Abstract
Objectives:
To evaluate the role of apparent diffusion coefficient (ADC) values in assessing response after chemo-radiotherapy in cervix cancer and investigate the utility of ADC as a tool to identify residual disease, after the treatment completion.
Methods:
A prospective study was done in 100 patients with histopathologically proven cancer of uterine cervix who were classified as either complete response (CR) or residual disease posttreatment. MRI was done pretreatment and after 6 weeks post-treatment with chemo-radiation. 53 patients among the cohort also underwent a fluoro-deoxy glucose positron-emission computed tomography (FDG-PET CT). ADC values, change in ADC values, and metabolic activity obtained from FDG-PET CT were correlated with clinical outcome, and statistical analysis was done to determine the better tool for assessing response evaluation between ADC and PET-CT.
Results:
Residual lesions have notably lower ADC value than that of posttreatment changes. The mean ADC values of residual tumors: 1.26 ± 0.238 × 10−3 mm2/s and mean ADC values of lesions due to posttreatment changes: 1.540 ± 0.218 × 10−3 mm2/s (statistically significant difference between malignant and posttreatment lesions, P < 0.05). ADC has 67% sensitivity, 83% specificity, 35% positive predictive values (PPV), 95% negative predictive values (NPV), and 81% accuracy in differentiating residual disease from post treatment changes. PPV, NPV, sensitivity, and specificity with PET-CT were 93%, 89%, 98%, and 73%, respectively. PPV, NPV, sensitivity, and specificity of contrast MRI were 16%, 91%, 58%, and 59%, respectively.
Conclusion:
Diffusion imaging differentiates residual cervix malignancies from post treatment changes based on ADC values and can be a promising and evocative biomarker. Complimentary use of ADC and PET/CT may increase diagnostic confidence.
Keywords: Apparent diffusion coefficient values, biomarker, fluoro-deoxy glucose positron-emission computed tomography, response assessment, uterine cervix
Introduction
GLOBOCAN fact sheet for India 2018 states uterine cervical carcinoma as the second most common cancer in India in women accounting for 16.5% of all cancer cases in women. Cervical cancer is the fourth-largest cause of cancer mortality in India accounting for nearly 8% of all cancer-related deaths in the country. The current estimates indicate approximately 96,922 new cases diagnosed and 60,078 deaths annually in India, accounting for nearly a third of the global cervical cancer deaths.[1]
There is a broad provincial disparity in the exercise of imaging modalities and magnetic resonance imaging (MRI) in particular, in the workup of cervical cancer. Accordingly, the Fédération Internationale de Gynécologie et d'Obstétrique (FIGO) classification relied exclusively on clinical examination in assessing tumor stage. The current FIGO classification acknowledges the use of imaging methods as an adjunct for cervical cancer staging, and a number of studies have shown that imaging, especially MRI, is better than clinical examination alone for appropriately evaluating cervical carcinoma stage.[2,3] Imaging within 3 months of therapy is principally exigent to interpret the (disease status) following radiotherapy as the tumor microenvironment is affected by hypoxia, granulation tissue, and edema and both residual disease (RD) and radiation fibrosis show increased T2 signal intensity.[4] This adds to the woes of the radiologist while trying to interpret the post treatment MRI of the cervix. Moreover, the changes in macroscopic tumor size significantly delay the biological and molecular changes that develop early in responders.[5]
The existence of residual tumor post treatment in locally advanced cervical cancer, is related to unfortunate clinical outcomes and is a harbinger for the progress of loco-regional recurrence or distant metastasis.[6] The advent of new functional MRI imaging techniques could give a way to the discovery of an imaging biomarker that can foresee poor response to radiotherapy and perceive RD, and recognizing early recurrence with superior accuracy would have insightful prognostic implications. Several authors have compared pre- treatment apparent diffusion coefficient (ADC) values in patients with versus without later tumor recurrence, finding that low pretreatment ADC values seem to be a strong predictor of later tumor recurrence.[7] In patients who fruitfully completed primary treatment, surveillance has been advocated to identify the residual or recurrent disease at curable stages. Where ever available, conventional MRI is the favored imaging modality for evaluating the local extent of cervical cancer due to its exceptional soft-tissue contrast. T2-weighted (T2W) imaging is the reference sequence for cervical cancer staging. Recurrent tumors are known to show high signal intensity on T2W MRI, contrasting with the low-signal intensity of the cervical stroma. However, some benign conditions such as necrosis inflammation and edema may also increase signal intensity on T2W images, posing a prospective challenge to the radiologist, particularly after radiotherapy.[8] Moreover, post treatment changes can result in areas of fibrosis that are also difficult to distinguish from recurrence. Although dynamic contrast-enhanced (DCE)-MRI was shown to be more accurate than T2W alone for tumor recurrence identification, the use of both sequences is recommended.[9] Until the last year, no prospective studies with a cohort of mid-term follow-up and a relatively large number of patients have been reported regarding the utility of ADC parameters as a prognostic factor for clinical outcome in patients with locally advanced cervical cancer. The percentage change of ADC was envisaged as a useful predictor of disease progression and survival in patients with cervical cancer treated with chemo-radiation.[10] Though the overall survival and change in ADC values were studied, there was a lacuna for the predictive ability of ADC to distinguish between RD and CR. Thus, the purpose of this study is to investigate ADC as a tool for clinical assessment post-radical chemo-radiation in the identification of RD and predict the ability of ADC as a biomarker for assessing clinical outcomes.
