Abstract
The innate immune response induced by type I interferons (IFNs) plays a critical role in the establishment of HIV infection. IFNs are induced early in HIV infection and trigger an antiviral defense program by signaling through the IFNα/β receptor (IFNAR), which consists of two subunits, IFNAR1 and IFNAR2. Changes in IFNAR expression in HIV target cells, as well as other immune cells, could therefore have important consequences for initial HIV spread. It was previously reported that IFNAR2 expression is increased in peripheral blood CD4+ CXCR4+ T cells of HIV+ patients compared to HIV uninfected controls, suggesting that HIV infection may alter the IFN responsiveness of target cells. However, the earliest immune cells affected by HIV in vivo reside in the gut-associated lymphoid tissue (GALT). To date, it remains unknown if IFNAR expression is altered in GALT immune cells in the context of HIV infection and exposure to IFNs, including the 12 IFNα subtypes. Here, we analyzed the expression of surface bound and soluble IFNAR2 on Lamina propria mononuclear cells (LPMCs) isolated from the GALT of HIV- individuals and in plasma samples of HIV+ patients. IFNAR2 expression varied between different T cells, B cells and natural killer cells, but was not altered following HIV infection. Furthermore, expression of the soluble IFNAR2a isoform was not changed in HIV+ patients compared to healthy donors, nor in LPMCs after HIV-1 infection ex vivo. Even though the 12 human IFNα subtypes trigger different biological responses and vary in their affinity to both receptor subunits, stimulation of LPMCs with different recombinant IFNα subtypes did not result in any significant changes in IFNAR2 surface expression. Our data suggests that potential changes in the IFN responsiveness of mucosal immune cells during HIV infection are unlikely dictated by changes in IFNAR2 expression.
Introduction
Natural transmission of HIV occurs via the vaginal or the gastrointestinal mucosa, where first responses against the invading virus are mounted. Following HIV infection, the gastrointestinal mucosa succumbs to profound enteropathy, including increased gastrointestinal inflammation, malabsorption, diarrhea and increased intestinal permeability [1], as well as microbial translocation and dysbiosis [2,3]. The gastrointestinal lymphoid tissue (GALT) shows stronger substantial depletion of CD4+ T cells, occurring mostly in CD4+ CCR5+ T cells [4,5] than peripheral mononuclear blood cells (PBMCs) which are commonly used for studying HIV immune responses. An earlier study conducted with simian immunodeficiency virus (SIV) proved the CD4+ T cell depletion not only to be more severe, but also to occur much faster in the GALT [6] and showed a delayed restoration of CD4+ T cell numbers following early combined antiretroviral therapy (cART) initiation in comparison to PBMCs [7]. As Lamina propria mononuclear cells (LPMCs), mucosal immune cells from the GALT, are highly susceptible for HIV infection and can be infected efficiently by CCR5-tropic HIV-1 strains, the Lamina propria aggregate culture (LPAC) can be used as an efficient ex vivo model to study HIV infection close to the physiological background [8].
Since adaptive immunity has yet to be mounted in the early stages of infection, innate immune responses are of great importance as the first line of defense. Early host immune responses in the GALT are mediated by type I interferons (IFNs), which are mainly secreted by plasmacytoid dendritic cells (pDC) [9]. Type I IFNs are a pleiotropic cytokine family consisting of IFNα, IFNβ, IFNε, IFNκ and IFNω. The human chromosome 9 contains 13 genes encoding for 12 individual IFNα subtypes [10], highly conserved proteins with an amino acid sequence homology of 75–99% [11]. All type I IFNs bind to the common IFNα/β receptor (IFNAR), which is widely expressed on most cell types [12]. The receptor consists of two subunits, IFNAR1 and IFNAR2, which associate with Janus kinases (Jak) Tyk2 (IFNAR1) and Jak1 (IFNAR2). Upon initial ligand binding by IFNAR2, IFNAR1 is recruited and subsequent to formation of the ternary complex out of IFNAR1, IFNAR2 and IFNα or IFNβ, Tyk2 and JAK1 become activated. Type I IFN signal transduction commonly takes place via the classical Jak-STAT pathway leading to the transcription of numerous IFN-stimulated genes (ISGs) [13]. The IFNAR2 subunit is of special interest, as it is responsible for initial ligand binding and three different isoforms are described. IFNAR2c contains long intracellular domains with associated kinases and is responsible for signal transduction. IFNAR2b is likewise a membrane bound isoform but lacks the intracellular domain, and is thought to be a negative regulator for type I IFN signaling [14]. Meanwhile, IFNAR2a is a soluble isoform, produced by either alternative splicing or by proteolytic cleavage from the cell surface and, in the murine organism, is independently regulated from trans-membranous IFNAR2 [15]. IFNAR2a is known to be increased in multiple sclerosis[16], adeno carcinoma and lung cancer [17,18] and was found to be elevated and negatively correlated with successful IFN therapy in Hepatitis C patients [19].
Compared to healthy individuals, IFNα expression is increased and the specific expression pattern of IFNα subtypes is changed in HIV+ patients. [20–22]. The exact role of IFNs in HIV infection is still under debate, beneficial implications of IFNα as suppressed viral load, increased NK cell function and enhanced suppressive capacity of CD8+ T cells as well as an increase in the expression of ISGs containing HIV restriction factors and thus hindering viral transmission and replication could be observed [23–25]. On the other hand, rescued CD4+ T cell depletion and restored cell function following blockade of IFNAR were reported [23,26], as well as systemic immune activation and limited antigen-specific T cell responses [24], thus indicating a potential detrimental influence of IFN on the course of HIV infection.
Due to their high antiviral potential, several studies testing IFNα as a treatment option for HIV were conducted, but patients showed no or only mild benefits from the treatment [27–29]. This, along with the development of highly effective antiretroviral therapies, led to decreased interest in IFNα as a potential therapeutic strategy against HIV [30]. Furthermore, several studies showed that the clinically approved IFNα2 subtype possesses only weak antiviral activity against HIV [9,31]. Thus the question remains, whether an IFNα subtype with higher antiviral capacities against HIV, such as IFNα14, might be of great use against HIV, for example as a potential addition to cART. Initial studies using IFNα14 as an antiviral agent in humanized mice as well as gene therapy approaches with IFNα14 encoding plasmids showed promising results [31–33].
While reduced expression of canonical ISGs in LPMCs infected with HIV [34] might indicate differences in the IFN responsiveness after HIV infection, differences in the ISG expression pattern can also be observed following stimulation with various IFNα subtypes [9]. Changes in IFNAR expression during infection or subsequent to stimulation with different IFNα subtypes would have the potential to modify IFN responsiveness and induce variations in the ISG expression pattern. A recent study observed increased IFNAR2 expression on CXCR4+ CD4+ T cells in peripheral blood of HIV+ patients [35]. However, while CXCR4 is expressed in equal amounts on PBMCs and LPMCs, LPMCs show higher CCR5 frequencies than PBMCs [8]. So far, no study compared IFNAR2 expression on CCR5+ CD4+ T cells in LPMCs from HIV+ patients and healthy donors. Up to date it is also unknown, if IFNα subtypes shape the IFNα response by differences in their potential to regulate receptor expression.
To mirror the physiological background of HIV infection, we performed experiments using LPMCs isolated from the GALT of otherwise healthy patients, undergoing abdominal surgery. Here, we determine the IFNAR2 expression on different immune cell subsets and investigate the influence of HIV infection on the expression of IFNAR2a and IFNAR2b/c. Varying levels of IFNAR2b/c expression on different immune cell subsets were observed, with the highest expression occurring in B cells, followed by NK and CD4+ and CD8+ T cells. HIV-1 infection did not change the expression of either the surface bound or the soluble isoform of IFNAR2. Finally, stimulation with a half maximal effective concentration (EC50) of different IFNα subtypes did not lead to any changes in receptor expression.
