Abstract
Background
Motivational Interviewing is an evidence-based, client-centred counselling technique that has been used effectively to increase physical activity, including for people with low back pain. One barrier to implementing Motivational Interviewing in health care settings more broadly is the extra treatment time with therapists. The aim of this paper is to describe the design of a cluster randomised controlled trial evaluating the effect of an intervention that pairs Motivational Interviewing embedded into usual physiotherapy care with a specifically designed app to increase physical activity in people with sub-acute low back pain.
Methods
The study is a cluster randomised controlled in which patients aged over 18 years who have sub-acute low back pain (3–12 weeks duration) are recruited from four public hospital outpatient clinics. Based on the recruitment site, participants either receive usual physiotherapy care or the Motivational Interviewing intervention over 6 consecutive weekly outpatient sessions with a specifically designed app designed to facilitate participant-led physical activity behaviour change in between sessions. Outcome measures assessed at baseline and 7 weeks are: physical activity as measured by accelerometer (primary outcome), and pain-related activity restriction and pain self-efficacy (secondary outcomes). Postintervention interviews with physiotherapists and participants will be conducted as part of a process evaluation.
Discussion
This intervention, which comprises trained physiotherapists conducting conversations about increasing physical activity with their patients in a manner consistent with Motivational Interviewing as part of usual care combined with a specifically designed app, has potential to facilitate behaviour change with minimal extra therapist time.
Keywords: Motivational interviewing, Low back pain, Health care app, Musculoskeletal diseases
1. Introduction
Low back pain (LBP) is a common condition and recurrent episodes are common [1]. Acute LBP, in the absence of medical red flags and cauda equina syndrome, has a favourable prognosis with minimal health provider input [2]. Despite this favourable prognosis, LBP remains a costly condition to treat [3], with the majority of costs incurred treating the small proportion of people who go on to experience chronic LBP [4] (an episode lasting 12 or more weeks) [5]. Psychosocial factors become an increasing barrier to recovery as the time since injury progresses, and are best addressed in the sub-acute phase (3–12 weeks post onset) [6]. For the management of acute to sub-acute LBP, international clinical practice guidelines advocate timely resumption of physical activity (PA) [7]. This presents a challenge for clinicians in that it can be difficult to motivate someone who is in pain to resume even low levels of PA.
Motivational Interviewing (MI) is an evidence-based, client-centred counselling technique used across healthcare domains to address ambivalence about healthy behaviour change [8]. It includes a relational component, the spirit of MI (collaboration, evocation, acceptance, compassion) and a technical component, its micro-skills (open questions, affirmations, reflective listening, summarising; OARS) with the intention of eliciting and strengthening client change talk in a positive direction [[8], [9], [10]]. Through the use of an empathic approach to develop patient engagement using technical skills such as reflective listening and directional open questions, MI fosters an environment whereby a person develops and strengthens his/her own arguments for healthy behaviour change [[11], [12], [13]].
When used as an adjunct to usual outpatient physiotherapy treatment, telephone-based MI has been shown to facilitate significant improvements in functional capacity in patients with acute to sub-acute LBP [14]. While telephone-based MI may be convenient the costs of providing this intervention as a stand-alone adjunct to usual care may limit its uptake clinically. Embedding MI within a usual physiotherapy consultation (physiotherapy integrated MI) is likely to be a more efficient alternative to an additional telephone-based MI intervention. Embedding MI within regular treatment modalities however limits MI exposure, potentially reducing effects on functional outcomes such as physical activity [15]. This issue may, in part, be addressed by having two components to an MI intervention; one component delivered by an MI-trained physiotherapist during a regular consultation in a time-efficient manner, and one component provided via a smartphone application (app) to be accessed at the discretion of the patient between physiotherapy consultations. By providing the bulk of MI remotely via an app, therapists could focus on the components of MI not yet able to be replicated in a virtual environment (e.g. empathic listening). This in turn would reduce the amount of MI the therapist needs to deliver within a session, making it more efficient to integrate with an intervention such as physiotherapy.
2. Methods
The study is funded by La Trobe University Sport, Exercise and Rehabilitation Research Focus Area Grant Scheme, the La Trobe University School of Psychology and Public Health (Internal Grant Scheme); The Alumni & Advancement Office, La Trobe University and Telstra Australia (Non-conditional financial support for the programming of the MiMate app and donation of smartphone and tablet hardware for research assistance).
The study has approval from the following Human Research Ethics Committees; Alfred Health (project number 47/15), Eastern Health (reference number E12-2014), La Trobe University (reference number ES12-2014) and Monash Health (reference number 15067X) and the protocol is registered at the Australian New Zealand Clinical Trials Registry number is 1261500724572.
The study design and protocol are consistent with the Consolidated Standards of Reporting Trials 2010 statement [16] and the protocols and reporting implemented according to the Recommendations for Interventional Trials (SPIRIT) guidelines [17].
2.1. Study objectives and hypotheses
2.1.1. Study objectives
The objective is to describe the design and implementation of a cluster randomised controlled trial that examines the efficacy of an innovative application of MI to increase PA in patients receiving physiotherapy for sub-acute LBP. The intervention combines physiotherapists using MI principles as part of their typical consultations with patients with a newly designed MI app for patient use between face-to-face treatment sessions. A secondary objective is to complete a process evaluation of the intervention.
2.1.2. Research hypotheses
The primary hypothesis is that participants in the intervention clusters (who will receive a purpose designed MI intervention in addition to usual physiotherapy care) will demonstrate a significant improvement in PA at 7-week follow up, when compared with participants in the control clusters (who will receive usual physiotherapy care). The secondary hypotheses are that at the 7-week follow up, a significant between-group improvement will also be demonstrated in pain-related self-efficacy and functional capacity (measured by standardised outcome measures) and that the proficiency of the practitioners delivering the MI will be demonstrated.
