Perceptions of Health Care Overuse Among Older US Adults: Results of a National Survey
INTRODUCTION
Overuse of health care, defined as the use of tests and treatments that are unlikely to improve outcomes and can lead to unnecessary harms, is common among older adults.1 Previous interventions to reduce overuse have had limited success,2 partly because many clinicians believe that patients feel more health care is usually better and do not perceive overuse as prevalent. For example, 7 in 10 US primary care physicians feel that patient requests for tests and treatments are a major barrier to reducing overuse.3 However, little is known about patient perceptions of overuse, or how these perceptions may differ across patients. The objectives of our study were to measure perceptions of health care overuse among older US adults and to identify characteristics associated with these perceptions.
METHODS
In October 2017, we conducted a nationally representative internet survey using GfK KnowledgePanel®, an online survey panel with approximately 55,000 US adults constructed and weighted to be representative of the US population. This survey was conducted through the University of Michigan (U-M) National Poll on Healthy Aging, a recurring online survey of GfK KnowledgePanel participants age 50 to 80. The U-M Medical School Institutional Review Board declared this study exempt.
Survey respondents were asked whether they agreed or disagreed that “when it comes to medical treatment, more is usually better” (5-point scale),4 “health care providers in general often recommend medications, tests, or procedures that patients do not really need” (4-point scale), and “my own health care provider often recommends medications, tests or procedures that I do not really need” (4-point scale). We used multivariable logistic regression to identify associations between respondents’ characteristics and agreement (strongly or somewhat agreeing) with each statement. Using estimated model coefficients, we report marginal estimates of the adjusted prevalence of perceptions as a function of respondents’ characteristics. Analyses used post-stratification sampling weights to draw national inferences and were performed with Stata version 15 (StataCorp, College Station, TX).
RESULTS
The survey completion rate determined using American Association for Public Opinion Research Cooperation Rate 15 was 73% (2007/2760). Respondents were more likely than non-respondents to be older, White, higher income, and better educated.
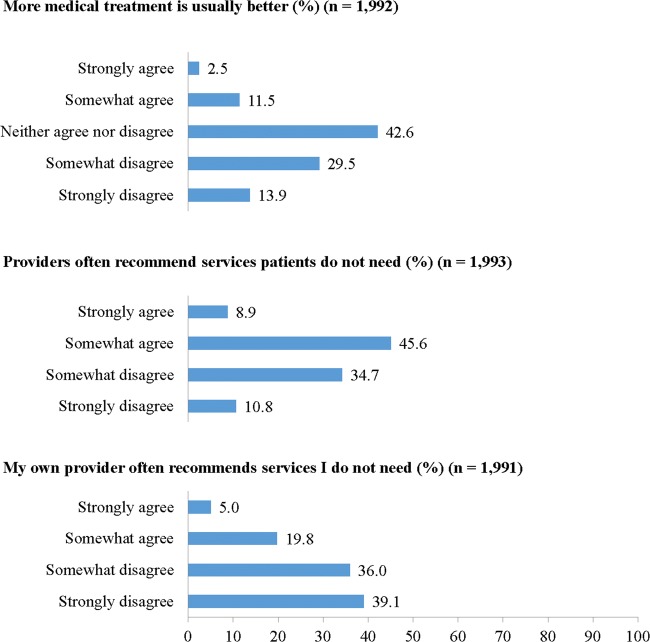
Few respondents (14.0%) agreed (strongly or somewhat) that more health care is usually better (Fig. 1). In multivariable logistic regression (Table 1), respondents age 65 to 80 were less likely than younger respondents to agree that more medical treatment is usually better (12.0% vs. 15.4%, P = 0.047). Non-White respondents were more likely than White respondents to agree that more medical treatment is usually better (20.3% vs. 11.7%, P < 0.001).
Figure 1.
Perceptions related to health care overuse among older US adults.
Table 1.
