Abstract
Background:
Whether medical or recreational cannabis legalization impacts alcohol or cigarette consumption is a key question as cannabis policy evolves, given the adverse health effects of these substances. Relatively little research has examined this question. The objective of this study was to examine whether medical or recreational cannabis legalization was associated with any change in state-level per capita alcohol or cigarette consumption.
Methods:
Dependent variables included per capita consumption of alcohol and cigarettes from all 50 U.S. states, estimated from state tax receipts and maintained by the Centers for Disease Control and National Institute for Alcohol Abuse and Alcoholism, respectively. Independent variables included indicators for medical and recreational legalization policies. Three different types of indicators were separately used to model medical cannabis policies. Indicators for the primary model were based on the presence of active medical cannabis dispensaries. Secondary models used indicators based on either the presence of a more liberal medical cannabis policy (“non-medicalized”) or the presence of any medical cannabis policy. Difference-in-difference regression models were applied to estimate associations for each type of policy.
Results:
Primary models found no statistically significant associations between medical or recreational cannabis legalization policies and either alcohol or cigarette sales per capita. In a secondary model, both medical and recreational policies were associated with significantly decreased per capita cigarette sales compared to states with no medical cannabis policy. However, post hoc analyses demonstrated that these reductions were apparent at least two years prior to policy adoption, indicating that they likely result from other time-varying characteristics of legalization states, rather than cannabis policy.
Conclusion:
We found no evidence of a causal association between medical or recreational cannabis legalization and changes in either alcohol or cigarette sales per capita.
INTRODUCTION
Although cannabis use has been illegal at the federal level in the United States since the 1930s, an array of liberalized state policies have removed or reduced criminal penalties and, in some cases, made cannabis commercially available. Furthermore, more than 35 states have passed medical cannabis policies (Cerdá et al., 2018), and recreational use will be legal in at least eleven states and the District of Columbia as of January 2020 (Marijuana Policy Project, 2019).
A large body of literature has examined the health effects of cannabis use. While there is strong evidence that cannabis impairs learning, attention, and memory, there is considerable debate about the long-term adverse health effects (Batalla et al., 2013; Volkow, Baler, Compton, & Weiss, 2014; National Academies of Sciences, 2017). However, if cannabis legalization results in increases in cannabis use, indirect effects on health may also occur by increasing or reducing the use of other drugs. For example, a number of studies have suggested that cannabis may serve as a substitute to licit and illicit opioid use, though more recent work has questioned this result (Bachhuber, Saloner, Cunningham, & Barry, 2014; Powell, Pacula and Jacobson 2015; Bradford, Bradford, Abraham, & Bagwell Adams, 2018; Wen & Hockenberry, 2018, Shover, Davis, Gordon, & Humphreys, 2019).
Most notably, cannabis policy may impact health through effects on alcohol and cigarette consumption. If cannabis becomes more readily available, people may turn from alcohol or cigarettes to cannabis, leading to a decrease in alcohol or cigarette consumption via economic substitution. On the other hand, if people prefer to use these drugs together, they may be economic complements, which would lead to increases in alcohol and/or cigarette consumption. Generally, researchers address the question of substitution versus complementarity by studying the effects of price or availability of one drug on the consumption of another. For example, Farrelly and colleagues found that increasing prices for alcohol resulted in reduced cannabis consumption among US youth, suggesting complementarity (Farrelly, Bray, Zarkin, Wendling, & Pacula, 1999). In contrast, Cameron & Williams, (2001) found that cannabis price increases in Australia led to decreased cannabis consumption in the general population, and DiNardo & Lemieux (2001) found negative associations between higher drinking ages and cannabis consumption. These latter two studies suggest cannabis-alcohol substitution. But whether an individual increases or decreases consumption of other drugs in response to legal access to cannabis may depend on the motivation behind that person’s use, which varies widely across individuals (Simons, Gaher, Correia, Hansen, & Christopher, 2005). For example, O’Hara, Armeli, & Tennen (2016) found that college students who used substances to cope with negative affect were more likely to substitute alcohol and cannabis for each other, whereas other students used these substances complementarity. If individual differences impact substitution and complementarity behaviors, then whether a pair of drugs acts as substitutes or complements to each other may vary by time, place, population, and the nature of the policy change itself. Therefore, it is not surprising that studies addressing these questions do not yield simple “one-size-fits-all” answers (see, for example, the review by Guttmannova et al., 2016).
Differences in individual responses notwithstanding, policymakers and health economists may be primarily interested in substitution and complementarity to inform prediction of the impacts of cannabis policy liberalization on other drugs at a population-level. Therefore, the aim of this study is to evaluate the effect of changes in cannabis policy on per capita cigarette and alcohol consumption. We exploit within-state policy differences over time to estimate associations between changes in state cannabis policy and changes in state-wide alcohol and cigarette consumption as measured by state tax receipt data. While we use the most recently available data (2016 at the time of writing), it still may be too early to draw conclusions about recreational cannabis legalization, which was only implemented in five states as of 2015 (Hall & Lynskey, 2016). Therefore, we also examine the impact of medical cannabis policies. As described below, because studies are mixed regarding whether all medical cannabis policies result in increased adult cannabis use, we take three different approaches in categorizing states with respect to details of their medical cannabis policy status.
Whether increases or decreases in alcohol or cigarette consumption occur in response to medical and recreational cannabis legalization depends on the degree to which these policies result in meaningful increases in cannabis use. With respect to medical cannabis legalization, it is not clear that passage of a medical cannabis policy per se results in increased prevalence or frequency of cannabis use (Harper, Strumpf, & Kaufman, 2012; Lynne-Landsman, Livingston, & Wagenaar, 2013; Pacula & Smart, 2017). On the other hand, there is convincing evidence that active dispensaries and other more permissive elements of medical cannabis policy increase the prevalence and frequency of cannabis use (Heaton, & Sevigny, 2015; Hockenberry, & Cummings, 2015; Pacula & Smart, 2017; Williams et al., 2017). There is relatively little research from nationally representative samples to date on the impact of recreational legalization of cannabis, and it may be too early to tell if such policies result in long-term and substantial changes in the cannabis use landscape (Hall & Lynskey, 2016; Pacula & Sevigny, 2014). However, one study has shown increases in the prevalence of cannabis use among adolescents after legalization in Washington, but not Colorado (Cerdá et al., 2017). A study focused on college students suggests increases in the prevalence of cannabis use following recreational legalization in Oregon (Kerr, Bae, & Koval, 2018). To date, no studies have appeared that have examined the effect of recreational policies on adult use. However, it is largely presumed that legalization leads to decreased price and that this almost certainly results in increased consumption. However, the degree to which this occurs remains unknown (Kilmer, Caulkins, Pacula, MacCoun, & Reuter, 2010).