2.2. Study design and setting
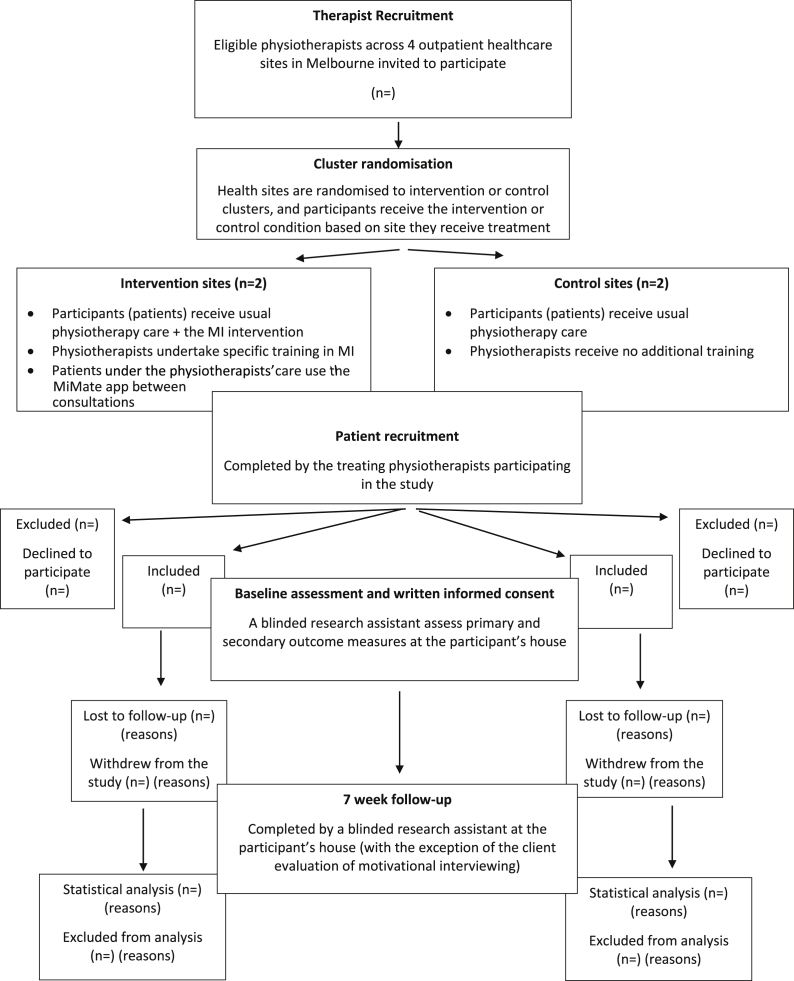
The study is conceptualised as having several phases. The first of these phases involved the design and development of the MI App (see 2.4.2.) which was undertaken over a 36-month period. The second phase involved training of the physiotherapists in how to utilise MI, embed it within conversations with their clients, how to use the MI App (see 2.4.3), and the assessment of the proficiency of the therapists in using MI (see 2.8). The third phase involves recruitment and implementation of a cluster randomised controlled trial conducted in the public outpatient physiotherapy departments of 4 major healthcare sites across Melbourne, Australia. Using pragmatic single block cluster randomisation [18], with the healthcare site as the unit of randomisation, physiotherapists working at each site are randomly assigned to provide usual physiotherapy care (control sites) or the newly developed MI intervention in addition to usual physiotherapy care (intervention sites). The name of each of site is placed in an opaque numbered envelope by an independent researcher and allocated to alternate clusters using a random number generator. Primary and Secondary outcome data (see 2.6.1. and 2.6.2.) are collected at baseline and at 7 weeks (Fig. 1).
Fig. 1.
Design of the study.
2.3. Recruitment and eligibility
Physiotherapists working in outpatient physiotherapy departments at participating healthcare sites are invited to participate in the study if they envisage working in the department for the duration of the study. The site investigator (a senior member of the physiotherapy department) provides eligible therapists with a brief overview of the study and a copy of the information and consent document. Upon reviewing this, therapists confirm their participation by providing written informed consent to one of the study coordinators.
Patient participants are recruited by their treating physiotherapist and are eligible to participate in the study if they are 18 years or older and meet the following inclusion criteria:
-
•
A current sub-acute episode of LBP (3 or more concurrent weeks of pain between the 12th rib and the gluteal fold [5] with or without radicular pain or radiculopathy, preceded by a 30-day period with either no symptoms or a discomfort/baseline pain level the person considers normal).
-
•
Access to a smartphone or tablet device running Apple's iOS© or Google's Android© operating system and access to an Apple App Store© or Google Play© account.
-
•
Competency in the use of simple apps requiring some text input.
-
•
Reside within 40 km of the recruiting health site.
Participants are excluded if they:
-
•
Are currently pregnant.
-
•
Are not fluent in English.
-
•
Have medical red flags which may indicate concurrent sinister medical pathology e.g. have cauda equina syndrome or a current spinal fracture.
-
•
Are waitlisted for lumbar spine surgery at the time of recruitment.
-
•
Have a high risk of severe or very severe Depression and/or Anxiety according to the 21-item self-report Depression, Anxiety and Stress Scale [19]. Participants identified as high risk of anxiety and or depression are followed up by telephone by a study coordinator (POH), (a current Australian registered and practicing psychologist), to ensure appropriate medical follow up is initiated.
