Abstract
Objective
Weight gain occurs during marriage yet obesity treatment is focused on individuals. Outcomes may be improved by targeting joint weight loss and the interpersonal milieu that fosters spousal interdependence. Self Determination Theory (SDT) posits that autonomy supportive environments (e.g., promote meaningful choice, minimize control) produce better health outcomes. This trial tested a SDT-informed weight loss intervention intended to facilitate autonomy support in couples.
Methods
Sixty-four couples were randomized to standard behavioral weight loss (BWL) that couples attended together or to a SDT-informed intervention (SDT-WL) that aimed to bolster autonomy support (AS). Groups met weekly for 6 months with assessments at 0, 3, 6, and 12 months.
Results
Percent weight loss at 6 and 12 months was 10.4±6.5 % and 9.2±8.2 %. No differences were observed between BWL or SDT-WL in percent weight loss or changes in AS. Across conditions, higher baseline AS predicted greater weight loss at 6 and 12 months, ps <.001. Increases in AS over time predicted greater weight loss at 6 and 12 months, ps≤ .02. Post-hoc moderation analysis indicated that only participants with low (but not high) baseline AS achieved greater improvements gains in AS at 12 months in SDT-WL than in BWL (p < .02).
Conclusions
While no differences were found between conditions on weight loss or changes in autonomy support behavior, autonomy support from one’s spouse predicted weight loss in both couples-based weight loss approaches. For couples with low levels of AS, a SDT-informed approach was effective at increasing this desirable interpersonal behavior.
Keywords: dyadic weight management, social support, home environment, Self-Determination Theory, couples
Body weights in spouses are interdependent (Katzmarzyk, Hebebrand and Bouchard 2002). Individuals tend to marry partners with a similar weight status (Jeffery and Rick 2002), and couples gain weight together in the first year of marriage (The and Gordon-Larsen 2009) with weight gain trajectories mirroring each other over time (Gorin et al. 2018, Jeffery and Rick 2002, Gorin et al. 2008, Christakis and Fowler 2007). Despite converging evidence of shared spousal obesity risk and the importance of the social and interpersonal environment on weight regulation (Burgess, Hassmen, and Pumpa, 2017, Mata, Richter, Schneider, and Hertwig, 2018, Saelens et al., 2018), behavioral weight loss treatment is typically individually focused (Jensen et al. 2013, LeBlanc, Patnode, Webber, Redmond, Ruskin, and O’Connor, 2018). This is a missed opportunity to address shared problematic dietary habits, physical activity patterns, and obesogenic factors within the home (Leroux, Moore, and Dube, 2013).
There are numerous examples of spouses participating in early behavioral weight management programs but these interventions tended to be quite brief with modest effects (Black, Gleser, and Kooyers 1990, McLean et al. 2003). Moreover, these “couples-based” approaches often focused only on one index participant, with spouses included in treatment with the intention of providing support for behavior change (Leroux et al. 2013). Recent work has revisited the efficacy of involving spouses in weight loss treatment with an increased focus on involving both members of the couple within a dyadic framework and on identifying the types of spousal support that are most beneficial for weight loss (Gorin et al. 2013, Cornelius et al. 2018, Gorin et al. 2014, Schierberl Scherr, McClure Brenchley, and Gorin 2013). For example, Gorin et al. (2013) found that including spouses or another adult household member in a comprehensive treatment targeting the home environment produced better short- and long-term weight loss outcomes. Within this intervention, only autonomy support from one’s partner (i.e., non-judgmental, empathic, responsive support) predicted better 6- and 18-month weight loss outcomes. Conversely, more directive forms of support (e.g., frequent reminders from one’s partner to eat healthy) hindered progress (Gorin et al. 2014).
Autonomy support emerges from Self-Determination Theory (SDT), which posits that environments that elicit, acknowledge, and value autonomy are critical to establishing self-directed personally meaningful choices (Ryan and Deci 2000b, Ryan and Deci 2000a). Environments that foster autonomy enhance internalized autonomous self-regulation, perceived competence, relationship satisfaction, and well-being (Deci et al. 2006, Koestner et al. 2012, Grolnick and Ryan 1987, Gorin et al. 2014). Furthermore, autonomous self-regulation is an established predictor of better outcomes in education and health domains (Teixeira et al. 2012, Deci et al. 1994, Joussemet et al. 2004, Levesque et al. 2007). Notably, positive effects of autonomy supportive environments are most apparent for sustained changes (Silva et al. 2011), precisely the shortfall of existing behavioral weight loss programs.
Many well-intentioned support partners engage in what they perceive to be helpful behavior, such as reminding a spouse to head to the gym, or interjecting when food choices are being made. While these efforts may be well meaning, evidence suggests that they are ineffective (Gorin et al., 2014). In contrast, autonomy support involves asking a partner what might be helpful, empathically responding to the difficulties of the process, and respecting and appreciating a partner’s choices and efforts. This is conceptually similar to the “secure base” responsive support proposed by Feeney (2004), whereby empathic responding is coupled with encouragement of exploration, interest in and acceptance of a partner’s goal strivings, and a balance of availability with an appreciation of a partner’s need for individual self-growth. Likewise, this model considers intrusive and/or interfering behavior as antithetical to true support.
In the domain of weight-related research, receiving autonomy support from spouses or romantic partners correlates with dietary change and weight loss (Gorin et al. 2014, Powers, Koestner and Gorin 2008), and is more beneficial than other, more directive forms of support (Gorin et al. 2014). There is also evidence that interventions delivered by health care professionals in an autonomy supportive fashion are associated with better health outcomes (Williams et al. 2006b, Silva et al. 2010, Williams et al. 2002), yet intervention research involving family members is lacking. Since much of weight management involves choices that are made at home (Smith, Ng, and Popkin 2013, Sturm 2004), intervening to improve autonomy support in the home may be particularly powerful. Whether autonomy support is indeed a modifiable intervention target within existing spousal dyads has not yet been established, thus, a necessary next step is to develop and test an intervention designed to engender autonomy support within couples for weight-related behavior change.
