Abstract
Background:
The identification of surgical risk factors for early anterior cruciate ligament (ACL) revision is important when appropriate treatment for patients undergoing primary ACL reconstruction is selected. The purposes of this study were to determine the short-term ACL revision rate of patients undergoing primary ACL reconstruction and to identify surgical risk factors for ACL revision within 2 years of primary ACL reconstruction.
Methods:
This study was based on data collected prospectively from the Norwegian and Swedish National Knee Ligament Registries. Patients who underwent primary ACL reconstruction from 2004 through 2014 were included. We examined revisions through 2016. The relative risks (RRs) of revision ACL reconstruction dependent on graft fixation, the time interval between injury and surgical procedure, and meniscal and cartilage injury were estimated by using generalized linear models with a binomial distribution and log-link function. The outcome was set as revision ACL reconstruction during the first 2 years.
Results:
A total of 58,692 patients were assessed for eligibility; of these, 18,425 patients were included. The overall 2-year revision rate was 2.1%. Patients treated with a metal interference screw had an increased risk of ACL revision when compared with patients who were treated with other femoral fixations (RR, 1.78 [95% confidence interval (CI), 1.38 to 2.29]; p < 0.001). The use of the RIGIDFIX Cross Pin System (DePuy Synthes) entailed a lower risk of ACL revision compared with other femoral fixations (RR, 0.58 [95% CI, 0.42 to 0.82]; p = 0.0017). Patients undergoing ACL reconstruction within 3 months of the injury had an increased risk of ACL revision (RR, 2.07 [95% CI, 1.64 to 2.61]; p < 0.001).
Conclusions:
Patients undergoing ACL reconstruction within 3 months of an injury, as well as patients treated with a metal interference screw in the femur, had a significantly higher risk of ACL revision, and patients treated with the RIGIDFIX Cross Pin in the femur had a significantly lower risk of ACL revision.
Level of Evidence:
Prognostic Level II. See Instructions for Authors for a complete description of levels of evidence.
The surgical reconstruction of the anterior cruciate ligament (ACL) is a procedure that is performed to improve knee stability and function. The surgical technique is well established, although many aspects are still progressing steadily1,2. Previous studies have shown that most reruptures and ACL revisions occur within 2 years of the primary ACL reconstruction3. The timing of ACL reconstruction is of interest, with recent studies suggesting that patients should undertake physical therapy for at least 3 months before a decision could be made with regard to the best treatment4-6.
Factors that may influence the risk of graft failure include technical errors, graft choice, preoperative and postoperative rehabilitation7-9, younger age10,11, and a higher activity level12,13. Fixation methods may play a role in the risk of ACL revision, because compromised strength at the tibial or femoral fixation point may lead to incomplete graft incorporation and predispose to early failure14,15.
The optimization of tendon-to-bone or bone-to-bone healing with appropriate graft fixation in a minimally invasive way is an important aspect of treatment. Various combinations of graft and fixation methods have been used in the past16. It is important to evaluate currently used fixation methods at the same time as new alternatives are introduced.
Another frequently discussed risk factor for ACL revision is the timing of an ACL reconstruction17. Theoretically, early stabilization of the knee joint may be beneficial for the early restoration of knee kinematics and rehabilitation to minimize the risk of further intra-articular injuries18,19, and patients with swelling or elevated inflammatory markers are less likely to be treated with early reconstruction. Previous studies have been unable to identify differences in the risk of ACL revision20 when comparing early ACL reconstruction with late reconstruction21, although, from a social health perspective, it is possibly more cost-effective to perform the ACL reconstruction early, depending on health-care infrastructure22. Previous registry studies23,24 have identified cartilage damage as a predictor of the risk of ACL revision. The menisci are important for knee stability, and residual laxity caused by a meniscal injury after ACL reconstruction may increase the risk that patients will require an ACL revision25.
The aims of this study were to determine the short-term ACL revision rate of patients undergoing primary ACL reconstruction and to identify risk factors for early ACL revision. We hypothesized that there would be no difference in the risk of 2-year revision dependent on surgical timing, fixation methods used, or concomitant intra-articular injuries at the time of primary ACL reconstruction.
Materials and Methods
Patients
Data were requested and were acquired from the Norwegian National Knee Ligament Registry (NKLR) and the Swedish National Knee Ligament Registry (SNKLR). The data included patients registered for primary ACL reconstruction from Norway (starting in 2004) or Sweden (starting in 2005) until December 31, 2016. Eligible patients had undergone ACL reconstruction with either hamstring tendon autografts or patellar tendon autografts and were between 13 and 59 years of age at the time of the primary ACL reconstruction. Patients with an unknown graft diameter, those who underwent contralateral ACL reconstruction, and those who had sustained a concomitant fracture or vascular or other ligament damage were excluded.
The Norwegian and Swedish National Knee Ligament Registries
The NKLR was initiated in 2004 and the SNKLR was initiated in 2005 to provide feedback to surgeons and hospitals, to identify surgical procedures with superior and inferior outcomes, and to prospectively collect patient-reported outcomes26. Patient demographic and surgical characteristics in the Scandinavian registries are comparable with those in other settings27.
The estimated coverage of the registries for primary ACL reconstruction is >90% in Sweden28 and 86% in Norway29 and is in line with those in other comparable ACL registries27. Data relating to the surgical procedures are documented by the operating surgeons, and patient-reported outcome data are provided by patients in both national registries. The databases have been described in previous publications30-32.
Registration was performed on a voluntary basis in both countries. No written consent is required for participation in national registry databases in Sweden26. A written informed consent is required from all patients in Norway, prior to inclusion. Investigators only had access to unidentifiable patient data. Data acquired from the NKLR were treated according to Norwegian legislation30.
Variables
The following 5 variables were investigated: femoral graft fixation, tibial graft fixation, the time interval between the injury and the surgical procedure, and the presence of a meniscal injury and a cartilage injury. Femoral fixation was classified into cortical fixation (for example, ENDOBUTTON [Smith & Nephew], TightRope [Arthrex], ToggleLoc [Zimmer Biomet]), and RIGIDFIX Cross Pin System (DePuy Synthes), metal interference screw, and bioabsorbable interference screw. Tibial fixation was classified into cortical fixation, post fixation, RIGIDFIX Cross Pin, metal interference screw, and bioabsorbable interference screw. The timing of the surgical procedure was analyzed for all grafts and separately for hamstring tendon autografts and patellar tendon autografts.
All registered injuries to cartilage or menisci were investigated, but no attempt was made to classify the severity or location of the injuries.