Related to our central question of whether medical and recreational cannabis policies lead to changes in per capita alcohol or cigarette consumption at the population level, the most relevant recent work may be a study suggesting a marked reduction in per capita alcohol sales in retail venues participating in the Nielsen point-of-sale scanner system in states that enacted medical cannabis policies during the years 2006-2015 (Baggio, Chong, & Kwon, 2017). We are unaware of any studies examining the impact of medical or recreational cannabis legalization on cigarette consumption, though Agrawal, Budney & Lynskey (2012) reviewed a number of economic and policy studies based on other policy variables that consistently suggested complementarity. Thus, there are few studies on the impact of medical or recreational cannabis policies on alcohol consumption, and, to our knowledge, there are no studies investigating the effect of cannabis policy change on cigarette consumption. Given that alcohol and cigarettes are among the top contributors to morbidity, mortality, and health care costs in the United States, the impact of medical and recreational legalization on consumption of these drugs is a key policy question. (Bouchery, Harwood, Sacks, Simon, & Brewer, 2011; Goodchild, Nargis, & Tursan d’Espaignet, 2018; Johnson et al., 2014; Stahre, Roeber, Kanny, Brewer, & Zhang, 2014).
METHODS
Overview.
Our objective was to examine the effect of state recreational and medical cannabis policies on per capita consumption of alcohol and cigarettes as measured by state tax receipts. We exploited variations in both types of policies between states and over time, utilizing a difference-in-differences regression approach, also known as a two-way fixed effects model (Angrist & Pischke, 2009). This approach estimates the effect of policy change on outcome variables independently of stable state characteristics and national trends by including dummy variables (fixed effects) for state and time. This is a multi-group multi-period extension of a simple difference-in-difference approach involving single treatment and control groups studied before and after a treatment or intervention. As such, regression coefficients reflect the magnitudes of within-state changes in cannabis policy in relation to within-state changes in alcohol and cigarette consumption. There are substantial differences in medical cannabis policy allowances across states, and we utilized several different series of model specifications to address these differences, with each series using a different coding approach for medical cannabis policy. Within each series, we estimated three models, with each successive model including additional state-level covariates.
Policy coding for the first series of models is based on the work of Pacula and colleagues (2015), who found that the presence of active medical cannabis dispensaries was associated with higher rates of recreational use. The second series of models is based on the work of Williams, Olfson, Kim, Martins & Kleber (2016), who differentiate between ‘medicalized’ and ‘non-medicalized’ medical cannabis policies. The former set of policies has characteristics similar to “traditional medical care and pharmaceutical regulation,” such as physician training and requirement of an established doctor-patient relationship, whereas the latter is less well-regulated and typically has much higher enrollment rates. States that implemented non-medicalized medical cannabis policies have experienced increases in cannabis use in adults aged 26 and older compared to states that implemented medicalized policies and states without any medical cannabis policy (Williams, Santaella-Tenorio, Mauro, Levin, & Martins, 2017). Finally, in the third series of models, we simply coded whether or not a state had implemented any medical cannabis policy. Pacula and colleagues showed that this approach may obscure the impact of more permissive medical policies on cannabis consumption, but, we employ this alternative specification because it has been used in a number of prior studies, (e.g., Anderson et al., 2013; Anderson, Hansen, & Rees, 2015; Anderson, Rees, & Sabia, 2014; Baggio et al., 2017; Bradford et al., 2018; Wen & Hockenberry, 2018).
Dependent Variables:
Per capita consumption of alcohol from all 50 states from 1990 to 2016 was obtained from the most recently available alcohol sales surveillance report of the National Institute on Alcohol Abuse and Alcoholism (NIAAA) (Haughwout & Slater, 2018). For the report, alcohol beverage sales in each state were compiled by the Alcohol Epidemiologic Data System (AEDS). The AEDS calculates sales data for wine, beer, and spirits from tax receipts and converts beverage volume into gallons of ethanol based on typical alcohol content for each type of beverage. Per capita consumption is then calculated by dividing by the state population of individuals over the age of 14. Per capita consumption data of cigarettes, measured in packs per person for each state from 1990 to 2016, was obtained from a report of the Centers for Disease Control and Prevention Office on Smoking and Health (2018). Sales are calculated from state-level cigarette tax receipts and collected from The Tax Burden on Tobacco (Orzechowski & Walker, 2013), the annual compendium on tobacco revenue and industry statistics.
Independent Variable:
State Cannabis Policies – For our primary models (Series I), we utilized the policy coding framework applied by Powell et al. (2015). This framework is based on earlier work by Pacula et al. (2015) differentiating states with operational medical cannabis dispensaries from states that have medical cannabis policies, but no operational dispensaries. For each year, the states’ policies were classified as follows: (a) legal recreational use, (b) legal medical use with operational dispensaries, (c) legal medical use without dispensaries or prohibited use. Two secondary series of models that took alternative policy coding approaches were also analyzed. The first of these alternative approaches used in models labeled “Series II” was based on Williams and colleagues’ (2016) study, who categorized state medical cannabis programs as either “medicalized” programs or “non-medicalized” programs. The results of this study suggest that non-medicalized programs had enrollment rates in the order of ~0.1% of the population or less, while non-medicalized programs accounted for over 99% of enrollment nationwide and were associated with increased rates of adult cannabis use. Thus, in the series of models utilizing this approach, we categorized states as: (a) legal recreational use, (b) non-medicalized legal medical use, and (c) medicalized legal medical use or prohibited use. In another series of secondary models, labeled “Series III”, we ignored between-state differences in medical cannabis policies and coded for the presence or absence of a policy permitting medical use of cannabis (Anderson et al., 2013). For this series, states were categorized as: (a) legal recreational use, (b) legal medical use, or (c) prohibited use. State policy categories for each of the three frameworks were extracted from supplementary tables in publications by Anderson et al. (2013), Powell et al. (2015), and Williams et al. (2016), respectively.
Covariates.
In addition to state and year fixed effects, we controlled for selected time-varying state economic and demographic variables that may be correlated with cannabis policy changes as well as alcohol or cigarette consumption rates. These included: percent of the population that were African American, Asian, Native American, and Hispanic; age distribution, i.e., percentages of individuals in the age categories 0-14, 15-19, 20-29, 30-49, 50-64, and 65 and over; percentage of families living in poverty, state unemployment rate averaged over each year, percentage of the population with a college degree, a measure of citizen political ideology, beer excise tax, cigarette excise tax, legal blood alcohol content limit of .08 for driving (as opposed to .10), and a measure of smoke free air policy restrictiveness. Data sources for these variables are listed in Table 1.
Table 1.
