Abstract
Aim of the Registry
The aim of the Danish Multidisciplinary Hip Fracture Registry (DMHFR) is to collect data on processes of treatment, nursing care and rehabilitation as well as outcomes for patients with hip fracture in Denmark, and thereby monitor and improve the quality.
Study Population
Hip fracture patients at age 65 or older that have undergone surgery with arthroplasty or internal fixation since 2004.
Main Variables
DMHFR collects quality indicators and descriptive variables. Quality indicators include eight process performance measures within treatment, nursing care and rehabilitation, reflecting recommendations from the national clinical guideline for hip fracture patients, and three outcome measures including survival within 30-days, unplanned acute readmission within 30 days and reoperation within 2 years. Descriptive variables include a number of patient- and surgery-related characteristics. All data are collected prospectively.
Results
By the end of 2018, the DMHFR included 86,438 hip fracture patients. Since 2006, all hospital departments in Denmark, treating patients with hip fracture, have reported improvement in quality of care and improvement in survival, and reoperation over time as well as high completeness of variables registration.
Conclusion
The DMHFR is a well-established nationwide clinical registry, which plays a key role for monitoring and improving hip fracture care in Denmark. The registry can further be linked to a range of other nationwide registries in order to answer a number of relevant clinical research questions.
Keywords: hip fracture, quality indicators, registry, mortality, reoperation, readmission
Introduction
The number of patients hospitalized due to hip fracture has been reported to be 620,000 in the European Union in 2010 and 210,000 per year between 2008 and 2011 in the United States.1,2 It is the dominant cause of trauma-related mortality in people above 65 years, and among the survivors, 50% never reached their previous functional level.3–6 Moreover, hip fracture is related to considerable healthcare costs.7–9 Previous research has indicated variation in outcome after hip fracture and only a slight improvement in survival over time.10–12 Western healthcare systems have therefore developed clinical guidelines for hip fracture care and countries including Sweden, Norway, Finland, Denmark and the United Kingdom have initiated continuous monitoring of the quality of care after hip fracture.13,14
The Danish Multidisciplinary Hip Fracture Registry (DMHFR) was initiated in 2003 as part of a national quality improvement project called the Danish National Indicator Project.15 The aim of the DMHFR is to monitor and support implementation of evidence-based clinical guidelines for hip fracture care and ultimately improve the quality and outcome of hip fracture patients. The registry has a multidisciplinary steering committee appointed by the Danish regions, the Danish Orthopedic Society, the Danish Geriatric Society, the Danish Nurses Organization and the Danish Society for Physiotherapists.16 The steering committee chose quality of care indicators, including process performance measures and outcome, as well as descriptive prognostic variables, which reflect current evidence-based approaches within multidisciplinary hip fracture care and their feasibility in clinical practice. The DMHFR is part of the umbrella organization Danish Clinical Registries, and the results are publically available in an annual report in aggregated form.16
Aim
The present paper aims to describe the organization and content of the DMHFR, to present results regarding demographics and quality indicators during the period 2006–2018 and to illustrate the potential of the DMHFR for clinical epidemiological research.
Materials and Methods
Setting
Denmark is a country with 5.7 million inhabitants with free access to medical care and a longstanding tradition for health-care registries.17 All patients with hip fracture are admitted to the nearest public hospital treating acute patients. All inhabitants have a unique civil registration number, which is used in all healthcare contacts and allows unambiguous linkage between the healthcare registries.18
Data Collection Procedures
Reporting to the DMHFR is mandatory by law for all hospitals from 2006.19 During the period from 2006 to 2018 all hospitals treating hip fracture patients were reporting to the registry. Data are prospectively collected on an individual-level by healthcare professionals involved in treatment of hip fracture patients from the time of hospital admission to discharge, covering different aspects of the clinical pathway. Detailed data definitions are developed prior to data collection. Fulfillment of the process performance measures are registered by the staff members prospectively as part of the clinical routine and are reported monthly to the registry. From 2004 to March 2010 the registry was a web-based standalone database, as data were collected using an independent web-based interface. From March 2010 and forward, the registry uses routine collected data retrieved directly from the Danish National Patient Registry to avoid double registration by clinicians.20
Study Population
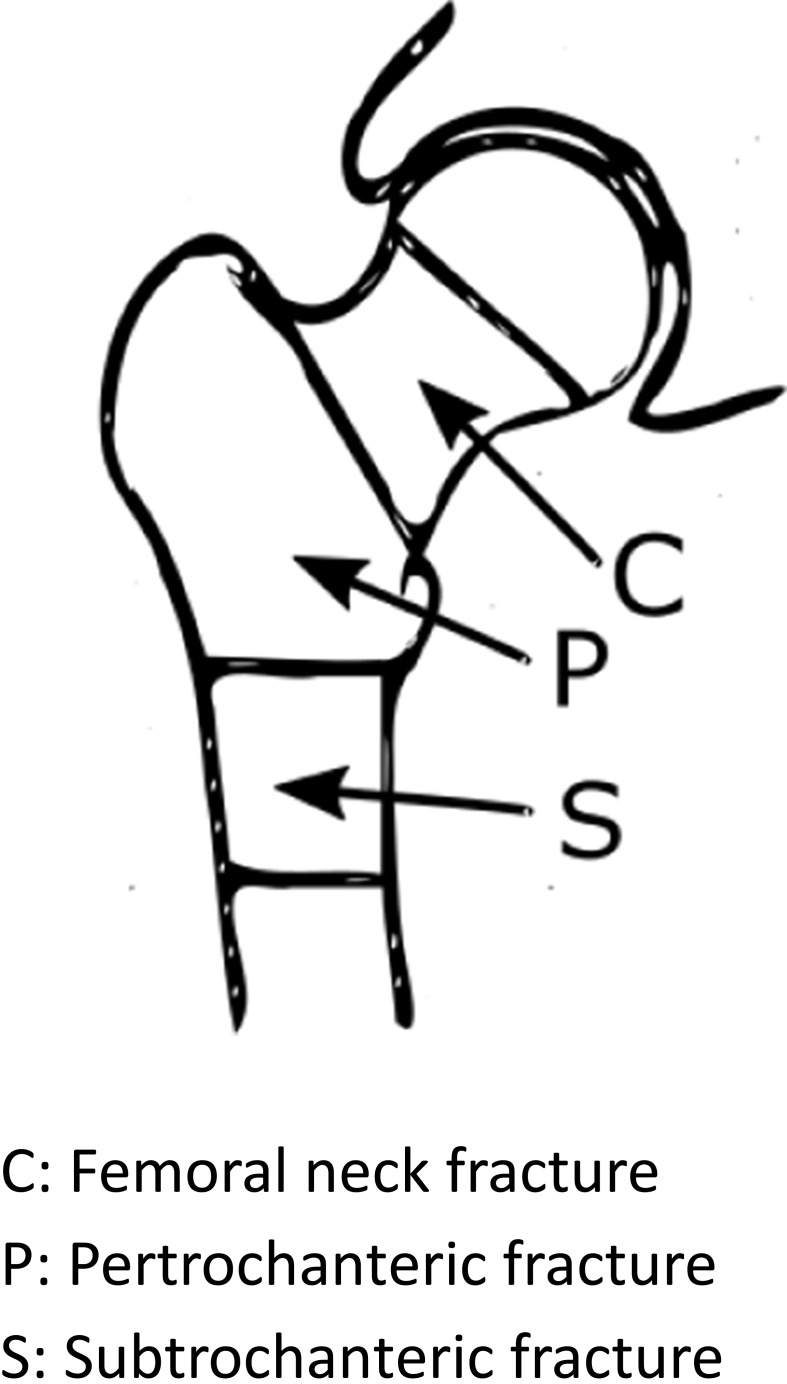
The DMHFR includes patients’ age ≥65 admitted acutely with a femoral neck, pertrochanteric (intertrochanterica femoris or trochanterica femoris) or subtrochanteric fracture (Figure 1) and treated surgically with osteosynthesis or total/hemi arthroplasty.