Outcome Measurements
The primary outcome of this study was set as the 2-year cumulative incidence of ACL revision surgical procedures, which were defined as ipsilateral ACL reconstruction within 2 years of the primary ACL reconstruction. The patients were followed for 2 years or until revision ACL was performed, whichever event occurred first.
Statistics
The data sets from the SNKLR and NKLR were merged manually, and statistical analyses were performed using the SAS System for Windows, version 9 (SAS Institute).
For categorical variables, the number and percentage are presented, and standard deviations are presented for continuous variables. The impact of surgical variables on early ACL revision surgical procedures is presented as relative risks (RRs) with 95% confidence intervals (CIs) and p values estimated by using generalized linear models with a binomial distribution and log-link function. Adjustments for known confounders were made using multivariable analysis.
All the tests were 2-sided and were conducted at the 5% significance level. Significance was defined as a 95% CI for risk estimates not including 1.00 and p < 0.05.
Results
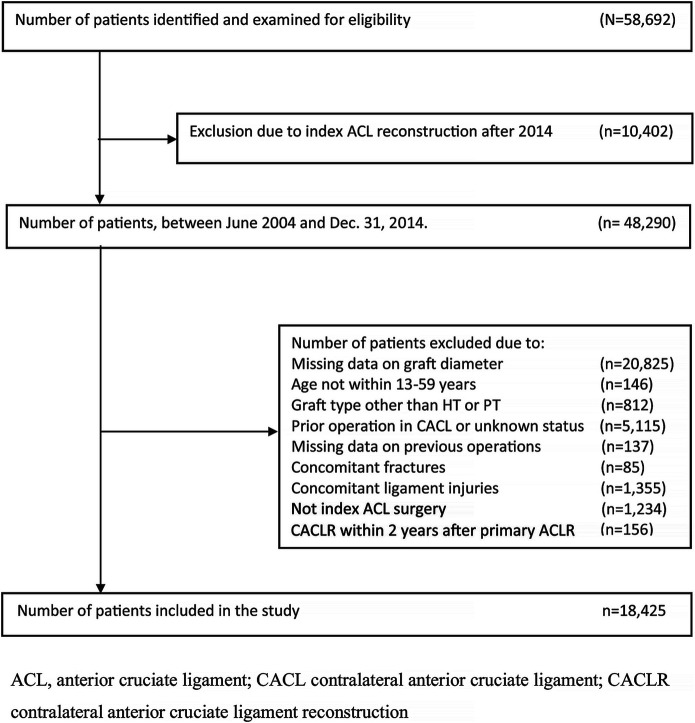
A total of 58,692 unique patients underwent primary ACL reconstruction and were registered in the SNKLR or NKLR during the study period. After an assessment of eligibility (Fig. 1), 18,425 patients (57% men) met the inclusion criteria. During the 2-year follow-up period, 391 patients (2.1%) underwent ACL revision. The number of men undergoing ACL revision within 2 years of the index ACL was 206 (2.0% of male participants), including 186 with hamstring tendon autografts and 20 with patellar tendon autografts, and 185 (2.3%) of the female participants (170 with hamstring tendon autografts and 15 with patellar tendon autografts) underwent ACL revision during the same time period (Table I). A total of 17,096 patients (93%) were treated with a hamstring tendon autograft, and 1,329 patients (7%) were treated with a patellar tendon autograft.
Fig. 1.
Flowchart showing inclusion and exclusion criteria. HT = hamstring tendon, PT = patellar tendon, and ACLR = ACL reconstruction.
TABLE I.
Baseline Demographic Data
| Total (N = 18,425) | Patellar Tendon Autograft (N = 1,329) | Hamstring Tendon Autograft (N = 17,096) | |
| Sex* (derived) | |||
| Male | 10,532 (57.2%) | 769 (57.9%) | 9,763 (57.1%) |
| Female | 7,893 (42.8%) | 560 (42.1%) | 7,333 (42.9%) |
| Age | |||
| At index ACL injury | |||
| No. of patients | 13,471 | 273 | 13,198 |
| Mean† (yr) | 24.9 ± 9.3 | 25.0 ± 8.8 | 24.9 ± 9.3 |
| Median‡ (yr) | 22.1 (6.3 to 58.9) | 22.7 (13.7 to 50.8) | 22.1 (6.3 to 58.9) |
| Interquartile range (yr) | 17.8, 29.8 | 17.9, 29.4 | 17.8, 29.8 |
| At index ACL reconstruction | |||
| No. of patients | 18,425 | 1,329 | 17,096 |
| Mean† (yr) | 26.8 ± 9.7 | 25.8 ± 8.8 | 24.9 ± 9.3 |
| Median‡ (yr) | 23.9 (13.0 to 59.9) | 22.6 (13.5 to 59.3) | 24.1 (13.0 to 59.9) |
| Interquartile range (yr) | 19.0, 33.0 | 18.5, 30.7 | 19.0, 33.2 |
| Adolescents§ | 5,663 (30.7%) | 474 (35.7%) | 5,189 (30.4%) |
| Duration of surgery | |||
| No. of patients | 14,378 | 304 | 14,074 |
| Mean† (min) | 74.4 ± 24.0 | 82.3 ± 27.5 | 74.2 ± 23.9 |
| Median‡ (min) | 70.0 (25.0 to 304.0) | 75.0 (40.0 to 184.0) | 70.0 (25.0 to 304.0) |
| Interquartile range (min) | 57.0, 90.0 | 62.5, 95.5 | 56.0, 90.0 |
| Time to surgical procedure | |||
| No. of patients | 16,774 | 1,242 | 15,532 |
| Mean† (mo) | 16.4 ± 29.8 | 14.3 ± 25.8 | 16.6 ± 30.1 |
| Median‡ (mo) | 8.0 (0.0 to 468.0) | 7.0 (0.0 to 367.0) | 8.0 (0.0 to 468.0) |
| Interquartile range (mo) | 5.0, 15.0 | 4.0, 13.0 | 5.0, 15.0 |
| Meniscal injury* | 8,656 (47.0%) | 695 (52.3%) | 7,961 (46.6%) |
| Cartilage injury* | 4,532 (24.6%) | 230 (17.3%) | 4,302 (25.2%) |
| Femoral fixation* # | |||
| Cortical fixation | 12,275 (66.9%) | 169 (12.8%) | 12,106 (71.0%) |
| RIGIDFIX Cross Pin | 2,874 (15.7%) | 51 (3.9%) | 2,823 (16.6%) |
| Metal interference screw | 2,913 (15.9%) | 885 (67.0%) | 2,028 (11.9%) |
| Bioabsorbable interference screw | 217 (1.2%) | 204 (15.5%) | 13 (0.1%) |
| Not classified | 81 (0.4%) | 11 (0.8%) | 70 (0.4%) |
| Missing | 65 | 9 | 56 |
| Tibial fixation* # | |||
| Cortical fixation | 954 (5.2%) | 14 (1.1%) | 940 (5.5%) |
| Post fixation | 1,253 (6.8%) | 5 (0.4%) | 1,248 (7.3%) |
| RIGIDFIX Cross Pin | 309 (1.7%) | 4 (0.3%) | 305 (1.8%) |
| Metal interference screw | 7,999 (43.4%) | 1,035 (77.9%) | 6,964 (40.7%) |
| Bioabsorbable interference screw | 7,697 (41.8%) | 249 (18.7%) | 7,448 (43.6%) |
| Not classified | 127 (0.7%) | 18 (1.4%) | 109 (0.6%) |
| Missing | 86 | 4 | 82 |
| Revision within 2 years** | |||
| Total | 391 (2.1%) | 35 (9.0%) | 356 (91.0%) |
| Male | 206 (1.1%) | 20 (9.7%) | 186 (90.3%) |
| Female | 185 (1.0%) | 15 (8.1%) | 170 (91.9%) |
The values are given as the number of patients, with the percentage in parentheses.
