Abstract
Objective
To survey care providers' willingness to use 2-mSv computed tomography (CT) in their usual practice for adolescents and young adults with suspected appendicitis.
Materials and Methods
An ethical committee approved this prospective study. We introduced 2-mSv CT in 20 hospitals through a pragmatic clinical trial. At the final phase of the trial, we invited 698 potentially-involved care providers in the survey regarding their willingness to use 2-mSv CT. Multivariable logistic regression analyses were performed to identify factors associated with willingness. Nine months after the completion of the trial patient recruitment, we surveyed whether the hospitals were using 2-mSv CT in usual practice.
Results
The analyses included responses from 579 participants (203 attendings and 376 trainees; 221 radiologists, 196 emergency physicians, and 162 surgeons). Regarding the willingness to immediately change their standard practice to 2-mSv CT, 158 (27.3%), 375 (64.8%), and 46 (7.9%) participants responded as “yes” (consistently), “partly” (selectively), and “no”, respectively. Willingness varied considerably across the hospitals, but only slightly across the participants' departments or job titles. Willingness was significantly associated with attendings (p = 0.004), intention to maintain the dedicated appendiceal CT protocol (p < 0.001), belief in compelling evidence on the carcinogenic risk of conventional-dose CT radiation (p = 0.028), and hospitals having more than 1000 beds (p = 0.031). Fourteen of the 20 hospitals kept using 2-mSv appendiceal CT in usual practice after the trial.
Conclusion
Despite the extensive efforts over the years of this clinical trial, many care providers were willing to use 2-mSv CT selectively or not willing to use.
Keywords: Appendicitis, Tomography, Radiation dosage, Surveys and questionnaires
INTRODUCTION
Acute appendicitis is the most common indication for emergency abdominal surgery. Computed tomography (CT) plays an important role in the diagnosis of appendicitis owing to the high availability and excellent diagnostic performance (1). Preoperative CT is used in approximately 90% of the patients undergoing appendectomy in the United States (2) and South Korea (3). Moreover, there are even more patients who undergo appendiceal CT and do not ultimately undergo appendectomy. Many patients undergoing appendiceal CT are adolescents and young adults having otherwise normal life expectancies, for whom the carcinogenic effect of typical abdominopelvic CT is still debated (4).
Retrospective studies have shown that reducing the radiation dose by 50–80% from conventional doses does not impair the diagnosis of appendicitis (5,6,7,8). A single-institutional randomized controlled trial has shown the non-inferiority of 2-mSv CT compared with 8-mSv conventional CT with respect to negative appendectomy rate in adolescents and young adults (9). Those promising study results were generalizable to 20 hospitals in a clinical trial setting (Low-dOse CT for Appendicitis Trial, LOCAT) (10).
However, there is a vast disparity between research studies and clinical practice regarding CT radiation dose, because care providers are reluctant to rely on noisy images of low-dose CT. For example, despite ample evidence supporting low-dose CT for renal colic, a national survey in the United States showed that only 7.6% of urinary stone CT examinations from 2015–2016 used low-dose techniques (11). For a successful implementation of a low-dose CT practice, it is important that all involved care providers (not only radiologists, but also referring physicians) are willing to use such a low radiation dose in their usual practice.
Acknowledging this challenge, LOCAT was designed as a pragmatic trial so that the participating hospitals could systematically incorporate 2-mSv CT into their usual practice by implementing LOCAT protocol (12). At the final phase of LOCAT, before LOCAT data analysis, we conducted a preplanned survey of the care providers participating in LOCAT regarding their willingness to use 2-mSv CT in their usual practice for adolescents and young adults with suspected appendicitis. We herein report the survey results.
MATERIALS AND METHODS
This prospective survey study was designed as a part of LOCAT, a large pragmatic clinical trial (10) which aimed to test the non-inferiority of 2-mSv CT compared to institutional conventional-dose (typically 8-mSv) CT in the diagnosis of appendicitis in patients aged 15–44 years. LOCAT involved 3074 patients and more than 500 care providers from 20 hospitals and was conducted from December 2013 through February 2017. The survey study was approved by the Institutional Review Board, which waived the need for written consent from the participating care providers. All data were anonymized. Three radiologists designed and coordinated the survey study.
Low-Dose CT
In LOCAT, 1535 and 1539 patients were randomly assigned to undergo 2-mSv or conventional-dose CT (≤ 8 mSv), respectively. The eligibility criteria were patients aged 15–44 years who were referred from the emergency departments for contrast-enhanced CT because of suspected appendicitis. There was no notable difference in their age (median [interquartile range], 28 [21–35] vs. 28 [21–35] years) or sex (female, 54.6% vs. 54.2%) between the 2-mSv or conventional-dose CT groups. The 20 participating hospitals used 2-mSv CT techniques in the patients in the low-dose group. 2-mSv was around the lowest dose level that had been tested in previous studies exploring low-dose appendiceal CT techniques (5,6).
