Abstract
Positive memory characteristics relate to posttraumatic stress disorder (PTSD) severity. We utilized a network approach to examine relations between PTSD clusters (intrusions, avoidance, negative alterations in cognitions and mood [NACM], alterations in arousal and reactivity [AAR]) and positive memory characteristics (count, valence, vividness, coherence, time perspective, sensory details). We identified differential relations between PTSD clusters and positive memory characteristics, and central/bridging symptoms. Participants were an Amazon Mechanical Turk-recruited sample of 206 participants (Mage = 35.36; 61.20% females). We estimated a regularized Gaussian Graphic Model comprising four nodes representing the PTSD clusters and six nodes representing positive memory characteristics. Regarding cross-community relations, AAR (highest node strength) was negatively associated with positive memory count, valence, coherence, and access; avoidance was positively and negatively associated with positive memory vividness and count respectively. The NACM-AAR and intrusion-avoidance edges were significantly stronger than most edges. From the PTSD community, AAR and avoidance had the highest bridge strength and bridge expected influence respectively; from the positive memory community, coherence and vividness had the highest bridge strength and bridge expected influence respectively. Results indicate the potential pivotal role of AAR, avoidance, coherence, and vividness in the PTSD-positive memory relation, which renders them assessment/treatment targets pending further investigation.
Keywords: PTSD, positive memories, network analyses, trauma
1. Introduction
Substantial evidence indicates that beyond traumatic memories, positive memory characteristics (processes such as retrieval difficulties and phenomenological qualities such as reduced accessibility of details) also contribute to posttraumatic stress disorder’s (PTSD) etiology and maintenance (Bernsten & Rubin, 2007; Contractor, Brown, et al., 2018; Hauer, Wessel, Engelhard, Peeters, & Dalgleish, 2009). Further, traumatic memories differ from positive memories on important phenomenological qualities (Byrne, Hyman, & Scott, 2001; Peace & Porter, 2004). Yet, most clinical work primarily targets only traumatic memories (Bernsten & Rubin, 2007; Schnurr, 2017), and rarely are PTSD symptoms investigated in relation to positive memory characteristics (Bohanek, Fivush, & Walker, 2005). Addressing this gap, the current study explored associations between PTSD symptom clusters and positive memory characteristics.
Difficulties with positive memory characteristics may render the onset/maintenance of PTSD more likely post-trauma (vulnerability hypothesis), or may be consequences of trauma/PTSD symptoms (scarring hypothesis; Williams et al., 2007). Examples of such positive memory characteristics include few salient pre-trauma positive experiences and corresponding memories (Hauer et al., 2009), genetic factors contributing to decreased encoding of positive memories (Dominique et al., 2012), difficulties retrieving and/or retaining positive memories (Porter & Peace, 2007; Williams et al., 2007), difficulties integrating positive memories with other autobiographical memories (Bernsten & Rubin, 2007; Berntsen & Rubin, 2006), attentional biases towards negative information and memories (Aupperle, Melrose, Stein, & Paulus, 2012; Fani et al., 2012; Sutherland & Bryant, 2005), rumination on negative memories cued by trauma reminders (Ehlers & Clark, 2000), and emotional numbing/dysregulation symptoms (Litz, Orsillo, Kaloupek, & Weathers, 2000; Weiss, Dixon-Gordon, Peasant, & Sullivan, 2018). Thus, there may be a bi-directional relation between positive memory characteristics and PTSD symptoms. Further, although not directly addressed, trauma theories implicitly reference positive memories in PTSD’s etiology and/or treatment. As an example, for Janoff-Bulman’s (1992) theory of shattered assumptions wherein traumatic events alter self-related beliefs, perhaps, eliciting positive memories may alter belief structures to facilitate a positive reframing of the trauma and posttraumatic growth (Brewin & Holmes, 2003). As another example, for conditioning and associative network theories, where integrating corrective information into the trauma memory is central to therapeutically weakening the fear network (Brewin & Holmes, 2003), perhaps eliciting positive and non-threatening memories (even those with conditioned stimuli) can aid therapeutic extinction and habituation. Unsurprisingly, intervention research supports an inverse relation between accessing specific (positive) memories and PTSD symptom severity (Moradi et al., 2014; Raes, Williams, & Hermans, 2009).
Indeed, trauma-exposed individuals with PTSD (McNally, Lasko, Macklin, & Pitman, 1995; Sutherland & Bryant, 2005), including those with probable PTSD as assessed by self-report measures (Megías, Ryan, Vaquero, & Frese, 2007), experience difficulties accessing positive memories. Beyond accessibility, other phenomenological qualities of positive memories have an established relation with trauma/PTSD severity; examples include valence (rating of memories as positive or negative), vividness (visual intensity and clarity), coherence (degree to which memories have a logical narrative), time perspective (ability to recall temporal information of an event), and sensory details (degree of re-experiencing non-visual sensory information during recall; Sutin & Robins, 2007). To elaborate, research indicates fewer emotional components (Porter & Birt, 2001), vividness (Peace, Porter, & Brinke, 2008), sensory details (Peace et al., 2008; Porter & Birt, 2001), and coherence (Berliner, Hyman, Thomas, & Fitzgerald, 2003; Fivush, Hazzard, Sales, Sarfati, & Brown, 2002) for positive vs. traumatic/negative memories among trauma-exposed samples; among these studies, only Berliner et al. (2003) reported number of individuals with a PTSD diagnosis (i.e., 5). Further, trauma-exposed participants have reported difficulties in remembering temporal details of positive memories (Peace & Porter, 2004); although such difficulties have been unrelated to PTSD severity (Megías et al., 2007).
However, some contradictory research indicates greater vividness in partly trauma-exposed samples (Byrne et al., 2001), sensory details in (partly or entirely) trauma-exposed samples (Berliner et al., 2003; Byrne et al., 2001), and coherence in samples reporting negative events (Bohanek et al., 2005; Porter & Birt, 2001; Waters, Bohanek, Marin, & Fivush, 2013) for positive vs. traumatic memories. For instance, Niziurski, Johannessen, and Berntsen (2018) found increasing coherence of positive memories with increasing PTSD severity in deployed soldiers. As an explanation, elevated emotional distress (Engelhard, van den Hout, & McNally, 2008; McNally, 2003) and affect intensity (Rubin, Boals, & Berntsen, 2008; Tull, Jakupcak, McFadden, & Roemer, 2007) among trauma-exposed samples may enhance the recall of positive memory phenomenological qualities. Complicating this issue, Bray, Brewer, Cameron, and Nixon (2018) found no comparative difference in the coherence of positive and negative narratives among children with high vs. low PTSD severity, Berliner et al. (2003) found that children receiving trauma intervention reported no difference in temporal details of their positive and traumatic memories, and some research indicates no comparative difficulties in recalling non-visual sensory details of positive and negative event memories (Byrne et al., 2001; Waters et al., 2013) even when comparing individuals with high vs. low PTSD severity (Megías et al., 2007).
This pattern of mixed findings may be attributed to differences in methodology and sample characteristics (Sotgiu & Mormont, 2008). Notably, few studies have examined PTSD severity in relation to positive memory characteristics (e.g., Gray & Lombardo, 2001; McKinnon, Brewer, Meiser-Stedman, & Nixon, 2017; Megías et al., 2007; Niziurski et al., 2018). Among such studies, none to our knowledge has examined the heterogeneous DSM-5 PTSD symptom clusters (intrusions, avoidance, negative alterations in cognitions and mood [NACM], alterations in arousal/reactivity [AAR]) which differentially relate to clinical correlates (Contractor, Armour, Forbes, & Elhai, 2016; Contractor et al., 2014; Contractor, Frankfurt, Weiss, & Elhai, 2017; Contractor, Greene, Dolan, & Elhai, 2018). Lastly, in investigating relations of singular positive memory characteristics to PTSD severity, interrelationships are discounted wherein the influence of all variables on each other is not considered, thus, yielding incomplete and/or un-interpretable results (Byrne et al., 2001; Waters et al., 2013). Addressing these limitations and drawing from an established relation between PTSD and positive memory characteristics with the nature of their relation being debatable/uncertain, the current study used network modeling to examine inter-relationships between PTSD symptom clusters and positive memory characteristics.
A network framework has been widely applied to the cross-sectional study of PTSD symptoms (Afzali et al., 2017; Armour, Fried, Deserno, Tsai, & Pietrzak, 2017; Ross, Murphy, & Armour, 2018). Relevant to the current study, PTSD symptoms and positive memory characteristics can be viewed as a network of mutually interacting and reinforcing symptoms which may/may not be causally connected in a direct manner (Epskamp, Borsboom, & Fried, 2018; McNally et al., 2015). For example, PTSD AAR symptoms may diminish one’s cognitive capacity reducing count/details of retrieved positive memories (Contractor, Banducci, Dolan, Keegan, & Weiss, in press; Harvey, Bryant, & Dang, 1998); this in turn, may increase or maintain negative affect/cognitions, intrusion of traumatic memories, and PTSD severity. Thus, certain PTSD symptoms may contribute to deficits in positive memory characteristics, while some positive memory characteristics may enhance the risk of developing/maintaining PTSD severity; such PTSD symptoms and positive memory characteristics would be considered bridge symptoms of this network (Cramer, Waldorp, van der Maas, & Borsboom, 2010b). An added advantage of a network framework is the ability to account/control for the influence of all variables when examining unique relations between two singular symptoms within or across constructs such as PTSD AAR symptoms and count of positive memories (i.e., partial correlations; Borsboom & Cramer, 2013). Such an approach further permits examining the influence of two variables on a third variable beyond just a direct relation between any two variables (Pearl, 2000), and considers the interaction between all symptoms in understanding construct co-occurrence (Fried & Cramer, 2017). Notably, PTSD network research, so far, has indicated least centrality (fewer and weaker connections) for PTSD’s memory impairment symptom (Armour et al., 2017; McNally et al., 2015), as supported by corresponding factor-analytical research (Contractor, Caldas, Dolan, Lagdon, & Armour, 2018; Contractor, Caldas, Dolan, Natesan, & Weiss, 2019). However, the amnesia symptom is specific to a traumatic memory; positive memory characteristics have not been examined in relation to PTSD severity using network analyses.
