pL0011 |
F | + | OCD, Anorexia, PD, Anxiety NOS, Dysthymia | SSRIs, venlafaxine, atypical neuroleptics, TCAs, mirtazapine, nefazodone, buproprion, ECT, anticonvulsants, buspirone | 33 | -6% | - | |
| 44 pL0020 pL0021 |
M | + | PD, Dysthymia | SSRIs, venlafaxine, mirtazapine, benzodiazepines | 29 | -17% | - | |
| 52 pL0025 pL0027 |
M | unknown | SSRIs, venlafaxine, lithium | 37 | -22% | - | ||
| 36 pL0028 pL0029 |
M | + | OCD, ADD | SSRIs, venlafaxine, TCA, MAOI, T3, stimulants, dopamine agonist, anticonvulsants | 27 | -26% | - | |
| 62 pL0030 pL0031 |
F | + | SSRIs, venlafaxine, anticonvulsant, atypical neuroleptic | 29 | -59% | + | ||
| 54 pL0059pL0069 |
M | + | SSRIs, venlafaxine, lithium, buspirone, TCA, anticonvulsants | 24 | -83% | + (remitted) |
||
| 61 pL0071 pL0072 |
M | + | OCD, ADD, dysthymia | SSRIs, venlafaxine, buproprion, benzodiazepine, stimulants, T4, nefazodone | 31 | -35% | - | |
| 27 pL0079pL0087 |
M | + | ADHD | GAD | SSRIs venlafaxine, atypical neuroleptic, mirtazapine | 38 | -50% | + |
| 41 pL0089 pL0095 |
M | + | SSRIs, venlafaxine, atypical neuroleptic | 28 | -64% | + |
M, male; F, female; MDD, major depressive disorder, OCD, obsessive compulsive disorder; ADD, attention deficit disorder; ADHD, attention deficit disorder with hyperactivity; PD, personality disorder; NOS, not otherwise specified; GAD, generalized anxiety disorder; SSRI, selective serotonin reuptake inhibitor; TCA, tricyclic antidepressant; ECT, electroconvulsive therapy; MAOI, monoamine oxidase inhibitor; T3, liothyronine;T4, levothyroxine; MADRS, Montgomery Asberg Depression Rating Scale
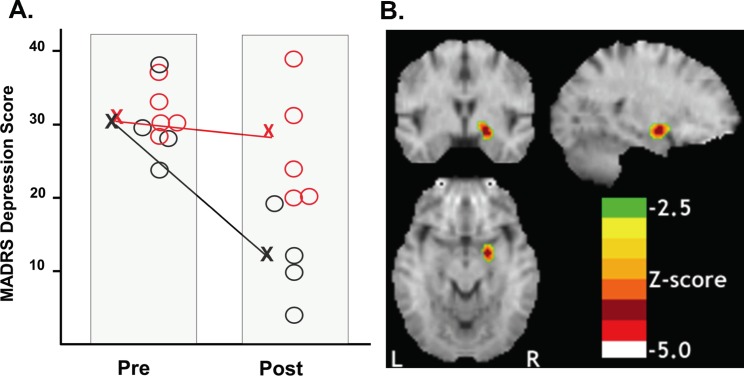
A 2 x 2 ANOVA with Treatment-response (responder vs. non-responder) as the between-subject factor and Time (post vs. pre-test) as the within-subject factor demonstrated a main effect of Time (F(1,7) = 195.2, P < .001), confirming that MADRS scores decreased significantly across sessions (Fig 2A). The interaction of Treatment-response X Time was also significant (F(1,7) = 43.9 P < .001). This interaction confirmed that responders showed significantly greater reductions in MADRS scores than non-responders.
Fig 2. Changes in depression ratings and regional glucose uptake before and after treatment.
(A) Individual MADRS scores of the responders and non-responders before and after treatment. (N = 9). Non-Responders, red circle; responders, black circle. X denotes group means. (B) Right amygdala metabolism in the brain of responders following olanzapine/fluoxetine treatment was the only significant decrease in the whole-brain voxelwise analysis. Upper left section, coronal; lower section, transverse; upper right section, sagittal.
Whole-brain exploratory image analysis
Voxel-wise comparisons of patients’ post- and pre-treatment scans revealed significant changes (Table 2; S2–S4 Figs). Patients were grouped as responders and non-responders (see above) to identify metabolic change associated with successful treatment.
Table 2. Significant changes in whole-brain voxelwise analysis.