LOCAT protocol mandated that each site set up a dedicated appendiceal CT protocol (from order entry to CT scanning) in the hospital information system and used the protocol in all eligible patients. Single breath-hold intravenous contrast-enhanced scans of the abdomen and pelvis were obtained using 22 different CT machines. Image section thickness was 5 mm or thinner, with a 20% or greater overlap. Otherwise, the imaging technique was followed according to each institutional protocol. Seven sites used iterative reconstruction techniques. The imaging techniques are detailed elsewhere (10,12).
One important purpose of LOCAT was to incorporate 2-mSv CT into the usual practice across the participating and other hospitals. We expected that the rigid frame of a clinical trial would help the involved care providers to adopt 2-mSv CT in their practice. For this reason, LOCAT was designed as a pragmatic trial so that each participating site could systematically incorporate the 2-mSv CT technique into their practices through the course of the trial. The pragmatic features were as follows. First, the eligibility criteria were broad and largely depended on the judgment of the individual care providers. Second, the requirements for the detailed CT imaging and interpretation protocol were minimized. Third, all co-interventions (i.e., diagnostic and therapeutic procedures other than the initial appendiceal CT) followed the site-standard practice without using extra resources.
Survey Participants
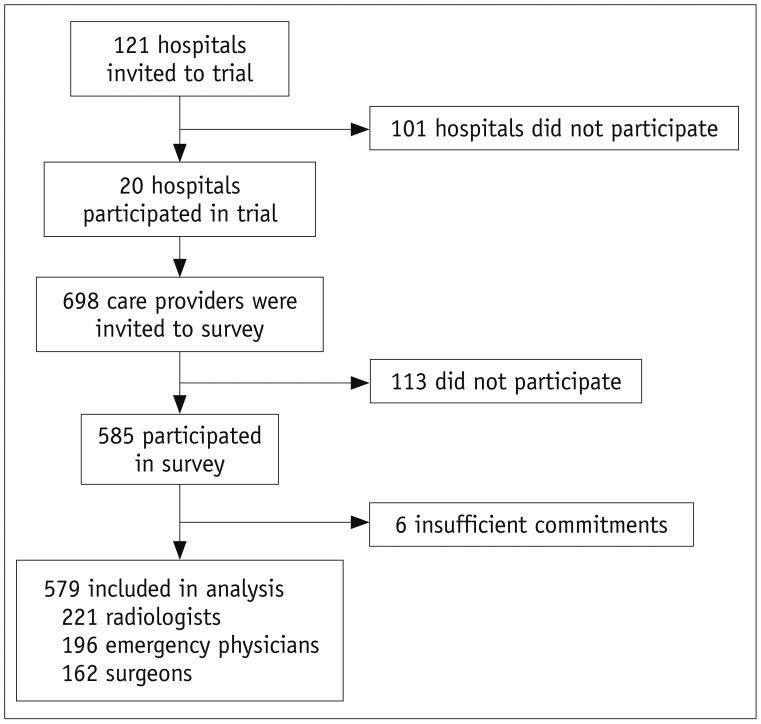
In October 2012, the LOCAT lead investigator invited 121 hospitals to LOCAT through the network of the Korean Society of Abdominal Radiology. Twenty teaching hospitals with a median of 269 (interquartile range, 158–428) annual appendectomies participated in LOCAT. For the survey, the coordinators of the present study invited all 698 care providers, including attendings (specialists, staff, or professor) and trainees (residents), who were reported by the site principal investigators to be potentially involved in the care of trial patients (Fig. 1). They were 227 radiologists, 253 emergency physicians, and 218 surgeons. We opted to include emergency physicians and surgeons as well as radiologists in the survey. Since emergency physicians and surgeons are often claimed to be ultimately responsible for appropriate diagnosis (13), their support and understanding of low-dose CT were essential for a successful implementation of low-dose CT practice.
Fig. 1. Flow diagram of study participants.
Development of the Survey
The study coordinators jointly created the survey questionnaire. The question items included the participants' willingness to change the standard practice to 2-mSv CT (Q1–Q4), the maintenance of the dedicated appendiceal CT protocol (whether it is low or conventional dose) in the hospital information system (Q5), the quality of CT reports (Q6 and Q7), and an estimation of the carcinogenic risk of conventional-dose CT radiation (Q8 and Q9) (Table 1). For most of the questions, responses were obtained as “yes,” “partly,” or “no.” We defined “yes” as ‘completely and consistently,’ and “partly” as ‘not consistently but selectively (e.g., during working hours).’ The participants were informed of these definitions.