Figure 1.
Types of collum femoris fractures included in the multidisciplinary hip fracture registry.
Main Variables
Quality Indicators
A documentary report, which reflects current evidence within multidisciplinary hip fracture care, is developed. On the basis of this evidence-based approach as well as feasibility in clinical practice, quality of care indicators are developed. The quality indicators in the DMHFR include process performance measures and outcome measures. Eight process performance measures are currently available and include timing of preoperative optimization, surgery delay (24 and 36 hours), mobilization within 24 hours, assessment of nutrition status, basic mobility score pre- and postoperative, rehabilitation program, osteoporosis- and fall prophylaxis. The process performance measures reflect key recommendations for healthcare processes, which are expected to be associated with patient outcome. The staff members classify the patient as eligible or non-eligible for the process performance measures according to detailed data definitions. Subsequently, the staff members register fulfillment or non-fulfillment of the measure. Missing registration of fulfillment would be coded as a non-fulfillment of the process performance measure.
Currently, three outcome measures are available: Survival within 30 days, readmission within 30 days after discharge and reoperation within two years. Due to the individual-level record linkage to other public registries and the civil registry number in Denmark, complete follow-up for every patient is possible for the outcome measures. Information on survival is obtained from the Civil Registration System, which has daily updated electronic records of all changes in vital status for the entire Danish population since 1968.18 Readmission is defined as an acute first time readmission to any hospital 24 hours after discharge from hip fracture with a length of stay of minimum 24 hours. Reoperation is defined in four different ways depending on fracture type and surgery type. Information on readmission and reoperation is obtained from the Danish National Patient Registry, which is a nationwide administrative registry that covers all admissions and discharges from Danish somatic hospitals since 1977. Since 1994, up to 20 diagnoses for every discharge are coded according to the Danish version of the International Classification of Diseases tenth edition.20
The core of the quality of care indicators has been quite consistent in the first ten years. However, demands for fulfillment of some process performance measures have increased over time and data definitions were adjusted. For instance, a timestamp for mobilization within 24 hours was implemented in 2015. Before 2015, the clinicians reported whether the patient was mobilized within 24 hours with the answer yes or no. After 2015, clinicians have reported the exact time for first mobilization. Likewise, in 2013, fulfillment of the measure basic mobility assessment presupposes that the CAS score value also was reported. Moreover, new quality indicators have been added by the steering committee regularly. Detailed specifications for the individual indicator calculation are publicly available through the Danish Clinical Registry’s website.16 A description of the measures used in the registry is presented in Table 1.
Table 1.
The Quality Indicators in the Multidisciplinary Hip Fracture Registry Through the Years
| Indicator Area | Indicator | 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Process Performance Measures | Pain assessment | Daily systematic pain assessment using a visual analog scale or a numeric rating scale at rest and during mobilization | + | + | + | + | + | + | + | + | + | ||||
| Mobilization within 24 hours | Being mobilized within 24 hours postoperatively, defined as assisting the patient from bed rest to walking or rest in a chair | + | + | + | + | + | +a | + | + | + | |||||
| Assessment of nutrition risk | Assessment of patients BMI and nutritional risk within two days after admission. | + | + | + | + | + | + | + | + | ||||||
| Osteoporotic medication | Evaluation of need of anti-osteoporotic medications, which includes continued anti-osteoporosis medication, no indication for treatment due to cancer or psychiatric condition or referring to DEXA scan | + | + | + | + | + | + | + | + | + | |||||
| Fall prevention | Initiation of treatment to prevent future fall accidents, including a fall risk assessment to account for co-existing medical conditions, medication, functional disability, symptoms from the central nervous system, musculoskeletal system and cardiopulmonary status | + | + | + | + | + | + | + | + | + | |||||
| Prevention of osteoporotic fractures | Initiation of treatment includes ordination of any anti-osteoporotic medications or calcium and d-vitamin or hip protectors | + | + | + | + | ||||||||||
| Post discharge rehabilitation program | Post discharge rehabilitation program including assessment of activities of daily living (ADL) with a validated test before the fracture and again before discharge | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Assessment of functional level prior to admission | Basic mobility assessment using a validated test such as Cumulated Ambulation Score (CAS), Barthel 20, Functional Recovery score or New Mobility score. From 2013, only CAS is measured at admission. | + | + | + | + | +a | + | + | +a | + | + | + | + | + | |
| Assessment of functional level at discharge | Basic mobility assessment using a validated test such as Cumulated Ambulation Score (CAS), Barthel 20, Functional Recovery score or New Mobility score. From 2013, only CAS is measured prior to discharge | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Surgical delay | Patient had surgery within 24 hours after admission to hospital (from 2016, admission time was changed to arrival time) | + | + | + | + | ||||||||||
| Patient had surgery within 36 hours after admission to hospital (from 2016, admission time was changed to arrival time) | + | + | + | + | |||||||||||
| Preoperative optimization | Assessment by a medical specialist intending to do a preoperative optimization plan within four hours after arrival to the hospital. | + | + | + | |||||||||||
| Outcome Measures | 30-day survival | Survival within 30 days after surgery date | + | + | + | + | + | + | + | + | + | + | + | + | + |
| Reoperation within two years after osteosynthesis | Reoperation within two years among patients, who have had a medial femoral fracture treated with osteosynthesis regardless of fracture displacement | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Reoperation within two years among patients, who have had a medial undisplaced femoral fracture treated with osteosynthesis. | + | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Reoperation within two years among patients, who have had a medial displaced femoral fracture treated with osteosynthesis regardless of fracture displacement | + | + | + | + | + | + | + | + | + | + | + | + | + | ||
| Reoperation within two years among patients, who have had a pertrochanter or subtrochanter femoral fracture treated with osteosynthesis. | |||||||||||||||
| Reoperation within two years after alloplastic | Reoperation within two years among patients, who have had an alloplastic regardless of fracture type | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Reoperation within two years due to infection | Reoperation within two years due to deep infection | + | + | + | + | + | + | + | + | + | + | + | + | + | |
| Acute readmission within 30-days after discharge | Acute readmission to any Danish hospital regardless of cause within 30 days after discharge with the hip fracture diagnosis | + | + | + |
Note: aChange in data definitions.
