Abstract
Human immunodeficiency virus (HIV) testing is important for prevention and treatment. Ending the HIV epidemic is unattainable if significant proportions of people living with HIV remain undiagnosed, making HIV testing critical for prevention and treatment. The Centers for Disease Control and Prevention (CDC) recommends routine HIV testing for persons aged 13 to 64 years in all health care settings. This study builds on prior research by estimating the extent to which HIV testing occurs during physician office and emergency department (ED) post 2006 CDC recommendations.
We performed an unweighted and weighted cross-sectional analysis using pooled data from 2 nationally representative surveys namely National Ambulatory Medical Care Survey and National Hospital Ambulatory Medical Care Survey from 2009 to 2014. We assessed routine HIV testing trends and predictive factors in physician offices and ED using multi-stage statistical survey procedures in SAS 9.4.
HIV testing rates in physician offices increased by 105% (5.6–11.5 per 1000) over the study period. A steeper increase was observed in ED with a 191% (2.3–6.7 per 1000) increase. Odds ratio (OR) for HIV testing in physician offices were highest among ages 20 to 29 ([OR] 7.20, 99% confidence interval [CI: 4.37–11.85]), males (OR 1.34, [CI: 0.91–0.93]), African-Americans (OR 2.97, [CI: 2.05–4.31]), Hispanics (OR 1.80, [CI: 1.17–2.78]), and among visits occurring in the South (OR 2.06, [CI: 1.23–3.44]). In the ED, similar trends of higher testing odds persisted for African Americans (OR 3.44, 99% CI 2.50–4.73), Hispanics (OR 2.23, 99% CI 1.65–3.01), and Northeast (OR 2.24, 99% CI 1.10–4.54).
While progress has been made in screening, HIV testing rates remains sub-optimal for ED visits. Populations visiting the ED for routine care may suffer missed opportunities for HIV testing, which delays their entry into HIV medical care. To end the epidemic, new approaches for increasing targeted routine HIV testing for populations attending health care settings is recommended.
Keywords: emergency department, HIV testing, physician office, predictors, screening, trends
1. Introduction
Current human immunodeficiency virus/acquired immunodeficiency syndrome (HIV/AIDS) surveillance estimates show approximately 1.1 million people are living with HIV (PLWH) in America.[1] Despite widespread availability of HIV testing, about 15% of PLWH remain unaware of their infection.[2] Undiagnosed PLWH miss benefits associated with HIV diagnosis such as early linkage to HIV care, reduction in viral load, professional and personal support to help improve their overall health.[3–6] To increase the proportion of PLWH who are aware of their HIV status, receive the aforementioned benefits, and prevent further transmission, the Centers for Disease Control and Prevention (CDC) recommends routine HIV testing for persons aged 13 to 64 years using routine opt-out HIV screening in health care settings where the prevalence of undiagnosed infection is at least 0.1%.[7] Previous studies classify health encounters by undiagnosed PLWH in health care settings such as the emergency department (ED) as missed opportunities for HIV testing.[8–12]
Providers play a key role in routine HIV testing with the relationship between physician decision-making and patient behavior established in literature.[13,14] Based on this relationship, the “Eisenberg model for clinician's decision-making” was selected as the theoretical model for this study.[15] This model posits that actual clinical decisions such as HIV testing are strongly influenced by interactions between the patient, clinician, sociological, and biomedical environment.[13,15–17] Prior reservations about the viability of conducting routine HIV testing in health facilities is reduced with the development of new and successful HIV algorithms such as the rapid test-immunoflourescence and ARCHITECT-Multispot-viral load algorithms.[9,18] These point-of-care testing options make HIV testing easier.[19] However, despite these improved HIV testing technologies and after a decade of CDC recommendations, studies show disproportionate HIV testing rates remain across demographic groups, and health care settings.[6,20,21] Previous studies did not specifically account for the impact of provider relationship in HIV testing decision-making. To address this problem, we applied the Einseberg model to this study, to examine HIV screening trends among persons aged 13 to 64 years visiting physician's offices or ED between 2009 and 2014. In contrast to previous studies, facility, provider, and patient-level characteristics associated with HIV testing and trends over the 6-year period are included as important predictors.