Table 1. Survey Questionnaire.
| Question Item | Question |
|---|---|
| Willingness to change to 2-mSv CT | |
| Q1. Willingness to immediately change* | Do you agree to change standard practice in your hospital to 2-mSv CT immediately? |
| Q2. Reasons for reluctance to change† | (For those who chose “partly” or “no” in Q1) Which disadvantage(s) of 2-mSv CT makes you hesitant to change your practice to 2-mSv CT? |
| Q3. Willingness to change in future* | (For those who chose “partly” or “no” in Q1) If not right away but shortly, do you agree with changing your standard practice to 2-mSv CT? |
| Q4. Acceptance of 2-mSv CT* | Is 2-mSv CT in your hospital acceptable for your practice? |
| Q5. Maintaining dedicated appendix CT protocol in hospital information system* | Even after ongoing trial is finished or your hospital discontinues participation in trial, do you feel that care providers in your hospital should continue to use dedicated “appendix CT” protocol (whether it is low or conventional dose) in hospital information system? |
| Quality of CT reports | |
| Q6. Timeliness and accuracy of CT reports* | Are radiologists in your hospital providing reports for appendix CT (regardless of radiation dose) accurately and rapidly? |
| Q7. Timeliness and accuracy of 2-mSv CT reports* | Are radiologists in your hospital providing reports for appendix 2-mSv CT accurately and rapidly? |
| Estimation of carcinogenic risk of conventional-dose CT radiation | |
| Q8. In comparison to natural background radiation‡ | How many times greater is radiation dose level of conventional-dose CT in comparison to annual dose of natural background radiation? |
| Q9. Evidence level of carcinogenic risk* | Is there compelling evidence on carcinogenic risk of single exposure to conventional-dose CT? |
| Q10. Commitment in responses§ | How would you describe your commitment to answering these questions? |
All questions were pertinent to CT in adolescent and young adults with suspected appendicitis. *Responses were obtained as “yes,” “partly,” or “no.” “Yes” indicated ‘completely and consistently,’ while “partly” indicated ‘not consistently but selectively (e.g., during working hours),’ †Participants were asked to choose one or more of followings: low image quality, impaired diagnostic performance, insufficient experience in 2-mSv CT, lack of published evidence justifying use of 2-mSv CT, and worrisome clinical outcomes, ‡Responses were obtained as 0.004-, 0.04-, 0.4-, 4-, 40-, or 400-fold, §Responses were obtained using 5-point Likert scale: never committed, hardly committed, unsure, partly committed, and fully committed.
The most important question item was Q1 regarding a care provider's willingness to immediately change the institutional standard dose for appendiceal CT to 2 mSv. At the end of the survey, each participant was asked to describe his or her commitment to answering the questions using a 5-point Likert scale (Q10). A research assistant formatted the questionnaires in a Web-based survey (SurveyMonkey, San Mateo, CA, USA).
Survey Procedure
The survey was conducted from February 2016 through November 2016, which was the final phase of LOCAT participant enrollment and before LOCAT data analysis. LOCAT participant enrollment was completed in August 2016. The study coordinators sent an invitation e-mail with a link to the survey to the 698 care providers. The rollout initiated with three hospitals and then gradually expanded to the remaining hospitals. This allowed the coordinators to concentrate on two or three new hospitals at a time. Until the response rate within a hospital reached 80%, we maintained weekly reminder e-mails to non-responding invitees in the hospital to participate. Participants were informed that all questions pertained to appendiceal CT in patients aged 15–44 years. We did not give any restraint as to if the survey participants could have a mutual discussion regarding the survey. We did not collect any data regarding if the participants had such a discussion.
In May 2017, nine months after LOCAT patient recruitment was completed, we conducted a follow-up online interview with 20 site principal investigators regarding whether each hospital are using 2-mSv appendiceal CT in the usual practice for patients aged 15–44 years. The interview included a question about how consistently the care providers were using the dedicated appendiceal CT protocol in the hospital information system.
Statistical Analysis
One of the study coordinators and a statistician planned all analyses before the data collection. The participants with insufficient self-reported commitment (defined as responses of “never committed,” “hardly committed” or “unsure” to Q10) were excluded from the data analysis. Descriptive statistics, including percentages and medians, were used to summarize the results.
We tabulated the results for participant subgroups categorized by their department and job title. Stacked bar graphs were generated to illustrate the individual hospital response results regarding the willingness to immediately change the institutional standard practice to 2-mSv CT (Q1). For the carcinogenic risk of conventional-dose CT radiation in comparison to natural background radiation (Q8), “4-fold” was considered as an accurate estimate (14,15).
To identify participant characteristics or hospital characteristics associated with the willingness to change to 2-mSv CT (Q1), we performed univariable and multivariable logistic regression analyses by regarding “yes” as a positive response and “partly” or “no” as a negative response for the willingness. The tested covariates included participant characteristics (department and job title), responses to question items Q4–Q9, and hospital characteristics (use of iterative reconstruction, annual number of appendectomies, number of beds, and number of patients enrolled in LOCAT). We were unable to test covariates regarding individual care providers' prior experience in 2-mSv CT or their active participation in LOCAT. LOCAT data were particularly incomplete regarding individual emergency physicians' participation because such data collection was unfeasible due to the complexity related to team-based approach and rotational shiftwork (12). Instead, we tested the per-site number of enrolled patients in LOCAT as a covariate with a subgrouping threshold of 100 which was close to the median of the data (16). Q4, Q6, and Q7 did not enter the multivariable analysis because we considered each of them directly connected with the respondents' overall satisfaction on 2-mSv CT and therefore with Q1, and because they were obviously intercorrelated with one another (17). A p value of < 0.05 was considered to indicate statistical significance. Statistics software (Stata 14.0; StataCorp., College Station, TX, USA) was used.
