Abstract
Background:
In settings where stigma and discrimination toward men who have sex with men (MSM) are high or illegal, like in Malaysia, innovative methods to anonymously reach them are urgently needed. The near ubiquitous availability of mobile technology, including smartphones, has the potential to open new frontiers (such as mHealth) to prevent HIV and other sexually transmitted infections (STIs). The extent to which MSM use mHealth tools for HIV and STI prevention in the Malaysia context, however, is unknown.
Methods:
A cross-sectional online survey in 622 Malaysian MSM was conducted between July and November 2017. Participants were recruited via advertisements on mobile apps frequently used by MSM. In addition to demographic, smartphone access and utilization, and other information were assessed using logistic regression to determine factors associated with the use of a smartphone to search for online sexual health information.
Results:
Nearly all (99.2%) participants owned a smartphone, with 63% reported having used one to seek sexual health information, including HIV/STIs. Overall, 96% used smartphones to find sexual partners, with high levels of HIV risk behavior reported. Independent correlates of smartphone use to seek online sexual health information included older age (aOR=0.943, p=0.005), higher education (aOR=2.14, p=027), recent (past year) HIV testing (aOR=3.91, p=0.026), and seeking sexual partners using geosocial networking apps (aOR=5.58, p=0.006).
Conclusion:
These findings suggest high smartphone use by high-risk MSM to seek sexual health information and suggests that mHealth strategies may be an effective strategy to engage MSM in HIV prevention activities.
Keywords: HIV, men who have sex with men, mHealth, smartphone, Malaysia
Introduction
Despite reductions in HIV incidence globally, HIV transmission among men who have sex with men (MSM) continues to increase markedly (Beyrer et al., 2012; UNAIDS, 2017), especially where sex between men remains highly stigmatized or illegal (Oldenburg et al., 2014; Oldenburg et al., 2018; Oldenburg, Perez-Brumer, Reisner, & Mimiaga, 2015). Malaysia, a middle-income country with low (0.4%) overall HIV prevalence, has an evolving epidemic in MSM with new HIV cases increasing from 10% in 2008 to 54% in 2016 (Ministry of Health Malaysia, 2016). Biobehavioral surveys now suggest that HIV prevalence among MSM is now at an all-time high of 21.6%, and is concentrated in the country’s capital, Kuala Lumpur, where HIV prevalence among MSM was 43% in 2018, up from 22% just four years before (Ministry of Health Malaysia, 2018). This growing epidemic among MSM has been associated with condomless sex (CS) and concomitant use of drugs and alcohol (Kanter et al., 2011; S. H. Lim, Akbar, Wickersham, Kamarulzaman, & Altice, 2018; S. H. Lim et al., 2013; S. H. Lim et al., 2015).
In Malaysia, homosexuality is illegal in both secular and Sharia law. Even when criminal sanctions are not enforced, MSM are highly stigmatized and often discriminated against. Consequently, reaching MSM in general, and certainly, those not identifying as “gay”, has been especially challenging with HIV prevention services (S. H. Lim et al., 2018; Sin How Lim et al., 2018). Traditional outreach at venues where MSM congregate has been challenging. For example, gay clubs are unviable option because of highly publicized police raids of such establishments with the press airing footage of MSM being forced to submit to urine drug testing or even pronouncements against lesbian, gay, bisexual, and transgender (LGBT) persons by leading governmental authorities, including to smear leading public figures seeking election. Consequently, innovative strategies to prevent HIV in MSM must not only be tailored to the context but must be adequately scaled-to-need (Beyrer & Baral, 2011; United Nations Development Programme, 2014).
The unprecedented expansion of mobile technologies, especially in emerging economies, as well as their potential application to reach groups who are not accessible using venue-based strategies, has opened new frontiers, including mHealth strategies, to promote personal healthcare engagement, including optimized prevention and treatment (Conserve et al., 2017; Cooper, Clatworthy, Whetham, & Consortium, 2017; Henny, Wilkes, McDonald, Denson, & Neumann, 2018; Marcolino et al., 2018). The enthusiasm about mHealth stems from its ability to address perennial barriers to healthcare access like cost, infrastructure, and accessibility (Alice et al., 2018; Krishnan & Cravero, 2017). mHealth strategies in systematic reviews have documented benefits for impact on medication adherence (Adler et al., 2017; Finitsis, Pellowski, & Johnson, 2014; Moore et al., 2018), appointment attendance (Free et al., 2013; Head, Noar, Iannarino, & Grant Harrington, 2013; Moore et al., 2018), and health-promoting behaviors (Free et al., 2013; Head et al., 2013; Kitsiou, Paré, Jaana, & Gerber, 2017; Overdijkink et al., 2018) in various patient groups across diverse settings. Thus, if found to be acceptable and made accessible, mHealth interventions have the potential to overcome known barriers to accessing HIV prevention and treatment services among Malaysian MSM and overcome existing barriers to prevention.
Adoption of smartphones has grown rapidly with 75.9% of Malaysians owning one by 2017. Furthermore, in 2017, there were 24.5 million Internet users with smartphones being the most common device accessing the Internet (89.4%) (MCMC, 2017a, 2017b). The extent to which MSM, especially high-risk MSM in Malaysia use smartphones and the internet, however, is unknown and assessment of their use and interest in using smartphones to access prevention information might provide new insights into reaching this hidden population in Malaysia. Specifically, there has not been an empirical study on the use of mHealth technology to seek sexual health information among Malaysia MSM. Understanding the characteristics of technology users will help us develop appropriate interventions for MSM who use smartphone technology to seek online HIV/sexually transmitted infection (STI) information. Therefore, we analyzed data from an online study among Malaysian MSM assessing HIV testing to investigate the characteristics of smartphone users and the use of a smartphone to seek online sexual health information, including HIV/STI.