The TEAMS (Talking about Eating, Activity, and Mutual Support) Trial examined the impact of a weight loss program rooted in SDT on autonomy support behavior and weight loss outcomes using a novel dyadic design that included both members of the couple in treatment and analyses (Gorin et al. 2017). Other SDT concepts were also examined (e.g., autonomous self-regulation, perceived competence for behavior change). The SDT-informed condition (SDT-WL) included training in the provision of autonomy support and was compared to a more traditional model of spouse involvement (i.e., spouses attended groups together but receive no training in providing autonomy support; BWL). The primary hypotheses were that compared to BWL, SDT-WL would result in: 1) greater increases in autonomy support from spouses, 2) greater increases in autonomous self-regulation and competence for healthy behaviors, and 3) greater weight loss at 6 and 12 months. Secondary aims compared SDT-WL and BWL on maintenance of weight loss (6–12 months), relationship satisfaction, and treatment satisfaction. Exploratory analyses compared the influence of autonomy support on weight loss with more directive forms of support and examined whether the effect of autonomy support on weight loss was mediated by autonomous self-regulation and perceived competence, as predicted by SDT. To guide future intervention tailoring efforts (Kreuter & Skinner, 2000), post hoc analyses examined whether baseline autonomy support moderated treatment outcomes. It was hypothesized that the SDT-informed intervention would be best suited to individuals entering treatment with lower levels of autonomy support.
Methods
TEAMS was funded by the National Heart Lung and Blood Institute. The protocol has been previously published (Gorin et al. 2017). A brief description of the study design and measures is provided below.
Participants
Married or cohabitating couples in the Greater Hartford, CT area participated in the study. Each partner had to be 18–70 years old with a body mass index (BMI) between 25–45 kg/m2. Couples were excluded if either spouse reported: current participation in a weight loss program, dieting, or taking medications that might affect weight; participation in a weight loss program in the past year; weight loss > 10% of body weight during the past 6 months; current participation in any other research study that may interfere with this study; current pregnancy, lactation, < 6 months postpartum, or plans to become pregnant during the study; cancer treatment within the past year, excluding skin cancer treatment; substance abuse, dependence, or current treatment for alcohol or substance abuse; a heart condition, chest pain during periods of activity or rest, or loss of consciousness on the PAR-Q (Thomas, Reading and Shephard 1992); uncontrolled hypertension, history of coronary heart disease, stroke, peripheral arterial disease or having a blood pressure ≥160/100 mmHg; chronic gastrointestinal disease; hepatitis B or C, cirrhosis, or HIV; or a significant psychiatric illness that might interfere with completion of the study. Those endorsing joint problems, diabetes, prescription medication usage to manage hypertension, hypercholesterolemia, or a heart condition, or any conditions that could limit exercise were required to obtain written physician consent to participate in the study.
Recruitment, screening, and randomization
Couples were recruited through local media advertisements and screened by phone for eligibility. Eligible couples were invited to an in-person orientation where detailed information about the study was provided and informed consent obtained. Once baseline assessments were completed, couples were randomized as a dyad via a simple, variable-block length randomization, to either behavioral weight loss (BWL) or behavioral weight loss informed by Self-Determination Theory (SDT-WL) using an online randomization program (Urbaniak and Plous, 2013), which ensured fairly equal allocations and made it difficult to guess future assignments.
Treatment overview
Couples in both conditions received 6 months of weekly weight loss group meetings and the same core information about diet and physical activity. Each member of the dyad was encouraged to engage in healthy behaviors and weight loss efforts and to serve as a model or cue for desired behavior changes. To isolate the unique effects of autonomy support training, dyads in SDT-WL additionally received training in how to provide autonomy support for weight loss.
Treatment components common to both conditions
Treatment structure
In both conditions, the 6-month treatment program was delivered in interactive weekly group sessions (check-in period, didactic information, and group discussion) lasting approximately one hour. This meeting schedule is consistent with best practices according to AHA/ACC/TOS guidelines (Jensen et al. 2013).
Interventionists
Individuals with advanced degrees in nutrition, exercise physiology, or psychology served as interventionists. Two Ph.D. level clinical psychologists (T.P. and A. A. G.) trained interventionists in how to work with couples, SDT, and strategies for building autonomy support. This ~10 hour training consisted of role-playing and discussion of didactic materials and the difference between conditions was reinforced during ongoing weekly supervision.
Diet
Participants were placed on a standard caloric and fat restricted diet (e.g., 1200–1800 kcals/day, <30% fat) (Jensen et al. 2013). They received sample meal plans, a fat and calorie guidebook and internet references, and a daily diary to self-monitor diet and physical activity. Participants were allowed to self-monitor via an online tracking program of their choice (e.g., MyFitnessPal). Interventionists provided weekly written feedback.
Exercise
Participants were encouraged to gradually increase their physical activity up to 50 minutes of moderate intensity activity on 5 days per week (100 min/weeks 1–4; 150 min/weeks 5–8; 200 min/weeks 9–16; 250 min/weeks 17+) (Jensen et al. 2013). Brisk walking and accumulating activity through multiple short bouts was encouraged (Pescatello, Arena, Riebe, and Thompson, 2013), and participants were instructed to self-monitor their daily exercise minutes (Musto et al. 2010).
Behavior Therapy
Behavioral and cognitive skills training included self-monitoring, stimulus control, problem solving, goal setting, cognitive restructuring, and relapse prevention (Butryn et al. 2011, Jensen et al. 2013, Wadden et al. 2006). After achieving 10% weight loss, keys to long-term success were reviewed and problem-solving emphasized (Perri et al. 2001).
Treatment components specific to the SDT condition
The only difference between conditions was that dyads in SDT-WL received additional training in how to provide autonomy support for each other’s weight loss efforts. Adapting effective strategies from the literature on autonomy supportive behaviors in educators, coaches, and healthcare providers (Williams et al. 2002, Williams et al. 2006b, Silva et al. 2010, Powers et al. 2008, Williams and Deci 2001, Williams, Freedman and Deci 1998, Williams et al. 2006c), spouses were encouraged to: 1) elicit and acknowledge the other’s perspective, 2) minimize efforts to control, 3) use non-judgmental, non-critical language, 4) support each other’s initiatives for change, and 5) develop empathic responding. Couples were taught basic concepts of autonomy support using an “ABC” model (Ask to avoid assumptions, Be empathic, and Curtail control and criticism (Gorin et al. 2017)) and were provided opportunities to practice these new behaviors in group meetings. Spouses were encouraged to incorporate these behaviors into their relationship between sessions and to monitor targeted support behaviors. Clinical tools used to facilitate adoption of these behaviors included: 1) ABC model handouts, 2) cartoon vignette dialogues depicting unhelpful communication patterns and more effective ways of communicating (Faber and Mazlish 1980), 3) interventionist-facilitated role-plays to provide couples the opportunity to practice autonomy supportive behaviors and receive personalized feedback, 4) group discussions, and 5) weekly written reflection on support provided and received from one’s spouse with examples shared at group sessions.
Assessments
Assessments were conducted at baseline, 3 months, 6 months, and 12 months by research assistants blinded to condition.
Demographics and weight history
Basic demographic information (e.g., age, sex, income) was assessed at baseline only.
Anthropometrics
Weight was measured in kilograms to the nearest 0.1 kg using a calibrated standard digital scale (Tanita BWB 800) with participants in light clothing and no shoes. Standing height was measured in participants without shoes using a portable stadiometer. All anthropometric measures were taken in duplicate and the mean was used in analyses.
