Abstract
Older adults with obesity are at a high risk of decline, particularly in rural areas. Our study objective was to gain insights into how a potential mobile health obesity wellness intervention (MOWI) in rural older adults with obesity, consisting of nutrition and exercise sessions, could be helpful to improve physical function. A qualitative methods study was conducted in a rural community, community-based aging center. Four community leaders, 7 clinicians and 29 patient participants underwent focus groups and semi-structured interviews. All participants had a favorable view of MOWI and saw its potential to improve health and create accountability. Participants noted that MOWI could overcome geographic barriers and provided feedback about components that could improve implementation. There was expressed enthusiasm over its potential to improve health. The use of technology in older adults with obesity in rural areas has considerable promise. There is potential that this intervention could potentially extend to distant areas in rural America that can surmount accessibility barriers. If successful, this intervention could potentially alter healthcare delivery by enhancing health promotion in a remote, geographically constrained communities. MOWI has the potential to reach older adults with obesity using novel methods in geographically isolated regions.
Keywords: obesity, rural, mobile health, older adults, qualitative
INTRODUCTION
Older adults with obesity are at a risk of functional decline 1 which threatens their capacity to live independently 2. Strategies focusing on lifestyle management only modestly provide safe and effective weight loss 3 as efforts fail to address disability attributed to weight loss-induced sarcopenia 4. Effective therapies for older, mobility-impaired adults are needed, particularly in rural regions – which have both the fastest growing population over 65 years and high rates of obesity 5. Implementing a standard facility-based program is impractical because patients must travel long distances to obtain care and few specialized services exist in remote environments 5. Mobile health (mHealth) technologies may provide a solution for delivering elder-specific health interventions that overcome these barriers 6, 7. Older adults are more technologically connected than previous 8, yet it is unknown how to leverage the promise of technology in delivering effective behavioral change to this at-risk, difficult-to-reach population6.
A mHealth Obesity Wellness Intervention program, with an adaptable, self-monitoring mHealth device coupled with nutrition and exercise sessions was developed. This intervention will use home-based telehealth systems to overcome rural geographic limitations. The purpose of this study aimed at improving the intervention’s acceptability and potential for uptake in rural older adults with obesity by interviewing patients, clinicians, and community leaders to inform efforts prior to intervention implementation 9.
METHODS
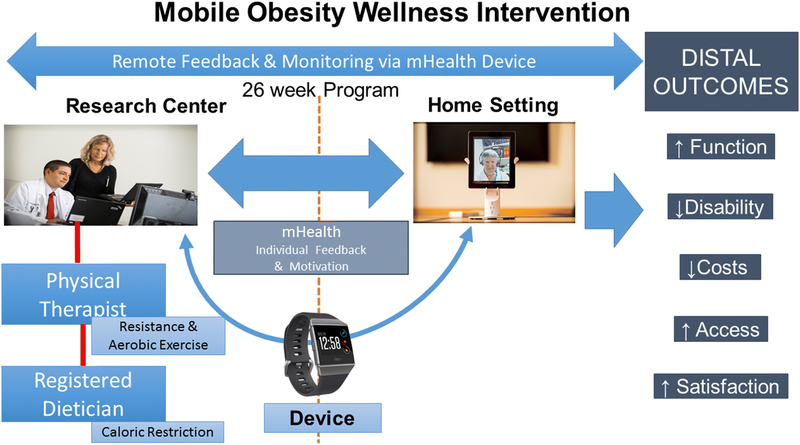
MOWI (Figure 1) is a 26-week program that includes evidenced-based strategies of caloric restriction, activity, and intensive behavioral therapy 10–12. The intervention includes weekly individual dietary counseling (15–20 minutes), biweekly group exercise sessions (70–90 minutes), and an mHealth device with ecological momentary assessment and physical activity monitoring. The dietician sessions consist of behavioral modification 13 and motivational interviewing 10 providing individualized programs of caloric restriction (500–750kCal/d), high protein (1–1.5g/kg/day)14, and 800IU vitamin D supplementation 15. The exercise sessions focus on progressive resistance, flexibility, balance and aerobic activity at moderate intensity 16. Exercises include upper- and lower-limb motions with adjustable cuff weights and resistance bands (e.g. Therabands); resistance training targeting major muscle groups, with increasing workloads; flexibility exercises including static stretches (30–60s); neuromotor training (static, dynamic, vestibular, Tai Chi) addressing agility, balance, and coordination. Participants are instructed to perform their own aerobic activity (minimum 10 minute bouts; total 150min/week). All participant-research team contact will occur via HIPAA-compliant videoconferencing on a tablet.
