Abstract
Inappropriate care for patients with cognitive dysfunction in the hospital could worsen quality of care and medical service satisfaction.
All elderly participants were recruited from acute wards of 5 departments in an university hospital. They were administered the Chinese version of Ascertain Dementia 8 (AD8) at admission and the Nursing Service Satisfaction Questionnaire before discharge.
A total of 345 participants completed the study. There were 91 (26.4%) participants with AD8 ≥ 2, the cut-off value of high risk of dementia. The prevalence was much higher than prior community-based reports. The Nursing Service Satisfaction Score was significantly lower in AD8 ≥ 2 than in AD8 < 2 (56.99 ± 0.94 vs 60.55 ± 0.48, P < .01).
Using AD8 in hospital-based screening might be more efficient than in the community in terms of cost-effectiveness due to higher positive rate and easier approach to diagnostic facilities. AD8 ≥ 2 is also an indicator to identify care dissatisfaction among inpatients. By identifying patients with cognitive dysfunction, such as its related communication barriers, care systems could be tailored for more friendly services.
Keywords: AD8, dementia screen, hospital-based, nursing satisfaction
1. Introduction
Dementia is one of the most important health issues worldwide. World Health Organization reported that dementia affects 50 million people and nearly 10 million new cases occur every year, causing disability and dependency among older people.[1] According to a nationwide survey of dementia in Taiwan, in the Taiwanese population aged ≥65 years, the age-adjusted prevalence of all-cause dementia was 8.04%. A previous study in Taiwan reported lower prevalence of dementia (1.7%–4.3%), which was possibly caused by differences in population age and inclusion criteria.[2] Dementia in patients admitted to hospitals for acute illness leads to longer stays and additional costs of up to 19% compared with those without dementia.[3,4] Hospitalization of a person with cognitive dysfunction is usually not well supported by the hospital staff. Medical staff lacking of interpersonal relationship skills and education about dementia care could cause negative experiences during the hospital stays of patients with dementia. When medical care involves minimal engagement with the patients, which result from cognitive impairment of patients, the patients might feel largely ignored. This also can produce a low-quality experience for the patients and care providers.[5,6] Therefore, to identify the in-patients with cognitive dysfunction and tailor the care should be necessary.
The need of dementia screening in community is controversial due to, in part, lack of a tool with enough sensitivity and specificity and low cost-effectiveness.[7] However, dementia screening among in-patients might be more cost-effectiveness. The Ascertain Dementia 8 (AD8) questionnaire was developed by Washington University in St Louis. It is not a performance-based tool but an evaluation of life changes during a given period. It has been validated in the community, primary health care units and hospitals.[8,9] Using cutoff values for two endorsed items, the sensitivity was 74% and specificity was 86% for reliably differentiating between nondemented and demented individuals.[10,11] The original English version of AD8 was translated into Traditional Chinese with sensitivity 95.89%, specificity 78.07%, and area under curve (AUC) 0.948 in discriminating CDR 0, normal cognition, from CDR 0.5, mild cognitive impairment, groups.[8] AD8 was used in a walk-in dementia screening of the general population in Taiwan, which showed 14% dementia positive rate in community.[12]
Among aged patients admitted to acute wards, dementia is usually underestimated, with only 35.6% to 50% of patients with cognitive dysfunction being promptly diagnosed.[13,14] In hospital for acute illness settings, the top causes of hospitalization are slightly different between patients with dementia and without dementia. Urinary tract infections, drug-related psychosis, delirium, and complications of dementia are more common in the dementia patients.[15] In another study, the leading causes to acute admission of patients with Alzheimer's disease are syncope or falls, ischemic heart disease, gastrointestinal disease, pneumonia, and delirium.[16] In Taiwan, most patients with these diseases are admitted in Cardiology, Orthopedics, Gastroenterology, Neurology, and Chest Medicine wards. People with cognitive dysfunction have higher risk of mortality, longer stays and higher costs. During hospitalization; thus, early identification and prompt tailoring care are crucial for good outcome.[13]
In this study, we aim to identify patients with high risk of cognitive dysfunction by using AD8 in hospital-based screening in various wards with presumed high prevalence of dementia among in-patients. We also studied the quality of care using Nursing Service Satisfaction Questionnaire to evaluate how cognitive dysfunction exerts influence on nursing service satisfaction.