Local and regional audits on quality indicators are carried out every third month. Further, the steering committee performs an annually structured audit process and publishes an annual report followed by comments and recommendations from the audits on how to improve quality of care.
Descriptive Variables
The DMHFR has information on a number of patient- and surgery-related variables, which, based on the current evidence, appear to be well-established prognostic factors. Patient-related variables included admission age, sex, Body Mass Index (BMI) and residence. In the period from 2005 to 2010 information on alcohol intake and smoking were collected. The surgery-related variables included type of fracture, fracture displacement, and type of surgery (Table 2). In the period from 2005 to 2010, information on the American Society of Anesthesiologists’ (ASA) classification score was collected. From 2010 and onward, the ASA score was replaced with the Charlson Comorbidity Index (CCI). The CCI is a method of categorizing comorbidities of patients based on ICD diagnosis codes from the Danish National Patient Registry.21 Surgical delay was included in the DMHFR as a prognostic factor in the period 2006 to 2014 and as a process performance measure since 2015.
Table 2.
Patient Characteristics of the Hip Fracture Population from 2006 to 2018
| 2006 | 2007 | 2008 | 2009 | 2010 | 2011 | 2012 | 2013 | 2014 | 2015 | 2016 | 2017 | 2018 | |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of Admissions | 6456 | 6566 | 7423 | 7155 | 5143 | 7158 | 6801 | 6904 | 6611 | 6789 | 6679 | 6502 | 6374 |
| Age, median year (Q1-Q3) | 83 | 83 | 84 | 84 | 83 (77–89) | 83(77–89) | 84(78–89) | 84(77–89) | 84(77–89) | 83(77–89) | 84(77–89) | 83(77–89) | 83(76–89) |
| Gender: | |||||||||||||
| Men | 1686 | 1784 | 1998 | 1939 | 1413 | 2038 | 1970 | 1988 | 1867 | 2021 | 2060 | 2035 | 2045 |
| Women | 4770 | 4782 | 5425 | 5216 | 3730 | 5120 | 4831 | 4916 | 4744 | 4768 | 4619 | 4467 | 4329 |
| Residence (2005–2009): | |||||||||||||
| Living together with another adult | 1673 | 1686 | 1969 | 1914 | |||||||||
| Living alone in one’s own home | 3244 | 3344 | 3946 | 3802 | |||||||||
| Other including living in a nursing home or other institution | 1060 | 1216 | 1256 | 1158 | |||||||||
| Missing | 479 | 320 | 252 | 281 | |||||||||
| Residence (2010→) | |||||||||||||
| Own home | 2871 | 4791 | 4540 | 4717 | 4457 | 4599 | 4609 | 4400 | 4501 | ||||
| Own home affiliated with an institution | 378 | 424 | 385 | 405 | 360 | 378 | 391 | 257 | 217 | ||||
| Institution | 871 | 1311 | 1227 | 1357 | 1182 | 1080 | 1147 | 1112 | 1136 | ||||
| Missing | 1023 | 632 | 649 | 425 | 612 | 732 | 532 | 733 | 520 | ||||
| ASA: (2006–2009) | |||||||||||||
| 0 | 602 | 543 | 570 | 546 | |||||||||
| 1 | 2977 | 3189 | 3538 | 3582 | |||||||||
| 2 | 2091 | 2207 | 2575 | 2383 | |||||||||
| 4 | 338 | 357 | 336 | 311 | |||||||||
| 5 | 10 | 12 | 12 | 9 | |||||||||
| Missing | 438 | 258 | 392 | 324 | |||||||||
| CCI (2010→): | |||||||||||||
| None 0 point | 2023 | 2800 | 2544 | 2399 | 2512 | 2420 | 2394 | 2307 | |||||
| Mild 1 point | 1201 | 1723 | 1718 | 1591 | 1510 | 1554 | 1497 | 1441 | |||||
| Moderate 2 points | 903 | 1266 | 1192 | 1154 | 1229 | 1199 | 1182 | 1151 | |||||
| Severe ≥ 3 points | 1016 | 1369 | 1450 | 1467 | 1538 | 1506 | 1429 | 1475 | |||||
| BMI (2010→): | |||||||||||||
| < 19: Underweight | 586 | 961 | 958 | 1030 | 943 | 881 | 1426 | 795 | 829 | ||||
| 20–25: Normal | 1770 | 2919 | 2850 | 2916 | 2811 | 2757 | 2644 | 2428 | 2327 | ||||
| 26–29: Overweight | 871 | 1540 | 1383 | 1455 | 1410 | 1484 | 1476 | 1394 | 1334 | ||||
| >30: Obese | 323 | 412 | 375 | 429 | 399 | 402 | 478 | 461 | 430 | ||||
| Missing | 1593 | 1326 | 1235 | 1074 | 1048 | 1055 | 655 | 1424 | 1454 | ||||
| Fracture Displacement | |||||||||||||
| Displaced | 4707 | 5375 | 6184 | 5880 | 3142 | 5314 | 4985 | 5202 | 4845 | 5081 | 4811 | 4266 | 3792 |