Figure #1.
Picture of Intervention and behavioral feedback
To evaluate MOWI’s feasibility prior to deployment, focus groups and semi-structured interviews during the 6 months after research approval were conducted. In a rural, academic setting, clinicians, patients, and community leaders were interviewed to enhance the credibility of findings by including diverse stakeholder perspectives. All participants provided a signed, informed consent document and the study was approved by the Committee for the Protection of Human Subjects at Dartmouth College. The study team anticipated different insights and viewpoints. All sampling was purposive. Clinicians were recruited from the academic practice. Community leaders who led local aging initiatives were approached using local networking/email lists. All patients were recruited through local listservs from our local interdisciplinary aging center, or through posters in clinic areas. Theoretical saturation was achieved when the team determined that no new data or concepts and themes were present.
The questions (Appendix 1), followed by clarifying probes to encourage elaboration, were part of a larger discussion on technology, behavioral change, and obesity stigma in older adults. This approach was designed and guided by the interdisciplinary team. Each focus group and individual patient interviews were conducted by two formally trained investigators whose purpose was to assess feasibility of MOWI. MOWI was described using a slide presentation with participants handling the mHealth device.
All interview audio-recordings were transcribed and uploaded into Dedoose, a qualitative software program. Codes were derived and generated 3 domains by inductive transcript review and structural codes were based on focus group and interview guides. Multiple researchers coded data to increase confidence in reporting the results and a third researcher resolved disagreements. Patient quantitative data were collected and descriptive statistics analyzed.
RESULTS
The cohort consisted of 4 community leaders, 7 clinicians, and 29 patients, had mean ages of 64.3 (50% female), 46.7 (71.4% female), and 72.9 years (55% female),), respectively. Patient’s body mass index was 32.9±2.5kg/m2 and 97% had previous technology exposure. Below, key qualitative findings related to benefits (Table 1), barriers, and missing intervention components (Table 2) are reported.
Table #1:
Participant Feedback - Benefits
| Code | Category | Illustrative Quote |
|---|---|---|
| Social | Engagement with others |
Clinician 3: So the ability to engage in this activity and engage, in fact, in some social activity as well without having to disrupt their routine Community 4: So, to be in a group with people where you can still see what your value is and um, against the things that you’re working on and so there’s a, and you see other people struggling. So I just think that multidimensional relationship with some people who are all working together will be a very cool element I guess. |
| Context | Within home setting | Community 1: Yeah, especially with the time commitment and the ability to be able to do it from their own home, I think is going to be huge |
| Distance |
Clinician 2: They can do it at their own home so transportation which I had mentioned as an issue will not be that much of a concern and they can even do it in the winter months. Like when access is going to be like you know they can do it even at home Clinician 6: But if they’re more, if they have those distance barriers to doing that sort of thing, or other barriers, they don’t drive, for whatever reason, don’t a have a car. If they don’t have the option |
|
| Health | Functional limitations | Focus Group 5: keep that hope out there that we don’t all have to end up with some of these disabling, devastating diseases and disorders if we get on board with this train of better health, you know, there’s so much that we can do in small ways, everyday, to improve |
| Quality of Life | Focus Group 5: Maybe we’re not going to be, you know, Olympic athletes but, but the quality of life can be so much better | |
| Accountability | Excuses |
Patient 3: I think the accountability factor. If you say yes to participating, and you have sort of these monitors or obligations and—and it’s been made fairly easy for you to participate, I—I think that’s what’s going to be critical—is you’re accountable and you really have little in the way of excuse. I guess depending on the timing of—of—of the meetings, you know, that’s going to be a factor, but so, yeah. Community 1: They’re also going to be working on—having more accountability for their own health. Clinician 6: I think the structure and the accountability would make things more likely to happen Patient 7: I did not think of that. Same thing, I don’t use Skype, but that’s a technological advance that—that’s really helpful and I think the videoconferencing—you can reach more people and we can, in a rural area, be able to participate without again, making an excuse: “Well, I’m not going to drive all the way to Dartmouth.” |