| X (mm) | Y (mm) | Z (mm) | Z-score | Region |
|---|---|---|---|---|
| All patients | ||||
| 12 | -35 | 54 | +3.4 | R paracentral lobule |
| 6 | -60 | 43 | +3.3 | R precuneus (BA7) |
| -12 | -60 | -20 | -4.6 | L Cerebellum |
| 17 | -94 | -4 | -3.7 | R Lingual Gyrus (BA18) |
| 28 | 14 | -20 | -3.6 | R Inferior Frontal Gyrus (BA47) |
| -15 | -33 | 7 | -3.6 | L Thalamus |
| -37 | -64 | -22 | -3.5 | L Cerebellum |
| 30 | -49 | -27 | -3.4 | R Cerebellum |
| -12 | -10 | 0 | -3.4 | L Thalamus |
| 10 | -1 | -4 | -3.3 | R globus pallidus |
| Non-responders | ||||
| -8 | -60 | -16 | -5.2 | L Cerebellum |
| 8 | -49 | -29 | -4.6 | R Cerebellum |
| -17 | -53 | 29 | -4.4 | L Cingulate Gyrus (BA31) |
| -44 | 32 | 7 | -3.9 | L Inferior Frontal Gyrus (BA45) |
| -10 | -10 | 2 | -3.9 | L Thalamus |
| 17 | -91 | -2 | -3.7 | R Lingual Gyrus (BA17) |
| -51 | -67 | 14 | -3.7 | L Middle Temporal Gyrus (BA39) |
| -21 | -73 | -18 | -3.7 | L Cerebellum |
| 1 | -19 | -16 | -3.4 | R Midbrain |
| -42 | -4 | 38 | -3.4 | L Precentral Gyrus (BA6) |
| Responders | ||||
| -48 | -13 | 2 | +3.5 | Left Superior Temporal Gyrus (BA22) |
| -53 | -24 | 18 | +3.4 | Left Post-Central Gyrus (BA40) |
| 6 | -49 | 36 | +3.3 | Right Precuneus (BA31) |
| 10 | -58 | 38 | +3.3 | Right Precuneus (BA7) |
| 19 | -1 | -7 | -4.4 | Right Dorsal Amygdala |
R, right; L, left; BA, Brodmann area
Responders showed increases in the left superior temporal and post-central gyri and right precuneus. Significantly reduced metabolism was confined to a peak in the right amygdaloid complex (see Fig 2B). Of note, liberalizing the threshold to P = .05 (uncorrected) revealed bilateral amygdala deactivations. Non-responders showed no significant increases in metabolism following treatment. Areas of reduced metabolism after treatment were found in non-responders in the bilateral cerebellum, lingual gyrus, middle temporal gyrus, thalamus, midbrain, and dorsal cingulate gyrus (see Table 2). For all patients as a group, no significant changes occurred in limbic structures in the whole-brain image analysis.
No studies have reported on individual metabolic patterns associated with unmedicated TRD. To explore this variability while accepting the limitation of the risk for false positive or negative responses, each TRD subject’s baseline warped FDG PET (i.e., after medication washout or baseline) was contrasted with those of a normative database with threshold set at t = 2.0 for visualization as performed previously [63]. These individual subtractions for the nine completers are shown in S5 Fig including both increases and decreases in metabolism. Examination of individual subject’s scans showed considerable heterogeneity in baseline scans with a mixture of positive, negative, or null changes in the BA25/VMPFC region. This variability suggests baseline heterogeneity in TRD or metabolic changes related to the previous history of failed treatments for TRD. If any antidepressant response occurred, a relationship to metabolic signature was not evident.
Region of interest analyses
ANOVA on amygdala, hippocampus, and VMPFC
The repeated measures ANOVA indicated significant main effects of TIME (F(1,8) = 5.992, P = .04) and ROI (F(2,16) = 24.94, P = .001) without significant interaction effects (S6 Fig; S2 Data). This result indicates that O/F reduces activity in all three ROIs. To explore potentially interesting relationships given the large number of comparisons, the analysis of the correlation matrix for the ROIs reached significance only for the correlation between the left and right sgACC post-treatment (r = .82, P = .007; S2 Table). O/F tended to increase each region’s inter-hemispheric functional connectivity compared to baseline.
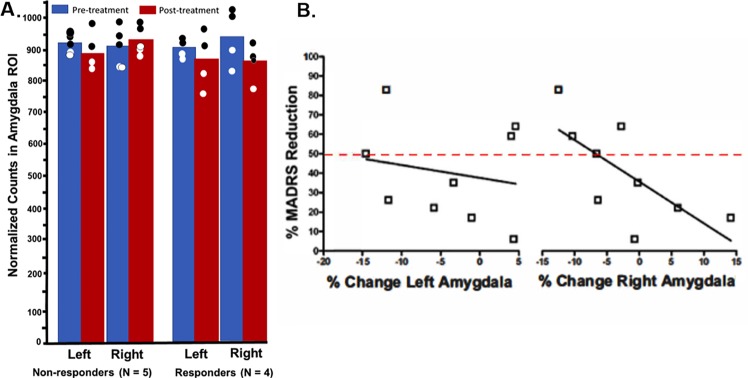
Amygdala region
Responders showed a significant reduction in mean glucose metabolism in the right amygdala ROI (t(3) = 3.38, P = .04), while non-responders showed no change with treatment (t(4) = -0.68, P = .54) (Fig 3A). There was no change in left amygdala metabolism in either group (responders: t(3) = 0.88, P = .45; non-responders: t(4) = 1.29, P = .28) (Fig 3A). Regression analyses showed no correlation between percent reduction in left amygdala metabolism and percent-reduction in MADRS scores across all subjects (Fig 3B, r = -.20, P = .61). This correlation was significant in the right amygdala (Fig 3B, r = -.70, P = .036). Because the hippocampus is near the amygdala and the resolution of PET in this study is low, the post hoc hippocampal region was also examined for changes in activity.
Fig 3. Changes in amygdala glucose uptake before and after treatment and its relationship to depression symptoms.
(A) Amygdala metabolism examined separately for responders vs. non-responders in the right and left amygdala before and after treatment. Blue denotes pretreatment; red denotes post-treatment. (B) Correlation between percentage change in MADRS scores and change in amygdala metabolism. Only the right amygdala showed a significant correlation between change in metabolism and change in MADRS scores. Red line identifies threshold for response.
Exploratory subgenual regions (BA 25 & sgACC/VMPFC)
Paired t-tests revealed no changes with treatment in either the left or right BA25 metabolism in either responders (left: t(3) = 0.05, P = .97; right: t(3) = 0.71, P = .53) or non-responders (left: t(4) = 1.13, P = .32; right: t(4) = 0.67, P = .54). Changes in left or right BA25 metabolism showed no correlation with changes from baseline MADRS (left: r = .29, P = .45; right: r = .15, P = .69). However, baseline right hemisphere BA25 metabolism showed a marginally significant correlation with change from baseline MADRS, whereby higher baseline metabolism predicted better response to O/F therapy (r = 0.68, P = .05). This correlation was not significant in the left hemisphere (r = 0.13, P = .74).