Methods
Study Design and Participants
A cross-sectional study assessing HIV testing practices among MSM in Malaysia was conducted from July to November 2017. Inclusion criteria were: i) 18 years or older; ii) identifies as male; iii) Malaysian citizen; iv) reporting recent (last 12 months) condomless anal sex with another man; and v)) able to read and understand English or Bahasa Malaysia.
Study Procedures
A convenience sample of MSM was recruited via advertisements on Grindr, the most commonly used social networking apps that MSM use, by providing banner promoting the survey. Interested app users who clicked on advertisements were directed to an eligibility screener hosted by RedCap (Harris et al., 2009). Each eligible participants voluntarily completed an online consent form by acknowledging that they understood the purpose, risks, and benefits of the study prior to completing the survey. On average, participants took 15-20 minutes to complete the anonymous online survey. The questionnaire was available in both English and Malay languages and was translated and back-translated to ensure culture meaning (Brislin, 1970). No payments were made for completing the surveys.
The primary study was approved by the Medical Ethics Committee of the University of Malaya.
Measures
Participant characteristics included age, ethnicity, educational status (university graduate), household status, employment status, disclosure of sexual orientation to family or friends, and self-reported history of HIV testing practices and current HIV status.
Sexual risk behaviors included the age of sexual debut, sex with regular and casual sex partners, serostatus of sex partners, consistent condom use, engagement in group sex, commercial sex and ‘chemsex’, and the use of alcohol before or during sex in a lifetime. Chemsex was defined as the use of a psychoactive substance (crystal methamphetamine/”Batu”/ice, ketamine, ecstasy, and gamma hydroxybutyrate “G”) before or during anal intercourse (Daly, 2013; Schmidt et al., 2016; Stephenson & Richardson, 2014).
Perceived social support was measured by a 12-item short version of the original 24-items Social Provisions Scale, which assesses the perceived availability of tangible, informational, emotional, and esteem support (Cutrona & Russell, 1987). The overall score was obtained by summing responses to all items with higher scores indicating higher perceived social support (α=0.89).
Depressive symptoms over the previous week were assessed using the 20-item Center for Epidemiological Studies Depression (CES-D) scale (Radloff, 1977). The total sum score ranges from 0-60, with standard cut-offs of >16 associated with moderate to severe depression (α=0.87).
Interpersonal violence (IPV) was assessed by asking the participants whether have been the victim of IPV in lifetime, including if they had been ‘hurt, hit, or slapped by a steady or casual partner’, ‘being forced by a steady or casual partner to have sex’, ‘being forced by a person who is not a steady or casual partner to have sex’, or ‘being fondled or forced into unwanted sexual touching (e.g. touch or grope in a way that person does not want)’. Lifetime IPV was indicated by a positive answer to any of the above items.
Smartphone access or use:
Participants were asked about their access to a smartphone and the utilization of the internet on a smartphone for various activities (e.g., general information search, information search related to sexual health, information search on clinic health care providers, communication with friends and family, to find sexual partner, entertainment, education purpose). Participants were further asked about their use of various social networking apps (e.g., Facebook, Twiter, Instagram) as well as geosocial networking apps (GSN) commonly used by MSM (e.g., Grindr, Blued, PlanetRomeo, Jack’d) on their phone. They were also asked if they used a smartphone to seek sexual health information online, including HIV and STIs.
Data Analysis
Analyses were performed using SPSS 23.0. The primary outcome was smartphone use to seek sexual health information. Estimates were evaluated for statistical significance based on 95% confidence intervals using p<0.05. We computed descriptive statistics, including frequencies and percentages for categorical variables and means, standard deviations, and ranges for continuous variables. After conducting bivariate logistic analyses for significant associations with the primary outcome (use of a smartphone to seek sexual health information), we conducted parsimonious multivariate logistic regression analyses by including variables on bivariate associations significant at p<0.10. Collinearity between variables was assessed using the variance inflation factor (VIF>10).
Results
Participant Characteristics
Table 1 provides summary data for the 622 MSM (mean age = 28.2, range: 18-64 years) who provided complete data, most of whom were Malay (66.7%), university graduates (78.6%), currently employed (75.7%), and reported to have disclosed their sexual orientation to family or friends. Overall, 239 (38.4%) participants had never tested for HIV, and 44.5% reported to have tested for HIV in the past 12 months. Of the total participants, 24.3% reported being HIV positive, and 60.8% met screening criteria for having moderate to severe depression.