Methods
After obtaining approval from the institutional review board, a prospective study was done over a period of 1 year including 100 patients who willingly present for MRI examination, treated with chemo-radiation for cervix carcinoma. Patients with any contraindication to MRI examination (cardiac pacemaker, aneurysmal clip, metal prosthesis, etc.) and those who had upfront surgery or were lost follow-up were excluded from the study. Conventional and diffusion-weighted (DW) MRI studies were performed with a Siemens 1.5 Avanto MRI scanner by using a pelvic body coil. Routine pelvic MRI was performed before the initiation of chemo- radiation and post completion of treatment. All of the patients underwent DWIs by using a multisection spin-echo single-shot echo-planar imaging (EPI) sequence. An average of 15 sections was obtained in the axial plane covering the area of interest. Imaging parameters were as follows: TR/TE of 10,000/108 ms, FOV of 23 × 23 cm, an acquisition matrix of 256 × 256, and section thickness of 5 mm with an intersection gap of 1–2 mm. Diffusion-probing gradients were applied in the three orthogonal directions (X, Y, and Z) with the same strength. DWI-MRIs were acquired with DW factor, factor b of 0, 400, and 800 s/mm2. Finally, post-contrast T1WIs (TR/TE of 800/15 ms) were obtained after an intravenous bolus injection of 0.2 mL/kg of body weight of gadolinium-based contrast in all of the patients.
All patients received external beam radiotherapy (EBRT) to the pelvis to a dose of 50 Gy/25 fractions on 6 MV Linac along with five cycles of concurrent weekly chemotherapy with Inj. Cisplatin 50 mg/m2. The overall treatment time was 40–52 days (median overall treatment time 45 days). Post completion of chemo-radiation therapy (CCRT), clinical responses were evaluated by physical examination, histopathology (Pap smear and biopsy wherever feasible) PET/CT, and pelvic MRI.
Region of interest circle (ROI) was drawn using the ADC maps generated from DWIs on the concerned area appearing suspicious for a residual lesion based on T2 hyper-intensity with corresponding restricted diffusion. Areas of abnormal enhancement are considered predominantly worrisome for residual or recurrent tumors. [Figure 1] Efforts were taken to avoid any necrotic areas while measuring initial ADC values (coined ADC 1) and to reproduce the same area of ROI in all the sample cases included in the study (an arbitrary area of 0.25 cm2). The ADC values obtained after chemo-radiotherapy treatment (coined ADC 2) were measured in the corresponding region as ADC 1 values. [Figure 2] Post treatment or final change in tumor ADC values (%) were calculated using the equation: % ADC change = (post treatment ADC − pretreatment ADC)/ pretreatment ADC × 100 [Figure 3].
Figure 1.
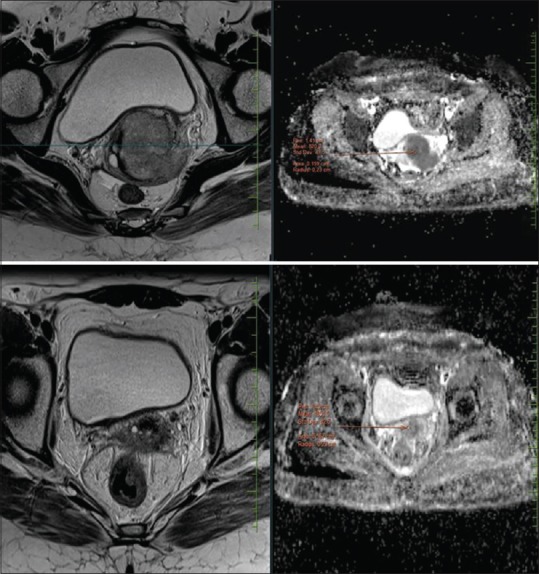
Case of Ca cervix. Top row shows pre chemo radiation mass seen in uterine cervix (mean ADC values marked). Bottom row shows post treatment fibrotic changes with ill-defined enhancing thickening predominantly involving the anterior lip of cervix. ADC values are not representative of residual disease. Histopathological correlation confirmed the above findings
Figure 2.
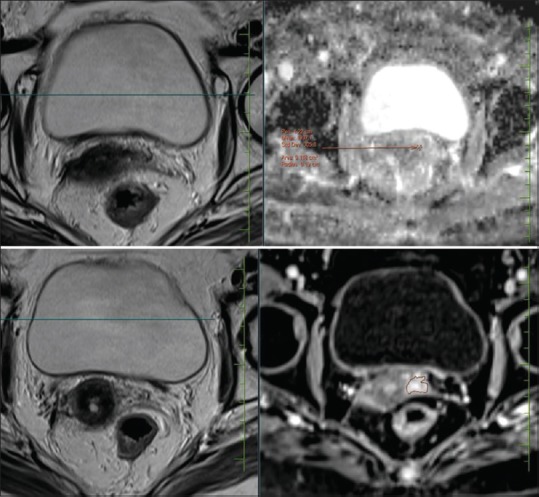
Case of Ca cervix. Status post RT/CCT followed by ICRT. Uterine cervix shows fibrotic changes with ill defined enhancing thickening involving the anterior lip and extending to left parametrium. ADC values suggested residual disease. Histopathological correlation confirmed residual carcinoma
Figure 3.