Materials & methods
LPMCs and plasma of HIV-infected patients
LPMCs were isolated from patients undergoing abdominal surgery at the University Hospital Essen. Samples were received via the Westdeutsche Biobank, pathologically evaluated and judged macroscopically normal and healthy. Gut samples from 19 different patients where used in this study, 8 of them female, 11 male. The average age was 55.8 years (+/-12 years). 31.5% of the patients underwent abdominal surgery due to various types of cancers (liposarcoma, Klatskin tumor, adenoma, colon carcinoma, neuroendocrine neoplasia), followed by removal of the pancreas (26.3%). Other reasons stated for undergoing abdominal surgery were gastrectomy, cholecystectomy as well as resection of small intestine and rectum. In order to isolate LPMCs, samples were processed as previously described [36]. Briefly, mucosal tissue was rinsed with HBSS and treated with 1.6 mM DTT (Applichem, Darmstadt, Germany) for 40 min at 37°C. The tissue was rinsed twice with HBSS, and the epithelium was removed with two 60 minute treatments of 1mM EDTA (Applichem) in HBSS and 0.1% BSA (Applichem) at 37°C. Afterwards, mucosal tissue was minced into 1–2 mm square portions and treated with 1-2mg/ml of collagenase D (Sigma Aldrich, St. Louis, USA) in RPMI1640 (Thermo Fisher, Waltham, USA) for two additional 60 minute treatments. LPMCs from each treatment were passed through a cell strainer, and stored in RPMI 1640 with 45% fetal calf serum (Biochrom, Berlin, Germany) and 10% DMSO (Applichem) in liquid nitrogen.
After thawing, up to 50% of viable cells were cultivated in RPMI1640 with 10% human serum (Type AB, Pan Biotech, Aidenbach, Germany), 1% Penicillin/Streptomycin (P/S) (Thermo Fisher), 1% L-Glutamine (Thermo Fisher) and 0.4% Piperacillin/Tazobactam (Fresenius Kabi, Bad Homburg an der Hoehe, Germany). Cells were incubated with 1x106 cells/ml (37 °C and 5% CO2) for the indicated time period. LPMC collection was approved by the Ethics Committee (No.:15–6310) of the medical faculty at the University of Duisburg-Essen.
Plasma samples of HIV+ patients (22 cART-naïve as well as 22 cART-experienced HIV+ patients) were collected from the clinics of dermatology at the University Hospital Essen; HIV- samples (n = 13) were donated by healthy individuals of the University Hospital Essen. Blood collection was approved by the Ethics Committee (No.:11–4715) of the medical faculty at the University of Duisburg-Essen. Viral loads among cART-naïve patients ranged from 223–3,8x106 copies/ml with a mean of 3,37x105 copies/ml. The CD4/CD8 ratio ranged from 0.06–2.28 (mean 0.49) in cART-naïve and 0.11–1.92 (mean 0.73) in cART-experienced patients. Further details can be found in Table 1.
Table 1. Clinical parameters of HIV-1+ patients.
| Characteristic | cART-naive | cART-experienced |
|---|---|---|
| Gender (male/female) | 17/5 | 15/7 |
| Age | 46.23 (30–69) | 44.27 (21–76) |
| HIV-1 subtype (B/non B) | 14/8* | 10/12* |
| CD4+ T cells (cells/μl) | 359.32 (7–877) | 518.32 (71–1230) |
| CD8+ T cells (cells/μl) | 851.64 (42–2380) | 883.27 (303–2540) |
| Ratio of CD4/CD8 | 0.49 (0.06–2.28) | 0.73 (0.11–1.92) |
| HIV-1 RNA (log10 copies /ml) | 5.52 (2.35–6.58) | ≤1.6 |
*cART-naïve: 13.6% C; 4.5% G, A/D, D/F, B/F & unknown
cART-experienced: 40% C; 9% A; 4.5% unknown
Infection
For the production of virus stocks, 6.5x105 HEK293T cells were cultivated in T175 flasks previously coated with 0.1% gelatin solution. Cell culture was performed with DMEM (Thermo Fisher) supplemented with 10% of heat-inactivated fetal calf serum (Merck Millipore, Darmstadt, Germany) and 1% P/S. Cells were transiently transfected with 9 μg HIV-1 NL4-3 nef recombinant virus containing the V3 loop region of the CCR5-tropic HIV-1 92TH014-2 strain (R5-tropic HIV-1NL4.3) [37,38]. 24 h following transfection, cells were supplemented with fresh IMDM (Thermo Fisher) containing 10% FCS and 1% P/S. 48 h after transfection, virus-containing supernatant was purified by centrifugation, aliquoted and stored until usage at -80°C.
Since HIV is not a plaque forming virus, the TCID50 of the virus stock was used to calculate the focus forming units and thus determine the multiplicity of infection (MOI) via TZM-bl Assay. 24 h after seeding TZM-bl cells in a 96 well plate, the media was removed and serial dilutions of virus stock were added to the cells. Two days post infection, supernatant was removed, cells were washed with cold PBS and subsequently fixed with formaldehyde and glutaraldehyde in PBS. The cells were again washed with cold PBS and staining solution was added. 24 h later, the assay was analyzed by counting wells that contained blue stained cells.
LPMCs were thawed one day prior to infection and infected with a MOI of 0.005, 0.01 or 0.02 (R5-tropic HIV-1NL4.3) and MOI 1 (HIV-1BaL) via spinoculation at 1000 g. Viral input was removed following spinoculation and cells were cultivated in fresh media with 1x106 cells/ml. Supernatant of HIV-infected and mock-treated cells were collected at the indicated time points and stored at -80°C until further use.
p24-ELISA
The p24 ELISA with supernatant from infected and non-infected LPMC cultures was performed according to the manufacturer’s protocol (R&D Systems, Minneapolis, USA). Absorbance was measured using the Spark® 10M multimode microplate reader (Tecan, Maennedorf, Switzerland).
FACS staining
Cell surface staining was performed using the following antibodies: anti-CD3 (SK7, BioLegend), anti-CD8 (RPA-T8, BioLegend, San Diego, USA), anti-CD19 (SJ25C1, BioLegend), anti-CD56 (NCAM16.2, BioLegend), anti-IFNAR2 (REA124, Miltenyi Biotech GmbH, Bergisch Gladbach, Germany), Fc Block human (Miltenyi Biotech GmbH). For surface staining, cells were washed once with FACS Buffer (PBS containing 0.1% BSA and 0.02% sodium azide), Pellets were then resuspended and incubated for 10 min with antibody mixture. Cells were washed once more with FACS Buffer and stored until acquisition. Dead cells were excluded from the analysis using Zombie Dye (BioLegend). Samples were acquired with a BD LSR II flow cytometer and a BD Symphony flow cytometer (Becton Dickinson, Franklin Lakes, USA) and data were analyzed using FACSDiva and FlowJo Version 10 (both Becton Dickinson).
sIFNAR2a ELISA
Supernatants of R5-tropic HIV-1NL4.3-infected LPMCs from Day 1, 4 and 7 post infection and plasma of HIV-infected patients (cART+ or cART-naïve) and healthy individuals were analyzed for the amount of sIFNAR2a by ELISA according to the manufacturer’s protocol (RayBiotech, Norcross, USA). For ELISA validation and quantification of results, a sIFNAR2a standard ranging from 0.16 ng/ml to 40 ng/ml was used. Absorbance was measured using the Spark® 10M multimode microplate reader (Tecan).
Magnetic cell separation
CD4+ T cells were isolated using a CD4+ T cell isolation Kit (Miltenyi), cells were isolated according to the manufacturer’s protocol.
Quantitative real time PCR
The mRNA of IFNα-stimulated LPMCs was isolated using the Direct Zol RNA Mini Prep Kit (Zymo Research, Irvine, USA), while mRNA of HIV-infected LPMCs was isolated using the RNeasy Mini Kit (Qiagen, Hilden, Germany). The mRNA samples of IFN-stimulated LPMCs were reverse transcribed using All in one cDNA Synthesis SuperMix (Bimake, Houston, USA) and the resulting cDNA was used for PCR. The mRNA of HIV-infected samples was subjected to one-step PCR. Quantification of the target mRNA was normalized according to the delta-delta Ct (ΔΔCt) method and the expression fold change (2-ΔΔCt) using GAPDH as reference. For the IFNAR2 isoforms IFNAR2a, IFNAR2b & IFNAR2c, Taqman PCR was performed using QuantiTect probe RT PCR Master Mix (Qiagen). Primer sequences were used as the following [39]: IFNAR2a (forward: gagcaagcagtaataaagtctcccttaa; reverse: ggctaaaaagttatg aaaattctgattcc; probe: Fam-aatgcaccctccttccacctggc-Tamra); IFNAR2b (forward: cttgaggca aggtctcgctaag; reverse: ggagtttgactgtagtgcattatga, probe: Fam-ctggaatgcagtggctattcacagg tgc-Tamra); IFNAR2c (forward: cccaaagtcttgaattttcataactt: reverse: aaatgacctccaccatatcca; probe: Fam-acctgccaccgttggaagcc-Tamra). PCRs for IFNAR1 were performed using the Powr Up SYBR Green Master Mix (Thermo Fisher), with the following primers [40]: forward: ttgtgtgaaagccagagcac; reverse: tcaagaagactttcgcagca. Amplification of IFNAR2b and IFNAR2c cDNA was performed with 40 cycles of annealing, extension and annealing steps at 95°C for 15 sec and 60°C for 1 min, following initial steps at 50°C for 2 min and 95°C for 10 minutes. For IFNAR2a, 50 cycles of 95°C for 15 sec, 67°C for 1 min and 70°C for 40 sec were used. Amplification of IFNAR1 cDNA was performed with 40 cycles at 95°C for 30 sec, 59°c for 30 sec and 70°C for 40 sec following an initial 5 min activation step at 95°C. For all one-step PCRs including reverse transcription, an initial step at 48°C for 30 min was added.
