Abstract
Objective:
Gout and hyperuricemia are common public health problem. There has been no epidemiological survey of gout and hyperuricemia in Tibet Autonomous Region, the southwest of China. Therefore, we estimated the prevalence of gout and hyperuricemia in Luoma Town, Naqu City, Tibet Autonomous Region of China.
Methods:
A population-based cross-sectional survey was conducted among 1458 residents of Luoma Town, Tibet Autonomous Region, age ≥40 years. We used questionnaires in face-to-face interviews, anthropometric measurements and serum uric acid test. Hyperuricemia was defined as serum uric acid level ≥7 mg/dl in men and ≥6 mg/dl in women. The definition of gout in this study was on the basis of new 2015ACR/EULAR classification criteria.
Results:
Nine hundred eighty-nine participants completed all items of gout and 818 participants attended to be taken blood samples for serum UA levels test. The overall crude prevalence of gout and hyperuricemia was 0.30% and 1.83% respectively. It was more prevalent in men than in women (2.86% vs 0.75%, P = .034) in hyperuricemia group. Tibetan had a lower age-standardized prevalence of gout 0.26% (95% confidence interval (CI): 0%–0.60%) and hyperuricemia 2.05% (95% confidence interval (CI): 0.99%–3.44%) compared with the China Health and Retirement Longitudinal Study results.
Conclusion:
This is the first large-scale population-based survey to demonstrate the prevalence of gout and hyperuricemia of the middle-aged and elderly population in Tibet Autonomous Region, China. The prevalence of gout and hyperuricemia is relatively lower than other places in China, and that might be influenced by ethnicity, genetic and environment factors. These findings will be useful for the future researches and health care strategies.
Keywords: epidemiology, gout, hyperuricemia, Tibet
1. Introduction
Gout is a common and chronic disease of deposition of monosodium urate crystals in synovial fluid and other tissues, which forms in the presence of increased urate concentrations.[1] It has 4 pathophysiological stages of the progression: hyperuricemia without monosodium urate crystal deposition or gout, crystal deposition without symptomatic gout, acute gout flares, and tophi, chronic gouty arthritis, radiographic erosions.[2] Despite the fact that hyperuricemia is the main pathogenic cause in gout, but many people with hyperuricemia do not develop gout or even form uric acid (UA) crystals. Hyperuricemia, nonetheless, has been an important chronic disease that threatens human health due to associate with an increased risk of multiple comorbidities and mortality.[3,4] Gout affects worldwide people, the prevalence ranges from 0.1% to about 10% in different countries,[5] especially among the middle-aged and elderly population, also the prevalence and incidence of gout are increasing.[6–8,] Different regions have geographic characteristics, genetic factors, which predispose individuals to hyperuricemia or gout.[9]
In general, the prevalence of gout and hyeruricemia is higher in developed countries than developing countries, but it has been increased persistent in many developing countries.[8,10,11] China is the largest developing country, with the economy and society developing in the last 30 years, people's living standard and life-style have changed greatly in most areas. Recent studies have shown that the prevalence of gout in many cities (Beijing, Shanghai, Qingdao, etc.) are increased.[12–15] However, the level of socio-economic development in Tibet Autonomous Region, the southwest of China remains singularly low and little attention has been paid to the prevalence of gout and hyperuricemia in the population of it. Tibet is a distinct area, with an average elevation over 4000 m above sea level, which spreads all over grassland, bare rock and snow. It has a unique culture and traditional lifestyle-nomadic pastoralism.[16] At the same time, obtaining data on this disease to improve medical and health status in this area is necessary. To our knowledge, the epidemiological survey of gout and hyperuricemia in Tibet is empty. Therefore, the aim of this study was to assess the prevalence of gout and hyperuricemia among middle and older adults in Tibet Autonomous Region of China.