Paired t-tests revealed a significant decrease in right but not left VMPFC metabolism in responders (left: t(3) = 0.07, P = .95; right: t(3) = 4.18, P = .02), and no significant change in VMPFC metabolism in non-responders (left: t(4) = 0.81, P = .47; right: t(4) = 0.53, P = .62). Changes in VMPFC metabolism showed no correlation with change in MADRS (left: r = .11; P = .77; right: r = .18, P = .64). Baseline metabolism in the right, but not left, VMPFC area correlated with MADRS reduction, with higher baseline metabolism predicting better response (left: r = 0.37, P = .33; right: r = .84, P = .018).
Discussion
This preliminary study found that medication-free TRD patients treated with O/F at therapeutic doses for an adequate duration showed a response-related decline in the metabolism of the right dorsal amygdala using a whole-brain, voxel-wise analysis. The dorsal amygdala in humans consists mostly of the central nucleus, the terminus of the spino-parabrachial-amygdaloid pain pathway and the principal efferent pathway for the emotional and physiological processing. Given the low resolution of the present study, caution is warranted in localization pending higher resolution techniques (e.g., higher resolution PET scanners and coregistered high resolution MRI). Several increases in metabolism surfaced also after treatment.
Two regions of interest (and one post-hoc region) based on existing literature were examined for drug-related changes in metabolism and relationship to response (see citations in Introduction). Following treatment, the change in metabolism of the right amygdala correlated with the change in MADRS score; no correlation was observed for the left amygdala. Treatment did not significantly change the smaller sgACC region defined as BA25. However, a broader ROI along the VMPFC approached significance despite the small sample size.
ANOVA of ROIs in the VMPFC, amygdala, and immediately adjacent hippocampus (a post hoc exploratory ROI) indicated a main effect of treatment and ROI without significant interactions. The VMPFC showed the highest activity. O/F was associated with reduced activity in all ROIs tested. The hippocampus did not appear responsible for the deactivation seen in the dorsal amygdala. However, the hippocampus may have followed similar changes with treatment that did not reach significance; such changes have been reported previously [22, 44].
Baseline metabolism in TRD may have relevance to treatment response and may, if confirmed, find utility for patient selection in treatment trials. Greater baseline metabolism in right BA25 and sgACC/VMPFC predicted better response to O/F therapy. Also, responders showed a significant decrease in metabolism following treatment in the right VMPC region which could reflect a higher initial baseline (as BA25 was included in the right VMPFC region). The higher baseline BA25 metabolism in responders to O/F may relate to 1) higher baseline resting sgACC/VMFPC blood flow seen in TRD patients when compared to controls during neuromodulation trials [10, 11]; 2) increased sgACC blood flow induced by sadness induction [82]; and 3) and increased resting blood flow in sgACC/VMFPC in healthy subjects high in negative affect [47]. Likewise, the decline in right VMPFC activity in TRD treated with O/F is analogous to the decline in resting blood flow in VMPFC in TRD responders treated with deep brain stimulation [10] as well as decreased VMPFC metabolism with chronic vagus nerve stimulation [17, 18].
Strengths of the study include the recruitment of severely ill TRD patients, medication washout before treatment, exploratory examination of individual TRD patients, and full course of treatment with O/F to maximal tolerated doses. These preliminary data suggest heterogeneity in metabolic signatures in TRD. If replicated, this heterogeneity requires consideration in the design of trials for TRD using medications or devices. However, the changes observed with treatment appear broadly like those reported in treatment-responsive major depression with other antidepressant treatments: decreased amygdala and VMPFC metabolism.
Limitations of this study include comorbidities, prior heterogeneous treatments during past failed trials, significant participant dropout, small final sample size, lack of a placebo, low PET resolution, multiple testing with potential for alpha error inflation, and confounding of depression with anxiety measures. Patient dropouts and comorbidities could limit generalizability. However, the whole brain analysis used a conservative threshold to address the large number of voxels in the brain, and the amygdala finding converges with the literature making a spurious finding unlikely. Most TRD patients do have comorbidity [5–8]. A larger replication sample could address whether major comorbidities represent a covariate of interest in the response as suggested by this study—likewise for dropouts. Future studies will need to account for the dropout during washout. The limited resolution of PET places some ambiguity in the precise determination of amygdala activity. However, the latest scanners with resolution of 3 mm full width at half maximum will improve localization in future studies. Of note, although the ROI analysis of the right amygdala confirmed significant deactivation after treatment that correlated with clinical response, the focus was only partially resolved from other nearby regions which showed a similar response pattern (e.g., hippocampus). Depression and anxiety are both prominent symptoms in TRD, and antidepressants/atypical neuroleptics often decrease both depression and anxiety scores. In this regard, HAMD and HAMA scores are inter-correlated [83]. Anxiety scores measured in this study in responders before and after treatments did not differ. Therefore, the decrease in amygdala activity does not likely reflect changes in anxiety, but rather depression. The severity of illness and risk of suicide precluded a placebo control. However, other studies using FDG PET and placebos in test-retest designs suggest high consistency in normalized regional activity and only small changes [84–86].
Conclusions
TRD patients show considerable baseline metabolic heterogeneity following medication washout. Whether this heterogeneity arises from differing disease pathologies or from effects of past treatments remains unclear. As reported for other antidepressant therapies in treatment-responsive depression, decline in amygdala and VMPFC activity surfaced here with O/F treatment. Furthermore, decreased metabolism in the right amygdala with treatment correlated with improvement in depression following O/F treatment.
Supporting information
(PDF)
Stereotactically normalized. Image left is right side of brain. AC-PC plane 0 mm. Color scale shows Z-scores with threshold Z = ±3.3.