2. Methods
2.1. The participants
We recruited participants ≥50 years old. All participants voluntarily joined the screening activity without any reward. They were recruited from the acute wards of five departments, namely Gastroenterology, Neurology, Orthopedics, Cardiology, and Chest Medicine in Taipei Medical University Shuang Ho Hospital, a tertiary referral hospital in northern Taiwan, from October 22, 2015 to October 22, 2017. All participants received a comprehensive medical evaluation, including clinical history, physical examination, and blood chemistry examinations according to clinical requirements. Participants needed to wear glasses and hearing aids if they presented hearing and vision impairment, to ensure that they understood the questions and their answer reflected real situation.
2.2. Evaluation
All procedures were approved by the Taipei Medical University Hospital Institutional Review Board, and written informed consent was obtained from all participants or their legal representatives. All recruited participants were administered the Chinese version AD8 and Nursing Service Satisfaction Questionnaire. Demographic data (age, gender) were gathered from medical records. To minimize selection bias, we also collected data regarding people who could not consent themselves by obtaining assent from their legal representatives.
2.3. Administration of AD8
AD8 contains 8 questions asking the participant or the informant to rate changes (Yes vs No vs N/A) in memory, problem-solving abilities, orientation, and daily activities. The answers with Yes are totaled to obtain the AD8 score. Using cutoff values for 2 endorsed items, the sensitivity was 74% and specificity was 86% that reliably differentiates between nondemented and demented individuals.[10,11] The benefits of AD8 are the simple scoring system, minimal training required and being less prone to bias from different education level.[17] The original English version of AD8 was translated into Traditional Chinese with sensitivity 95.89%, specificity 78.07%, and area under curve (AUC) 0.948 in discriminating CDR 0 from CDR 0.5 group.[8] In this study, Traditional Chinese version of AD8 was independently administered to all participants. We define participants with AD8 ≥ 2 as cognitive dysfunction group.
2.4. Administration of nursing service satisfaction questionnaire
The Nursing Service Satisfaction Questionnaire was developed through Delphi method with content validity index 92.76%. It covers 5 major aspects, namely environmental control, care attitude, care process, respect for care, and others, which are taken as routine evaluation of nursing care quality in Taipei Medical University Shuang Ho Hospital. Participants were guided to rate each item on a scale from 0 to 4 (17 items, scores ranging from 0 to 68).[18] The primary fillers of this questionnaire is the patients. Only when the patients cannot consent for themselves, the family members have to fill it.
2.5. Statistical analysis
Data analysis was conducted in GraphPad Prism version 5. All statistical tests were two-tailed, and an alpha of 0.05 was taken to indicate significance. Descriptive statistics were used to report the demographic and clinical characteristics of the patients, including age, sex, AD8 scores, and Nursing Service Satisfaction Score. The differences in Nursing Service Satisfaction Score were assessed using t tests (AD8). Pearson Chi-squared tests were used to examine the relationship between categorical data. Analysis of variance was used for group differences between continuous variables. Pearson correlation was used to measure the linear correlation between two variable AD8 scores and total Nursing Service Satisfaction Score.
