Abstract
Composite trichoblastoma and inverted follicular keratosis is extremely rare and the histogenesis is unclear. To date, only four cases have been described in a report. We report a case of 62-year-old woman patient with a palpable cutaneous nodule on the buttock. The patient had a history of squamous cell carcinoma on the lower lip 13 months ago. Excisional biopsy was done, and the microscopic examination revealed composite tumor of trichoblastoma and inverted follicular keratosis. The patient has not been experienced recurrence after surgery.
Keywords: Composite tumor, trichoblastoma, inverted follicular keratosis
Introduction
Trichoblastomas (TBs) are rare benign tumors of the hair germ in which follicle development may be partly or completely recapitulated [1]. Ackerman et al. have used ‘trichoblastoma’ as a generic term for all neoplasms of the skin and subcutaneous fat that are composed mostly of follicular germinative cells [2]. TBs are usually greater than 1 cm in diameter and involve the deep dermis and subcutis. They usually present as a slowly growing nodule. The face, scalp and pelvic girdle are common sites [2,3]. TBs are not aggressive, but a few cases of malignant change have been rarely described [4-6].
Most frequently TB occurs sporadically. A few cases of composite tumor which is composed of TB and another neoplasm such as apocrine poroma [7] or seborrheic keratosis (SK) [8] have been reported. Battistella et al. reported six cases of composite tumors associating trichoblastoma and another benign neoplasm, including SK, inverted follicular keratosis (IFK) or verruca vulgaris [9]. Here, we report a case of composite TB and IFK that developed on the buttock.
Case report
A 62-year-old female patient presented with a palpable mass on the right buttock for a duration of one month. Dermatological examination revealed a solitary asymptomatic, round to oval, verrucous plaque measuring 0.5 × 0.4 cm. Thirteen months previously, the patient underwent wide excision for palpable mass of the lower lip, and the pathologic diagnosis was squamous cell carcinoma, well differentiated. There has been no other remarkable past medical history. Her laboratory tests were within normal limits. Complete excisional biopsy was done. Microscopic examination of the excised specimen showed a well-demarcated skin lesion with exophytic and endophytic proliferation of epidermal squamous and basaloid cells (Figure 1A). Epidermal hyperkeratosis and parakeratosis as well as acanthosis were prominent. Squamous eddies were seen in focal areas. In the center of the lesion, pseudo-invasion was observed (Figure 1B). However, infiltrative growth at the periphery of lesion was not seen. In the superficial dermis, irregular nests of basaloid cells with peripheral palisading of nuclei were identified (Figure 1C). There was no cleft between neoplastic cell nests and peritumoral stroma. No direct connection was observed between both lesions. We reviewed the slides of the previous squamous cell carcinoma of lower lip, and confirmed that these two tumors are histologically distinct neoplasms. Immunohistochemical staining was performed to investigate the characteristics of each component of the tumor. The nested tumor cells in superficial dermis were positive for Bcl-2 (Figure 1D), and negative for CD10 (Figure 1E), calretinin and HPV. Peritumoral stroma showed immunoreactivity for CD10 (Figure 1E). The epidermal component was negative for: Bcl-2, CD10, calretinin and HPV. Based on the clinical and histopathologic findings, we diagnosed this case as a composite TB and IFK. After wide excision of the entire lesion, the patient is currently well, and has not experienced recurrence after 2 months. Informed consent was obtained from the patient presented in this case report.
Figure 1.