| Undisplaced | 932 | 1149 | 1209 | 1243 | 549 | 835 | 787 | 828 | 744 | 680 | 657 | 542 | 464 |
| Unspecified | 817 | 42 | 30 | 32 | 1452 | 1009 | 1029 | 874 | 1022 | 1028 | 1211 | 1694 | 2118 |
| Type of Fracture | |||||||||||||
| Medial femoral neck | 3253 | 3334 | 3786 | 3597 | 2662 | 3671 | 3619 | 3815 | 3630 | 3781 | 3691 | 3498 | 3371 |
| Pertrochanteric | 2628 | 2721 | 3075 | 2966 | 2093 | 2949 | 2704 | 2593 | 2714 | 2526 | 2502 | 2495 | 2527 |
| Subtrochanteric | 410 | 484 | 551 | 577 | 388 | 538 | 478 | 496 | 526 | 482 | 486 | 509 | 476 |
| Missing | 165 | 27 | 11 | 15 | |||||||||
| Type of Surgery | |||||||||||||
| Osteosynthesis | 4597 | 4734 | 5309 | 5018 | 3538 | 4877 | 4435 | 4464 | 4336 | 4365 | 4325 | 4176 | 4082 |
| Hemi/total arthroplasty | 1572 | 1611 | 1945 | 1964 | 1605 | 2281 | 2366 | 2440 | 2275 | 2424 | 2354 | 2326 | 2292 |
| Missing | 287 | 221 | 169 | 173 | |||||||||
| Alcohol Intake (2006–2009) | |||||||||||||
| ≤ 14/21 per week for women/men | 4405 | 4801 | 5759 | 5307 | |||||||||
| >14/21 units per week for women/men | 188 | 230 | 272 | 230 | |||||||||
| Missing | 1863 | 1535 | 1392 | 1618 | |||||||||
| Smoking Habits (2006–2009) | |||||||||||||
| Current | 1366 | 1412 | 1657 | 1532 | |||||||||
| Former | 1001 | 1151 | 1422 | 1401 | |||||||||
| Never | 2180 | 2431 | 2837 | 2516 | |||||||||
| Missing | 1909 | 1572 | 1507 | 1706 | |||||||||
| Time to Surgery (hours)a | |||||||||||||
| <24 hours | 3293 | 3405 | 3855 | 3901 | 2858 | 3899 | 4299 | 4392 | 4377 | ||||
| 24-48 hours | 2197 | 2104 | 2502 | 2286 | 1584 | 2361 | 1876 | 1890 | 1827 | ||||
| > 48 hours | 759 | 781 | 858 | 714 | 693 | 893 | 626 | 617 | 402 | ||||
| Missing | 207 | 276 | 208 | 254 | 8 | 5 | 5 | 5 | |||||
| Region | |||||||||||||
| North Denmark | 925 | 872 | 852 | 606 | 913 | 844 | 765 | 783 | 769 | 800 | 804 | 702 | |
| Central Denmark | 1607 | 1675 | 1628 | 1097 | 1513 | 1455 | 1509 | 1421 | 1454 | 1449 | 1419 | 1428 | |
| Southern Denmark | 1844 | 1818 | 1757 | 1196 | 1714 | 1566 | 1566 | 1607 | 1556 | 1559 | 1566 | 1670 | |
| Capital region | 1343 | 1780 | 1791 | 1434 | 1949 | 1898 | 1917 | 1777 | 1871 | 1770 | 1618 | 1495 | |
| Zeeland region | 1079 | 1142 | 1127 | 810 | 1069 | 1038 | 1147 | 1023 | 1139 | 1101 | 1095 | 1079 |
Note: aFrom 2015 and onward time to surgery is collected as a process performance measure.
Abbreviations: BMI, Body Mass Index; ASA, American Society of Anesthesiologists’ classification score; CCI, Charlson Comorbidity Index.
Results
Patient Characteristics
During the period 2006–2018, the DMHFR included 87,803 hip fracture patients. The number of patients varied slightly during the study period, but the average was 6,800 patients (Table 2). The majority of hip fracture patients are women with a median age of 84 years, living alone. The most frequent fracture type is a femoral neck fracture and the most frequent surgery type is internal fixation. The proportion of hip fracture patients with comorbidity has increased over time (Table 2).
Quality Indicators
Process Performance Measures
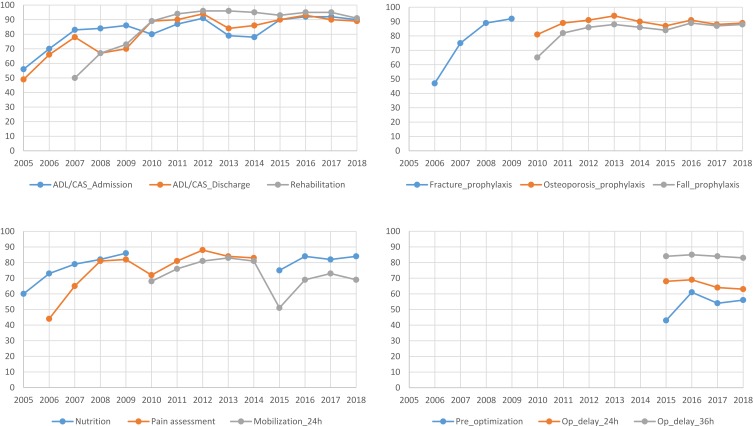
For the process performance measures, improvement over the years has been observed for most of the measures even though the demands for fulfillment of the process performance measures have increased over the period (Figure 2). An exception is the process performance measures implemented in 2015, including preoperative optimization and surgery within 24 and 36 hours respectively, where the fulfillment has not improved over the three years. A decrease in fulfillment of some of the process performance measures such as mobilization within 24 hours in 2015 and basic mobility assessment in 2013 may be related to change in data definitions (Figure 2).
Figure 2.
Proportion of patients in percent that have fulfilled the individual process performance measures over time.