Self Determination Theory measures
Autonomy support was measured with the Important Other Climate Questionnaire (IOCQ) (Williams et al. 2006a) assessing the perceptions of autonomy support that partners experience from one another (e.g., “My partner conveys confidence in my ability to control my own weight”) (Cronbach’s α ≥ .82 at each timepoint). Seven items representing more directive forms of support, similar to those used in previous research (Powers et al. 2008, Gorin et al. 2014), were also assessed (Cronbach’s α ≥ .86 at each timepoint). Examples of such items are “My partner has been reminding me about what I need to be doing”, and “My partner has been problem solving about my weight loss plans”.
Autonomous self-regulation was assessed with 6-items from the Reasons for Weight Control scale adapted from Levesque et al. (Levesque et al. 2007) which asks participants to report their reasons for losing weight (e.g., “Because I feel that I want to take responsibility for my own health”) (Cronbach’s α ≥ .85 at each timepoint). Participants also completed the 4-item Perceived Competence Scale (Williams et al. 2006b, Williams and Deci 2001) to assess perceived competence for weight management (Cronbach’s α ≥ .93 at each timepoint). Items on all three SDT measures were rated on a 7-point Likert scale, with higher values representing greater autonomy support, autonomous self-regulation, and perceived competence. Mean values were calculated for each scale
Relationship quality
To assess marital satisfaction and cohesion, participants completed 6-items from the Quality Marriage Index (QMI) (Norton 1983) (Cronbach’s α ≥ .94 at each timepoint).
Treatment satisfaction
A 5-item measure was created to assess satisfaction with the treatment program (e.g., “How satisfied were you with the Project TEAMS weight loss program”) and was completed at the 6-month assessment (Cronbach’s α = .80).
Quality Control and Safety Procedures
Intervention manuals were developed for each condition. All group sessions were audiotaped. To assess treatment fidelity, approximately 20% of sessions were reviewed by study investigators to: 1) determine whether they could identify which condition the particular session belongs to, 2) assess whether key elements in each session were covered, and 3) whether any cross-contamination occurred. A data safety monitoring board (DSMB) was established to assure safety and study integrity.
Procedures to retain the sample
Retention at follow-up visits was promoted through strategies used effectively in other studies (e.g., collecting information of relatives/friends who could be contacted if unable to reach the participant). For each visit, participants were scheduled by phone or email, sent reminders via mail/text/or email, and contacted the day before. Missed visits were rescheduled. Childcare and costs for transportation were provided to participants if these were significant barriers to assessment visits. If necessary, assessments were completed at participants’ homes or an agreed upon public location. Participants received an honorarium of $10 at 3 months, $25 at 6 months, and $40 at 12 months for completing assessments.
Data Analysis Strategy
Data from couples are interdependent, which violates traditional statistical assumptions (Kenny et al. 2010). Linear multilevel models were specified using the MIXED command in SPSS, with the dyad as the unit of analysis and with couple members nested within dyad. Because both members received treatment and because there were mixed-sex couples enrolled, data were not distinguishable (i.e., there was not a single distinguishing variable that was the same for each couple, such as “man” and “woman,” or “treated” and “untreated” spouse). Participant characteristics were examined as means and standard deviations, or percentage, as appropriate. Preliminary analyses tested assumptions of normality (e.g., normally distributed residuals) and examined the comparability of participants on demographic characteristics assigned to BWL and SDT-WL using multilevel models. Next, differences in weight change (percent change and kg change) at 3, 6, and 12 months, and between 6 and 12 months, by condition, were examined using multilevel models with condition (contrast coded; BWL = −1, SDT-WL = 1) as the sole predictor. To examine whether SDT-WL led to increases in core SDT variables (i.e., autonomy support, autonomous self-regulation, and perceived competence), changes in each of these variables were specified as the outcome; the association of SDT variables with weight change was also examined. Where appropriate, full SDT mediation models were tested, with (1) increases in autonomy support as a prospective predictor of changes in (2a) autonomous self-regulation and (2b) perceived competence, and (3) weight. We also explored whether the intervention impacted relationship satisfaction. Finally, differences in treatment satisfaction by condition were examined. All available data were used at each timepoint (note that sensitivity analyses examining the effect of condition on percent weight change replicated full data analyses). The trial, which is the first to compare two active couples-based weight loss approaches, was powered to detect a medium to large effect size (equal to d = .71 at the dyad level, and .62 at the individual level, adjusting for interdependence within dyads, (Kenny et al., 2010) for the primary weight loss comparison, with 80% power for a two-tailed test at alpha = .05.
The study protocol was approved by the Institutional Review Board at the University of Connecticut
Results
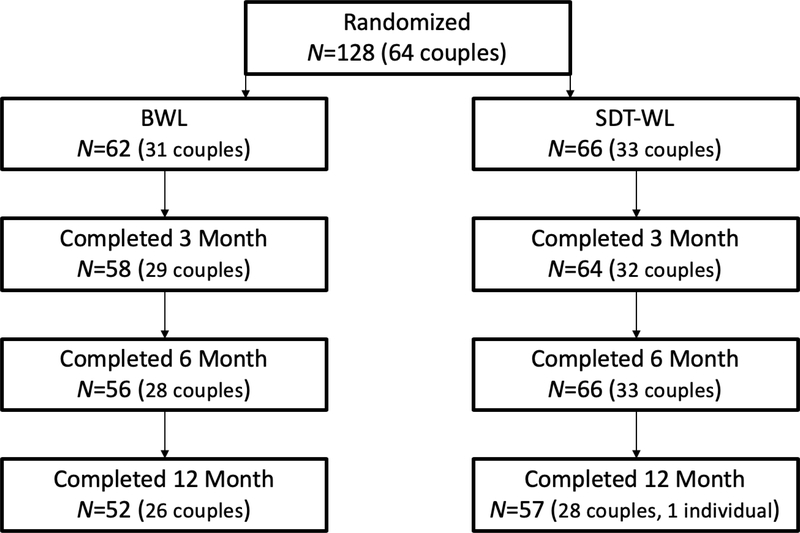
There were no demographic differences between BWL participants (n = 62; 31 couples) and SDT-WL participants (n = 66; 33 couples) at baseline (Table 1a). Of the 128 participants enrolled, all but 19 completed the 12-month assessment (85.2% retention; Figure 1). Those who did not complete the 12-month assessment did not differ from completers in terms of age, sex, condition, baseline autonomy support, baseline weight, or percent weight change at 6 months. Baseline SDT variables are reported in Table 1b. Preliminary analyses indicated that assumptions of normality were met.