(PDF)
Stereotactically normalized. Image left is right side of brain. AC-PC plane 0 mm. Color scale shows Z-scores with threshold at Z = ±3.3.
(PDF)
Stereotactically normalized. Image left is right side of brain. AC-PC plane 0 mm. Color scale shows Z-scores with threshold at Z = ±3.3.
(PDF)
For visualizing individual metabolic fingerprints of all nine subjects, the threshold was set at t = 2.0 that is the usual threshold used for studying change in individuals [42]. Each subject is represented by a study number (e.g., pL0009). Age regression was used to match individual subject’s age to that of the normative group. R, right; L, left, A, anterior; P, posterior. The patterns are heterogenous. For example, some individuals have sgACC/VMPFC hypoactive, hyperactivity, or no change.
(PDF)
(PDF)
(PDF)
Green cells below diagonal are for Pre-treatment; blue cells above diagonal are for Post-treatment. R, right; L, left; Hippo, hippocampus; sgACC, subgenual anterior cingulate/VMPFC. † P = .007
(PDF)
(PDF)
(PDF)
Acknowledgments
This work was supported through an Investigator-Initiated Grant from Eli Lilly & Company and the Department of Veterans Affairs (I01CX000501). A fixed dose of olanzapine and fluoxetine combination with trade name Symbyax has been approved by the USA Food and Drug Administration with indications for TRD and bipolar I depression. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript. We thank Hemant Shah for assistance in data collection and thank the volunteers for their patience and perseverance.
Data Availability
The minimal data set with the raw data used for the figures and tables is in the Supporting Information files as "Supplementary Information w data.pdf." Parties interested in data sharing policies should contact the Minneapolis Veterans Health Care System IRB (IRBMN@va.gov) to establish a data use agreement. This does not alter our adherence to PLOS ONE policies on sharing data and materials. The authors of the present study had no special access privileges in accessing data from the Minneapolis Veterans Health Care System which other interested researchers would not have.
Funding Statement
This work was supported by JVP (PI) Department of Veterans Affairs, I01CX000501, www.minneapolis.va.gov; JVP (PI); Eli Lilly & Co.; lilly.com; The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Thase ME, Rush AJ. When at first you don't succeed: Sequential strategies for antidepressant nonresponders. J Clin Psychiatry. 1997;58 Suppl 13:23–9. [PubMed] [Google Scholar]
- 2.Nemeroff CB. Prevalence and management of treatment-resistant depression. J Clin Psychiatry. 2007;68 Suppl 8:17–25. [PubMed] [Google Scholar]
- 3.Fagiolini A, Kupfer DJ. Is treatment-resistant depression a unique subtype of depression? Biol Psychiatry. 2003;53(8):640–8. 10.1016/s0006-3223(02)01670-0 [DOI] [PubMed] [Google Scholar]
- 4.Rush AJ, Trivedi MH, Wisniewski SR, Nierenberg AA, Stewart JW, Warden D, et al. Acute and longer-term outcomes in depressed outpatients requiring one or several treatment steps: A STAR*D report. Am J Psychiatry. 2006;163(11):1905–17. 10.1176/ajp.2006.163.11.1905 [DOI] [PubMed] [Google Scholar]
- 5.Rizvi SJ, Grima E, Tan M, Rotzinger S, Lin P, McIntyre RS, et al. Treatment-resistant depression in primary care across Canada. Can J Psychiatry. 2014;59(7):349–57. 10.1177/070674371405900702 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.De Carlo V, Calati R, Serretti A. Socio-demographic and clinical predictors of non-response/non-remission in treatment resistant depressed patients: A systematic review. Psychiatry Res. 2016;240:421–30. 10.1016/j.psychres.2016.04.034 [DOI] [PubMed] [Google Scholar]
- 7.Papakostas GI, Petersen TJ, Farabaugh AH, Murakami JL, Pava JA, Alpert JE, et al. Psychiatric comorbidity as a predictor of clinical response to nortriptyline in treatment-resistant major depressive disorder. J Clin Psychiatry. 2003;64(11):1357–61. 10.4088/jcp.v64n1112 [DOI] [PubMed] [Google Scholar]
- 8.Souery D, Oswald P, Massat I, Bailer U, Bollen J, Demyttenaere K, et al. Clinical factors associated with treatment resistance in major depressive disorder: Results from a European multicenter study. J Clin Psychiatry. 2007;68(7):1062–70. 10.4088/jcp.v68n0713 [DOI] [PubMed] [Google Scholar]
- 9.GBD 2015 Disease and Injury Incidence and Prevalence Collaborators (Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. ). Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990–2015: A systematic analysis for the global burden of disease study 2015. Lancet. 2016;388(10053):1545–602. 10.1016/S0140-6736(16)31678-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mayberg HS, Lozano AM, Voon V, McNeely HE, Seminowicz D, Hamani C, et al. Deep brain stimulation for treatment-resistant depression. Neuron. 2005;45(5):651–60. 10.1016/j.neuron.2005.02.014 [DOI] [PubMed] [Google Scholar]
- 11.Dougherty DD, Weiss AP, Cosgrove GR, Alpert NM, Cassem EH, Nierenberg AA, et al. Cerebral metabolic correlates as potential predictors of response to anterior cingulotomy for treatment of major depression. J Neurosurg. 2003;99(6):1010–7. 10.3171/jns.2003.99.6.1010 [DOI] [PubMed] [Google Scholar]