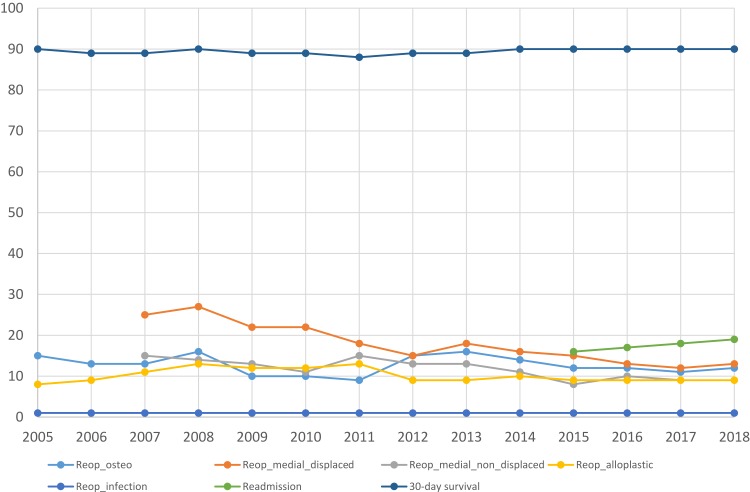
Outcome Measures 30-Day Mortality, Readmission and Reoperation
The overall 30-day survival varied from 90% to 88% during 2006–2018. The proportion of patients that were re-operated within two years has decreased over the study period, from 27% to 13% among patients with a displaced medial femoral neck fracture, and from 15% to 9% among patients with un-displaced medial fracture (Figure 3). Reoperations among patients treated with an arthroplasty were highest in the period from 2008 to 2011 with around 13%, and have decreased to 9% subsequently. Almost 1820% of patients were readmitted within 30 days during 2015 to 2018.
Figure 3.
Proportion of patients with 30-day survival and readmission and reoperation within two years over time.
Examples of Research
The DMHFR data are accessible for research after application to the Danish Clinical Registries.16 Published papers are based on the DMHFR data linked to other Danish health registries, including the Danish National Patient Registry, the Civil Registration System, the Danish Transfusion Database, the Danish Prescription Database, the Laboratory Information System, and the Integrated Database for Labour Marked Research. The studies have focused on variation in the outcome measures among patient types and hospitals.22–24 An association between fulfillment of the process performance measures and better survival and lower readmission rate has been found25–28 as well as an association between orthogeriatric specialization or patient volume and outcome.29–31 In addition, associations between transfusion practice and outcome,32,33 association between surgery delay and post-operative complications,34,35 associations between some commonly used medication preoperatively, including antidepressants, anticoagulants and anti-inflammatory drugs and post-operative complications36–40 have been observed. Moreover, studies have found that about 15% of hip fracture patients develop an acute kidney injury within 5 days of surgery41,42 and about 15% of patients sustain post-operative infections within 30 days of surgery,43,44 complications which are strongly associated with 30 days mortality. Besides, hip fracture patients were at increased excess risk of venous thromboembolism, myocardial infarction and stroke up to one year following fracture.45,46
Discussion
The DMHFR is a nationwide registry established in 2003 with the aim of monitoring and improving hip fracture treatment and care in Denmark. The hip fracture population in Denmark is characterized by a median age of 84 years and a high completeness of reporting. The quality of treatment and care reflected by receiving guideline recommended recommendations has increased over the years. The 30-day survival has improved from 88% to 90% in the period. The proportion of reoperations has decreased especially among patients with medial femoral neck fracture. In contrast, the risk for acute readmission has increased from 16% to 20% in the last three years.
Comparison with Other Hip Fracture Registries
Continuous monitoring of the quality of healthcare has been implemented in many European countries14 including Finland (PERFormance, Effectiveness and Cost of Treatment episodes),47 Sweden (Rikshöft),48 the United Kingdom (UK) (the National Hip Fracture Database),13,49 Scotland (the Scottish Hip Fracture Audit),50 Italy (Regional Outcome Evaluation Program in the Lazio region51 and Gruppo Italiano di Ortogeriatria),52 Norway (The Norwegian Hip Fracture Registry),53 Spain (National Hip Fracture Registry),54 Ireland (Irish Hip Fracture database),55 Nederlands (Dutch National Hip Fracture Audit),56 Germany (Alterstrauma register),57 and Denmark (DMHFR). However, the majority of these registries47,50,51,53–55 mainly monitor outcome performance measures, eg, mortality and readmissions at the hospital level, and lack continuous monitoring of process performance measures. Exceptions are the DMHFR, Rikshöft48 and the National Hip Fracture Database in the UK,13,49 which contain valuable information on process performance measures according to clinical guideline recommendations. The measures monitored in the National Hip Fracture Database in the UK are comparable to the process performance measures as they monitor mobilization on the first postoperative day, bone-protection medication and geriatric assessment. The fulfillment of the process performance measures is generally higher in the UK compared to Denmark, eg, 69% were mobilized on the first operative day in Denmark whereas 79% were mobilized in the UK. Likewise is the survival lower in Denmark compared to the UK and Sweden, as they report an overall 30-day mortality rate below 8% compared to 10% in Denmark.58,59 The lower mortality may be explained by different inclusion criteria in the hip fracture registries, eg, different inclusion ages, which may impact the risk of mortality. For instance, the Scottish Hip Fracture Audit, the Swedish Rikshöft registry and the Finish PERFECT registry include hip fracture patients from 50 years, whereas the Danish Multidisciplinary hip fracture registry includes patients from 65 years.
Perspective
The efforts are on-going to improve the fulfillment of the process performance measures and thereby improve the hip fracture patients´ survival. The completeness of registered variables for each patient is high, however an in-depth validation of the data in the DMHFR with focus on completeness and positive predictive value of the registered data needs to be done. The length of hospital stay has decreased, which includes earlier discharge to care in the community settings or at home with support from home care or mobile rehabilitation units. The hip fracture registries therefore need data from the community setting including primary healthcare services to improve our knowledge on the full clinical pathway of hip fracture patients and it impact on the patient outcome.
Administrative Issues and Funding
The clinicians reporting to the registry have no economic incentives, but there is an increasing interest from politicians, hospital boards of directors and patient organizations regarding fulfillment of the quality indicators. DMHFR is funded by the Danish Regions and receives epidemiological, statistical and administrative support from the Danish Clinical Registries (RKKP), which has a budget of 9.9 million USD to operate 80 databases in Denmark. DMHFR receives 16,000 USD yearly for holding audits, multidisciplinary seminars and revising data definitions. The DMHFR is approved as a national clinical quality database by the National Board of Health and the Data Protection Agency. Permission to access the data from the DMHFR has been granted by the Data Protection Agency and the steering Committee following an application to the Data Protection Agency and RKKP.