Table 1a.
Demographics for the overall sample and by condition, reported as mean (standard deviation) or n (%).
| Overall (N = 128; 64 couples) | BWL (N = 62; 31 couples) | SDT-WL (N = 66; 33 couples) | ||
|---|---|---|---|---|
| Age | 53.45 (10.04) | 52.76 (10.24) | 54.11 (9.88) | |
| Sex | Female | 64 (50.0%) | 31 (50.0%) | 33 (50.0%) |
| Marital Status | Married | 124 (96.9%) | 60 (96.8%) | 64 (97.0%) |
| Same-Sex Couplea | Yes | 2 (3.1%) | 0 (0.0%) | 2 (6.1%) |
| Race | White | 118 (92.2%) | 56 (90.3%) | 62 (93.9%) |
| Black | 4 (3.1%) | 3 (4.8%) | 1 (1.5%) | |
| Asian | 4 (3.1%) | 3 (4.8%) | 1 (1.5%) | |
| Hispanic/Latino | 2 (1.6%) | 0 (0.0%) | 2 (3.0%) | |
| Education | Grades 9–11 | 1 (0.8%) | 1 (1.6%) | 0 (0.0%) |
| Grade 12 or GED | 14 (10.9%) | 5 (8.1%) | 9 (13.6%) | |
| Some College or Technical School | 19 (14.8%) | 13 (21.0%) | 6 (9.1%) | |
| Associate’s or Technical Degree | 19 (14.8%) | 7 (11.3%) | 12 (18.2%) | |
| Bachelor’s Degree | 26 (20.3%) | 15 (24.2%) | 11 (16.7%) | |
| Graduate or Professional Degree | 49 (38.3%) | 21 (33.9%) | 28 (42.4%) | |
| Income | $20,000–$29,000 | 3 (2.4%) | 3 (5.0%) | 0 (0.0%) |
| $30,000–$39,000 | 3 (2.4%) | 2 (3.3%) | 1 (1.5%) | |
| $40,000–$49,000 | 1 (0.8%) | 0 (0.0%) | 1 (1.5%) | |
| $50,000–$59,000 | 2 (1.6%) | 2 (3.3%) | 0 (0.0%) | |
| $60,000–$69,000 | 10 (8.0%) | 4 (6.7%) | 6 (9.2%) | |
| $70,000–$79,000 | 8 (6.4%) | 4 (6.7%) | 4 (6.2%) | |
| $75,000 or above | 98 (78.4%) | 45 (75.0%) | 53 (81.5%) | |
| Baseline Height (cm) | 170.38 (9.76) | 169.95 (9.63) | 170.79 (9.94) | |
| Baseline Weight (kg) | 97.67 (19.93) | 95.90 (20.31) | 99.33 (19.57) | |
| Baseline BMI (kg/m2) | 33.50 (5.44) | 33.04 (5.57) | 33.93 (5.33) | |
Note: Significant differences between conditions on age, height, weight, and weight change were tested using multilevel univariate models, with condition as the sole predictor.
p < .05
p < .01.
Reported at the level of the dyad.
Figure 1.
Study flow for N = 128 randomized couples.
Note: A total of 5 couples dropped out in the BWL condition, and 4 couples plus 1 individual in SDT-WL. One couple did not complete the 3-month assessments for SDT-WL but returned for 6- and 12-month assessments.
Table 1b.
Baseline characteristics on key variables for the overall sample and by condition, reported as mean (standard deviation).
| Overall (N = 128; 64 couples) | BWL (N = 62; 31 couples) | SDT-WL (N = 66; 33 couples) | |
|---|---|---|---|
| M (SD) | M (SD) | M (SD) | |
| Autonomy Support | 5.65 (1.04) | 5.64 (1.01) | 5.66 (1.07) |
| Directive Support | 3.35 (1.56) | 3.54 (1.60) | 3.18 (1.51) |
| Autonomous Self-Regulation | 6.42 (0.66) | 6.35 (0.74) | 6.48 (0.57) |
| Perceived Competence | 4.70 (1.34) | 4.86 (1.44) | 4.56 (1.22) |
| Baseline Relationship Satisfaction | 37.87 (6.96) | 38.36 (5.91) | 37.41 (7.84) |
Note: Significant differences between conditions were tested using multilevel univariate models, with condition as the sole predictor.
p < .05
p < .01.
Percent weight change
Participants lost an average of 7.1% (SD = 3.7) at 3 months, 10.4% (SD = 6.5) at 6 months, and 9.2 % (SD = 8.2) at 12 months (kg change is reported in Table 2). There was a small 1.1% (SD = 3.3) weight gain between 6 and 12 months. There were no significant differences in weight change between BWL and SDT-WL participants (Table 2). Weight change was significantly related within couples, such that, if one member of the couple lost more (or less) weight at any given time, the other member of the couple also tended to lose more (or less) weight. The intraclass correlation for percent weight change at 3 months was .43, 95% CI [.20, .61], p < .001; at 6 months, ICC = .66 [.48, .78], p < .001; at 12 months, ICC = .66 [.48, .79], p < .001; and from 6 to 12 months, ICC = .43 [.18, .63], p < .001. The interclass correlations at each time were also examined separately for BWL and SDT-WL couples; the one difference between conditions was found in the correlation between partners from 6–12 months, which remained significant for the SDT-WL condition, but not the BWL condition (analyses not shown).
Table 2.
Weight loss, in both kg (difference score) and percent change, for the overall sample and separated by condition.
| Overall | BWL | SDT-WL | ||||
|---|---|---|---|---|---|---|
| kg change | % change | kg change | % change | kg change | % change | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| 3 Months | −7.04 (4.43)** | −7.08 (3.77)** | −6.70 (4.14) | −6.92 (3.86) | −7.35 (4.69) | −7.22 (3.72) |
| 6 Months | −10.31 (7.17)** | −10.44 (6.49)** | −10.43 (6.91) | −10.93 (6.67) | −10.21 (7.43) | −10.04 (6.36) |
| 12 Months | −9.03 (8.53)** | −9.20 (8.15)** | −8.43 (8.73) | −8.90 (8.58) | −9.60 (8.37) | −9.49 (7.79) |
| 6 to 12 Months | 1.09 (3.53)** | 1.06 (3.33)** | 1.46 (3.49) | 1.43 (3.18) | 0.75 (3.56) | 0.71 (3.44) |
Note: Changes over time were examined using intercept-only multilevel models; differences between conditions were tested using multilevel univariate models, with condition as the sole predictor. Significance for change over time is noted in the “Overall” columns; differences across condition are noted in the BWL/SDT-WL columns.
p < .05
p < .01.