- 12.Seminowicz DA, Mayberg HS, McIntosh AR, Goldapple K, Kennedy S, Segal Z, et al. Limbic-frontal circuitry in major depression: A path modeling metanalysis. Neuroimage. 2004;22(1):409–18. 10.1016/j.neuroimage.2004.01.015 [DOI] [PubMed] [Google Scholar]
- 13.Li CT, Wang SJ, Hirvonen J, Hsieh JC, Bai YM, Hong CJ, et al. Antidepressant mechanism of add-on repetitive transcranial magnetic stimulation in medication-resistant depression using cerebral glucose metabolism. J Affect Disord. 2010;127(1–3):219–29. 10.1016/j.jad.2010.05.028 [DOI] [PubMed] [Google Scholar]
- 14.Li CT, Su TP, Wang SJ, Tu PC, Hsieh JC. Prefrontal glucose metabolism in medication-resistant major depression. Br J Psychiatry. 2015;206(4):316–23. 10.1192/bjp.bp.113.140434 [DOI] [PubMed] [Google Scholar]
- 15.Li CT, Chen MH, Lin WC, Hong CJ, Yang BH, Liu RS, et al. The effects of low-dose ketamine on the prefrontal cortex and amygdala in treatment-resistant depression: A randomized controlled study. Hum Brain Mapp. 2016;37(3):1080–90. 10.1002/hbm.23085 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Conway CR, Chibnall JT, Gebara MA, Price JL, Snyder AZ, Mintun MA, et al. Association of cerebral metabolic activity changes with vagus nerve stimulation antidepressant response in treatment-resistant depression. Brain Stimul. 2013;6(5):788–97. 10.1016/j.brs.2012.11.006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Pardo JV, Sheikh SA, Schwindt GC, Lee JT, Surerus-Johnson C, Pardo PJ, et al. Functional neuroimaging in treatment-resistant depression. Depression: Mind and Body. 2007;3(2):57–70 https://pdfs.semanticscholar.org/f975/b867629c541e404216caa92980707beb28c8.pdf. [Google Scholar]
- 18.Pardo JV, Sheikh SA, Schwindt GC, Lee JT, Kuskowski MA, Surerus C, et al. Chronic vagus nerve stimulation for treatment-resistant depression decreases resting ventromedial prefrontal glucose metabolism. Neuroimage. 2008;42(2):879–89. 10.1016/j.neuroimage.2008.04.267 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Mayberg HS. Targeted electrode-based modulation of neural circuits for depression. J Clin Invest. 2009;119(4):717–25. 10.1172/JCI38454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Drevets WC. Neuroimaging abnormalities in the amygdala in mood disorders. Ann N Y Acad of Sci. 2006;985:420–44. [DOI] [PubMed] [Google Scholar]
- 21.Drevets WC, Savitz J, Trimble M. The subgenual anterior cingulate cortex in mood disorders. CNS Spectr. 2008;13(8):663–81. 10.1017/s1092852900013754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kennedy SH, Evans KR, Kruger S, Mayberg HS, Meyer JH, McCann S, et al. Changes in regional brain glucose metabolism measured with positron emission tomography after paroxetine treatment of major depression. Am J Psychiatry. 2001;158(6):899–905. 10.1176/appi.ajp.158.6.899 [DOI] [PubMed] [Google Scholar]
- 23.Mayberg HS, Brannan SK, Tekell JL, Silva JA, Mahurin RK, McGinnis S, et al. Regional metabolic effects of fluoxetine in major depression: Serial changes and relationship to clinical response. Biol Psychiatry. 2000;48(8):830–43. 10.1016/s0006-3223(00)01036-2 [DOI] [PubMed] [Google Scholar]
- 24.Li CT, Chen LF, Tu PC, Wang SJ, Chen MH, Su TP, et al. Impaired prefronto-thalamic functional connectivity as a key feature of treatment-resistant depression: A combined MEG, PET and rTMS study. PLoS One. 2013;8(8):e70089 10.1371/journal.pone.0070089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cao B, Luo Q, Fu Y, Du L, Qiu T, Yang X, et al. Predicting individual responses to the electroconvulsive therapy with hippocampal subfield volumes in major depression disorder. Sci Rep. 2018;8(1):5434 10.1038/s41598-018-23685-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Gosnell SN, Curtis KN, Velasquez K, Fowler JC, Madan A, Goodman W, et al. Habenular connectivity may predict treatment response in depressed psychiatric inpatients. J Affect Disord. 2019;242:211–9. 10.1016/j.jad.2018.08.026 [DOI] [PubMed] [Google Scholar]
- 27.Hamilton JP, Siemer M, Gotlib IH. Amygdala volume in major depressive disorder: a meta-analysis of magnetic resonance imaging studies. Mol Psychiatry. 2008;13(11):993–1000. 10.1038/mp.2008.57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Brown SSG, Rutland JW, Verma G, Feldman RE, Alper J, Schneider M, et al. Structural MRI at 7T reveals amygdala nuclei and hippocampal subfield volumetric association with major depressive disorder symptom severity. Sci Rep. 2019;9(1):10166 10.1038/s41598-019-46687-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Sheline YI, Barch DM, Donnelly JM, Ollinger JM, Snyder AZ, Mintun MA. Increased amygdala response to masked emotional faces in depressed subjects resolves with antidepressant treatment: an fMRI study. Biol Psychiatry. 2001;50(9):651–8. 10.1016/s0006-3223(01)01263-x [DOI] [PubMed] [Google Scholar]