Conclusion
The DMHFR plays an important key role in monitoring and improving hip fracture care in Denmark due to prospectively collected high-validity data. Furthermore, the DMHFR has been linked to a wide range of other national registries in order to answer a number of relevant clinical questions regarding the treatment and outcome of hip fracture patients. Thus, the DMHFR is a valuable tool for both quality improvement and epidemiological research.
Acknowledgments
We thank the staff at the hospital departments involved in treatment of patients with hip fracture for their continuous effort and contribution in acquiring the data in the DMHFR. Also, we thank the steering Committee of the DMHFR for their ongoing effort with development, interpretation and evaluation of quality indicators and thereby quality improvement.
Funding Statement
This work was supported by the Health Research Fund of Central Denmark Region (Pia Kjær Kristensen). The financial sponsors did not play a role in the design, execution, analysis, interpretation of data, or writing of the study.
Ethics
The study was approved by the Danish Data Protection Agency (journal number 2012-41-1274) and carried out in accordance with the principle of the Declaration of Helsinki. The requirement for consent was waived as registry-based studies do not require formal ethical approval according to the Danish law. Patient data was kept confidential.
Disclosure
Pia Kristensen reports grants from Health Research Fund of Central Denmark Region, during the conduct of the study. The authors report no other conflicts of interest in this work.
References
- 1.Kanis JA, Oden A, McCloskey EV, et al. A systematic review of hip fracture incidence and probability of fracture worldwide. Osteoporos Int. 2012;23(9):2239–2256. doi: 10.1007/s00198-012-1964-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Singer A, Exuzides A, Spangler L, et al. Burden of illness for osteoporotic fractures compared with other serious diseases among postmenopausal women in the United States. Mayo Clin Proc. 2015;90(1):53–62. doi: 10.1016/j.mayocp.2014.09.011 [DOI] [PubMed] [Google Scholar]
- 3.Roche JJ, Wenn RT, Sahota O, Moran CG. Effect of comorbidities and postoperative complications on mortality after hip fracture in elderly people: prospective observational cohort study. BMJ. 2005;331(7529):1374. doi: 10.1136/bmj.38643.663843.55 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002;359(9319):1761–1767. doi: 10.1016/S0140-6736(02)08657-9 [DOI] [PubMed] [Google Scholar]
- 5.Cauley JA. Public health impact of osteoporosis. J Gerontol a Biol Sci Med Sci. 2013;68(10):1243–1251. doi: 10.1093/gerona/glt093 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Katsoulis M, Benetou V, Karapetyan T, et al. Excess mortality after hip fracture in elderly persons from Europe and the USA: the CHANCES project. J Intern Med. 2017;281(3):300–310. doi: 10.1111/joim.12586 [DOI] [PubMed] [Google Scholar]
- 7.Brauer CA, Coca-Perraillon M, Cutler DM, Rosen AB. Incidence and mortality of hip fractures in the United States. JAMA. 2009;302(14):1573–1579. doi: 10.1001/jama.2009.1462 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Tosteson AN, Burge RT, Marshall DA, Lindsay R. Therapies for treatment of osteoporosis in US women: cost-effectiveness and budget impact considerations. Am J Manag Care. 2008;14(9):605–615. [PubMed] [Google Scholar]
- 9.Burge R, Dawson-Hughes B, Solomon DH, Wong JB, King A, Tosteson A. Incidence and economic burden of osteoporosis-related fractures in the United States, 2005-2025. J Bone Miner Res. 2007;22(3):465–475. doi: 10.1359/jbmr.061113 [DOI] [PubMed] [Google Scholar]
- 10.Cauley JA, Chalhoub D, Kassem AM, Fuleihan G-H. Geographic and ethnic disparities in osteoporotic fractures. Nat Rev Endocrinol. 2014;10(6):338–351. [DOI] [PubMed] [Google Scholar]
- 11.Fisher ES, Wennberg DE, Stukel TA, Gottlieb DJ, Lucas FL, Pinder EL. The implications of regional variations in medicare spending. Part 2: health outcomes and satisfaction with care. Ann Intern Med. 2003;138(4):288–298. doi: 10.7326/0003-4819-138-4-200302180-00007 [DOI] [PubMed] [Google Scholar]
- 12.Thygesen LC, Christiansen T, Garcia-Armesto S et al. Potentially avoidable hospitalizations in five European countries in 2009 and time trends from 2002 to 2009 based on administrative data. European Journal of Public Health 2015;25(suppl_1):35–43. [DOI] [PubMed] [Google Scholar]
- 13.Patel NK, Sarraf KM, Joseph S, Lee C, Middleton FR. Implementing the national hip fracture database: an audit of care. Injury. 2013;44(12):1934–1939. doi: 10.1016/j.injury.2013.04.012 [DOI] [PubMed] [Google Scholar]
- 14.Saez-Lopez P, Branas F, Sanchez-Hernandez N, Alonso-Garcia N, Gonzalez-Montalvo JI. Hip fracture registries: utility, description, and comparison. Osteoporos Int. 2017;28(4):1157–1166. doi: 10.1007/s00198-016-3834-x [DOI] [PubMed] [Google Scholar]
- 15.Mainz J, Krog BR, Bjornshave B, Bartels P. Nationwide continuous quality improvement using clinical indicators: the Danish National Indicator Project. Int J Qual Health Care. 2004;16(Suppl 1):i45–I50. doi: 10.1093/intqhc/mzh031 [DOI] [PubMed] [Google Scholar]
- 16.Regionernes Kliniske Kvalitets Program. De kliniske kvalitetsdatabaser. 2015. Available from: http://www.rkkp.dk/. Accessed January10, 2019.
