Abstract
Infected popliteal aneurysm is a high-risk condition that may present as an emergency requiring an urgent attention with acute rupture and sepsis. The management of acute ischemia in the presence of local and systemic sepsis is challenging, and infection control and perioperative management during surgery are important. Here we report successful case of treating a patient with an infected popliteal aneurysm. The infection seemed to arise from the soft tissue surrounding the aneurysm, following cellulitis. Our report also includes a review of the related literature and suggests that devising methods for infection control is critical in achieving acceptable outcomes in such cases.
Keywords: infected popliteal aneurysm, resection, revascularization
Introduction
Infected popliteal aneurysms are rare.1,2) Although early surgical treatment is required to prevent rupture, it should also be noted that infection control and perioperative management are important. Here, we report the case of a patient with an infected popliteal aneurysm secondary to lower extremity cellulitis.
Case Report
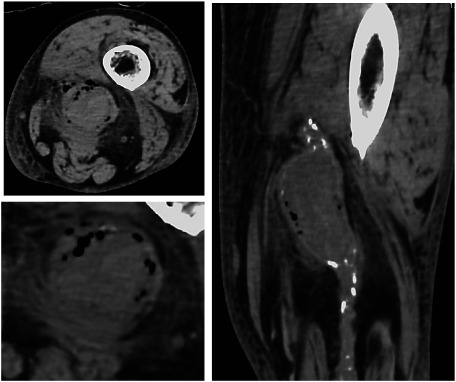
A 70-year-old male came to the emergency department, suffering from fever and swelling in the left lower limb. He received antibiotic treatment for lower extremity cellulitis. However, the symptoms did not improve. Because the cellulitis worsened and the swelling spread to the thighs and buttocks, computed tomography (CT) was performed. He was referred to our hospital because a popliteal artery aneurysm was detected on CT. He had a medical history of hypertension, hyperlipidemia, and chronic renal failure. He was also receiving chemotherapy for colon cancer. It was then revealed after clinical examination that he was pyrexic; painful pulsatile swelling of the left popliteal fossa and signs indicating local inflammation were noted. Laboratory data showed a significantly elevated white blood cell count of 140.4×102/µL and a C-reactive protein level of 25.52 mg/dL. The blood cultures were initially negative. The preoperative ankle-brachial pressure index was 0.73 in the left lower extremity. Moreover, CT showed a thickening of the subcutaneous fat layer, an increase in the fat density from the popliteal region to the buttocks, and a large popliteal aneurysm of size 47×37 mm, with gas at the periphery of the aneurysm and on the outside of the mural thrombus. Around the aneurysm, an enhancement effect of soft tissue shadow was observed (Fig. 1).
Fig. 1 Preoperative computed tomography revealed left popliteal artery pseudoaneurysm with a gas shadow. The soft tissue shadow around the aneurysm was enhanced.
A saphenous vein graft was used as an in situ graft to reduce the exfoliation area, and a below-knee bypass was performed.
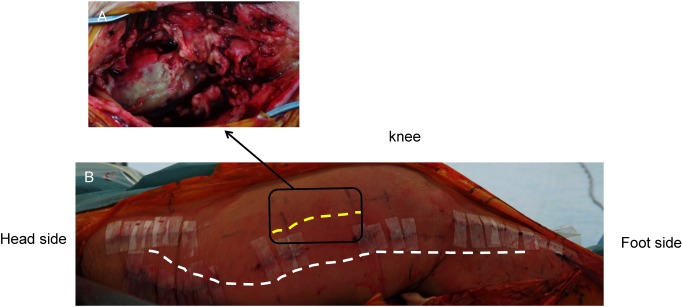
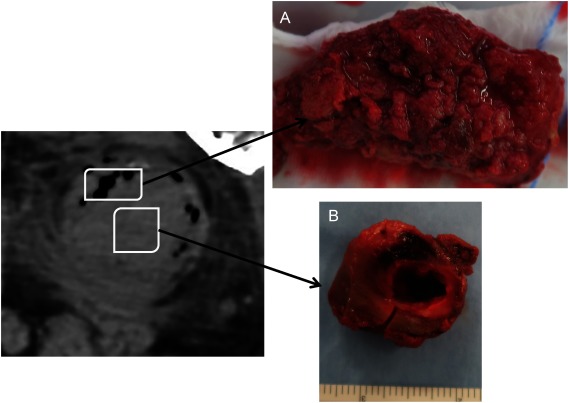
We anastomosed at sites as remote from the infected popliteal aneurysm as necessary and ligated the popliteal artery on the distal side of the proximal anastomosis. We also secured the wound to prevent contamination. We dissected the skin directly above the aneurysm (Fig. 2). Pus had been noticed to have accumulated under the fascia. In addition, the tissue surrounding the aneurysm was full of pus. We then cultured samples of pus collected from each site. The aneurysm had a thin, fragile, edematous wall and was adjudged a true aneurysm. We were unable to clearly identify the adventitia of the aneurysm because of the infection. Blood flow was controlled using a tourniquet wrapped around the thigh. After peeling off the proximal and distal side of the popliteal artery, the aneurysm was excluded with ligation of the popliteal artery. The aneurysm was opened and decompressed. Organized thrombus formation was detected, and evidence of purulence was noted; multiple samples, including tissues from the aneurysm sac, were extracted for culturing. The thrombus closer to the aneurysm wall had small holes consistent with the gas image on CT. No such structures were noted on the thrombus inside the aneurysm, and it had a uniform surface (Fig. 3). Subsequently, the proximal part of the popliteal artery was closed, and the distal part of the popliteal artery was ligated. Finally, we attached the vacuum-assisted closure (VAC) system to the wound and completed the procedure.
