Abstract
Primary paraganglioma-like dermal melanocytic tumor (PDMT) is a rare dermal melanocytic tumor first recognized in 2004. The cases in previous reports suggested a benign course with a favorable prognosis. Herein, we describe a case of PDMT in the right neck from a 33-year-old man. The tumor cells with mild atypia and low level mitosis consisted of epithelioid cells or spindle cells and were divided into organoid or nest-like structures by fibrous strands and blood vessels, resembling a paraganglioma growth pattern. No necrosis was seen. These cells were positive for HMB45, Melan A, and S-100 with < 5% cells positive for Ki67. Although the morphology conformed to benign features, it recurred after 2 years. In conclusion, while more data are needed to confirm the biologic behavior of this tumor, at least a low malignant potential cannot be excluded.
Keywords: Primary dermal melanocytic tumors, paraganglioma-like structure, PDMT, local recurrence, benign course
Introduction
Primary dermal melanocytic tumors includes several groups of lesions, such as blue nevus, melanocytic schwannoma, melanoma, and clear cell sarcoma. However, there is a group that cannot be classified as any of these entities. This lesion is characterized by a paraganglioma-like structure having no connection with intraepithelial components and immunohistochemical positivity formelanocytic markers, that has been defined as “primary paraganglioma-like dermal melanocytic tumor” (PDMT) by Deyrup et al in 2004 [1]. Currently only 12 cases have been described in the English literature. Previous reports suggested a benign course with a favorable prognosis, however, we report a case with local recurrence 2 years after first resection.
Case report
A 33-year-old man noticed a mass about 0.8 cm in diameter in his right neck 11 years prior to presentation which was asymptomatic. However, the mass began growing rapidly up to 2.5 cm in diameter 2 years ago, so the patient was admitted to our hospital. Physical examination showed a movable painless mass, located at the upper edge of thyroid cartilage in the right middle region of the neck with skin slightly darkened, but having no swelling, ulceration, or warmth. The neck CT showed a well-defined lesion without connection to skin in the right neck and laboratory examination did not show any abnormality, so a hemangioma was considered (Figure 1A). A complete resection of the mass was carried out, following which 3 rounds of interferon treatment were given for the pathologic diagnosis of low grade malignant melanoma. Two years later, the patient was admitted again for a local recurrence of the mass, so a second surgery with extended resection was performed (Figure 1B).
Figure 1.
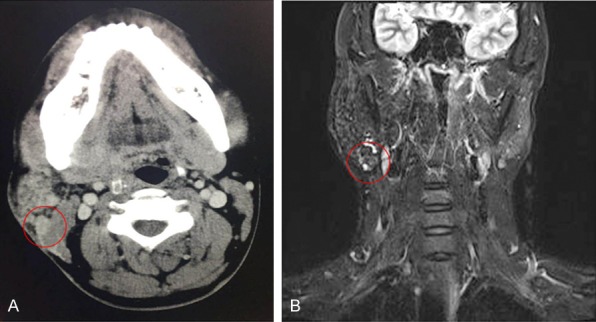
A. CT showed a well-defined lesion without connection to the skin in the right neck. B. MRI showed local tumor recurrence.
Pathological examination of the primary mass showed a complete capsule 2.5 cm × 2.3 cm × 2.0 cm in size without contact to skin. The recurrent mass was a 2.0 × 1.7 × 1.0 cm nodule. Microscopically, these two masses had a clear boundary (Figure 2A, 2B), possessing similar morphologic features. Capsular invasion was observed in the primary but not the secondary mass (Figure 2C). The nodules were divided into packets, nests or short cords by fibrous septa, resembling paraganglioma-like growth pattern (Figure 2D, 2E). Epithelioid or spindle cells were found with mild atypia, eosinophilic to clear cytoplasm, distinct round to oval nuclei, and prominent red nucleoli. Fine dust-like melanin pigment was occasionally observed in the cytoplasm, but deep pigment was apparent around the lesion (Figure 2F). No mitosis or necrosis was seen. Immunohistochemical staining showed that the tumor cells were positive for HMB45 (Figure 3A), Melan A, S-100 (Figure 3B), and vimentin and negative for cytokeratins, EMA, CD34, CgA, synaptophysin, desmin, and SMA. Fewer than 5% cells were positive for Ki67.
Figure 2.