- 17.Schmidt M, Schmidt SAJ, Adelborg K, et al. The Danish health care system and epidemiological research: from health care contacts to database records. Clin Epidemiol. 2019;11:563. doi: 10.2147/CLEP.S179083 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Schmidt M, Pedersen L, Sorensen HT. The Danish Civil Registration System as a tool in epidemiology. Eur J Epidemiol. 2014;29(8):541–549. doi: 10.1007/s10654-014-9930-3 [DOI] [PubMed] [Google Scholar]
- 19.Ministry D. The Danish health act legislation number 546 from 24 June 2005. Danish legislation number 546. Vol 546. [Google Scholar]
- 20.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sorensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449–490. doi: 10.2147/CLEP.S91125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Kirkland LL, Kashiwagi DT, Burton MC, Cha S, Varkey P. The Charlson Comorbidity Index Score as a predictor of 30-day mortality after hip fracture surgery. Am J Med Qual. 2011;26(6):461–467. doi: 10.1177/1062860611402188 [DOI] [PubMed] [Google Scholar]
- 22.Kristensen PK, Merlo J, Ghith N, Leckie G, Johnsen SP. Hospital differences in mortality rates after hip fracture surgery in Denmark. Clin Epidemiol. 2019;11:605. doi: 10.2147/CLEP.S213898 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Kristensen PK, Johnsen SP, Mor A, Thillemann TM, Pedersen AB. Is the higher mortality among men with hip fracture explained by sex-related differences in quality of in-hospital care? A population-based cohort study. Age Ageing. 2017;46(2):193–199. doi: 10.1093/ageing/afw225 [DOI] [PubMed] [Google Scholar]
- 24.Kristensen PK, Thillemann TM, Pedersen AB, Soballe K, Johnsen SP. Socioeconomic inequality in clinical outcome among hip fracture patients: a nationwide cohort study. Osteoporos Int. 2017;28(4):1233–1243. doi: 10.1007/s00198-016-3853-7 [DOI] [PubMed] [Google Scholar]
- 25.Kristensen PK, Thillemann TM, Soballe K, Johnsen SP. Are process performance measures associated with clinical outcomes among patients with hip fractures? A population-based cohort study. Int J Qual Health Care. 2016;28(6):698–708. doi: 10.1093/intqhc/mzw093 [DOI] [PubMed] [Google Scholar]
- 26.Nielsen KA, Jensen NC, Jensen CM, et al. Quality of care and 30 day mortality among patients with hip fractures: a nationwide cohort study. BMC Health Serv Res. 2009;9:186-6963-6969-6186. doi: 10.1186/1472-6963-9-186 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kristensen PK, Sogaard R, Thillemann TM, Soballe K, Johnsen SP. High quality of care did not imply increased hospital spending- nationwide cohort study among hip fracture patients. Int J Qual Health Care. 2019. doi: 10.1093/intqhc/mzy243 [DOI] [PubMed] [Google Scholar]
- 28.Kristensen MT, Ozturk B, Rock ND, Ingeman A, Palm H, Pedersen AB. Regaining pre-fracture basic mobility status after hip fracture and association with post-discharge mortality and readmission-a nationwide register study in Denmark. Age Ageing. 2019;48(2):278–284. doi: 10.1093/ageing/afy185 [DOI] [PubMed] [Google Scholar]
- 29.Kristensen PK, Thillemann TM, Johnsen SP. Is bigger always better? A nationwide study of hip fracture unit volume, 30-day mortality, quality of in-hospital care, and length of hospital stay. Med Care. 2014;52(12):1023–1029. doi: 10.1097/MLR.0000000000000234 [DOI] [PubMed] [Google Scholar]
- 30.Kristensen PK, Thillemann TM, Soballe K, Johnsen SP. Can improved quality of care explain the success of orthogeriatric units? A population-based cohort study. Age Ageing. 2015;45:66–71. [DOI] [PubMed] [Google Scholar]
- 31.Kristiansen NS, Kristensen PK, Norgard BM, Mainz J, Johnsen SP. Off-hours admission and quality of hip fracture care: a nationwide cohort study of performance measures and 30-day mortality. Int J Qual Health Care. 2016;28(3):324–331. doi: 10.1093/intqhc/mzw037 [DOI] [PubMed] [Google Scholar]
- 32.Viberg B, Gundtoft PH, Schonnemann J, et al. Introduction of national guidelines for restrictive blood transfusion threshold for hip fracture patients–a consecutive cohort study based on complete follow-up in national databases. J Orthop Surg Res. 2018;13(1):116. doi: 10.1186/s13018-018-0828-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Pedersen AB, Cronin Fenton D, Norgaard M, Kristensen NR, Kuno Moller B, Erikstrup C. Body mass index, risk of allogeneic red blood cell transfusion, and mortality in elderly patients undergoing hip fracture surgery. Osteoporos Int. 2016;27(9):2765–2775. doi: 10.1007/s00198-016-3594-7 [DOI] [PubMed] [Google Scholar]
- 34.Glassou EN, Kjorholt KK, Hansen TB, Pedersen AB. Delay in surgery, risk of hospital-treated infections and the prognostic impact of comorbidity in hip fracture patients. A Danish nationwide cohort study, 2005-2016. Clin Epidemiol. 2019;11:383–395. doi: 10.2147/CLEP.S200454 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Ozturk B, Johnsen SP, Rock ND, Pedersen L, Pedersen AB. Impact of comorbidity on the association between surgery delay and mortality in hip fracture patients: a Danish nationwide cohort study. Injury. 2019;50(2):424–431. doi: 10.1016/j.injury.2018.12.032 [DOI] [PubMed] [Google Scholar]
- 36.Bruun SB, Petersen I, Kristensen NR, Cronin-Fenton D, Pedersen AB. Selective serotonin reuptake inhibitor use and mortality, postoperative complications, and quality of care in hip fracture patients: a Danish nationwide cohort study. Clin Epidemiol. 2018;10:1053–1071. doi: 10.2147/CLEP.S166309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Daugaard C, Pedersen AB, Kristensen NR, Johnsen SP. Preoperative antithrombotic therapy and risk of blood transfusion and mortality following hip fracture surgery: a Danish nationwide cohort study. Osteoporos Int. 2019;30(3):583–591. doi: 10.1007/s00198-018-4786-0 [DOI] [PubMed] [Google Scholar]