- 30.Victor TA, Furey ML, Fromm SJ, Ohman A, Drevets WC. Relationship between amygdala responses to masked faces and mood state and treatment in major depressive disorder. Arch Gen Psychiatry. 2010;67(11):1128–38. 10.1001/archgenpsychiatry.2010.144 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Siegle GJ, Carter CS, Thase ME. Use of FMRI to predict recovery from unipolar depression with cognitive behavior therapy. Am J Psychiatry. 2006;163(4):735–8. 10.1176/appi.ajp.163.4.735 [DOI] [PubMed] [Google Scholar]
- 32.Siegle GJ, Steinhauer SR, Thase ME, Stenger VA, Carter CS. Can't shake that feeling: event-related fMRI assessment of sustained amygdala activity in response to emotional information in depressed individuals. Biol Psychiatry. 2002;51(9):693–707. 10.1016/s0006-3223(02)01314-8 [DOI] [PubMed] [Google Scholar]
- 33.Cullen KR, Westlund MK, Klimes-Dougan B, Mueller BA, Houri A, Eberly LE, et al. Abnormal amygdala resting-state functional connectivity in adolescent depression. JAMA Psychiatry. 2014;71(10):1138–47. 10.1001/jamapsychiatry.2014.1087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ramasubbu R, Konduru N, Cortese F, Bray S, Gaxiola-Valdez I, Goodyear B. Reduced intrinsic connectivity of amygdala in adults with major depressive disorder. Front Psychiatry. 2014;5:17 10.3389/fpsyt.2014.00017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ambrosi E, Arciniegas DB, Madan A, Curtis KN, Patriquin MA, Jorge RE, et al. Insula and amygdala resting-state functional connectivity differentiate bipolar from unipolar depression. Acta Psychiatr Scand. 2017;136(1):129–39. 10.1111/acps.12724 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Tang Y, Kong L, Wu F, Womer F, Jiang W, Cao Y, et al. Decreased functional connectivity between the amygdala and the left ventral prefrontal cortex in treatment-naive patients with major depressive disorder: a resting-state functional magnetic resonance imaging study. Psychol Med. 2013;43(9):1921–7. 10.1017/S0033291712002759 [DOI] [PubMed] [Google Scholar]
- 37.Price JL. Comparative aspects of amygdala connectivity. Ann N Y Acad Sci. 2003;985:50–8. 10.1111/j.1749-6632.2003.tb07070.x [DOI] [PubMed] [Google Scholar]
- 38.Senn V, Wolff Steffen BE, Herry C, Grenier F, Ehrlich I, Gründemann J, et al. Long-range connectivity defines behavioral specificity of amygdala neurons. Neuron. 2014;81(2):428–37. 10.1016/j.neuron.2013.11.006 [DOI] [PubMed] [Google Scholar]
- 39.Sharma KK, Kelly EA, Pfeifer CW, Fudge JL. Translating fear circuitry: Amygdala projections to subgenual and perigenual anterior cingulate in the macaque. Cereb Cortex. 2019. 10.1093/cercor/bhz106 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Drevets WC, Price JL, Simpson JR Jr., Todd RD, Reich T, Vannier M, et al. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386(6627):824–7. 10.1038/386824a0 [DOI] [PubMed] [Google Scholar]
- 41.Rajkowska G, Miguel-Hidalgo JJ, Wei J, Dilley G, Pittman SD, Meltzer HY, et al. Morphometric evidence for neuronal and glial prefrontal cell pathology in major depression. Biol Psychiatry. 1999;45(9):1085–98. 10.1016/s0006-3223(99)00041-4 [DOI] [PubMed] [Google Scholar]
- 42.Botteron KN, Raichle ME, Drevets WC, Heath AC, Todd RD. Volumetric reduction in left subgenual prefrontal cortex in early onset depression. Biol Psychiatry. 2002;51(4):342–4. 10.1016/s0006-3223(01)01280-x [DOI] [PubMed] [Google Scholar]
- 43.Mayberg HS, Silva JA, Brannan SK, Tekell JL, Mahurin RK, McGinnis S, et al. The functional neuroanatomy of the placebo effect. Am J Psychiatry. 2002;159(5):728–37. 10.1176/appi.ajp.159.5.728 [DOI] [PubMed] [Google Scholar]
- 44.Nobler MS, Oquendo MA, Kegeles LS, Malone KM, Campbell C, Sackeim HA, et al. Decreased regional brain metabolism after ECT. Am J Psychiatry. 2001;158(2):305–8. 10.1176/appi.ajp.158.2.305 [DOI] [PubMed] [Google Scholar]
- 45.Riva-Posse P, Choi KS, Holtzheimer PE, McIntyre CC, Gross RE, Chaturvedi A, et al. Defining critical white matter pathways mediating successful subcallosal cingulate deep brain stimulation for treatment-resistant depression. Biol Psychiatry. 2014. 76(12):963–9. 10.1016/j.biopsych.2014.03.029 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Fox MD, Buckner RL, White MP, Greicius MD, Pascual-Leone A. Efficacy of transcranial magnetic stimulation targets for depression is related to intrinsic functional connectivity with the subgenual cingulate. Biol Psychiatry. 2012;72(7):595–603. 10.1016/j.biopsych.2012.04.028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Zald DH, Mattson DL, Pardo JV. Brain activity in ventromedial prefrontal cortex correlates with individual differences in negative affect. Proc Natl Acad Sci U S A. 2002;99(4):2450–4. 10.1073/pnas.042457199 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Epstein LR. Symbyax: The first medication approved for treatment-resistant depression. Pharmanote. 2009;24(11):1–6. [Google Scholar]
- 49.Shelton RC, Williamson DJ, Corya SA, Sanger TM, Van Campen LE, Case M, et al. Olanzapine/fluoxetine combination for treatment-resistant depression: A controlled study of SSRI and nortriptyline resistance. J Clin Psychiatry. 2005;66(10):1289–97. 10.4088/jcp.v66n1012 [DOI] [PubMed] [Google Scholar]