2. Methods
2.1. Study design and data sources
We conducted a serial cross-sectional study design, using physician office and ED visits data obtained from the National Ambulatory Medical Care Survey (NAMCS) and National Hospital Ambulatory Medical Care Survey (NHAMCS) from 2009 through 2014. Both are nationally representative annual surveys that collect visit level data using a 4-stage probability sampling design from physician offices and hospitals in all 50 states and the District of Columbia. Details of these surveys are available elsewhere.[22] We included visits made by persons aged 13 to 64 years over 6 years to conform with the CDC HIV testing guidelines. Total sample size for NAMCS from 2009 to 2014 was (unweighted n = 1002,) and for NHAMCS (unweighted n = 783). We extracted data from 2009 to 2014 because distinct questions were added to the surveys in 2009 to determine whether HIV testing was provided during the visits. Unweighted visits are only provided in the tables to show the number of sample cases, because each record can represent thousands of visits.
2.2. Variables
The outcome variable for this study is a dichotomous variable defined as “HIV testing during the visit (Yes/No).” Based on Eisenberg model of clinicians’ decision making,[15] we selected patient level characteristics (age, sex, race, ethnicity, source of payment, and reason of visit) and system level characteristics (seen by physician, primary care provider, ownership of facilities, practice region, metropolitan statistical area, and episode of care) as explanatory variables.
2.3. Statistical analysis
Sample weights accounting for selection probability, nonresponse and ratio adjustments for each year's total sample size were applied to generate robust national estimates of both ED and physician office visits. Variables with unweighted values less than 30 were excluded to ensure reliable estimates. Adjusted sample weights, strata, and primary sampling design units provided by both NAMCS and NHAMCS were applied using multi-stage survey methods. Statistical procedures used include PROC SURVEYFREQ, SURVEYMEANS, and SURVEYLOGISTIC. We calculated proportions with corresponding confidence intervals (CIs) for all years using the total visits as denominator. National rates were calculated using the following equation[23]:
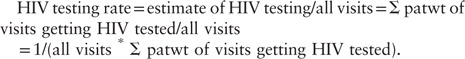 |
We used Student t tests and Pearson Chi-square statistics to assess differences and associations between proportions during bivariate analysis. We used multivariable survey logistic regression to evaluate trends in HIV testing associated with explanatory variables across both physician offices and EDs separately. Odds ratios (ORs), 99% CIs, and significance level (P < .01 was considered as significant to account for large weighted sample sizes) for each factor are reported. No multiple comparison adjustments were made given the exploratory nature of this study. All analyses were performed using SAS 9.4. The study was approved as exempt by the University of South Carolina Institutional Review Board (#Pro00071226).
3. Results
3.1. Trends in medical visits and HIV testing rates
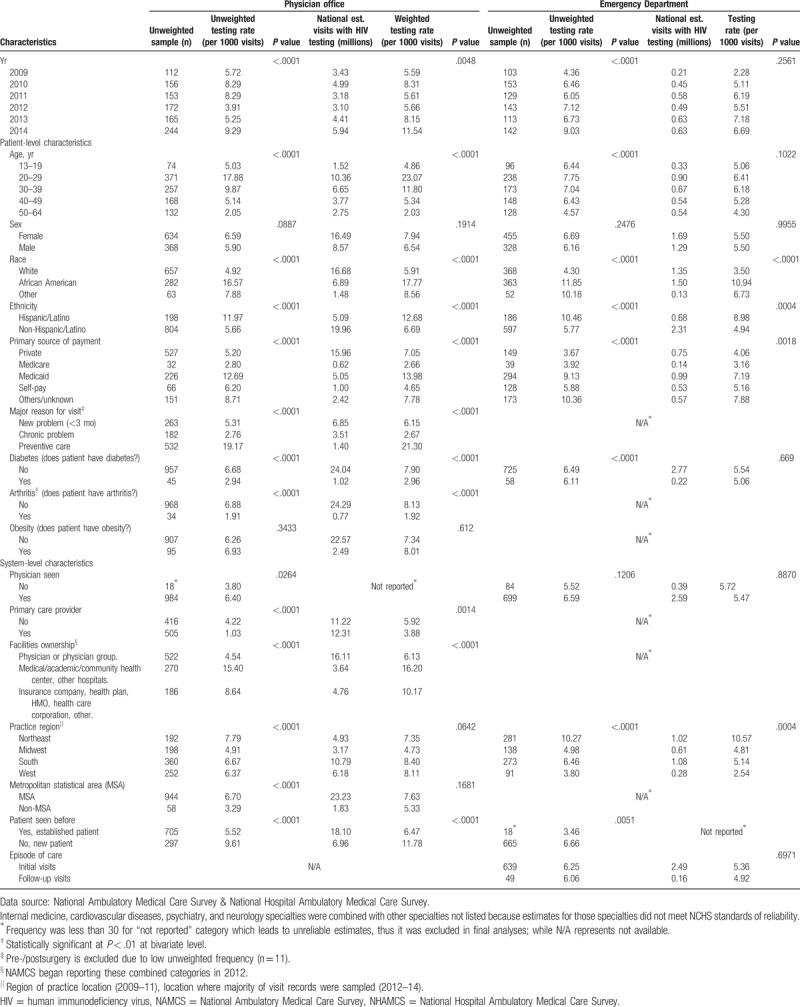