Table 1:
Characteristics of participants and sexual behaviors, stratified by smartphone use to seek sexual health information (N=622)
| Variables | Entire Sample (N = 622) |
Use of Smartphone to Seek Sexual Health Information |
Unadjusted ORe (95% CIf) | pf | |
|---|---|---|---|---|---|
| No (n = 230) | Yes (n = 392) | ||||
| Frequency (%) | |||||
| Characteristics of participants | |||||
| Age (years): Mean (SD, Range)a | 28.2 (6.9, 18–64) | 29.1 (8.3) | 27.6 (5.9) | 0.971 (0.949, 0.994) | 0.012 |
| Ethnicity | |||||
| Malay | 415 (66.7) | 156 (25.1) | 259 (41.6) | - | - |
| Indian | 120 (3.0) | 44 (7.1) | 76 (12.2) | 1.040 (0.683, 1.585) | 0.854 |
| Chinese | 29 (4.7) | 11 (1.8) | 18 (2.9) | 0.986 (0.454, 2.141) | 0.971 |
| Other | 58 (9.3) | 19 (3.1) | 39 (6.3) | 1.236 (0.690, 2.215) | 0.476 |
| University graduateb | |||||
| No | 133 (21.4) | 64 (10.3) | 69 (11.1) | - | - |
| Yes | 489 (78.6) | 166 (26.7) | 323 (51.9) | 1.805 (1.224, 2.661) | 0.003 |
| Household status | |||||
| Family | 278 (44.7) | 106 (17.0) | 172 (27.7) | - | - |
| Friends | 145 (23.3) | 49 (7.9) | 96 (15.4) | 1.207 (0.793, 1.839) | 0.380 |
| Regular partner | 67 (10.8) | 28 (4.5) | 39 (6.3) | 0.858 (0.499, 1.477) | 0.581 |
| Alone/others | 132 (21.2) | 47 (7.6) | 85 (13.7) | 1.115 (0.725, 1.715) | 0.622 |
| Currently employed | |||||
| No | 151 (24.3) | 58 (9.3) | 93(15.0) | - | - |
| Yes | 471 (75.7) | 172 (27.7) | 299 (48.1) | 1.084 (0.743, 1.582) | 0.675 |
| Ever had HIV test | |||||
| No | 239 (38.4) | 113 (18.2) | 126 (20.3) | - | - |
| Yes | 383 (61.6) | 117 (18.8) | 266 (42.8) | 2.039 (1.460, 2.848) | <0.001 |
| HIV status | n = 383 | ||||
| Negative | 290 (75.7) | 105 (27.4) | 185 (48.3) | - | - |
| Positive | 93 (24.3) | 12 (3.1) | 81 (21.1) | 3.831 (1.996, 7.352) | <0.001 |
| Social Support: Mean (SD, Range)a | 36.2 (6.3, 12–48) | 36.1 (6.1) | 36.3 (6.4) | 1.005 (0.979, 1.031) | 0.716 |
| Moderate to severe depression | |||||
| No | 244 (39.2) | 94 (15.1) | 150 (24.1) | - | - |
| Yes | 378 (60.8) | 136 (21.9) | 242 (38.9) | 1.115 (0.800, 1.555) | 0.521 |
| Victim of IPVC | |||||
| No | 469 (75.4) | 183 (29.4) | 286 (46.0) | - | - |
| Yes | 153 (24.6) | 47 (7.6) | 106 (17.0) | 1.443 (0.977, 2.132) | 0.066 |
| Disclosure of sexual orientation | |||||
| No | 129 (20.7) | 52 (8.4) | 77 (12.4) | - | - |
| Yes | 493 (79.3) | 178 (28.6) | 315 (50.6) | 1.195 (0.804, 1.777) | 0.379 |
| Sexual behaviors | |||||
| Age of sexual debut: Mean (SD, Range)a | 17.3 (3.8, 7–21) | 17.4 (3.7) | 17.3 (3.8) | 0.998 (0.956, 1.042) | 0.924 |
| Sex with regular partner | |||||
| No | 353 (56.8) | 138 (22.2) | 215 (34.6) | - | - |
| Yes | 269 (43.2) | 92 (14.8) | 177 (28.5) | 1.235 (0.887, 1.718) | 0.211 |
| Serodiscordant relationship | n = 269 | ||||
| No | 249 (92.6) | 89 (33.1) | 160 (59.5) | - | - |
| Yes | 20 (7.4) | 3 (1.1) | 17 (6.3) | 3.152 (0.899, 11.051) | 0.073 |
| Sex with casual partner (past 12 months) | |||||
| No | 207 (33.3) | 91 (14.6) | 116 (18.6) | - | - |
| Yes | 415 (66.7) | 139 (22.3) | 276 (44.4) | 1.558 (1.107, 2.193) | 0.011 |
| Consistent condom use (past 3 months) | |||||
| No | 338 (54.3) | 132 (21.2) | 206 (33.1) | - | - |
| Yes | 284 (45.7) | 98 (15.8) | 186 (29.9) | 1.216 (0.876, 1.688) | 0.242 |
| Condom use (last sex) | |||||
| No | 368 (59.2) | 143 (23.0) | 225 (36.2) | - | - |
| Yes | 254 (40.8) | 87 (14.0) | 167 (26.8) | 1.220 (0.874, 1.703) | 0.242 |
| Ever engaged in group sex | |||||
| No | 367 (59.0) | 151 (24.3) | 216 (34.7) | - | - |
| Yes | 255 (41.0) | 79 (12.7) | 176 (28.3) | 1.557 (1.112, 2.182) | 0.010 |
| Ever engaged in commercial sex | |||||
| No | 468 (75.2) | 175 (28.1) | 293 (47.1) | - | - |
| Yes | 154 (24.8) | 55 (8.8) | 99(15.9) | 1.075 (0.736, 1.571) | 0.708 |
| Meets sexual partners via GSN appsd | |||||
| No | 25 (4.0) | 17 (2.7) | 8 (1.3) | - | - |
| Yes | 597 (96.0) | 213 (34.2) | 384 (61.7) | 3.831 (1.626, 9.025) | 0.002 |
| Ever engaged in Chemsex | |||||
| No | 482 (77.5) | 190 (30.5) | 292 (46.9) | - | - |
| Yes | 140 (6.4) | 40 (6.4) | 100 (16.1) | 1.627 (1.080, 2.450) | 0.020 |
| Drink alcohol before or during sex | |||||
| No | 486 (78.1) | 179 (28.8) | 307 (49.4) | - | - |
| Yes | 136 (21.9) | 51 (8.2) | 85 (13.7) | 0.972 (0.656, 1.440) | 0.886 |
Note:
SD: Standard deviation
Includes college, university, professional degree
IPV: intimate partner violence
Geosocial networking
Odds ratio
Confidence interval;
p-value
In terms of sexual behaviors, 43.2% of participants reported having a regular sex partner in the past three months, with 7.4% of them being in an HIV serodiscordant relationship. Over two-thirds (66.7%) had casual sex partners, and over 45% have engaged in inconsistent condom use in the past three months. A minority (6.4%) reported having ever engaged in Chemsex, and 41% reported to have engaged in group sex. Interestingly, nearly all of the participants (96%) reported having ever used a GSN app to find sexual partners (Table 1).