The values are given as the mean and the standard deviation.
The values are given as the median, with the range in parentheses.
Adolescents are 13 to 19 years of age.
The percentages in this section were based on the number of patients with available data.
The values are given as the number of patients, with the row percentage in parentheses for the subgroups.
Graft Fixation
Femoral Graft Fixation
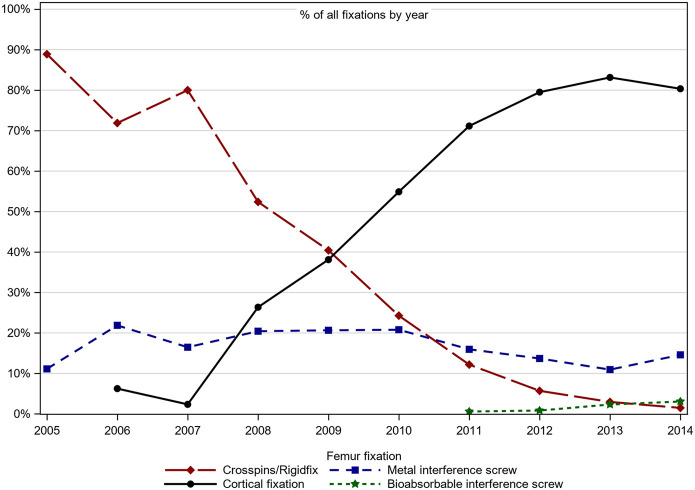
During the period from 2004 to 2009, the RIGIDFIX Cross Pin was the most commonly used implant for femoral fixation, and the use of cortical fixation increased during the latter half of the study period, reaching its peak in 2013 with >80% usage (Fig. 2).
Fig. 2.
Trends for femoral fixation during the study period.
The most commonly used fixations in the femur were cortical fixation (n = 12,275), followed by a metal interference screw (n = 2,913) and RIGIDFIX Cross Pin (n = 2,874). These 3 methods accounted for a combined total of 98% of cases. Patients treated with a metal interference screw had an increased risk of 2-year ACL revision when compared with patients treated with all other graft fixations in the femur (RR, 1.78 [95% CI, 1.38 to 2.29]; p < 0.001). Patients treated with the RIGIDFIX Cross Pin had a lower risk of early ACL revision when compared with patients treated with other fixations in the femur (RR, 0.58 [95% CI, 0.42 to 0.82]; p = 0.0017) (Table II).
TABLE II.
Femoral Graft Fixation: Incidence of Revision Surgical Procedures Within 2 Years After Primary Reconstruction
| Femoral Graft Fixation Technique | Incidence Comparison with All Other Techniques (%) | Unadjusted | Adjusted* | ||
| RR† | P Value | RR† | P Value | ||
| Cortical fixation | 1.98 vs. 2.43 | 0.81 (0.67 to 1.00) | 0.046 | 0.80 (0.64 to 1.00) | 0.053 |
| RIGIDFIX Cross Pin | 1.53 vs. 2.24 | 0.68 (0.50 to 0.93) | 0.015 | 0.66 (0.47 to 0.91) | 0.0013 |
| Metal interference screw | 3.36 vs. 1.90 | 1.77 (1.42 to 2.22) | <0.001 | 1.95 (1.53 to 2.50) | <0.001 |
| Bioabsorbable interference screw | 1.38 vs. 2.14 | 0.65 (0.21 to 2.00) | 0.44 | 0.50 (0.15 to 1.61) | 0.24 |
The techniques were adjusted for age, graft type, diameter, interaction of graft × diameter, tibial fixation, and concomitant meniscal injury.
The values are given as the RR, with the 95% CI in parentheses.
Tibial Graft Fixation
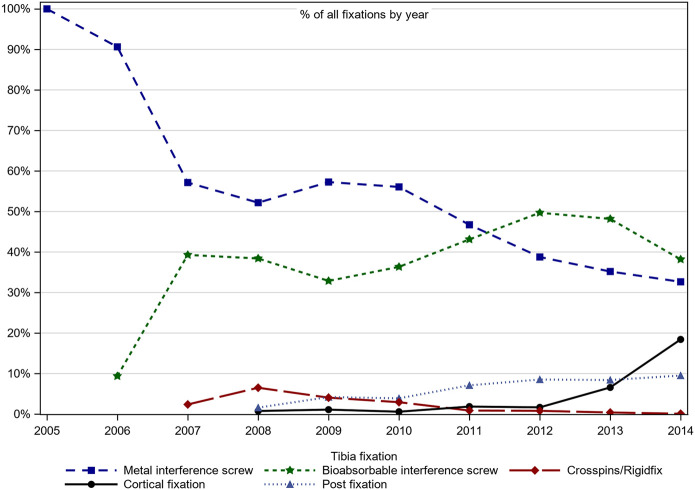
The temporal trends for tibial graft fixation are presented in Figure 3. From the beginning of the registration and until 2010, a metal interference screw was the treatment of choice for femoral fixation, while the use of a bioabsorbable interference screw increased considerably after 2007.
Fig. 3.
Trends for tibial fixation during the study period.