The current study, thus, examined the utility of the network methodology to examine the relation between PTSD symptom clusters and positive memory characteristics within a cross-sectional framework. We investigated (1) differential relations of PTSD symptom clusters with positive memory characteristics; and (2) most central (strongly connected) symptoms accounting for overall connectedness in the network as well as symptoms with the strongest cross-community/construct connections (bridge centrality). By incorporating critical correlates such as positive memory characteristics beyond PTSD-related symptoms in the network system (Fried & Cramer, 2017) and examining central symptoms (including bridge centrality) and differential relations in a network (Ross et al., 2018), results may outline possible mechanisms underlying their co-occurrence and inform future studies examining onset/maintenance of these constructs (Cramer, Waldorp, van der Maas, & Borsboom, 2010a; Fried & Cramer, 2017).
2. Methods
2.1. Procedure and Participants
The study was approved by [redacted] Institutional Review Board and was conducted in accordance with the Declaration of Helsinki. We recruited participants via Amazon’s Mechanical Turk (MTurk) platform and described the study as an examination of the relation between positive memory recall/processes and emotional distress indicators among individuals experiencing stressful life events. Inclusionary criteria were: >/=18 years, working knowledge of English, endorsement of a stressful life experience, and no current/previous diagnosis of sleep apnea. Participation was restricted to MTurk individuals from the US with a > 90% approval rating (i.e., proportion of MTurk surveys completed by a participant that were approved by researchers) consistent with implemented practices to increase the validity of MTurk-obtained data (Hauser & Schwarz, 2016; Shapiro, Chandler, & Mueller, 2013). Eligible participants who provided informed consent after reviewing a full description of study procedures and completed the entire survey validly received $1.50 as compensation.
2.2. Exclusions, Missing Data, and Sample Characteristics
A total of 695 participants attempted the survey; we excluded 299 responses because they were duplicates due to multiple attempts (remainder n = 466). We excluded 89 individuals who did not meet inclusionary criteria, 138 individuals for failing validity checks included to ensure attention and comprehension (Meade & Craig, 2012; Oppenheimer, Meyvis, & Davidenko, 2009), one individual for not endorsing any traumatic event on the Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013), and 32 individuals who did not follow the Memory Experiences Questionnaire–Short Form (MEQ-SF; Luchetti & Sutin, 2016) instructions. The final sample included 206 individuals who averaged 35.36 years of age (SD = 11.50); 126 were female (61.20%). Eighty-eight (42.70%) participants had probable PTSD based on the PTSD Checklist for DSM-5 (PCL-5; F.W. Weathers et al., 2013) cut-off score > 31 (Bovin et al., 2016; Wortmann et al., 2016). Detailed information on demographics and psychopathology variables is provided in Table 1. The network was estimated using complete pairwise observations (i.e., using all available data).
Table 1.
Descriptive characteristics of the sample
| Variable | Mean (SD) |
|---|---|
| Age | 35.36 (11.50) |
| Years of schooling | 15.37 (2.36) |
| Count of recalled positive memories | 7.56 (2.11) |
| Accessibility of positive memory | 4.36 (0.87) |
| Valence of positive memory | 4.60 (0.68) |
| Vividness of positive memory | 4.39 (0.76) |
| Coherence of positive memory | 4.19 (0.79) |
| Time perspective of positive memory | 3.96 (0.84) |
| Sensory details of positive memory | 4.01 (0.78) |
| PTSD intrusions | 1.47 (1.07) |
| PTSD avoidance | 1.68 (1.25) |
| PTSD NACM | 1.29 (1.04) |
| PTSD AAR | 1.28 (1.02) |
| n (%) | |
| Gender | |
| Male | 78 (37.90%) |
| Female | 126 (61.20%) |
| Transgender | 1 (.50%) |
| Gender queer | 1 (.50%) |
| Employment status | |
| Part time | 31 (15.00%) |
| Full time | 146 (70.90%) |
| Retired | 4 (1.90%) |
| Unemployed | 20 (9.70%) |
| Unemployed student | 5 (2.40%) |
| Relationship status | |
| Single | 65 (31.60%) |
| Living with significant other | 36 (17.50%) |
| Married | 84 (40.80%) |
| Divorced | 18 (8.70%) |
| Separated | 2 (1.00%) |
| Widowed | 1 (.50%) |
| Ethnicity | |
| Hispanic or Latino | 17 (8.30%) |
| Not Hispanic or Latino | 186 (90.30%) |
| Unknown | 3 (1.50%) |
| Racial status (could endorse more than one category) | |
| Caucasian or White | 171 (83.00%) |
| African American or Black | 27 (13.10%) |
| Asian | 8 (3.90%) |
| American Indian or Alaskan Native | 7 (3.40%) |
| Native Hawaiian/other Pacific Islander | 1 (.50%) |
| Unknown | 1 (.50%) |
| Income | |
| Less than $15,000 | 15 (7.30%) |
| $15,000 – $24,999 | 26 (12.60%) |
| $25,000 – $34,999 | 18 (8.70%) |
| $35,000 – $49,999 | 43 (20.90%) |
| $50,000 – $64,999 | 43 (20.90%) |
| $65,000 – $79,999 | 24 (11.70%) |
| $80,000 and higher | 37 (18.00%) |
| Treatment for mental health/emotional problem (could endorse more than one category) | |
| Currently in therapy | 29 (14.10%) |
| Been in therapy in the past | 90 (43.70%) |
| Currently taking medications for mental health/emotional problem | 44 (21.40%) |
| Have taken medications in the past for mental health/emotional problem | 59 (28.60%) |
| Never received treatment (therapy/medications) for mental health/emotional problem | 78 (37.90%) |
| Worst traumatic event endorsed on the LEC-5 | |
| Natural disaster | 26 (12.60%) |
| Fire or explosion | 5 (2.40%) |
| Transportation accident | 33 (16.00%) |
| Serious accident at work/home/during recreational activity | 9 (4.40%) |
| Exposure to a toxic substance | 0 (0%) |
| Physical assault | 16 (7.80%) |
| Assault with a weapon | 7 (3.40%) |
| Sexual assault | 34 (16.50%) |
| Other unwanted/uncomfortable sexual experience | 8 (3.90%) |
| Combat or exposure to war | 1 (.50%) |
| Forced captivity | 0 (0%) |
| Life-threatening illness | 11 (5.30%) |
| Severe human suffering | 3 (1.50%) |
| Sudden, violent death | 15 (7.30%) |
| Sudden, accidental death | 15 (7.30%) |
| Serious injury/harm/death you caused to someone else | 4 (1.90%) |
| None of these events happened to me | 19 (9.20%) |
Note. PTSD is posttraumatic stress disorder; NACM is negative alternations in cognitions and mood; AAR is alterations in arousal and reactivity; LEC-5 is Life Events Checklist for DSM-5; valid percentages were used to account for missing data.
2.3. Measures
2.3.1. Demographic information.
We obtained information on age, gender, income, relationship status, racial and ethnic status, educational level, and mental health treatment.
2.3.2. Life Events Checklist for DSM-5 (LEC-5; Weathers et al., 2013).
The LEC-5 is a 17-item self-report measure that evaluates exposure to lifetime traumatic events. An 18th item evaluated the most distressing traumatic event, and the subsequent PTSD measure was completed in reference to this endorsed trauma. Participants indicated their exposure to each event on a 6-point nominal scale: happened to me, witnessed it, learned about it, part of my job, not sure, and does not apply. In the current study, endorsing either of the first four response options for LEC-5 items 1–16 was considered as a positive endorsement of a trauma consistent with the DSM-5 Criterion A (American Psychiatric Association, 2013).
2.3.3. PTSD Checklist for DSM-5 (PCL-5; Weathers et al., 2013).
The PCL-5 is a 20-item self-report measure assessing PTSD symptom severity referencing the past month. Response options range from 0 (not at all) to 4 (extremely). The PCL-5 has excellent psychometric properties (Bovin et al., 2016; Wortmann et al., 2016). Intrusions, avoidance, NACM, and AAR subscale scores were computed as an average of the items comprising each domain; Cronbach’s α values were .90, .86, .89, and .87, respectively.
2.3.4. Autobiographical Memory Test (AMT; Williams & Broadbent, 1996).
The AMT examined the count of recalled positive memories. Participants viewed 10 positively-valenced cue words, specifically: friendly, happy, honest, kind, humorous, cheer, pleased, relieved, lively, and glorious (Kleim & Ehlers, 2008; McNally et al., 1995), and then received a prompt to recall one specific and meaningful memory of an event to each cue word within 60 seconds (J. M. Williams & Broadbent, 1996). Instructions for this task were adapted from previous studies examining autobiographical memory recall (Henderson, Hargreaves, Gregory, & Williams, 2002; Williams et al., 1996; Zinbarg, Rekart, & Mineka, 2006). All AMT responses were coded as recalled (specific [memory of an event that occurred in a certain place within one day], extended [memory of an event that lasted longer than one day], or categoric [memory as a summary of many repeated events]) or failed to recall (semantic associate [no personal memory], omission [did not recall the memory within 60 seconds or unable to recall a memory], or non-positive) based on previous studies (Griffith et al., 2009; Sutherland & Bryant, 2008). Following the Coding and Assessment System for Narratives of Trauma (CASNOT; Fernández-Lansac & Crespo, 2017), a memory description was coded as non-positive if the emotional tone and/or the emotional valence of the description was rated as mainly negative (i.e., scores of 3–4 on a scale from 0 [completely positive] to 4 [completely negative]). For the current study, the total number of AMT responses coded as recalled was used as the “count of positive memories” variable (range was 0–10 for each participant).