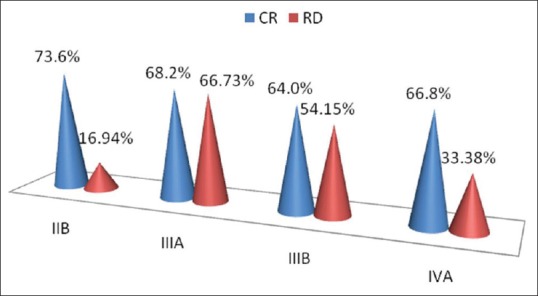
Bar graph showing the percentage of ADC values after completion of treatment and initial clinical FIGO stage
Based on clinical outcome, integrating clinical findings and final histopathological diagnosis, patients were classified as either having no RD or those with CR. Statistical testing was conducted with the statistical package for the social science system version SPSS 21.0. Nominal categorical data between the groups were compared using analysis of variance (ANOVA) and one way ANCOVA test as appropriate. A paired t-test was been used to compare the ADC values for the two groups. ANOVA has been was used to find the significance of study parameters between the groups of patients. Student t-test (two-tailed, dependent) has been used to find the significance of study parameters on a continuous scale between two groups (CR and RD—intergroup analysis) on metric parameters. A receiver operating characteristic (ROC) curve was used to determine the most clinically useful cut-off value of variables in predicting tumor recurrence. The analysis was performed to determine the cut-off ADC value offering an optimal specificity and sensitivity for predicting response to treatment. CR was defined as no clinical complains, with normal Pap smear and uterine cervix examination. In doubtful cases, clinical opinion was sought from imaging and whenever necessary standard histopathological examination was referred to as gold standard. For all statistical tests, a P value of <0.05 was taken to indicate a significant difference.
Results
One-hundred female patients with mean age 53.1 years (28–79 years) and histopathologically confirmed diagnosis of carcinoma (97 patients had squamous cell carcinoma and 3 adenocarcinomas) of uterine cervix were enrolled in this study, including 8 cases of FIGO stage IIa, 43 cases of IIb, 14 cases of IIIa, 31 cases of IIIb, and 4 cases of IVa. In the present study, the most common age group was between 40 and 59 years and the least common between 20–29 and >70 years. Clinical follow-up and standard histopathological examination after chemo-radiation classified 88 patients as CR and 12 patients as RD. For group CR, the ADC value increased gradually after the initiation of therapy, and pretreatment and posttreatment ADC values varied significantly (P < 0.001). For group RD, the ADC value increased gradually after therapy initiated, and pretreatment and posttreatment ADC values varied significantly (P < 0.001).
In order to evaluate the predictive ability of ADC values in classifying the patients as the CR or RD, it is pertinent to first identify and be able to register whether ADC values changed significantly after treatment. We, therefore, compared the difference in the two ADC values (pre and posttreatment) for all the 100 patients, using a paired t-test. The mean percentage change of ADC values [(ADC 2 − ADC 1)/ADC 1]*100 is 66%. From the paired t-test results, it can be concluded that this is a significant difference in the two values (P < 0.05). We, therefore, reject the null hypothesis (no difference between ADC values measured before and after the treatment) and accept the alternative hypothesis (significant difference between ADC values measured before and after the treatment). In further analysis, the post treatment ADC values (ADC 2) are compared between the groups of patients showing CR and those who showed RD.
One-way ANOVA is used to examine the significance of the difference between the ADC values of two groups (CR and RD). The results indicate P < 0.05 suggesting that the null hypothesis (no difference between the ADC 2 values between the group of patients with RD and patients showing CR) be rejected. This implies that there exists a significant difference between the posttreatment ADC values of patients with RD and patients showing CR. In order to test the influence of pretreatment ADC values (ADC 1) on our ANOVA results, we further tested the significance of difference between the posttreatment ADC values (ADC 2) of patients of group 1 (CR) and group 2 (RD), by introducing ADC 1 as covariate and performing a one-way ANCOVA. The results show that there are statistically significant (P < 0.05) differences in posttreatment ADC values between the groups (CR and RD) when adjusted for pretreatment ADC values (ADC 1—, that is, the covariate). The mean values were chalked of the adjusted means (i.e., the original means adjusted for the covariate).