RESULTS
Of the 698 invitees, 585 (83.8%) participated in the survey. The participation rate of radiologists, emergency physicians, and surgeons was 98.7% (224/227), 78.3% (198/253), and 74.8% (163/218), respectively (Table 2). Three radiologists, two emergency physicians, and a surgeon were excluded from the analysis because their self-reported commitments to the responses (Q10) were insufficient (Supplementary Table 1). Subsequent analyses, therefore, included the remaining 579 participants (median per hospital, 24; interquartile range, 21–33), comprising 221 radiologists, 196 emergency physicians, and 162 surgeons. They were 203 attendings and 376 trainees. The attendings had a median clinical experience of 8 years (interquartile range: 4–13) (Supplementary Table 2).
Table 2. Number of Participants.
| Care Providers | Invitees | Participants | Included in Analysis |
|---|---|---|---|
| Total | 698, 31 (24–39)* | 585 (83.8%), 25 (22–34)* | 579 (83.0%), 24 (21–33)* |
| Radiologists | 227, 11 (8–14)* | 224 (98.7%), 10 (8–14)* | 221 (97.4%), 10 (8–13)* |
| Attending | 66, 3 (2–4)* | 64 (97%), 3 (2–3)* | 64 (97%), 3 (2–4)* |
| Trainee | 161, 7 (6–11)* | 160 (99%), 8 (6–11)* | 157 (98%), 7 (6–10)* |
| Emergency physicians | 253, 11 (9–14)* | 198 (78.3%), 9 (6–12)* | 196 (77.5%), 9 (6–12)* |
| Attending | 89, 4 (3–5)* | 69 (78%), 3 (2–4)* | 68 (76%), 3 (2–4)* |
| Trainee | 164, 7 (4–11)* | 129 (79%), 6 (3–9)* | 128 (78%), 6 (3–9)* |
| Surgeons | 218, 9 (7–13)* | 163 (74.8%), 7 (5–12)* | 162 (74.3%), 7 (5–12)* |
| Attending | 101, 6 (4–8)* | 71 (70%), 4 (2–5)* | 71 (70%), 4 (2–5)* |
| Trainee | 117, 5 (1–9)* | 92 (79%), 3 (1–8)* | 91 (78%), 4 (1–8)* |
Data are numbers of care providers (and percentages out of invitees). *Data are median numbers (and interquartile ranges) of care providers per hospital.
Table 3 summarizes the overall and subgroup responses to each question item. Regarding the willingness to immediately change the institutional standard practice to 2-mSv CT (Q1), 158 (27.3%; 95% confidence interval, 23.8–30.9%), 375 (64.8%, 60.6–68.6%), and 46 (7.9%; 5.7–10.4%) participants responded as “yes,” “partly,” and “no,” respectively. As we mentioned earlier, “yes” indicated ‘completely and consistently,’ while “partly” indicated ‘not consistently but selectively (e.g., during working hours).’ Only the 421 participants who responded as “partly” or “no” to Q1 were asked questions Q2 and Q3. Of the 421 participants, 248 (58.9%), 213 (50.6%), 78 (18.5%), 71 (16.9%), and 48 (11.4%) responded that the reasons for their reluctance to the immediate change were “low image quality,” “impaired diagnostic performance,” “insufficient experience in 2-mSv CT,” “lack of published evidence justifying the use of 2-mSv CT,” and “worrisome clinical outcomes,” respectively (Q2).
Table 3. Survey Results.