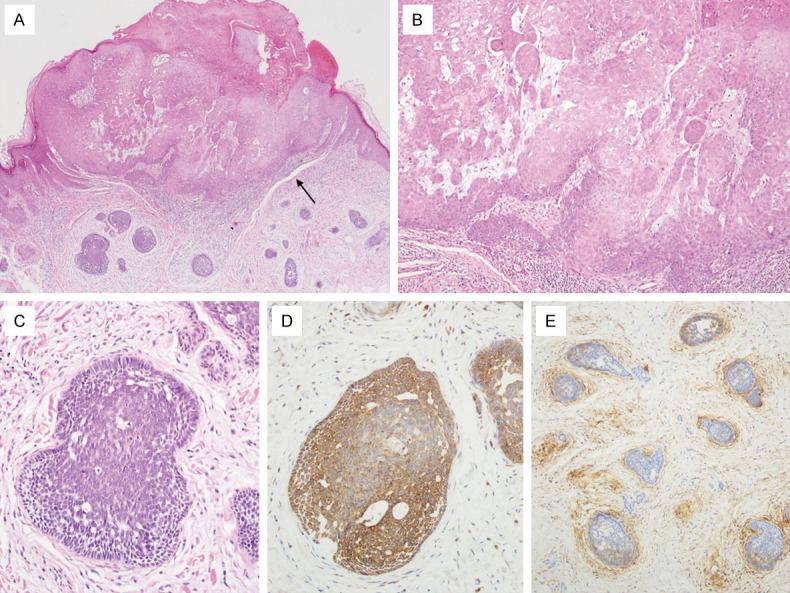
(A) At low power, composite trichoblastoma (TB) and inverted follicular keratosis (IFK) are present, separately. Clefts (arrow) between the follicular stroma of TB and the normal dermis are identified. (B) At medium power, IFK is characterized by an epithelial cell proliferation with various stages of squamous differentiation and residual foci of basaloid cell (arrow). (C) Trichoblastoma has a nest of basaloid cells with peripheral palisading of nuclei, surrounded by follicular stroma. By immunohistochemistry, Bcl-2 was expressed in tumor cells of TB. (D) CD10 was negative in tumor cells (D), whereas it was positive in peritumoral stroma (E) of TB.
Discussion
To the best of our knowledge, very few cases of trichoblastoma (TB) coexisting with another epithelial neoplasm have been reported so far [7-9]. Among 8 cases that have been reported, 4 cases were a composite tumor of TB and inverted follicular keratosis (IFK) [9], 3 cases were TB with SK [8] and 1 case was TB with eccrine poroma [7]. We herein report a composite TB and IFK. Our patient was a 64-year-old female, and the lesion occurred in the buttock. The buttock is a part of the pelvic girdle that is among the sites having a predilection for sporadic TB, following the face and scalp [2,3].
It is sometimes difficult to distinguish TB from basal cell carcinoma (BCC) histologically. Both lesions are composed of proliferative basaloid cell nests. However, TB is histologically characterized by follicular stroma, mild cell atypia, and absence of invasive growth, while BCC has a diffusely myxoid stroma, more amount of cellular atypia, tumor clefts, and infiltrative growth. According to histologic features, the TB component in present case showed follicular stroma, minimal atypia, no myxoid stroma, and tumor clefts,consistent with TB. Additionally, immunohistochemical staining may help this differential diagnosis. CD10 expression can distinguish between TB with peritumoral stromal staining and BCC with epithelial staining, whereas Bcl-2 is expressed in tumor cells of both lesions [10]. In our case, tumor cells of TB were Bcl-2-positive and CD10-negative. CD10 was expressed in only the peritumoral stromal area. These resultsfavor TB rather than BCC.
The histogenesis and nosological status of IFK are not clear. Mostly, IFK has been regarded as a variant of SK. Others consider IFK as a viral-induced epithelial hyperplasia with follicular patterns [11,12]. In our case, however, koilocytotic atypia was not detected and tumor cells of both components were negative for HPV immunohistochemistry. Some authors insist that SK and IFK are distinguishable on clinical and histologic grounds [13]. Ko et al. reported the finding that Bcl-2 positive epidermal dendritic cells are identified in IFK but not SqCC or SK [14]. González-Guerra et al. revealed that the epithelium of the most superficial areas of IFK are positive for calretinin, whichnormally labels the innermost layer of the outer root sheath of hair follicles by immunohistochemistry [15]. In our case, however, neither Bcl-2-positive epidermal dendritic cells nor calretinin-positivity were detected in the IFK component. These results do not support the hypothesis of a the follicular nature of IFK. If IFK is regarded as a variant of SK, in this case, TB and IFK can be considered to originate from different origins and exist together.
We report herein a rare and interesting case of a composite TB and IFK. Further study is required to clarify the histogenesis of IFK and the relationship between TB and IFK.
Disclosure of conflict of interest
None.