During the study period, the most common choice of graft fixation in the tibia was a metal interference screw (n = 7,999), and a bioabsorbable interference screw (n = 7,697) and post fixation (n = 1,253) were the other large groups of graft fixation in the tibia. When the early risk of ACL revision for tibial fixation was compared, there was no difference between the tibial fixation categories (Table III).
TABLE III.
Tibial Graft Fixation: Incidence of Revision Surgical Procedures Within 2 Years After Primary Reconstruction
| Tibial Fixation Technique | Incidence Comparison with All Other Techniques (%) | Unadjusted | Adjusted* | ||
| RR† | P Value | RR† | P Value | ||
| Cortical fixation | 1.78 vs. 2.15 | 0.83 (0.51 to 1.34) | 0.44 | 0.90 (0.55 to 1.47) | 0.68 |
| Post fixation | 2.00 vs. 2.14 | 0.93 (0.62 to 1.39) | 0.73 | 0.92 (0.60 to 1.41) | 0.70 |
| RIGIDFIX Cross Pin | 1.62 vs. 2.14 | 0.76 (0.32 to 1.81) | 0.53 | 0.97 (0.39 to 2.42) | 0.95 |
| Metal interference screw | 2.31 vs. 1.99 | 1.16 (0.95 to 1.41) | 0.14 | 1.20 (0.98 to 1.46) | 0.08 |
| Bioabsorbable interference screw | 2.04 vs. 2.20 | 0.93 (0.76 to 1.13) | 0.46 | 0.97 (0.79 to 1.20) | 0.78 |
These values were adjusted for age, graft type, diameter, interaction of graft × diameter, femoral fixation, and concomitant meniscal injury.
The values are given as the RR, with the 95% CI in parentheses.
Timing of the Surgical Procedures
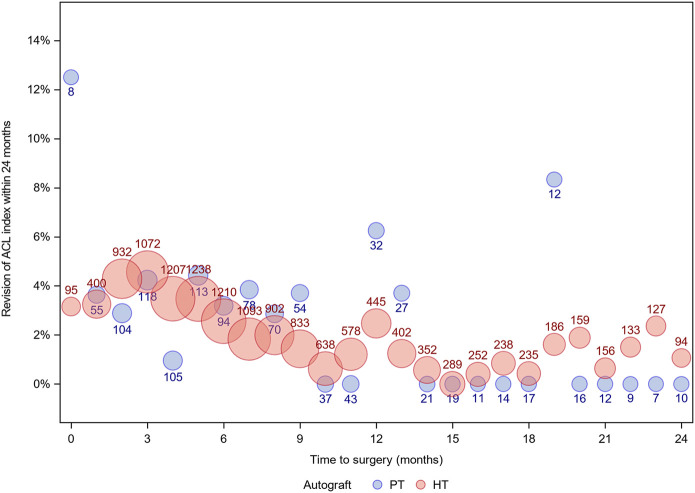
Data with regard to the timing of ACL reconstruction were available for 93.5% of patients treated with patellar tendon autografts and 90.9% of patients treated with hamstring tendon autografts. Patients who were treated with hamstring tendon autografts (Table IV) had a significantly increased risk (p < 0.001) of 2-year ACL revision when the operation took place within 3 months of the ACL injury compared with patients who were treated later. The risk of 2-year ACL revision was also increased for patients who were treated earlier than 6 months, 1 year, and 2 years after the ACL injury compared with patients who were treated after the subsequent time intervals.
TABLE IV.
Hamstring Tendon Autografts: Incidence of Revision Surgical Procedures Within 2 Years After Primary Reconstruction and the Timing of Surgical Procedures
| Surgical Procedure Timing After Injury | Incidence Comparison with All Other Times (%) | Unadjusted | Adjusted* | ||
| RR† | P Value | RR† | P Value | ||
| Hamstring tendon autografts | |||||
| <1 vs. ≥1 mo | 3.76 vs. 2.06 | 1.82 (0.92 to 3.62) | 0.085 | 1.66 (0.84 to 3.29) | 0.15 |
| <3 vs. ≥3 mo | 4.38 vs. 1.79 | 2.45 (1.93 to 3.11) | <0.001 | 2.18 (1.71 to 2.77) | <0.001 |
| <6 vs. ≥6 mo | 3.77 vs. 1.27 | 2.98 (2.42 to 3.67) | <0.001 | 2.53 (2.04 to 3.13) | <0.001 |
| <1 vs. ≥1 yr | 2.72 vs. 1.08 | 2.52 (1.95 to 3.26) | <0.001 | 1.97 (1.52 to 2.56) | <0.001 |
| <2 vs. ≥2 yr | 2.40 vs. 1.00 | 2.39 (1.72 to 3.32) | <0.001 | 1.72 (1.23 to 2.40) | 0.0016 |
| Patellar tendon autografts | |||||
| <1 vs. ≥1 mo | 3.57 vs. 2.61 | 1.37 (0.19 to 9.63) | 0.75 | 1.24 (0.18 to 8.75) | 0.83 |
| <3 vs. ≥3 mo | 3.56 vs. 2.45 | 1.45 (0.67 to 3.16) | 0.34 | 1.64 (0.74 to 3.62) | 0.22 |
| <6 vs. ≥6 mo | 3.60 vs. 1.94 | 1.85 (0.96 to 3.59) | 0.063 | 2.07 (1.05 to 4.09) | 0.036 |
| <1 vs. ≥1 yr | 3.23 vs. 1.39 | 2.33 (0.97 to 5.56) | 0.049 | 2.64 (1.09 to 6.41) | 0.032 |
| <2 vs. ≥2 yr | 2.87 vs. 1.60 | 1.8 (0.64 to 5.04) | 0.26 | 1.99 (0.70 to 5.67) | 0.2 |
| All autografts | |||||
| <1 vs. ≥1 mo | 3.73 vs. 2.18 | 1.71 (0.89 to 3.27) | 0.1 | 1.58 (0.83 to 3.02) | 0.16 |
| <3 vs. ≥3 mo | 4.29 vs. 1.90 | 2.26 (1.80 to 2.85) | <0.001 | 2.07 (1.64 to 2.61) | <0.001 |
| <6 vs. ≥6 mo | 3.75 vs. 1.31 | 2.86 (2.32 to 3.51) | <0.001 | 2.49 (2.01 to 3.08) | <0.001 |
| <1 vs. ≥1 yr | 2.76 vs. 1.05 | 2.64 (2.00 to 3.50) | <0.001 | 2.13 (1.60 to 2.83) | <0.001 |
| <2 vs. ≥2 yr | 2.43 vs. 0.89 | 2.74 (1.79 to 4.21) | <0.001 | 1.98 (1.29 to 3.06) | 0.0019 |
Hamstring tendon autografts were adjusted for age, diameter, femoral fixation, tibial fixation, and concomitant meniscal injury. Patellar tendon autografts were adjusted for age, diameter, femoral cortical fixation, tibial interference screw, and concomitant meniscal injury. All autografts were adjusted for age, graft type, interaction of graft × diameter, femoral cortical fixation, and concomitant meniscal injury.