Stimulation with different human IFNα subtypes
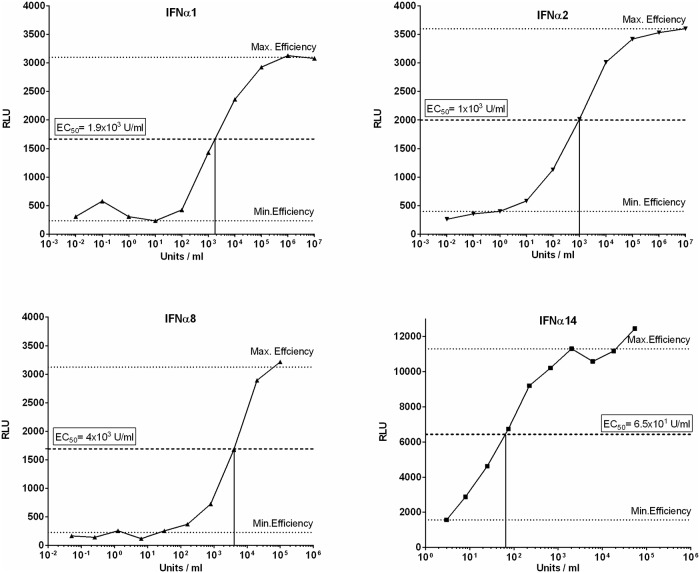
IFNα subtypes were produced and purified as previously described [31]. The activity of each subtype was determined using the human ISRE-Luc reporter cell line, a retinal pigment epithelial cell line transfected with a plasmid containing the Firefly Luciferase gene, stably integrated under control of the IFN-stimulation-response element (ISRE). Following stimulation with IFNα, chemiluminescence can be detected and used to calculate the respective activity in units against commercially available IFNα (PBL assays sciences, Piscataway, USA) [31]. For stimulation experiments, thawed LPMCs were cultivated for the indicated time points with the EC50 of each subtype: IFNα1 1.9x103 U/ml (equals 1.78 ng/ml), IFNα2 1x103 U/ml (equals 4.8 ng/ml), IFNα8 4x103 U/ml (equals 52.6 ng/ml), IFNα14 65 U/ml (equals 0.26 ng/ml).
Statistical analysis
Statistical analysis and graphical presentations were carried out with Graph Pad Prism v6. For comparisons of two datasets, paired t-test was performed. For data including several groups one way ANOVA and Bonferroni’s multiple comparison test was performed.
Results
IFNAR2 expression after HIV-1 infection
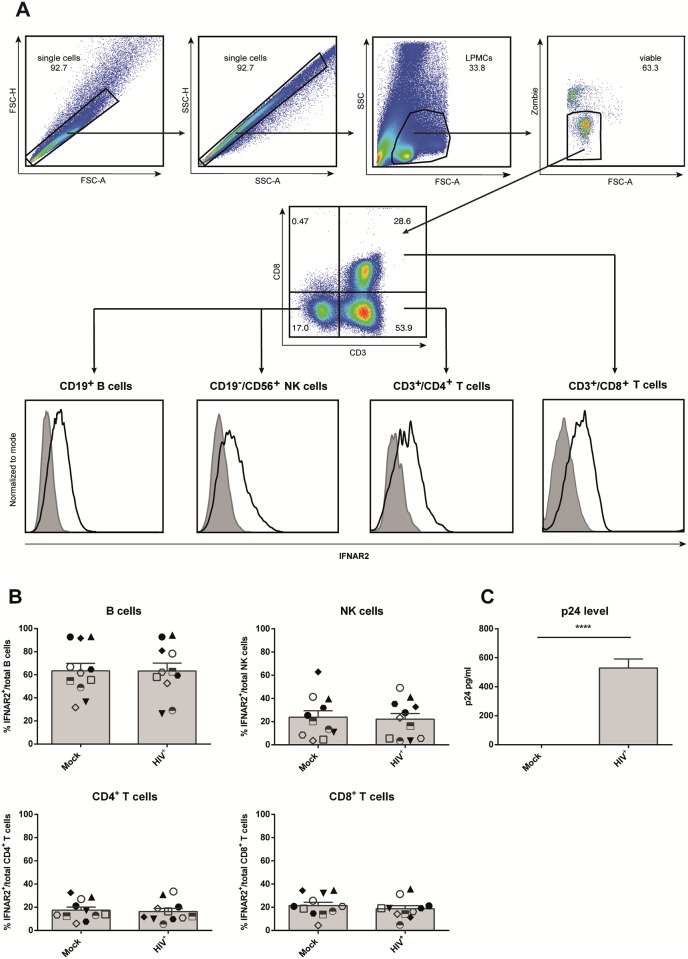
The gut-associated lymphoid tissue is a major site of HIV replication and spread shortly after transmission due to the high numbers of activated, effector memory CD4+ T cells that express the co-receptor CCR5 in this compartment. This process highly depends on type I IFN mediated innate immune responses. The IFN α/β receptor consists of the two subunits IFNAR1 and IFNAR2, of which IFNAR2 is responsible for initial ligand binding. To analyze the impact of HIV-1 infection on IFNα signaling, we determined the surface expression of IFNAR2 on NK cells, B cells, CD4+ and CD8+ T cells among LPMCs isolated from the gastrointestinal mucosa of 11 healthy donors, undergoing abdominal surgery (Fig 1). All gut samples were pathologically evaluated and judged macroscopically normal and healthy by a pathologist. To exclude possible doublets from the analysis, we used forward scatter area versus forward scatter height and sideward scatter area versus sideward scatter height blots, respectively. The remaining single cells were further gated for immune cells based on forward scatter area and sideward scatter area and subsequently gated on viable cells. Using fluorescence minus one controls (FMO), IFNAR2 expression was then analyzed on CD4+ T cells, CD8+ T cells, B cells and NK cells (Fig 1A).
Fig 1. IFNAR2 expression following HIV-1 infection of LPMCs.
LPMCs from healthy donors were infected with R5-tropic HIV-1NL4.3 and cultivated for 4 days. (A) Surface expression of IFNAR2 (black line) on mock-treated and infected cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells using fluorescence minus one controls (tinted area). Histograms and dot plots of one representative LPMC sample are shown. (B) Individual frequencies of IFNAR2-expressing cells and mean values (+SEM) are shown as dots and bars (n = 11). Differences between the groups were analyzed by paired student’s t-test. (C) P24 expression of mock-treated and HIV-infected samples was analyzed by ELISA, p24 expression and mean values (+SEM) are shown by bars (n = 8). Differences between the groups were analyzed by paired student’s t-test, **** indicates p<0.0001.
Of the four immune cell populations analyzed in this study, CD4+ T cells are the most common cell type, accounting for an average of 58.3% (+/- 26.4%) of all viable cells, followed by CD8+ T cells (mean 21.2% +/-15.77%), and B cells (mean 9.8%, +/- 18.10%). The least abundant subtype are NK cells (mean 2.2%, +/- 2.0%).
The percentages of IFNAR2-expressing cells varied strongly between different immune cell subsets, with B cells containing almost three times more IFNAR2-expressing cells (mean 54.7%) than NK cells (mean 20.3%). The smallest proportion of IFNAR2+ cells was found among CD4+ T cells (mean 12.3%) and CD8+ T cells (mean 13.8%) (Fig 1B). Analyzing the mean fluorescence intensity (MFI) at a single cell level, few differences between immune cell subsets were observed with individual NK cells expressing only slightly higher IFNAR2 levels, followed by B cells and both CD4+ T cells and CD8+ T cells (S1 Fig). Following infection with R5-tropic HIV-1NL4.3 with different MOIs (MOI 0.005, MOI 0.01 and MOI 0.02) and HIV-1BaL with MOI 1, neither the percentages of IFNAR2 expressing cells (Fig 1B and S1 Fig) between immune cell subsets, nor the amount of IFNAR2 molecules on the single cell level (MFI, S1 and S2 Figs) changed four or seven days post infection (S3 Fig), indicating that HIV itself has no effect on IFNAR2 surface expression. Successful infection of LPMCs was examined by p24 ELISA (Fig 1C and S1 Fig).