Potentially eligible patient participants are contacted by telephone by a research assistant who arranges a time to visit the person's home for an initial assessment and obtains written informed consent.
2.4. Intervention design and development
2.4.1. Intervention rationale and design
This study involves the design and development of a time-efficient MI intervention for physiotherapists to integrate into their usual treatment for sub-acute LBP. Using an approach that combines physiotherapists embedding MI during consultations with an app, there is scope to deliver the majority of the MI content via an app between therapist consultations. This enables the face-to-face sessions with the physiotherapist to be used primarily to develop participant engagement and therefore intervention adherence and deliver the elements of MI that are not yet possible to deliver through the app alone, such as the therapist demonstrating empathy by reflecting to the patient their perceived understanding of their core barriers and facilitators to change.
2.4.2. The MI app
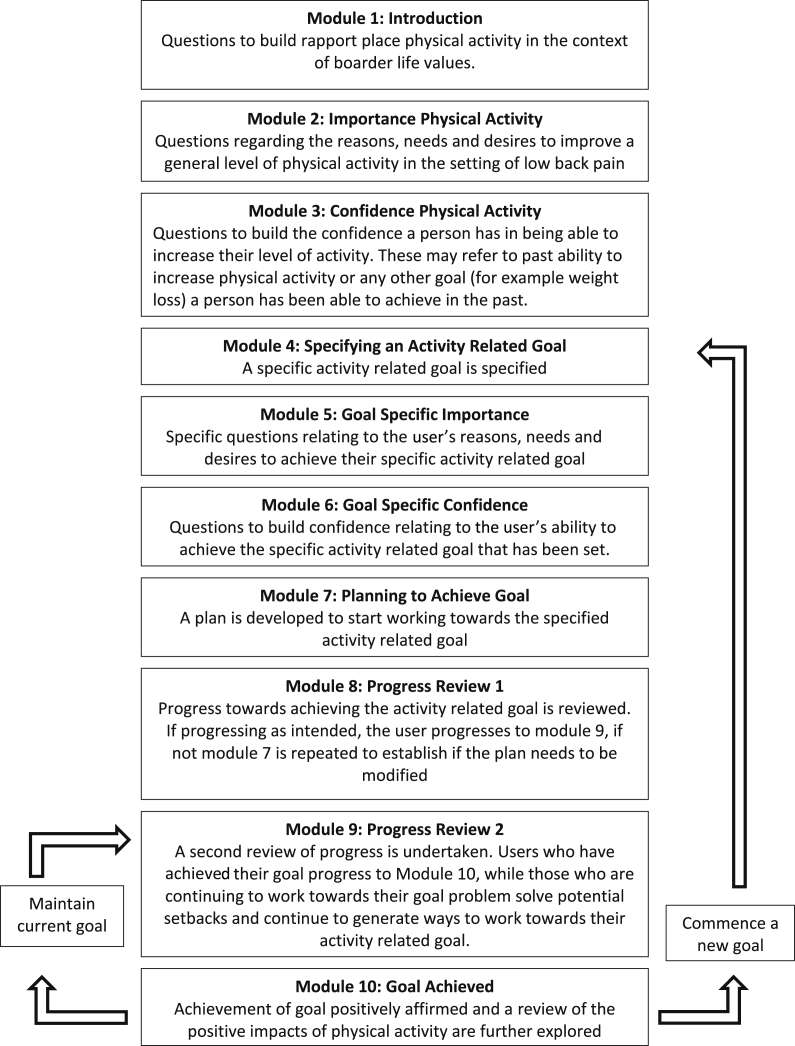
The app, known as MiMate, was developed by the research team from extant literature and the training expertise of the research team (a combined total of over 25 years of MI training experience that includes membership of the Motivational Interviewing Network of Trainers). Using the principles of MI, the MiMate app aims to facilitate an increase in PA in people with sub-acute LBP using a self-directed format that requires minimal additional therapist input. The app was developed as 10 modules (Fig. 2) designed to elicit responses that are consistent with change, referred to as change talk [8]. Increased change talk is identified as a predictor of increased motivation and is a core goal of MI [8,12]. The 10 modules (Fig. 2) are designed to facilitate a participant's motivation for increasing physical activity as part of their rehabilitation through a series of questions and prompts designed to:
Fig. 2.
The interplay between the various modules of the smartphone application.
Identify values of the participant that are related to physical activity (module 1).