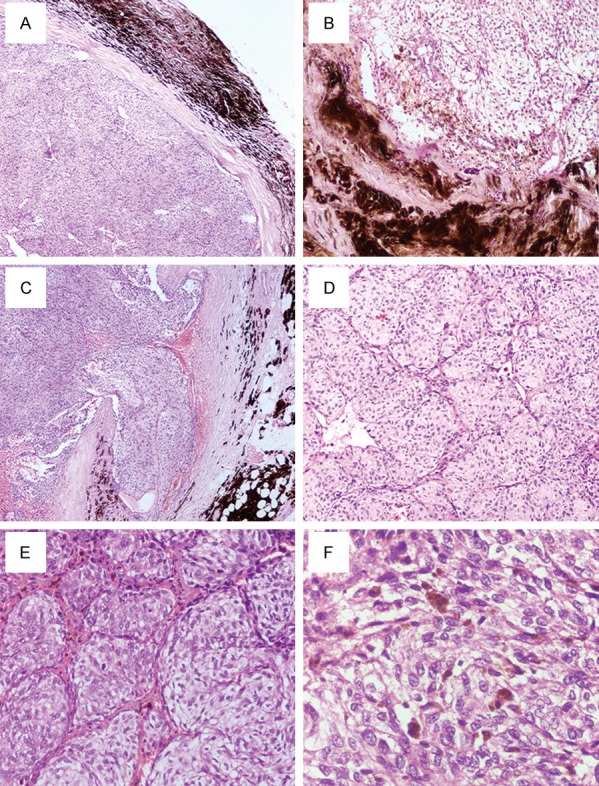
(A) The primary mass showed a complete capsule with deep brown pigment around the mass (×40). (B) The recurrent mass showed a clear margin with the peripheral fat and muscle tissue (×100). (C) Capsular invasion was observed in the primary mass (×40). The nodules in the primary mass (D) (×100) and in the recurrent mass (E) (×200) were divided into packets, nests, or short cords by fibrous septa. (F) Tumor cells with mild atypia consisted of epithelioid cells or spindle cells with eosinophilic to clear cytoplasm, distinct round to oval nuclei, and prominent red nucleoli. Fine dust-like melanin pigment was occasionally observed in the cytoplasm (×400).
Figure 3.
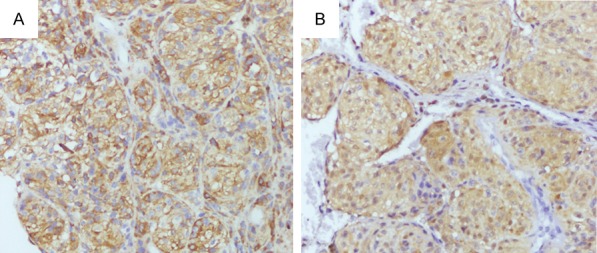
The tumor cells were immunohistochemically positive for HMB45 (A) and S-100 (B) (×200).
The first pathologic diagnosis was low grade malignant melanoma. But through experienced pathologists’ consultation, the recurrent tumor was diagnosed as “paraganglioma-like dermal melanocytic tumor” (PDMT) and the previous case was also revised as this tumor. The patient received no subsequent treatment after the secondary resection and no recurrence or metastasis was seen during 4 years of follow-up.
Discussion
12 cases have been reported since PDMT, a dermal melanocytic tumors with paraganglioma-like growth pattern, was described by Deyrup et al in 2004 [1-5] (Table 1). The age of patients ranged from 13 to 60 years (median 36 years) and male to female ratio was 4:8. The tumor diameter was between 0.5 cm to 5 cm (median 1.7 cm). 6 cases occurred on the thigh, 2 cases on elbow, 1 case on cheek, 1 case on hip, 1 case on knee joint and 1 case was submandibular. The patients usually complained of slowly growing lesions existing for a long time, without any discomfort.
Table 1.