Expression of IFNAR2 isoforms
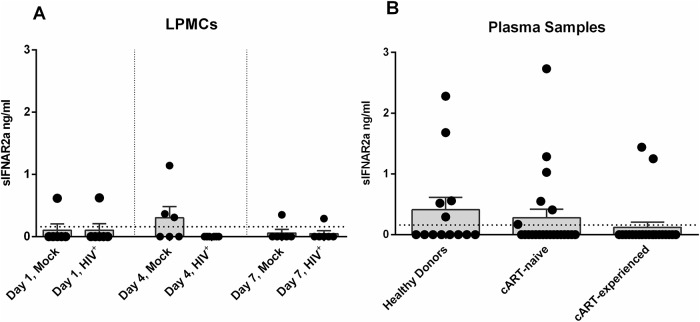
The IFNAR2 receptor subunit is expressed in three different isoforms: IFNAR2a, IFNAR2b and IFNAR2c. IFNAR2c and IFNAR2b are membrane-bound isoforms, IFNAR2c being responsible for signal transduction while IFNAR2b, which lacks the necessary intracellular domains, is thought to be a negative regulator for type I IFN signaling [14]. IFNAR2a is a soluble isoform, which can be produced through alternative splicing or proteolytic cleavage from the cell surface. Since we could not observe any difference in IFNAR2b/c surface expression following HIV-infection (Fig 1B), we next analyzed the expression of soluble IFNAR2 (sIFNAR2a) in the supernatant of mock-treated and HIV-infected LPMCs at days 1, 4 and 7 post infection via ELISA (Fig 2A). Similar to the surface expression of IFNAR2 (Fig 1B), we did not observe any significant differences in the sIFNAR2a expression between mock-treated and HIV-infected LPMCs for any of the indicated time points (Fig 2A). To examine possible effects of HIV-1 infection in vivo, we compared the sIFNAR2 expression in plasma samples of healthy donors (mean 0.41 ng/ml) with plasma samples of HIV-1+ cART-naïve (mean 0.40 ng/ml) and cART-experienced patients (mean 0.21 ng/ml) (Fig 2B). According to the in vitro HIV-infected LPMC results, sIFNAR2a levels did not significantly differ between the groups. Furthermore, we did not find any correlation between viral loads and sIFNAR2a expression in cART-naïve patients. Additionally, no association between the cART regimen and sIFNAR2a expression was observed in cART-experienced HIV+-patients.
Fig 2. Soluble IFNAR2a expression in HIV-1-infected LPMCs and plasma samples.
Supernatant of mock-treated and R5-tropic HIV-1NL4.3-infected LPMCs from days 1, 4 and 7 post infection (A, n = 6) and plasma samples (B) from healthy donors (n = 13), cART-naïve (n = 22) and cART-experienced HIV-1+ patients (n = 22) were analyzed for sIFNAR2a expression via ELISA. The dotted line indicates the detection limit of 0.16 ng/ml. Individual frequencies of sIFNAR2a-expressing samples and mean values (+SEM) are shown as dots and bars. Statistically significant differences between the groups were analyzed by paired student‘s t-test (LPMCs) and ordinary one way ANOVA analysis with Bonferroni’s multiple comparison (plasma samples).
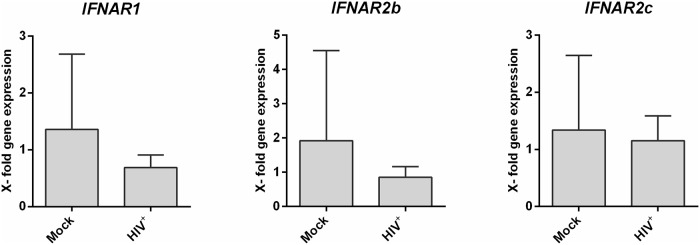
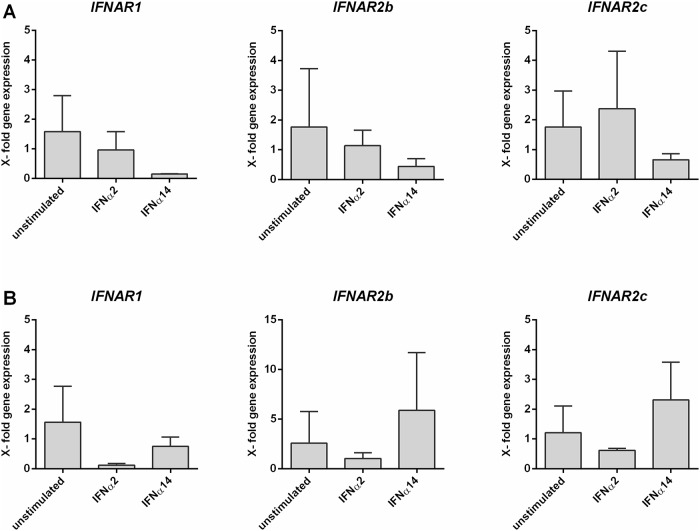
To further validate the previous IFNAR2 protein data and to distinguish between the isoforms IFNAR2b and IFNAR2c, we performed quantitative real time (qRT)-PCR analysis. Therefore, we infected LPMCs from different donors with R5-tropic HIV-1NL4.3, cultivated the cells for 4 days and isolated the mRNA of separated CD4+ T cells. In accordance to the protein surface expression data (Fig 1B), we could not detect any significant changes in IFNAR2b and IFNAR2c mRNA transcripts between mock-treated and HIV-infected LPMCs (Fig 3). Furthermore, we did not detect any IFNAR2a mRNA in our samples, supporting the results from the sIFNAR2a ELISA (Fig 2A). We also determined the mRNA expression of IFNAR1, however, we did not detect any significant differences in transcription level after HIV infection (Fig 3).
Fig 3. IFNAR1 and IFNAR2 mRNA expression in HIV-1-infected LPMCs.
LPMCs were infected with R5-tropic HIV-1NL4.3 and cultivated for 4 days. Following CD4+ T cell isolation, mRNA expression levels of IFNAR1, IFNAR2b and IFNAR2c were analyzed via qRT-PCR. Quantification of the target mRNA was normalized according to the delta-delta Ct (ΔΔCt) method and the expression fold change (2-ΔΔCt) using GAPDH as reference. The mean gene fold expression (+SEM) of each target is shown in bars (n = 4). Differences between the groups were analyzed by paired student’s t-test.
IFNAR2 expression following IFNα subtype stimulation
IFNAR1 and IFNAR2 are known to be differentially regulated and their expression can decrease upon ligand binding [41]. Since the 12 individual human IFNα subtypes differ in their antiviral capacity against HIV [9,31], we sought to compare subtypes with very high (IFNα8 & IFNα14) to those with very low (IFNα1 & IFNα2) antiviral activities, with respect to their potential to influence receptor expression. Furthermore, the chosen IFNα subtypes represent subtypes with high (α14, α2), middle (α8) and low (α1) affinity to IFNAR2.
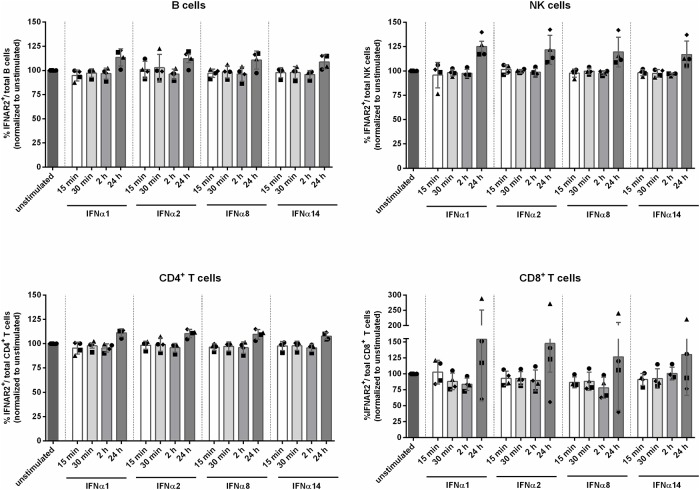
LPMCs from four different healthy donors were stimulated with the EC50 (Fig 4) of IFNα1, IFNα2, IFNα8 and IFNα14 for 15 min, 30 min, 2 h and 24 h. Subsequently, surface receptor expression was determined via flow cytometry. We did not see significant differences in the surface expression of IFNAR2 on CD4+ and CD8+ T cells, B cells and NK cells after stimulation with the different IFNα subtypes. Furthermore, stimulation did not lead to changes in IFNAR2 expression compared to the unstimulated control. Slight elevations of IFNAR2 expression up to approximately 130% compared to the unstimulated control were observed 24 h following stimulation for all tested cell populations. Interestingly, one of the four tested LPMC donors exhibited an increase of IFNAR2 expression up to 270% on CD8+ T cells after IFNα stimulation (Fig 5). In addition to the percentages of IFNAR2 expressing cells, no significant differences were detected at the single cell level when analyzing the MFI (S4 Fig).