-
•
Elicit and strengthen the importance to the participant of increasing their PA (module 2) (Fig. 3)
-
•
Increase a participant's confidence in their ability to increase and sustain PA even in the presence of pain or discomfort (module 3)
-
•
Guide development and implementation of PA-related goals (modules 4–6)
-
•
Elicit and strengthen a participant's readiness for increasing PA (module 7)
-
•
Allow users to monitor the implementation of PA-related goals including planning for potential setbacks (modules 8–10)
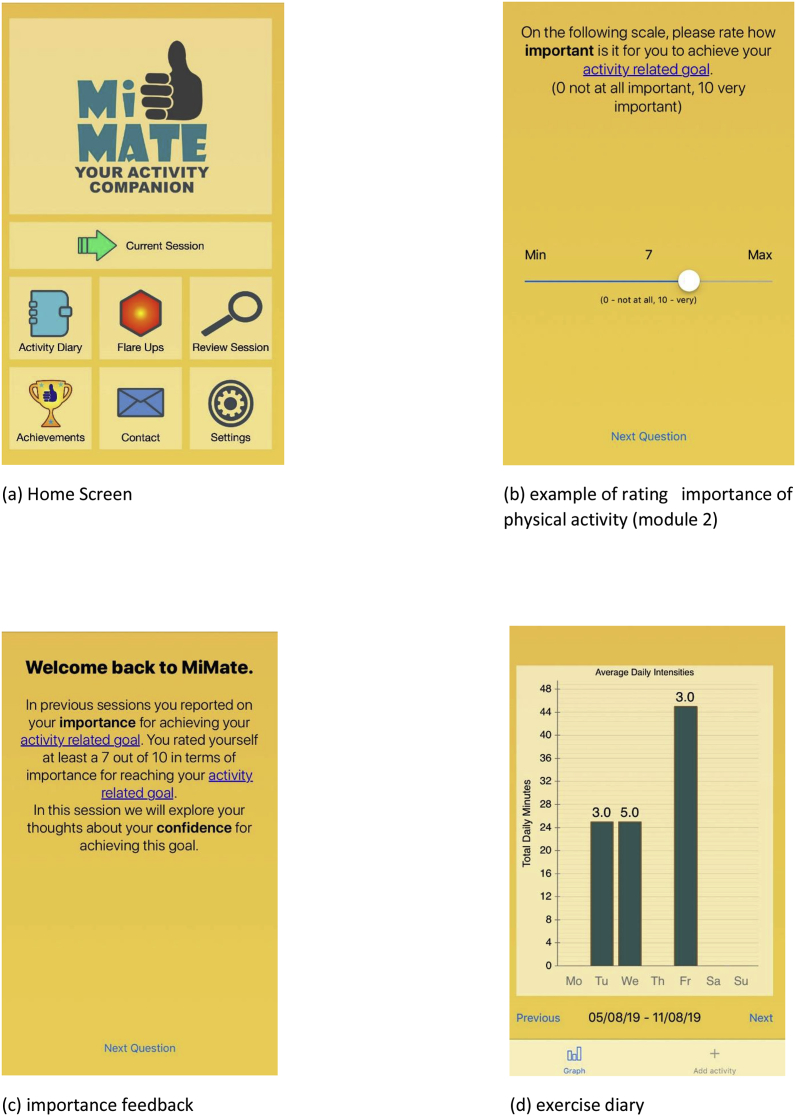
Fig. 3.
Screenshots of the Mimate smartphone application. (a) Home Screen, (b) example of rating importance of physical activity (module 2), (c) importance feedback, (d) exercise diary.
A series of questions and prompts are delivered within the modules to facilitate a participant's motivation for increasing PA as part of their rehabilitation (Fig. 2).
To facilitate the building of motivation through offering feedback of results [8], the MiMate app has an “activity diary” where users enter the amount and intensity of physical activity completed each day (Fig. 3). This information is relayed to users via a bar graph of daily and weekly totals. A “flare up” module is also included, allowing users to obtain basic information and advice on how to problem solve an increase in their symptoms.
The MiMate app was programmed by a team of independent coders from the initial design brief developed by the research team. A selection of smart phone users from the general population piloted the initial version and provided feedback on the language (pitched at non-scientific, non-medical English-speaking population) and usability.
2.4.3. Motivational interviewing embedded physiotherapy
Physiotherapists at intervention sites participate in a purpose designed MI training program developed by the research team (Table 1). Rather than setting aside an allotted time for MI, physiotherapists are trained to integrate the principles of MI into usual conversational patterns that take place throughout a regular physiotherapy consultation. The goal is for the physiotherapist to elicit and strengthen the patient's readiness to undertake PA in a non-threatening manner.
Table 1.
Components of the motivational interviewing training program and app.
| Motivational Interviewing Construct | Embedding within a Physiotherapy Consultation | Supplementation with the App |
|---|---|---|
| Change Talk: Developing reasons, needs and desires to increase level of physical activity. | Throughout usual conversations within a usual physiotherapy consultation, physiotherapists are taught how to facilitate change talk. For example, the physiotherapist is taught how to enquire as to why increasing physical activity might be useful in relation to a patient's values, needs and desires. |
Module 1 of the app askes users about some of the things they value in life. For example a person may say they value playing with their children or walking their dog. The physiotherapist can build on this during consultations by facilitating the patient to link how increasing physical activity may fit in with these broader things they value. |
| Change Talk: Fostering and building confidence to increase level of physical activity. | Therapists are taught how to foster change talk regarding positive past performances during conversations with their patients during consultations. These may or may not be related to physical activity and are designed to build confidence in a persons' ability to implement a change, no matter how seemingly small. |
Modules 3 and 6 of the app ask users a series of specific questions relating to past abilities. These are tailored towards a person's self-reported level of confidence. For example, someone who has a low level of confidence may receive a question about how they were able to achieve a goal in the past. |
| Reflections: Simple: Repeat or slightly rephrase what has been said Complex: Goes beyond a simple reflection in that we reflect what we understood was meant (can involve taking an informed guess) |
Throughout usual conversations within a physiotherapy consultation, therapists are taught to reflect key components of a person's language to foster further change talk. An example of a complex reflection during a supervised exercise session; A patient may comment that the exercise is hard “In a good way”. The therapist may then reflect to the patient “It feels good to be moving again”. |
The app can offer simple reflections. For example, in module 4 when users are asked to set an activity related goal, the app may reflect back “So your activity related goal is to… is this correct?“. The user may answer yes or no and may be asked to clarify if required. |
| Summaries: Are useful for bringing important information together, moving forward or providing an opportunity for patients to correct misunderstandings | Therapists are taught how to summarise a patient's core points related to change in physical activity. For example, therapists are taught how to take a brief moment at the start of the consultation to summarise progress over the last week or clarify any issues. | At the end of each module the app provides a summary of what was covered and this is repeated at the start of each module. |
Training is delivered by the primary and secondary authors at the relevant healthcare site over 2 x 4-h sessions a week apart. The group sessions comprise core MI content and specific training in how to embed MI into conversations during regular treatment. As part of this, therapists are taught how to use and access the MiMate app and how to facilitate the use of the app in an MI consistent manner.