- 50.Shelton RC, Tollefson GD, Tohen M, Stahl S, Gannon KS, Jacobs TG, et al. A novel augmentation strategy for treating resistant major depression. Am J Psychiatry. 2001;158(1):131–4. 10.1176/appi.ajp.158.1.131 [DOI] [PubMed] [Google Scholar]
- 51.Haridas RM, Parkar SR, Ghulam R, Amin G, Thombre KG, Srivastava A, et al. Olanzapine and fluoxetine combination in severe or resistant depression. Indian J Psychiatry. 2003;45(4):234–8. [PMC free article] [PubMed] [Google Scholar]
- 52.Bobo WV, Shelton RC. Efficacy, safety and tolerability of Symbyax for acute-phase management of treatment-resistant depression. Expert Rev Neurother. 2010;10(5):651–70. 10.1586/ern.10.44 [DOI] [PubMed] [Google Scholar]
- 53.Trivedi MH, Thase ME, Osuntokun O, Henley DB, Case M, Watson SB, et al. An integrated analysis of olanzapine/fluoxetine combination in clinical trials of treatment-resistant depression. J Clin Psychiatry. 2009;70(3):387–96. 10.4088/jcp.08m04064 [DOI] [PubMed] [Google Scholar]
- 54.Brunner E, Tohen M, Osuntokun O, Landry J, Thase ME. Efficacy and safety of olanzapine/fluoxetine combination vs fluoxetine monotherapy following successful combination therapy of treatment-resistant major depressive disorder. Neuropsychopharmacology. 2014;39(11):2549–59. 10.1038/npp.2014.101 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Luan S, Wan H, Wang S, Li H, Zhang B. Efficacy and safety of olanzapine/fluoxetine combination in the treatment of treatment-resistant depression: A meta-analysis of randomized controlled trials. Neuropsychiatr Dis Treat. 2017;13:609–20. 10.2147/NDT.S127453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Dodd S, Berk M. Olanzapine/fluoxetine combination for treatment-resistant depression: Efficacy and clinical utility. Expert Rev Neurother. 2008;8(9):1299–306. 10.1586/14737175.8.9.1299 [DOI] [PubMed] [Google Scholar]
- 57.Zhang W, Perry KW, Wong DT, Potts BD, Bao J, Tollefson GD, et al. Synergistic effects of olanzapine and other antipsychotic agents in combination with fluoxetine on norepinephrine and dopamine release in rat prefrontal cortex. Neuropsychopharmacology. 2000;23(3):250–62. 10.1016/S0893-133X(00)00119-6 [DOI] [PubMed] [Google Scholar]
- 58.Koch S, Perry KW, Bymaster FP. Brain region and dose effects of an olanzapine/fluoxetine combination on extracellular monoamine concentrations in the rat. Neuropharmacology. 2004;46(2):232–42. 10.1016/j.neuropharm.2003.09.001 [DOI] [PubMed] [Google Scholar]
- 59.Horowitz JM, Goyal A, Ramdeen N, Hallas BH, Horowitz AT, Torres G. Characterization of fluoxetine plus olanzapine treatment in rats: A behavior, endocrine, and immediate-early gene expression analysis. Synapse. 2003;50(4):353–64. 10.1002/syn.10276 [DOI] [PubMed] [Google Scholar]
- 60.Kodama M, Fujioka T, Duman RS. Chronic olanzapine or fluoxetine administration increases cell proliferation in hippocampus and prefrontal cortex of adult rat. Biol Psychiatry. 2004;56(8):570–80. 10.1016/j.biopsych.2004.07.008 [DOI] [PubMed] [Google Scholar]
- 61.Agostinho FR, Reus GZ, Stringari RB, Ribeiro KF, Pfaffenseller B, Stertz L, et al. Olanzapine plus fluoxetine treatment increases NT-3 protein levels in the rat prefrontal cortex. Neurosci Lett. 2011;497(2):99–103. 10.1016/j.neulet.2011.04.039 [DOI] [PubMed] [Google Scholar]
- 62.Spitzer RL, Williams JB, Gibbon M, First MB. The Structured Clinical interview for DSM-III-R (SCID). I: History, rationale, and description. Arch Gen Psychiatry. 1992;49(8):624–9. 10.1001/archpsyc.1992.01820080032005 [DOI] [PubMed] [Google Scholar]
- 63.Pardo JV, Lee JT, Kuskowski MA, Munch KR, Carlis JV, Sheikh SA, et al. Fluorodeoxyglucose positron emission tomography of mild cognitive impairment with clinical follow-up at 3 years. Alzheimers Dement. 2010;6(4):326–33. 10.1016/j.jalz.2009.09.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.First MB, Gibbon M, Spitzer RL, Williams JBW. Structured Clinical Interview for DSM-IV Axis I Disorders, Clinician Version (SCID-CV). Washington, D.C.: American Psychiatric Press, Inc, 1996. New York: American Psychiatric Publishing, Inc.; 1996. [Google Scholar]
- 65.Montgomery SA, Asberg M. A new depression scale designed to be sensitive to change. Br J Psychiatry. 1979;134:382–9. 10.1192/bjp.134.4.382 [DOI] [PubMed] [Google Scholar]
- 66.Corruble E, Purper D, Payan C, Guelfi J. Inter-rater reliability of two depression rating scales, MADRS and DRRS, based on videotape records of structured interviews. Eur Psychiatry. 1998;13(5):264–6. 10.1016/S0924-9338(98)80032-1 [DOI] [PubMed] [Google Scholar]
- 67.Fantino B, Moore N. The self-reported Montgomery-Asberg Depression Rating Scale is a useful evaluative tool in Major Depressive Disorder. BMC Psychiatry. 2009;9:26 10.1186/1471-244X-9-26 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Zimovetz EA, Wolowacz SE, Classi PM, Birt J. Methodologies used in cost-effectiveness models for evaluating treatments in major depressive disorder: a systematic review. Cost Eff Resour Alloc. 2012;10(1):1 10.1186/1478-7547-10-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Hamilton M. The assessment of anxiety states by rating. Br J Med Psychol. 1959;32(1):50–5. 10.1111/j.2044-8341.1959.tb00467.x [DOI] [PubMed] [Google Scholar]