Change in SDT variables
Autonomy support was significantly higher at 3, 6, and 12 months than at baseline; however, there was a significant decrease from 6 to 12 months. This pattern replicated for perceived competence. For autonomous self-regulation, no increase was observed, however, there was a significant decrease in autonomous self-regulation from 6 to 12 months. No difference in these patterns emerged between BWL and SDT-WL (Table 3). Condition was also unrelated to changes in directive support (analyses not shown).
Table 3.
Change in SDT variables (difference scores) for the overall sample and separated by condition.
| Autonomy Support | Autonomous Self-Regulation | Perceived Competence | |||||||
|---|---|---|---|---|---|---|---|---|---|
| Overall | BWL | SDT-WL | Overall | BWL | SDT-WL | Overall | BWL | SDT-WL | |
| M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | M (SD) | |
| 3 Months | 0.59 (0.87)** | 0.64 (0.78) | 0.55 (0.96) | 0.02 (0.65) | 0.04 (0.56) | −0.01 (0.73) | 0.66 (1.30)** | 0.56 (1.32) | 0.75 (1.29) |
| 6 Months | 0.60 (0.96)** | 0.58 (0.93) | 0.62 (0.99) | 0.11 (0.61) | 0.11 (0.47) | 0.11 (0.72) | 0.80 (1.56)** | 0.62 (1.58) | 0.95 (1.53) |
| 12 Months | 0.33 (1.08)** | 0.21 (0.98) | 0.44 (1.15) | −0.02 (0.63) | −0.09 (0.68) | 0.05 (0.58) | 0.34 (1.99) | 0.10 (2.15) | 0.56 (1.83) |
| 6 to 12 Months | −0.31 (0.71)** | −0.37 (0.77) | −0.26 (0.66) | −0.14 (0.66)* | −0.23 (0.58) | −0.06 (0.72) | −0.53 (1.20)** | −0.59 (1.29) | −0.48 (1.13) |
Note: Changes over time were examined using intercept-only multilevel models; differences between conditions were tested using multilevel univariate models, with condition as the sole predictor. Significance for change over time is noted in the “Overall” columns; differences across condition are noted in the BWL/SDT-WL columns.
p < .05
p < .01.
Exploratory moderation analyses
Because baseline autonomy support was quite high in both BWL and SDT-WL (means over 5.6 on a 7-point scale), exploratory analyses tested whether the effect of the intervention on change in autonomy support was moderated by baseline autonomy support. In other words, did the intervention “work” for individuals who had room to increase? The moderation effect was not significant at 3 or 6 months; however, the effect of condition on change in autonomy support from baseline to 12 months was moderated by baseline autonomy support, B = −0.18 [−0.24, −0.03], p = .017. When baseline autonomy support was high (+1SD), condition was not significant, B = −0.07 [−0.33, 0.18], p = .57. When baseline autonomy support was low, SDT-WL participants experienced a larger increase in autonomy support from baseline to 12 months than BWL participants, B = 0.31 [0.06, 0.56], p = .015.
SDT variables and weight change
Because no differences were uncovered between BWL and SDT-WL conditions when examining changes in weight or in SDT variables, the full SDT model was examined in all participants; condition was included as a covariate only.
Autonomy support and percent weight change
First, we examined whether increases in autonomy support predicted subsequent percent weight change, controlling for baseline autonomy support. Participants who had higher levels of autonomy support at baseline had greater percent weight loss at 6 months, B = −2.31 [−3.86, −0.76], p = .004. Participants who had an increase in autonomy support at 3 months also lost more weight at 6 months than those who did not, B = −2.12 [−3.91, −0.34], p = .020. This pattern replicated at 12 months. Greater baseline autonomy support predicted more weight loss at 12 months, B = −3.84 [−5.62, −2.06], p < .001, as did increases in autonomy support from baseline to 6 months, B = −3.60 [−5.47, −1.73], p < .001. Additional analyses explored the relationship between directive support and weight change. No significant associations emerged (not shown).
Autonomous self-regulation and percent weight change
Participants who had higher levels of autonomous self-regulation at baseline had greater percent weight loss at 6 months, B = −1.56 [−3.01, −0.11], p = .036; however, change in autonomous self-regulation from baseline to 3 months was not associated with 6-month weight change, B = −0.29 [−1.75, 1.18], p = .699. For 12-month weight change, neither baseline autonomous self-regulation nor change in autonomous self-regulation from baseline to 6 months predicted weight outcomes, B = −2.09 [−4.36, 0.18], p = .071; and, B = −0.77 [−3.54, 2.00], p = .582, respectively.
Perceived competence and percent weight change
Participants who had higher levels of perceived competence at baseline had greater percent weight loss at 6 months, B = −1.03 [−1.89, −0.17], p = .019. Participants who had an increase in perceived competence from baseline to 3 months lost more weight than those who did not, B = −1.58 [ 2.43, 0.72], p < .001. This pattern replicated at 12 months. Baseline perceived competence was negatively associated with percent weight gain at 12 months, B = −2.39 [−3.52, −1.27], p < .001, as was increase in perceived competence from baseline to 6 months, B = −3.17 [−4.17, −2.16], p < .001.
SDT Mediation Models
Autonomy support and autonomous self-regulation
Increases in autonomy support from baseline to 3 months predicted greater increases in autonomous self-regulation at 6 months, B = 0.15 [0.00, 0.30], p = .047; 6-month increases in autonomy support were marginally associated with changes in 12-month autonomous self-regulation, B = 0.16 [−0.00, 0.33], p = .052. However, change in autonomous self-regulation at 6 months (controlling for changes in autonomy support at 3 months) was not associated with 12-month weight change, B = −0.99 [−3.82, 1.83], p = .486; thus, a formal test of mediation was not pursued.
Autonomy support and perceived competence
Increases in autonomy support at 3 months had a marginal positive association with increases in perceived competence at 6 months, B = 0.31 [−0.05, 0.66], p = .087; 6-month increases in autonomy support significantly predicted 12-month increases in perceived competence, B = 0.99 [0.61, 1.38], p < .001. Because a formal mediation test required a 3-month change in support receipt predicting a 6-month change in perceived competence (to predict 12-month weight change), a full SDT mediation model was not pursued.
Relationship Satisfaction
Changes in relationship satisfaction did not differ between BWL and SDT-WL (Table 4). There was a significant increase in relationship satisfaction from baseline to 6 months; however, there was a significant decrease in satisfaction between 6 and 12 months. Baseline relationship satisfaction was marginally related to decreases in autonomy support at 3 months, B = −0.02 [−0.05, 0.00], p = .060, and 6 months, b = −0.02 [−0.05, 0.00], p = .093, and increases from 6 to 12 months, B = 0.02 [0.00, 0.04, p = .019, but was not related to weight change at any timepoint, ps > .45.