Average annual number of visits to the physician's office decreased from 3.38 (2009) to 2.77 (2014) visits per person representing a 18% decrease over 6 years (Table 1). National HIV testing rates in both the ED and physician offices trended upwards as shown in Figure 1. Unexplained dips in HIV testing rates were observed for physician offices in 2011 and for ED visits in 2012. Table 2 shows national weighted and unweighted estimates of HIV testing rates in physician offices and EDs across different provider, patient, and facility level characteristics. Unweighted estimates mostly mirrored weighted estimates except in a few instances. The largest differences in HIV testing rates across various characteristics occurred during physician office visits. HIV testing rates fluctuated annually but were highest in physician offices in 2014 (11.54 per 1000 visits). HIV testing rates in physician offices were highest among those aged 20 to 29 (23.07 per 1000), African Americans (17.77 per 1000), Hispanics (12.68 per 1000), and Medicaid beneficiaries (13.98 per 1000). Similarly, African Americans (10.94 per 1000) and Hispanics (8.98 per 1000) had the highest rates of HIV testing during ED visits. For physician office visits, HIV testing rates were higher for new patients (11.78 per 1000) compared to established patients. Conversely, HIV testing rates were lowest among patients visiting primary care providers (3.88 per 1000), facilities owned by physician groups (6.13 per 1000) or making visits in nonmetropolitan areas (5.33 per 1000).
Table 1.
Average annual number of visits to physician offices and emergency departments, 2009 to 2014.
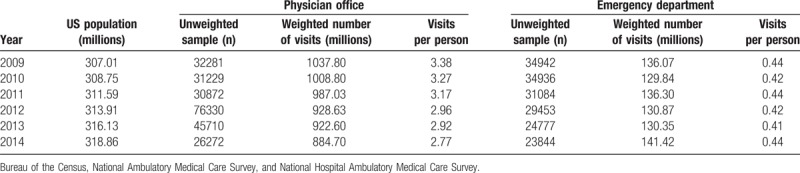
Figure 1.
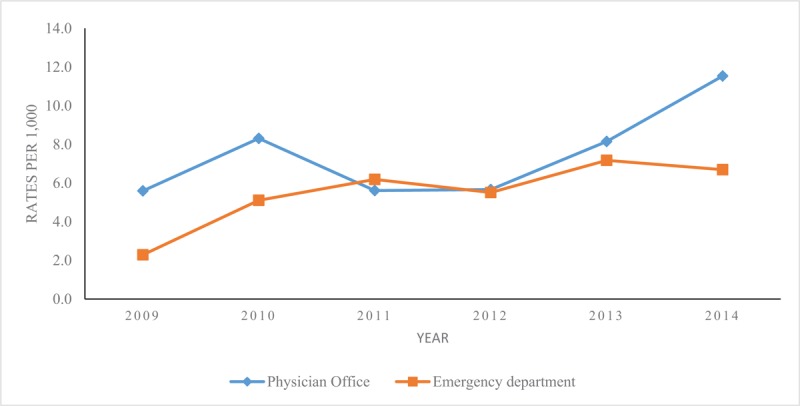
HIV screening rates in physician offices and emergency departments in the US, 2009 to 2014. Plots represent national HIV testing rate per 1000 occurring in Physician Offices (National Ambulatory Medical Care Survey [NAMCS] data) and Emergency Departments (National Hospital Ambulatory Medical Care Survey [NHAMCS] data), from 2009 to 2014. HIV testing rate was calculated using the equation below: Estimate of HIV testing/all visits = Σpatwt of visits getting HIV tested/all visits = 1/(all visits ∗Σ patwt of visits getting HIV tested). HIV = human immunodeficiency virus.
Table 2.
National estimates and rates of HIV testing in physician offices and emergency departments by patient and facility level factors, NAMCS and NHAMCS pooled data 2009 to 2014.
3.2. Predictors of HIV testing
3.2.1. Patient-level characteristics
Table 3 displays the unweighted and weighted factors associated with HIV testing in physician offices. Four patient level characteristics – age, race and ethnicity, sex and reason for visit were significantly associated with HIV testing. Individuals aged 20 to 29 years had the highest odds for testing (OR 7.20, 99% CI 4.37–11.85) compared to the elderly age group (50–64 years). Odds for testing was higher for males (OR 1.34, 99% CI 0.91–0.93) compared to females. Patients visiting for preventive care had higher odds for testing (OR 5.29, 99% CI 3.25–8.61) compared to those with a chronic problem. Sex-age interaction was not statistically significant for physician office/ED visits; hence data were not displayed in Tables 3 and 4.