Table #2 –
Participant Feedback – Barriers/Missing Features
| Technology | Internet access |
Clinician 7: And the lack of Internet and the lack of, I mean I guess if they are technophobic, they might not have Internet access because they can’t get it but they also might just not be interested in that kind of thing Clinician 2: something unless they can be assured that they have that Internet connection wherever they travel because they will travel within that 6-month period Participant 2:That’s not going to be a hindrance [video-conferencing] if they were already tech savvy to being with and if they have strong Internet connection then it’s a must anyway Patient 4: Well my wi-fi signal is good. (chuckle) So that could be a problem for some people in, in a rural area. |
| Expertise | Focus Group 4: Well I ... No, for me, I mean, iťs embarrassing. My computer skills are so limited | |
| Privacy | Invasive |
Clinician 1: I can see some people not liking, not wanting other people and I can see some people being motivated by that so option to try it both ways. And is the exercise group, are they doing it? Is it essentially like an exercise video where you are mimicking the exercises Clinician 1: And then so is there a HIPPA concern? Or anything like that? Or does everybody sign waivers? Are they all in this |
| Timing | Schedule or Season |
Patient 3: I guess depending on the timing of the meetings, you know, that’s going to be a factor. Patient 2: I like mornings, but it would probably be in the early afternoon, because in the evenings or after like 3 or something, my granddaughter always has some type of a sport or something, and if we have to travel to it or something like that, I’d like to go. Focus Group Participants: Participant a) Maybe the amount of time and all. Participant b) Yeah, commitment. Time commitment. Participant C) But for me, um, you know, I can stop what I’m doing and, and go to an appointment, which I do all the time, but, you know, yeah, iťs a win-win. |
|
Patient 3: You know, I think—I think other than having some level of tolerance for, you know, people’s schedules. I mean, I think if you commit to this, you got to be fairly flexible in adjusting your schedule, but on the other hand, there are going to be times when you simply can’t be on the video when, you know, it’s like you can’t make every meeting sometimes. I think there has to be some level of—of appreciation and tolerance for that… Focus Group 2: Yeah twice a week is a lot. Community 2: “Well, you know, this three times a week, uh, thaťs a bit much for me,” or something. I, I’m thinking that ... and I’m, you know, I’m reacting initially to everything- |
||
| Social | Gatherings |
Patient 3: Well, I think—I think the benefit would be ease of access to something I said earlier, that is, being able to access not only the professional input, but to be communicating with others who are going through the same process, you know, like in an AA meeting, not like I’ve ever been to one—dissuade you of that notion, but—and also what I’m anticipating would be a lot of feedback information that you really don’t have to do a whole lot in order to communicate it to the professional through—through the electronic connections. You know, I guess that’s going to be pretty seamless and somewhat automatic. Clinician 3: That would be good. I wonder about family engagement. A lot of my folks are not the people who do the shopping, they are not the people who do the cooking, meals of wheels, there are other things so is there a way to interface with the social network around this patients that’s going to help support or not support the behavior modifications. Focus group 3: Participant a) Question I would have. None of us, as far ... Oh, there are a couple (laughs) but, uh, I’ve never met any of these people. I feel comfortable having them meet people. Who ... We’re- we have a- a shared common enemy. What seems to be missing in this is there’s a certain amount of isolation. I would like there to be somewhere where I could meet the other people who- |
| Providers | Missing providers | Focus Group 5: And it seems like the individual counseling could also help people, you know, set goals and figure out “How am I doing on my goals and what do I want to do next week, readjust my thinking or my, you know, what, you know, am I going to try to do the process next week and, and have somebody give you feedback to say, you know, “Well good job” or, you know “Have you thought about this?” As a strategy type thing. |
| Physical barriers | Participant: Technologically unsavvy or intimidated. Hearing and vision issues. Cognitive issues |
Benefits of MOWI
All groups agreed that MOWI would achieve its objectives towards promoting healthier lifestyle among rural older adults with obesity. Participants perceived that virtual group interaction would improve overall experience.