2.3.5. Memory Experiences Questionnaire–Short Form (MEQ-SF; Luchetti & Sutin, 2016).
The MEQ-SF examines 10 phenomenological qualities of a positive memory. For the current study, we specifically used six subscales assessing accessibility and content details (valence, vividness, time perspective, sensory details, coherence) based on the research questions and a small sample size insufficient to incorporate all 10 MEQ-SF subscales. Response options on each subscale ranged from 1 (strongly disagree) to 5 (strongly agree); subscale scores were calculated as an average of the items comprising each domain. In the current study, participants were asked to recall one specific, positively valanced memory based on adapted instructions from previous studies (Boyacioglu & Akfirat, 2015; Janssen, Hearne, & Takarangi, 2015; Wing, Schutte, & Byrne, 2006) before completing the MEQ-SF. MEQ-SF memory descriptions were coded using the CASNOT dimensions of emotional tone and valence (Fernández-Lansac & Crespo, 2017) to ensure that they were positively valanced. The MEQ-SF has demonstrated acceptable psychometric properties (Luchetti & Sutin, 2016). Cronbach’s α values in the current study were as follows: accessibility = .82, valence = .71, vividness = .69, time perspective = .50, sensory details = .64, and coherence =.67.
2.4. Statistical Analyses
For a partial correlation network of 11 nodes, we had 55 parameters (Epskamp & Fried, 2018). Following the guidelines of at least 3 individuals per parameter, our sample size was sufficient for exploratory data-driven analyses (Epskamp & Fried, 2018).
2.4.1. Network Estimation, Visualization, and Accuracy.
None of the variables violated normality according to benchmarks of skewness >2 and/or kurtosis >7 (Curran, West, & Finch, 1996); PTSD subscales had skewness values ranging from .13 to .41 and kurtosis values ranging from −1.14 to −.78, and positive memory characteristics had skewness values ranging from −1.87 to −.49 and kurtosis values ranging from −.14 to 2.71. Thus, the appropriate Pairwise Markov Random Field (PRMF) model was the Gaussian Graphical Model (GGM; Costantini et al., 2015), which was used to estimate an undirected network (Cox & Wermuth, 1994; McNally et al., 2015). To reduce the likelihood of spurious edges and obtain a sparse/parsimonious network, we estimated a regularized partial correlation network structure (Pearson correlation) using the graphical least absolute shrinkage and selection operator (glasso; Epskamp & Fried, 2018; Friedman, Hastie, & Tibshirani, 2008), with Extended Bayesian Information Criterion (EBIC; Chen & Chen, 2008) to select a value for the tuning parameter. In the current network, a node indicated a variable of interest (PTSD symptom clusters; count of recalled positive memories; positive memory phenomenological qualities of vividness, valence, coherence, time perspective, sensory details, and accessibility) and an edge depicted a regularized partial correlation between two nodes after controlling statistically for other nodes in the network (Borsboom & Cramer, 2013). For each edge, we examined its weight reflecting strength and sign reflecting direction (Costantini et al., 2019); weights were graphically represented by line thickness (Borsboom & Cramer, 2013; Costantini et al., 2019). The network’s graphical layout was based on the Fruchterman-Reingold algorithm (Fruchterman & Reingold, 1991) which placed connected nodes closer and unconnected nodes farther apart. We used the bootnet (Epskamp et al., 2018) and qgraph (Epskamp, Cramer, Waldorp, Schmittmann, & Borsboom, 2012) packages in R. Finally, to examine network accuracy, we estimated confidence intervals (CIs) on the edge-weights (nonparametric bootstrapping with replacement; Supplementary Figure A. 1) and significant differences between edge-weights (bootstrapped difference test; Supplemental Figure A. 2; Epskamp et al., 2018).
2.4.2. Stability and Accuracy of the Centrality Index.
Using the R package qgraph (Epskamp et al., 2012), we examined the node centrality index to quantify the relative strength of each of the 11 nodes in the network (Costantini et al., 2019; McNally et al., 2015). We calculated node strength, which references the sum of weights (i.e., regularized partial correlation magnitudes) of each edge linked to the node (Epskamp & Fried, 2018) and created this centrality plot. Higher values reflected a node’s greater centrality to the overall network (Epskamp & Fried, 2018). We further examined node strength stability under observing subsets of cases (case-dropping subset bootstrap; Supplemental Figure A. 3; Epskamp et al., 2018) by computing the correlation stability (CS) coefficient implemented in the R package bootnet (Epskamp et al., 2018). This index quantifies the proportion of data that can be dropped to retain a correlation of ≥ .70 with the original centrality coefficient at a 95% certainty level (Epskamp & Fried, 2018). Guidelines suggest to not interpret a centrality index if the CS-coefficient is < .25, and a value of .50 indicates sufficient stability (Costantini et al., 2019; Epskamp & Fried, 2018). Lastly, to estimate node strength accuracy, we computed CIs on strength node and tested for their significant differences (bootstrapped difference test; Supplemental Figure A. 4; Epskamp et al., 2018).
2.4.3. Bridge Centrality.
PTSD symptom clusters and positive memory characteristics represented two distinct communities of nodes based on theory and conceptual meaning. We examined bridge centrality values for nodes across these two communities to examine cross-community connectivity (Jones, Ma, & McNally, 2019, April 25). Using the networktools R package, we computed (1) bridge strength as the sum of absolute values of edges between a node of one community and all nodes of the second community (node’s total connectivity with the other community), and (2) bridge expected influence as the sum of all edges between a node of one community and all nodes of the second community (node’s overall positive connectivity with the other community accounting for positive and negative edges; Jones, 2018; Jones et al., 2019, April 25). Compared to bridge strength, bridge expected influence indicates overall increase in node activation considering that a node may be associated with an increase in activation with some nodes and/or decrease in activation with other nodes (Jones, 2018; Jones et al., 2019, April 25).
3. Results
3.1. Network Estimation, Visualization, and Accuracy.
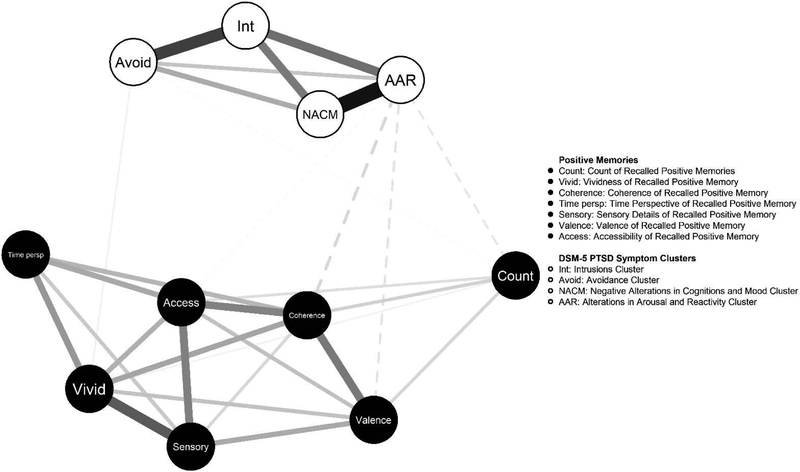
Figure 1 indicates the regularized partial correlation network corresponding to Table 2 values. Examining the edge weights within the PTSD symptom clusters community, the strongest associations were between AAR and NACM (.51), intrusions and avoidance (.38), intrusions and NACM (.25), and intrusions and AAR (.27). Within the positive memory characteristics community, the strongest association were between sensory details and vividness (.31), coherence and valence (.25), coherence and accessibility (.23), and accessibility and sensory details (.24).
Figure 1.
Regularized partial correlation network
Note. Solid lines indicate positive associations; dashed lines indicate negative associations.
Table 2.
Regularized partial correlation matrix
| 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Count of positive memory recall | 0 | .06 | .07 | .02 | .08 | 0 | 0 | 0 | −.01 | 0 | −.04 |
| 2. Accessibility | 0 | .11 | .14 | .23 | .16 | .24 | 0 | 0 | 0 | −.01 | |
| 3. Valence | 0 | .11 | .25 | .07 | .15 | 0 | 0 | 0 | −.06 | ||
| 4. Vividness | 0 | .16 | .19 | .31 | 0 | .02 | 0 | 0 | |||
| 5. Coherence | 0 | .13 | .07 | 0 | 0 | 0 | −.07 | ||||
| 6. Time perspective | 0 | .09 | 0 | 0 | 0 | 0 | |||||
| 7. Sensory Details | 0 | 0 | 0 | 0 | 0 | ||||||
| 8. PTSD intrusion | 0 | .38 | .25 | .27 | |||||||
| 9. PTSD avoidance | 0 | .15 | .10 | ||||||||
| 10. PTSD NACM | 0 | .51 | |||||||||
| 11. PTSD AAR | 0 |
Note. NACM is PTSD’s negative alterations in cognitions and mood cluster; AAAR is PTSD’s alterations in arousal and reactivity cluster.
The cross-community connections were far weaker. Nevertheless, a number of edges were identified, most of which were negative. AAR was negatively associated with coherence of the recalled positive memory (−.07), valence of the recalled positive memory (−.06), count of recalled positive memories (−.04), and accessibility of the recalled positive memory (−.01). Avoidance was positively associated with vividness of the recalled positive memory (.02) and negatively associated with count of recalled positive memories (−.01).
Regarding network accuracy (Supplemental Figures 1 and 2), results indicated that the NACM-AAR edge weight was significantly stronger than other edge weights, excluding the intrusions-avoidance edge weight. Further, the intrusions-avoidance edge weight was significantly stronger than more than approximately two-third of the other edge weights. Additionally, the intrusions-AAR and vividness-sensory details edge weights were significantly stronger than approximately half of the other edge weights.