Since the presence of nodes is an important indicator of the presence of RD, we explored whether ADC 2 values were different in patients showing the presence of nodes versus the patients with no visible nodes present. Investigating this shall provide further support to the accuracy of ADC values and their role in predicting the presence of a tumor. An independent sample t-test was used to test the significance of the difference between the two groups. The results [Tables 1 and 2] indicate P > 0.05, suggesting that the null hypothesis (no difference between the posttreatment ADC values of the group showing the presence of nodes and the group without any nodes present) is accepted (Ref. [Tables 1 and 2). PET-CT was performed on 53/100 patients due to economic constraints on part of the patient. In order to understand the extent to which PET-CT results and ADC values can predict the clinical response outcome independently; we ran a logistical regression analysis where ADC values and PET-CT observations were taken as independent or predictor variables and clinical response as the dependent or the outcome variable. The logistic regression model was statistically significant, P < 0.05. ADC values negatively correlate with the clinical response, suggesting that higher ADC values are associated with CR. With an odds ratio of 259.806, PET-CT outcome is likely to be a better predictor of results in the clinical response compared to ADC values [Table 3].
Table 1.
Group statistics
| Nodes | n | Mean | Std. deviation | Std. error mean |
|---|---|---|---|---|
| ADC 2 | ||||
| Y | 26 | 1.49023 | 0.256406 | 0.050285 |
| N | 74 | 1.51312 | 0.233829 | 0.027182 |
Table 2.
T-test for equality of means
| t | df | Sig. (2-tailed) | Mean Difference | Std. error difference | 95% Confidence interval of the difference | ||
|---|---|---|---|---|---|---|---|
| Lower | Upper | ||||||
| ADC 2 | |||||||
| Equal variances assumed | −0.419 | 98 | 0.676 | −0.022891 | 0.054668 | −0.131377 | 0.085595 |
| Equal variances not assumed | −0.400 | 40.559 | 0.691 | −0.022891 | 0.057162 | −0.138370 | 0.092588 |
Table 3.
Variables in the equation : ADC values negatively correlate with the clinical response, suggesting higher ADC values are associated with complete response. With an odds ratio of 139.3, PETCT outcome is likely to be a better predictor of results in the clinical response compared to ADC values
| B | Wald | df | P | Odds ratio | |
|---|---|---|---|---|---|
| Step 1a | |||||
| PET-CT (1) | 5.560 | 5.742 | 1 | 0.017 | 259.806 |
| ADC 2 | −13.614 | 4.061 | 1 | 0.044 | 0.000 |
| Constant | 14.752 | 3.038 | 1 | 0.081 | 2551725.417 |
To test the contribution of contrast MRI we regressed the outcome of contrast MRI on clinical outcome (n = 100). However, the results did not support the assertion that post-contrast MRI findings can be used to predict the clinical response outcome (P > 0.05). The ROC analysis to assess the diagnostic ability of ADC values in the detection of post treatment response of cancer patients was plotted using SPSS (version 21.0). The area under the curve (AUC) is 0.811 at 95% CI and P < 0.05 [Figure 4].
Figure 4.
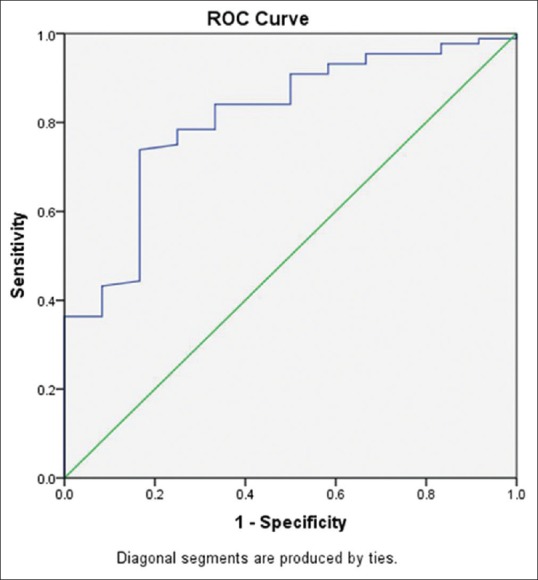
Receiver operating characteristic (ROC) curve obtained with the help of statistical analysis software SPSS. The area under the curve (AUC) is 0.811 at 95% CI and P < 0.05
Upon quantitative analysis of the DWI data, a threshold ADC value of 1.36 × 10−3 mm2/s used for differentiating between post treatment changes and residual cancer showed the highest combined sensitivity, specificity, and accuracy. Refer tabulated Supplementary Data added after references for detailed statistical analysis.
Discussion
DWI is a functional MR technique that has become an unvarying additive to morphologic imaging and its role has been already studied extensively. It can be performed on most MRI machines without any additional new equipment or intravenous contrast agents. It has become increasingly important in the assessment of tumors and evaluation of response during follow-up with various treatment modalities, and it has been recommended as a cancer imaging biomarker in the clinical trials by the National Cancer Institute (NCI) of the USA.[11] DWI combined with ADC mapping has been also investigated as a useful biomarker for assessing and monitoring early treatment response to CRT. However, whether the pre-CRT mean ADC value of cervical cancer could be a reliable predictor of tumor response to CRT has remained controversial. Several studies have confirmed that cellular tumors with low pretreatment ADC values show a better response to various therapies than those with high pretreatment ADC values.[12] In accordance with this study, we found that the pretreatment ADC value (ADC 1) of group CR was almost comparable to that of group RD. (ADC 1/pretreatment in CR was 0.934 and RD was 0.923). Moreover, posttreatment ADC value (ADC 2) of group CR was significantly higher than that of group RD. (ADC 2/posttreatment in CR was 1.5 and RD was 1.26). There were significantly lower ADC 2 values in the RD group as compared to the CR group.