Adjusted Prevalence of Agreement with Statements about Overuse Among Older US Adults
| Characteristic | More medical treatment is usually better* (n = 1989) | Clinicians often recommend services patients do not need† (n = 1990) | My own clinician often recommends services I do not need‡ (n = 1988) |
|---|---|---|---|
| Adjusted prevalence (95% CI)§ | |||
| Age | |||
| 50 to 64 (n = 1005) | 15.4 (13.0 to 17.7) | 53.5 (50.2 to 56.8) | 25.5 (22.6 to 28.3) |
| 65 to 80 (n = 1002) | 12.0 (9.7 to 14.2)** | 56.1 (52.7 to 59.5) | 23.7 (20.7 to 26.7) |
| Race/ethnicity | |||
| White, non-Hispanic (n = 1529)‖ | 11.7 (9.9 to 13.4) | 55.8 (53.1 to 58.5) | 25.0 (22.6 to 27.4) |
| Minority (n = 478) | 20.3 (16.4 to 24.3)‡‡ | 51.1 (46.2 to 56.1) | 24.3 (20.0 to 28.6) |
| US Census region | |||
| Northeast (n = 402)‖ | 17.2 (13.1 to 21.3) | 52.6 (47.3 to 57.8) | 27.1 (22.4 to 31.8) |
| Midwest (n = 465) | 16.2 (12.4 to 19.9) | 54.0 (49.0 to 58.9) | 27.0 (22.7 to 31.3) |
| South (n = 698) | 13.2 (10.5 to 15.9) | 57.6 (53.7 to 61.5) | 25.4 (21.9 to 28.9) |
| West (n = 442) | 11.2 (8.0 to 14.3)** | 51.4 (46.2 to 56.6) | 19.9 (15.6 to 24.1)** |
| Chronic conditions | |||
| 0 or 1 (n = 470)‖ | 12.7 (10.3 to 15.1) | 56.0 (52.6 to 59.4) | 25.7 (22.7 to 28.7) |
| 2 or 3 (n = 937) | 15.2 (12.2 to 18.2) | 55.1 (51.0 to 59.2) | 24.4 (20.8 to 28.0) |
| 4 or more (n = 600) | 16.0 (11.2 to 20.7) | 47.2 (40.4 to 54.1)** | 22.6 (16.9 to 28.3) |
| Number of different clinicians seen in last year | |||
| 0 or 1 (n = 660)‖ | 11.6 (8.8 to 14.3) | 59.6 (55.5 to 63.6) | 28.1 (24.3 to 31.8) |
| 2 or 3 (n = 974) | 14.5 (12.0 to 17.0) | 52.3 (48.8 to 55.8)** | 22.9 (19.9 to 25.8)** |
| 4 or more (n = 370) | 18.3 (13.7 to 22.8)** | 49.2 (43.2 to 55.2)†† | 22.8 (17.7 to 28.0) |
**P < 0.05; ††P < 0.01; ‡‡P < 0.001
*Agreement (strongly or somewhat) that “when it comes to medical treatment, more is usually better.”
†Agreement (strongly or somewhat) that “health care providers in general often recommend medications, tests, or procedures that patients do not really need.”
‡Agreement (strongly or somewhat) that “my own health care provider often recommends medications, tests or procedures that I do not really need.”
§Marginal estimates of the weighted prevalence of agreement (strongly or somewhat) adjusted for all other variables listed in table in addition to gender, education, household income, and health status.
Reference group for tests for statistical significance. P values < 0.05 (denoted by the **, ††, and ‡‡ symbols) indicate statistically significant differences between that respective group and the reference group.
Chronic conditions included attention deficit hyperactivity disorder, asthma, chronic bronchitis or chronic obstructive pulmonary disease, cancer (excluding skin), diabetes, chronic pain, heart attack, heart disease, hepatitis C, hypertension, high cholesterol, human immunodeficiency virus or acquired immune deficiency syndrome, kidney disease, multiple sclerosis, osteoarthritis, joint pain or inflammation, osteoporosis or osteopenia, psoriasis, pulmonary arterial hypertension, rheumatoid arthritis, and stroke.
Over half (54.5%) of respondents agreed that in general clinicians often recommend services patients do not need. Respondents who saw at least 4 clinicians in the last year were less likely than respondents who saw 0 or 1 clinicians to agree that in general clinicians often recommend unneeded services (49.2% vs. 59.6%, P = 0.007). Individuals with 4 or more chronic conditions were less likely than those with 0 or 1 chronic conditions to agree that in general clinicians often recommend unneeded services (47.2% vs. 56.0%, P = 0.031).