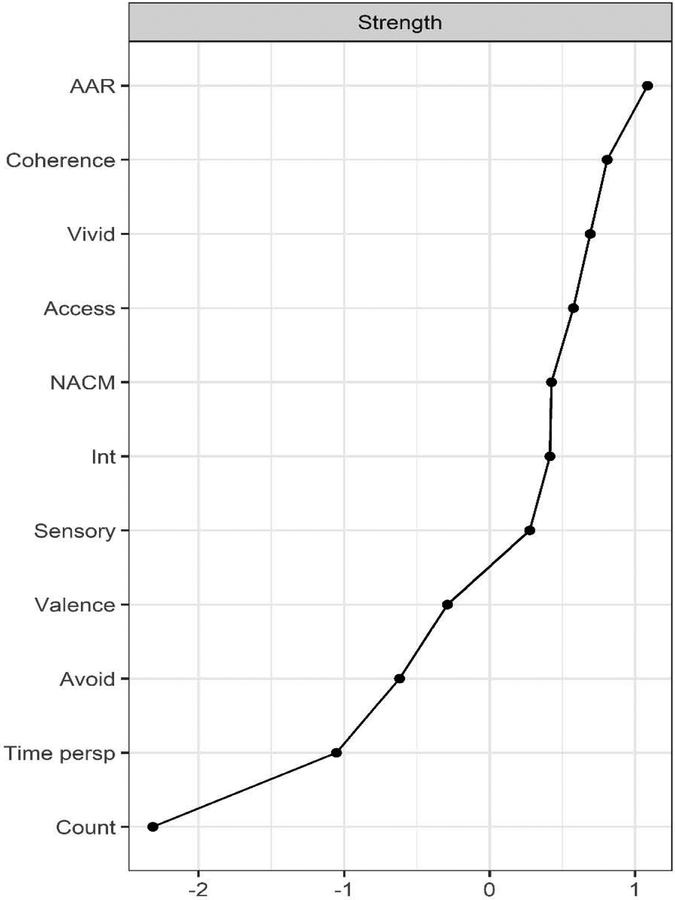
3.2. Centrality Index Estimation (Stability and Accuracy; Supplemental Figures 3 and 4).
The CS-coefficient for node strength (CS[cor = 0.7] = 0.67) indicates interpretability and stability under subsetting cases. According to the centrality plot, there were no significant differences in centrality other than AAR with the highest node strength which was significantly greater than avoidance, count of recalled positive memories, and time perspective. Count of recalled positive memories and time perspective of the recalled positive memory were least central to the overall network.
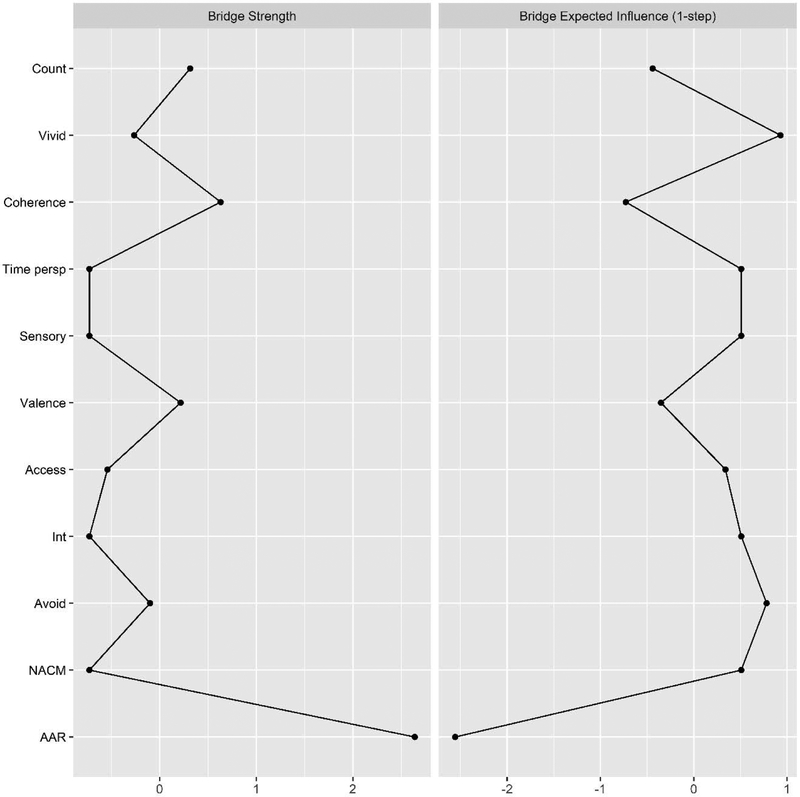
3.3. Bridge Centrality.
Standardized bridge centrality indices are presented in Figure 3. From the PTSD cluster community, AAR with the highest bridge strength value had the highest bridge associations with positive memory characteristics (in either direction). From the positive memory characteristics community, coherence of a recalled positive memory with the highest bridge strength had the highest bridging associations with PTSD symptom clusters (in either direction). In terms of positive connectivity with nodes of another community, avoidance (closely followed by intrusions and NACM) with the highest bridge expected influence value had the most bridge associations with positive memory characteristics, and vividness of a recalled positive memory with the highest bridge expected influence had the most bridge associations with PTSD symptom clusters.
Figure 3.
Bridge centrality
Note. AAR is PTSD’s anxious alterations in arousal and reactivity cluster; NACM is PTSD’s negative alterations in cognitions and mood cluster; Int is PTSD’s intrusions cluster; Avoid is PTSD’s avoidance cluster; coherence is the coherence phenomenological quality of positive memories; vivid is the vividness phenomenological quality of positive memories; access is the accessibility phenomenological quality of positive memories; sensory is the sensory details phenomenological quality of positive memories; valence is the valence phenomenological quality of positive memories; time persp is the time perspective phenomenological quality of positive memories; count is the count of recalled positive memories.
4. Discussion
PTSD symptoms have empirically-established associations with positive memory characteristics (e.g., Bernsten & Rubin, 2007; Gray & Lombardo, 2001; McKinnon et al., 2017; Megías et al., 2007; Niziurski et al., 2018; Porter & Birt, 2001). Uniquely, the current study implemented a network methodology to explore the relations between PTSD symptom clusters and positive memory characteristics (including central nodes within this network) among trauma-exposed community individuals. Results primarily indicated the potential pivotal role of PTSD’s AAR and avoidance symptom clusters, coherence of the recalled positive memory, and vividness of the recalled positive memory in the PTSD-positive memory relationship.
Current study results indicated that PTSD’s AAR symptom cluster was relatively central in the overall estimated network, including in influencing/being influenced (in a negative or positive direction) by positive memory characteristics, with the highest node strength (significantly greater than PTSD’s avoidance, count of recalled positive memories, time perspective of the recalled positive memory, and valence of the recalled positive memory) and the highest bridge strength. Referencing intra-community connections, AAR’s relation with other PTSD symptom clusters such as NACM and intrusions is consistent with evidence indicating its pivotal role in influencing other PTSD symptom clusters (Marshall, Schell, Glynn, & Shetty, 2006; Schell, Marshall, & Jaycox, 2004). Referencing cross-community connections, AAR was negatively associated with several positive memory characteristics (count of recalled positive memories, valence of the recalled positive memory, coherence of the recalled positive memory, accessibility of the recalled positive memory).
A strong AAR-NACM relation (one of the stronger edges in the estimated network) may explain AAR’s negative relation with positive memory characteristics. Trauma-exposed individuals may expend cognitive/behavioral/emotional energy to manage arousal symptoms, thus reducing emotional resources and increasing NACM emotion dysregulation symptoms (Foa, Zinbarg, & Rothbaum, 1992; Litz, 1992; Tull & Roemer, 2003); alternatively, suppression of emotional expression (NACM symptoms) may lead to greater physiological arousal (Notarious & Levenson, 1979). Thus, AAR’s association with greater negative affect (PTSD’s NACM symptoms) may activate more negative vs. positive memories (Bower’s associative network theory; Bower, 1981), and AAR’s association with reduced positive affect (PTSD’s NACM symptoms) may trigger reduced count and phenomenological qualities of positive memories (affect intensity theory; Larsen & Diener, 1987; Werner-Seidler & Moulds, 2011). Additionally, a strong AAR-intrusions relation (another relatively stronger edge in the estimated network) may also explain AAR’s negative relation with positive memory characteristics. According to trauma theorists (Chemtob, Roitblat, Hamada, Carlson, & Twentyman, 1988; Foa & Kozak, 1986; Foa, Steketee, & Rothbaum, 1989; Foa et al., 1992), trauma-exposed individuals form new associations between previously unrelated factors, which they perceive as dangerous, and experience distressing intrusion and arousal symptoms on activation of the fear network by trauma reminders. Consequently, they attempt to block out activated and intrusive traumatic memories to avoid consequent negative emotions, thoughts, and physiological symptoms (Dalgleish, Rolfe, Golden, Dunn, & Barnard, 2008; Hermans, Defranc, Raes, Williams, & Eelen, 2005; Moradi et al., 2008). Simultaneously, they may also block out positively-valenced memories because they are unable to effectively regulate triggered positive emotions (Weiss et al., 2018).
Notably, PTSD’s avoidance had the highest bridge expected influence, implying that it may play a critical role in positively influencing/being influenced by positive memory characteristics. In other words, activation of PTSD’s avoidance symptom cluster may relate to activation of positive memory characteristics. Referencing more specific associations, while avoidance was negatively correlated with count of recalled positive memories as expected, it was positively associated with vividness of the recalled positive memory. Drawing from an executive control viewpoint (Dalgleish et al., 2007), trauma-exposed individuals who exercise cognitive control as evidenced by PTSD’s avoidance symptoms to deal with distressing trauma-related information may perform well on the memory tasks eliciting (details of) positive memories (requires high amount of cognitive control; Moradi et al., 2008). Future research can investigate the moderating effect of cognitive control on PTSD’s relation with positive memories.