Sources for each variable used in the regression models
| Alcohol Consumption | National Institute on Alcohol Abuse and Alcoholism (Haughwout and Slater, 2018; Table 2) (https://pubs.niaaa.nih.gov/publications/surveillance110/CONS16.pdf). |
| Cigarette Consumption | CDC: Office of Smoking and Health - The Tax Burden on Tobacco, Volume 51 https://chronicdata.cdc.gov/Policy/The-Tax-Burden-on-Tobacco-Volume-51-1970-2016/7nwe-3aj9 |
| Marijuana Policies | Anderson et al, 2013 (Anderson et al., 2013), Powell et al, 2015 (Powell et al., 2015) , Williams et al, 2017 (Williams et al., 2016) |
| Age composition | National Cancer Institute: Surveillance, Epidemiology, and End Results. https://seer.cancer.gov/popdata/download.html |
| Ethnicity composition | National Cancer Institute: Surveillance, Epidemiology, and End Results https://seer.cancer.gov/popdata/download.html |
| Per capita income | University of Kentucky: Center for Poverty Research. http://www.ukcpr.org/data |
| Poverty rate | University of Kentucky: Center for Poverty Research. http://www.ukcpr.org/data |
| Unemployment rate | Bureau of Labor Statistics: Local Area Unemployment Statistics. https://www.bls.gov/web/laus/laumstch.htm |
| College graduation rate | University of Minnesota Integrated Public Use Microdata Series - Current Population Survey. https://cps.ipums.org/cps/citation.shtml |
| Political ideology | Update of Berry et al (1998) (Berry, Ringquist, Fording, & Hanson, 1998) https://rcfording.wordpress.com/state-ideology-data/ |
| Beer tax | Alcohol Policy Information System for 1999-2016 (https://alcoholpolicy.niaaa.nih.gov/file-page/data-request-form/78) Statewide Availability Data System for 1990-1999 (Ponicki, 2004) |
| Cigarette tax | CDC: Office of Smoking and Health - The Tax Burden on Tobacco, Volume 51 https://chronicdata.cdc.gov/Policy/The-Tax-Burden-on-Tobacco-Volume-51-1970-2016/7nwe-3aj9 |
| BAC <0.08 law | Alcohol Policy Information System for 1999-2016 Statewide Availability Data System for 1990-1999 https://alcoholpolicy.niaaa.nih.gov/file-page/data-request-form/78 |
| Smoke free air law | CDC: Office of Smoking and Health https://chronicdata.cdc.gov/Legislation/CDC-STATE-System-Tobacco-Legislation-Smokefree-Ind/32fd-hyzc |
Statistical analysis.
We used linear regression to model state per capita alcohol and cigarette consumption as a function of state medical and recreational cannabis policy. The dependent variables were log-transformed so that regression coefficients could be interpreted as the proportional change in alcohol or cigarette consumption associated with a change in policy, relative to cannabis-prohibiting states (more precisely, the proportional change would be exp(β)-1, but for small absolute values of β, such as 0.1 or less, the two are approximately equal). For each outcome and within each of the three series of models, we estimated three linear regression models with each successive model incorporating additional time-varying covariates. In the first model, we included recreational and medical cannabis policy indicators, and state and year fixed effects only. In the second model, we added covariates for state demographics, i.e., race/ethnicity and age composition. Finally, in the third model, we added the state policy and economic covariates listed above. Analyses were weighted by population estimates for each state and year using the United States Census intercensal estimates (“Surveillance, Epidemiology, and End Results (SEER) Program” n.d.). Models were estimated for the full-time period from 1990 to 2016. To account for within-state clustering of observations, models were estimated using the SAS procedure “surveyreg” specifying state as the clustering unit (SAS Institute, Cary, NC).
Post hoc Analyses.
As described in “Results,” inconsistent results were observed for models examining per capita cigarette sales in relation to cannabis policies and coefficient estimates were highly sensitive to covariate inclusion, suggesting that observed and possibly unobserved time-varying factors might be contributing to trends in per capita cigarette sales. We undertook two post hoc analyses to address this possibility. In the first, we re-estimated the fully adjusted Series III models (which suggested significant negative associations between cannabis policies and per capita cigarette sales), with the addition of state-specific time trends. This approach uses a continuous time variable interacted with state to further control for linear trends in the outcome that might vary by state. Second, we re-estimated the fully-adjusted model without state-specific trends, but with the inclusion of pre-trend indicators, i.e., lead policy variables that would detect any significant differences in per capita cigarette sales prior to the implementation of cannabis policy. Specifically, we included leading indicators for one- and two-year periods prior to implementation of medical or recreational cannabis policies (The rationale behind both of these types of robustness checks is explained in a recent review by Wing, Simon, & Bello-Gomez (2018)). We also applied these same checks to our primary model series (Series I) for per capita alcohol sales to assess the robustness of those results to alternative specifications. An additional post hoc analysis was aimed at understanding why results were sensitive to model specification: we examined whether any of the time-varying state-level covariates included in our adjusted models were significantly associated with the passage of policies. In other words, we used the covariate as the dependent variable and policy as the predictor variable while adjusting for state and year fixed effects.
RESULTS
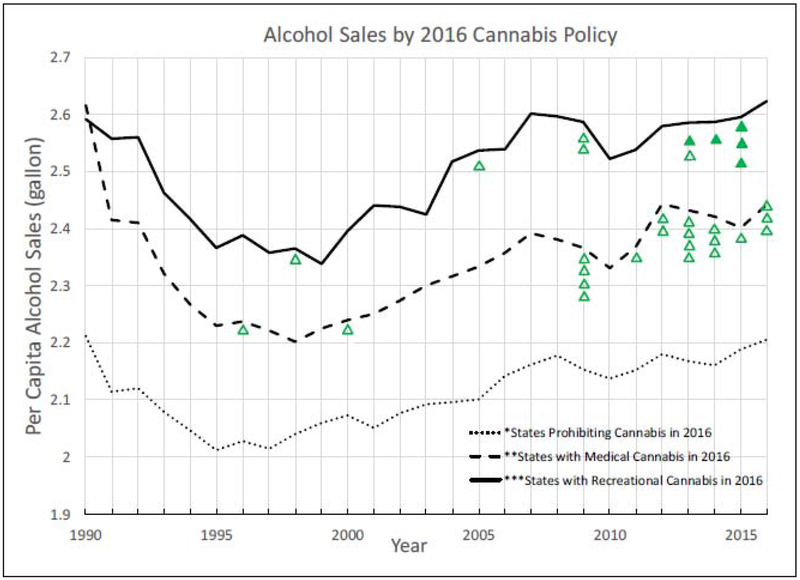
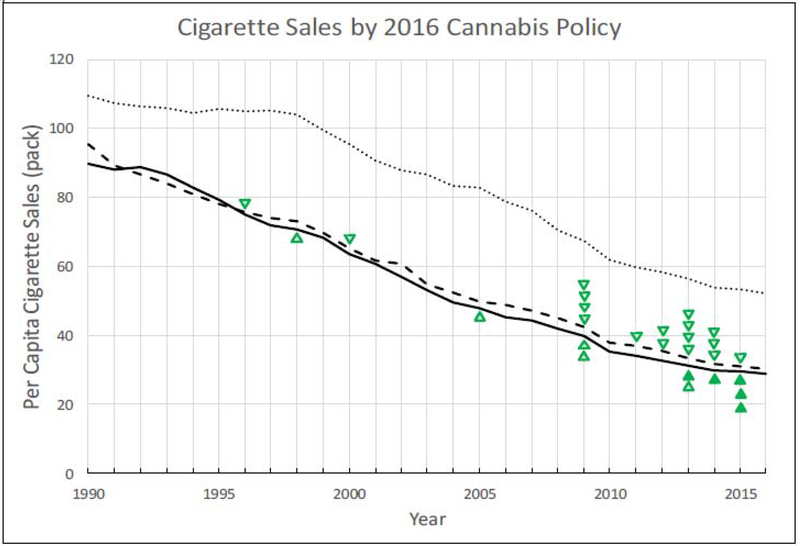
Figures 1 and 2 compare trends in per capita alcohol and cigarette sales over time categorized by whether the state had implemented a medical marijuana policy (with active dispensaries) or enacted a recreational marijuana legalization policy by 2016. Per capita alcohol sales declined for all states through the 1990s (Figure 1), but began increasing around 2000, regardless of 2016 cannabis policy. States that had implemented recreational cannabis policies tended to have higher per capita alcohol sales rates across the full study period compared to other states. States with neither legalized medical nor recreational cannabis use had lower per capita alcohol sales compared to other states. Per capita cigarette sales declined monotonically since 1990 in all states regardless of cannabis policy (Figure 2). Notably, per capita cigarette sales were highest in states that did not adopt medical or recreational legalization; sales were lower, but very close to each other, in states that had adopted medical and/or recreational cannabis policies.