Fewer respondents (24.8%) felt their own clinician often recommends services they do not need. Respondents who saw 2 or 3 clinicians in the last year were less likely than respondents who saw 0 or 1 clinicians to agree that their own clinician often orders unneeded services (22.9% vs. 28.1%, P = 0.035).
DISCUSSION
Contrary to the majority view among clinicians that patients’ requests drive overuse, we found that few older US adults agree that more treatment is usually better and over half agree that clinicians often order unneeded services.
Limitations include an inability to determine whether respondents actually experienced overuse. KnowledgePanel participants may be more willing and able to complete internet surveys than non-participants. Although our analyses used weights that accounted for sampling design and survey non-response, respondents could have had different perceptions of overuse than non-respondents.
Our results suggest many clinicians need to rethink their assumptions regarding what older patients, even populations who historically have experienced underuse,6 believe about aggressive medical care. Future efforts to reduce overuse in this population should prioritize helping clinicians better understand older patients’ perceptions and targeting system-level factors that drive overuse.
Acknowledgments
The authors thank Erica Solway, PhD, MSW, MPH of the University of Michigan Institute for Healthcare Policy and Innovation for feedback on this manuscript, for which she was not compensated beyond her usual salary.
Funding Information
The study was funded by Michigan Medicine and AARP, neither of which had any role in study design; collection, analysis, or interpretation of the data; and the decision to approve publication. Support was also provided by the Department of Veterans Affairs, Veterans Health Administration, Health Services Research and Development (HSR&D) Service. Dr. Kullgren is a VA HSR&D Career Development awardee (CDA 13-267) at the Ann Arbor VA.
Compliance with Ethical Standards
Conflict of Interest
Dr. Kullgren has received consulting fees from SeeChange Health and HealthMine, and honoraria from AbilTo, Inc., the Robert Wood Johnson Foundation, the American Diabetes Association, and the Kansas City Area Life Sciences Institute. Dr. Kerr is on the clinical advisory board for BIND Health Insurance. All other authors declare no conflicts of interest.
Disclaimer
The views expressed in this article are those of the authors and do not necessarily reflect the position or policy of the Department of Veterans Affairs or the US government.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Schwartz AL, Landon BE, Elshaug AG, Chernew ME, McWilliams JM. Measuring Low-Value Care in Medicare. JAMA Intern Med. 2014;174(7):1067–1076. doi: 10.1001/jamainternmed.2014.1541. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Colla Carrie H., Mainor Alexander J., Hargreaves Courtney, Sequist Thomas, Morden Nancy. Interventions Aimed at Reducing Use of Low-Value Health Services: A Systematic Review. Medical Care Research and Review. 2016;74(5):507–550. doi: 10.1177/1077558716656970. [DOI] [PubMed] [Google Scholar]
- 3.Zikmund-Fisher BJ, Kullgren JT, Fagerlin A, Klamerus ML, Bernstein SJ, Kerr EA. Perceived Barriers to Implementing Individual Choosing Wisely® Recommendations in Two National Surveys of Primary Care Providers. J Gen Intern Med. 2017;32(2):210–217. doi: 10.1007/s11606-016-3853-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Scherer LD, Caverly TJ, Burke J, et al. Development of the Medical Maximizer-Minimizer Scale. Health Psychol. 2016;35(11):1276–1287. doi: 10.1037/hea0000417. [DOI] [PubMed] [Google Scholar]
- 5.Standard Definitions: Final Dispositions of Case Codes and Outcome Rates for Surveys. 9th Edition. The American Association f or Public Opinion Research; 2016. http://www.aapor.org/AAPOR_Main/media/publications/Standard-Definitions20169theditionfinal.pdf. Accessed 22 Oct 2019
- 6.Kressin NR, Lin M-Y. Race/ethnicity, and Americans’ perceptions and experiences of over- and under-use of care: a cross-sectional study. BMC Health Services Research. 2015;15(1):443. doi: 10.1186/s12913-015-1106-7. [DOI] [PMC free article] [PubMed] [Google Scholar]