2. Materials and methods
This was a cross-sectional survey and the target population was aged 40 years and older living in the Tibet in southwest China. Luoma Town was randomly selected from total of 12 towns in Seni Communities, Naqu City, Tibet Autonomous Region. Luoma Town lies in northern Tibet with an average altitude above 4500 m. This area was considered on behalf of nomadic people in Tibet. The first step, one community was randomly selected from Naqu City. The next step, one town was randomly selected from the former selected community. The cluster (Luoma Town) contents 12 villages and all households in the cluster were included in this study. The study was approved by Peking University People's Hospital Health Science Center Ethics Committee and informed consent was obtained from all study participants.
2.1. Participants
Trained health local professionals administered the survey questionnaires, as it was anticipated that many study participants would be illiterate and could not speak mandarin. All interviewers, clinical examiners, and laboratory tests were trained under the supervision of the study chief investigators. Data were collected at local Luoma Town Health Station, with trained interviewers going to enumerate face-to-face and interview all men and women with a questionnaire, aged 40 years or older, who were self-described residents of Luoma Town. Individuals who self-reported disability, mental disease, malignant tumor, clinotherapy, or egresses works and live away from home over half year were excluded from further participation. The questionnaire form, which includes sociodemographic status (e.g., sex, age, education level, etc.), ethics and marital status, was required to be completed.
2.2. Clinical examination and Serum uric acid test
Height was measured with a wall-mounted stadiometer, using the average of 2 measurements taken. Body weight was assessed using a beam balance scale with 0.1-kg precision. Two professionals administered the history-taking. Participants reported occurrence of at least one episode of swelling, pain, or tenderness in a peripheral joint or bursa were further examinations according to the American College of Rheumatology and European Against Rheumatism (ACR/EULAR) gout classification criteria by trained doctors from our hospital.[17]
Venous blood was collected from each consented respondent by medically-trained staff from the local institution based on a standard protocol. Participants were not asked to have fasted overnight. The centrifuged blood samples were stored in a deep freezer in the local health station. After samples were collected completely, the blood-based bioassays were performed at laboratory in local hospital. The serum urate levels were all determined using enzymatic method. And we retested the blood samples in other hospital used the same method. Then we checked two results consistency with intraclass correlation coefficient (ICC).
2.3. Definitions of gout, hyperuricemia, and other factors
The definition of gout in this study was on the basis of new 2015ACR/EULAR classification criteria. Using sex-specific serum urate distributions to define hyperuricemia, serum urate level of ≥7.0 mg/dl (416.0 μmol/L) in men and ≥6 mg/dl (357.0 μmol/L) in women.[18] The values for serum urate levels are reported in milligrams per deciliter and can be converted to micromoles per liter by multiplying by 59.48.
We divided all subjects into 4 age groups (i.e., 40–49 years, 50–59 years, 60–69 years, and ≥70 years). The levels of education attainment were classified as elementary school and below, middle school, high school and college and higher. Subjects were classified by body mass index (BMI) as underweight (<18.5 kg/m2 =, normal (18.5–22.9 kg/m2), overweight (23–27.4 kg/m2) and obesity (≥27.5 9 kg/m2).[19]
2.4. Statistical analysis
Data was inputted and managed through Epidata software with double entry and validation, version 3.0 (Epidata Association, Odense, Denmark). All analyses and calculations were performed using SPSS statistical package, version 22.0 (SPSS, Inc., Chicago, IL). We used the mean ± standard error and proportions represented continuous variables and categorical variables respectively. Quantitative variables were summarized in terms of means and 95% confidence interval (CI). Differences between subjects were analyzed by Chi-square tests or Fisher exact tests for categorical data, if appropriate. Univariate and multivariate logistic regression analyses were used to estimate the odds ratio (OR) and 95% CI comparing associated influenced factors on gout or hyperuricemia occurrence. P < .05 was considered significant.