Figure 1 -.
Per capita state alcohol sales from 1990-2016. States are categorized into 3 groups based on cannabis policy in year 2015. Medical cannabis policy is categorized according to the primary specification based on work by Pacula et al (2015a). Dotted lines represent states where both medical and recreational cannabis remained illegal, dashed lines represent states with medical but not recreational legalization, and solid lines represent states that had both medical and recreational legalization as of 2016. Hollow triangles passage of medical cannabis laws. Solid triangles represent passage of recreational cannabis laws.
Figure 2 -.
Per capita state cigarette sales from 1990-2016. States are categorized into 3 groups based on cannabis policy in year 2016. Medical cannabis policy is categorized according to the primary specification based on work by Pacula et al (2015a) Dotted lines represent states where both medical and recreational cannabis remained illegal, dashed lines represent states with medical but not recreational legalization, and solid lines represent states that had both medical and recreational legalization as of 2016. Hollow triangles indicate states passing medical cannabis laws. Solid triangles represent states passing recreational cannabis laws. (Direction of triangles varies only to fit symbols in space between lines.)
To present results succinctly for both the main and alternative independent variable codings, and for all three steps of covariate inclusion, only the regression coefficients for medical and recreational policy indicators are shown in the tables presented in the main body of the text (Tables 2 and 3 for alcohol and cigarette analyses, respectively). The textual presentation focuses mainly on the primary series of models that contrast states with legal, active medical cannabis dispensaries from other states. We briefly discuss general trends and statistical significance for coefficients derived from the two series of secondary models; policy coefficient estimates from all series of models are presented in Tables 2 and 3. Coefficients for covariates estimated from the primary (Series I) models are shown in Supplementary Tables 1 and 2 for alcohol and cigarette analyses, respectively.
Table 2.
Effect of cannabis policy on alcohol consumption in a 3-tier regression for 3 policy specifications.a
| Policy Specification | Law Type | Model Ib | Model IIc | Model IIId | |||
|---|---|---|---|---|---|---|---|
| βe | 95% CI | βe | 95% CI | βe | 95% CI | ||
| Series I | Medical | −0.031 | −0.064; 0.003 | −0.002 | −0.017; 0.013 | 0.005 | −0.011; 0.021 |
| Recreational | −0.023 | −0.068; 0.022 | 0.007 | −0.035; 0.050 | 0.013 | −0.028; 0.055 | |
| Series II | Medical | −0.035 | −0.070; 0.001 | −0.007 | −0.024; 0.010 | −0.003 | −0.020; 0.014 |
| Recreational | −0.034 | −0.089; 0.020 | 0.003 | −0.045; 0.050 | 0.003 | −0.042; 0.048 | |
| Series III | Medical | −0.020 | −0.052; 0.012 | −0.002 | −0.017; 0.012 | 0.004 | −0.007; 0.015 |
| Recreational | −0.026 | −0.081; 0.029 | 0.006 | −0.038; 0.051 | 0.014 | −0.025; 0.053 | |
Note: This table lists only the association between cannabis policy and alcohol consumption. See supplementary Table 3 for full covariate listing. No estimates were significant at the p<0.05 threshold.
Series I, II and III specifications correspond to codings derived from Pacula et al (2015a), Williams et al (2016), and Anderson et al (2013), respectively.
Model I incorporates only state and year fixed effects as covariates.
Model II incorporates additional covariates for state distributions of age and race.
Model III further incorporates additional state-level covariates including per capita income, poverty rate, unemployment rate, college graduation rate, political ideology, alcohol tax, 0.08 BAC law, cigarette tax, and smoke-free air legislation.
Proportional change in alcohol consumption, relative to states prohibiting cannabis use, can be derived as [exp(β)-1]. For |β| << 1, β ~ exp(β).
Table 3.
Effect of cannabis policy on cigarette consumption in a 3-tier regression for 3 policy specifications.a
| Policy Specification | Law Type | Model Ib | Model IIc | Model IIId | |||
|---|---|---|---|---|---|---|---|
| βe | 95% CI | βe | 95% CI | βe | 95% CI | ||
| Series I | Medical | −0.105 | −0.225; 0.015 | −0.035 | −0.132; 0.061 | 0.022 | −0.044; 0.087 |
| Recreational | −0.198 | −0.424; 0.027 | −0.990 | −0.303; 0.105 | −0.047 | −0.175; 0.081 | |
| Series II | Medical | −0.130* | −0.251; −0.008 | −0.080* | −0.154; −0.006 | −0.038 | −0.092; 0.014 |
| Recreational | −0.240 | −0.496; 0.017 | −0.146 | −0.349; 0.058 | −0.101 | −0.219; 0.018 | |
| Series III | Medical | −0.176*** | −0.238; −0.114 | −0.119** | −0.197; −0.042 | −0.062* | −0.120; −0.003 |
| Recreational | −0.313*** | −0.529; −0.097 | −0.202* | −0.374; −0.031 | −0.132* | −0.239; −0.025 | |
Note: This table lists only the association between cannabis policy and cigarette consumption. See supplementary Table 3 for full covariate listing.
P-values:
<0.05,
0.001
Series I, II and III specifications correspond to codings derived from Pacula et al (2015a), Williams et al (2016), and Anderson et al (2013), respectively.
Model I incorporates only state and year fixed effects as covariates.
Model II incorporates additional covariates for state distributions of age and race.