3. Results
AD8 was administered to 345 participants between October 22, 2015 and October 22, 2017. In all, 53 participants were from the Neurology ward, 87 from the Orthopedics ward, 93 from the Gastroenterology ward, 90 from the Cardiology ward, and 22 from the Chest Medicine ward. 67 out of 345 participants were not able to consent themselves and needed assent from their legal representatives. The AD8 and Nursing Service Satisfaction Questionnaire of these participants were informant based. The participant's mean age at time of assessment was 69.9 ± 10.8 years (range 50–98 years); 46% of the participants were women. The mean age was significantly different among the 5 wards (P = .03), with the highest average age 74.4 years in Chest Medicine ward and lowest average age 68 years in Orthopedics ward. (Table 1) The mean age of AD8 ≥ 2 group was also significantly older than AD8 < 2 group. (Table 2) Participants were predominantly men (64%), and there were significant differences with regard to gender proportion in the wards, with proportion of women being the highest in Orthopedics ward (63%), P < 0.001. The prevalence of AD8 ≥ 2 among participants was 26.4%, highest in the Neurology ward (49%) and lowest in the Cardiology ward (12%). Totally, 91 participants had AD8 ≥ 2, and among them, 15 (16.5%) had been previously diagnosed with dementia. (Table 1) The average Nursing Service Satisfaction Score was 59.6. Significant difference was revealed between participants with AD8 ≥ 2 and AD8 < 2 (56.99 ± 0.9 vs 60.55 ± 0.5, P < .01), with poorer nursing satisfaction in AD8 ≥ 2 group. The AD8 total score showed negative correlation to Nursing Service Satisfaction Score with statistically significance (Fig. 1; Pearson correlation coefficient (r) = −0.3413 and P < .05). However, no significant difference of Nursing Service Satisfaction Score between genders or among the 5 wards was shown. Age was not correlated to the Nursing Service Satisfaction Score (Fig. 2; Pearson correlation coefficient (r) = −0.0210, P = .77). For the proportion of reported change in each subitem of AD8, the subitems with the highest positive rate were AD8-3 and AD8-8, which reached 17.4% and 35.1% positive rate, respectively. Significant differences in the positive rate of AD8 subitems were observed among the AD8 ≥ 2 and AD8 < 2 groups. (Table 3) In AD8 ≥ 2 participants, the scores of subitems associated with communication in Nursing Service Satisfaction questionnaire, including 02, 03, 04, and 16 were relatively lower than those of other subitems, mean score below or equal to 3.3. (Table 4)
Table 1.
Demographic characteristics of all participants.

Table 2.
Characteristics of AD8 ≥ 2 or AD8 < 2 participants.

Figure 1.
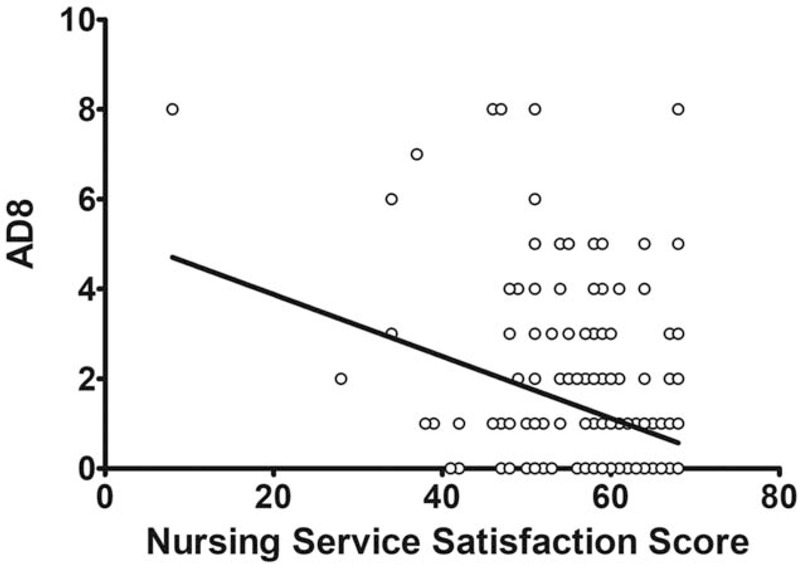
Scatter plot of AD8 and Nursing Service Satisfaction Score. Pearson correlation coefficient (r) = -0.3413, P < .05.
Figure 2.