3. Results
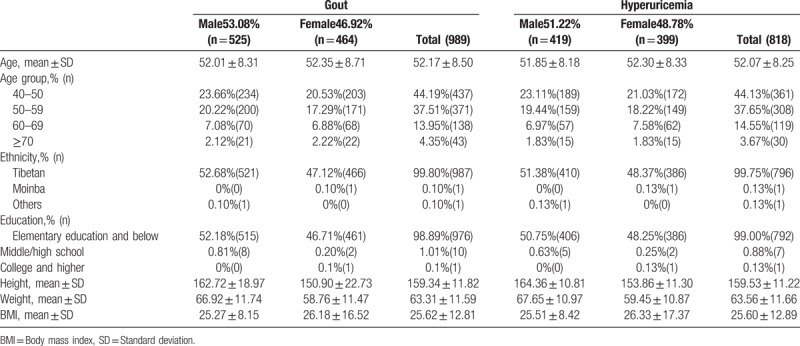
This study was a population-based screening in Luoma Town, Naqu Ctity, Tibet Autonomous Region. A total of 2088 subjects were reported age≥ 40 years in this town. Of all these subjects, 256 were excluded from our study participation due to death, moving away, egresses working, and disability. The remanding 1832 subjects were enrolled, and 1458 (80%) of these subjects consented to enter into this study and completed it in September and October 2018. The consented participants were younger than those who declined to participate (mean ± standard deviation (SD), 53.0 ± 9.2 vs 58.5 ± 3.42, P = .106). Nine hundred eighty-nine participants completed all items of gout and 818 participants attended to be taken blood samples for serum UA levels test. The background characteristics of the gout group and hyperuricemia group participants were presented in Table 1. In gout group, slightly more than half (53.08%) of subjects were men and the mean age of whom (52.01 ± 8.31) was almost equal to women (52.35 ± 8.71). The percentage of Tibetan was approximately approach to 100%. For education distribution, most of men and women only receive elementary or seldom have any formal education (98.89%). The mean BMI of women was greater than men, but all of them are overweight. These characteristics of hyperuricemia group were similar to the gout group.
Table 1.
The characteristics of participants in this study.
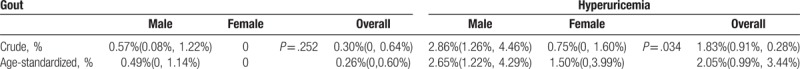
The ICC of 2 blood sample test results was 0.9 which means the blood uric acid result of local hospital was credible. The overall crude prevalence of gout and hyperuricemia was approximately 3.03 per 1000 persons and 18.3 per 1000 persons respectively. It was more prevalent in men than in women (2.86% vs 0.75%, P = 0.034) in hyperuricemia group. The age-standardized prevalence of gout and hyperuricemia were 0.26% (95% confidence interval (CI): 0%–0.60%) and 2.05% (95% CI: 0.99%–3.44%)(Table 2). We examined the association of each factor (age, ethnicity, education, obesity) with the odds of gout and hyperuricemia, for overall and sex-specific. But there was no significant result.
Table 2.
The prevalence of Gout and Hyperuricemia.
4. Discussion
In this population-based study of the middle-aged and older people in Tibet region, the age-standardize prevalence of hyperuricemia (2.05%) was lower than the level of Mainland China (6.2%) based on China Health and Retirement Longitudinal Study (CHARLS).[20] In that study, the prevalence of hyperuricemia was 7.8% in men and 4.8% in women by the definition of UA level (higher than 7.0 mg/dl and 6.0 mg/dl respectively). In our study it was 2.65% in men and 1.49% in women according to the same criteria. That was significantly lower than CHARLS results. Sex hormones may explain the difference between the sexes and hyperuricemia was still a male-dominated disease. Previous studies have presented that the prevalence of hyperuricemia differs in different regions of china, which suggest the etiology of this disease was influence by both gene and environment factors.[18] The geographical environment of Tibet area is different from inland or coastal areas of China due to the high altitude and alpine climate which means their food resources and diversity are limited.[21] They prefer to eat yak meat, yak buttermilk tea and highland barley. At the same time, a study shown that native Tibetan adults’ alcohol consumption rat was near 50%, which is higher than the average of the nation.[22] Hyperuricemia is one of the metabolic diseases related to dietary habits. To our knowledge, certain food like alcohol, fat-rich diet and yak meat containing rich purine can increase the risks of hyperuricemia.[23] Qinghai province, located in Qinghai-Tibet Plateau has similar environment factors and lifestyle to Tibet, with a moderate prevalence of hyperuricemia (5.2%).[20] In addition, Xin et al reported that there is a high prevalence of hyperuricemia (37.2%) in Ganzi Tibetan Autonomous Prefecture, which border on the Tibet Autonomous Region.[24] Interestingly, our study obtained the opposite result. The most likely reason is construction of ethnicity (Han 20.90%, Tibetan 69.50%, Yi 9.70%) in that study was different from our study (Tibetan 99.8%) with a high percentage of farmers-herdsmen. Therefore, our study participants represented the prevalence of hyperuricemia of Tibetan ethnicity in nature nomadic area. The serum uric acid level is affected by race and the prevalence of huyperuricemia is more prevalent in cities than that in rural areas.[18] At the same time, recent study shown that genetic variants have a much greater contribution to hyperuricaemia in the general population than dietary exposure.[25] This may explain the different prevalence in these studies, but further research is necessary.