Ownership of and utilization of Smartphone
Figure 1 describes smartphone use characteristics. Nearly all participants (99.2%) reported owning a smartphone. Social networking apps (e.g., Facebook, Grindr, Blued, PlanetRomeo; 88.1%), followed by general information searches (86%) and communication with friends and family (80.2%) were the most common reasons for using the internet on a smartphone. Almost two-thirds (63%) of participants reported smartphone use to search for information on sexual health, including HIV/STIs, and 28.8% for information search on finding clinic or healthcare providers. In terms of the use of social networking apps, the majority of the participants reported the current use of Facebook (85.9%) and Instagram (73.5%). Similarly, the majority of participants (78.1%) used at least one GSN app to talk with or meet other men. Figure 2 shows GSN app use among participants who reported having ever used a GSN app. Grindr (72.5%) was the most commonly used app, followed by Blued (25.9%), PlanetRomeo (16.7%), and Jack’d (14.1%); increased use of Grindr may be related to recruitment.
Figure 1:
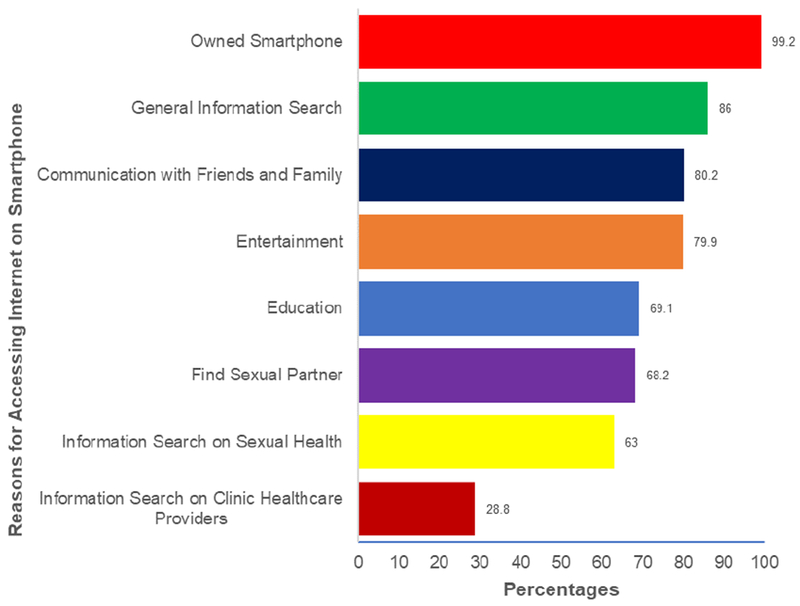
Ownership of and utilization of Smartphone among study participants (N=622)
Figure 2:
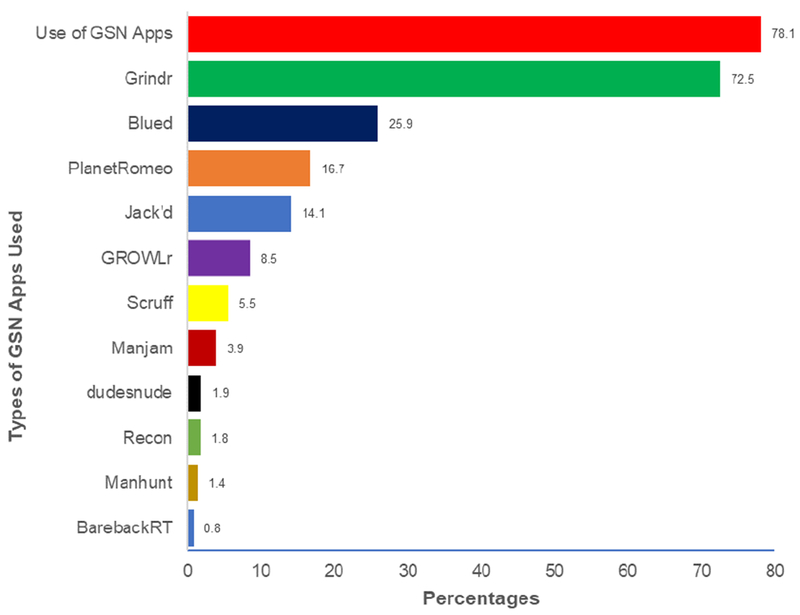
Use of different geosocial networking (GSN) apps by the study participants (N=622)
Note:
GSN: Geosocial networking
Correlates of smartphone use to find sexual health information online
Table 1 shows the bivariate correlates and odds ratio of sexual health information seeking through a smartphone. Of note, factors associated with using a smartphone to find sexual health information were being younger (p=0.012), a university graduate (p=0.003), having ever tested for HIV (p<0.001), having engaged in chemsex (p=0.020), and having sought sexual partners via an online app (p=0.002). In the multivariate logistic regression model, being a university graduate (aOR=2.13, p=027), having tested for HIV (aOR=3.91, p=0.026), and having met sexual partner via online GSN app (aOR=5.58, p=0.006) were more likely to use a smartphone to seek sexual health information online. Meanwhile, older age were associated with lower use of a smartphone to search for sexual health information (aOR=0.94, p=0.005).