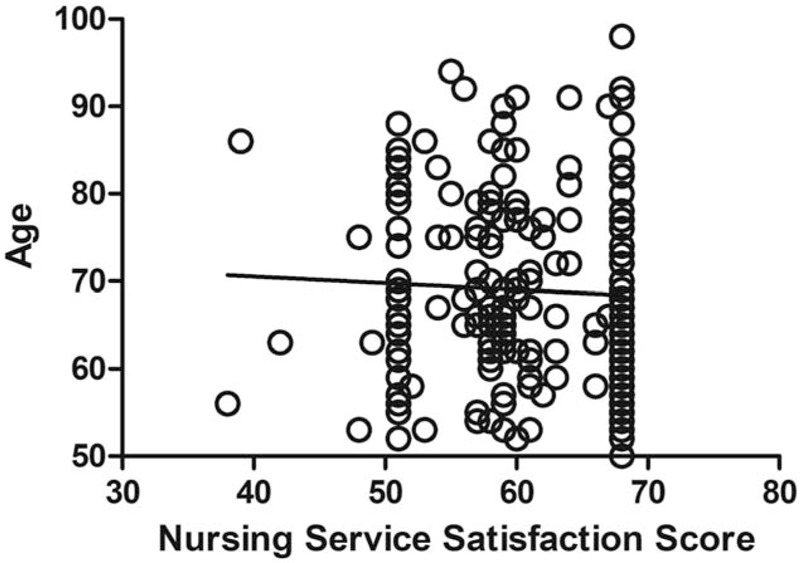
Scatter plot of Age and Nursing Service Satisfaction Score. Pearson correlation coefficient (r) = -0.0210, P = .77.
Table 3.
Positivity rate in each AD8 subitem of AD8 ≥ 2 or AD8 < 2 participants.

Table 4.
Nursing service satisfaction score in AD8 ≥ 2 group.

4. Discussion
In this study, we recruited a total of 345 participants ≥50 years old in five different wards (Table 1). There were more female patients in orthopedic ward, which might be caused by higher incidence of osteoporosis in female population. Old age is associated with AD8 ≥2 and female gender confers a borderline high risk of dementia (Table 2). Only 16.5% of AD8 ≥2 participants, or 4.4% of all participants, had been previously diagnosed with dementia; most of them had Alzheimer's dementia. This finding implied that unmet timely diagnosis among high risk participants (AD8 ≥ 2 group). In addition, the results also showed higher AD8-positive rate (26.4%) than AD8 screening in the community. A study in Taiwan screened 2,171 participants, and the overall positive rate of AD8 ≥2 was 13.6%.[12] In another community-based screening study in a rural region of Taiwan, the positive rate with AD8 ≥ 2 was only 8.6% in 30,164 participants.[19] The elderly in-patients should confer more established risk factors for cognitive dysfunction, including advanced age, chronic systemic diseases such as diabetes mellitus, hypertension, dyslipidemia, and chronic renal disease, etc. Cerebral vascular diseases also could worsen cognitive performance. The frequency of dementia among in-patients varied in different prior studies according to the methods used and populations. A study of 21,251 patients aged ≥60 from the database of Johns Hopkins Hospital showed age-dependent prevalence of dementia (ICD-9-CM code indicative of any form of Dementia) among discharged patients (age 60–64, prevalence = 2.6%; age ≥85, prevalence = 8.9%). Though the prevalence of dementia increased with ageing in the above study, underestimation of the dementia population size was possible because no real screening tests were applied during hospital stay in that study.[20] In this study, it is highlighted that AD8 ≥2 rates were relatively high in Chest Medicine and Neurology wards. (Table 1) A study of 1,424 patients with obstructive airway disease (mean age of the men 79 ± 8 years and women 81 ± 8 years) showed 30% with mild and 22% with moderate to severe dementia as defined by the Global Deterioration Scale.[20] The prevalence is close to our finding in the Chest Medicine ward, 41%. In the Neurology ward, ischemic stroke is the most common cause of admission. It is well documented that Alzheimer's dementia as well as vascular dementia, the 2 most prevalent dementia etiologies, share many common risk factors and that may explain why AD8 ≥2 rate was highest in the neurology ward.[21] In summary, using AD8 in hospital based screening showed significantly higher positive rate and that indicated better cost-effectiveness than community based screening. The further confirmation of diagnosis requires detailed medical history as well as cognitive assessment, continuous follow-up and sometimes advanced imaging and biomarkers survey, and hospitals should offer better approaches with enough diagnostic facilities.