Fig. 2 (A) An edematous and fragile aneurysm wall. Transmission and infection of the surrounding soft tissue and muscle tissue. (B) Wounds of the aneurysm approach and bypass wounds were separated as far as possible to prevent infection.
Fig. 3 (A) Small holes consistent with the gas image on computed tomography of the thrombus outside the aneurysm. (B) Internal lumen. Uniform thrombus inside the aneurysm.
Cultures of pus around the aneurysm and thrombus outside the aneurysm wall tested positive for Klebsiella pneumonia, whereas the culture of the thrombus inside the aneurysm wall tested negative for the same species. Echocardiography findings were normal, and no other signs of sepsis were noted. The patient received an antibiotic treatment with vancomycin and metronidazole for a month. He was discharged home on the 22nd postoperative day with an oral antibiotic prescription for one month and antiplatelet therapy with aspirin. Clinical follow-up showed no signs of recurrent infection, and a patent bypass was performed after 6 months. The soft tissue swelling from the thigh to the buttocks disappeared, as confirmed by postoperative CT.
Discussion
The most common symptom of popliteal aneurysms is ischemia due to peripheral thromboembolism caused by the scattering of mural thrombi; however, rupture and infection are rare. Since 2005, we have encountered 21 cases of popliteal aneurysm surgery but only two cases of infected popliteal aneurysm.3,4)
Peripheral mycotic aneurysms are uncommon and have only been described in a few case reports. The pathogenesis of mycotic aneurysms includes four different mechanisms: (1) mycotic aneurysm caused by infective endocarditis, (2) microbial arteritis with aneurysm caused by bacterial infection of an intimal injury or an atherosclerotic plaque during bacteremia, (3) infected preexisting aneurysm, and (4) post-traumatic infected false aneurysm caused by direct bacterial inoculation at the time of arterial trauma.5)
The initial finding in the present case was lower extremity cellulitis that had spread to the thigh. CT detected a thickening of the subcutaneous fat layer from the popliteal region to the buttocks, an increase in fat tissue density, and a popliteal aneurysm with gas around and outside the aneurysm. The culture results of the abscess around the aneurysm and the thrombus of the pore-like structure on the side of the aneurysm wall were positive. However, the culture result of the thrombus on the side of the lumen was negative. Thus, this was considered to be a case of preexisting aneurysm infection derived from the cellulitis, which led to an infection of the popliteal aneurysm.
Plain CT helped identify the infected popliteal aneurysms. The diagnosis of infection is usually based on the clinical course and blood test, edema of surrounding tissues via CT, and others. In the present case, the CT image strongly indicated infection (gas image).
The treatment of infected popliteal aneurysms generally involves resection of the aneurysm and infected tissue and concurrent revascularization.2,6) It was reported that endovascular treatment was successful for patients with infected ruptured popliteal aneurysms in poor general condition.7,8) However, several issues related to long-term results and infection control are yet to be clarified.
The operative procedure should be individualized based on criteria such as the location of the aneurysm, spread of infection, and presence or absence of collateral circulation. Moreover, it is necessary to devise techniques to achieve reliable infection control and revascularization and to prevent the spreading of infection. There is no consensus on the best way to maintain limb circulation, and the decision is usually individualized according to the patient’s general health condition and the severity of local and systemic sepsis.