Table 4.
Change in relationship satisfaction for the overall sample and separated by condition
| Relationship Satisfaction | |||
|---|---|---|---|
| Overall | BWL | SDT-WL | |
| M (SD) | M (SD) | M (SD) | |
| 3 Months | −0.36 (7.55) | −0.71 (9.42) | −0.33 (5.31) |
| 6 Months | 1.48 (4.72)** | 1.56 (4.42) | 1.42 (5.00) |
| 12 Months | 0.47 (6.23) | −0.25 (6.54) | 0.33 (5.97) |
| 6 to 12 Months | −1.21 (5.31)* | −1.90 (6.24) | −0.57 (4.25) |
Note: Changes over time were examined using intercept-only multilevel models; differences between conditions were tested using multilevel univariate models, with condition as the sole predictor. Significance for change over time is noted in the “Overall” columns; differences across condition are noted in the BWL/SDT-WL columns.
p < .05
p < .01.
Treatment Satisfaction
Treatment satisfaction was high in both BWL (M = 6.6, SD = 0.6) and SDT-WL (M = 6.6, SD = 0.7), where 7 was the highest possible score (e.g., “very satisfied”; Range 3.8, 7.0). Participants who reported more autonomy support at baseline were significantly more satisfied with treatment, B = 0.24 [.13, .34], p < .001.
Discussion
In light of reports of the interdependence of weight and related behaviors within couples (Christakis and Fowler 2007, Cornelius, Gettens and Gorin 2016, Mata et al., 2018), there is a need to revisit couples weight loss from a theory-based lens to determine when and how spouses can best support each other’s weight management goals. This study tested whether a SDT-informed approach to couples weight loss (SDT-WL) had added benefit over standard behavioral treatment delivered to couples (BWL). Results suggest that couples weight loss interventions are broadly effective and confirm autonomy support as a critical determinant of weight loss and weight-loss maintenance success. However, the SDT-informed intervention designed to improve autonomy support did not produce significant gains in autonomy support or greater weight loss, leaving questions about how best to engage this intervention target.
On average, participants lost 10% of their body weight and were able to sustain this loss. These results are an improvement over earlier couples’ weight loss programs which tended to be of a shorter duration (Black et al. 1990), focused on one index participant, and did not incorporate theory-based support training. This was true in both the BWL and SDT-WL conditions, suggesting that a dyadic and couple-targeted approach may be sufficiently powerful to harness dyadic processes that promote positive behavior changes. Providing even further support for the concept of treating couples together, and consistent with previous evidence (Christakis and Fowler 2007), weight loss was correlated in couples. A potentially meaningful result was discovered at follow-up, with the correlation within spousal dyads diminishing in BWL, but remaining significant in SDT-WL. It is possible the autonomy support intervention promoted greater interconnectedness among the partners over time.
Both baseline autonomy support and increases in autonomy support over time were consistently associated with greater weight loss, whereas more directive support (e.g., frequent reminders, pressuring) from partners did not. These findings replicate previous SDT literature (Gorin et al. 2014, Powers et al. 2008) but with an objectively measured health outcome: weight. While Gorin et al. (2014) found directive “support” to be negatively related to weight loss, there was no relation in the current study to any of the study variables. Further research is needed to determine if this kind of support is deleterious or simply ineffective. Interestingly, autonomy support improved over the course of the program, but there were no significant differences between the conditions. It is likely quite difficult to impact longstanding interpersonal behavior patterns, especially with a relatively limited intervention. It is possible that a more robust intervention would have had a greater effect. For example, the intervention could have been longer, it could have been more individualized, or it could have included greater personalized attention from the interventionists rather than being delivered in a group format. Another compelling explanation is self-selection bias in the study sample. Couples who entered the study were already high in autonomy support at baseline, diminishing the probability (or possibility, due to ceiling effects) of demonstrating significant increases in autonomy supportive behavior as a result of the intervention. Indeed, couples with lower baseline autonomy support (i.e., those with “room to be influenced”) appeared to gain the most from the SDT-WL intervention at 12-months. This type of intervention may work better with those who need it more, and may exert its effect over time, rather than immediately. It is possible that targeting only these individuals, and/or intervening at the beginning of the maintenance phase rather than the treatment phase might be a cleaner test of the hypotheses, and perhaps lead to a more effective use of the intervention. Future work should test this possibility by targeting couples who are lower in autonomy support at treatment entry.
The SDT model was partially supported. Changes in autonomy support were positively associated with prospective increases in autonomous self-regulation and perceived competence, however, only perceived competence was significantly related to weight loss, and only at follow-up. Results from the present study instead suggest that the association of autonomy support to weight loss is direct, or may be mediated through another mechanism not measured in this intervention or not accounted for in the SDT model at present. Previous research has also failed to demonstrate the mediation of autonomy support through changes in self-regulation, and so, revision of the theoretical model—at least in relation to weight outcomes, which are more distal than health behaviors—may be necessary (Gorin et al. 2014). Baseline autonomous self-regulation was also quite high in this sample, thereby restricting the likelihood of predicting weight loss. It is possible that studies including participants who are reluctant to or ambivalent about change would be necessary to sufficiently test this potential pathway. In addition, changes in basic need satisfaction and need thwarting were not directly assessed in the study, and these may have shed some light on the weight loss results, especially during maintenance. However, relationship satisfaction was assessed and the results were not significant.
The study has some limitations. In addition to issues with self-selection, the sample was largely white, middle-class, and heterosexual reflecting the geographic area in which recruitment occurred. Future research would benefit from including a larger, more diverse sample. The study did include a 6-month follow-up assessment; however, a longer follow-up period may be needed to detect the full SDT mediation model when the outcome concerns weight loss rather than the associated behaviors that are more proximal to the SDT model (i.e., diet, physical activity). A longer follow up is also needed to test the theoretical predictions that increased autonomy support and autonomous self-regulation should exert their greatest impact on maintenance of behavior change after the intervention has ended. Finally, SDT-WL may not have been sufficiently robust to produce the impact for which it was intended. Revisions to the intervention model need to be considered for future examination.
The TEAMS trial was innovative in several ways. Married and cohabitating couples, not individuals, were the unit of treatment and analysis. The intervention was delivered to both spouses, and the statistical approach fully utilized the dyadic nature of the data to explore how couples lose weight together. In contrast to earlier couples-based weight loss interventions (Black et al. 1990, McLean et al. 2003), a clear theoretical framework guided both the treatment and assessment protocols. Autonomy support was well defined and distinguished from more directive types of support over the 12-month study, allowing for a prospective test of the SDT model and an analysis of the unique contribution of autonomy support to weight loss outcomes.