Among the subitems of AD8, we found that AD8-3: repeats questions, stories, or statements, and AD8-8: consistent problems with thinking and/or memory were top 2 rated questions which reached 17.4% and 35.1% positive rate respectively (Table 3). This result was compatible with another study which showed AD8-3 and AD8-8 to be the most frequently positive in northern Taiwan. In that study, the authors illustrated that the population in northern or urban Taiwan have higher daily cost of living causing residents more anxious and stressed, which might lead to memory problem and to repeat questions, stories, or statements.[12] Significant higher positive rate of each AD8 subitem was observed among the AD8 ≥ 2 group, which indicated that every each functional domain decline in AD8 was more prevalent in AD8≥ 2 group. This finding reminds us not to overlook changes of any AD8 subitem, such as AD8-2: reduced interest in hobbies/activities or AD8-5: forgetting correct month or year; both which people may usually regard as normal ageing.
Nursing Service Satisfaction Questionnaire was developed to evaluate care quality through feedback from patients and their family and it is routinely used to evaluate nursing care quality in many hospitals in Taiwan. The AD8 ≥ 2 group had significantly lower Nursing Service Satisfaction Questionnaire score compared with AD8 < 2 group (56.99 ± 0.9 vs 60.55 ± 0.5, P < .01) (Table 2). Nursing Service Satisfaction Questionnaire score was negatively correlated with AD8 score (Fig. 1). Both results indicated that cognitive dysfunction could be an important factor for nursing care quality. The age was significant older in AD8 ≥ 2 group (Table 2), which was compatible with age-dependent prevalence of cognitive dysfunction.[15] However, there was no significant correlation between Nursing Service Satisfaction Questionnaire score and age in our study (Pearson correlation coefficient (r) = −0.0210, P = .77). It indicates that age was not the critical variant for nursing care quality. The participants with AD8 ≥ 2 suffered from more cognitive dysfunction and related disturbance of daily activity. Cognitive dysfunction could become an obstacle on communication and interfere with medical treatment and nursing care.[22] The subitems of the Nursing Service Satisfaction Questionnaire with relatively lower scores in AD8 ≥ 2 group were 02: (Staff) introduces herself (himself) to you, 03: (Staff) introduces the environment and hospital regulations to you, 04: (Staff) keep their promises and respond to it; if not, they respond actively and explain the reason and 16: (Staff) maintenance of the tranquility of the ward (Table 4). The context of these subitems is mostly about communication between patients, care-givers and nurses. The Alzheimer's Society identified key areas of dissatisfaction for carers relating to nurses are not recognizing or understanding dementia; and key areas of concern by nursing staff were managing difficult unpredictable behaviors and communicating. That shows the quality of dementia care and care-givers’ satisfaction in the hospital both depend on better communication and mutual understanding.[23] A study which examined carers’ views and experiences of the delivery of patient care for people with dementia in an acute general hospital concluded that nurse leaders play an important role in creating conditions and fostering a culture that enables and rewards the delivery of “relationship-centered” care for dementia population.[24] That highlighted the importance of interactions amongst people again. Hospitalization is a great challenge to people in illness, especially those with cognitive dysfunction. If caring system does not pay right attention to improve communication, the patient might feel largely frustrated. Thus, communication barriers made reciprocal negative effects and less availability to good nursing care, eventually leading to lower Nursing Service Satisfaction Questionnaire score. The consequence is not surprisingly a poor-quality experience for the patients, care-givers and nurses.[5,6]
This study had a number of limitations. First, this study did not involve in-patients by really randomization. Only the patients from acute wards of five departments were included. The characteristics of these 5 specialty wards are different, therefore the final recruitment numbers are different. This unbalanced sampling manner might bias the representation of whole hospitalized individuals. Second, clinical entities of patients were diverse including different diseases with varies severity, which could influence functional capacity to perform activity of daily living. The disability could possibly be misinterpreted as a consequence of cognitive impairment which in fact caused by underlying diseases. However, according to AD8 guideline, a response of “Yes, a change” indicates that there has been a change in the last several years caused by cognitive problems. Thus, acute physical illness which leads to hospitalization can be differentiated through onset timing of functional changes. Third, we only used AD8 without imaging data or other neuropsychological tests to confirm the diagnosis. Although, AD8 has been validated as a reliable tool with high sensitivity and specificity in screening cognitive dysfunction, further study is needed to verify the results by performance-based tools. Final, whether AD8 ≥ 2 group had more comorbidity or severer diseases which could result in complexity of care and poor outcome, then further reduced the nursing service satisfaction in addition to cognitive dysfunction itself is uncertain. Some of our participants had memory problems. In our study, it was not easy to conclude whether memory problem alone had positive or negative effect on the perception of the care provided by the nursing staff. Further study will be necessary to clarify how comorbidity could affect nursing service satisfaction among cognitive dysfunction patients.