Gout is a systemic disease due to deposition of monosodium urate crystals in tissues when the serum uric acid is above a specific threshold. The dietary habit of Tibetan is the risk factor of gout as well. In this representative sample of Tibetan nomadic adults, the age-standardized prevalence of gout was 0.26% totally, 0.49% in men and not found in women. Previous epidemiological studies have shown that the prevalence of gout varies from 0.43% to 1.53% among geographical regions in China and a meta-analysis pooled prevalence of gout was 1.1%.[15] Noteworthy, the prevalence of gout in Tibetan area was lower than other regions of China, and the sexual diversity was the same as the previous studies even there was no statistical significance.[26] In that meta-analysis, however, the individual studies were generally small-scale local investigations and the majority (71.0%) participants from the urban area.[15] In other words, gout is more common in economically developed areas, such as urban areas.[10] At the same time, the varying prevalence of gout suggests race, gene and metabolism may influence the pidemiology of gout. MacFarlane et al. found that the race and ethnicity changed the risk of developing hyperuricemia and gout.[27] In addition, many studies support the existence of familial aggregation of gout is strong.[28,29] Tibet is isolated from inland China and the highlanders have lived there for generations, which means they have distinct genetic backgrounds with a lower level of heterozygosity, and a higher level of runs of homozygosity.[30] Maybe this could at least explain the lower prevalence in Tibetan areas even with the risk factors.
Our study is the first large-scale population-based survey to demonstrate the prevalence of gout and hyperuricemia of the middle-aged and elderly population in Tibet Autonomous Region. Almost all the participants of this study are Tibetan race. Thus, the findings are generalizable to describe the prevalence of aborigines in Tibet.
5. Limitations
This study has several limitations. First, it was a cross-sectional study, which could not provide any information about the cause and effect. Further studies are required to investigate the findings. Second, we did not ask participants to fast overnight before venous blood collection, which may cause the increasing of the rate of false positives. Third, the data of dietary and medication use was not included, which is an important component of the level of uric acid. Thus we were not able to assess whether the level of uric acid was influenced by purine-rich food and medication use. Tough Tibetan people give priority to meat, fat-rich food and alcohol, the prevalence of gout and hyperuricemia were still lower than excepted results.
6. Conclusion
In conclusion, the prevalence of gout and hyperuricemia is relatively low in Tibet Autonomous Region, China. Based on previous studies, it maybe related to the ethnicity, genetic, and environment factors. Consequently, these findings will be useful for the future researches and health care strategies. But large well-designed multicenter epidemic investigations are required.
Acknowledgments
We acknowledge the staff of Luoma town health station and Tibet Autonomous Region People's Hospital, Lhasa People's Hospital and Tibet Center for Disease control and Prevention. We thank School of Public Health, Peking University for the statistical consultation.
Author contributions
Conceptualization: Hong Qiang Gong, Yun Ting Wang, Jian Hao Lin.
Data curation: Qing Xi Zhang, Hong Qiang Gong, Chu Tong Lin, Yangjin Baima.
Formal analysis: Qing Xi Zhang.
Investigation: Qing Xi Zhang, Hong Qiang Gong, Jian Hao Lin.