The values are given as the RR, with the 95% CI in parentheses.
Patients who were treated with a patellar tendon autograft and underwent an ACL reconstruction within 6 months of the injury had a significantly higher risk (p = 0.036) of an early ACL revision surgical procedure compared with patients who were treated at least 6 months after the primary injury.
When both autograft types were combined (Table IV, Fig. 4), patients had a significantly higher risk (p < 0.001) of early ACL revision when the operation took place within 3 months of the initial injury compared with those treated at least 3 months after the injury. The risk of early ACL revision was increased for all patients treated prior to the time intervals in the study, compared with patients treated after the subsequent time intervals.
Fig. 4.
Graph showing the available data for the timing of the surgical procedure after the injury compared with the 2-year ACL revision rate. The numbers given in or with the circles are the number of patients. HT = hamstring tendon and PT = patellar tendon.
Meniscal and Cartilage Injuries
At the time of the index ACL reconstruction, 8,656 patients (47.0%) had a meniscal injury, 4,532 patients (24.6%) had a cartilage injury, and 2,946 patients (16.0%) had both a meniscal injury and a cartilage injury. No difference in the risk of early ACL revision was identified for patients with a meniscal injury, a cartilage injury, or a combined cartilage and meniscal injury (Table V).
TABLE V.
Concomitant Meniscal and Cartilage Injuries: Incidence of Revision Surgical Procedure Within 2 Years After Primary Reconstruction
| Injury at Reconstruction | Incidence Comparison with All Other Injuries (%) | Unadjusted | Adjusted* | ||
| RR† | P Value | RR† | P Value | ||
| Hamstring tendon autograft | |||||
| Meniscal injury | 1.75 vs. 2.38 | 0.74 (0.60 to 0.91) | 0.004 | 0.85 (0.68 to 1.06) | 0.14 |
| Cartilage injury | 1.70 vs. 2.21 | 0.77 (0.59 to 0.99) | 0.041 | 1.22 (0.93 to 1.60) | 0.15 |
| Meniscal and cartilage injury | 1.72 vs. 2.30 | 0.75 (0.55 to 1.01) | 0.059 | 1.15 (0.84 to 1.58) | 0.38 |
| Patellar tendon autograft | |||||
| Meniscal injury | 3.02 vs. 2.21 | 1.37 (0.70 to 2.67) | 0.36 | 1.35 (0.69 to 2.64) | 0.38 |
| Cartilage injury | 3.91 vs. 2.37 | 1.65 (0.79 to 3.48) | 0.18 | 1.79 (0.84 to 3.81) | 0.13 |
| Meniscal and cartilage injury | 4.37 vs. 2.39 | 1.83 (0.82 to 4.07) | 0.14 | 1.86 (0.82 to 4.18) | 0.14 |
| All autografts | |||||
| Meniscal injury | 1.85 vs. 2.36 | 0.78 (0.64 to 0.95) | 0.015 | 0.89 (0.72 to 1.09) | 0.25 |
| Cartilage injury | 1.81 vs. 2.22 | 0.81 (0.64 to 1.04) | 0.092 | 1.25 (0.97 to 1.61) | 0.084 |
| Meniscal and cartilage injury | 1.90 vs. 2.30 | 0.83 (0.62 to 1.09) | 0.18 | 1.22 (0.91 to 1.63) | 0.19 |
Hamstring tendon autografts were adjusted for age, diameter, femoral fixation, tibial fixation, and days to the surgical procedure. Patellar tendon autografts were adjusted for age, diameter, femoral cortical fixation, tibial interference screw, and the days to the surgical procedure. All autografts were adjusted for age, graft type, diameter, interaction of graft × diameter, femoral cortical fixation, and days to the surgical procedure.
The values are given as the RR, with the 95% CI in parentheses.
Discussion
The key findings in this study were the increase in the risk of early ACL revision for patients treated with a metal interference screw as a femoral fixation compared with all other femoral fixations, as well as a decreased risk of early ACL revisions for patients treated with the RIGIDFIX Cross Pin. A shorter time from ACL injury to reconstruction was consistently associated with an increased risk of undergoing ACL revision. The early ACL revision rate in this study was 2.1%, and it is comparable with the rate in other registry studies with similar patient epidemiology27,33.
Graft Fixation
Femoral Graft Fixation
In this study, patients who were treated with a metal interference screw as femoral graft fixation had an increased risk of early ACL revision, and patients who were treated with the RIGIDFIX Cross Pin had a significantly lower risk of early ACL revision when compared with all other femoral graft fixations. Previous studies have either been unable to give clear indications of the optimal femoral graft fixation choice23,34,35 or have indicated that, for hamstring tendon autografts, the transfemoral fixation of the RIGIDFIX Cross Pin yields a lower risk of revision in comparison with cortical fixation (ENDOBUTTON)36,37.
The majority of the patients treated with the RIGIDFIX Cross Pin underwent primary reconstruction early during the study period, and surgeons might not have been as willing to proceed to revision ACL reconstruction during this time frame as they would later during the study period. A more plausible explanation is that the cortical fixation was used when the anteromedial hole drilling technique was introduced. In their study, Eysturoy et al.38 drew the conclusion that patients treated with the anteromedial technique during this period had a higher risk of revision ACL compared with the older transtibial drilling technique, because of a learning curve when a new, complex technique is being introduced.
Tibial Graft Fixation
No independent tibial graft fixation was identified as a risk factor for early ACL revision in the current study. This is in contrast to a previous study in the SNKLR that found that a metal interference screw reduced the risk of revision surgical procedures when used in conjunction with a semitendinosus tendon autograft23. However, this was not found for the majority of patients in the hamstring tendon group in their study who received a combination of semitendinosus and gracilis tendons (79%). The largest categories in the current study are tibial fixations with either a metal interference screw or a bioabsorbable interference screw, accounting for a combined total of 86% of the patients. Recent studies have been unable to identify any significant differences in the risk of ACL revision between these treatment alternatives39,40. It is noteworthy that differences in mechanical environment between separate graft fixation methods have not been addressed in the current study.