Discussion
To our knowledge, this is the first study to assess smartphone use in Malaysian MSM, a setting where MSM are stigmatized and discriminated against and consequently difficult to reach with effective HIV prevention. This study provides important insights into the use of smartphone technology by MSM in Malaysia, specifically to seek sexual health information online about HIV and STIs. Specifically, the use of a smartphone to find online sexual health information, including information on HIV and STIs, was a common practice among this sample. This finding is similar to that observed among MSM in Hanoi, Vietnam (Nguyen et al., 2017). Our results further suggest the prevalent use of social networking apps to socialize and find sex partners among our sample - not surprising since MSM were recruited in part from GSN apps. This is much higher than those reported with MSM elsewhere (Goedel & Duncan, 2015; Grosskopf, LeVasseur, & Glaser, 2014; Landovitz et al., 2013; Rhoton et al., 2016; Ventuneac, John, Whitfield, Mustanski, & Parsons, 2018; Zou & Fan, 2017). This finding is particularly important in the Malaysian context where there are limited physical venues for MSM to meet face-to-face, socialize and even to seek healthcare since homosexuality is illegal - a consequence of the increasingly hostile socio-political environment facing LGBT people in Malaysia. With a large proportion of Malaysian MSM utilizing smartphones to seek sexual partners and sexual health information, prevention programs need to be tailored to these contexts that increase the use of anonymous interfaces and reduce “in person” interventions.
Though reported previously (Kanter et al., 2011; S. H. Lim et al., 2013; S. H. Lim et al., 2015; Sin How Lim et al., 2017), MSM in our sample also faced several vulnerabilities to HIV, including inconsistent condom use during sex and engagement in commercial sex, chemsex, and group sex, but at higher levels than previously reported, supporting the evolving HIV epidemic in MSM. The large proportion of MSM at substantial risk for acquiring HIV infection and underutilization of available HIV prevention services, as evident in our sample, partly explain an increasing HIV incidence among MSM in Malaysia. These findings, thus, underscore the urgent need for enhanced primary prevention approaches aimed at more effectively and efficiently preventing HIV in this high-risk population.
The findings that younger and more educated MSM were using a smartphone to search for sexual health information online may be reflective of the population subgroups who have better access to smartphones in general and as described in previous research. Prior research has indicated that adolescents and young adults represent the ‘digital generation’ and utilize the internet as a primary source of information gathering, communication, and social networking (Bien et al., 2015; Zou & Fan, 2017). With such widespread access, younger MSM have been found to heavily utilize smartphones to gain information on sex behavior, sexuality, and sexual health (Holloway et al., 2014; Landovitz et al., 2013). Furthermore, it may be that men with higher education are more likely to have higher income,(Hader, 2011) and that more affluent MSM are able to afford a smartphone as compared to their counterparts. These findings, along with the estimate that 35% of new infections in Malaysia occur among people 13-29 years of age (Ministry of Health Malaysia, 2018), further emphasize the potential for smartphone-based interventions to reach the most vulnerable individuals.
Our findings reveal that a high proportion (38.4%) of Malaysian MSM in the study had never been tested for HIV prior to the study representing a gap in scale-up of HIV testing services among this vulnerable group. This finding suggests the need for interventions to scale-up routine HIV testing among MSM, including the expansion of community-based testing services and at-home HIV testing kits, and innovative online testing programs (e.g., online-to-offline model) (Anand et al., 2017). As for MSM who had been tested for HIV, testing services could have enhanced their awareness about HIV and motivation to search for online information on prevention and care. Since specific temporal information was not collected; however, it is also plausible that having been HIV tested resulted in online health information-seeking behavior. Nonetheless, the fact that MSM who had never been tested for HIV were less likely to seek sexual health information related to HIV/STI online indicates the need for research on integrating health information, especially information related to HIV/AIDS, into the GSN apps, which are frequently used by MSM in Malaysia.
Our findings further revealed that the smartphone GSN apps are popular as a means for meeting sex partners among Malaysian MSM. This finding is consistent with previous studies, which investigated the role of GSN apps for meeting potential sex partners (Goedel & Duncan, 2015; Grosskopf et al., 2014; Landovitz et al., 2013; Rhoton et al., 2016; Ventuneac et al., 2018; Zou & Fan, 2017). Also, those who met a sexual partner via GSN apps were more likely to use a smartphone to search for HIV/STI information online. It is possible that individuals who seek sex partners online are making a rational judgment about their risk levels when considering whether to look for information on HIV/STI prevention and care online. Other possible reasons included their preference for online platforms via smartphone, instead of traditional venue-based approach, due to issues related to stigma and discrimination as discussed above. Regardless, our findings indicate the potential for the use of smartphone-based platforms to scale-up HIV prevention efforts among MSM in Malaysian settings.
Future Implications
While tremendous advances in HIV prevention and treatment have been achieved, these advances are still not reaching some of the most vulnerable populations. In Malaysia, the longstanding cultural and legal prohibitions of sex between men have further marginalized MSM and prevented them from accessing HIV prevention services [e.g., HIV testing, pre-exposure prophylaxis (PrEP), HIV treatment as prevention (TasP)] due to issues related to stigma and discrimination. Our findings support the potential use of mHealth-based approaches, particularly smartphone-based apps, to promote HIV testing and deliver HIV interventions or to facilitate linkage to HIV prevention services among MSM in Malaysia. The existence of inadequate access to HIV prevention services (which are primarily facility-based), significant wait-time at existing clinics, stigma, and discrimination are more likely to dissuade MSM from seeking traditional venue-based HIV prevention services, especially if they have to discuss their sexual practices. Given the difficulties faced in targeting MSM to engage in traditional HIV prevention efforts, there may be opportunities via smartphone-based apps or via web-based approaches to facilitate HIV prevention efforts. For example, there are several smartphone app-based HIV prevention interventions in the United States aimed at improving both the HIV treatment cascade (e.g., PositiveLinks) and PrEP clinical care (e.g., Nurx) among diverse patient populations. Future research should, therefore, focus on adapting/developing similar app-based approaches and conducting feasibility and acceptability trials among MSM in Malaysian contexts.