Participant-5: We think this may improve the health of overweight adults.
Clinician-2: There’s that sense of being part of a group.
Participant-6: There’s energy in the group, if…you’re like “oh I’m really tired today. I don’t really want to do this” and you get in there…and you just do it because it’s a group activity/participation…
Participants saw the potential for MOWI to overcome common barriers to delivering wellness intervention in rural environments, including time, weather and distance.
Clinician-4: If transportation is the barrier, this gets around that. If they’re otherwise homebound, this is great.
Focus Group Participant-4: If weather and roads are a problem and my husband won’t drive, I’d opt for [MOWI].
Focus Group Participant-5: For people to go a long distance twice week would be a challenge, and this kind of overcomes that geographic piece.
Participants identified that MOWI has the potential to improve health by providing an accountability structure.
Patient-7: I would say it’s amazing. And this [MOWI components].…I would have no excuses for being healthier.
Clinician-1: I think it’s hard to make excuses with something this easy…but I think it’s setup so well that you can do it in your home…It would be hard for them to not participate.
Barriers to Using MOWI
Despite the overall positive response toward MOWI, participants identified important barriers pertaining to technology availability and seasonality specific to older adults that could impact the uptake and use of this intervention. Participants raised few privacy concerns.
Clinician-7: There’s a subset of people excluded by virtue of not having a screen or not having Wi-Fi access.
Community-2: I think that anytime you bring technology into that conversation with a lot of these folks, they immediately say, “That’s not for me. “ They are resilient enough and they’ve learned and know these things.
Patient-6: They don’t want to divulge information like this. People are kind of funny about their weight. You don’t [want to be] embarrassed.
Missing Components in MOWI
Participants noted potential missing components of MOWI, including regular social connectedness.
Patient-6: Do you need a psychologist, I don’t know?…You have your MD or nurse practitioner, your nutritionist, your physical therapist for the exercise, and then add a psychologist…
Patient-8: …the lack of social connection...… you can be in the greatest of health and you’re going to go downhill.
DISCUSSION
Participants saw the potential of MOWI to achieve weight loss and improved function and the ability to improve social health, accessibility, and accountability. Improving these factors can positively affect health behavior change 17, 18 suggesting that MOWI may offer a holistic approach to improving health in this population.
It is often said that technology can pose challenges for elders without relevant technical skills. The patient cohort in this study was savvy in using technology and lack of technical expertise did not emerge as a major concern. Older adults are the fastest growing demographic using technology, and studies have proven their ability to learn new skills 19. This knowledge and data will inform how technology can be integrated into MOWI. For instance, the device’s user-interface can be simplified to ease navigation of its functions, and educational sessions on technology can be conducted. This initial usability step will help address early difficulties and enable users to engage effectively with mHealth tools.
Participants emphasized the importance of social connectedness to foster accountability, and community support, which can positively influence health 17, 18. MOWI’s structure (individual dietitian and group exercise sessions) may contribute to a sense of social connectedness. Group sessions allow individuals to feed off other’s thoughts and struggles, while individual sessions provide more personalized support. Both can be conducted via video-conferencing that can be accessed continually and conveniently.