Among positive memory characteristics, coherence and vividness were relatively central in the overall estimated network with high node strength (both significantly greater than time perspective). Referencing intra-community connections, the relation between vividness and sensory details was relatively stronger than several other relations, probably attributed to the fact that both of these phenomenological qualities reference sensory details of the recalled positive memory. Referencing cross-community connections, results indicated that positive memory characteristics were primarily related to PTSD symptom clusters via the effects of coherence (highest bridge strength) and vividness (highest bridge expected influence) of the recalled positive memory. More specifically, perhaps, the current AMT and MEQ-SF tasks may have elicited/amplified a discrepancy between currently experienced negative belief/affect and positive beliefs/affect experienced during the positive memory event; this discrepancy, negative beliefs associated with PTSD symptoms (Agar, Kennedy, & King, 2006; O’Donnell, Elliott, Wolfgang, & Creamer, 2007), and negative affect associated with PTSD symptoms (Bradley et al., 2011) may relate to reduced coherence of the recalled positive memory. Indeed, research has indicated that emotional state at retrieval impacts details of retrieved memories (Schaefer & Philippot, 2005); a sad mood state was related to reduced coherence of positive memories among trauma-exposed individuals with PTSD (Rubin, 2011). This reduced coherence of positive memories may contribute to a decrease in psychological well-being (Waters & Fivush, 2015) and greater psychiatric problems (Adler, Chin, Kolisetty, & Oltmanns, 2012), including an increase in PTSD severity. Further, activation of vividness may be positively related to activation of PTSD symptom clusters, possibly due to the cognitive control explanation as already elaborated.
Implications
Study results have important theoretical and clinical implications pending further empirical investigations and replications. First, although not directly examined, our results suggest that certain positive memory characteristics may be impaired in relation to AAR and avoidance severity. Thus, traumatic and non-traumatic memories both may be impaired among trauma-exposed individuals, consistent with the trauma equivalency theory of memory (Brewin & Holmes, 2003; Porter & Birt, 2001; Waters et al., 2013). Second, PTSD may be primarily related to and co-occur with positive memory characteristics via PTSD’s AAR and avoidance symptoms and positive memory phenomenological qualities of vividness and coherence. Following from this, positive memory interventions (Arditte Hall, De Raedt, Timpano, & Joormann, 2018; Moradi et al., 2014; Raes et al., 2009; Steel et al., 2015) may benefit from addressing AAR and avoidance symptoms, in particular, to influence affect, cognitions, and post-trauma outcomes. Further, with evidence indicating that phenomenological qualities of memories are related to well-being/treatment indicators (Alvarez-Conrad, Zoellner, & Foa, 2001; Pennebaker, 1997; Pennebaker & Francis, 1996), a special assessment and treatment focus may be needed on positive memory characteristics of coherence and vividness to influence PTSD symptom severity. Indeed, trauma treatments work on increasing visual details (Tuerk et al., 2011) as well as coherence of the trauma narrative(s) (Robjant & Fazel, 2010) to effectively impact outcomes.
When considering the aforementioned implications, it must be noted that the cross-sectional nature of the current study implies (vs. does not examine) a dynamic nature of network symptoms and provides indications of the most central symptoms (e.g., PTSD’s AAR and avoidance symptoms) contributing to onset/maintenance of co-occurring conditions and representing therapeutic targets (Borsboom & Cramer, 2013; McNally et al., 2015; Rhemtulla et al., 2016). Such potential central symptoms need to be explored within temporal models (Bringmann & Eronen, 2018) considering that central symptoms across PTSD network studies are not consistent (Contreras, Nieto, Valiente, Espinosa, & Vazquez, 2019) and central symptoms for an aggregated network may not apply to individuals (Fisher, Reeves, Lawyer, Medaglia, & Rubel, 2017). If PTSD’s AAR and avoidance symptoms, and positive memory qualities of coherence and vividness could be confirmed as central (bridge) nodes using time-series data and person-centered approaches (Fisher et al., 2017; Ross et al., 2018), they may be investigated as targets for trauma interventions (McNally et al., 2015), wherein a change in their severity may in turn alter the severity of other related symptoms, thus initiating/enhancing therapeutic benefits spreading to the entire network (McNally et al., 2015). Notably, such therapeutic propagating effects have not yet been shown in research (Rodebaugh et al., 2018), central symptoms may not be ideal intervention targets because feedback loops may re-activate central symptoms after they have been targeted successfully in treatment (Fried et al., 2018), and there is debate on whether the nature of central nodes as well as their rank-order is replicable/stable across studies (Forbes, Wright, Markon, & Krueger, 2017). Nevertheless, our results provide some direction for future longitudinal empirical examination.
Limitations and Future Research
Our study results need to be considered in light of limitations/concerns specific to a network perspective to disorders. First, there is an on-going debate on the theoretical foundations of network models. A network perspective has been contrasted with a latent variable approach to disorders in terms of their underlying premise of whether co-occurring symptoms interact dynamically to reflect a disorder vs. sharing a common underlying/latent cause (the disorder itself; Borsboom & Cramer, 2013). Recently, investigators are debating whether these differences are better represented (1) as being symptom-oriented vs. syndrome-oriented, and (2) as a dynamic vs. a static perspective to disorders (Bringmann & Eronen, 2018). Our study is not confined to any of these perspectives; rather our results can set the groundwork to explore the PTSD-positive memory relationship combining the network and latent variable perspectives within a temporal framework (Bringmann & Eronen, 2018; Forbes et al., 2017). Second, evidence indicates concerns about replicability of network models, primarily regarding estimates of edges, most central nodes, and rank-order of node centrality attributed to measurement error of nodes (Forbes et al., 2017). Relatedly, given that a network methodology is data-driven, and hence specific to the characteristics of this sample (Epskamp et al., 2018), replication in more demographically and clinically diverse samples is needed to ascertain generalizability of the current study findings.
Third, such cross-sectional network models are exploratory and generate hypothetical structures with potential causal effects to be explored in longitudinal/experimental studies (Epskamp & Fried, 2018); any non-zero relation between two variables can indicate a direct causal relation between them, a reciprocal causal relation between them, or the causal influence of both variables on a third variable (Pearl, 2000). Fourth, the current study did not investigate the 20 PTSD symptoms separately (vs. PTSD symptom clusters) which would have allowed us to explore more nuanced associations. To use the 20 PTSD symptoms, we would need a minimum sample size of 351 individuals (27 nodes). Given that a small and inadequate sample size has been shown to influence unstable networks and reduce reliability of results (Epskamp et al., 2018), we decided to use the four PTSD symptom clusters vs. the 20 PTSD symptoms for the current study. Relatedly, if using individual PTSD items, it would be important to consider the reliability of these single-item estimates because of measurement error (Fried & Cramer, 2017). In essence, longitudinal studies with larger sample sizes are needed to examine causal inferences between these variables (Epskamp et al., 2018; Fried & Cramer, 2017).
Beyond limitations related to network models, it should be noted that poor/questionable internal consistencies of certain memory phenomenological qualities such as vividness, time perspective, sensory details, and coherence suggests that the combination of items in these domains may not accurately reflect these memory constructs; this may have negatively impacted the current study’s statistical power to detect significant findings (Henson, 2001). Further, although excluding individuals making multiple attempts to complete the survey improves data quality, the rate of duplicate responses in the current study was higher compared to other MTurk studies (e.g., Martin, Reimann, & Norton, 2016; Wessling, Huber, & Netzer, 2017), which could have influenced the pattern of findings. Lastly, the moderating influences of factors such as cognitive skills (Gray & Lombardo, 2001), gender (Porter & Birt, 2001), retention interval (Waters et al., 2013), and trauma types (Contractor, Caldas, Fletcher, Shea, & Armour, 2018) could be examined in future research. Relatedly, it is important to consider that the valence of a memory may not be the only factor influencing all phenomenological qualities (Kensinger & Schacter, 2006; Porter & Birt, 2001); other memory-related characteristics such as physiological arousal associated with recall may be important to investigate in future research.
In conclusion, by focally highlighting the role of PTSD’s AAR and avoidance symptoms, and positive memory characteristics of coherence and vividness, current study results extend research supporting a link between increasing PTSD severity and difficulties recalling specific positive memories (Contractor et al., in press; de Decker, Hermans, Raes, & Eelen, 2003; Hayes, VanElzakker, & Shin, 2012). This exploratory study indicated weak yet important trends worthy of further longitudinal investigation. Results inform trauma treatments that may capitalize on positive memories to improve treatment outcomes and retention (Contractor, Brown, et al., 2018), provide support to investigate sensation-focused (especially related to visual details) treatments for PTSD (Hinton et al., 2005), and contribute to the onset and maintenance hybrid models of PTSD (Fried & Cramer, 2017).
Supplementary Material
Figure 2.
Strength centrality
Note. AAR is PTSD’s anxious alterations in arousal and reactivity cluster; NACM is PTSD’s negative alterations in cognitions and mood cluster; Int is PTSD’s intrusions cluster; Avoid is PTSD’s avoidance cluster; coherence is the coherence phenomenological quality of positive memories; vivid is the vividness phenomenological quality of positive memories; access is the accessibility phenomenological quality of positive memories; sensory is the sensory details phenomenological quality of positive memories; valence is the valence phenomenological quality of positive memories; time persp is the time perspective phenomenological quality of positive memories; count is the count of recalled positive memories.
Highlights.
We conducted a PTSD-positive memory network analysis with 206 traumatized individuals.
High bridge centrality PTSD nodes were arousal (strength) and avoidance (expected influence).
High bridge centrality positive memory nodes were coherence (strength) and vividness (expected influence).
Arousal was negatively associated with memory count, valence, coherence, and access.
Avoidance was positively and negatively associated with memory vividness and count respectively.
Funding:
The research described here was supported, in part, by a grant from the National Institute on Drug Abuse (K23DA039327) awarded to the fourth co-author. NIDA had no role in the study design, collection, analysis or interpretation of the data, writing the manuscript, or the decision to submit the paper for publication.
Footnotes
Conflict of Interest: All authors declare that they have no conflict of interest.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Contributor Information
Ateka A. Contractor, Department of Psychology, University of North Texas, Denton, TX, USA
Talya Greene, Department of Community Mental Health, University of Haifa, Israel.
Megan Dolan, Department of Psychology, University of North Texas, Denton, TX, USA.
Nicole H. Weiss, Department of Psychology, University of Rhode Island, RI, TX, USA
Cherie Armour, School of Psychology, Queens University Belfast, Northern Ireland, UK..