- 38.Glassou EN, Kristensen N, Moller BK, Erikstrup C, Hansen TB, Pedersen AB. Impact of preadmission anti-inflammatory drug use on the risk of RBC transfusion in elderly hip fracture patients: a Danish nationwide cohort study, 2005-2016. Transfusion. 2019;59(3):935–944. doi: 10.1111/trf.2019.59.issue-3 [DOI] [PubMed] [Google Scholar]
- 39.Bruun SB, Petersen I, Kristensen NR, Cronin-Fenton D, Pedersen AB. Selective serotonin reuptake inhibitor use in hip fracture patients: a Danish nationwide prevalence study. Acta Orthop. 2019;90(1):33–39. doi: 10.1080/17453674.2018.1543842 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Simoni AH, Nikolajsen L, Olesen AE, Christiansen CF, Pedersen AB. Opioid use after hip fracture surgery: a Danish nationwide cohort study from 2005 to 2015. Eur J Pain. 2019;23(7):1309–1317. doi: 10.1002/ejp.1392 [DOI] [PubMed] [Google Scholar]
- 41.Pedersen AB, Christiansen CF, Gammelager H, Kahlert J, Sorensen HT. Risk of acute renal failure and mortality after surgery for a fracture of the hip: a population-based cohort study. Bone Joint J. 2016;98-b(8):1112–1118. doi: 10.1302/0301-620X.98B8.37497 [DOI] [PubMed] [Google Scholar]
- 42.Pedersen AB, Gammelager H, Kahlert J, Sorensen HT, Christiansen CF. Impact of body mass index on risk of acute kidney injury and mortality in elderly patients undergoing hip fracture surgery. Osteoporos Int. 2017;28(3):1087–1097. doi: 10.1007/s00198-016-3836-8 [DOI] [PubMed] [Google Scholar]
- 43.Kjorholt KE, Kristensen NR, Prieto-Alhambra D, Johnsen SP, Pedersen AB. Increased risk of mortality after postoperative infection in hip fracture patients. Bone. 2019;127:563–570. doi: 10.1016/j.bone.2019.07.023 [DOI] [PubMed] [Google Scholar]
- 44.Kjorholt KE, Johnsen SP, Kristensen NR, Prieto-Alhambra D, Pedersen AB. Increasing risk of hospital-treated infections and community-based antibiotic use after hip fracture surgery: a nationwide study 2005-2016. J Bone Miner Res. 2019;34(3):437–446. doi: 10.1002/jbmr.3620 [DOI] [PubMed] [Google Scholar]
- 45.Pedersen AB, Ehrenstein V, Szepligeti SK, Sorensen HT. Excess risk of venous thromboembolism in hip fracture patients and the prognostic impact of comorbidity. Osteoporos Int. 2017;28(12):3421–3430. doi: 10.1007/s00198-017-4213-y [DOI] [PubMed] [Google Scholar]
- 46.Pedersen AB, Ehrenstein V, Szepligeti SK, Sorensen HT. Hip fracture, comorbidity, and the risk of myocardial infarction and stroke: a Danish nationwide cohort study, 1995-2015. J Bone Miner Res. 2017;32(12):2339–2346. doi: 10.1002/jbmr.v32.12 [DOI] [PubMed] [Google Scholar]
- 47.Sund R, Juntunen M, Luthje P, Huusko T, Hakkinen U. Monitoring the performance of hip fracture treatment in Finland. Ann Med. 2011;43(Suppl 1):S39–S46. doi: 10.3109/07853890.2011.586360 [DOI] [PubMed] [Google Scholar]
- 48.Thorngren KG. National registration of hip fractures. Acta Orthop. 2008;79(5):580–582. doi: 10.1080/17453670810016579 [DOI] [PubMed] [Google Scholar]
- 49.Hawkes D, Baxter J, Bailey C, et al. Improving the care of patients with a hip fracture: a quality improvement report. BMJ Qual Saf. 2015;24(8):532–538. doi: 10.1136/bmjqs-2014-003700 [DOI] [PubMed] [Google Scholar]
- 50.Farrow L, Hall A, Wood AD, et al. Quality of care in hip fracture patients: the relationship between adherence to national standards and improved outcomes. J Bone Joint Surg Am. 2018;100(9):751–757. doi: 10.2106/JBJS.17.00884 [DOI] [PubMed] [Google Scholar]
- 51.Renzi C, Sorge C, Fusco D, Agabiti N, Davoli M, Perucci CA. Reporting of quality indicators and improvement in hospital performance: the P.Re.Val.E. regional outcome evaluation program. Health Serv Res. 2012;47(5):1880–1901. doi: 10.1111/hesr.2012.47.issue-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Zurlo Amedeo BG. Orthogeriatrics in Italy: the Gruppo Italiano di Ortogeriatria (GIOG) audit on hip fractures in the elderly. Geriatr Care. 2018;4(2):33–35. [Google Scholar]
- 53.Gjertsen JE, Dybvik E, Furnes O, et al. Improved outcome after hip fracture surgery in Norway. Acta Orthop. 2017;88(5):505–511. doi: 10.1080/17453674.2017.1344456 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Ojeda-Thies C, Saez-Lopez P, Currie CT, et al. Spanish National Hip Fracture Registry (RNFC): analysis of its first annual report and international comparison with other established registries. Osteoporos Int. 2019;30(6):1243–1254. doi: 10.1007/s00198-019-04939-2 [DOI] [PubMed] [Google Scholar]
- 55.Hughes AJ, Hennessy O, Brennan L, Rana A, Murphy CG. How accurate is the data provided to the Irish hip fracture database? Ir J Med Sci. 2019;188(1):13–18. doi: 10.1007/s11845-018-1810-5 [DOI] [PubMed] [Google Scholar]
- 56.Voeten SC, Arends AJ, Wouters MWJM, et al. The Dutch Hip Fracture Audit: evaluation of the quality of multidisciplinary hip fracture care in the Netherlands. Arch Osteoporos. 2019;14(1):28. doi: 10.1007/s11657-019-0576-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.der Unfallchirurgie AA, AA DGU. Das AltersTraumaRegister DGU®–aktueller Stand, Methodik und Publikationsrichtlinie. Unfallchirurg. 2019;122:1–3. [DOI] [PubMed] [Google Scholar]
- 58.Mattisson L, Bojan A, Enocson A. Epidemiology, treatment and mortality of trochanteric and subtrochanteric hip fractures: data from the Swedish fracture register. BMC Musculoskelet Disord. 2018. doi: 10.1186/s12891-018-2276-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Sayers A, Whitehouse MR, Berstock JR, Harding KA, Kelly MB, Chesser TJ. The association between the day of the week of milestones in the care pathway of patients with hip fracture and 30-day mortality: findings from a prospective national registry - The National Hip Fracture Database of England and Wales. BMC Med. 2017. doi: 10.1186/s12916-017-0825-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Citations
- Regionernes Kliniske Kvalitets Program. De kliniske kvalitetsdatabaser. 2015. Available from: http://www.rkkp.dk/. Accessed January10, 2019.