The clinicopathologic features of reported PDMT case
| Age/Sex | Location | Size (cm) | Cytologic atypia | Cytoplasm pigment | Hemorrhage or necrosis | Dermis infiltration | Follow up | Ref. |
|---|---|---|---|---|---|---|---|---|
| 34 F | Lower leg | 4.2 | Mild | Barely | No/No | Favorable | 1 | |
| 23 F | Hip | 0.5 | Mild | Barely | No/No | Yes | Favorable | 1 |
| 18 F | Thigh | 0.5 | Mild | Barely | No/No | Yes | Favorable | 1 |
| 53 M | Thigh | 1.5 | Mild | Barely | No/No | Favorable | 1 | |
| 45 M | Knee | 1.5 | Moderate | Barely | Yes/No | Favorable | 1 | |
| 27 F | Elbow | 0.6 | Mild | Barely | No/No | Favorable | 1 | |
| 53 F | Thigh | 1.2 | Mild | Barely | No/No | Yes | Favorable | 1 |
| 24 F | Elbow | 0.5 | Mild | Barely | No/No | Favorable | 1 | |
| 60 M | Cheek | 0.8 | Mild | No | No/No | No | NA | 2 |
| 13 F | Leg | 5 | Mild | No | No/No | Yes | Favorable | 3 |
| 60 F | Leg | 1-3 | Mild | No | No/No | No | NA | 4 |
| 53 F | Thigh | 1.2 | Mild | No | No/No | No | NA | 5 |
| 33 M | Neck | 2.5 | Mild | Few | No/No | Capsular invasion | Local recurrence | Pre. |
PDMT usually exhibits well-circumscribed single or multiple nodules, occasionally with infiltration into the surrounding dermis [3]. Typically, the nodules involved the deep dermis without connecting with epidermis. Tumor cells, consisting of epithelioid cells or spindle cells with eosinophilic to clear cytoplasm, were divided into organoid or nest-like structures by fibrous strands and blood vessels. The nuclei displayed no atypia or only mild atypia, mitotic activity was low, and necrosis was rare [1]. The cytoplasm did not usually contain melanin pigment or was lightly stained with dust-like melanin pigment. Immunohistochemically, tumor cells were positive for melanocytic markers, such as HMB45, Melan A, and S-100. PDMT needs to be distinguished from other dermal tumors as cellular blue nevus, which is characterized by a poorly circumscribed, infiltrative proliferation, epidermal invasion, and lack of paraganglioma-like growth pattern. Other malignant tumors, such as primary/metastatic melanoma and clear cell sarcoma can be easily excluded because of high-grade nuclear features, high mitotic activity, infiltrative proliferation, and epidermal invasion. In our case, although packets, nests, or short cords separated by fibrous septa were present, the tumor cell nuclei in the primary mass showed mild atypia and capsular invasion which when examined by an inexperienced pathologist, was easy to diagnose as low grade malignant melanoma.
PDMT is considered a benign process because of bland nuclear features, low mitotic activity, and no necrosis, although low malignant potential cannot be excluded [6]. In our case, however, although the morphology suggested benign features and complete resection was conducted on first admission, recurrence emerged 2 years later. Conversely, extensive resection was performed in the second operation, after which the patient was alive with no evidence of relapse or metastasis during a 4 year-follow-up. Our experience indicates even with the benign course of PDMT, an extensive but not complete resection should be done, to avoid a risk of recurrence. Moreover, before concluding this tumor is benign and has a favorable prognosis, more data should be collected and experienced pathologists’ consultation is crucial to clarify its biologic behavior.
Conclusion
We report a rare case of PDMT characterized by a paraganglioma-like structure with mild cellular atypia. Local recurrence appeared 2 years after the first complete resection, but during 4 years of follow-up after the second extensive resection, the patient had no recurrence.
Disclosure of conflict of interest
None.
References
- 1.Deyrup AT, Althof P, Zhou M, Morgan M, Solomon AR, Bridge JA, Weiss SW. Paraganglioma-like dermal melanocytic tumor: a unique entity distinct from cellular blue nevus, clear cell sarcoma, and cutaneous melanoma. Am J Surg Pathol. 2004;28:1579–1586. doi: 10.1097/00000478-200412000-00005. [DOI] [PubMed] [Google Scholar]
- 2.Sarma DP, Teruya B, Wang B. Paraganglioma-like dermal melanocytic tumor: a case report. Cases J. 2008;1:48. doi: 10.1186/1757-1626-1-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Cimpean AM, Ceausu R, Raica M. Paraganglioma-like dermal melanocytic tumor: a case report with particular features. Int J Clin Exp Pathol. 2010;3:222–225. [PMC free article] [PubMed] [Google Scholar]
- 4.Thyvalappil A, Sudhamani B, Kizhakkethara G, Sridharan R, Kunjan R. Paraganglioma-like dermal melanocytic tumor. Indian J Dermatol. 2015;60:80–81. doi: 10.4103/0019-5154.147804. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zinovkin DA, Aliaksinski VS, Hryb AK, Dedik SY. Paraganglioma-like dermal melanocytic tumor: a rare skin lesion. Exp Oncol. 2015;37:156–157. [PubMed] [Google Scholar]
- 6.Elder DE, Murphy GF. Atlas of tumor pathology: melanocytic tumors of the skin. Washington, DC: Armed Forces Institute of Pathology; 2010. pp. 183–185. [Google Scholar]