2.5. Intervention implementation
Physiotherapists at intervention sites embed MI within their usual 30-min one-on-one physiotherapy consultation over 6 consecutive weekly outpatient sessions. Providing treatment over a 6-week timeframe increases the likelihood that participants will remain in the sub-acute phase for the entirety of the intervention. To allow for a patient-centred intervention, no time requirement is placed on the ratio of MI and traditional physiotherapy intervention content administered by the physiotherapist in each 30-min session. The therapist has access to the MiMate app modules completed by their patients through a central web server and, with patient consent, may use this to facilitate a discussion about change in the next face-to-face session. For example, a physiotherapist may, while providing treatment, ask a patient about his/her use of the MiMate app over the last week and how he/she rated the importance of engaging in more PA using the MiMate app. The therapist then reflects to the patient his/her understanding, based on what the therapist viewed on the server, of why the patient believes increasing PA is important for recovery. These types of reflective statements, which cannot currently be accurately provided by an app are integral to the change process in MI [8].
The MiMate app can be accessed daily, and patients are able to work through the modules at their own pace. A maximum of one MI module can be completed each day, to allow time for reflection and consolidation of material covered within each completed module.
Physiotherapists at control sites provide their usual physiotherapy care throughout a 30-min consultation, once a week for 6 weeks.
2.6. Outcome measures
All outcome measures are assessed at baseline and 7 weeks (one week following completion of the intervention).
2.6.1. Primary outcome measure: physical activity
The primary outcome variable is the level of PA, measured objectively. The adopted definition of PA does not only refer to structured exercises, but rather any movement of the body bought about by skeletal muscle contraction, producing a resultant expenditure of energy [20].
The average number of daily minutes of moderate to vigorous PA is measured by accelerometer. The ActivePal3 Micro (PAL Technologies, Glasgow, UK) is a small, wireless, accelerometer worn on the anterolateral thigh and detects movement in 3 anatomical planes of motion; vertical, coronal and sagittal [21]. Participants are instructed to wear the accelerometer under a waterproof dressing for 7 continuous days, removing it only for showering or water-based activities. Data are sampled at 20 Hz, stored on the device and downloaded to proprietary software [21] for decryption and analysis by one of the trial coordinators (JH). To establish if PA is moderate to vigorous, each sampling point is assigned a metabolic equivalent (MET) value. A MET value of between 3 and 6 is considered moderate to vigorous [22] and represents a point energy expenditure of 3–6 times the basal metabolic rate [23]. Activities that require removal of the accelerometer (e.g. swimming) are recorded by the participant in an activity diary separate to the MiMate app, and an appropriate MET value assigned based on the description of the activity [24].
2.6.2. Secondary outcome measures
Pain-related activity restriction is assessed by two self-report questionnaires; the Oswestry Disability Index (ODI) and the Patient Specific Functional Scale (PSFS). The 10-item ODI yields a percentage score, with higher scores indicating greater pain related activity restriction [25]. When used to assess activity restriction in relation to LBP, the ODI has a reported intraclass correlation coefficient (ICC) of 0.84 (0.73–0.91) between two test occasions [26]. The PSFS assesses pain-related limitation in up to 5 nominated activities [27]. Each activity is ranked out of 10 with higher scores indicating greater limitation with reference to the individual's pre-injury level. Two scores are provided; the primary activity and the average of the number of activities listed. The PSFS has a reported ICC of 0.85 (0.77, 0.90) when used in acute LBP [28].
Pain-related self-efficacy is assessed on the Pain Self Efficacy Questionnaire (PSEQ), a 10-item self-report questionnaire [29]. The PESQ has been shown to be a valid measure of self-efficacy in people with chronic LBP, when measured against other standardised measures of pain related coping strategies [29].
2.7. Process evaluation
The 16-item Client Evaluation of Motivational Interviewing (CEMI) [30] questionnaire is administered to participants in the intervention clusters at the conclusion of their final treatment session. By assessing a participant's perception of the interactions with their physiotherapist throughout the duration of a consultation, the CEMI provides a quantitative measure of MI treatment fidelity [30]. To minimise confusion pertaining to the content of the CEMI, the word “counsellor” is replaced with “physiotherapist”.
To evaluate how participants (both physiotherapists and patients with LBP) perceived the intervention in its entirety, all physiotherapists and a subset of patient participants (selected randomly) are invited to participate in semi-structured interviews conducted at the conclusion of the data collection. Physiotherapists are asked about issues such as their experiences of the MI training, how the MI training impacted their communication during sessions, how they felt the participants responded to their communication during the sessions and perceived facilitators and barriers to implementation. The patient participants are asked about their experiences of the face-to-face sessions with the physiotherapists, their use of the MiMate app, facilitators and barriers to use of the MiMate app, and their suggested improvements. The same research assistant (not otherwise associated with the study) conducts each interview over the phone.
2.8. Intervention fidelity
A measure of therapist proficiency in the delivery of MI is assessed using the Motivational Interviewing Treatment Integrity scale 4.2.1 (MITI 4.2.1.) [31]. At the conclusion of the final MI training session, physiotherapists participate in a 20-min real play with one of the study coordinators (POH or JH), assuming the role of a patient with an actual behavioural change they have been considering implementing (distinct from a role play which is fictional). A third-party assessor, trained in the use of the MITI and not otherwise associated with the study, reviews and scores the interaction. This process is repeated 6 weeks after the physiotherapist has treated their first participant, to assess potential changes in therapist proficiency.