Timing of the Surgical Procedure
The timing of ACL reconstruction was a risk factor for early ACL revision in the current study. These findings are in line with the findings of Frobell et al.41, suggesting that patients undergoing an ACL reconstruction within 3 months after the injury do not have better patient-reported outcomes compared with other patients. Previous studies have indicated that, in the long term, it is beneficial to undergo ACL reconstruction early after the injury to prevent further meniscal operations or to reduce the risk of degeneration in the affected knee18,19,42.
One important factor that could explain the results of the current study could be that patients with a high pre-injury activity level often choose to undergo ACL reconstruction early after an ACL injury in an effort to recover their pre-injury level of activity17 as soon as possible43. Patients who return to a high activity level have an increased risk of reinjury and subsequent ACL revision. Another explanation for the lower rerupture rate in patients who undergo delayed ACL reconstruction could be that the period prior to the surgical procedure allows time not only for preoperative rehabilitation but also for psychologically processing the impact of the injury and thereby adjusting the activity level.
The current clinical trend in Scandinavia is to perform ACL reconstruction early for active, young individuals44 in an attempt to improve knee function and to avoid further injuries.
Meniscal and Cartilage Injuries
Neither meniscal nor cartilage injury at the time of primary ACL reconstruction was associated with a reduced risk of early ACL revision compared with all other patients. In a recent systematic review from the Scandinavian registries32, the included studies have found that cartilage damage at the time of the ACL reconstruction either reduced the risk of ACL revision or had a limited impact on revision risk. However, meniscal injuries at the time of ACL reconstruction were not found to be predictive of ACL revision. Patients with a meniscal injury at the time of primary ACL reconstruction are more likely to have sustained greater trauma and have more severe soft-tissue injuries compared with other patients45,46. Another explanation is that patients with intra-articular damage to the knee do not return to their pre-injury level, with the majority undergoing a partial meniscectomy47, thereby accelerating degenerative joint changes. The results of the current study are not in line with those of previous studies23 from the Scandinavian registries that found that patients with a cartilage injury have a decreased risk of early ACL revision.
Limitations
Because the primary outcome of this study is ACL revision, a limitation of this study was that the true incidence of graft failure was therefore underestimated, given that many patients did not undergo ACL revision in spite of clinical graft failure, potentially accepting occasional instability or lower activity level. In the registries, there was no information about the activity level of patients. This information on activity level would have helped us to analyze the risks of a new injury associated with activity. Another limitation was that the information on autograft positions was not available from the registries. Although 58,692 patients were included in the registries during the study period, only 18,425 patients were included in the current study, largely because of missing data on autograft diameter or a lack of follow-up.
One important strength of this study is the large cohort of patients undergoing ACL reconstruction in Norway and Sweden. All the data were registered prospectively, independent of other studies.
Conclusions
The 2-year ACL revision rate in this study was 2.1%. Patients undergoing ACL reconstruction within 3 months of the injury, as well as patients treated with a metal interference screw in the femur, had a significantly higher risk of ACL revision, and patients treated with the RIGIDFIX Cross Pin in the femur had a significantly lower risk of ACL revision.
Footnotes
Investigation performed at the Institute of Clinical Sciences, The Sahlgrenska Academy, University of Gothenburg, Gothenburg, Sweden
Disclosure: The authors indicated that no external funding was received for any aspect of this work. On the Disclosure of Potential Conflicts of Interest forms, which are provided with the online version of the article, one or more of the authors checked “yes” to indicate that the author had other relationships or activities that could be perceived to influence, or have the potential to influence, what was written in this work (http://links.lww.com/JBJSOA/A133).
References
- 1.Middleton KK, Hamilton T, Irrgang JJ, Karlsson J, Harner CD, Fu FH. Anatomic anterior cruciate ligament (ACL) reconstruction: a global perspective. Part 1. Knee Surg Sports Traumatol Arthrosc. 2014. Jul;22(7):1467-82. Epub 2014 Feb 5. [DOI] [PubMed] [Google Scholar]
- 2.Kaeding CC, Pedroza AD, Reinke EK, Huston LJ, Hewett TE, Flanigan DC, Spindler KP; MOON Knee Group. Change in anterior cruciate ligament graft choice and outcomes over time. Arthroscopy. 2017. Nov;33(11):2007-14. Epub 2017 Aug 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Paterno MV, Rauh MJ, Schmitt LC, Ford KR, Hewett TE. Incidence of second ACL injuries 2 years after primary ACL reconstruction and return to sport. Am J Sports Med. 2014. Jul;42(7):1567-73. Epub 2014 Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. BMJ. 2013. Jan 24;346:f232. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Frobell RB, Roos HP, Roos EM, Roemer FW, Ranstam J, Lohmander LS. Treatment for acute anterior cruciate ligament tear: five year outcome of randomised trial. Br J Sports Med. 2015. May;49(10):700. [DOI] [PubMed] [Google Scholar]
- 6.Filbay SR, Roos EM, Frobell RB, Roemer F, Ranstam J, Lohmander LS. Delaying ACL reconstruction and treating with exercise therapy alone may alter prognostic factors for 5-year outcome: an exploratory analysis of the KANON trial. Br J Sports Med. 2017. Nov;51(22):1622-9. Epub 2017 May 17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kamelger FS, Onder U, Schmoelz W, Tecklenburg K, Arora R, Fink C. Suspensory fixation of grafts in anterior cruciate ligament reconstruction: a biomechanical comparison of 3 implants. Arthroscopy. 2009. Jul;25(7):767-76. Epub 2009 Apr 26. [DOI] [PubMed] [Google Scholar]