Model III further incorporates additional state-level covariates including per capita income, poverty rate, unemployment rate, college graduation rate, political ideology, alcohol tax, 0.08 BAC law, cigarette tax, and smoke-free air legislation.
Proportional change in alcohol consumption, relative to states prohibiting cannabis use, can be derived as [exp(β)-1]. For |β| << 1, β ~ exp(β).
The association between per capita alcohol sales and both medical and recreational cannabis policies (Table 2) was not statistically significant at the conventional p<0.05 threshold for any model in any of the three series. In the Series I model, adjusting only for state and year fixed effects, there was a trend toward a negative association of medical cannabis policies and per capita alcohol sales (β= −0.031; 95% CI: −0.064, 0.003, p=0.075)—suggesting a possible reduction in per capita alcohol sales associated with medical cannabis legalization. However, after covariate adjustment, this coefficient was very close to zero (β=0.005; 95% CI: −0.011, 0.021, p=0.88) as was the coefficient for recreational policy. Several time-varying covariates were associated with alcohol consumption (Supplementary Table 1). Specifically, per capita income was positively associated with alcohol consumption, while age and proportion of Hispanic residents was negatively associated.
Results of models for the association between cigarette consumption and cannabis policies are summarized in Table 3, full covariate listings for the adjusted primary (Series I) models are provided in Supplementary Table 2. For the primary models, in the specification adjusting only for state and year fixed effects, there was a non-significant trend toward reduced cigarette consumption for both medical (β=−0.105; 95% CI: −0.225, 0.015, p=0.09) and recreational policies (β=−0.198; 95% CI: −0.424, 0.027, p=0.056) but these coefficients were markedly reduced in the partially and fully adjusted models (fully adjusted model, for medical cannabis policies, β=0.022; 95% CI: −0.044, 0.087, p=0.51; recreational β=−0.047; 95% CI: −0.175, 0.081, p=0.47). Series II models contrasted states with non-medicalized cannabis policies from those with medicalized policies combined with states without medical cannabis. Non-medicalized cannabis policies were significantly and negatively associated with cigarette consumption in the two partially adjusted models, but not in the fully adjusted models, and the policy coefficient estimates were highly sensitive to model specification. In Series III models— that contrasted states with any medical cannabis policy with those with none, regardless of dispensaries or medicalization—the coefficients were statistically significant even in the fully adjusted models. However, as with the other two model series, each step of covariate adjustment resulted in a marked reduction in the magnitude of these coefficients. Several of the state-level covariates were significantly associated with per capita cigarette sales, including Native and Asian ethnicity (negative and positive, respectively), as well as cigarette taxes and stronger smoke-free air policies, both of which were negatively associated with cigarette consumption (Supplementary Table 2).
Results of Post hoc analyses.
Because of the sensitivity of estimates to model specification, we sought to examine the robustness of the results from the Series III models, which suggested that implementation of any medical or recreational cannabis policy was associated with reductions in per capita cigarette sales. In the first post hoc analysis, we added terms for state-specific linear trends (i.e., state interacted with year cast as a continuous variable). This resulted in a marked reduction in the magnitude of the estimates for both the medical and recreational policy coefficients such that neither approached statistical significance (β=−.019; 95% CI: −0.051, 0.013; p=0.24 for medical and β=−0.052; 95% CI: −0.120, 0.016; p=0.70 for recreational). In a second post hoc robustness check, one- and two-year policy lead indicators were included in the model (but state-by-year linear trends were not included, because this approach may be overly-conservative; see Wing et al., 2018). When these were included, the estimates for policy effects were non-significant and slightly positive (Supplementary Table 3). The estimates for the two-year policy lead indicators were comparable in magnitude to those of the estimates of the policy effects in the specification that did not include leading indicators. These results indicated that trends toward lower per capita cigarette sales were evident at least two years prior to the implementation of policy liberalization in states that adopted these policies.
The same robustness checks were conducted for the primary alcohol analyses. This was done to check the possibility that liberalization states experienced reductions in per capita alcohol sales that might have been obscured by differential state trends prior to policy implementation. The addition of state-specific linear trends did not result in substantial changes in the estimates for the policy effects – both remained close to zero and non-significant (Supplementary Table 4). The same was true of both one- and two-year policy lead indicators, suggesting that, on average, trends in per capita alcohol sales in medical and recreational legalization states were similar to those in non-legalization states during the years prior to policy implementation.
DISCUSSION
The results of this study do not suggest that cannabis legalization results in either reduced or increased per capita sales of alcohol or cigarettes, and do not support either substitution or complementarity hypotheses about the relations between cannabis consumption and either alcohol or cigarette consumption. The interpretation is most straightforward for alcohol: using three different policy variable specifications, there were no significant associations between either medical or recreational legalization and per capita alcohol sales. Near-significant associations suggesting slightly lower per capita alcohol sales (~2-4%) were evident in models including only state and year fixed effects but not for those including time-varying state covariates. Estimates in the fully adjusted models were very close to zero. Regarding medical cannabis policy, we cannot rule out 1 or 2% increases or decreases in sales based on 95% confidence intervals. For recreational policy, confidence intervals are wider, and increases or decreases in per capita alcohol sales in the order of 3-5% cannot be ruled out. Additional years of post-legalization data will facilitate more precise estimates of the effects of recreational legalization policy in the near future.
The results for per capita cigarette sales are more complex. Although our primary series of analyses did not suggest statistically significant reductions in sales, coefficient estimates for most models were negative, and for the models that treated all medical legalization states similarly (i.e., disregarded dispensary presence or other policy details), estimates were statistically significant and suggested substantial reductions per capita in cigarette sales: about 6% for medical legalization and 13% for recreational legalization. However, post hoc analyses suggested that these effects were due to trends that were in place in states that adopted these policies prior to the actual implementation of the policies. This result is partially foreshadowed in Figure 2, which plots the per capita cigarette sales trends in the recreational, medical, and non-legalization states. It can be seen that sales trends were less negative in the non-legalization compared to other states over the years 1990-1999 but paralleled trends in states that eventually legalized medical and recreational marijuana in later years. Furthermore, post hoc analyses treating medical and recreational policy implementation as dependent variables showed that liberalization states were more likely to adopt smoke-free air policies and to undergo demographic shifts in the population toward older age over time. In other words, there are important, time-varying differences between states that have liberalized cannabis policies compared to those that have not.
Our findings do not suggest either substitution or complementarity effects, but it may be that the impact of these policies on the prevalence and frequency of cannabis use is too small to translate into changes in consumption of either alcohol or cigarettes. Nonetheless, our results contradict the findings of Baggio and colleagues (2017) who found that medical cannabis legalization resulted in a 13% reduction in per capita alcohol sales. A strength of that study was the availability of county-level sales data, which allowed those authors to compare geographically proximate counties in medical cannabis states with those in states without medical cannabis policies. The availability of monthly data also allowed a more fine-grained analysis of policy timing (lead and lag effects), which suggested that the reduction in per capita alcohol sales corresponded closely in time with the implementation of medical cannabis policies (Baggio et al., 2017). On the other hand, that study relied on Nielsen retail scanner data, which is not universal in coverage, i.e., it captures sales from participating retailers but does not capture all sales within a state in the manner that tax receipts do (“American Economic Association” n.d.). As a proprietary product, it would be difficult to evaluate the degree to which the percentage of sales captured by the Nielsen data varies by state, time, or both.