Methodology: Chu Tong Lin, Qiang Liu.
Project administration: Yun Ting Wang, Jian Hao Lin.
Software: Qing Xi Zhang.
Writing – original draft: Qing Xi Zhang.
Writing – review & editing: Yun Ting Wang, Jian Hao Lin.
Footnotes
Abbreviations: ACR/EULAR = American College of Rheumatology and European Against Rheumatism, BMI = body mass index, CHARLS = China Health and Retirement Longitudinal Study, CI = confidence interval, ICC = intraclass correlation coefficient, OR = odds ratio, SD = standard deviation, UA = uric acid.
How to cite this article: Zhang Q, Gong H, Lin C, Liu Q, Baima Y, Wang Y, Lin J. The prevalence of gout and hyperuricemia in middle-aged and elderly people in Tibet Autonomous Region, China: A preliminary study. Medicine. 2020;99:2(e18542).
QZ and HG contributed equally to this work.
This study was supported by the National Natural Science Foundation of China (No. 81672183, 81501919), Peking University People's Research Development Funds (No.2127000091) and Technology Science and Technology Major Projects of Beijing Municipal Science and Technology Commission of China (No. Z181100001818008, D171100003217002, Z171100002717094).
The authors declare that they have no conflicts of interest.
References
- [1].McCarty DJ, Hollander JL. Identification of urate crystals in gouty synovial fluid. Ann Intern Med 1961;54:452–60. [DOI] [PubMed] [Google Scholar]
- [2].Dalbeth N, Stamp L. Hyperuricaemia and gout: time for a new staging system? Ann Rheum Dis 2014;73:1598–600. [DOI] [PubMed] [Google Scholar]
- [3].Niskanen LK, Laaksonen DE, Nyyssonen K, et al. Uric acid level as a risk factor for cardiovascular and all-cause mortality in middle-aged men: a prospective cohort study. Arch Intern Med 2004;164:1546–51. [DOI] [PubMed] [Google Scholar]
- [4].Puig JG, Martínez MA. Hyperuricemia, gout and the metabolic syndrome. Curr Opin Rheumatol 2008;20:187–91. [DOI] [PubMed] [Google Scholar]
- [5].Kuo CF, Grainge MJ, Zhang W, et al. Global epidemiology of gout: prevalence, incidence and risk factors. Nat Rev Rheumatol 2015;11:649–62. [DOI] [PubMed] [Google Scholar]
- [6].Kuo C-F, Grainge MJ, Mallen C, et al. Rising burden of gout in the UK but continuing suboptimal management: a nationwide population study. Ann Rheum Dis 2015;74:661–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [7].Wallace KL, Riedel AA, Joseph-Ridge N, et al. Increasing prevalence of gout and hyperuricemia over 10 years among older adults in a managed care population. J Rheumatol 2004;31:1582–7. [PubMed] [Google Scholar]
- [8].Zhu Y, Pandya BJ, Choi HK. Prevalence of gout and hyperuricemia in the US general population: the National Health and Nutrition Examination Survey 2007–2008. Arthritis Rheum 2011;63:3136–41. [DOI] [PubMed] [Google Scholar]
- [9].Mikuls T, Farrar J, Bilker W, et al. Suboptimal physician adherence to quality indicators for the management of gout and asymptomatic hyperuricaemia: results from the UK General Practice Research Database (GPRD). Rheumatology 2005;44:1038–42. [DOI] [PubMed] [Google Scholar]
- [10].Dalbeth N, Merriman TR, Stamp LK. Gout. Lancet 2016;388:2039–52. [DOI] [PubMed] [Google Scholar]
- [11].Lohsoonthorn V, Dhanamun B, Williams MA. Prevalence of hyperuricemia and its relationship with metabolic syndrome in a adults receiving annual health exams. Arch Med Res 2006;37:883–9. [DOI] [PubMed] [Google Scholar]
- [12].Dai SM1, Han XH, Zhao DB, et al. Prevalence of rheumatic symptoms, rheumatoid arthritis, ankylosing spondylitis, and gout in Shanghai, China: a COPCORD study. J Rheumatol 2003;30:2245–51. [PubMed] [Google Scholar]