Fig 4. Titration of individual IFNα subtype activity.
The recombinant human reporter cell line ISRE-Luc was stimulated with series dilutions of each IFNα subtype. Maximal and minimal effective concentrations were determined and the EC50 was calculated. The upper and lower dotted lines indicate maximal and minimal effective concentration of the respective IFNα subtype, the middle dotted line indicates the EC50.
Fig 5. IFNAR2 expression following stimulation with IFNα subtypes.
LPMCs were stimulated with the EC50 of IFNα1, IFNα2, IFNα8 and IFNα14 for 15 min, 30 min, 2 h and 24 h. Surface expression of IFNAR2 on unstimulated and stimulated cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Individual frequencies of IFNAR2-expressing cells and mean values (+SEM) are shown as dots and bars (n = 4). Differences between the groups were analyzed by ordinary one way ANOVA analysis and Bonferroni’s multiple comparisons.
To further investigate the impact of IFN-stimulation on IFNAR expression and regulation, we determined the mRNA expression of the three IFNAR2 isoforms and IFNAR1. To this end, we isolated mucosal CD4+ T cells from LPMCs by magnetic cell separation and stimulated them with the EC50 of IFNα2 and IFNα14. After 30 min and 24 hours of incubation, mRNA was isolated and its expression was analyzed using isoform-specific primer. Similar to the qRT-PCRs performed on HIV-infected LPMCs (Fig 3), we could not detect any significant changes in the transcription level of IFNAR1, IFNAR2b and IFNAR2c following stimulation with IFNα subtypes for 30 min (Fig 6A) or 24 h (Fig 6B) when compared to the unstimulated controls, supporting the protein surface expression data shown in Fig 5. In accordance to qRT-PCRs performed on HIV-infected LPMCs and to the results from the sIFNAR2a ELISA (Fig 2A), we did not detect any IFNAR2a mRNA in our samples.
Fig 6. IFNAR1 and IFNAR2 mRNA expression in IFNα subtype-stimulated cells.
After isolation of CD4+ T cells from LPMCs, cells were stimulated with the EC50 of IFNα1, IFNα2, IFNα8 and IFNα14 for 30 min (A) and 24 h (B). Following mRNA isolation and reverse transcription, transcription levels of IFNAR1, IFNAR2b and IFNAR2c were analyzed via qRT-PCR. Quantification of the target mRNA was normalized according to the delta-delta Ct (ΔΔCt) method and the expression fold change (2-ΔΔCt) using GAPDH as reference. The mean gene fold expression (+ SEM) of each target is shown in bars (n = 3). Differences between the groups were analyzed by ordinary one way ANOVA analysis and Bonferroni’s multiple comparisons.
Discussion
IFNα/β responses are the immediate early host reaction against invading viruses and crucial for mounting immune responses. Upon engagement of IFNAR, signal transduction results in the expression of hundreds of ISGs, among them several genes encoding for antiviral proteins. Even though all 12 human IFNα subtypes bind the same receptor, they trigger different biological responses and vary strongly in their antiviral activity against HIV. Whereas the only clinically approved subtype IFNα2 exhibits merely weak antiviral effects, other subtypes, such as IFNα14, are highly antiviral against HIV [9,31]. In this study, we aimed to determine whether the different responses are based on differential expression of IFNAR2 on various immune cell populations and if receptor expression levels might be altered upon infection with HIV. Indeed we could find strong differences in the percentages of IFNAR2 expressing cells, which were almost three times as high on B cells compared to CD4+ and CD8+ T cells (Fig 1B). These findings are in agreement with other studies, which also showed higher expression of IFNAR2 on B and NK compared to T cells [42,43]. Whereas Killian et al. [35] observed increased IFNAR2 expression on CXCR4+ CD4+ T cells in whole blood of HIV+ patients compared to healthy donors, we did not see any differences in IFNAR2 surface expression on the analyzed immune cell subsets following HIV infection of LPMCs in vitro. Taken into account that the biological effect of IFNα subtypes highly depends on the microenvironment and cell type [44], differences in receptor expression between different tissues are not unexpected. Furthermore, Killian et al. found increased IFNAR2 expression only on CXCR4+ CD4+ T cells of HIV+ patients compared to healthy donors, but not on CCR5+ CD4+ T cells. We did not determine the ratio of CXCR4+ CD4+ T cells versus CCR5+ CD4+ T cells in our samples. However, while only a small proportion of peripheral CD4+ T cells express CCR5, the majority of CD4+ T cells in LPMCs are reported to be CCR5+ [8]. For HIV+ patients, increased IFNAR2 expression was associated with clinical progression despite effective antiviral therapy progression [35]. Perhaps additional time points after infection are necessary to detect significant changes in IFNAR2 expression when using the LPAC model. Finally, Killian et al. only saw a significant increase in IFNAR2 expression on HAART-patients, and not on therapy-naïve long-term non-progressors, possibly indicating that HAART has an influence on IFNAR2 expression rather than HIV itself [35]. Other studies in mouse models reported a downregulation of IFNAR1 and IFNAR2 during influenza A infections, caused by viral proteins [45,46]. Influenza A was also shown to downregulate IFNAR1 and IFNAR2 in human monocyte-derived macrophages, however ex vivo infection of human lung tissue with Influenza A only reduced the expression of IFNAR1, but not IFNAR2 [46].
Our findings concerning the expression of the soluble isoform of IFNAR2, sIFNAR2a, are in accordance with the results for IFNAR2b/c surface expression. We detected trace amounts of sIFNAR2a in the supernatant of HIV-infected LPMCs (Fig 2A) and we did not see any difference in sIFNAR2a concentrations in the plasma of healthy donors and HIV+ cART-naïve and cART-experienced patients (Fig 2B). Both agonistic and antagonistic properties of sIFNAR2a where shown in mice, specifically concerning their ability to influence the efficacy of therapeutic IFNα treatment [15,47]. In mouse cell lines and primary cells overexpressing sIFNAR2a, the antiproliferative and antiviral effects of IFNα and IFNβ stimulation were inhibited. Recombinant sIFNAR2a was able to bind IFNα and IFNβ and complex with IFNAR1 on the surface of IFNAR2-/- thymocytes, leading to an antiproliferative response [15]. A later study by the same group proofed transgenic mice with elevated sIFNAR2a expression to be more susceptible to LPS-mediated septic shock, in which IFNβ plays a major role. Spleen cells of those transgenic mice overexpressing sIFNAR2a showed a faster, higher and more sustainable activation of STAT1 and STAT3, hence highlighting the agonistic abilities of sIFNAR2a [47]. Organ-dependent ratios of the mRNA for sIFNAR2a versus the mRNA for transmembranous IFNAR2 indicate an independent regulation from transmembranous IFNAR2 and a possibly organ specific biological function [15]. In humans, sIFNAR2a is reported to be elevated in systemic lupus [48] and various types of cancer [17] and to be associated with rather aggressive types of lung cancer [18]. Contradicting findings of elevated [16], decreased [49] and unchanged [48] sIFNAR2a levels in multiple sclerosis compared to healthy patients were reported. IFN therapy was further shown to induce elevated levels of sIFNAR2a compared to differentially treated multiple sclerosis patients and healthy donors [48]. This finding reflects what is seen during hepatitis C infection, in which sIFNAR2a expression was found to be predictive for the response to IFNα2 therapy [19]. One study reported a negative correlation between IFNAR2a expression and B cell exhaustion as well as impaired antibody production in the blood of HIV+ ART- treated, but not HIV+ ART naïve patients [50], which indicates ART rather than HIV itself as the primary effector and thus supports the data mentioned before [35]. Since we did not perform functional analysis of B cells in our samples, we cannot exclude the possibility of an association between sIFNAR2a levels and impaired B cell function. Given that we did not observe any differences between cART-naïve and cART-experienced patients, it is rather unlikely that HIV infection has any influence on the expression of the different IFNAR2 isoforms on LPMCs.