The impact of increased cannabis consumption on the use of other drugs is a key unknown in trying to anticipate the economic and public health impacts of cannabis legalization. States can anticipate cost savings from increases in tax revenue and decreases in enforcement costs. These are partially offset by the costs of regulation and anticipated increases in the number of people seeking treatment, but these are believed to be comparatively small. (Kilmer et al., 2010). In 2017, the six states with operational legalized cannabis sales collected over $600 million in tax revenue, very roughly $10 per capita (Davis, Misha, & Phillips, 2019). Economic analysis of prohibition enforcement costs yields additional savings estimates of similar magnitude (Kilmer et al., 2010). By way of comparison, the cost per capita of alcohol consumption was estimated at about $750 in 2006; smoking costs are on the same order of magnitude (Bouchery et al., 2011; Centers for Disease Control, 2019). It is immediately clear that 5-10 percent increases in either cigarette or alcohol consumption would more than offset the economic benefits of cannabis legalization, and conversely, that any decrease in consumption of these drugs would be a more substantial economic and public health benefit than the cost-savings of legalization. Our results provide some evidence against both the best- and worst-case scenarios regarding alcohol and cigarette consumption. However, there is enough uncertainty associated with our estimates that economically significant changes cannot be ruled out. Nonetheless, our findings provide an important counterpoint to an earlier study (Baggio, Chong & Kwon, 2017).
Another main finding of our analyses relates to the endogeneity of cannabis liberalization policies. The strong dependence of estimates of policy effects on covariate inclusion indicates that state and year fixed effects do not adequately control for confounding. This suggests that critical time-varying differences exist in factors that influence alcohol and cigarette consumption in states with liberalized cannabis policies compared to those with prohibitive policies. Prior work has also shown that the apparent effects of medical cannabis policy on health outcomes can be highly sensitive to the choice of covariates (Grucza et al., 2015). Our post hoc analyses identified two such factors that are associated with cigarette consumption: age distribution of state-populations and smoke-free air policies. Age distribution was also associated with alcohol consumption and, although smoke-free air policies were not, other studies have shown that tobacco control policies can impact alcohol use (Young-Wolff et al., 2013; Krauss, Cavazos-Rehg, Plunk, Bierut, & Grucza, 2014; Young-Wolff, Kasza, Hyland, & McKee, 2014). Thus, we detected and attempted to adjust for confounding by observed factors, but the effects of such factors indicate that cannabis policies do not meet the “strict exogeneity” assumption on which difference-in-difference analyses are based (Wing et al., 2018). For example, we found that cannabis policies are associated with smoke-free air policies over time and that this contributed to a spurious association between cannabis liberalization and decreased rates of smoking in our secondary model specifications (Table 3, Series II and III models). If states that implement liberalized cannabis policies are generally more committed to public health, then adaptation of other pro-public health policies may occur proximally in time to cannabis policy change, giving rise to other spurious correlations between cannabis policy liberalization and favorable public health outcomes.
Key strengths of this study include the use of objectively measured alcohol and cigarette consumption using tax receipt data, which are expected to accurately assess all sales and consumption from all US states. The use of multiple policy specifications with convergent results is an additional strength. A limitation of our study is that the granularity of our geographic and temporal data is limited to state and year, respectively. A further limitation is the lack of individual-level data, which would allow us to conduct analyses focused on demographic groups most likely to use alcohol or cigarettes, and which might demonstrate complementarity and/or substitution effects among specific subpopulations, even as the net population effect is zero. Related to this, an additional limitation is our inability to detect small effect sizes, particularly in the case of the cigarette analyses, where confidence intervals were fairly wide. Additionally, there is heterogeneity in state cannabis policy, commercial availability, and local control, all of which might contribute to heterogeneity of effects by state (which were not a focus of this investigation). Limitations notwithstanding, our results suggest that cannabis liberalization policies do not have strong positive or negative effects on either cigarette or alcohol consumption in contrast to at least one prior study (Baggio et al 2017). Future studies may be warranted to examine these outcomes as cannabis policy evolves further and to assess whether alcohol or tobacco use changes among vulnerable such as adolescents.
Supplementary Material
Table 4.
Association between various time-varying covariates and state cannabis policy adjusting for state and year fixed effects
| Covariate | Medical Cannabis Policya | Recreational Cannabis Policy | ||||
|---|---|---|---|---|---|---|
| β | SE | P | β | SE | P | |
| Under 65 % | −0.296 | 0.133 | 0.031 | −0.826 | 0.196 | 0.000 |
| White % | −1.224 | 0.772 | 0.119 | −1.301 | 1.240 | 0.299 |
| PC Income | −0.009 | 0.012 | 0.480 | 0.011 | 0.018 | 0.556 |
| Poverty % | 0.007 | 0.026 | 0.786 | −0.059 | 0.045 | 0.194 |
| Unemployment % |
0.022 | 0.036 | 0.546 | −0.069 | 0.067 | 0.307 |
| College Grad % | −0.008 | 0.012 | 0.487 | −0.017 | 0.013 | 0.196 |
| Political Ideology | 1.162 | 0.921 | 0.213 | 0.773 | 1.304 | 0.556 |
| Beer Tax | 1.903 | 0.980 | 0.058 | 7.772 | 3.968 | 0.056 |
| Bac08Law | ---- | ---- | ---- | ---- | ---- | ---- |
| Cigarette Tax | −0.050 | 0.080 | 0.535 | −0.090 | 0.139 | 0.532 |
| SFA Score | 1.555 | 0.316 | 0.000 | 2.5337 | 0.439 | 0.000 |
Classified according to the primary specification for cannabis policy from work by Pacula et al.
Acknowledgements:
This work was conducted as part of a class project in the Master of Population Health Sciences Program, Washington University School of Medicine.
Funding Sources: Washington University School of Medicine, NIH R01 DA040411, R01 DA042195, T32 DA15035.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Conflicts: The authors declare no conflicts of interest relevant to this work.
Contributor Information
Sirish Veligati, Master of Population Health Sciences Program, Washington University, St. Louis, MO, USA.
Seth Howdeshell, Master of Population Health Sciences Program, Washington University, St. Louis, MO, USA; Brown School, Washington University, St. Louis, MO, USA.
Sara Beeler-Stinn, Washington University, St. Louis, MO, USA.
Deepak Lingam, Master of Population Health Sciences Program, Washington University, St. Louis, MO, USA.
Phylicia C. Allen, Brown School, Washington University, St. Louis, MO, USA.