A rural population was targeted, so the intervention must address physical, technological, and financial barriers 20. Participants noted distance, transportation and time difficulties when traveling frequently to receive care. Telemedicine alleviates much of this burden through remote consultation and instruction. Though technological barriers exist, such as poor Internet connections 21, they will decline as Internet accessibility increases. Financial concerns can be addressed through emerging legislation covering remote technologies and health promotion strategies. Proving MOWI’s effectiveness is an important next step to facilitate widespread dissemination.
This current analysis has limitations. Participants were chosen through purposive sampling and data was self-reported. Academic physicians were included and community leaders worked favorably with our organization. The sample lacked racial and ethnic diversity, reflecting high levels of education, and most were Internet users, suggesting the need for diverse older adult populations in future studies.
CONCLUSIONS
This study provides preliminary findings on the potential acceptability and value of implementing a rural, telehealth-delivered intervention for older adults with obesity. Limited transportation and mobility present challenges for rural elderly in engaging in health promotion and may result in social isolation and reduced motivation to engage in behavioral change. MOWI may provide a perception of connectedness that fosters accountability and social support to potentially overcome these challenges, necessitating a future effectiveness study.
Supplementary Material
CLINICAL IMPLICATIONS.
Mobile health technologies have the potential to augment behavioral change in older adults with obesity
Video-conferencing is of particular importance in that it could potential allow the delivery of interventions to individuals without regular access to obesity care
Acknowledgments
FINANCIAL DISCLOSURE
Dr. Batsis’ research reported in this publication was supported in part by the National Institute on Aging of the National Institutes of Health under Award Number K23AG051681. Support was also provided by the Dartmouth Health Promotion and Disease Prevention Research Center supported by Cooperative Agreement Number U48DP005018 from the Centers for Disease Control and Prevention and the Dartmouth Clinical and Translational Science Institute, under award number UL1TR001086 from the National Center for Advancing Translational Sciences (NCATS). The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health or represent the official position of the Centers for Disease Control and Prevention. Dr. Batsis has received honoraria from the Royal College of Physicians of Ireland, the Endocrine Society and provided services to Dinse, Knapp & McAndrew legal firm.
Dr. Bartels receives funding from the National Institute of Mental Health (K12 HS0217695 (AHRQ), NIMH: T32 MH073553, R01 MH078052, R01 MH089811; R24 MH102794 CDC U48DP005018. Drs. Kotz and Naslund report receiving support from the National Institute on Drug Abuse (P30 DA029926). Dr. Carpenter-Song is supported in part by the National Institute on Aging K23AG051681. Dr. Kotz is also supported from the National Science Foundation Grants CNS-1314281 and CNS-1619970.
ABBREVIATIONS
- mHealth
mobile health
- MOWI
mHealth Obesity Wellness Intervention
Footnotes
There are no conflicts of interest pertaining to this manuscript
ETHICS APPROVAL
The Committee for the Protection of Human Subjects approved this human research study (CPHS #28905)
Publisher's Disclaimer: This Author Accepted Manuscript is a PDF file of an unedited peer-reviewed manuscript that has been accepted for publication but has not been copyedited or corrected. The official version of record that is published in the journal is kept up to date and so may therefore differ from this version.