- 8.Houck DA, Kraeutler MJ, McCarty EC, Bravman JT. Fixed- versus adjustable-loop femoral cortical suspension devices for anterior cruciate ligament reconstruction: a systematic review and meta-analysis of biomechanical studies. Orthop J Sports Med. 2018. Oct 19;6(10):2325967118801762. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lind M, Menhert F, Pedersen AB. Incidence and outcome after revision anterior cruciate ligament reconstruction: results from the Danish registry for knee ligament reconstructions. Am J Sports Med. 2012. Jul;40(7):1551-7. Epub 2012 May 4. [DOI] [PubMed] [Google Scholar]
- 10.Webster KE, Feller JA. Exploring the high reinjury rate in younger patients undergoing anterior cruciate ligament reconstruction. Am J Sports Med. 2016. Nov;44(11):2827-32. Epub 2016 Jul 7. [DOI] [PubMed] [Google Scholar]
- 11.Kaeding CC Pedroza AD Reinke EK Huston LJ Spindler KP; MOON Consortium. Risk factors and predictors of subsequent ACL injury in either knee after ACL reconstruction: prospective analysis of 2488 primary ACL reconstructions from the MOON cohort. Am J Sports Med. 2015. Jul;43(7):1583-90. Epub 2015 Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Nagelli CV, Hewett TE. Should return to sport be delayed until 2 years after anterior cruciate ligament reconstruction? Biological and functional considerations. Sports Med. 2017. Feb;47(2):221-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Yabroudi MA, Björnsson H, Lynch AD, Muller B, Samuelsson K, Tarabichi M, Karlsson J, Fu FH, Harner CD, Irrgang JJ. Predictors of revision surgery after primary anterior cruciate ligament reconstruction. Orthop J Sports Med. 2016. Sep 27;4(9):2325967116666039. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Chen JL, Allen CR, Stephens TE, Haas AK, Huston LJ, Wright RW, Feeley BT; Multicenter ACL Revision Study (MARS) Group. Differences in mechanisms of failure, intraoperative findings, and surgical characteristics between single- and multiple-revision ACL reconstructions: a MARS cohort study. Am J Sports Med. 2013. Jul;41(7):1571-8. Epub 2013 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Persson A, Kjellsen AB, Fjeldsgaard K, Engebretsen L, Espehaug B, Fevang JM. Registry data highlight increased revision rates for ENDOBUTTON/BIOSURE HA in ACL reconstruction with hamstring tendon autograft: a nationwide cohort study from the Norwegian Knee Ligament Registry, 2004-2013. Am J Sports Med. 2015. Sep;43(9):2182-8. Epub 2015 May 14. [DOI] [PubMed] [Google Scholar]
- 16.Kraeutler MJ, Wolsky RM, Vidal AF, Bravman JT. Anatomy and biomechanics of the native and reconstructed anterior cruciate ligament: surgical implications. J Bone Joint Surg Am. 2017. Mar 1;99(5):438-45. [DOI] [PubMed] [Google Scholar]
- 17.Andernord D, Karlsson J, Musahl V, Bhandari M, Fu FH, Samuelsson K. Timing of surgery of the anterior cruciate ligament. Arthroscopy. 2013. Nov;29(11):1863-71. Epub 2013 Sep 18. [DOI] [PubMed] [Google Scholar]
- 18.Karikis I, Åhlén M, Sernert N, Ejerhed L, Rostgård-Christensen L, Kartus J. The long-term outcome after early and late anterior cruciate ligament reconstruction. Arthroscopy. 2018. Jun;34(6):1907-17. Epub 2018 Mar 6. [DOI] [PubMed] [Google Scholar]
- 19.Kay J, Memon M, Shah A, Yen YM, Samuelsson K, Peterson D, Simunovic N, Flageole H, Ayeni OR. Earlier anterior cruciate ligament reconstruction is associated with a decreased risk of medial meniscal and articular cartilage damage in children and adolescents: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2018. Dec;26(12):3738-53. Epub 2018 Jun 6. [DOI] [PubMed] [Google Scholar]
- 20.Smith TO, Davies L, Hing CB. Early versus delayed surgery for anterior cruciate ligament reconstruction: a systematic review and meta-analysis. Knee Surg Sports Traumatol Arthrosc. 2010. Mar;18(3):304-11. Epub 2009 Oct 17. [DOI] [PubMed] [Google Scholar]
- 21.Deabate L, Previtali D, Grassi A, Filardo G, Candrian C, Delcogliano M. Anterior cruciate ligament reconstruction within 3 weeks does not increase stiffness and complications compared with delayed reconstruction: a meta-analysis of randomized controlled trials. Am J Sports Med. 2019. Aug 5:363546519862294. [Epub 2019 ahead of print.] [DOI] [PubMed] [Google Scholar]
- 22.Mather RC, 3rd, Hettrich CM, Dunn WR, Cole BJ, Bach BR, Jr, Huston LJ, Reinke EK, Spindler KP. Cost-effectiveness analysis of early reconstruction versus rehabilitation and delayed reconstruction for anterior cruciate ligament tears. Am J Sports Med. 2014. Jul;42(7):1583-91. Epub 2014 May 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Andernord D, Björnsson H, Petzold M, Eriksson BI, Forssblad M, Karlsson J, Samuelsson K. Surgical predictors of early revision surgery after anterior cruciate ligament reconstruction: results from the Swedish National Knee Ligament Register on 13,102 patients. Am J Sports Med. 2014. Jul;42(7):1574-82. Epub 2014 Apr 28. [DOI] [PubMed] [Google Scholar]
- 24.Gifstad T, Foss OA, Engebretsen L, Lind M, Forssblad M, Albrektsen G, Drogset JO. Lower risk of revision with patellar tendon autografts compared with hamstring autografts: a registry study based on 45,998 primary ACL reconstructions in Scandinavia. Am J Sports Med. 2014. Oct;42(10):2319-28. Epub 2014 Sep 8. [DOI] [PubMed] [Google Scholar]
- 25.Musahl V, Rahnemai-Azar AA, Costello J, Arner JW, Fu FH, Hoshino Y, Lopomo N, Samuelsson K, Irrgang JJ. The Influence of meniscal and anterolateral capsular injury on knee laxity in patients with anterior cruciate ligament injuries. Am J Sports Med. 2016. Dec;44(12):3126-31. Epub 2016 Aug 9. [DOI] [PubMed] [Google Scholar]