Conclusion
The TEAMS trial tested the benefits of approaching weight management as a couples’ health issue, and results suggest that involving couples together in a weight management program can produce significant and robust weight loss. While the present intervention, designed to improve autonomy supportive behavior did not lead to overall increases in such behavior or to greater weight loss, autonomy support remains a significant predictor of behavior change. Although it is clear that social factors influence weight and related behaviors, our understanding of how to involve spouses in the weight loss process is in its infancy. To date, most couples’ weight loss programs have been of limited duration, lack a social-relational model to guide treatment development and assessment, and have had minimal impact (Leroux et al. 2013). This study continues the evolution of couples’ interventions not only by taking a truly dyadic approach, but also by parsing support dynamics through a SDT-informed lens; however, a longer full-up period may be needed to test the full SDT mediation model. Autonomy support consistently predicted behavior change, while more directive forms of support did not, suggesting that the type of support encouraged in couples’ interventions is critical to consider. Finding ways to improve the delivery of autonomy support for crucial health behaviors remains a fundamentally important goal for researchers and practitioners alike. Finally, results suggested that couples who struggle more with autonomy support may benefit more from SDT-informed interventions. It is plausible that targeting these particular couples for training in the provision of autonomy support may prove particularly effective, bolstering the potency of couple-targeted interventions even further.
Acknowledgments
FUNDING: NIH/NHLBI R21 HL125157
Footnotes
DISCLOSURES: None
TRIAL REGISTRATION: clinicaltrials.gov
References
- Black DR, Gleser LJ & Kooyers KJ (1990) A meta-analytic evaluation of couples weight-loss programs. Health Psychol, 9, 330–47. [DOI] [PubMed] [Google Scholar]
- Burgess E, Hassmen P, & Pumpa KL (2017). Determinants of adherence to lifestyle intervention in adults with obesity: a systematic review. Clin Obes, 7, 123–135. [DOI] [PubMed] [Google Scholar]
- Busby DM, Christensen C, Crane DR & Larson JH (1995) A revision of the Dyadic Adjustment Scale for use with distressed and nondistressed couples: Construct hierarchy and multidimensional scales. Journal of Marital and Family Therapy, 21, 289–308. [Google Scholar]
- Christakis NA & Fowler JH (2007) The spread of obesity in a large social network over 32 years. N Engl J Med, 357, 370–9. [DOI] [PubMed] [Google Scholar]
- Cornelius T, Gettens K & Gorin AA (2016) Dyadic Dynamics in a Randomized Weight Loss Intervention. Ann Behav Med, 50, 506–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cornelius T, Gettens K, Lenz E, Wojtanowski AC, Foster GD & Gorin AA (2018) How prescriptive support affects weight loss in weight-loss intervention participants and their untreated spouses. Health Psychol, 37, 775–781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deci EL, Eghrari H, Patrick BC & Leone DR (1994) Facilitating internalization: the self-determination theory perspective. J Pers, 62, 119–42. [DOI] [PubMed] [Google Scholar]
- Deci EL, La Guardia JG, Moller AC, Scheiner MJ & Ryan RM (2006) On the benefits of giving as well as receiving autonomy support: mutuality in close friendships. Pers Soc Psychol Bull, 32, 313–27. [DOI] [PubMed] [Google Scholar]
- Faber A & Mazlish E. 1980. How to talk so kids will listen and listen so kids will talk. New York: Avon Books. [Google Scholar]
- Feeney BC (2004). A secure base: responsive support of goal strivings and exploration in adult intimate relationships. Journal of Personality and Social Psychology, 87(5), 631. [DOI] [PubMed] [Google Scholar]
- Gorin AA, Lenz EM, Cornelius T, Huedo-Medina T, Wojtanowski AC & Foster GD (2018) Randomized Controlled Trial Examining the Ripple Effect of a Nationally Available Weight Management Program on Untreated Spouses. Obesity (Silver Spring), 26, 499–504. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Powers TA, Gettens K, Cornelius T, Koestner R, Mobley AR, Pescatello L & Medina TH (2017) Project TEAMS (Talking about Eating, Activity, and Mutual Support): a randomized controlled trial of a theory-based weight loss program for couples. BMC Public Health, 17, 749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Powers TA, Koestner R, Wing RR & Raynor HA (2013) Autonomy Support, Self-Regulation, and Weight Loss. Health Psychol. 33, 332–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gorin AA, Wing RR, Fava JL, Jakicic JM, Jeffery R, West DS, Brelje K & Dilillo VG (2008) Weight loss treatment influences untreated spouses and the home environment: evidence of a ripple effect. Int J Obes (Lond), 32, 1678–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grolnick WS & Ryan RM (1987) Autonomy in children’s learning: an experimental and individual difference investigation. J Pers Soc Psychol, 52, 890–8. [DOI] [PubMed] [Google Scholar]
- Jeffery RW & Rick AM (2002) Cross-sectional and longitudinal associations between body mass index and marriage-related factors. Obes Res, 10, 809–15. [DOI] [PubMed] [Google Scholar]
- Jensen MD, Ryan DH, Apovian CM, Loria CM, Ard JD, Millen BE, Comuzzie AG, Nonas CA, Donato KA, Pi-Sunyer FX, Hu FB, Stevens J, Hubbard VS, Stevens VJ, Jakicic JM, Wadden TA, Kushner RF, Wolfe BM & Yanovski SZ (2013) 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults: A Report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and The Obesity Society. J Am Coll Cardiol. [DOI] [PubMed] [Google Scholar]
- Joussemet M, Koestner R, Lekes N & Houlfort N (2004) Introducing uninteresting tasks to children: a comparison of the effects of rewards and autonomy support. J Pers, 72, 139–66. [DOI] [PubMed] [Google Scholar]
- Katzmarzyk PT, Hebebrand J & Bouchard C (2002) Spousal resemblance in the Canadian population: implications for the obesity epidemic. Int J Obes Relat Metab Disord, 26, 241–6. [DOI] [PubMed] [Google Scholar]
- Kenny DA, Kashy DA, Cook WL & Simpson JA. 2010. Dyadic Data Analysis (Methodology in the Social Sciences). Guilford Press. [Google Scholar]
- Koestner R, Powers TA, Carbonneau N, Milyavskaya M & Chua SN (2012) Distinguishing autonomous and directive forms of goal support: their effects on goal progress, relationship quality, and subjective well-being. Pers Soc Psychol Bull, 38, 1609–20. [DOI] [PubMed] [Google Scholar]