Li-Shiun Chen, Department of Psychiatry, School of Medicine, Washington University, St. Louis, MO, USA.
Richard A. Grucza, Department of Psychiatry, School of Medicine, Washington University, St. Louis, MO, USA.
References
- Agrawal A, Budney AJ, & Lynskey MT (2012). The co-occurring use and misuse of cannabis and tobacco: a review. Addiction (Abingdon, England), 107(7), 1221–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ahrnsbrak R, Bose J, Hedden Sarra L., Lipari Rachel N. R.N., & Park-Lee E (2017). Key Substance Use and Mental Health Indicators in the United States: Results from the 2016 National Survey on Drug Use and Health | CBHSQ. Retrieved October 17, 2018, from https://www.samhsa.gov/data/report/kev-substance-use-and-mental-health-indicators-united-states-results-2016-national-survey. Accessed 2/11/2019.
- American Economic Association: RFE. (n.d.). Retrieved January 8, 2019, from https://www.aeaweb.org/rfe/showRes.php7rfe_id=1936&cat_id=5. Accessed 2/11/2019.
- Anderson DM, Hansen B, & Rees DI (2013). Medical Marijuana Laws, Traffic Fatalities, and Alcohol Consumption. The Journal of Law and Economics, 56(2), 333–369. [Google Scholar]
- Anderson DM, Hansen B, & Rees DI (2015). Medical Marijuana Laws and Teen Marijuana Use. American Law and Economics Review, 17(2), 495–528. [Google Scholar]
- Anderson DM, Rees DI, & Sabia JJ (2014). Medical marijuana laws and suicides by gender and age. American Journal of Public Health, 104(12), 2369–2376. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Angrist J, & Pischke J-S (2009). Mostly Harmless Econometrics: An Empiricist’s Companion. In Mostly Harmless Econometrics: An Empiricist’s Companion.
- Bachhuber MA, Saloner B, Cunningham CO, & Barry CL (2014). Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Internal Medicine, 174(10), 1668–1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baggio M, Chong A, & Kwon S (2017). Helping Settle the Marijuana and Alcohol Debate: Evidence from Scanner Data (SSRN Scholarly Paper No. ID 3063288). Rochester, NY: Social Science Research Network; Retrieved from https://papers.ssrn.com/abstract=3063288. Accessed 2/11/2019 [Google Scholar]
- Batalla A, Bhattacharyya S, Yücel M, Fusar-Poli P, Crippa JA, Nogué S, … Martin-Santos R(2013). Structural and Functional Imaging Studies in Chronic Cannabis Users: A Systematic Review of Adolescent and Adult Findings. PLOS ONE, 8(2), e55821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry WD, Ringquist EJ, Fording RC, & Hanson RL (1998). Measuring citizen and government ideology in the American states, 1960-93. Am. J. Pol. Sci, 42( 1), 327–348. [Google Scholar]
- Bouchery EE, Harwood HJ, Sacks JJ, Simon CJ, & Brewer RD (2011). Economic Costs of Excessive Alcohol Consumption in the U.S., 2006. American Journal of Preventive Medicine, 41(5), 516–524. [DOI] [PubMed] [Google Scholar]
- Bradford AC, Bradford WD, Abraham A, & Bagwell Adams G (2018). Association Between US State Medical Cannabis Laws and Opioid Prescribing in the Medicare Part D Population. JAMA Internal Medicine, 178(5), 667–672. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cameron L, & Williams J (2001). Cannabis, alcohol and cigarettes: substitutes or complements? Economic Record, 77(236), 19–34. [Google Scholar]
- CDC Office on Smoking and Health. (2018). National Tobacco Control Program Fact Sheets Data Sources and Methodologies. Retrieved from https://www.cdc.gov/tobacco/about/osh/program-funding/pdfs/ntcp-factsheets-data-sources-methodologies-3-20-508.pdf. Accessed 2/11/2019.
- Cerdá M, Wall M, Feng T, Keyes KM, Sarvet A, Schulenberg J, … Hasin DS(2017) Association of State Recreational Marijuana Laws With Adolescent Marijuana Use. JAMA Pediatrics, 171(2), 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cerdá M, Sarvet AL, Wall M, Feng T, Keyes KM, Galea S, & Hasin DS (2018). Medical marijuana laws and adolescent use of marijuana and other substances: Alcohol, cigarettes, prescription drugs, and other illicit drugs. Drug and Alcohol Dependence, 183, 62–68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Degenhardt L, Ferrari AJ, Calabria B, Hall WD, Norman RE, McGrath J, … Vos T(2013). The global epidemiology and contribution of cannabis use and dependence to the global burden of disease: results from the GBD 2010 study. PloS One, 8(10), e76635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- DiNardo J, & Lemieux T (2001). Alcohol, marijuana, and American youth: the unintended consequences of government regulation. Journal of Health Economics, 20(6), 991–1010. [DOI] [PubMed] [Google Scholar]
- Farrelly MC, Bray JW, Zarkin GA, Wendling BW, & Pacula RL (1999). The effects of prices and policies on the demand for marijuana: Evidence from the National Household Surveys on Drug Abuse. National Bureau of Economic Research. [DOI] [PubMed] [Google Scholar]
- Gage SH, Jones HJ, Burgess S, Bowden J, Davey Smith G, Zammit S, & Munafò MR (2017). Assessing causality in associations between cannabis use and schizophrenia risk: a two-sample Mendelian randomization study. Psychological Medicine, 47(5), 971–980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gage SH, Hickman M, & Zammit S (2016). Association Between Cannabis and Psychosis: Epidemiologic Evidence. Biological Psychiatry, 79(7), 549–556. [DOI] [PubMed] [Google Scholar]
- Goodchild M, Nargis N, & Tursan d’Espaignet E (2018). Global economic cost of smoking-attributable diseases. Tobacco Control, 27(1), 58–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grucza RA, Hur M, Agrawal A, Krauss MJ, Plunk AD, Cavazos-Rehg PA, … Bierut LJ(2015). A reexamination of medical marijuana policies in relation to suicide risk. Drug and Alcohol Dependence, 152, 68–72. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guttmannova K, Lee CM, Kilmer JR, Fleming CB, Rhew IC, Kosterman R, & Larimer ME (2016). Impacts of Changing Marijuana Policies on Alcohol Use in the United States. Alcoholism: Clinical and Experimental Research, 40(1), 33–46 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall W, & Lynskey M (2016). Why it is probably too soon to assess the public health effects of legalisation of recreational cannabis use in the USA. The Lancet Psychiatry, 3(9), 900–906. [DOI] [PubMed] [Google Scholar]
- Harper S, Strumpf EC, & Kaufman JS (2012). Do medical marijuana laws increase marijuana use? Replication study and extension. Annals of Epidemiology, 22(3), 207–212. [DOI] [PubMed] [Google Scholar]
- Haughwout S, & Slater M (2018). Surveillance Report# 110: Apparent per capita alcohol consumption: National, state, and regional trends, 1977-2016. Bethesda, MD: NIAAA; Retrieved from https://pubs.niaaa.nih.gov/publications/surveillance110/CONS16.pdf. Accessed 2/11/2019. [Google Scholar]