References
- 1.Headington JT. Differentiating neoplasms of hair germ. J Clin Pathol. 1970;23:464–471. doi: 10.1136/jcp.23.6.464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Ackerman A, Reddy V, Soyer H. Neoplasms with follicular differentiation. New York, NY: Ardor Scribendi; 2001. [Google Scholar]
- 3.Schirren CG, Rutten A, Kaudewitz P, Diaz C, McClain S, Burgdorf WH. Trichoblastoma and basal cell carcinoma are neoplasms with follicular differentiation sharing the same profile of cytokeratin intermediate filaments. Am J Dermatopathol. 1997;19:341–350. doi: 10.1097/00000372-199708000-00005. [DOI] [PubMed] [Google Scholar]
- 4.Rofagha R, Usmani AS, Vadmal M, Hessel AB, Pellegrini AE. Trichoblastic carcinoma: a report of two cases of a deeply infiltrative trichoblastic neoplasm. Dermatol Surg. 2001;27:663–666. doi: 10.1046/j.1524-4725.2001.00186.x. [DOI] [PubMed] [Google Scholar]
- 5.Regauer S, Beham-Schmid C, Okcu M, Hartner E, Mannweiler S. Trichoblastic carcinoma (“malignant trichoblastoma”) with lymphatic and hematogenous metastases. Mod Pathol. 2000;13:673–678. doi: 10.1038/modpathol.3880118. [DOI] [PubMed] [Google Scholar]
- 6.Kazakov DV, Vittay G, Michal M, Calonje E. High-grade trichoblastic carcinosarcoma. Am J Dermatopathol. 2008;30:62–64. doi: 10.1097/DAD.0b013e31815c6c7f. [DOI] [PubMed] [Google Scholar]
- 7.Santos-Briz A, Rodriguez-Peralto JL, Miguelez A, Lopez-Rios F. Trichoblastoma arising within an apocrine poroma. Am J Dermatopathol. 2002;24:59–62. doi: 10.1097/00000372-200202000-00012. [DOI] [PubMed] [Google Scholar]
- 8.Loh SH, Lew BL, Sim WY. Composite tumor associating trichoblastoma and seborrheic keratosis. Ann Dermatol. 2015;27:601–604. doi: 10.5021/ad.2015.27.5.601. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Battistella M, Peltre B, Cribier B. Composite tumors associating trichoblastoma and benign epidermal/follicular neoplasm: another proof of the follicular nature of inverted follicular keratosis. J Cutan Pathol. 2010;37:1057–1063. doi: 10.1111/j.1600-0560.2009.01341.x. [DOI] [PubMed] [Google Scholar]
- 10.Cordoba A, Guerrero D, Larrinaga B, Iglesias ME, Arrechea MA, Yanguas JI. Bcl-2 and CD10 expression in the differential diagnosis of trichoblastoma, basal cell carcinoma, and basal cell carcinoma with follicular differentiation. Int J Dermatol. 2009;48:713–717. doi: 10.1111/j.1365-4632.2009.04076.x. [DOI] [PubMed] [Google Scholar]
- 11.Spielvogel RL, Austin C, Ackerman AB. Inverted follicular keratosis is not a specific keratosis but a verruca vulgaris (or seborrheic keratosis) with squamous eddies. Am J Dermatopathol. 1983;5:427–442. doi: 10.1097/00000372-198310000-00003. [DOI] [PubMed] [Google Scholar]
- 12.Reed RJ, Pulitzer DR. Inverted follicular keratosis and human papillomaviruses. Am J Dermatopathol. 1983;5:453–465. doi: 10.1097/00000372-198310000-00006. [DOI] [PubMed] [Google Scholar]
- 13.Mehregan AH. Inverted follicular keratosis is a distinct follicular tumor. Am J Dermatopathol. 1983;5:467–470. doi: 10.1097/00000372-198310000-00007. [DOI] [PubMed] [Google Scholar]
- 14.Ko CJ, Kim J, Phan J, Binder SW. Bcl-2-positive epidermal dendritic cells in inverted follicular keratoses but not squamous cell carcinomas or seborrheic keratoses. J Cutan Pathol. 2006;33:498–501. doi: 10.1111/j.1600-0560.2006.00462.x. [DOI] [PubMed] [Google Scholar]
- 15.Gonzalez-Guerra E, Requena L, Kutzner H. Immunohistochemical study of calretinin in normal hair follicles and tumors with follicular differentiation. Actas Dermosifiliogr. 2008;99:456–463. [PubMed] [Google Scholar]