Pretreatment ADC values in this study did not exhibit significantly comparable differences between CR and RD groups. One possible explanation for the above observation is that necrotic tumors offer higher ADC values due to breakdown of the cellular membrane, thereby allowing an increase of diffusing molecules leading to hypoxia, acidosis, and poorly perfusion and thus diminished sensitivity to chemotherapy and radiation therapy. Furthermore, the circulation of chemotherapeutic agents in necrotic tumors may be less proficient because of inadequate vascularity. Therefore, it may be hypothesized that patients with necrotic areas in their tumors, and thus high pretreatment ADC values, would have a poorer treatment outcome. These results demonstrate the possibility of using ADC values for pre treatment prediction of responders from non-responders in patients with uterine cervical cancer that are undergoing chemo-radiation.
Meanwhile, we also found that a few tumors did not respond favorably to the treatment despite having lower pretreatment ADC values. The hypothesis to explain this is necrosis within a tumor may not always be associated with a high ADC. In theory, coagulative necrosis without tumor cell liquefaction may not increase the ADC. It is therefore not adequate to use only pretreatment ADC value for response prediction since it may bring about bias.
It would be preferable to have an early assessment during the course of treatment, which presented a window of the prospect to optimize or alter the treatment plan in those patients who are not undergoing an expected response. Efficient anticancer treatment results in tumor lysis, loss of cell membrane integrity, an augmented extracellular space with an ensuing reduction in tumor cell density, which facilitates water molecule diffusion. Decreases in tumor cellularity will eventually lead to a reduction in tumor size, and this reduction in tumor size can be expected after 2–3 cycles of systemic treatment, which usually is between 6 and 12 weeks after the start of treatment.[13] Studies confirm that changes in ADC values precede changes in tumor size, since early after the start of treatment changes in cellularity and necrosis may already occur. It seems conceivable that DWI had a potential ability to provide an early marker for treatment efficacy regarding microstructure changes, which may precede significant conventional morphologic alterations. Tumor heterogeneity is seen, not just from patient to patient but within the same primary tumor mass itself. Whether it would be possible to precisely predict a tumor's behavior, and to predict the time window for early detection of tumor response after the start of treatment is a key issue.
Payne et al. showed that there was no significant difference in tumor ADCs when separated by other characteristics like tumor type and lymph node metastases.[14] In our study, we also did not find any statistically significant relationship between ADC values and tumor subtype, which may primarily due to the high prevalence of squamous cell type cases. Previous studies showed no significant difference in ADC values between squamous cell carcinomas and adenocarcinoma, whereas Liu et al.[15] showed a significant difference between the two histological types, although with considerable overlap between them. As explained earlier, this may be attributed to a small number of adenocarcinoma included in this cohort, mainly reflecting the less frequent occurrence of this histological type.
Naganawa et al. applied DWI to cervical carcinoma and found that the mean ADC value of cervical cancer lesions (1.09 ± 0.20 × 10−3 mm2/s) was lower than that of the normal cervix (1.79 ± 0.24 × 10−3 mm2/s), and increased after therapy (1.48 ± 0.23 × 10−3 mm2/s).[13] In a study by Chen et al., the ADC values of normal cervical tissue, cervical carcinoma before and after chemoradiotherapy, were measured respectively and found that the mean ADC value of cervical carcinoma (1.013 ± 0.094 × 10−3 mm2/s) in 22 patients was lower than that of normal cervical tissue (1.593 ± 0.151 × 10−3 mm2/s) and increased following the completion of therapy (1.436 ± 0.129 × 10−3 mm2/s).[4] Our study shows similar results. [Refer 5,6] Liu et al. reported that the pre-CRT mean ADC value of tumors with a partial response was the pre-CRT mean ADC value of a tumor did not significantly correlate with tumor response, the mid-CRT ADC value or change of the ADC value during CRT, compared with pre-CRT, has been reported to be significantly correlated with treatment response.[15] This is in accordance with our study where we found that posttreatment ADC 2 values and change in ADC values were more sensitive markers of disease progression.
The necessity of ADC parameters other than mean ADC has been emphasized for a more precise prediction of the treatment response. Cellular characteristics and hypoxia of tumors influence the tumor response to CRT and treatment outcomes. Necrotic tumors are frequently hypoxic and poorly perfused, leading to diminished sensitivity and poor local control to CRT. Thus, necrotic tumors are prone to tumor progression and recurrence after CRT. On DWI, although the mean ADC value of the tumor increases as tumoral necrosis progresses, it tends to be influenced more by the tumor portion with the highest cellularity. From this perspective, it was postulated that high percentile ADC values through histogram analysis could represent the regions with high necrotic fraction within the heterogeneous tumor and, in turn, be associated with poor clinical outcome in patients with uterine cervical cancer treated with chemo-radiation.