Table 3.
Predictors of HIV testing among patients attending physician offices, pooled NAMCS data 2009 to 2014.
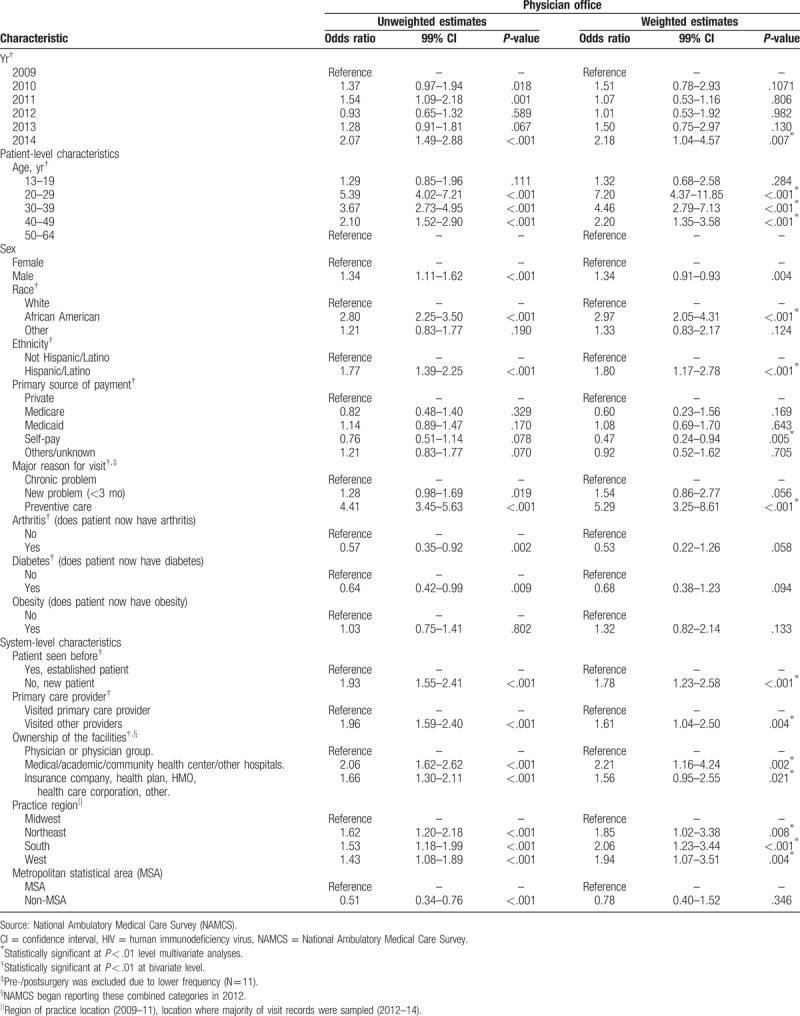
Table 4.
Predictors of HIV testing in emergency departments, pooled NHAMCS data 2009 to 2014.