The different affinities of IFNα to both receptor subunits and their respective cell surface density is pivotal for regulation of the biological IFNα response [44,51]. For IFNAR2, a correlation between affinity and antiviral activity was observed [9], while antiproliferative effects seem to be more associated with the affinity to IFNAR1 and the stability of the ternary complex, respectively [52,53]. In addition to the specific dose of IFNα the cell is receiving, micro-environmental factors [45,54] and precise timing of exposure to IFNα in reference to proceeding or subsequent priming of the target cells as well as the duration of ligand binding influence the biological outcome of IFN stimulation [44]. To this end, we analyzed the effect of stimulating LPMCs with four IFNα subtypes, representing subtypes with high (IFNα14), middle (IFNα2 & IFNα8) and low (IFNα1) binding affinity to IFNAR2. Though IFNα8 and especially IFNα14 are highly antiviral against HIV, IFNα1 and IFNα2 exhibit only weak antiviral effects against HIV [9,31,52]. With all four tested subtypes, we did not see any differences in IFNAR2 expression on CD4+ T cells, CD8+ T cells, B cells or NK cells at 15 min, 30 min, 2 h and 24 h post stimulation (Fig 5). Following IFN-stimulation with much higher concentrations than the reported EC50, we observed a downregulation of IFNAR2 on lymphocytes (unpublished data), however these concentrations exceed physiologically tolerable levels of IFNα, and thus are not applicable for therapeutic treatments. As recently reviewed [51], low doses of IFNα have only marginal effects on receptor expression, whereas high doses result in a stronger downregulation of receptor from the cell surface, since a considerably higher amount of receptor molecules is engaged [51] and thus showing a ligand induced dose dependent receptor downregulation.
With all IFNα subtypes possessing different affinities to both receptor subunits, it is likely that they also differ in their influence on ligand induced downregulation of the receptor. Several studies have shown downregulation of both IFNAR1 and IFNAR2 after ligand stimulation on cell lines [41] and on human PBMCs [43], however, only IFNα2 was tested in these studies. In contrast to our findings, Tochizawa et al. [43] observed decreased IFNAR2 expression on PBMCs following 2 h stimulation with 100 U/ml and 1000 U/ml IFNα2, the latter being equal to the EC50 for IFNα2 used in our experiments. As discussed above, it is possible that LPMCs react differently than PBMCs to IFNα stimulation and further elucidation of which cell types exactly exhibit the observed IFNAR2 downregulation is needed. Out of the four cell lines tested by Marijanovic et al. [41], IFNAR2 downregulation was only detected on Hek293T and on HeLa cells, but not on Daudi or Jurkat cells. Among those four, Daudi and Jurkat cells are the only ones originating from immune cells, with Daudi cells being Burkitt Lymphoma cells and Jurkat cells originate from human T cells. Thus, the expression profile of IFNAR1 and IFNAR2 on Daudi and Jurkat cells is more likely to resemble the expression profile of human ex vivo LPMC samples than the expression profiles of HeLa and Hek293T cells. Additionally, the downregulation measured on HeLa and Hek293T cells was more pronounced for IFNAR1 than it was for IFNAR2. Due to the tight regulation of IFNAR1 expression on the cell surface it is likely that IFNAR1 expression is more sensitive to IFNα subtype induced downregulation and its expression has greater influence in shaping the IFNα subtype dependent biological response [55].
In conclusion, neither HIV infection nor IFNα stimulation seem to influence the expression of IFNAR2, which therefore likely does not to affect the IFN responsiveness of cells in the gut during HIV infection.
Supporting information
LPMCs from healthy donors were infected with MOI 1 of CCR5-tropic HIV-1BaL and cultivated for 4 days. Surface expression (A) as wells as MFI (B) of IFNAR2 on mock-treated and infected cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Mean frequencies (+SEM) and mean MFI values (+SEM) of IFNAR2-expressing cells are shown as bars (n = 3). Differences between the groups were analyzed by paired student’s t-test. (C) P24 expression of mock-treated and HIV-infected samples was analyzed by p24 ELISA, mean values (+SEM) are shown as bars (n = 3). Differences between the groups were analyzed by paired student’s t-test, **** indicates p<0.0005.
(TIF)
LPMCs from healthy donors were infected with R5-tropic HIV-1NL4.3 and cultivated for 4 days. Surface expression of IFNAR2 on mock-treated and infected cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Individual MFIs of IFNAR2-expressing cells and mean values (+SEM) are shown as dots and bars (n = 11). Differences between the groups were analyzed by paired student’s t-test.
(TIF)
LPMCs were infected with R5-tropic HIV-1NL4.3 and cultivated for 4 or 7 days respectively. Surface expression (A) as wells as MFI (B) of IFNAR2 on mock-treated and infected cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Mean frequencies (+SEM) and mean MFI values (+SEM) of IFNAR2-expressing cells are shown as bars (n = 3). Differences between the groups were analyzed by paired student’s t-test.
(TIF)
LPMCs were stimulated with the EC50 of IFNα1, IFNα2, IFNα8 and IFNα14 for 15 min, 30 min, 2 h and 24 h. Surface expression of IFNAR2 on unstimulated and stimulated cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Individual MFIs of IFNAR2-expressing cells and mean values (+SEM) are shown as dots and bars (n = 4). Differences between the groups were analyzed by ordinary one way ANOVA analysis and Bonferroni’s multiple comparisons.
(TIF)
Acknowledgments
We would like to acknowledge Stefan Esser for providing plasma samples of HIV+ infected patients, the Westdeutsche Biobank for providing gut biopsies from patients at the University Hospital Essen and Barbara Bleekmann for excellent technical assistance. TZM-bl cells were a kind gift from the NIH AIDS reagent program.
Data Availability
All relevant data are within the manuscript and its Supporting Information files.
Funding Statement
This study was funded by the priority programme "Innate Rensing and Restriction of Retroviruses" (SPP 1923) by the Deutsche Forschungsgemeinschaft to UD and KS. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Brenchley JM, Douek DC. HIV infection and the gastrointestinal immune system. Mucosal Immunol. 2008;1: 23–30. 10.1038/mi.2007.1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Marchetti G, Tincati C, Silvestri G. Microbial Translocation in the Pathogenesis of HIV Infection and AIDS. Clin Microbiol Rev. 2013;23 10.1128/CMR.00050-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Zevin AS, McKinnon L, Burgener A, Klatt NR. Microbial translocation and microbiome dysbiosis in HIV-associated immune activation. Curr Opin HIV AIDS. NIH Public Access; 2016;11: 182–90. 10.1097/COH.0000000000000234 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Brenchley JM, Schacker TW, Ruff LE, Price DA, Taylor JH, Beilman GJ, et al. CD4 + T Cell Depletion During All Stages of HIV Disease Occurs Predominantly in the Gastrointestinal Tract. Pediatrics. 2017;116: 572.1–573. 10.1542/peds.2005-0698bbbb [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Schneider T, Jahn H, Schmidt W, Riecken E, Zeitz M, Ullrich R, et al. Loss of CD4 T lymphocytes in patients infected with human immunodeficiency virus type 1 is more pronounced in the duodenal mucosa than in the peripheral blood [Internet]. Gut. 1995. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1382905/pdf/gut00529-0094.pdf [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Belyakov IM, Ahlers JD. Functional CD8+ CTLs in mucosal sites and HIV infection: moving forward toward a mucosal AIDS vaccine. Trends Immunol. Elsevier Current Trends; 2008;29: 574–585. 10.1016/J.IT.2008.07.010 [DOI] [PubMed] [Google Scholar]