References
- Adler JM, Chin ED, Kolisetty AP, & Oltmanns TF (2012). The distinguishing characteristics of narrative identity in adults with features of borderline personality disorder: an empirical investigation. Journal of Personality Disorders, 26, 498–512. doi: 10.1521/pedi.2012.26.4.498 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Afzali MH, Sunderland M, Batterham PJ, Carragher N, Calear A, & Slade T (2017). Network approach to the symptom-level association between alcohol use disorder and posttraumatic stress disorder. Social Psychiatry and Psychiatric Epidemiology, 52, 329–339. doi: 10.1007/s00127-016-1331-3 [DOI] [PubMed] [Google Scholar]
- Agar E, Kennedy P, & King NS (2006). The role of negative cognitive appraisals in PTSD symptoms following spinal cord injuries. Behavioural and Cognitive Psychotherapy, 34, 437–452. doi: 10.1017/S1352465806002943 [DOI] [Google Scholar]
- Alvarez-Conrad J, Zoellner L, & Foa E (2001). Linguistic predictors of trauma pathology and physical health. Applied Cognitive Psychology, 15, 159–170. doi: 10.1002/acp.839 [DOI] [Google Scholar]
- American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders (5th ed.). Washington, DC: American Psychiatric Association. [Google Scholar]
- Arditte Hall KA, De Raedt R, Timpano KR, & Joormann J (2018). Positive memory enhancement training for individuals with major depressive disorder. Cognitive Behaviour Therapy, 47, 155–168. doi: 10.1080/16506073.2017.136429 [DOI] [PubMed] [Google Scholar]
- Armour C, Fried EI, Deserno MK, Tsai J, & Pietrzak RH (2017). A network analysis of DSM-5 posttraumatic stress disorder symptoms and correlates in US military veterans. Journal of Anxiety Disorders, 45, 49–59. doi: 10.1016/j.janxdis.2016.11.008 [DOI] [PubMed] [Google Scholar]
- Aupperle RL, Melrose AJ, Stein MB, & Paulus MP (2012). Executive function and PTSD: Disengaging from trauma. Neuropharmacology, 62, 686–694. doi: 10.1016/j.neuropharm.2011.02.008 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berliner L, Hyman I, Thomas A, & Fitzgerald M (2003). Children’s memory for trauma and positive experiences. Journal of Traumatic Stress, 16, 229–236. doi: 10.1023/A:1023787805970 [DOI] [PubMed] [Google Scholar]
- Bernsten D, & Rubin DC (2007). When a trauma becomes a key to identity: Enhanced integration of trauma memories predicts posttraumatic stress disorder symptoms. Applied Cognitive Psychology, 21, 417–431. doi: 10.1002/acp.1290 [DOI] [Google Scholar]
- Berntsen D, & Rubin DC (2006). The Centrality of Event Scale: A measure of integrating a trauma into one’s identity and its relation to post-traumatic stress disorder symptoms. Behavior Research and Therapy, 44, 219–231. doi: 10.1016/j.brat.2005.01.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bohanek JG, Fivush R, & Walker E (2005). Memories of positive and negative emotional events. Applied Cognitive Psychology, 19, 51–66. doi: 10.1002/acp.1064 [DOI] [Google Scholar]
- Borsboom D, & Cramer AO (2013). Network analysis: An integrative approach to the structure of psychopathology. Annual Review of Clinical Psychology, 9, 91–121. doi: 10.1146/annurev-clinpsy-050212-185608 [DOI] [PubMed] [Google Scholar]
- Bovin MJ, Marx BP, Weathers FW, Gallagher MW, Rodriguez P, Schnurr PP, et al. (2016). Psychometric properties of the PTSD Checklist for Diagnostic and Statistical Manual of Mental Disorders–Fifth Edition (PCL-5) in veterans. Psychological Assessment, 28, 1379–1391. doi: 10.1037/pas0000254 [DOI] [PubMed] [Google Scholar]
- Bower GH (1981). Mood and memory. American Psychologist, 36, 129–148. [DOI] [PubMed] [Google Scholar]
- Boyacioglu I, & Akfirat S (2015). Development and psychometric properties of a new measure for memory phenomenology: The Autobiographical Memory Characteristics Questionnaire. Memory, 23, 1070–1092. doi: 10.1080/09658211.2014.953960 [DOI] [PubMed] [Google Scholar]
- Bradley B, DeFife JA, Guarnaccia C, Phifer MJ, Fani MN, Ressler KJ, et al. (2011). Emotion dysregulation and negative affect: association with psychiatric symptoms. The Journal of Clinical Psychiatry, 72, 685–691. doi: 10.4088/JCP.10m06409blu [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bray J, Brewer N, Cameron K, & Nixon RD (2018). Comparing children’s memories for negative versus positive events in the context of posttraumatic stress symptoms. Behavior Therapy, 49, 32–45. doi: 10.1016/j.beth.2017.03.006 [DOI] [PubMed] [Google Scholar]
- Brewin CR, & Holmes EA (2003). Psychological theories of posttraumatic stress disorder. Clinical Psychology Review, 23, 339–376. doi: 10.1016/S0272-7358(03)00033-3 [DOI] [PubMed] [Google Scholar]
- Bringmann LF, & Eronen MI (2018). Don’t blame the model: Reconsidering the network approach to psychopathology. Psychological Review, 125, 606–615. doi: 10.1037/rev0000108 [DOI] [PubMed] [Google Scholar]
- Byrne CA, Hyman IE, & Scott KL (2001). Comparisons of memories for traumatic events and other experiences. Applied Cognitive Psychology, 15, S119–S133. doi: 10.1002/ACP.837 [DOI] [Google Scholar]
- Chemtob C, Roitblat HL, Hamada RS, Carlson JG, & Twentyman CT (1988). A cognitive-action theory of post-traumatic stress disorder. Journal of Anxiety Disorders, 2, 253–275. doi: 10.1016/0887-6185(88)90006-0 [DOI] [Google Scholar]
- Chen J, & Chen Z (2008). Extended Bayesian information criteria for model selection with large model spaces. Biometrika, 95, 759–771. doi: 10.1093/biomet/asn034 [DOI] [Google Scholar]
- Contractor AA, Armour C, Forbes D, & Elhai JD (2016). PTSD’s underlying dimensions and their relation with impulsivity facets. The Journal of Nervous & Mental Disease, 204, 20–25. doi: 10.1097/NMD.0000000000000417 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Banducci AN, Dolan M, Keegan F, & Weiss NH (in press). Relation of positive memory recall count and accessibility with posttrauma mental health. Memory. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Brown LA, Caldas S, Banducci AN, Taylor DJ, Armour C, et al. (2018). Posttraumatic stress disorder and positive memories: Clinical considerations. Journal of Anxiety Disorders, 58, 22–32. doi: 10.1016/j.janxdis.2018.06.007 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Caldas S, Fletcher S, Shea MT, & Armour C (2018). Empirically-derived lifespan polytraumatization typologies: A systematic review. Journal of Clinical Psychology, 74, 1137–1159. doi: 10.1002/jclp.22586 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Caldas SV, Dolan M, Lagdon S, & Armour C (2018). PTSD’s factor structure and measurement invariance across subgroups with differing count of trauma types. Psychiatry Research, 264, 76–84. doi: 10.1016/j.psychres.2018.03.065 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Caldas SV, Dolan M, Natesan P, & Weiss NH (2019). Invariance of the construct of Posttraumatic stress disorder: A systematic review. Journal of Traumatic Stress doi: 10.1002/jts.22389 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Durham TA, Brennan JA, Armour C, Wutrick HR, Frueh CB, et al. (2014). DSM-5 PTSD’s symptom dimensions and relations with major depression’s symptom dimensions in a primary care sample. Psychiatry Research, 215, 146–153. doi: 10.1016/j.psychres.2013.10.015 [DOI] [PubMed] [Google Scholar]
- Contractor AA, Frankfurt S, Weiss NH, & Elhai JD (2017). Latent-level relations between DSM-5 PTSD symptom clusters and problematic smartphone use. Computers in Human Behavior, 72, 170–177. doi: 10.1016/j.chb.2017.02.051 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contractor AA, Greene T, Dolan M, & Elhai JD (2018). Relations between PTSD and depression symptom clusters in samples differentiated by PTSD diagnostic status. Journal of Anxiety Disorders, 59, 17–26. doi: 10.1016/j.janxdis.2018.08.004 [DOI] [PubMed] [Google Scholar]
- Contreras A, Nieto I, Valiente C, Espinosa R, & Vazquez C (2019). The study of psychopathology from the network analysis perspective: A systematic review. Psychotherapy and Psychosomatics, 88, 71–83. doi: 10.1159/000497425 [DOI] [PubMed] [Google Scholar]
- Costantini G, Epskamp S, Borsboom D, Perugini M, Mõttus R, Waldorp LJ, et al. (2015). State of the aRt personality research: A tutorial on network analysis of personality data in R. Journal of Research in Personality, 54, 13–29. doi: 10.1016/j.jrp.2014.07.003 [DOI] [Google Scholar]
- Costantini G, Richetin J, Preti E, Casini E, Epskamp S, & Perugini M (2019). Stability and variability of personality networks. A tutorial on recent developments in network psychometrics. Personality and Individual Differences, 136, 68–78. doi: 10.1016/j.paid.2017.06.011 [DOI] [Google Scholar]
- Cox DR, & Wermuth N (1994). A note on the quadratic exponential binary distribution. Biometrika, 81, 403–408. doi: 10.1093/biomet/81.2.403 [DOI] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, & Borsboom D (2010a). Comorbidity: A network perspective. The Behavioral and Brain Sciences, 33, 137–150. doi: 10.1017/S0140525X09991567 [DOI] [PubMed] [Google Scholar]
- Cramer AOJ, Waldorp LJ, van der Maas HLJ, & Borsboom D (2010b). Complex realities require complex theories: Refining and extending the network approach to mental disorders. Behavioral and Brain Sciences, 33, 178–193. doi: 10.1017/S0140525X10000920 [DOI] [Google Scholar]