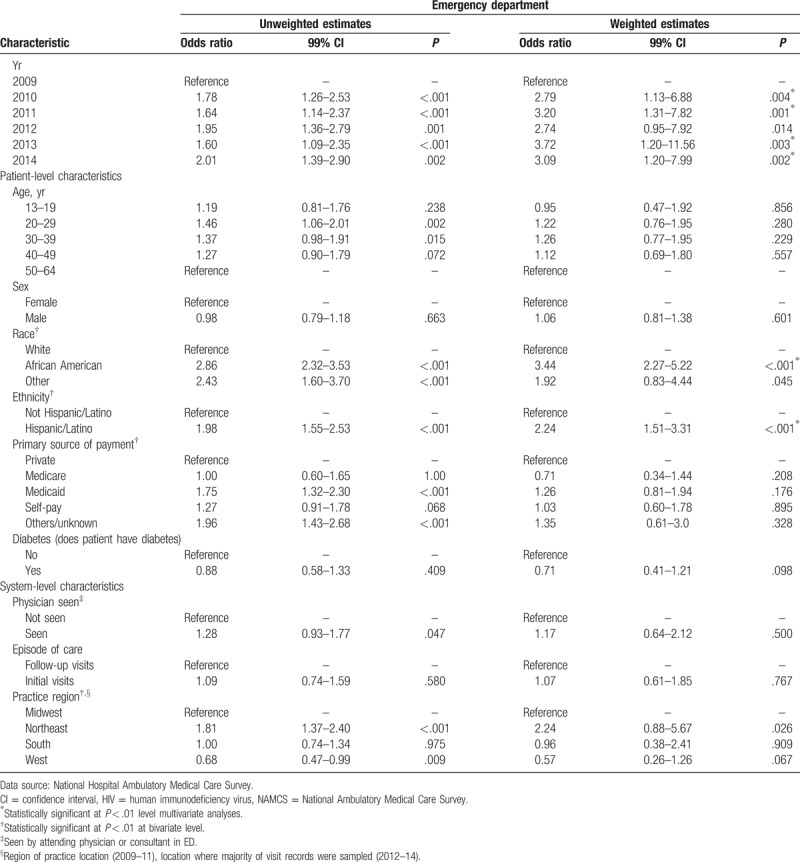
By race, African Americans (OR 2.97, 99% CI 2.05–4.31) and Hispanics (OR 1.80, 99% CI 1.17–2.78) had higher odds of receiving an HIV test during an office visit than Whites. Self-pay individuals (OR 0.47, 99% CI 0.24–0.94) had lower odds of HIV testing compared with the privately insured. Patients visiting for preventive care had higher odds for testing (OR 5.29, 95% CI 3.25–8.61) compared to those with a chronic problem. For ED visits, only 2 patient-level variables – race and ethnicity showed significant associations with HIV testing (Table 4). African Americans (OR 3.44, 99% CI 2.27–5.22) and Hispanics (OR 2.24, 99% CI 1.51–3.31) had higher odds of getting tested compared to non-Hispanic Whites.
3.2.2. System-level characteristics
All 3 system-level characteristics (usual source of care captured based on new/follow-up visit determination; primary care provider visited and facility ownership) were significantly associated with HIV testing during physician office visits (Table 3). New patients (OR 1.78, 99% CI 1.23–2.58) making a physician office visit had higher odds for HIV testing compared to established patients. Similarly, patients visiting nonprimary care providers or facilities (OR 1.61, 99% CI 1.04–2.50) had higher odds of HIV testing. Patients visiting medical/academic/community health center/other hospitals (OR 2.21, 99% CI 1.16–4.24) had higher odds of HIV testing compared to patients visiting physician group run facilities. By region, the odds of HIV testing occurring during a physician office visit was highest in the South (OR 2.06, 99% CI 1.23–3.44).
4. Discussion
This study investigated HIV testing trends across patient and system level characteristics at the physician office and ED. In agreement with prior studies,[6,21] overall U.S. HIV testing increased from 2009 to 2014.
4.1. Patient-level characteristics
Consistent with previous studies, African-Americans and Hispanics remained most likely to test for HIV in both physician offices and ED.[20,21] African Americans and Hispanics have increased risk of HIV infection, and account for most new HIV diagnoses.[24,25] However, HIV testing was most likely to occur in the ED for both African-Americans and Hispanics. This agrees with recent study findings showing minority Medicaid recipients and the uninsured as most likely to receive HIV testing in the ED.[21] One factor predicting where minority populations receive HIV testing is a lack of a usual source of care. Race, mistrust of the health system, segregation in primary care based on socioeconomic status are factors influencing minorities use of the ED for routine care and by extension HIV testing.[26] In contrast to the literature, this study found the highest likelihood for HIV testing by age occurring among those aged 20 to 29 in physician offices. This contradicts previous study findings of no difference in HIV testing by age.[5] The finding that visits to a primary care provider had lower odds of getting HIV tested is expected. Primary care providers often have in-depth knowledge of their patients, which enables them to assess risk and determine if a patient needs HIV testing. As a result, providers may be less prone to provide/recommend HIV screening during such visits. In contrast, a previous study that analyzed NAMCS survey focusing on men aged 15 to 25 years reported that visits to the primary care physician had a higher likelihood for HIV testing in physician offices.[3]
Findings from previous literature associated with the influence of primary payment source on HIV testing are mixed. Some of the studies support our finding of no significant effect on HIV testing for most payment sources except for self-pay patients who had a lesser likelihood of HIV testing.[5] Other studies reported the opposite, with Medicaid recipients reported to test more often in both physician offices and EDs.[21] Carter et al did not find any variation in HIV testing among men aged 15 to 25 years in physician office visits based on payment type.[27]
4.2. System-level characteristics
In general, patients visiting medical, academic, community health centers, or other hospitals regulated by insurance company, health plan, Health Maintenance Organizations (HMO) or health corporation had higher odds for HIV testing. A prior study established that patient-provider interaction plays a leading role in subsequent decision making of the physician.[28] This study found that established patients had significantly lower odds of getting tested for HIV while visiting physician offices, but no significant variations were reported for ED visits. Lower testing rates for established patients are plausible because in most cases there is ongoing physician-patient engagement and as well as an established medical history. Another important systems-level characteristic is the provider's interaction with the health system. A prior study demonstrated that provider decision-making is largely affected by the type of facilities, region of the facilities, and whether the facility is in metro or non-metro areas.[28] In this study people from the South had significantly higher odds of getting an HIV test during a physician office visit. HIV testing was higher in the Northeast region for visits to the ED and in the South for physician office visits. Findings related to the influence of region on HIV testing are mixed.[5,21,29] A recent study examining regional impact on HIV testing during patient visits supports our finding.[21] Another study conducted on ED visits did not find significant variation across geographic regions for HIV testing.[5] However two 2018 studies report on the prevalence of undiagnosed HIV in the ED, as well as the difficulties in selecting patients for screening in the ED[30,31]