| Question Items | Overall (n = 579) | Department | Job Title | |||
|---|---|---|---|---|---|---|
| Radiologists (n = 221) | Emergency Physicians (n = 196) | Surgeons (n = 162) | Attendings (n = 203) | Trainees (n = 376) | ||
| Q1. Willingness to immediately change | ||||||
| Yes (%) | 158 (27.3) | 62 (28.1) | 45 (23) | 51 (32) | 73 (36.0) | 85 (22.6) |
| Partly (%) | 375 (64.8) | 143 (64.7) | 134 (68) | 98 (61) | 118 (58.1) | 257 (68.4) |
| No (%) | 46 (7.9) | 16 (7.2) | 17 (9) | 13 (8) | 12 (5.9) | 34 (9.0) |
| Q2. Reasons for reluctance to change* | ||||||
| Low image quality (%) | 248 (58.9) | 87 (55) | 100 (66) | 61 (55) | 69 (53) | 179 (61.5) |
| Impaired diagnostic performance (%) | 213 (50.6) | 81 (51) | 67 (44) | 65 (59) | 63 (49) | 150 (51.5) |
| Insufficient experience in 2-mSv CT (%) | 78 (18.5) | 37 (24) | 21 (14) | 20 (18) | 32 (25) | 46 (15.8) |
| Lack of published evidence justifying use of 2-mSv CT (%) | 71 (16.9) | 29 (18) | 20 (13) | 22 (20) | 23 (18) | 48 (16.5) |
| Worrisome clinical outcomes | 48 (11.4) | 14 (9) | 20 (13) | 14 (13) | 16 (12) | 32 (11.0) |
| Q3. Willingness to change in future* | ||||||
| Yes (%) | 276 (65.6) | 112 (70) | 103 (68) | 61 (55) | 99 (76) | 177 (60.8) |
| Partly (%) | 108 (25.7) | 39 (25) | 34 (23) | 35 (32) | 26 (20) | 82 (28.2) |
| No (%) | 37 (8.8) | 8 (5) | 14 (9) | 15 (14) | 5 (4) | 32 (11.0) |
| Q4. Acceptance of 2-mSv CT | ||||||
| Yes (%) | 396 (68.4) | 178 (80.5) | 124 (63) | 94 (58) | 156 (76.8) | 240 (63.8) |
| Partly (%) | 166 (28.7) | 41 (18.6) | 67 (34) | 58 (36) | 43 (21.2) | 123 (32.7) |
| No (%) | 17 (2.9) | 2 (0.9) | 5 (3) | 10 (6) | 4 (2.0) | 13 (3.5) |
| Q5. Maintaining dedicated appendix CT protocol in hospital information system | ||||||
| Yes (%) | 298 (51.5) | 108 (48.9) | 99 (51) | 91 (56) | 122 (60.1) | 176 (46.8) |
| Partly (%) | 135 (23.3) | 62 (28.1) | 45 (23) | 28 (17) | 45 (22.2) | 90 (23.9) |
| No (%) | 146 (25.2) | 51 (23.1) | 52 (27) | 43 (27) | 36 (17.7) | 110 (29.3) |
| Q6. Timeliness and accuracy of CT reports | ||||||
| Yes (%) | 471 (81.3) | 208 (94.1) | 147 (75) | 116 (72) | 181 (89.2) | 290 (77.1) |
| Partly (%) | 88 (15.2) | 13 (5.9) | 39 (20) | 36 (22) | 16 (7.9) | 72 (19.1) |
| No (%) | 20 (3.5) | 0 (0.0) | 10 (5) | 10 (6) | 6 (3.0) | 14 (3.7) |
| Q7. Timeliness and accuracy of 2-mSv CT reports | ||||||
| Yes (%) | 468 (80.8) | 206 (93.2) | 156 (80) | 106 (65) | 182 (89.7) | 286 (76.1) |
| Partly (%) | 98 (16.9) | 15 (6.8) | 31 (16) | 52 (32) | 18 (8.9) | 80 (21.3) |
| No (%) | 13 (2.2) | 0 (0.0) | 9 (5) | 4 (3) | 3 (1.5) | 10 (2.7) |
| Q8. In comparison to natural background radiation† | ||||||
| 0.004-fold (%) | 29 (5.0) | 8 (3.6) | 7 (4) | 14 (9) | 7 (3.4) | 22 (5.9) |
| 0.04-fold (%) | 72 (12.4) | 17 (7.7) | 26 (13) | 29 (18) | 16 (7.9) | 56 (14.9) |
| 0.4-fold (%) | 77 (13.3) | 28 (12.7) | 22 (11) | 27 (17) | 26 (12.8) | 51 (13.6) |
| 4-fold‡ (%) | 200 (34.5) | 100 (45.2) | 63 (32) | 37 (23) | 84 (41.4) | 116 (30.9) |
| 40-fold (%) | 124 (21.4) | 48 (21.7) | 43 (22) | 33 (20) | 46 (22.7) | 78 (20.7) |
| 400-fold (%) | 77 (13.3) | 20 (9.0) | 35 (18) | 22 (14) | 24 (11.8) | 53 (14.1) |
| Q9. Evidence level of carcinogenic risk† | ||||||
| Yes (%) | 181 (31.3) | 67 (30.3) | 83 (42) | 31 (19) | 71 (35.0) | 110 (29.3) |
| Partly (%) | 173 (29.9) | 56 (25.3) | 59 (30) | 58 (36) | 61 (30.0) | 112 (29.8) |
| No (%) | 225 (38.9) | 98 (44.3) | 54 (28) | 73 (45) | 71 (35.0) | 154 (41.0) |
Data are number of participants (and percentages). Shade of each cell indicates percentage categorized as follows: 0–20%, 21–40%, 41–60%, 61–80%, or 81–100%. Each percentage is that of given response out of all participants of that category. Darker shade represents higher percentage. Percentages may not add up to 100% because of rounding. For questions regarding willingness or acceptance, “yes” indicated ‘completely and consistently’ while “partly” indicated ‘not consistently but selectively (e.g., during working hours)’. For Q2, participant could choose one or more answers. *These questions were asked to only 421 participants who responded as “partly” or “no” to Q1, †Estimation of carcinogenic risk of conventional-dose CT radiation, ‡Considered as accurate estimate.
There were small but still statistically significant variations in the response pattern across the participants' departments or job titles (Table 3) (Supplementary Fig. 1). On the other hand, there was considerable inter-hospital variation in the willingness to immediately change to 2-mSv CT (Q1) (Supplementary Fig. 2).