REFERENCES
- 1.Schaap LA, Koster A, Visser M. Adiposity, muscle mass, and muscle strength in relation to functional decline in older persons. Epidemiol Rev. December 4 2013;35:51–65. [DOI] [PubMed] [Google Scholar]
- 2.Zizza CA, Herring A, Stevens J, Popkin BM. Obesity affects nursing-care facility admission among whites but not blacks. Obes Res. August 2002;10(8):816–823. [DOI] [PubMed] [Google Scholar]
- 3.Jensen MD, Ryan DH, Apovian CM, et al. 2013 AHA/ACC/TOS Guideline for the Management of Overweight and Obesity in Adults. Circulation. June 24 2014;129(25 suppl 2):S102–S138. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cruz-Jentoft AJ, Landi F, Schneider SM, et al. Prevalence of and interventions for sarcopenia in ageing adults: a systematic review. Report of the International Sarcopenia Initiative (EWGSOP and IWGS). Age Ageing. November 2014;43(6):748–759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gamm LD , Hutchison LL, Dabney BJ, Dorsey AM. Rural Health People 2010: A Companion Document to Health People 2010. Vol 1 College Station, Texas: The Texas A&M University System Health Science Center, School of Rural Public Health, Southwest Rural Health Research Center; 2003. [Google Scholar]
- 6.Brignell M, Wootton R, Gray L. The application of telemedicine to geriatric medicine. Age Ageing. July 2007;36(4):369–374. [DOI] [PubMed] [Google Scholar]
- 7.Cline AD, Wong M. New frontiers in using telemedicine for nutrition intervention. J Am Diet Assoc. November 1999;99(11):1442–1443. [DOI] [PubMed] [Google Scholar]
- 8.Smith A. Older Adults and Technology Use: Pew Research Center; 2014. [Google Scholar]
- 9.Lewis CC, Fischer S, Weiner BJ, Stanick C, Kim M, Martinez RG. Outcomes for implementation science: an enhanced systematic review of instruments using evidence-based rating criteria. Implement Sci. November 04 2015;10:155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Jay M, Gillespie C, Schlair S, Sherman S, Kalet A. Physicians’ use of the 5As in counseling obese patients: is the quality of counseling associated with patients’ motivation and intention to lose weight? BMC Health Serv Res. June 09 2010;10:159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Pahor M, Guralnik JM, Ambrosius WT, et al. Effect of structured physical activity on prevention of major mobility disability in older adults: the LIFE study randomized clinical trial. JAMA. June 18 2014;311(23):2387–2396. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Villareal DT, Aguirre L, Gurney AB, et al. Aerobic or Resistance Exercise, or Both in Dieting Obese Older Adults. N Engl J Med. 2017;376:1943–1955. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hartmann-Boyce J, Johns DJ, Jebb SA, Aveyard P, Behavioural Weight Management Review G. Effect of behavioural techniques and delivery mode on effectiveness of weight management: systematic review, meta-analysis and meta-regression. Obes Rev. July 2014;15(7):598–609. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Bauer J, Biolo G, Cederholm T, et al. Evidence-based recommendations for optimal dietary protein intake in older people: a position paper from the PROT-AGE Study Group. J Am Med Dir Assoc. August 2013;14(8):542–559. [DOI] [PubMed] [Google Scholar]
- 15.American Geriatrics Society. Workgroup on Vitamin, D. Supplementation for Older Adults: Recommendations abstracted from the American Geriatrics Society Consensus Statement on vitamin D for Prevention of Falls and Their Consequences. J Am Geriatr Soc. January 2014;62(1): 147–152. [DOI] [PubMed] [Google Scholar]
- 16.American College of Sports M, Chodzko-Zajko WJ, Proctor DN, et al. American College of Sports Medicine position stand. Exercise and physical activity for older adults. Med Sci Sports Exerc. July 2009;41(7):1510–1530. [DOI] [PubMed] [Google Scholar]
- 17.Czaja SJ, Boot WR, Charness N, Rogers WA, Sharit J. Improving Social Support for Older Adults Through Technology: Findings From the PRISM Randomized Controlled Trial. Gerontologist. February 15 2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Pruchno RA, Wilson-Genderson M, Rose M, Cartwright F. Successful aging: early influences and contemporary characteristics. Gerontologist. December 2010;50(6):821–833. [DOI] [PubMed] [Google Scholar]
- 19.Kiel JM. The digital divide: Internet and e-mail use by the elderly. Med Inform Internet Med. March 2005;30(1):19–23. [DOI] [PubMed] [Google Scholar]
- 20.Krupinski E. High Volume Teleradiology Service: focus on radiologist and patient satisfaction In: Kumar S, Krupinski E, eds. Teleradiology. Berlin: Spring-Heidelberg; 2008:240–252. [Google Scholar]
- 21.Perrin A. Digital gap between rural and non-rural America persists: Pew Research Institute; 2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.