- 26.Granan LP, Forssblad M, Lind M, Engebretsen L. The Scandinavian ACL registries 2004-2007: baseline epidemiology. Acta Orthop. 2009. Oct;80(5):563-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Prentice HA, Lind M, Mouton C, Persson A, Magnusson H, Gabr A, Seil R, Engebretsen L, Samuelsson K, Karlsson J, Forssblad M, Haddad FS, Spalding T, Funahashi TT, Paxton LW, Maletis GB. Patient demographic and surgical characteristics in anterior cruciate ligament reconstruction: a description of registries from six countries. Br J Sports Med. 2018. Jun;52(11):716-22. Epub 2018 Mar 24. [DOI] [PubMed] [Google Scholar]
- 28.Kvist J, Kartus J, Karlsson J, Forssblad M. Results from the Swedish National Anterior Cruciate Ligament Register. Arthroscopy. 2014. Jul;30(7):803-10. Epub 2014 Apr 18. [DOI] [PubMed] [Google Scholar]
- 29.Magnussen RA, Trojani C, Granan LP, Neyret P, Colombet P, Engebretsen L, Wright RW, Kaeding CC; MARS Group; SFA Revision ACL Group. Patient demographics and surgical characteristics in ACL revision: a comparison of French, Norwegian, and North American cohorts. Knee Surg Sports Traumatol Arthrosc. 2015. Aug;23(8):2339-48. Epub 2014 May 22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Granan LP, Bahr R, Steindal K, Furnes O, Engebretsen L. Development of a national cruciate ligament surgery registry: the Norwegian National Knee Ligament Registry. Am J Sports Med. 2008. Feb;36(2):308-15. Epub 2007 Nov 7. [DOI] [PubMed] [Google Scholar]
- 31.Ahldén M, Samuelsson K, Sernert N, Forssblad M, Karlsson J, Kartus J. The Swedish National Anterior Cruciate Ligament Register: a report on baseline variables and outcomes of surgery for almost 18,000 patients. Am J Sports Med. 2012. Oct;40(10):2230-5. Epub 2012 Sep 7. [DOI] [PubMed] [Google Scholar]
- 32.Svantesson E, Hamrin Senorski E, Baldari A, Ayeni OR, Engebretsen L, Franceschi F, Karlsson J, Samuelsson K. Factors associated with additional anterior cruciate ligament reconstruction and register comparison: a systematic review on the Scandinavian knee ligament registers. Br J Sports Med. 2019. Apr;53(7):418-25. Epub 2018 Jul 17. [DOI] [PubMed] [Google Scholar]
- 33.Rahr-Wagner L, Thillemann TM, Pedersen AB, Lind M. Comparison of hamstring tendon and patellar tendon grafts in anterior cruciate ligament reconstruction in a nationwide population-based cohort study: results from the Danish registry of knee ligament reconstruction. Am J Sports Med. 2014. Feb;42(2):278-84. Epub 2013 Nov 25. [DOI] [PubMed] [Google Scholar]
- 34.Ilahi OA, Nolla JM, Ho DM. Intra-tunnel fixation versus extra-tunnel fixation of hamstring anterior cruciate ligament reconstruction: a meta-analysis. J Knee Surg. 2009. Apr;22(2):120-9. [DOI] [PubMed] [Google Scholar]
- 35.Aydin D, Ozcan M. Evaluation and comparison of clinical results of femoral fixation devices in arthroscopic anterior cruciate ligament reconstruction. Knee. 2016. Mar;23(2):227-32. Epub 2015 May 1. [DOI] [PubMed] [Google Scholar]
- 36.Persson A, Gifstad T, Lind M, Engebretsen L, Fjeldsgaard K, Drogset JO, Forssblad M, Espehaug B, Kjellsen AB, Fevang JM. Graft fixation influences revision risk after ACL reconstruction with hamstring tendon autografts. Acta Orthop. 2018. Apr;89(2):204-10. Epub 2017 Nov 24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Eysturoy NH, Nissen KA, Nielsen T, Lind M. The influence of graft fixation methods on revision rates after primary anterior cruciate ligament reconstruction. Am J Sports Med. 2018. Mar;46(3):524-30. Epub 2018 Jan 16. [DOI] [PubMed] [Google Scholar]
- 38.Eysturoy NH, Nielsen TG, Lind MC. Anteromedial portal drilling yielded better survivorship of anterior cruciate ligament reconstructions when comparing recent versus early surgeries with this technique. Arthroscopy. 2019. Jan;35(1):182-9. [DOI] [PubMed] [Google Scholar]
- 39.Mascarenhas R, Saltzman BM, Sayegh ET, Verma NN, Cole BJ, Bush-Joseph C, Bach BR, Jr. Bioabsorbable versus metallic interference screws in anterior cruciate ligament reconstruction: a systematic review of overlapping meta-analyses. Arthroscopy. 2015. Mar;31(3):561-8. Epub 2014 Dec 31. [DOI] [PubMed] [Google Scholar]
- 40.Debieux P, Franciozi CE, Lenza M, Tamaoki MJ, Magnussen RA, Faloppa F, Belloti JC. Bioabsorbable versus metallic interference screws for graft fixation in anterior cruciate ligament reconstruction. Cochrane Database Syst Rev. 2016. Jul 24;7:CD009772. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Frobell RB, Roos EM, Roos HP, Ranstam J, Lohmander LS. A randomized trial of treatment for acute anterior cruciate ligament tears. N Engl J Med. 2010. Jul 22;363(4):331-42. [DOI] [PubMed] [Google Scholar]
- 42.Brambilla L, Pulici L, Carimati G, Quaglia A, Prospero E, Bait C, Morenghi E, Portinaro N, Denti M, Volpi P. Prevalence of associated lesions in anterior cruciate ligament reconstruction: correlation with surgical timing and with patient age, sex, and body mass index. Am J Sports Med. 2015. Dec;43(12):2966-73. Epub 2015 Oct 15. [DOI] [PubMed] [Google Scholar]
- 43.Grindem H, Snyder-Mackler L, Moksnes H, Engebretsen L, Risberg MA. Simple decision rules can reduce reinjury risk by 84% after ACL reconstruction: the Delaware-Oslo ACL Cohort study. Br J Sports Med. 2016. Jul;50(13):804-8. Epub 2016 May 9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Herbst E, Hoser C, Gföller P, Hepperger C, Abermann E, Neumayer K, Musahl V, Fink C. Impact of surgical timing on the outcome of anterior cruciate ligament reconstruction. Knee Surg Sports Traumatol Arthrosc. 2017. Feb;25(2):569-77. Epub 2016 Aug 22. [DOI] [PubMed] [Google Scholar]
- 45.Pike AN, Patzkowski JC, Bottoni CR. Meniscal and chondral pathology associated with anterior cruciate ligament injuries. J Am Acad Orthop Surg. 2019. Feb 1;27(3):75-84. [DOI] [PubMed] [Google Scholar]
- 46.Cox CL, Huston LJ, Dunn WR, Reinke EK, Nwosu SK, Parker RD, Wright RW, Kaeding CC, Marx RG, Amendola A, McCarty EC, Spindler KP. Are articular cartilage lesions and meniscus tears predictive of IKDC, KOOS, and Marx activity level outcomes after anterior cruciate ligament reconstruction? A 6-year multicenter cohort study. Am J Sports Med. 2014. May;42(5):1058-67. Epub 2014 Mar 19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Noyes FR, Barber-Westin SD. Treatment of meniscus tears during anterior cruciate ligament reconstruction. Arthroscopy. 2012. Jan;28(1):123-30. Epub 2011 Nov 9. [DOI] [PubMed] [Google Scholar]