- Curran PJ, West SG, & Finch JF (1996). The robustness of test statistics to nonnormality and specification error in confirmatory factor analysis. Psychological Methods, 1, 16–29. doi: 10.1037/1082-989X.1.1.16 [DOI] [Google Scholar]
- Dalgleish T, Rolfe J, Golden AM, Dunn BD, & Barnard PJ (2008). Reduced autobiographical memory specificity and posttraumatic stress: Exploring the contributions of impaired executive control and affect regulation. Journal of Abnormal Psychology, 117, 236–241. doi: 10.1037/0021-843X.117.1.236 [DOI] [PubMed] [Google Scholar]
- Dalgleish T, Williams JMG, Golden AMJ, Perkins N, Barrett LF, Barnard PJ, et al. (2007). Reduced specificity of autobiographical memory and depression: The role of executive processes. Journal of Experimental Psychology: General, 136, 23–42. doi: 10.1037/0096-3445.136.1.23 [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Decker A, Hermans D, Raes F, & Eelen P (2003). Autobiographical memory specificity and trauma in inpatient adolescents. Journal of Clinical Child and Adolescent Psychology, 32, 22–31. doi: 10.1207/15374420360533031 [DOI] [PubMed] [Google Scholar]
- Dominique JF, Kolassa IT, Ackermann S, Aerni A, Boesiger P, Demougin P, et al. (2012). PKCα is genetically linked to memory capacity in healthy subjects and to risk for posttraumatic stress disorder in genocide survivors. Proceedings of the National Academy of Sciences, 109, 8746–8751. doi: 10.1073/pnas.1200857109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ehlers A, & Clark DM (2000). A cognitive model of posttraumatic stress disorder. Behavior Research and Therapy, 38, 319–324. doi: 10.1016/S0005-7967(99)00123-0 [DOI] [PubMed] [Google Scholar]
- Engelhard IM, van den Hout MA, & McNally RJ (2008). Memory consistency for traumatic events in Dutch soldiers deployed to Iraq. Memory, 16, 3–9. Memory, 16, 3–9. doi: 10.1080/09658210701334022 [DOI] [PubMed] [Google Scholar]
- Epskamp S, Borsboom D, & Fried EI (2018). Estimating psychological networks and their accuracy: A tutorial paper. Behavior Research Methods, 50, 195–212. doi: 10.3758/s13428-017-0862-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Epskamp S, Cramer A, Waldorp L, Schmittmann VD, & Borsboom D (2012). qgraph: Network visualizations of relationships in psychometric data. Journal of Statistical Software, 48, 1–18. [Google Scholar]
- Epskamp S, & Fried EI (2018). A tutorial on regularized partial correlation networks. Psychological Methods, 23, 617–634. doi: 10.1037/met0000167 [DOI] [PubMed] [Google Scholar]
- Fani N, Tone EB, Phifer J, Norrholm SD, Bradley B, Ressler KJ, et al. (2012). Attention bias toward threat is associated with exaggerated fear expression and impaired extinction in PTSD. Psychological Medicine, 42, 533–543. doi: 10.1017/S0033291711001565 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fernández-Lansac V, & Crespo M (2017). Presentation of the Coding and Assessment System for Narratives of Trauma (CASNOT): Application in Spanish battered women and preliminary analyses. The Spanish Journal of Psychology, 20, 1–12. doi: 10.1017/sjp.2017.31 [DOI] [PubMed] [Google Scholar]
- Fisher AJ, Reeves JW, Lawyer G, Medaglia JD, & Rubel JA (2017). Exploring the idiographic dynamics of mood and anxiety via network analysis. Journal of Abnormal Psychology, 126, 1044–1056. doi: 10.1037/abn0000311 [DOI] [PubMed] [Google Scholar]
- Fivush R, Hazzard A, Sales JM, Sarfati D, & Brown T (2002). Creating coherence out of chaos? Children’s narratives of emotionally negative and positive events. Applied Cognitive Psychology, 16, 1–19. doi: 10.1080/15248372.2011.590787 [DOI] [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20–35. doi: 10.1037//0033-2909.99.1.20 [DOI] [PubMed] [Google Scholar]
- Foa EB, Steketee G, & Rothbaum BO (1989). Behavioral/cognitive conceptualizations of post-traumatic stress disorder. Behavior Therapy, 20, 155–176. doi: 10.1016/S0005-7894(89)80067-X [DOI] [Google Scholar]
- Foa EB, Zinbarg R, & Rothbaum BO (1992). Uncontrollability and unpredictability in post-traumatic stress disorder: An animal model. Psychological Bulletin, 112, 218–238. doi: 10.1037/0033-2909.112.2.218 [DOI] [PubMed] [Google Scholar]
- Forbes MK, Wright AG, Markon KE, & Krueger RF (2017). Evidence that psychopathology symptom networks have limited replicability. Journal of Abnormal Psychology, 126, 969–988. doi: 10.1037/abn0000276 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fried EI, & Cramer AO (2017). Moving forward: Challenges and directions for psychopathological network theory and methodology. Perspectives on Psychological Science, 12, 999–1020. doi: 10.1177/1745691617705892 [DOI] [PubMed] [Google Scholar]
- Fried EI, Eidhof MB, Palic S, Costantini G, Huisman-van Dijk HM, Bockting CLH, et al. (2018). Replicability and generalizability of posttraumatic stress disorder (PTSD) networks: A cross-cultural multisite study of PTSD symptoms in four trauma patient samples. Clinical Psychological Science, 6, 335–351. doi: 10.1177/2167702617745092 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Friedman JH, Hastie T, & Tibshirani R (2008). Sparse inverse covariance estimation with the graphical lasso. Biostatistics, 9, 432–441. doi: 10.1093/biostatistics/kxm045 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fruchterman TM, & Reingold EM (1991). Graph drawing by force- directed placement. Software: Practice and Experience, 21, 1129–1164. doi: 10.1002/spe.4380211102 [DOI] [Google Scholar]
- Gray MJ, & Lombardo TW (2001). Complexity of trauma narratives as an index of fragmented memory in PTSD: A critical analysis. Applied Cognitive Psychology, 15, 171–186. doi: 10.1002/acp.840 [DOI] [Google Scholar]
- Griffith JW, Sumner JA, Debeer E, Raes F, Hermans D, Mineka S, et al. (2009). An item response theory/confirmatory factor analysis of the Autobiographical Memory Test. Memory, 17, 609–623. doi: 10.1080/09658210902939348 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Harvey AG, Bryant RA, & Dang ST (1998). Autobiographical memory in acute stress disorder. Journal of Consulting and Clinical Psychology, 66, 500–506. doi: 10.1037/0022-006X.66.3.500 [DOI] [PubMed] [Google Scholar]
- Hauer BJ, Wessel I, Engelhard IM, Peeters LL, & Dalgleish T (2009). Prepartum autobiographical memory specificity predicts post-traumatic stress symptoms following complicated pregnancy. Memory, 17, 544–556. doi: 10.1080/09658210902953836 [DOI] [PubMed] [Google Scholar]
- Hauser DJ, & Schwarz N (2016). Attentive Turkers: MTurk participants perform better on online attention checks than do subject pool participants. Behavior Research Methods, 48, 400–407. doi: 10.3758/s13428-015-0578-z [DOI] [PubMed] [Google Scholar]
- Hayes JP, VanElzakker MB, & Shin LM (2012). Emotion and cognition interactions in PTSD: A review of neurocognitive and neuroimaging studies. Frontiers in Integrative Neuroscience, 6(89). doi: 10.3389/fnint.2012.00089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henderson D, Hargreaves I, Gregory S, & Williams JMG (2002). Autobiographical memory and emotion in a non- clinical sample of women with and without a reported history of childhood sexual abuse. British Journal of Clinical Psychology, 41, 129–141. doi: 10.1348/014466502163921 [DOI] [PubMed] [Google Scholar]
- Henson RK (2001). Understanding internal consistency reliability estimates: A conceptual primer on coefficient alpha (Methods, plainly speaking). Measurement and Evaluation in Counseling and Development, 34, 177–190. [Google Scholar]
- Hermans D, Defranc A, Raes F, Williams JMG, & Eelen P (2005). Reduced autobiographical memory specificity as an avoidant coping style. British Journal of Clinical Psychology, 44, 583–589. doi: 10.1348/014466505X53461 [DOI] [PubMed] [Google Scholar]
- Hinton DE, Chhean D, Pich V, Safren SA, Hofmann SG, & Pollack MH (2005). A randomized controlled trial of cognitive- behavior therapy for Cambodian refugees with treatment- resistant PTSD and panic attacks: A cross- over design. Journal of Traumatic Stress, 18, 617–629. doi: 10.1002/jts.20070 [DOI] [PubMed] [Google Scholar]
- Janoff-Bulman R (1992). Shattered assumptions: Toward a new psychology of trauma. New York, NY: Free Press. [Google Scholar]
- Janssen SM, Hearne TL, & Takarangi MK (2015). The relation between self-reported PTSD and depression symptoms and the psychological distance of positive and negative events. Journal of behavior therapy and experimental psychiatry, 48, 177–184. doi: 10.1016/j.jbtep.2015.04.002 [DOI] [PubMed] [Google Scholar]
- Jones P (2018). Networktools: tools for identifying important nodes in networks R package version 1.1.1., from https://CRAN.R-project.org/package=networktools
- Jones PJ, Ma R, & McNally RJ (2019, April 25). Bridge centrality. A network approach to understanding comorbidity. [DOI] [PubMed] [Google Scholar]
- Kensinger EA, & Schacter DL (2006). When the Red Sox shocked the Yankees: Comparing negative and positive memories. Psychonomic Bulletin & Review, 13, 757–763. doi: 10.3758/BF03193993 [DOI] [PubMed] [Google Scholar]
- Kleim B, & Ehlers A (2008). Reduced autobiographical memory specificity predicts depression and posttraumatic stress disorder after recent trauma. Journal of Consulting and Clinical Psychology, 76, 231–242. doi: 10.1037/0022-006X.76.2.231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larsen RJ, & Diener E (1987). Affect intensity as an individual difference characteristic: A review. Journal of Research in Personality, 21, 1–39. doi: 10.1016/0092-6566(87)90023-7 [DOI] [Google Scholar]