2.9. Data collection and analysis
All outcome measures, including demographic data (age, gender, time since injury, occupation, sick leave status), except for the Client Evaluation of MI and the MITI scale, are assessed at baseline and 7 weeks by a blinded research assistant. Blinding is not possible for outcome measures relating to MI fidelity and process evaluation, as these measures relate specifically to the intervention.
2.9.1. Data management
Outcome measures and demographic data are entered into a de-identified spreadsheet by one of the study coordinators.
2.9.2. Statistical analysis
2.9.2.1. Sample size considerations
To achieve 80% power at a 0.05 significance level with a large effect size (demonstrated when a single behaviour is targeted and MI proficiency is confirmed) [32], 34 participants are required [33]. Being a cluster randomised trial, a recommended intracluster correlation coefficient of 0.05 is applied to account for variation between clusters, increasing the target sample size to 14 participants per cluster [34,35]. Allowing for a conservative loss to follow up (given the relatively short 6-week intervention) the final target sample size is 15 participants per cluster and 60 participants overall.
2.9.2.2. Data analysis
An analysis of covariance (ANCOVA) will be applied to examine between-group differences at 7 weeks for all primary and secondary outcome measures, with baseline scores entered as covariates [36]. Each baseline variable will be screened prior to entry as a covariate, to ensure the ANCOVA assumptions (normality, collinearity and homogeneity of variance) are not violated [37]. If observed differences suggest possible between-group differences other variables may be included as covariates in the ANCOVA. The MITI 4.2.1. scores of physiotherapists in the intervention clusters will be analysed with a paired-samples t-test to establish any changes in MI proficiency during the trial. Finally, the mean and standard deviation of scores on the Client Evaluation of MI will be analysed descriptively in relation to treatment fidelity. An intention to treat analysis will be applied to all analyses. The recorded qualitative data will be transcribed for thematic analysis using an inductive approach.
3. Discussion
Effective LBP management often requires behaviour change and physiotherapists have expressed the need for more time efficient motivational techniques to help address this issue [38]. This paper outlines a new intervention to assist with this process. This intervention is compared with usual physiotherapy care in a cluster randomised controlled trial of patients with sub-acute LBP across 4 major healthcare sites in metropolitan Melbourne, Australia. As part of this intervention, an MI-based app, known as MiMate, allows the bulk of MI to be delivered remotely, lessening the demands on therapist time. At the same time integrating MI within usual physiotherapy sessions ensures the components of MI that (currently) can only be facilitated though human interaction, are not lost.
There are several strengths with the proposed study design. The cluster analysis prevents contamination between therapists and patients. As well, the proficiency of the physiotherapists is assessed prior to the commencement of the intervention and at the midpoint using a validated measure of treatment fidelity. While there have been over 850 published trials reporting to use MI, it is unclear how many were delivered as intended and with fidelity so there is a clear need to ensure delivery as intended [39,40]. Further, the primary outcome (PA) is assessed using objective measures and process evaluation data for both recipients of the intervention and therapists delivering the intervention are collected at the completion of the study by an independent researcher.
There are some limitations associated with this study. The sample is confined to patients receiving treatment within the public health system, and similar results cannot be assumed in the private health care sector. Furthermore, although a pilot of the MiMate app was conducted during the app's development, this involved a small number of operating systems. There are a multitude of devices running different operating systems which are compatible with the MiMate app. Without first testing the app on all of these devices, which is beyond the scope of the current study, it is possible that some users will experience issues with app reliability which may impact the results. As well, given that experienced therapists are recruited from outpatient health care settings there is a possibility that some of the therapists in the control sites may have had some previous training in MI which may have some impact on interactions with clients at these sites. However, due to randomisation, it would be expected that the level of physiotherapist previous MI experience will be similar in each group. Further, although fidelity is assessed through an assessment of therapist proficiency in MI (on two occasions) using a validated instrument and a client evaluation of the practitioners use of MI, there is no direct assessment of fidelity during client and practitioner sessions.
This paper describes the protocol of a trial of a new intervention to increase physical activity in people with sub-acute LBP that combines a specifically designed app (MiMate) with MI integrated physiotherapy. Despite the challenges noted above this trial will provide data that could facilitate the adoption of more efficient modes of behaviour change for management of musculoskeletal conditions in major health care settings.
Acknowledgements
We would like to thank the management, physiotherapists and participants from Alfred Health, Eastern Health and Monash Health for their participation and support, the research assistants involved with data collection and the funding bodies who contributed to this study. The study is funded by La Trobe University Sport, Exercise and Rehabilitation Research Focus Area Grant Scheme, the La Trobe University School of Psychology and Public Health (Internal Grant Scheme); The Alumni & Advancement Office, La Trobe University and Telstra Australia ( Non-conditional financial support for the programming of the MiMate app and donation of smartphone and tablet hardware for research assistance).
Contributor Information
Paul D O’ Halloran, Email: p.ohalloran@latrobe.edu.au.
Jason Holden, Email: j.holden@latrobe.edu.au.
Jeff Breckon, Email: j.breckon@shu.ac.uk.
Megan Davidson, Email: m.davidson@latrobe.edu.au.
Wenny Rahayu, Email: w.rahayu@latrobe.edu.au.
Melissa Monfries, Email: melissa.monfries@rmit.edu.au.