Kinkel et al. found that DCE-MRI is helpful in improving the specificity and accuracy of tumor recurrence detection. They also proved that in the first 5 months after radiation therapy, induced inflammatory changes are known to be responsible for early enhancement that mimics recurrence. We strengthened our study by collaborating qualitative assessment of contrast enhancement and ADC values after the radical completion of treatment.[14] In the study by Hricak et al., there was a nonspecific enhancement of the cervix after radiation therapy related to benign changes such as post-irradiation fibrosis, inflammation, and necrosis.[9]
Nakamura et al. indicated that mean ADC of the tumor was lower in FIGO stage IIb-IVa and with parametrial, vaginal, pelvic lymph node involvement. The pre- and posttreatment mean ADC were not statistically associated with vaginal invasion and pelvic lymph node metastases. In our study, we did not find any statistically significant relationship between ADC values and lymph node status.[7]
McVeigh et al. reported that the median ADC of cervical cancers (1.09 ± 0.20) was lower than that of control cervical tissue (2.09 ± 0.46) with very little overlap. They showed that the median ADC of cervical cancer was significantly lower in FIGO stages T1B/T2a compared to T2b and T3/T4.[16] Our study shows median ADC values 0.915 ± 0.149, consistent with the earlier study. The tumor ADC values of patients with early FIGO stage II were higher those with late FIGO stage III/IV at pre-treatment evaluation but there was no statistically significant difference.
Liu et al. reported that the pre-CRT mean ADC value of tumors with a partial response was significantly higher than that of tumors with CR in cervical cancer. In contrast, although the pre-CRT mean ADC value of a tumor did not significantly correlate with tumor response, the mid-CRT ADC value or change of the ADC value during CRT, compared with pre-CRT, has been reported to be significantly correlated with treatment response.[15] This is in accordance with our study where we found that post treatment ADC 2 values and change in ADC values were more sensitive markers of disease progression. A significant difference was found between pre treatment and post treatment (both P < 0.001). The reason for the reduction in ADC value within the tumor is due to hypercellularity within the malignant tissue causing restriction of the diffusion of water molecules. The increase in ADC values following CRT may be presumably due to cellular apoptosis and an increase in extracellular space resulting in increased water diffusion. However, the cause for the ADC values to be still lower than that of normal cervical tissue may be due to the presence of edema, hyaline degeneration, and granulation tissue in the cervical tissue after therapy.
Recent literature has shown preliminary results highlighting a good correlation between simultaneously obtained morphological (RECIST) and PET-based (PERCIST) criteria for the assessment of therapy response in the uterine cervix. But, the study is carried on a very small cohort of patients.[17]
Conclusion
This study highlights that MRI-derived imaging parameters can be a promising and meaningful biomarker of clinic-pathological features and prognosis in cancer of the uterine cervix. DWI also carries the potential of predicting early indications of the therapeutic outcome because molecular and cellular changes typically precede observable macroscopic changes in gross tumor size, thus, providing a window of opportunity to modify the initial treatment regimen to improve the clinical outcome and minimize the morbidity associated with prolonged and ineffective treatment. DWI also holds promise for distinguishing residual tumors from radiation changes. Furthermore, when compared with PET-CT, ADC yielded better specificity and negative predictive value, with almost comparable levels of accuracy. So, a favorable comparison of ADC studies with PET-CT may further cement its role in the management of treated cervix cancers.
However, the cost and logistics of MRI is an important factor in routine clinical implementation. In developing countries like India, where carcinoma cervix is associated with poor socioeconomic status, affordability and logistics of routine pretreatment MRI, is an issue that limits the wider application in general and as per FIGO guidelines should be considered currently as an adjuct in management.
Informed consent
Written informed consent was waived by the Institutional Review Board.
Ethical approval
Institutional Review Board approval was obtained.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
Acknowledgement
The authors would like to thank Dr. Raghunadharao Digumarti (Director of Medical Oncology in Homi Bhabha Cancer Hospital and Research Centre, Visakhapatnam, India) for his valuable comments and feedback on the paper.
Supplementary Data
Table S1 summarizes the measures of central tendency for ADC values 1 and 2 for both groups (CR and RD). Skewness and Kurtosis represent the variation of the data from a standard normally distributed bell curve.
Table S1.
Descriptive statistics
| Group | n | Range | Min | Max | Mean | Std. deviation | Skewness | Kurtosis | ||
|---|---|---|---|---|---|---|---|---|---|---|
| Statistic | Statistic | Statistic | Statistic | Statistic | Statistic | Statistic | Std. Error | Statistic | Std. Error | |
| CR | ||||||||||
| ADC 2 | 88 | 1.255 | 0.683 | 1.938 | 1.54070 | 0.218182 | −0.964 | 0.257 | 1.832 | 0.508 |
| ADC 1 | 88 | 0.846 | 0.683 | 1.529 | 0.93406 | 0.153671 | 1.083 | 0.257 | 2.343 | 0.508 |
| Valid N (list wise) | 88 | |||||||||
| RD | ||||||||||
| ADC 2 | 12 | 0.914 | 0.708 | 1.622 | 1.26125 | 0.248425 | −0.672 | 0.637 | 1.172 | 1.232 |
| ADC 1 | 12 | 0.427 | 0.785 | 1.212 | 0.92325 | 0.124140 | 1.105 | 0.637 | 1.407 | 1.232 |
| Valid N (list wise) | 12 | |||||||||
In order to evaluate the predictive ability of ADC values in classifying the patients as the CR or RD, it is pertinent to first identify and be able to register whether ADC values changed significantly after treatment. We, therefore, compared the difference in the two ADC values (pre- and posttreatment) for all the 100 patients using a paired t-test. Also called dependent sample t-test, the paired t-test is used to assess group differences in a repeated measures design or before and after studies.
