Abstract
Primary lung lymphoma is one of the rarest forms of lymphoma and pulmonary space-occupying lesions. This case report represents the F-18 fluorodeoxyglucose positron emission tomography/computed tomography images of the most severe form of the primary pulmonary lymphoma reported in the literature.
Keywords: Fluorodeoxyglucose, lung lymphoma, positron emission tomography/computed tomography
Primary lung lymphoma is an extremely rare diagnosis presented in only 10% of the non-Hodgkin's lymphoma and 0.4% of all lymphomas.[1] The most effective imaging modality in the staging of lymphoma is accepted to be the F-18 fluorodeoxyglucose positron emission tomography/computed tomography (F-18 FDG PET/CT). The definition of primary lung lymphoma includes sole involvement of the lung parenchyma with or without mediastinal lymph nodes but necessarily not distant involvement.[2] Usually, mucosa-associated lymphoid tissue (MALT) type is associated with primary lung lymphoma, but diffuse large B-cell lymphoma subtype has also been reported.[3] A recent case report showed primary pulmonary lymphoma with F-18 FDG PET/magnetic resonance (MR) images involving single lobe.[4] This case presentation shows the most severe involvement of the lungs in the literature with F-18 FDG PET/CT images.
A 47-year-old man with the anamnesis of dyspnea attended the hospital. The patient had severe parenchymal disease with suspicious pathology result of lymphoma. The F-18 FDG PET/CT imaging was planned in the patient to determine the lymphoma and to find out another biopsy site. The PET/CT imaging was performed by administration of 8.8 mCi FDG via venous line in the state of fasting for 14 h and the blood glucose level of 108 mg/dl. The imaging was performed in craniocaudal direction in three-dimensional acquisition mode for 1 min per bed position with nondiagnostic CT scan for attenuation correction and oral contrast administration. The F-18 FDG PET/CT images demonstrated nothing but severe involvement of both lungs with significant FDG accumulation in the lesions (maximum standardized uptake value of 6.6). [Figure 1] and the pathology results verified the diagnosis of primary lung B cell MALT lymphoma [Figure 2].
Figure 1.
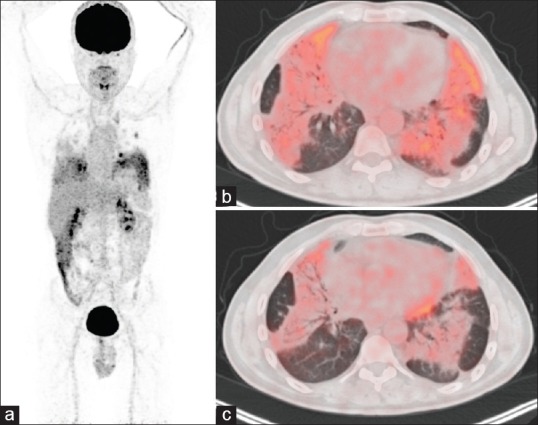
(a) Maximum intensity projection images of fluorodeoxyglucose positron emission tomography/computed tomography showing increased accumulation of activity in both lungs. (b) Cross-sectional transaxial images of both lungs in lung parenchyma window level demonstrating severe hypermetabolic lesions in both lungs. (c) The improvement of the lesions in both lungs are observed in the corresponding slice in the 2-month follow-up
Figure 2.