The multivariable logistic regression analysis showed that willingness was significantly associated with attendings (p = 0.004), intention to maintain the dedicated appendiceal CT protocol in the hospital information system (p < 0.001), belief in compelling evidence on the carcinogenic risk of CT radiation (p = 0.028), and hospitals having more than 1000 beds (p = 0.031) (Supplementaly Table 3).
Nine months after LOCAT patient recruitment was completed, the institutional standard radiation dose for appendiceal CT in adolescents and young adults was set as 2-, 4-, 5-, 6-, 8-, and 10-mSv in 14, 2, 1, 1, 1, and 1 hospital(s), respectively. Four hospitals were using the dedicated appendiceal CT protocol in the hospital information system consistently in adolescents and young adults with suspected appendicitis, six were partly using the dedicated protocol, and ten abandoned the dedicated protocol in their usual practice.
DISCUSSION
Our survey, which was conducted during the final phase of LOCAT, showed that 375 of the 579 participating care providers (64.8%) were willing to use 2-mSv CT selectively (“partly”), and 46 (7.9%) were not willing to use 2-mSv CT. Despite the extensive efforts over the years of LOCAT design and conduct, the survey results showed difficulties in the reality of implementing 2-mSv CT in usual practice. First, not all participants were enthusiastic about the change to 2-mSv. The participants who responded as “partly” or “no” to Q1 cited “low image quality” or “impaired diagnostic performance” as the main reasons for their reluctance to the change to 2-mSv CT. It is disappointing that such a large number of care providers, even though they were from hospitals participating in LOCAT, were still unaware of or disregarded previous study results consistently showing that a radiation dose of around 2-mSv in appendiceal CT is comparable to conventional doses regarding diagnostic performance and clinical outcomes (5,6,7,8,9,10). Second, 6 of the 20 sites withdrew the institutional standard dose from 2-mSv to higher doses in usual practice nine months after the completion of LOCAT patient recruitment after the completion of LOCAT patient recruitment. Although these results may sound partly disappointing, they could be expected considering the known vast disparity between research studies and clinical practice regarding CT radiation dose (11). In addition, further follow-up and audits are needed to confirm that the use of 2-mSv CT will be truly sustained and consistent. It would be particularly interesting if the care providers' knowledge of LOCAT results could affect their willingness to use 2-mSv CT.
Our subgroup analyses revealed that several care provider or hospital characteristics were associated with the willingness to change to 2-mSv CT. Specifically, in the multivariable analysis, willingness was significantly associated with attendings, intention to maintain the dedicated appendiceal CT protocol in the hospital information system, belief in compelling evidence on the carcinogenic risk of CT radiation, and hospitals having more than 1000 hospital beds. These results tell us which characteristics represent challenges in implementing 2-mSv CT in usual practice. Therefore, for a successful implementation, the reluctant care providers and sites should be the focus of further education and encouragement.
Interestingly, willingness was not significantly associated with the number of patients enrolled in LOCAT, indicating that prior institutional experience in low-dose CT may not be an important factor affecting the perceived preparedness for using low-dose CT. Willingness was not significantly associated with the use of iterative reconstruction. Previous studies have not shown significant clinical or diagnostic advantages of iterative reconstruction techniques in 2-mSv appendiceal CT (10,18). However, newer iterative reconstruction techniques may show more obvious advantages in the future, particularly at even lower radiation doses. Willingness was significantly associated with the belief in compelling evidence on the carcinogenic risk of CT radiation, but not with the particular knowledge of conventional-dose CT radiation in comparison to natural background radiation. These findings may indicate that future education aiming at low-dose CT practice should focus on the health effects of radiation than numerical comparisons of radiation doses.
Importantly, the willingness or reluctance varied only slightly across the participants' departments or job titles, but considerably across the hospitals. This reflects the fact that the implementation of 2-mSv CT practice is a matter of a hospital system rather than of individual department or job title (19). Therefore, successful implementation requires hospital-wide, systematic, and collaborative efforts. Although we did not show it in the present study, we believe that one requisite for successful implementation of 2-mSv CT would likely be a motivated lead radiologist championing the use of 2-mSv CT through persistent efforts such as education of colleague care providers (20), regular audits of doses, and constructive feedback to reluctant care providers.
To our knowledge, our study was one of the largest surveys for care providers' willingness to adopt a new imaging protocol. Our survey involved 579 participants from 20 hospitals, including 221 radiologists, 196 emergency physicians, and 162 surgeons. The participants had different levels of clinical experience, including 376 trainees, which reflect the usual practice pattern for suspected appendicitis in the catchment area, South Korea. Our study showed a reasonably high overall response rate (83.0%), particularly for radiologists (97.4%).