In conclusion, hospital-based cognitive dysfunction screening using AD8 showed significantly higher positive rate than community based screening which should draw more attention and also indicated hospital-based screening with better cost-effectiveness for dementia screening. AD8 ≥ 2 participants had significantly lower Nursing Service Satisfaction Questionnaire score, suggesting cognitive dysfunction could influence medical care quality during hospitalization. The reasons could be owing to communication barriers with reciprocal effect and lack of care skills for cognitive dysfunction patients. Awareness of cognitive dysfunction among in-patients and early identifying them might help the hospitals to provide more dementia-friendly medical service and thus improve care quality.
Author contributions
Conceptualization: Hsun-Hua Lee.
Data curation: Yao-Tung Lee.
Formal analysis: Li-Kai Huang.
Investigation: Yi-Chun Kuan.
Methodology: Jui-Chen Tsai, Yi-Chun Kuan.
Resources: Yao-Tung Lee.
Software: Shu-Ping Chao.
Supervision: Jui-Chen Tsai, Shu-Ping Chao, Chaur-Jong Hu.
Writing – original draft: Li-Kai Huang.
Writing – review & editing: Chia-Pei Lin, Chaur-Jong Hu.
Footnotes
Abbreviations: AD8 = Ascertain Dementia 8, AUC = area under curve.
How to cite this article: Huang LK, Tsai JC, Lee HH, Kuan YC, Lee YT, Lin CP, Chao SP, Hu CJ. Dementia screening for elderly in-patients and its association with nursing care satisfaction-an observational study. Medicine. 2020;99:2(e18741).
All procedures were approved by the Taipei Medical University Hospital Institutional Review Board.
This study is sponsored by the research grant of Shuang Ho Hospital, Taipei Medical University, New Taipei City, Taiwan (104-SHH-HHC-001).
The authors have no conflicts of interest to declare.
References
- [1].“Dementia.” World Health Organization, World Health Organization, 2017, www.who.int/news-room/fact-sheets/detail/dementia Accessed November 01, 2019. [Google Scholar]
- [2].Sun Y, Lee H-J, Yang S-C, et al. A nationwide survey of mild cognitive impairment and dementia, including very mild dementia, in Taiwan. PloS One 2014;9:e100303. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Motzek T, Junge M, Marquardt G. Impact of dementia on length of stay and costs in acute care hospitals. Z Gerontol Geriatr 2017;50:59–66. [DOI] [PubMed] [Google Scholar]
- [4].Connolly S, O'Shea E. The impact of dementia on length of stay in acute hospitals in Ireland. Dementia (London, England) 2015;14:650–8. [DOI] [PubMed] [Google Scholar]
- [5].Chen H, Li M, Wang J, et al. Factors influencing inpatients’ satisfaction with hospitalization service in public hospitals in Shanghai, People's Republic of China. Patient Prefer Adherence 2016;10:469. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].Digby R, Lee S, Williams A. The experience of people with dementia and nurses in hospital: an integrative review. J Clin Nurs 2017;26:1152–71. [DOI] [PubMed] [Google Scholar]
- [7].Lafortune L, Khan A, Martin S, et al. A systematic review of costs and benefits of population screening for dementia. Lancet 2013;382:S56. [Google Scholar]
- [8].Yang Y-H, Galvin JE, Morris JC, et al. Application of AD8 questionnaire to screen very mild dementia in Taiwanese. Am J Alzheimers Dis Other Demen 2011;26:134–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Shaik MA, Khoo CH, Thiagarajah AG, et al. Pilot evaluation of a dementia case finding clinical service using the informant ad8 for at-risk older adults in primary health care: a brief report. J Am Med Dir Assoc 2016;17:673.e5-.e8. [DOI] [PubMed] [Google Scholar]