Encouragingly, the likelihood of being tested for HIV increased significantly among visits to the ED as well as during preventative care visits to physician offices. The finding that the likelihood for HIV testing is higher for new patient visits in physician offices is expected. New patient visits typically include the investigation of existing chronic conditions with appropriate testing including HIV testing. But contrary to the finding of no differences by type of setting by Tai & Merchant (2014), we found HIV testing rates were not uniformed between physician offices and ED. Plausible explanations for the reason of HIV testing differs across both health care settings were not assessed during this study. Reasons provided by previous studies about failure to conduct routine HIV testing in health settings among clinicians include a lack of knowledge of the CDC's testing guidelines; belief that patients are not at risk for HIV and assuming HIV testing is the responsibility of other health care professionals.[20]
In addition, lack of awareness and misconceptions regarding HIV testing by physicians and the patients, barriers at facility and legislative levels, costs associated with testing are major barriers affecting the CDC's recommendation.[30] Additional explanations for these variations include the following. First, full adoption of the 2006 CDC guidelines takes time and implementation may differ by health facility. There could also be facility and legislative level barriers, along with lack of awareness, resistance, and misconceptions regarding HIV testing by both physicians and patients.[32] Second, in the absence of a clear mandate for clinicians and health facilities to perform routine HIV screening, as well as poor communication or dissemination of the CDC guidelines, uptake in HIV testing rates may lag across health settings. Third, the lack of strategic planning and financial support to purchase and deploy portable point of care HIV testing equipment could limit uptake of HIV testing in health settings.[7] Fourth, physician behavior and reaction to the guidelines directly influence HIV testing among patients, and physicians may continue to rely on clinical presentations rather than the guidelines to recommend HIV testing. Fifth, the NAMCS and NHAMCS data may not accurately capture all HIV testing.
4.3. Study limitations
The results of this study should be considered with some limitations in mind. HIV testing rates do not reflect exact incidence rates. Incidence rates cannot be estimated since the same patients could make more than 1 visit. Information about who was offered testing and reasons why HIV testing was not performed was not collected. Patients not tested might have declined testing because of prior screening from another visit. Unrecognized sampling biases might hamper the national representativeness of the population sample, while errors in data collection might affect appropriate measure of HIV testing rates.[5,15,20] For instance, nonresponse to participate in the survey might have resulted in underestimation or overestimation of HIV testing. Moreover, sexual behavior or intravenous drug use data are absent, so estimation of HIV testing representing these factors was not possible.
5. Conclusions
The overall rates of HIV testing increased over the study period; however, increased HIV testing rates are not uniformed across different facilities and subpopulations. System level factors may play a significant role in improving HIV testing among minority populations. While our study could not investigate provider knowledge and practice, factors such as lack of time, funding constraints as well as lack of staff could impact decision to test or offer testing. The lower rates of HIV testing observed in the ED is worrisome, particularly for populations without a usual source of care. Tailored interventions for the ED may be necessary to reduce missed opportunities for HIV testing. To develop such interventions, future studies should examine factors such as reason of visit, testing history, and the reasons for offering/taking or not offering/taking HIV tests to understand both clinician and patients’ behavior appropriately. Future research should also examine which sub-populations (based on demographics and transmission risks) are more likely to get or not get tested, regardless of the health settings. In addition, future studies should also assess the knowledge, clarity and application of CDC testing guidelines among providers. Monitoring the response of health care settings, providers and patients to the CDC's HIV testing guidelines is important to achieve the goal of increasing HIV testing in the United States, and a key component of ending the epidemic. Therefore, careful and thoughtful approaches are needed for identifying HIV infections during physician and ED visits nationally.