Nicholas F. Taylor, Email: nicholas.taylor@easternhealth.org.au, n.taylor@latrobe.edu.au.
List of Abbreviations
- App
Smartphone application
- CEMI
Client Evaluation of Motivational Interviewing
- ICC
Intraclass correlation coefficient
- LBP
Low back pain
- MET
Metabolic Equivalent
- MI
Motivational Interviewing
- MITI
Motivational Interviewing Treatment Integrity
- PA
Physical Activity
- ANCOVA
Analysis of Covariance
References
- 1.Pengel L., Herbert R., Maher C.G., Refshauge K. Acute low back pain: systematic review of its prognosis. BMJ. 2003;237:1–5. doi: 10.1136/bmj.327.7410.323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Balagué F., Mannion A.F., Pellisé F., Cedraschi C. Non-specific low back pain. Lancet. 2012;379(9814):482–491. doi: 10.1016/S0140-6736(11)60610-7. [DOI] [PubMed] [Google Scholar]
- 3.Dagenais S., Caro J., Haldeman S. A systematic reveiw of low back pain cost of illness studies in the United States and internationally. Spine J. 2008;8:8–20. doi: 10.1016/j.spinee.2007.10.005. [DOI] [PubMed] [Google Scholar]
- 4.Wasiak R., Kim J., Pransky G. Work disability and costs caused by recurrence of low back pain: longer and more costly than in first episodes. Spine. 2006;31(2):219–225. doi: 10.1097/01.brs.0000194774.85971.df. [DOI] [PubMed] [Google Scholar]
- 5.Hoy D., Bain C., Williams G., March L., Brooks P., Blyth F. A systematic review of the global prevalence of low back pain. Arthritis Rheum. 2012;64(6):2028–2037. doi: 10.1002/art.34347. [DOI] [PubMed] [Google Scholar]
- 6.Waddell G., Burton K., Main C. Royal Society of Medicine Press Ltd; London: 2003. Screening to Identify People at Risk of Long-Term Incapacity for Work a Conceptual and Scientific Review. [Google Scholar]
- 7.Dagenais S., Tricco A.C., Haldeman S. Synthesis of recommendations for the assessment and management of low back pain from recent clinical practice guidelines. Spine J. 2010;10(6):514–529. doi: 10.1016/j.spinee.2010.03.032. [DOI] [PubMed] [Google Scholar]
- 8.Miller W., Rollnick S. third ed. Guilford Press; New York: 2012. Motivational Interviewing: Helping People Change. [Google Scholar]
- 9.Breckon J.D. Motivational Interviewing to promote physical activity and nutrition behaviour change. In: Andersen Mark B., Stephanie J., Hanrahan, editors. Doing Exercise Psychology. 2015. pp. 75–100. Doing Exercise Psychology, Champaign, IL. [Google Scholar]
- 10.O'Halloran P., Blackstock F., Shields N., Holland A., Iles R., Kingsley M. Motivational interviewing to increase physical activity in people with chronic health conditions: a systematic review and meta-analysis. Clin. Rehabil. 2014;28(12):1159–1171. doi: 10.1177/0269215514536210. [DOI] [PubMed] [Google Scholar]
- 11.Madson M.B., Loignon A.C., Lane C. Training in motivational interviewing: a systematic review. J. Subst. Abus. Treat. 2009;36(1):101–109. doi: 10.1016/j.jsat.2008.05.005. [DOI] [PubMed] [Google Scholar]
- 12.Magill M., Gaume J., Apodaca T.R., Walthers J., Mastroleo N.R., Borsari B. The technical hypothesis of motivational interviewing: a meta-analysis of MI's key causal model. J. Consult. Clin. Psychol. 2014;82(6):973–983. doi: 10.1037/a0036833. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Miller W., Rose G. Toward a theory of motivational interviewing. Am. Psychol. 2009;64(6):527–537. doi: 10.1037/a0016830. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Iles R., Taylor N.F., Davidson M., O'Halloran P. Telephone coaching can increase activity levels for people with non-chronic low back pain: a randomised trial. J. Physiother. 2011;57(4):231–238. doi: 10.1016/S1836-9553(11)70053-4. [DOI] [PubMed] [Google Scholar]
- 15.Heinrich E., Candel M.J., Schaper N.C., de Vries N.K. Effect evaluation of a Motivational Interviewing based counselling strategy in diabetes care. Diabetes Res. Clin. Pract. 2010;90(3):270–278. doi: 10.1016/j.diabres.2010.09.012. [DOI] [PubMed] [Google Scholar]
- 16.Schulz K.F., Altman D.G., Moher D. CONSORT 2010 Statement: updated guidelines for reporting parallel group randomised trials. BMC Med. 2010;8(1):18. doi: 10.1186/1741-7015-8-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Chan A.-W., Tetzlaff J.M., Altman D.G., Laupacis A., Gøtzsche P.C., Krleža-Jerić K. SPIRIT 2013 statement: defining standard protocol items for clinical trials. Ann. Intern. Med. 2013;158(3):200–207. doi: 10.7326/0003-4819-158-3-201302050-00583. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Altman D.G., Bland J.M. How to randomise. BMJ. 1999;319(7211):703–704. doi: 10.1136/bmj.319.7211.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Lovibond S., Lovibond P. The Psychology Foundation of New South Wales, University of New South Wales; Sydney, Australia: 1995. Manual for the Depression Anxiety Stress Scales. [Google Scholar]