- [13].Li R, Sun J, Ren LM, et al. Epidemiology of eight common rheumatic diseases in China: a large-scale cross-sectional survey in Beijing. Rheumatology (Oxford) 2012;51:721–9. [DOI] [PubMed] [Google Scholar]
- [14].Miao Z, Li C, Chen Y, et al. Dietary and lifestyle changes associated with high prevalence of hyperuricemia and gout in the Shandong coastal cities of Eastern China. J Rheumatol 2008;35:1859–64. [PubMed] [Google Scholar]
- [15].Liu R, Han C, Wu D, et al. Prevalence of Hyperuricemia and Gout in Mainland China from 2000 to 2014: A Systematic Review and Meta-Analysis. Biomed Res Int 2015;10:1155–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Jones S. Tibetan nomads: Environment, pastoral, and material culture. 1996;New York: Rhodos International Science and Art Publishers, ISBN-10: 8772455675;ISBN-13: 9788772455679. [Google Scholar]
- [17].Neogi T, Jansen TL, Dalbeth N, et al. 2015 Gout Classification Criteria: an American College of Rheumatology/European League Against Rheumatism collaborative initiative. Ann Rheum Dis 2015;74:1789–98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Liu H, Zhang XM, Wang YL, et al. Prevalence of hyperuricemia among Chinese adults: a national cross-sectional survey using multistage, stratified sampling. J Nephrol 2014;27:653–8. [DOI] [PubMed] [Google Scholar]
- [19].Barba C, Cavalli-Sforza T, Cutter J, et al. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet 2004;363:157–63. [DOI] [PubMed] [Google Scholar]
- [20].Peige Song, He Wang, Wei Xia, et al. Prevalence and correlates of hyperuricemia in the middle-aged and older adults in China. Sci Rep 2018;8:4314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Kimura Y, Okumiya K, Sakamoto R, et al. Comprehensive geriatric assessment of elderly highlanders in Qinghai, China IV: comparison of food diversity and its relation to health of Han and Tibetan elderly. Geriatr Gerontol Int 2009;9:359–65. [DOI] [PubMed] [Google Scholar]
- [22].Ge K, Zhai F, Wang Q. Effect of nationality on dietary pattern and meal behavior in China. Am J Clin Nutr 1997;65: 4 Suppl: 1290S–4S. [DOI] [PubMed] [Google Scholar]
- [23].Choi HK, Liu S, Curhan G. Intake of purine-rich foods, protein, and dairy products and relationship to serum levels of uric acid. The Third National Health and Nutrition Examination Survey. Arthr Rheum 2005;52:283–389. [DOI] [PubMed] [Google Scholar]
- [24].Zhang X, Meng Q, Feng J, et al. The prevalence of hyperuricemia and its correlates in Ganzi Tibetan Autonomous Prefecture, Sichuan Province, China. Lipids Health Dis 2018;17:235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Major TJ, Topless RK, Dalbeth N, et al. Evaluation of the diet wide contribution to serum urate levels: meta-analysis of population based cohorts. MBJ 2018;363:k3951. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Hak AE, Curhan GC, Grodstein F, et al. Menopause, postmenopausal hormone use and risk of incident gout. Ann Rheum Dis 2010;69:1305–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].MacFarlane LA, Kim SC. Gout: a review of nonmodifiable and modifiable risk factors. Rheum Dis Clin N Am 2014;40:581–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Mituszova M, Judak A, Poor G, et al. Clinical and family studies in Hungarian patients with gout. Rheumatol Int 1992;12:165–8. [DOI] [PubMed] [Google Scholar]
- [29].Choi HK, Zhu Y, Mount DB. Genetics of gout. Curr Opin Rheumatol 2010;22:144–51. [DOI] [PubMed] [Google Scholar]
- [30].Lu D, Lou H, Yuan K, et al. Ancestral origins and genetic history of Tibetan highlanders. Am J Hum Genet 2016;99:580–94. [DOI] [PMC free article] [PubMed] [Google Scholar]