Author contributions
Conceptualization: Bankole Olatosi
Data curation: Khairul Alam Siddiqi
Formal analysis: Bankole Olatosi, Khairul Alam Siddiqi, Donaldson Fadael Conserve
Investigation: Bankole Olatosi
Methodology: Bankole Olatosi, Khairul Alam Siddiqi
Software: Bankole Olatosi
Supervision: Bankole Olatosi, Donaldson Fadael Conserve
Writing – original draft: Bankole Olatosi, Khairul Alam Siddiqi
Writing – review and editing: Bankole Olatosi, Donaldson Fadael Conserve
Footnotes
Abbreviations: AIDS = acquired immunodeficiency syndrome, CDC = Centers for Disease Control and Prevention, CI = confidence interval, ED = emergency department, HIV = human immunodeficiency virus, HMO = health maintenance organizations, MSA = metropolitan statistical area, NAMCS = National Ambulatory Medical Care Survey, NHAMCS = National Hospital Ambulatory Medical Care Survey, OR = odds ratio, PLWH = people living with HIV.
How to cite this article: Olatosi B, Siddiqi KA, Conserve DF. Towards ending the human immunodeficiency virus epidemic in the US: State of human immunodeficiency virus screening during physician and emergency department visits, 2009 to 2014. Medicine. 2020;99:2(e18525).
The authors have no funding and conflicts of interest to disclose.
References
- [1].Centers for Disease Control and Prevention. HIV in the United States: At a Glance. 2017; Available at: https://www.cdc.gov/hiv/statistics/overview/ataglance.html. [Accessed June 29, 2017] [Google Scholar]
- [2].Centers for Disease Control Prevention. HIV Surveillance Report, 2015; vol. 27. 2016. Available at: https://www.cdc.gov/hiv/pdf/library/reports/surveillance/cdc-hiv-surveillance-report-2015-vol-27.pdf. [Google Scholar]
- [3].Agency for Healthcare Research and Quality. Connecting Underserved Patients to Primary Care After Emergency Department Visits. 2012. Available at: https://innovations.ahrq.gov/perspectives/connecting-underserved-patients-primary-care-after-emergency-department-visits. [Accessed June 12, 2017] [DOI] [PubMed] [Google Scholar]
- [4].Marks G, Crepaz N, Janssen RS. Estimating sexual transmission of HIV from persons aware and unaware that they are infected with the virus in the USA. Aids 2006;20:1447–50. [DOI] [PubMed] [Google Scholar]
- [5].Hoover JB, Tao G, Heffelfinger JD. Monitoring HIV testing at visits to emergency departments in the United States: very-low rate of HIV testing. J Acquir Immune Defic Syndr 2013;62:90–4. [DOI] [PubMed] [Google Scholar]
- [6].Johnson AS, Heitgerd J, van Koenig L, et al. Vital signs: HIV testing and diagnosis among adults-United States, 2001–2009. Morbidity Mortality Wkly Rep 2010;59:1550–5. [PubMed] [Google Scholar]
- [7].Branson BM, Handsfield HH, Lampe MA, et al. Revised recommendations for HIV testing of adults, adolescents, and pregnant women in health-care settings. MMWR Recomm Rep 2006;55:1–7. [PubMed] [Google Scholar]
- [8].Liddicoat RV, Horton NJ, Urban R, et al. Assessing missed opportunities for HIV testing in medical settings. J Gen Intern Med 2004;19:349–56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Tillison AS, Avery AK. Evaluation of the impact of routine HIV screening in primary care. J Int Assoc Providers AIDS Care 2017;16:18–22. [DOI] [PubMed] [Google Scholar]
- [10].Geren KI, Lovecchio F, Knight J, et al. Identification of acute HIV infection using fourth-generation testing in an opt-out emergency department screening program. Ann Emerg Med 2014;64:537–46. [DOI] [PubMed] [Google Scholar]
- [11].Moschella PC, Hart KW, Ruffner AH, et al. Prevalence of undiagnosed acute and chronic HIV in a lower-prevalence urban emergency department. Am J Public Health 2014;104:1695–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Signer D, Peterson S, Hsieh Y-H, et al. Scaling up HIV testing in an academic emergency department: an integrated testing model with rapid fourth-generation and point-of-care testing. Public Health Rep 2016;131: 1_suppl: 82–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Kaplan SH, Gandek B, Greenfield S, et al. Patient and visit characteristics related to physicians’ participatory decision-making style: results from the medical outcomes study. Med Care 1995;1176–87. [DOI] [PubMed] [Google Scholar]