- Hickman M, Vickerman P, Macleod J, Kirkbride J, & Jones PB (2007). Cannabis and schizophrenia: model projections of the impact of the rise in cannabis use on historical and future trends in schizophrenia in England and Wales. Addiction (Abingdon, England), 102(4), 597–606. [DOI] [PubMed] [Google Scholar]
- Johnson NB, Hayes LD, Brown K, Hoo EC, Ethier KA, & Centers for Disease Control and Prevention (CDC). (2014). CDC National Health Report: leading causes of morbidity and mortality and associated behavioral risk and protective factors--United States, 2005-2013. MMWR Supplements, 63(4), 3–27. [PubMed] [Google Scholar]
- Kerr DCR, Bae H, & Koval AL (2018). Oregon recreational marijuana legalization: Changes in undergraduates’ marijuana use rates from 2008 to 2016. Psychology of Addictive Behaviors, 32(6), 670–678. [DOI] [PubMed] [Google Scholar]
- Kilmer B, Caulkins JP, Pacula RL, MacCoun RJ, & Reuter PH (2010). Altered State? (Product Page). Retrieved from https://www.rand.org/pubs/occasional_papers/OP315.html. Accessed 2/11/2019
- Krauss MJ, Cavazos-Rehg PA, Plunk AD, Bierut LJ, & Grucza RA (2014). Effects of State Cigarette Excise Taxes and Smoke-Free Air Policies on State Per Capita Alcohol Consumption in the United States, 1980 to 2009. Alcoholism: Clinical and Experimental Research, 38(10), 2630–2638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynne-Landsman SD, Livingston MD, & Wagenaar AC (2013). Effects of state medical marijuana laws on adolescent marijuana use. American Journal of Public Health, 103(8), 1500– 1506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Academies of Sciences, E. (2017). The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Retrieved from https://www.nap.edu/resource/24625/Cannabis_committee_conclusions.pdf. Accessed 2/11/2019. [PubMed]
- O’Hara RE, Armeli S, & Tennen H (2016). Alcohol and cannabis use among college students: Substitutes or complements? Addictive Behaviors, 58, 1–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula R, & Smart R (2017). Medical Marijuana and Marijuana Legalization. Annual Review of Clinical Psychology, 13(1), 397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, Powell D, Heaton P, & Sevigny EL (2015b). Assessing the Effects of Medical Marijuana Laws on Marijuana Use: The Devil is in the Details: Assessing the Effects of Medical Marijuana Laws. Journal of Policy Analysis and Management, 34( 1), 7–31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pacula RL, & Sevigny EL (2014). Marijuana Liberalization Policies: Why We Can’t Learn Much from Policy Still in Motion: Point/Counterpoint. Journal of Policy Analysis and Management, 33(1), 212–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ponicki W (2004). Statewide Availability Data System II: 1933-2003 National Institute on Alcohol Abuse and Alcoholism Research Center Grant P60-AA006282-23. Pacific Institute for Research and Evaluation Prevention Research Center, Berkeley, CA: Obtained through https://alcoholpolicy.niaaa.nih.gov/file-page/data-request-form/78. Accessed 2/11/2018. [Google Scholar]
- Powell D, Pacula RL, & Jacobson M (2015). Do Medical Marijuana Laws Reduce Addictions and Deaths Related to Pain Killers? (Working Paper No. 21345) National Bureau of Economic Research. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shover CL, Davis CS, Gordon SC, & Humphreys K (2019). Association between medical cannabis laws and opioid overdose mortality has reversed over time. Proceedings of the National Academy of Sciences, 116(26), 12624–12626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simons JS, Gaher RM, Correia CJ, Hansen CL, & Christopher MS (2005). An affective-motivational model of marijuana and alcohol problems among college students. Psychology of Addictive Behaviors, 19(3), 326–334. [DOI] [PubMed] [Google Scholar]
- Stahre M, Roeber J, Kanny D, Brewer RD, & Zhang X (2014). Contribution of excessive alcohol consumption to deaths and years of potential life lost in the United States. Preventing Chronic Disease, 11, E109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Surveillance, Epidemiology, and End Results (SEER) Program (www.seer.cancer.gov) SEER*Stat Database: Populations - Total U.S. (1969-2016) - Linked To County Attributes - Total U.S., 1969-2016 Counties, National Cancer Institute, DCCPS, Surveillance Research Program, released November 2017 (n.d.). [Google Scholar]
- van Winkel R, & Kuepper R (2014). Epidemiological, Neurobiological, and Genetic Clues to the Mechanisms Linking Cannabis Use to Risk for Nonaffective Psychosis. Annual Review of Clinical Psychology, 10( 1), 767–791. [DOI] [PubMed] [Google Scholar]
- Volkow ND, Baler RD, Compton WM, & Weiss SRB (2014). Adverse Health Effects of Marijuana Use. New England Journal of Medicine, 370(23), 2219–2227. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, & Hockenberry JM (2018). Association of Medical and Adult-Use Marijuana Laws With Opioid Prescribing for Medicaid Enrollees. JAMA Internal Medicine, 178(5), 673–679. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wen H, Hockenberry JM, & Cummings JR (2015). The effect of medical marijuana laws on adolescent and adult use of marijuana, alcohol, and other substances. Journal of Health Economics, 42, 64–80. [DOI] [PubMed] [Google Scholar]
- Williams AR, Olfson M, Kim JH, Martins SS, & Kleber HD (2016). Older, Less Regulated Medical Marijuana Programs Have Much Greater Enrollment Rates Than Newer “Medicalized” Programs. Health Affairs, 35(3), 480–488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams AR, Santaella-Tenorio J, Mauro CM, Levin FR, & Martins SS (2017). Loose regulation of medical marijuana programs associated with higher rates of adult marijuana use but not cannabis use disorder. Addiction (Abingdon, England), 112(11), 1985–1991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing C, Simon K, & Bello-Gomez RA (2018). Designing Difference in Difference Studies: Best Practices for Public Health Policy Research. Annual Review of Public Health, 39(1), 453–469. [DOI] [PubMed] [Google Scholar]
- Young-Wolff KC, Hyland AJ, Desai R, Sindelar J, Pilver CE, & McKee SA (2013) Smoke-free policies in drinking venues predict transitions in alcohol use disorders in a longitudinal U.S. sample. Drug and Alcohol Dependence, 128(3), 214–221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Young-Wolff KC, Kasza KA, Hyland AJ, & McKee SA (2014). Increased Cigarette Tax is Associated with Reductions in Alcohol Consumption in a Longitudinal U.S. Sample. Alcoholism, Clinical and Experimental Research, 38(1), 241–248. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.