- 7.Guadalupe M, Reay E, Sankaran S, Prindiville T, Flamm J, Mcneil A, et al. Severe CD4 T-Cell Depletion in Gut Lymphoid Tissue during Primary Human Immunodeficiency Virus Type 1 Infection and Substantial Delay in Restoration following Highly Active Antiretroviral Therapy. J Virol. 2003;77: 11708–11717. 10.1128/JVI.77.21.11708-11717.2003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Lapenta C, Boirivant M, Marini M, Santini SM, Logozzi M, Viora M, et al. Human intestinal lamina propria lymphocytes are naturally permissive to HIV-1 infection. Eur J Immunol. 1999;29: 1202–1208. [DOI] [PubMed] [Google Scholar]
- 9.Harper MS, Guo K, Gibbert K, Lee EJ, Dillon SM, Barrett BS, et al. Interferon-α Subtypes in an Ex Vivo Model of Acute HIV-1 Infection: Expression, Potency and Effector Mechanisms. PLOS Pathog. 2015;11: e1005254 10.1371/journal.ppat.1005254 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Weissmann C, Weber H. The interferon genes. Prog Nucleic Acid Res Mol Biol. 1986;33: 251–300. Available: http://www.ncbi.nlm.nih.gov/pubmed/3025923 10.1016/s0079-6603(08)60026-4 [DOI] [PubMed] [Google Scholar]
- 11.Hardy MP, Owczarek CM, Jermiin LS, Ejdebäck M, Hertzog PJ. Characterization of the type I interferon locus and identification of novel genes. Genomics. 2004;84: 331–345. 10.1016/j.ygeno.2004.03.003 [DOI] [PubMed] [Google Scholar]
- 12.De Weerd NA, Nguyen T. The interferons and their receptors-distribution and regulation. Immunol Cell Biol. Nature Publishing Group; 2012;90: 483–491. 10.1038/icb.2012.9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Sutter K, Dickow J, Dittmer U. Interferon α subtypes in HIV infection. Cytokine Growth Factor Rev. Elsevier; 2018;40: 13–18. 10.1016/j.cytogfr.2018.02.002 [DOI] [PubMed] [Google Scholar]
- 14.Gazziola C, Cordani N, Carta S, De Lorenzo E, Colombatti A, Perris R. The relative endogenous expression levels of the IFNAR2 isoforms influence the cytostatic and pro-apoptotic effect of IFNα on pleomorphic sarcoma cells. Int J Oncol. Spandidos Publications; 2005;26: 129–140. 10.3892/ijo.26.1.129 [DOI] [PubMed] [Google Scholar]
- 15.Hardy MP, Owczarek CM, Trajanovska S, Liu X, Kola I, Hertzog PJ. The soluble murine type I interferon receptor Ifnar-2 is present in serum, is independently regulated, and has both agonistic and antagonistic properties. Blood. 2001;97: 473–482. 10.1182/blood.v97.2.473 [DOI] [PubMed] [Google Scholar]
- 16.Chadha K, Weinstock-Guttman B, Zivadinov R, Bhasi K, Muhitch J, Feichter J, et al. Interferon Inhibitory Activity in Patients With Multiple Sclerosis. Arch Neurol. 2006;63: 1579 10.1001/archneur.63.11.1579 [DOI] [PubMed] [Google Scholar]
- 17.Ambrus JLS, Dembinski W, Ambrus JLJ, Sykes DE, Akhter S, Kulaylat MN, et al. Free interferon-?/? receptors in the circulation of patients with adenocarcinoma. Cancer. 2003;98: 2730–2733. 10.1002/cncr.11843 [DOI] [PubMed] [Google Scholar]
- 18.Tanaka S, Hattori N, Ishikawa N, Horimasu Y, Deguchi N, Takano A, et al. Interferon (alpha, beta and omega) receptor 2 is a prognostic biomarker for lung cancer. Pathobiology. 2012;79: 24–33. 10.1159/000331230 [DOI] [PubMed] [Google Scholar]
- 19.Mizukoshi E, Kaneko S, Kaji K, Terasaki S, Matsushita E, Muraguchi M, et al. Serum Levels of Soluble Interferon Alfa / Beta Receptor as an Inhibitory Factor of Interferon in the Patients With Chronic Hepatitis C. Hepatology. 1999;30: 1325–1331. 10.1002/hep.510300516 [DOI] [PubMed] [Google Scholar]
- 20.Li Y, Sun B, Esser S, Jessen H, Streeck H, Widera M, et al. Expression Pattern of Individual IFNA Subtypes in Chronic HIV Infection. J Interf Cytokine Res. 2017;37: 541–549. 10.1089/jir.2017.0076 [DOI] [PubMed] [Google Scholar]
- 21.Stacey AR, Norris PJ, Qin L, Haygreen EA, Taylor E, Heitman J, et al. Induction of a striking systemic cytokine cascade prior to peak viremia in acute human immunodeficiency virus type 1 infection, in contrast to more modest and delayed responses in acute hepatitis B and C virus infections. J Virol. American Society for Microbiology (ASM); 2009;83: 3719–33. 10.1128/JVI.01844-08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.von SYDOW M, SÖNNERBORG A, GAINES H, STRANNEGÅRD Ö. Interferon-Alpha and Tumor Necrosis Factor-Alpha in Serum of Patients in Various Stages of HIV-1 Infection. AIDS Res Hum Retroviruses. 1991;7: 375–380. 10.1089/aid.1991.7.375 [DOI] [PubMed] [Google Scholar]
- 23.Cheng L, Yu H, Li G, Li F, Ma J, Li J, et al. Type I interferons suppress viral replication but contribute to T cell depletion and dysfunction during chronic HIV-1 infection. JCI Insight. 2017;2 10.1172/jci.insight.94366 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Utay NS, Douek DC. Interferons and HIV Infection: The Good, the Bad, and the Ugly. Pathog Immun. 2016;1: 107 10.20411/pai.v1i1.125 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Kwaa AKR, Talana CAG, Blankson JN. Interferon Alpha Enhances NK Cell Function and the Suppressive Capacity of HIV-Specific CD8+ T Cells. 2019; 10.1128/JVI.01541-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cheng L, Ma J, Li J, Li D, Li G, Li F, et al. Blocking type I interferon signaling enhances T cell recovery and reduces HIV-1 reservoirs. J Clin Invest. 2017;127: 269–279. 10.1172/JCI90745 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Alston B, Ellenberg JH, Standiford HC, Muth K, Martinez A, Greaves W, et al. A multicenter, randomized, controlled trial of three preparations of low-dose oral alpha-interferon in HIV-infected patients with CD4+ counts between 50 and 350 cells/mm(3). Division of AIDS Treatment Research Initiative (DATRI) 022 Study Group. J Acquir Immune Defic Syndr. 1999;22: 348–57. Available: http://www.ncbi.nlm.nih.gov/pubmed/10634196 10.1097/00126334-199912010-00005 [DOI] [PubMed] [Google Scholar]
- 28.Bosinger SE, Utay NS. Type I Interferon: Understanding Its Role in HIV Pathogenesis and Therapy. Curr HIV/AIDS Rep. Springer US; 2015;12: 41–53. 10.1007/s11904-014-0244-6 [DOI] [PubMed] [Google Scholar]
- 29.Katabira ET, Sewankambo NK, Mugerwa RD, Belsey EM, Mubiru FX, Othieno C, et al. Lack of eYcacy of low dose oral interferon alfa in symptomatic HIV-1 infection: a randomised, double blind, placebo controlled trial [Internet]. Available: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC1758122/pdf/v074p00265.pdf [DOI] [PMC free article] [PubMed]
- 30.Doyle T, Goujon C, Malim MH. HIV-1 and interferons: Who’s interfering with whom? Nat Rev Microbiol. Nature Publishing Group; 2015;13: 403–413. 10.1038/nrmicro3449 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Lavender KJ, Gibbert K, Peterson KE, Van Dis E, Verheyen J, Müller JA, et al. Interferon Alpha Subtype-Specific Suppression of HIV-1 Infection In Vivo. J Virol. 2016;90: 6001–6013. 10.1128/JVI.00451-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Abraham S, Choi J-G, Ortega NM, Zhang J, Shankar P, Swamy NM. Gene therapy with plasmids encoding IFN-β or IFN-α14 confers long-term resistance to HIV-1 in humanized mice. Oncotarget. Impact Journals, LLC; 2016;7: 78412–78420. 10.18632/oncotarget.12512 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Sutter K, Lavender KJ, Messer RJ, Widera M, Williams K, Race B, et al. Concurrent administration of IFNα14 and cART in TKO-BLT mice enhances suppression of HIV-1 viremia but does not eliminate the latent reservoir. Sci Rep. Nature Research; 2019;9 10.1038/s41598-019-54650-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Yoder AC, Guo K, Dillon SM, Phang T, Lee EJ, Harper MS, et al. The transcriptome of HIV-1 infected intestinal CD4+ T cells exposed to enteric bacteria. Desrosiers RC, editor. PLOS Pathog. Public Library of Science; 2017;13: e1006226 10.1371/journal.ppat.1006226 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Killian MS, Fujimura SH, Sudhagoni RG. Increased expression of the Type i interferon receptor on CD4 + T lymphocytes in HIV-1-infected individuals. J Acquir Immune Defic Syndr. 2017;74: 473–478. 10.1097/QAI.0000000000001280 [DOI] [PubMed] [Google Scholar]