- [10].Galvin JE, Roe CM, Xiong C, et al. Validity and reliability of the AD8 informant interview in dementia. Neurology 2006;67:1942–8. [DOI] [PubMed] [Google Scholar]
- [11].Galvin J, Roe C, Powlishta K, et al. The AD8: a brief informant interview to detect dementia. Neurology 2005;65:559–64. [DOI] [PubMed] [Google Scholar]
- [12].Chen C-H, Wang L-C, Ma T-C, et al. A walk-in screening of dementia in the general population in Taiwan. ScientificWorldJournal 2014;2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Sampson EL, Blanchard MR, Jones L, et al. Dementia in the acute hospital: prospective cohort study of prevalence and mortality. Br J Psychiatry 2009;195:61–6. [DOI] [PubMed] [Google Scholar]
- [14].Timmons S, Manning E, Barrett A, et al. Dementia in older people admitted to hospital: a regional multi-hospital observational study of prevalence, associations and case recognition. Age Ageing 2015;44:993–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Lyketsos CG, Sheppard J-ME, Rabins PV. Dementia in elderly persons in a general hospital. Am J Psychiatry 2000;157:704–7. [DOI] [PubMed] [Google Scholar]
- [16].Rudolph JL, Zanin NM, Jones RN, et al. Hospitalization in community-dwelling persons with Alzheimer's disease: frequency and causes. J Am Geriatr Soc 2010;58:1542–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Chen H-H, Sun F-J, Yeh T-L, et al. The diagnostic accuracy of the Ascertain Dementia 8 questionnaire for detecting cognitive impairment in primary care in the community, clinics and hospitals: a systematic review and meta-analysis. Fam Pract 2017;35:239–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Chen H-L, Tzeng W-C, Lu M-S, et al. Reliability and validity testing of the Taiwanese inpatient nursing care satisfaction scale: a pilot-study. Hu Li Za Zhi 2016;63:42. [DOI] [PubMed] [Google Scholar]
- [19].Lee SD. Taoyuan County. Potential dementia in community screening study. Research report; 2012:17-18. Available at: https://www.tycg.gov.tw/uploaddowndoc?file=infopublic/201612301625280.pdf&filedisplay=E6A183E59C92E7B8A3101E5B9B4E5BAA6E6BD9BE59CA8E5A4B1E699BAE79787E7A4BEE58D80E7AFA9E6AAA2E8A888E795ABE7A094E7A9B6E6A188E7A094E7A9B6E5A0B1E5918A.doc.pdf&flag=doc. Accessed November 01, 2019. [Google Scholar]
- [20].Constantine G, Lyketsos, Jeannie-Marie E, et al. Dementia in elderly persons in a general hospital. Am J Psychiatry 2000;157:704–7. [DOI] [PubMed] [Google Scholar]
- [21].Arvanitakis Z, Capuano AW, Leurgans SE, et al. Relation of cerebral vessel disease to Alzheimer's disease dementia and cognitive function in elderly people: a cross-sectional study. Lancet Neurol 2016;15:934–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].Yi M, Yih BS. A conversation analysis of communication between patients with dementia and their professional nurses. J Kor Acad Nurs 2006;36:1253–64. [DOI] [PubMed] [Google Scholar]
- [23].Society As. Counting the cost: Caring for people with dementia on hospital wards: Alzheimer's Society. 2009:25. Available at: https://www.alzheimers.org.uk/sites/default/files/2018-05/Counting_the_cost_report.pdf. Accessed November 01, 2019. [Google Scholar]
- [24].Nolan MR, Davies S, Brown J, et al. Beyond ‘person-centred’care: a new vision for gerontological nursing. J Clin Nurs 2004;13:45–53. [DOI] [PubMed] [Google Scholar]