Our study had limitations. First, notwithstanding the large scale and high response rate, our survey results may not apply to other care providers in different settings. All the 20 sites were teaching hospitals and voluntarily participated in LOCAT. They may have been more motivated or resourced towards the use of standardized 2-mSv CT practice than average hospitals. The adoption would be even more difficult if all institutions in real-world practice (including those that declined to participate in the trial) are considered. Second, our survey based on voluntary participation carried the risk that participants may have had higher willingness to use 2-mSv CT than non-participants. This is a fundamental limitation of any survey study. Third, due to limitations of LOCAT data, we were unable to test the association of willingness to use 2-mSv CT and individual care providers' active participation in LOCAT. Instead, we showed that the per-site number of enrolled patients in LOCAT was not significantly associated with the willingness.
In conclusion, we attempted to systematically incorporate a 2-mSv appendiceal CT technique into the usual practice in 20 hospitals through the course of a large pragmatic clinical trial. At the final phase of the trial, 64.8% of the 579 care providers involved in the trial were willing to use 2-mSv CT selectively, and 7.9% were not willing to use 2-mSv CT for adolescents and young adults with suspected appendicitis. Further practical efforts are needed beyond scientific evidence to implement 2-mSv CT in usual practice.
Footnotes
This study was supported by grants from the Dong Kook Pharm. Co., Ltd. (DR 16-03) and the Korea Health Technology R&D Project of the Korea Health Industry Development Institute (KHIDI), funded by the Ministry of Health & Welfare, Republic of Korea (No. HI13C0004 and HI15C1052). This research work was a part of the investigations of LOCAT (Low-dOse CT for acute Appendicitis Trial) Group, which was endorsed by the Radiology Imaging Network of Korea for Clinical Research (RINK-2015-003).
Conflicts of Interest: The authors have no potential conflicts of interest to disclose.
Supplementary Materials
The Data Supplement is available with this article at https://doi.org/10.3348/kjr.2019.0010.
Q10 Commitment to Responses
Participant Job Title and Clinical Experience
Willingness to immediately change to 2-mSv CT (Q1), categorized by participants' department (A) and job title (B). For responses, “yes” indicated ‘completely and consistently’ while “partly” indicated ‘not consistently but selectively (e.g., during working hours).’
Stacked bar graph shows per site survey responses for willingness to immediately change to 2-mSv CT (Q1). Length of each stack indicates percentage of participants in category. Each number is that of participants included in stack. Nine months after completion of Low-dOse CT for Appendicitis Trial patient recruitment, radiation dose for appendiceal CT in usual practice for adolescents and young adults was 2-mSv in 14 sites (denoted as *), 4-mSv in two sites (denoted as †), and 5-mSv or higher in four sites (denoted as ‡). For responses, “yes” indicated ‘completely and consistently’ while “partly” indicated ‘not consistently but selectively (e.g., during working hours).’ LDCT = low-dose CT
Multivariable Logistic Regression Analysis for Willingness to Immediately Change to 2-mSv CT
References
- 1.Bhangu A, Søreide K, Di Saverio S, Assarsson JH, Drake FT. Acute appendicitis: modern understanding of pathogenesis, diagnosis, and management. Lancet. 2015;386:1278–1287. doi: 10.1016/S0140-6736(15)00275-5. [DOI] [PubMed] [Google Scholar]
- 2.Drake FT, Florence MG, Johnson MG, Jurkovich GJ, Kwon S, Schmidt Z, et al. SCOAP Collaborative. Progress in the diagnosis of appendicitis: a report from Washington State's Surgical Care and Outcomes Assessment Program. Ann Surg. 2012;256:586–594. doi: 10.1097/SLA.0b013e31826a9602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Park JH LOCAT Group. Diagnostic imaging utilization in cases of acute appendicitis: multi-center experience. J Korean Med Sci. 2014;29:1308–1316. doi: 10.3346/jkms.2014.29.9.1308. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Pearce MS, Salotti JA, Little MP, McHugh K, Lee C, Kim KP, et al. Radiation exposure from CT scans in childhood and subsequent risk of leukaemia and brain tumours: a retrospective cohort study. Lancet. 2012;380:499–505. doi: 10.1016/S0140-6736(12)60815-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Yoon HM, Suh CH, Cho YA, Kim JR, Lee JS, Jung AY, et al. The diagnostic performance of reduced-dose CT for suspected appendicitis in paediatric and adult patients: a systematic review and diagnostic meta-analysis. Eur Radiol. 2018;28:2537–2548. doi: 10.1007/s00330-017-5231-z. [DOI] [PubMed] [Google Scholar]
- 6.Yun SJ, Ryu CW, Choi NY, Kim HC, Oh JY, Yang DM. Comparison of low- and standard-dose CT for the diagnosis of acute appendicitis: a meta-analysis. AJR Am J Roentgenol. 2017;208:W198–W207. doi: 10.2214/AJR.16.17274. [DOI] [PubMed] [Google Scholar]