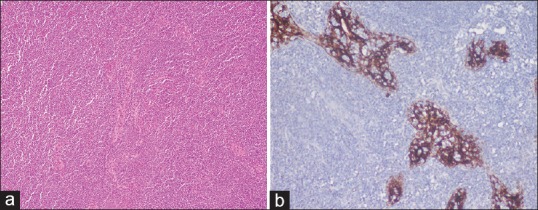
(a) Hematoxylin and eosin images of the lung parenchyma biopsy sample-bearing mucosa-associated lymphatic tissue-type lymphomatous infiltration of lung parenchyma verified by immunochemistry staining by CD20. (b) Contrary to expectations, the patient's positron emission tomography/computed tomography imaging could not find out any other biopsy site. The patient was considered to have primary lung lymphoma; however, thoracotomy and open biopsy of the lung parenchyma were planned and demonstrated the B-cell mucosa-associated lymphoid tissue lymphoma
The lung parenchyma findings are not specific for lymphoma, thus should be differentiated from malignant primary lung diseases. In case of nodal involvement, lymph node biopsy could be considered for the diagnosis of lymphoma. MALT type has indolent disease course with spontaneous regression; however, diffuse B-cell type is an aggressive form.[5] The primary lung lymphoma might be presented with single parenchyma opacity and focus with significant FDG uptake[6] or infiltrative parenchyma disease as in the presented case. To provide a diagnosis of primary lung lymphoma, the disease has to be limited to the thorax at the time of diagnosis and 3-month follow-up.[7,8] This case report shows atypical severe parenchyma involvement of MALT type B-cell lymphoma with any nodal involvement in the F-18 FDG PET/CT.
Declaration of patient consent
The authors certify that they have obtained all appropriate patient consent forms. In the form the patient(s) has/have given his/her/their consent for his/her/their images and other clinical information to be reported in the journal. The patients understand that their names and initials will not be published and due efforts will be made to conceal their identity, but anonymity cannot be guaranteed.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
References
- 1.Zinzani PL, Martelli M, Poletti V, Vitolo U, Gobbi PG, Chisesi T, et al. Practice guidelines for the management of extranodal non-Hodgkin's lymphomas of adult non-immunodeficient patients. Part I: Primary lung and mediastinal lymphomas. A project of the Italian Society of Hematology, the Italian Society of Experimental Hematology and the Italian Group for Bone Marrow Transplantation. Haematologica. 2008;93:1364–71. doi: 10.3324/haematol.12742. [DOI] [PubMed] [Google Scholar]
- 2.Cooksley N, Judge DJ, Brown J. Primary pulmonary Hodgkin's lymphoma and a review of the literature since 2006. BMJ Case Rep. 2014;2014 doi: 10.1136/bcr-2014-204020. pii: bcr2014204020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Wróbel T, Dzietczenia J, Prochorec-Sobieszek M, Mazur G, Piwkowski P. Primary pulmonary diffuse large B-cell lymphoma. Am J Hematol. 2012;87:107–8. doi: 10.1002/ajh.22116. [DOI] [PubMed] [Google Scholar]
- 4.Xu H, Xu K, Wang R, Liu X. Primary pulmonary diffuse large B-cell lymphoma on FDG PET/CT-MRI and DWI. Medicine (Baltimore) 2015;94:e1210. doi: 10.1097/MD.0000000000001210. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Zhu Z, Liu W, Mamlouk O, O'Donnell JE, Sen D, Avezbakiyev B. Primary pulmonary diffuse large B cell non-Hodgkin's lymphoma: A case report and literature review. Am J Case Rep. 2017;18:286–90. doi: 10.12659/AJCR.901528. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yoshino N, Hirata T, Takeuchi C, Usuda J, Hosone M. A case of primary pulmonary diffuse large B-cell lymphoma diagnosed by transbronchial biopsy. Ann Thorac Cardiovasc Surg. 2015;21:396–8. doi: 10.5761/atcs.cr.14-00298. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Graham BB, Mathisen DJ, Mark EJ, Takvorian RW. Primary pulmonary lymphoma. Ann Thorac Surg. 2005;80:1248–53. doi: 10.1016/j.athoracsur.2005.04.014. [DOI] [PubMed] [Google Scholar]
- 8.Vanden Eynden F, Fadel E, de Perrot M, de Montpreville V, Mussot S, Dartevelle P. Role of surgery in the treatment of primary pulmonary B-cell lymphoma. Ann Thorac Surg. 2007;83:236–40. doi: 10.1016/j.athoracsur.2006.08.026. [DOI] [PubMed] [Google Scholar]