Limitations
Several limitations of this study need to be acknowledged. First, we used a convenience sample of MSM recruited via gay social media (e.g., Grindr) rather than a representative sample of all MSM in Malaysia. The online methodology used in our study may have excluded MSM without access to the Internet on which the study was advertised. Second, the use of self-reported measures in the current study may have resulted in participants inaccurate reporting of socially undesirable behaviors (e.g., sex-related behaviors). Third, the use of cross-sectional study design limited our ability to make causal inferences.
Conclusion
Our study suggests high smartphone use by high-risk MSM to seek sexual health information. Smartphone use for seeking sexual health information is likely to increase in prevalence in the coming years among MSM in Malaysia, as it is currently common among younger age groups. These trends reinforce the potential value of engaging MSM in this setting through online smartphone-based interventions. The findings here suggest the need for further research to assess the feasibility and acceptability of smartphone-based interventions as part of overall HIV prevention efforts to address the HIV epidemic among this high-risk, underserved group.
Table 2:
Independent correlates of smartphone use to seek sexual health information about HIV and Sexually Transmittted Infections (N=622)
| Variables | Use of Smartphone to Seek Sexual Health Information (HIV, STIs) |
||
|---|---|---|---|
| aOR d | 95% CI e | p f | |
| Age, years (continuous) | 0.94 | 0.90 0.98 | 0.005 |
| University graduate a | |||
| No | referent | - | - |
| Yes | 2.13 | 1.09, 4.19 | 0.027 |
| HIV testing (past 12 months) | |||
| No | referent | - | - |
| Yes | 3.91 | 1.17, 13.01 | 0.026 |
| HIV status | |||
| Negative | referent | - | - |
| Positive | 1.66 | 0.90, 3.04 | 0.099 |
| Experienced IPV b | |||
| No | referent | - | - |
| Yes | 1.43 | 0.72 2.85 | 0.297 |
| Serodiscordant relationship | |||
| No | referent | - | - |
| Yes | 2.27 | 0.49, 10.51 | 0.294 |
| Ever engaged in group sex | |||
| No | referent | - | - |
| Yes | 1.43 | 0.79, 2.58 | 0.226 |
| Meets sexual partners via GSN app c | |||
| No | referent | - | - |
| Yes | 5.58 | 1.65, 18.86 | 0.006 |
| Ever engaged in Chemsex | |||
| No | referent | - | - |
| Yes | 1.09 | 0.57, 2.10 | 0.784 |
| R2 = 19.99 | |||
| Hosmer and Lemeshow Test: Chi-square = 7.18; p = 0.517 | |||
Note:
Includes college, university, professional degree
IPV: intimate partner violence
Geosocial networking
Odds ratio
Confidence interval
p-value
Acknowledgments:
This work was supported by grants from the National Institute on Drug Abuse for career development (K24 DA017072 to FLA; K02 DA033139 to MMC; K01 DA038529 to JW).
Footnotes
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
Conflict of interest: The authors declare that they have no conflict of interest.
Human participants: The study protocol was approved by the Medical Ethics Committee of the University of Malaya, Malaysia.
Informed consent: The interviewees provided written informed consent before participating in the study.
References
- 1.Adler AJ, Martin N, Mariani J, Tajer CD, Owolabi OO, Free C, . . . Perel P (2017). Mobile phone text messaging to improve medication adherence in secondary prevention of cardiovascular disease. Cochrane Database Syst Rev, 4, Cd011851. doi: 10.1002/14651858.CD011851.pub2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Alice G, Serene Y, Rachel S, Hopin L, Nicole N, & Luke W (2018). Improving the public health impact of eHealth and mHealth interventions. Australian and New Zealand Journal of Public Health, 42(2), 118–119. doi: doi: 10.1111/1753-6405.12771 [DOI] [PubMed] [Google Scholar]
- 3.Anand T, Nitpolprasert C, Trachunthong D, Kerr SJ, Janyam S, Linjongrat D, . . . Phanuphak N (2017). A novel Online-to-Offline (O2O) model for pre-exposure prophylaxis and HIV testing scale up. J Int AIDS Soc, 20(1), 21326. doi: 10.7448/ias.20.1.21326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Beyrer C, & Baral SD (2011). MSM, HIV and the law: the case of gay, bisexual and other men who have sex with men (MSM). Geneva: Global Commission on HIV and the Law. [Google Scholar]
- 5.Beyrer C, Baral SD, Van Griensven F, Goodreau SM, Chariyalertsak S, Wirtz AL, & Brookmeyer R (2012). Global epidemiology of HIV infection in men who have sex with men. The Lancet, 380(9839), 367–377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Bien CH, Best JM, Muessig KE, Wei C, Han L, & Tucker JD (2015). Gay Apps for Seeking Sex Partners in China: Implications for MSM Sexual Health. AIDS and Behavior, 19(6), 941–946. doi: 10.1007/s10461-014-0994-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Brislin RW (1970). Back-Translation for Cross-Cultural Research. J Cross-Cultural Psych, 1, 185–216. [Google Scholar]