The following null hypotheses are proposed:
Ha0: There is no difference between ADC values measured before and after the treatment
Ha1: There is a significant difference between ADC values measured before and after the treatment
From the master chart, it follows that the mean percentage change of ADC values [(ADC 2 − ADC 1)/ADC 1]*100 is 66%. From the paired t-test results as shown in Table S2, it can be concluded that this is a significant difference in the two values (P < 0.05). We, therefore, reject the null hypothesis Ha0 and accept the alternate hypothesis Ha1.
Table S2.
Paired samples test
| Paired differences | t | df | Sig. (2-tailed) | |||||
|---|---|---|---|---|---|---|---|---|
| Mean | Std. deviation | Std. error mean | 95% confidence interval of the difference | |||||
| Lower | Upper | |||||||
| Pair 1 | ||||||||
| ADC 1-ADC 2 | −0.574410 | 0.303046 | 0.030305 | −0.634541 | −0.514279 | −18.955 | 99 | 0.000 |
In further analysis, the posttreatment ADC values (henceforth referred to as ADC 2) are compared between the groups of patients showing CR and those who showed RD. We hypothesize the following:
Hb0: There is no difference between the ADC 2 values between the group of patients with RD and patients showing CR.
Hb1: There is a significant difference between the ADC 2 values between the group of patients with RD and patients showing CR.
One-way ANOVA is used to examine the significance of the difference between the ADC values of two groups (CR and RD). The results indicateP < 0.05 suggesting that the null hypothesis Hb0 be rejected. This implies that there exists a significant difference between the posttreatment ADC values of patients with RD and patients showing CR.
The results of one-way ANOVA are summarized in Table S3.
Table S3.
ANOVA
| ADC 2 | |||||
|---|---|---|---|---|---|
| Sum of squares | df | Mean square | F | Sig. | |
| Between groups | 0.825 | 1 | 0.825 | 16.766 | 0.000 |
| Within groups | 4.820 | 98 | 0.049 | ||
| Total | 5.645 | 99 | |||
In order to test the influence of pretreatment ADC values (referred to as ADC 1) on our ANOVA results, we further tested the significance of difference between the posttreatment ADC values (ADC 2) of patients of group 1 (CR) and group 2 (RD), by introducing ADC 1 as covariate and performing a one-way ANCOVA. The results [Table S4] show that there are statistically significant (P < 0.05) differences in posttreatment ADC values between the groups (CR and RD) when adjusted for pretreatment ADC values (ADC 1, that is, the covariate).
Table S4.
Tests of between-subjects effects Dependent Variable: ADC 2
| Source | Type III sum of squares | df | Mean square | F | Sig. | Partial ETA squared |
|---|---|---|---|---|---|---|
| Corrected model | 1.010a | 2 | 0.505 | 10.574 | 0.000 | 0.179 |
| Intercept | 6.773 | 1 | 6.773 | 141.754 | 0.000 | 0.594 |
| ADC 1 | 0.186 | 1 | 0.186 | 3.887 | 0.052 | 0.039 |
| Group | 0.843 | 1 | 0.843 | 17.638 | 0.000 | 0.154 |
| Error | 4.635 | 97 | 0.048 | |||
| Total | 232.801 | 100 | ||||
| Corrected total | 5.645 | 99 |
aR2=0.179 (adjusted R2=0.162)
The mean values in the estimates table [Table S5] below represent the adjusted means (i.e., the original means adjusted for the covariate).
Table S5.