The treatment and revascularization of infectious popliteal aneurysms were reportedly performed in a single-stage manner using both posterior and internal approaches, with satisfactory results.4) In the present case, although the inflammatory response was high, it did not lead to sepsis. Moreover, the patient’s general condition was relatively stable. Thus, to control infection reliably with single-stage surgery, the VAC system was applied, and surgery was performed.
In the present case, a patent great saphenous vein could be confirmed at a site distant from the planned route to the aneurysm by CT examination. Therefore, we decided to separate the wounds of the aneurysm and approach the wound of the bypass as much as possible to prevent infection and performed a bypass with the internal approach. We performed an in situ bypass to minimize the exfoliation of the bypass graft. This method seemed beneficial in terms of infection prevention. In the approach to aneurysms, vascular control is usually performed at healthy central and peripheral sites. However, in the present case, we wanted to avoid incising the uninfected tissue to control blood flow in the aneurysm. Consequently, the superficial femoral artery was ligated in advance at the peripheral portion of the proximal anastomosis in the bypass, blood flow was controlled with a tourniquet, and the aneurysm and infected tissue were resected. Moreover, VAC was applied on the area where the aneurysm was resected.
Postoperative antibiotic treatment is reportedly necessary for a minimum of 6 weeks postoperatively.5) In the current case, antibiotic treatment was administered for 2 months after the surgery. Postoperative infection control yielded satisfactory results, and recurrence or anastomotic abnormalities have not been observed to date. Cases of leg amputation have been reported when infection control is poor or an anastomotic abnormality occurs.5,9) Therefore, infection control is important from the outset. Because infection was noted in the present case, treatment of the aneurysm and revascularization were conducted using a single-stage procedure via an internal approach. In addition, a surgical method was also devised to achieve reliable infection control, infection spread prevention, and revascularization, which we believe led to the satisfactory outcome.
Conclusion
This report described a surgical case of infectious popliteal aneurysm. Our findings indicated that the source of infection was from outside the mass due to cellulitis. We performed resection and revascularization of the infected aneurysm and obtained satisfactory results by devising techniques to control the infection. Our report suggests that applying methods for infection control is necessary for achieving acceptable outcomes in such cases.
Disclosure Statement
All authors have no conflict of interest.
Author Contributions
Study conception: TS, TN
Data collection: TS, TN
Writing: TN
Critical review and revision: all authors
Final approval of the article: all authors
Accountability for all aspects of the work: all authors
References
- 1).Bonds JW Jr, Fabian TC. Surgical treatment of mycotic popliteal artery aneurysm: a case report and review of the literature. Surgery 1985; 98: 979-82. [PubMed] [Google Scholar]
- 2).Safar HA, Cinà CS. Ruptured mycotic aneurysm of the popliteal artery. A case report and review of the literature. J Cardiovasc Surg (Torino) 2001; 42: 237-40. [PubMed] [Google Scholar]
- 3).Edogawa S, Shibuya T, Kurose K, et al. Clinical Study on Surgical Cases of Popliteal Artery Aneurysms. J Jpn Coll Angiol. 2012; 52: 265-70. (in Japanese) [Google Scholar]
- 4).Tauchi Y, Shibuya T, Shibukawa T, et al. A case of infected popliteal aneurysm treated by resection and revascularisation simultaneously. Jpn J Vasc Surg 2014; 23: 748-51. (in Japanese) [Google Scholar]
- 5).Killeen SD, O’Brien N, O’Sullivan MJ, et al. Mycotic aneurysm of the popliteal artery secondary to Streptococcus pneumoniae: a case report and review of the literature. J Med Case Reports 2009; 3: 117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6).Mann CF, Barker SGE. Occluded mycotic popliteal aneurysm secondary to infective endocarditis. Eur J Vasc Endovasc Surg 1999; 18: 169-70. [DOI] [PubMed] [Google Scholar]
- 7).Bani-Hani MG, Elnahas L, Plant GR, et al. Endovascular management of ruptured infected popliteal artery aneurysm. J Vasc Surg 2012; 55: 532-4. [DOI] [PubMed] [Google Scholar]
- 8).Ghassani A, Delva JC, Berard X, et al. Stent graft exclusion of a ruptured mycotic popliteal pseudoaneurysm complicating sternoclavicular joint infection. Ann Vasc Surg 2012; 26: 730.e13-5. [DOI] [PubMed] [Google Scholar]
- 9).Jebara VA, Nasnas R, Achouh PE, et al. Mycotic aneurysm of the popliteal artery secondary to tuberculosis. A case report and review of the literature. Tex Heart Inst J 1998; 25: 136-9. [PMC free article] [PubMed] [Google Scholar]