- [14].Menear M, Garvelink MM, Adekpedjou R, et al. Factors associated with shared decision making among primary care physicians: Findings from a multicentre cross-sectional study. Health Expect 2017;21:212–21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Eisenberg JM. Sociologic influences on decision-making by clinicians. Ann Intern Med 1979;90:957–64. [DOI] [PubMed] [Google Scholar]
- [16].Chenneville T. HIV, confidentiality, and duty to protect: a decision-making model. Professional Psychol Res Pract 2000;31:661. [Google Scholar]
- [17].Hooper EM, Comstock LM, Goodwin JM, et al. Patient characteristics that influence physician behavior. Med Care 1982;20:630–8. [DOI] [PubMed] [Google Scholar]
- [18].Centers for disease control and prevention. National HIV testing day and new testing recommendations. MMWR Morb Mortal Wkly Rep 2014;63:537. [PMC free article] [PubMed] [Google Scholar]
- [19].Drain PK, Rousseau C. Point of care diagnostics: extending the laboratory network to reach the last mile. Curr Opin HIV AIDS 2017;12:175–81. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [20].Ham DC. Health care use and HIV testing of males aged 15–39 years in physicians’ offices—United States, 2009–2012. MMWR Morb Mortal Wkly Rep 2016;65:619–22. [DOI] [PubMed] [Google Scholar]
- [21].Tai M, Merchant RC. HIV testing in US emergency departments, outpatient ambulatory medical departments, and physician offices, 1992–2010. AIDS Care 2014;26:1105–8. [DOI] [PubMed] [Google Scholar]
- [22].Centers for Disease Control and Prevention. Questionnaires, Datasets, and Related Documentation. Retrieved August 2017. Available at: https://www.cdc.gov/nchs/ahcd/ahcd_questionnaires.htm. [Accessed June 13, 2017] [Google Scholar]
- [23].Myrick KL. Understanding and Analyzing Ambulatory Health Care Data - The NAMCS & NHAMCS. Basic Data Analysis. 2015. Available at: https://www.cdc.gov/nchs/ppt/nchs2015/Myrick_Monday_GlenEcho_A2.pdf. [Google Scholar]
- [24].Centers for Disease Control and Prevention. HIV among African Americans. 2017. Available at: https://www.cdc.gov/hiv/group/racialethnic/africanamericans/index.html. [Accessed June 29, 2017] [Google Scholar]
- [25].Centers for Disease Control and Prevention. HIV Among Hispanics/Latinos. 2017. Available at: https://www.cdc.gov/hiv/group/racialethnic/hispaniclatinos/index.html. [Accessed June 29, 2017] [Google Scholar]
- [26].Arnett M, Thorpe R, Gaskin D, et al. Race, medical mistrust, and segregation in primary care as usual source of care: findings from the exploring health disparities in integrated communities study. J Urban Health 2016;93:456–67. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [27].Carter G, Owens C, Lin H-C. HIV screening and the affordable care act. Am J Mens Health 2017;11:233–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Lin H-C, Erickson SR, Balkrishnan R. Physician prescribing patterns of innovative antidepressants in the United States: the case of MDD patients 1993–2007. Int J Psychiatry Med 2011;42:353–68. [DOI] [PubMed] [Google Scholar]
- [29].Hsieh Y-H, Rothman RE, Newman-Toker DE, et al. National estimation of rates of HIV serology testing in US emergency departments 1993–2005: baseline prior to the 2006 Centers for Disease Control and Prevention recommendations. AIDS 2008;22:2127–34. [DOI] [PubMed] [Google Scholar]
- [30].Zink JA, Fiske S, Schammel C, et al. 332 “Opt-Out” HIV screening in the emergency department discovers a high prevalence of undiagnosed HIV in the upstate of South Carolina: brief report on the conclusion of an 8-year Emergency Department Collaboration with South Carolina Department of Health and Environmental Control. Ann Emerg Med 2018;72:S131. [Google Scholar]
- [31].Haukoos JS, Lyons MS, Rothman RE. The evolving landscape of HIV screening in the emergency department. Ann Emerg Med 2018;72:54–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Rizza SA, MacGowan RJ, Purcell DW, et al. (2012, September). HIV screening in the health care setting: status, barriers, and potential solutions. In Mayo Clinic Proceedings (Vol. 87, No. 9, pp. 915–924) Elsevier. [DOI] [PMC free article] [PubMed] [Google Scholar]