- 8.Conserve DF, Jennings L, Aguiar C, Shin G, Handler L, & Maman S (2017). Systematic review of mobile health behavioural interventions to improve uptake of HIV testing for vulnerable and key populations. Journal of Telemedicine and Telecare, 23(2), 347–359. doi: 10.1177/1357633x16639186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cooper V, Clatworthy J, Whetham J, & Consortium E (2017). mHealth Interventions To Support Self-Management In HIV: A Systematic Review. The open AIDS journal, 11, 119–132. doi: 10.2174/1874613601711010119 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cutrona CE, & Russell DW (1987). The provisions of social relationships and adaptation to stress. Advances in personal relationships, 1(1), 37–67. [Google Scholar]
- 11.Daly M (2013). The Meth-Fuelled, Wee-Long Orgies Ravaging London’s Gay Sex Party Scene. Vice 3rd June. [Google Scholar]
- 12.Finitsis DJ, Pellowski JA, & Johnson BT (2014). Text Message Intervention Designs to Promote Adherence to Antiretroviral Therapy (ART): A Meta-Analysis of Randomized Controlled Trials. PLoS ONE, 9(2), e88166. doi: 10.1371/journal.pone.0088166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Free C, Phillips G, Galli L, Watson L, Felix L, Edwards P, . . . Haines A (2013). The Effectiveness of Mobile-Health Technology-Based Health Behaviour Change or Disease Management Interventions for Health Care Consumers: A Systematic Review. PLoS Med, 10(1), e1001362. doi: 10.1371/journal.pmed.1001362 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Goedel WC, & Duncan DT (2015). Geosocial-Networking App Usage Patterns of Gay, Bisexual, and Other Men Who Have Sex With Men: Survey Among Users of Grindr, A Mobile Dating App. JMIR Public Health and Surveillance, 1(1), e4. doi: 10.2196/publichealth.4353 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grosskopf NA, LeVasseur MT, & Glaser DB (2014). Use of the Internet and mobile-based “apps” for sex-seeking among men who have sex with men in New York City. Am J Mens Health, 8(6), 510–520. doi: 10.1177/1557988314527311 [DOI] [PubMed] [Google Scholar]
- 16.Hader R (2011). Education matters: Does higher learning yield higher income? Nursing Management, 42(7), 22–27. doi: 10.1097/01.numa.0000398920.55764.73 [DOI] [PubMed] [Google Scholar]
- 17.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, & Conde JG (2009). Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform, 42(2), 377–381. doi: 10.1016/j.jbi.2008.08.010 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Head KJ, Noar SM, Iannarino NT, & Grant Harrington N (2013). Efficacy of text messaging-based interventions for health promotion: A meta-analysis. Social science & medicine, 97, 41–48. doi: 10.1016/i.socscimed.2013.08.003 [DOI] [PubMed] [Google Scholar]
- 19.Henny KD, Wilkes AL, McDonald CM, Denson DJ, & Neumann MS (2018). A Rapid Review of eHealth Interventions Addressing the Continuum of HIV Care (2007–2017). AIDS and behavior, 22(1), 43–63. doi: 10.1007/s10461-017-1923-2 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Holloway IW, Rice E, Gibbs J, Winetrobe H, Dunlap S, & Rhoades H (2014). Acceptability of Smartphone Application-Based HIV Prevention Among Young Men Who Have Sex With Men. AIDS and behavior, 18(2), 285–296. doi: 10.1007/si0461-013-0671-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kanter J, Koh C, Razali K, Tai R, Izenberg J, Rajan L, . . . Kamarulzaman A (2011). Risk behaviour and HIV prevalence among men who have sex with men in a multiethnic society: a venue-based study in Kuala Lumpur, Malaysia. IntJ STD AIDS, 22(1), 30–37. doi: 10.1258/ijsa.2010.010277 [DOI] [PubMed] [Google Scholar]
- 22.Kitsiou S, Pare G, Jaana M, & Gerber B (2017). Effectiveness of mHealth interventions for patients with diabetes: An overview of systematic reviews. PLoS ONE, 12(3), e0173160. doi: 10.1371/journal.pone.0173160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krishnan A, & Cravero C (2017). A multipronged evidence-based approach to implement mHealth for underserved HIV-infected populations. Mobile Media & Communication, 5(2), 194–211. doi: 10.1177/2050157917692390 [DOI] [Google Scholar]
- 24.Landovitz RJ, Tseng C-H, Weissman M, Haymer M, Mendenhall B, Rogers K, . . . Shoptaw S (2013). Epidemiology, Sexual Risk Behavior, and HIV Prevention Practices of Men who Have Sex with Men Using GRINDR in Los Angeles, California. Journal of Urban Health, 90(4), 729–739. doi: 10.1007/S11524-012-9766-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lim SH, Akbar M, Wickersham JA, Kamarulzaman A, & Altice FL (2018). The management of methamphetamine use in sexual settings among men who have sex with men in Malaysia. IntJ Drug Policy, 55, 256–262. doi: 10.1016/j.drugpo.2018.02.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Lim SH, Bazazi AR, Sim C, Choo M, Altice FL, & Kamarulzaman A (2013). High rates of unprotected anal intercourse with regular and casual partners and associated risk factors in a sample of ethnic Malay men who have sex with men (MSM) in Penang, Malaysia. Sex Transm Infect, 89(8), 642–649. doi: 10.1136/sextrans-2012-050995 [DOI] [PubMed] [Google Scholar]
- 27.Lim SH, Brown S-E, Shaw SA, Kamarulzaman A, Altice FL, & Beyrer C (2018). “You Have to Keep Yourself Hidden”: Perspectives From Malaysian Malay-Muslim Men Who Have Sex With Men on Policy, Network, Community, and Individual Influences on HIV Risk. Journal of Homosexuality, 1–23. doi: 10.1080/00918369.2018.1525946 [DOI] [PubMed] [Google Scholar]