- 20.Caspersen C.J., Powell K.E., Christenson G.M. vol. 100. 1985. pp. 126–131. (Physical Activity, Exercise, and Physical Fitness: Definitions and Distinctions for Health-Related Research Public Health Reports). 2. [PMC free article] [PubMed] [Google Scholar]
- 21.Stanton R., Vandelanotte C., Duncan M.J. Interdevice baseline signal magnitude variability of the ActivPAL3 activity monitor. Gait Posture. 2014;39(1):618–620. doi: 10.1016/j.gaitpost.2013.06.013. [DOI] [PubMed] [Google Scholar]
- 22.Plasqui G., Bonomi A., Westerterp K. Daily physical activity assessment with accelerometers: new insights and validation studies. Obes. Rev. 2013;14(6):451–462. doi: 10.1111/obr.12021. [DOI] [PubMed] [Google Scholar]
- 23.Byrne N.M., Hills A.P., Hunter G.R., Weinsier R.L., Schutz Y. Metabolic equivalent: one size does not fit all. J. Appl. Physiol. 2005;99(3):1112–1119. doi: 10.1152/japplphysiol.00023.2004. [DOI] [PubMed] [Google Scholar]
- 24.Choi B.C., Pak A.W., Choi J.C. Daily step goal of 10,000 steps: a literature review. Clin. Investig. Med. 2007;30(3):E146–E151. doi: 10.25011/cim.v30i3.1083. [DOI] [PubMed] [Google Scholar]
- 25.Fairbank J., Couper J., Davies J., O'Brian J. The Oswestery low back pain disability questionnaire. Physiotherapy. 1980;66(8):271–273. [PubMed] [Google Scholar]
- 26.Davidson M., Keating A J.L. Comparison of five low back disability questionnaires: reliability and responsiveness. Phys. Ther. 2002;82(1):8–24. doi: 10.1093/ptj/82.1.8. [DOI] [PubMed] [Google Scholar]
- 27.Stratford P. Assessing disability and change on individual patients: a report of a patient specific measure. Physiother. Can. Off. 1995;47(4):258–263. [Google Scholar]
- 28.Costa L., Maher C., Latimer J., Henrique Ferreira P., Ferreira M., Campos Pozzi G. Clinimetric testing of three self-report outcome measures for low back pain patients in Brazil: which one is the best? Spine. 2008;33(22):2459–2463. doi: 10.1097/BRS.0b013e3181849dbe. [DOI] [PubMed] [Google Scholar]
- 29.Nicholas M.K. The pain self-efficacy questionnaire: taking pain into account. Eur. J. Pain. 2007;11(2):153–163. doi: 10.1016/j.ejpain.2005.12.008. [DOI] [PubMed] [Google Scholar]
- 30.Madson M.B., Mohn R.S., Zuckoff A., Schumacher J.A., Kogan J., Hutchison S. Measuring client perceptions of motivational interviewing: factor analysis of the Client Evaluation of Motivational Interviewing scale. J. Subst. Abus. Treat. 2013;44(3):330–335. doi: 10.1016/j.jsat.2012.08.015. [DOI] [PubMed] [Google Scholar]
- 31.Moyers T., Manuel J., Ernst D. University of New Mexico, Center on Alcoholism, Substance Abuse and Addictions (CASAA); 2015. Motivational Interviewing Treatment Integrity Coding Manual 4.2.1.http://casaa.unm.edu/download/MITI4_2.pdf accessed 13 October 2017. [Google Scholar]
- 32.O'Halloran P.D., Shields N., Blackstock F., Wintle E., Taylor N.F. Motivational interviewing increases physical activity and self-efficacy in people living in the community after hip fracture: a randomized controlled trial. Clin. Rehabil. 2015;30(11):1108–1119. doi: 10.1177/0269215515617814. [DOI] [PubMed] [Google Scholar]
- 33.Faul F., Erdfelder E., Lang A.-G., Buchner A. G* Power 3: a flexible statistical power analysis program for the social. Behav. Biomed. Sci. Behav. Res. Methods. 2007;39(2):175–191. doi: 10.3758/bf03193146. [DOI] [PubMed] [Google Scholar]
- 34.Machin D., Campbell M.J., Tan S., Tan S. 3 ed. John Wiley & Sons Ltd; West Sussex, UK: 2009. Sample Size Tables for Clinical Studies. [Google Scholar]
- 35.van Breukelen G.J., Candel M.J. Calculating sample sizes for cluster randomized trials: we can keep it simple and efficient! J. Clin. Epidemiol. 2012;65(11):1212–1218. doi: 10.1016/j.jclinepi.2012.06.002. [DOI] [PubMed] [Google Scholar]
- 36.Stevens J.P. fifth ed. Taylor and Francis; Hoboken: 2012. Applied Multivariate Statistics for the Social Sciences. 5 ed. [Google Scholar]
- 37.Pallant J. 5 Revised ed. Allen & Unwin; Sydney, Australia: 2012. SPSS Survival Manual; pp. 307–328. [Google Scholar]
- 38.Holden J., Davidson M., O'Halloran P. Health coaching for low back pain: a systematic review of the literature. Int. J. Clin. Pract. 2014;68(8):950–962. doi: 10.1111/ijcp.12444. [DOI] [PubMed] [Google Scholar]
- 39.Breckon J.D., Johnston L.H., Hutchison A. Physical activity counseling content and competency: a systematic review. J. Phys. Act. Health. 2008;5(3):398–417. doi: 10.1123/jpah.5.3.398. [DOI] [PubMed] [Google Scholar]
- 40.Wierts C., Wilson P., Mack D. Awareness and use of motivational interviewing reported by Canadian university sport coaches. Int. J. Evid. Based Coach. Mentor. 2019;17(1):63–71. [Google Scholar]