- Kreuter MW, & Skinner CS (2000). Tailoring: what’s in a name?. Health Education Research, 15, 1–4. [DOI] [PubMed] [Google Scholar]
- LeBlanc ES, Patnode CD, Webber EM, Redmond N, Rushkin M, & O’Connor EA (2018). Behavioral and pharmacotherapy weight loss interventions to prevent obesity-related morbidity and mortality in adults: Updated evidence report and systematic review for the US Prevention Services Task Force, JAMA, 320, 1172–1191. [DOI] [PubMed] [Google Scholar]
- Leroux JS, Moore S & Dube L (2013) Beyond the “I” in the obesity epidemic: a review of social relational and network interventions on obesity. J Obes, 2013, 348249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Levesque CS, Williams GC, Elliot D, Pickering MA, Bodenhamer B & Finley PJ (2007) Validating the theoretical structure of the Treatment Self-Regulation Questionnaire (TSRQ) across three different health behaviors. Health Educ Res, 22, 691–702. [DOI] [PubMed] [Google Scholar]
- Mata J, Richter D, Schneider T, & Hertwig R (2018). How cohabitation, marriage, separation, and divorce influence BMI: a prospective study. Health Psychology, 37, 948–958. [DOI] [PubMed] [Google Scholar]
- McLean N, Griffin S, Toney K & Hardeman W (2003) Family involvement in weight control, weight maintenance and weight-loss interventions: a systematic review of randomised trials. Int J Obes Relat Metab Disord, 27, 987–1005. [DOI] [PubMed] [Google Scholar]
- Musto A, Jacobs K, Nash M, DelRossi G & Perry A (2010) The effects of an incremental approach to 10,000 steps/day on metabolic syndrome components in sedentary overweight women. J Phys Act Health, 7, 737–45. [DOI] [PubMed] [Google Scholar]
- Norton R (1983) Measuring marital quality: A critical look at the dependent variable. Journal of Marriage and The Family, 45, 10. [Google Scholar]
- Perri MG, Nezu AM, McKelvey WF, Shermer RL, Renjilian DA & Viegener BJ (2001) Relapse prevention training and problem-solving therapy in the long-term management of obesity. J Consult Clin Psychol, 69, 722–6. [PubMed] [Google Scholar]
- Pescatello LS, Arena R, Rieble D, Thompson P, M. (2013). ACSM’s Guidelines for Exercise Testing and Prescription, 9th edition. Baltimore, MD: Lippincott Williams & Wilkins. [DOI] [PubMed] [Google Scholar]
- Powers TA, Koestner R & Gorin AA (2008) Autonomy support from family and friends and weight loss in college women. Families, Systems, and Health, 26, 13. [Google Scholar]
- Ryan RM & Deci EL (2000a) Intrinsic and Extrinsic Motivations: Classic Definitions and New Directions. Contemp Educ Psychol, 25, 54–67. [DOI] [PubMed] [Google Scholar]
- Ryan RM & Deci EL (2000b) Self-determination theory and the facilitation of intrinsic motivation, social development, and well-being. Am Psychol, 55, 68–78. [DOI] [PubMed] [Google Scholar]
- Saelens BE, Arteaga SS, Berrigan D, Ballard RM, Gorin AA, Powell-Wiley TM, Pratt C, Reedy J, & Zenk SN (2018). Accumulating data to optimally predict obesity treatment (ADOPT) core measures: Environmental domain. Obesity, 26, S35–S44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schierberl Scherr AE, McClure Brenchley KJ & Gorin AA (2013) Examining a ripple effect: do spouses’ behavior changes predict each other’s weight loss? J Obes, 2013, 297268. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silva MN, Markland D, Carraca EV, Vieira PN, Coutinho SR, Minderico CS, Matos MG, Sardinha LB & Teixeira PJ (2011) Exercise autonomous motivation predicts 3-yr weight loss in women. Med Sci Sports Exerc, 43, 728–37. [DOI] [PubMed] [Google Scholar]
- Silva MN, Vieira PN, Coutinho SR, Minderico CS, Matos MG, Sardinha LB & Teixeira PJ (2010) Using self-determination theory to promote physical activity and weight control: a randomized controlled trial in women. J Behav Med, 33, 110–22. [DOI] [PubMed] [Google Scholar]
- Smith LP, Ng SW & Popkin BM (2013) Trends in US home food preparation and consumption: analysis of national nutrition surveys and time use studies from 1965–1966 to 2007–2008. Nutr J, 12, 45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sturm R (2004) The economics of physical activity: societal trends and rationales for interventions. Am J Prev Med, 27, 126–35. [DOI] [PubMed] [Google Scholar]
- Teixeira PJ, Silva MN, Mata J, Palmeira AL & Markland D (2012) Motivation, self-determination, and long-term weight control. Int J Behav Nutr Phys Act, 9, 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- The NS & Gordon-Larsen P (2009) Entry into romantic partnership is associated with obesity. Obesity (Silver Spring), 17, 1441–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Thomas S, Reading J & Shephard RJ (1992) Revision of the Physical Activity Readiness Questionnaire (PAR-Q). Can J Sport Sci, 17, 338–45. [PubMed] [Google Scholar]
- Urbaniak GC, & Plous S (2013). Research Randomizer (Version 4.0) [Computer software]. http://www.randomizer.org/.
- Wadden TA, West DS, Delahanty L, Jakicic J, Rejeski J, Williamson D, Berkowitz RI, Kelley DE, Tomchee C, Hill JO & Kumanyika S (2006) The Look AHEAD study: a description of the lifestyle intervention and the evidence supporting it. Obesity (Silver Spring), 14, 737–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GC & Deci EL (2001) Activating patients for smoking cessation through physician autonomy support. Med Care, 39, 813–23. [DOI] [PubMed] [Google Scholar]
- Williams GC, Freedman ZR & Deci EL (1998) Supporting autonomy to motivate patients with diabetes for glucose control. Diabetes Care, 21, 1644–51. [DOI] [PubMed] [Google Scholar]
- Williams GC, Gagne M, Ryan RM & Deci EL (2002) Facilitating autonomous motivation for smoking cessation. Health Psychol, 21, 40–50. [PubMed] [Google Scholar]
- Williams GC, Lynch MF, McGregor HA, Ryan RM, Sharp D & Deci EL. 2006a. Validation of the “Important Other” Climate Questionnaire: Assessing autonomy support for health-related change. 179–194. Families, Systems, and Health. [Google Scholar]
- Williams GC, McGregor H, Sharp D, Kouldes RW, Levesque CS, Ryan RM & Deci EL (2006b) A self-determination multiple risk intervention trial to improve smokers’ health. J Gen Intern Med, 21, 1288–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams GC, McGregor HA, Sharp D, Levesque C, Kouides RW, Ryan RM & Deci EL (2006c) Testing a self-determination theory intervention for motivating tobacco cessation: supporting autonomy and competence in a clinical trial. Health Psychol, 25, 91–101. [DOI] [PubMed] [Google Scholar]