- 70.Guy W. ECDEU Assessment Manual For Psychopharmacology. Rockville, MD: US Department of Heath, Education, and Welfare Public Health Service Alcohol, Drug Abuse, and Mental Health Administration; 1976. [Google Scholar]
- 71.Folstein MF, Folstein SE, McHugh PR. "Mini-mental state". A practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res. 1975;12(3):189–98. 10.1016/0022-3956(75)90026-6 [DOI] [PubMed] [Google Scholar]
- 72.Zachary RA. Shipley Institute of Living Scale Revised Manual. Los Angeles: Western Psychological Services; 1986. [Google Scholar]
- 73.Oldfield RC. The assessment and analysis of handedness: The Edinburgh inventory. Neuropsychologia. 1971;9(1):97–113. 10.1016/0028-3932(71)90067-4 [DOI] [PubMed] [Google Scholar]
- 74.McNair DM, Lorr M, Droppleman LF. Manual for the Profile Of Mood States. San Diego, CA: Educational and Industrial Testing Services; 1971. [Google Scholar]
- 75.Watson D, Clark LA. Preliminary manual for the positive affective negative affect schedule. J Pers Soc. 1999;44:644–51. [Google Scholar]
- 76.Minoshima S, Koeppe RA, Frey KA, Kuhl DE. Anatomic standardization: Linear scaling and nonlinear warping of functional brain images. J Nucl Med. 1994;35(9):1528–37. [PubMed] [Google Scholar]
- 77.Lee JT, Munch KR, Carlis JV, Pardo JV. Internet image viewer (iiv). BMC Med Imaging. 2008;8:10 10.1186/1471-2342-8-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Talairach J, Tournoux P. Coplanar Stereotaxic Atlas of the Human Brain. New York: Thieme; 1988. [Google Scholar]
- 79.Drevets WC, Savitz J, Trimble M. The subgenual cingulate cortex in mood disorde. CNS Spectr. 2008;13(8): 663–681. 10.1017/s1092852900013754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Lancaster JL, Woldorff MG, Parsons LM, Liotti M, Freitas CS, Rainey L, et al. Automated Talairach atlas labels for functional brain mapping. Hum Brain Mapp. 2000;10(3):120–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Zald DH, Lee JT, Fluegel KW, Pardo JV. Aversive gustatory stimulation activates limbic circuits in humans. Brain. 1998;121 (Pt 6):1143–54. [DOI] [PubMed] [Google Scholar]
- 82.Liotti M, Mayberg HS. The role of functional neuroimaging in the neuropsyhcology of depression. J Clin Exp Neuropsychol. 2001; 23(1):121–36. 10.1076/jcen.23.1.121.1223 [DOI] [PubMed] [Google Scholar]
- 83.Vaccarino AL, Evans KR, Sills TL, Kalali AH. Symptoms of anxiety in depression: Assessment of item performance of the hamilton anxiety rating scale in patients with depression. Depress Anxiety. 2008;25(12):1006–13. 10.1002/da.20435 [DOI] [PubMed] [Google Scholar]
- 84.Schmidt ME, Ernst M, Matochik JA, Maisog JM, Pan BS, Zametkin AJ, et al. Cerebral glucose metabolism during pharmacologic studies: Test-retest under placebo conditions. J Nucl Med. 1996;37(7):1142–9. [PubMed] [Google Scholar]
- 85.Schaefer SM, Abercrombie HC, Lindgren KA, Larson CL, Ward RT, Oakes TR, et al. Six-month test-retest reliability of MRI-defined PET measures of regional cerebral glucose metabolic rate in selected subcortical structures. Hum Brain Mapp. 2000;10(1):1–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Fallmar D, Lilja J, Kilander L, Danfors T, Lubberink M, Larsson EM, et al. Validation of true low-dose 18F-FDG PET of the brain. Am J Nucl Med Mol Imaging. 2016;6(5):269–76. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(PDF)
Stereotactically normalized. Image left is right side of brain. AC-PC plane 0 mm. Color scale shows Z-scores with threshold Z = ±3.3.
(PDF)
Stereotactically normalized. Image left is right side of brain. AC-PC plane 0 mm. Color scale shows Z-scores with threshold at Z = ±3.3.
(PDF)
Stereotactically normalized. Image left is right side of brain. AC-PC plane 0 mm. Color scale shows Z-scores with threshold at Z = ±3.3.
(PDF)
For visualizing individual metabolic fingerprints of all nine subjects, the threshold was set at t = 2.0 that is the usual threshold used for studying change in individuals [42]. Each subject is represented by a study number (e.g., pL0009). Age regression was used to match individual subject’s age to that of the normative group. R, right; L, left, A, anterior; P, posterior. The patterns are heterogenous. For example, some individuals have sgACC/VMPFC hypoactive, hyperactivity, or no change.
(PDF)
(PDF)
(PDF)
Green cells below diagonal are for Pre-treatment; blue cells above diagonal are for Post-treatment. R, right; L, left; Hippo, hippocampus; sgACC, subgenual anterior cingulate/VMPFC. † P = .007
(PDF)
(PDF)
(PDF)
Data Availability Statement
The minimal data set with the raw data used for the figures and tables is in the Supporting Information files as "Supplementary Information w data.pdf." Parties interested in data sharing policies should contact the Minneapolis Veterans Health Care System IRB (IRBMN@va.gov) to establish a data use agreement. This does not alter our adherence to PLOS ONE policies on sharing data and materials. The authors of the present study had no special access privileges in accessing data from the Minneapolis Veterans Health Care System which other interested researchers would not have.