Estimates
| Dependent variable: ADC 2 | ||||
|---|---|---|---|---|
| Group | Mean | Std. error | 95% confidence interval | |
| Lower bound | Upper bound | |||
| 1 | 1.541a | 0.023 | 1.495 | 1.587 |
| 2 | 1.259a | 0.063 | 1.133 | 1.384 |
aCovariates appearing in the model are evaluated at the following values: ADC 1=0.93276
References
- 1.Ferlay J, Soerjomataram I, Ervik M, Dikshit R, Eser S, Mathers C, et al. GLOBOCAN 2012 v10, Cancer Incidence and Mortality Worldwide: IARC Cancer Base No 11. Lyon, France: 2013. [Last accessed on 2014 Sep 04]. Available from: http://globocaniarc fr . [Google Scholar]
- 2.Dhoot NM, Kumar V, Shinagare A, Kataki AC, Barmon D, Bhuyan U. Evaluation of carcinoma cervix using magnetic resonance imaging: Correlation with clinical FIGO staging and impact on management. J Med Imaging Radiat Oncol. 2012;56:58–65. doi: 10.1111/j.1754-9485.2011.02333.x. [DOI] [PubMed] [Google Scholar]
- 3.Kraljević Z, Visković K, Ledinsky M, Zadravec D, Grbavac I, Bilandzija M, et al. Primary uterine cervical cancer: Correlation of preoperative magnetic resonance imaging and clinical staging (FIGO) with histopathology findings. Coll Antropol. 2013;37:561–8. [PubMed] [Google Scholar]
- 4.Chen J, Zhang Y, Liang B, Yang Z. The utility of diffusion-weighted MR imaging in cervical cancer. Eur J Radiol. 2010;74:e101–6. doi: 10.1016/j.ejrad.2009.04.025. [DOI] [PubMed] [Google Scholar]
- 5.Harry VN, Semple SI, Gilbert FJ, Parkin DE. Diffusion weighted magnetic resonance imaging in the early detection of response to chemoradiation in cervical cancer. Gynecol Oncol. 2008;111:213–20. doi: 10.1016/j.ygyno.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 6.Schwarz JK, Siegel BA, Dehdashti F, Grigsby PW. Association of posttherapy positron emission tomography with tumor response and survival in cervical carcinoma. JAMA. 2007;298:2289–95. doi: 10.1001/jama.298.19.2289. [DOI] [PubMed] [Google Scholar]
- 7.Nakamura K, Joja I, Nagasaka T, Fukushima C, Kusumoto T, Seki N, et al. The mean apparent diffusion coefficient value (ADC mean) on primary cervical cancer is a predictive marker for disease recurrence. Gynecol Oncol. 2012;127:478–83. doi: 10.1016/j.ygyno.2012.07.123. [DOI] [PubMed] [Google Scholar]
- 8.Antunes D, Cunha TM. Recurrent cervical cancer: How can radiology be helpful. OMICS J Radiology. 2013;2:138. [Google Scholar]
- 9.Kinkel K, Ariche M, Tardivon AA, Spatz A, Castaigne D, Lhomme C, et al. Differentiation between recurrent tumor and benign conditions after treatment of gynecologic pelvic carcinoma: Value of dynamic contrast-enhanced subtraction MR imaging. Radiology. 1997;204:55–63. doi: 10.1148/radiology.204.1.9205223. [DOI] [PubMed] [Google Scholar]
- 10.Gu KW, Kim CK, Choi CH, Yoon YC, Park W. Prognostic value of ADC quantification for clinical outcome in uterine cervical cancer treated with concurrent chemoradiotherapy. Eur Radiol. 2019;29:6236–44. doi: 10.1007/s00330-019-06204-w. [DOI] [PubMed] [Google Scholar]
- 11.Padhani AR, Liu G, Koh DM, Chenevert TL, Thoeny HC, Takahara T, et al. Diffusion-weighted magnetic resonance imaging as a cancer biomarker: Consensus and recommendations. Neoplasia. 2009;11:102–25. doi: 10.1593/neo.81328. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Cui Y, Zhang XP, Sun YS, Tang L, Shen L. Apparent diffusion coefficient: Potential imaging biomarker for prediction and early detection of response to chemotherapy in hepatic metastases 1. Radiology. 2008;248:894–900. doi: 10.1148/radiol.2483071407. [DOI] [PubMed] [Google Scholar]
- 13.Liu Y, Bai R, Sun H, Liu H, Wang D. Diffusion-weighted magnetic resonance imaging of uterine cervical cancer. J Comput Assist Tomogr. 2009;33:858–62. doi: 10.1097/RCT.0b013e31819e93af. [DOI] [PubMed] [Google Scholar]
- 14.Harry VN, Semple SI, Gilbert FJ, Parkin DE. Diffusion-weighted magnetic resonance imaging in the early detection of response to chemoradiation in cervical cancer. Gynecol Oncol. 2008;111:213–20. doi: 10.1016/j.ygyno.2008.07.048. [DOI] [PubMed] [Google Scholar]
- 15.Vincens E, Balleyguier C, Rey A, Uzan C, Zareski E, Gouy S, et al. Accuracy of magnetic resonance imaging in predicting residual disease in patients treated for stage IB2/II cervical carcinoma with chemoradiation therapy: Correlation of radiologic findings with surgicopathologic results. Cancer. 2008;113:2158–65. doi: 10.1002/cncr.23817. [DOI] [PubMed] [Google Scholar]
- 16.McVeigh PZ, Syed AM, Milosevic M, Fyles A, Haider MA. Diffusion-weighted MRI in cervical cancer. Eur Radiol. 2008;18:1058–64. doi: 10.1007/s00330-007-0843-3. [DOI] [PubMed] [Google Scholar]
- 17.Sarabhai T, Tschischka A, Stebner V, Nensa F, Wetter A, Kimmig R, et al. Simultaneous multiparametric PET/MRI for the assessment of therapeutic response to chemo radiotherapy or concurrent chemoradiotherapy of cervical cancer patients: Preliminary results. Clin Imaging. 2018;49:163–8. doi: 10.1016/j.clinimag.2018.03.009. [DOI] [PubMed] [Google Scholar]