- 28.Lim SH, Cheung DH, Guadamuz TE, Wei C, Koe S, & Altice FL (2015). Latent class analysis of substance use among men who have sex with men in Malaysia: Findings from the Asian Internet MSM Sex Survey. Drug Alcohol Depend, 151, 31–37. doi: 10.1016/j.drugalcdep.2015.02.040 [DOI] [PubMed] [Google Scholar]
- 29.Lim SH, Mburu G, Bourne A, Pang J, Wickersham JA, Wei CKT, . . . Azwa I (2017). Willingness to use pre-exposure prophylaxis for HIV prevention among men who have sex with men in Malaysia: Findings from an online survey. PLOSONE, 12(9), e0182838. doi: 10.1371/journal.pone.0182838 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Marcolino MS, Oliveira JAQ, D’Agostino M, Ribeiro AL, Alkmim ΜBM, & Novillo-Ortiz D (2018). The Impact of mHealth Interventions: Systematic Review of Systematic Reviews. JMIR mHealth and uHealth, 6(1), e23. doi: 10.2196/mhealth.8873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.MCMC. (2017a). Hand phone users survey 2017. Malaysia. [Google Scholar]
- 32.MCMC. (2017b). Internet users survey 2017. Malaysia. [Google Scholar]
- 33.Ministry of Health Malaysia. (2016). Global AIDS Response Progress Report: Malaysia 2016. Malaysia. [Google Scholar]
- 34.Ministry of Health Malaysia. (2018). HIV prevalence among men who have sex with men (MSM): Results of the biobehavioral survey. [Google Scholar]
- 35.Moore DJ, Jain S, Dube MP, Daar ES, Sun X, Young J, . . . Morris SR (2018). Randomized Controlled Trial of Daily Text Messages to Support Adherence to Preexposure Prophylaxis in Individuals at Risk for Human Immunodeficiency Virus: The TAPIR Study. Clinical Infectious Diseases, 66(10), 1566–1572. doi: 10.1093/cid/cix1055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Nguyen MX, Krishnan A, Le GM, Nguyen QT, Bhadra NM, Nguyen SM, . . . Go VF (2017). The use of technology to find sexual health information online among men who have sex with men in Hanoi, Vietnam, 2016. International Journal of STD & AIDS, 29(5), 505–510. doi: 10.1177/0956462417738680 [DOI] [PubMed] [Google Scholar]
- 37.Oldenburg CE, Perez-Brumer AG, Reisner SL, Mattie J, Barnighausen T , Mayer KH, & Mimiaga MJ (2014). Global burden of HIV among men who engage in transactional sex: a systematic review and meta-analysis. PLoS One, 9(7), e103549. doi: 10.1371/journal.pone.0103549 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Oldenburg CE, Perez-Brumer AG, Reisner SL, Mayer KH, Mimiaga MJ, Hatzenbuehler ML, & Barnighausen T (2018). Human rights protections and HIV prevalence among MSM who sell sex: Cross-country comparisons from a systematic review and meta-analysis. Glob Public Health, 13(4), 414–425. doi: 10.1080/17441692.2016.1149598 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Oldenburg CE, Perez-Brumer AG, Reisner SL, & Mimiaga MJ (2015). Transactional Sex and the HIV Epidemic Among Men Who have Sex with Men (MSM): Results From a Systematic Review and Meta-analysis. AIDS Behav, 19(12), 2177–2183. doi: 10.1007/s10461-015-1010-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Overdijkink BS, Velu VA, Rosman NA, van Beukering DMM, Kok M, & Steegers-Theunissen PMR (2018). The Usability and Effectiveness of Mobile Health Technology?Based Lifestyle and Medical Intervention Apps Supporting Health Care During Pregnancy: Systematic Review. JMIR mHealth uHealth, 6(4), e109. doi: 10.2196/mhealth.8834 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Radloff LS (1977). The CES-D scale: A self-report depression scale for research in the general population. Applied psychological measurement, 1(3), 385–401. [Google Scholar]
- 42.Rhoton J, Wilkerson JM, Mengle S, Patankar P, Rosser BRS, & Ekstrand ML (2016). Sexual Preferences and Presentation on Geosocial Networking Apps by Indian Men Who Have Sex With Men in Maharashtra. JMIR mHealth and uHealth, 4(4), e120. doi: 10.2196/mhealth.5600 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Schmidt AJ, Bourne A, Weatherburn P, Reid D, Marcus U, & Hickson F (2016). Illicit drug use among gay and bisexual men in 44 cities: Findings from the European MSM Internet Survey (EMIS). International Journal of Drug Policy, 38, 4–12. [DOI] [PubMed] [Google Scholar]
- 44.Stephenson G, & Richardson A (2014). New psychoactive substances in England: a review of the evidence.
- 45.UNAIDS. (2017). Global HIV statistics. Geneva, Switzerland. [Google Scholar]
- 46.United Nations Development Programme. (2014). The policy and legal environments related to HIV services in Malaysia: Review and consultation. Kuala Lumpur, Malaysia. [Google Scholar]
- 47.Ventuneac A, John SA, Whitfield THF, Mustanski B, & Parsons JT (2018). Preferences for Sexual Health Smartphone App Features Among Gay and Bisexual Men. AIDS and Behavior. doi: 10.1007/s10461-018-2171-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Zou H, & Fan S (2017). Characteristics of Men Who Have Sex With Men Who Use Smartphone Geosocial Networking Applications and Implications for HIV Interventions: A Systematic Review and Meta-Analysis. Archives of Sexual Behavior, 46(4), 885–894. doi: 10.1007/s10508-016-0709-3 [DOI] [PubMed] [Google Scholar]