- 36.Howe R, Dillon S, Rogers L, Mccarter M, Kelly C, Madinger N, et al. Evidence for Dendritic Cell-Dependent CD4+ T Helper-1 Type Responses to Commensal Bacteria in Normal Human Intestinal Lamina Propria. Clini Immunol. 2010;131: 317–332. 10.1016/j.clim.2008.12.003.Evidence [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Münch J, Rajan D, Schindler M, Specht A, Rücker E, Novembre FJ, et al. Nef-Mediated Enhancement of Virion Infectivity and Stimulation of Viral Replication Are Fundamental Properties of Primate Lentiviruses. J Virol. 2007;81: 13852–13864. 10.1128/JVI.00904-07 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Papkalla A, Münch J, Otto C, Kirchhoff F. NOTES Nef Enhances Human Immunodeficiency Virus Type 1 Infectivity and Replication Independently of Viral Coreceptor Tropism. J Virol. 2002;76: 8455–8459. 10.1128/JVI.76.16.8455-8459.2002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Bauer A, Rudzki D, Auer M, Hegen H, Deisenhammer F. Expression of interferon type-I receptor isoforms, clinical response and development of neutralizing antibodies in multiple sclerosis patients–results of a prospective study. LaboratoriumsMedizin. De Gruyter; 2016;40: 119–124. 10.1515/labmed-2015-0020 [DOI] [Google Scholar]
- 40.Farmer JR, Altschaefl KM, O’Shea KS, Miller DJ. Activation of the Type I Interferon Pathway Is Enhanced in Response to Human Neuronal Differentiation. Vasilakis N, editor. PLoS One. Public Library of Science; 2013;8: e58813 10.1371/journal.pone.0058813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Marijanovic Z, Ragimbeau J, van der Heyden J, Uzé G, Pellegrini S. Comparable potency of IFNalpha2 and IFNbeta on immediate JAK/STAT activation but differential down-regulation of IFNAR2. Biochem J. Portland Press Ltd; 2007;407: 141–51. 10.1042/BJ20070605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Killian MS, Fujimura SH, Sudhagoni RG. Increased expression of the Type i interferon receptor on CD4+T lymphocytes in HIV-1-infected individuals. J Acquir Immune Defic Syndr. 2017;74: 473–478. 10.1097/QAI.0000000000001280 [DOI] [PubMed] [Google Scholar]
- 43.Tochizawa S, Akamatsu S, Sugiyama Y, Muraguchi M, Ohmoto Y, Ono Y, et al. A flow cytometric method for determination of the interferon receptor IFNAR2 subunit in peripheral blood leukocyte subsets. J Pharmacol Toxicol Methods. Elsevier; 2004;50: 59–66. 10.1016/J.VASCN.2004.02.003 [DOI] [PubMed] [Google Scholar]
- 44.Tomasello E, Pollet E, Vu Manh TP, Uzé G, Dalod M. Harnessing mechanistic knowledge on beneficial versus deleterious IFN-I effects to design innovative immunotherapies targeting cytokine activity to specific cell types. Front Immunol. 2014;5: 1–27. 10.3389/fimmu.2014.00001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Xia C, Vijayan M, Pritzl CJ, Fuchs SY, McDermott AB, Hahm B. Hemagglutinin of Influenza A Virus Antagonizes Type I Interferon (IFN) Responses by Inducing Degradation of Type I IFN Receptor 1. J Virol. 2016;90: 2403–2417. 10.1128/JVI.02749-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Jia D, Rahbar R, Chan RWY, Lee SMY, Chan MCW, Wang BX, et al. Influenza virus non-structural protein 1 (NS1) disrupts interferon signaling. PLoS One. 2010;5 10.1371/journal.pone.0013927 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Samarajiwa SA, Mangan NE, Hardy MP, Najdovska M, Dubach D, Braniff S-J, et al. TLR4-Mediated Septic Shock Type I IFN Signaling and Exacerbates Soluble IFN Receptor Potentiates In Vivo. 2014;. [DOI] [PubMed]
- 48.Fatakdawala T, Skawinski M, Ferriera J, Stauffer T, Lavoie T. Soluble Type I Interferon Receptor 2 Is Elevated By Interferon Treatment and In Certain Autoimmune Diseases—ACR Meeting Abstracts [Internet]. 2013 [cited 2 Jun 2019]. Available: https://acrabstracts.org/abstract/soluble-type-i-interferon-receptor-2-is-elevated-by-interferon-treatment-and-in-certain-autoimmune-diseases/
- 49.Órpez-Zafra T, Pavía J, Hurtado-Guerrero I, Pinto-Medel MJ, Rodriguez Bada JL, Urbaneja P, et al. Decreased soluble IFN-β receptor (sIFNAR2) in multiple sclerosis patients: A potential serum diagnostic biomarker. Mult Scler J. SAGE PublicationsSage UK: London, England; 2017;23: 937–945. 10.1177/1352458516667564 [DOI] [PubMed] [Google Scholar]
- 50.Abudulai L, CHa L, Fernandez S, French M. INCREASED INTERFERON-ALPHA ACTIVITY MAY CONTRIBUTE TO DEFECTS OF B CELLS AND ANTIBODY PRODUCTION CAUSED BY HIV-1 INFECTION. In: Jornal of Virus Eradication, Abstratcs of the IAS 2016 Towards and HIV Cure Symposium [Internet]. 2016 [cited 2 Jun 2019]. http://viruseradication.com/abstract-details.php?abstract_id=1002
- 51.Fuchs SY. Hope and Fear for Interferon: The Receptor-Centric Outlook on the Future of Interferon Therapy. J Interf Cytokine Res. Mary Ann Liebert, Inc.; 2013;33: 211 10.1089/JIR.2012.0117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Lavoie TB, Kalie E, Crisafulli-Cabatu S, Abramovich R, DiGioia G, Moolchan K, et al. Binding and activity of all human alpha interferon subtypes. Cytokine. Elsevier Ltd; 2011;56: 282–289. 10.1016/j.cyto.2011.07.019 [DOI] [PubMed] [Google Scholar]
- 53.Jaks E, Gavutis M, Uzé G, Martal J, Piehler J. Differential Receptor Subunit Affinities of Type I Interferons Govern Differential Signal Activation. J Mol Biol. 2007;366: 525–539. 10.1016/j.jmb.2006.11.053 [DOI] [PubMed] [Google Scholar]
- 54.Katlinski K V., Gui J, Katlinskaya Y V., Ortiz A, Chakraborty R, Bhattacharya S, et al. Inactivation of Interferon Receptor Promotes the Establishment of Immune Privileged Tumor Microenvironment. Cancer Cell. 2017; 10.1016/j.ccell.2017.01.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Ragimbeau J, Dondi E, Alcover A, Eid P, Uzé G, Pellegrini S. The tyrosine kinase Tyk2 controls IFNAR1 cell surface expression. EMBO J. 2003;22: 537–547. 10.1093/emboj/cdg038 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
LPMCs from healthy donors were infected with MOI 1 of CCR5-tropic HIV-1BaL and cultivated for 4 days. Surface expression (A) as wells as MFI (B) of IFNAR2 on mock-treated and infected cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Mean frequencies (+SEM) and mean MFI values (+SEM) of IFNAR2-expressing cells are shown as bars (n = 3). Differences between the groups were analyzed by paired student’s t-test. (C) P24 expression of mock-treated and HIV-infected samples was analyzed by p24 ELISA, mean values (+SEM) are shown as bars (n = 3). Differences between the groups were analyzed by paired student’s t-test, **** indicates p<0.0005.
(TIF)
LPMCs from healthy donors were infected with R5-tropic HIV-1NL4.3 and cultivated for 4 days. Surface expression of IFNAR2 on mock-treated and infected cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Individual MFIs of IFNAR2-expressing cells and mean values (+SEM) are shown as dots and bars (n = 11). Differences between the groups were analyzed by paired student’s t-test.
(TIF)
LPMCs were infected with R5-tropic HIV-1NL4.3 and cultivated for 4 or 7 days respectively. Surface expression (A) as wells as MFI (B) of IFNAR2 on mock-treated and infected cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Mean frequencies (+SEM) and mean MFI values (+SEM) of IFNAR2-expressing cells are shown as bars (n = 3). Differences between the groups were analyzed by paired student’s t-test.
(TIF)
LPMCs were stimulated with the EC50 of IFNα1, IFNα2, IFNα8 and IFNα14 for 15 min, 30 min, 2 h and 24 h. Surface expression of IFNAR2 on unstimulated and stimulated cells was determined via flow cytometry on CD4+ T cells, CD8+ T cells, B cells and NK cells. Individual MFIs of IFNAR2-expressing cells and mean values (+SEM) are shown as dots and bars (n = 4). Differences between the groups were analyzed by ordinary one way ANOVA analysis and Bonferroni’s multiple comparisons.
(TIF)
Data Availability Statement
All relevant data are within the manuscript and its Supporting Information files.