- 7.Kim SY, Lee KH, Kim K, Kim TY, Lee HS, Hwang SS, et al. Acute appendicitis in young adults: low-versus standard-radiation-dose contrast-enhanced abdominal CT for diagnosis. Radiology. 2011;260:437–445. doi: 10.1148/radiol.11102247. [DOI] [PubMed] [Google Scholar]
- 8.Seo H, Lee KH, Kim HJ, Kim K, Kang SB, Kim SY, et al. Diagnosis of acute appendicitis with sliding slab ray-sum interpretation of low-dose unenhanced CT and standard-dose i.v. contrast-enhanced CT scans. AJR Am J Roentgenol. 2009;193:96–105. doi: 10.2214/AJR.08.1237. [DOI] [PubMed] [Google Scholar]
- 9.Kim K, Kim YH, Kim SY, Kim S, Lee YJ, Kim KP, et al. Low-dose abdominal CT for evaluating suspected appendicitis. N Engl J Med. 2012;366:1596–1605. doi: 10.1056/NEJMoa1110734. [DOI] [PubMed] [Google Scholar]
- 10.LOCAT Group. Low-dose CT for the diagnosis of appendicitis in adolescents and young adults (LOCAT): a pragmatic, multicentre, randomised controlled non-inferiority trial. Lancet Gastroenterol Hepatol. 2017;2:793–804. doi: 10.1016/S2468-1253(17)30247-9. [DOI] [PubMed] [Google Scholar]
- 11.Weisenthal K, Karthik P, Shaw M, Sengupta D, Bhargavan-Chatfield M, Burleson J, et al. Evaluation of kidney stones with reduced-radiation dose CT: progress from 2011-2012 to 2015-2016-Not there yet. Radiology. 2018;286:581–589. doi: 10.1148/radiol.2017170285. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Ahn S LOCAT group. LOCAT (low-dose computed tomography for appendicitis trial) comparing clinical outcomes following low- vs standard-dose computed tomography as the first-line imaging test in adolescents and young adults with suspected acute appendicitis: study protocol for a randomized controlled trial. Trials. 2014;15:28. doi: 10.1186/1745-6215-15-28. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Brown TW, McCarthy ML, Kelen GD, Levy F. An epidemiologic study of closed emergency department malpractice claims in a national database of physician malpractice insurers. Acad Emerg Med. 2010;17:553–560. doi: 10.1111/j.1553-2712.2010.00729.x. [DOI] [PubMed] [Google Scholar]
- 14.Dixon AK, Goldstone KE. Abdominal CT and the Euratom Directive. Eur Radiol. 2002;12:1567–1570. doi: 10.1007/s00330-001-1268-z. [DOI] [PubMed] [Google Scholar]
- 15.United Nations. Report of the United Nations Scientific Committee on the effects of atomic radiation: sixtyfifth session. United Nations; 2018. [Accessed August 2, 2018]. Available at: https://documents-dds-ny.un.org/doc/UNDOC/GEN/V08/558/99/PDF/V0855899.pdf?OpenElement. [Google Scholar]
- 16.Motulsky H. Graphing continous data. In: Motulsky H, editor. Intuitive biostatistics: a nonmathematical guide to statistical thinking. 4th ed. New York, NY: Oxford University Press; 2018. pp. 63–74. [Google Scholar]
- 17.Motulsky H. Multiple regression. In: Motulsky H, editor. Intuitive biostatistics: a nonmathematical guide to statistical thinking. 4th ed. New York, NY: Oxford University Press; 2018. pp. 378–394. [Google Scholar]
- 18.Park JH, Kim B, Kim MS, Kim HJ, Ko Y, Ahn S, et al. Comparison of filtered back projection and iterative reconstruction in diagnosing appendicitis at 2-mSv CT. Abdom Radiol (NY) 2016;41:1227–1236. doi: 10.1007/s00261-015-0632-4. [DOI] [PubMed] [Google Scholar]
- 19.Park SB, Kim MJ, Ko Y, Sim JY, Kim HJ, Lee KH LOCAT Group. Structured reporting versus free-text reporting for appendiceal computed tomography in adolescents and young adults: preference survey of 594 referring physicians, surgeons, and radiologists from 20 hospitals. Korean J Radiol. 2019;20:246–255. doi: 10.3348/kjr.2018.0109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Goo HW. CT radiation dose optimization and estimation: an update for radiologists. Korean J Radiol. 2012;13:1–11. doi: 10.3348/kjr.2012.13.1.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Q10 Commitment to Responses
Participant Job Title and Clinical Experience
Willingness to immediately change to 2-mSv CT (Q1), categorized by participants' department (A) and job title (B). For responses, “yes” indicated ‘completely and consistently’ while “partly” indicated ‘not consistently but selectively (e.g., during working hours).’
Stacked bar graph shows per site survey responses for willingness to immediately change to 2-mSv CT (Q1). Length of each stack indicates percentage of participants in category. Each number is that of participants included in stack. Nine months after completion of Low-dOse CT for Appendicitis Trial patient recruitment, radiation dose for appendiceal CT in usual practice for adolescents and young adults was 2-mSv in 14 sites (denoted as *), 4-mSv in two sites (denoted as †), and 5-mSv or higher in four sites (denoted as ‡). For responses, “yes” indicated ‘completely and consistently’ while “partly” indicated ‘not consistently but selectively (e.g., during working hours).’ LDCT = low-dose CT
Multivariable Logistic Regression Analysis for Willingness to Immediately Change to 2-mSv CT