- Litz BT (1992). Emotional numbing in combat-related post-traumatic stress disorder: A critical review and reformulation. Clinical Psychology Review, 12, 417–432. doi: 10.1016/0272-7358(92)90125-R [DOI] [Google Scholar]
- Litz BT, Orsillo SM, Kaloupek D, & Weathers F (2000). Emotional processing in posttraumatic stress disorder. Journal of Abnormal Psychology, 109, 26–39. doi: 10.1037/0021-843X.109.1.26 [DOI] [PubMed] [Google Scholar]
- Luchetti M, & Sutin AR (2016). Measuring the phenomenology of autobiographical memory: A short form of the Memory Experiences Questionnaire. Memory, 24, 592–602. doi: 10.1080/09658211.2015.1031679 [DOI] [PubMed] [Google Scholar]
- Marshall GN, Schell TL, Glynn SM, & Shetty V (2006). The role of hyperarousal in the manifestation of posttraumatic psychological distress following injury. Journal of Abnormal Psychology, 115, 624–628. doi: 10.1037/0021-843X.115.3.624 [DOI] [PubMed] [Google Scholar]
- Martin JM, Reimann M, & Norton MI (2016). Experience theory, or how desserts are like losses. Journal of Experimental Psychology: General, 145, 1460–1472. doi: 10.1037/xge0000215 [DOI] [PubMed] [Google Scholar]
- McKinnon A, Brewer N, Meiser-Stedman R, & Nixon R (2017). Trauma memory characteristics and the development of acute stress disorder and post-traumatic stress disorder in youth. Journal of Behavior Therapy and Experimental Psychiatry, 54, 112–119. doi: 10.1016/j.jbtep.2016.07.009 [DOI] [PubMed] [Google Scholar]
- McNally RJ (2003). Remembering Trauma Cambridge, MA.: The Belknap Press of Harvard University Press. [Google Scholar]
- McNally RJ, Lasko NB, Macklin ML, & Pitman RK (1995). Autobiographical memory disturbance in combat-related posttraumatic stress disorder. Behavior Research and Therapy, 33, 619–630. doi: 10.1016/0005-7967(95)00007-K [DOI] [PubMed] [Google Scholar]
- McNally RJ, Robinaugh DJ, Wu GW, Wang L, Deserno MK, & Borsboom D (2015). Mental disorders as causal systems: A network approach to posttraumatic stress disorder. Clinical Psychological Science, 836–849. doi: 10.1177/2167702614553230 [DOI] [Google Scholar]
- Meade AW, & Craig SB (2012). Identifying careless responses in survey data. Psychological Methods, 17, 437–455. doi: 10.1037/a0028085 [DOI] [PubMed] [Google Scholar]
- Megías JL, Ryan E, Vaquero JM, & Frese B (2007). Comparisons of traumatic and positive memories in people with and without PTSD profile. Applied Cognitive Psychology, 21, 117–130. doi: 10.1002/acp.1282 [DOI] [Google Scholar]
- Moradi AR, Herlihy J, Yasseri G, Shahraray M, Turner S, & Dalgleish T (2008). Specificity of episodic and semantic aspects of autobiographical memory in relation to symptoms of posttraumatic stress disorder (PTSD). Acta Psychologica, 127, 645–653. doi: 10.1016/j.actpsy.2007.11.001 [DOI] [PubMed] [Google Scholar]
- Moradi AR, Moshirpanahi S, Parhon H, Mirzaei J, Dalgleish T, & Jobson L (2014). A pilot randomized controlled trial investigating the efficacy of MEmory Specificity Training in improving symptoms of posttraumatic stress disorder. Behavior Research and Therapy, 56, 68–74. doi: 10.1016/j.brat.2014.03.002 [DOI] [PubMed] [Google Scholar]
- Niziurski JA, Johannessen KB, & Berntsen D (2018). Emotional distress and positive and negative memories from military deployment: The influence of PTSD symptoms and time. Memory, 26, 1093–1104. doi: 10.1080/09658211.2017.1418380 [DOI] [PubMed] [Google Scholar]
- Notarious CI, & Levenson RJ (1979). Expressive tendencies and physiological response to stress. Journal of Personality and Social Psychology, 37, 1204–1210. doi: 10.1037/0022-3514.37.7.1204 [DOI] [PubMed] [Google Scholar]
- O’Donnell ML, Elliott P, Wolfgang BJ, & Creamer M (2007). Posttraumatic appraisals in the development and persistence of posttraumatic stress symptoms. Journal of Traumatic Stress, 20, 173–182. doi: 10.1002/jts.20198 [DOI] [PubMed] [Google Scholar]
- Oppenheimer DM, Meyvis T, & Davidenko N (2009). Instructional manipulation checks: Detecting satisficing to increase statistical power. Journal of Experimental Social Psychology, 45, 867–872. doi: 10.1016/j.jesp.2009.03.009 [DOI] [Google Scholar]
- Peace KA, & Porter S (2004). A longitudinal investigation of the reliability of memories for trauma and other emotional experiences. Applied Cognitive Psychology, 18, 1143–1159. doi: 10.1002/acp.1046 [DOI] [Google Scholar]
- Peace KA, Porter S, & Brinke LT (2008). Are memories for sexually traumatic events “special”? A within-subjects investigation of trauma and memory in a clinical sample. Memory, 16, 10–21. doi: 10.1080/09658210701363583 [DOI] [PubMed] [Google Scholar]
- Pearl J (2000). Causality: Models, reasoning, and inference Cambridge, UK: Cambridge University Press. [Google Scholar]
- Pennebaker JW (1997). Writing about emotional experiences as a therapeutic process. Psychological Science, 8, 162–166. doi: 10.1111/j.1467-9280.1997.tb00403.x [DOI] [Google Scholar]
- Pennebaker JW, & Francis ME (1996). Cognitive, emotional, and language processes in disclosure. Cognition and Emotion, 10, 601–626. doi: 10.1080/026999396380079 [DOI] [Google Scholar]
- Porter S, & Birt AR (2001). Is traumatic memory special? A comparison of traumatic memory characteristics with memory for other emotional life experiences. Applied Cognitive Psychology, 15, 101–117. doi: 10.1002/acp.766 [DOI] [Google Scholar]
- Porter S, & Peace KA (2007). The scars of memory: A prospective, longitudinal investigation of the consistency of traumatic and positive emotional memories in adulthood. Psychological Science, 18, 435–441. doi: 10.1111/j.1467-9280.2007.01918.x [DOI] [PubMed] [Google Scholar]
- Raes F, Williams JMG, & Hermans D (2009). Reducing cognitive vulnerability to depression: A preliminary investigation of MEmory Specificity Training (MEST) in inpatients with depressive symptomatology. Journal of Behavior Therapy and Experimental Psychiatry, 40, 24–38. doi: 10.1016/j.jbtep.2008.03.001 [DOI] [PubMed] [Google Scholar]
- Rhemtulla M, Fried EI, Aggen SH, Tuerlinckx F, Kendler KS, & Borsboom D (2016). Network analysis of substance abuse and dependence symptoms. Drug and Alcohol Dependence, 161, 230–237. doi: 10.1016/j.drugalcdep.2016.02.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robjant K, & Fazel M (2010). The emerging evidence for narrative exposure therapy: A review. Clinical Psychology review, 30, 1030–1039. doi: 10.1016/j.cpr.2010.07.004 [DOI] [PubMed] [Google Scholar]
- Rodebaugh TL, Tonge NA, Piccirillo ML, Fried E, Horenstein A, Morrison AS, et al. (2018). Does centrality in a cross-sectional network suggest intervention targets for social anxiety disorder? Journal of Consulting and Clinical Psychology, 86, 831–844. doi: 10.1037/ccp0000336 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ross J, Murphy D, & Armour C (2018). A network analysis of DSM-5 posttraumatic stress disorder and functional impairment in UK treatment-seeking veterans. Journal of Anxiety Disorders, 57, 7–15. doi: 10.1016/j.janxdis.2018.05.007 [DOI] [PubMed] [Google Scholar]
- Rubin DC (2011). The coherence of memories for trauma: Evidence from posttraumatic stress disorder. Consciousness and Cognition, 20, 857–865. doi: 10.1016/j.concog.2010.03.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rubin DC, Boals A, & Berntsen D (2008). Memory in posttraumatic stress disorder: Properties of voluntary and involuntary, traumatic and nontraumatic autobiographical memories in people with and without posttraumatic stress disorder symptoms. Journal of Experimental Psychology: General, 137, 591–614. doi: 10.1037/a0013165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schaefer A, & Philippot P (2005). Selective effects of emotion on the phenomenal characteristics of autobiographical memories. Memory, 13, 148–160. doi: 10.1080/09658210344000648 [DOI] [PubMed] [Google Scholar]
- Schell TL, Marshall GN, & Jaycox LH (2004). All symptoms are not created equal: The prominent role of hyperarousal in the natural course of posttraumatic psychological distress. Journal of Abnormal Psychology, 113, 189–197. doi: 10.1037/0021-843X.113.2.189 [DOI] [PubMed] [Google Scholar]
- Schnurr PP (2017). Focusing on trauma-focused psychotherapy for posttraumatic stress disorder. Current Opinion in Psychology, 14, 56–60. doi: 10.1016/j.copsyc.2016.11.005 [DOI] [PubMed] [Google Scholar]
- Shapiro DN, Chandler J, & Mueller PA (2013). Using Mechanical Turk to study clinical populations. Clinical Psychological Science, 1, 213–220. doi: 10.1177/2167702612469015 [DOI] [Google Scholar]
- Sotgiu I, & Mormont C (2008). Similarities and differences between traumatic and emotional memories: Review and directions for future research. The Journal of Psychology, 142, 449–470. doi: 10.3200/JRLP.142.5.449-470 [DOI] [PubMed] [Google Scholar]
- Steel C, van der Gaag M, Korrelboom K, Simon J, Phiri P, Baksh MF, et al. (2015). A randomised controlled trial of positive memory training for the treatment of depression within schizophrenia. BMC Psychiatry, 15, 85–90. doi: 10.1186/s12888-015-0453-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sutherland K, & Bryant RA (2005). Self- defining memories in post- traumatic stress disorder. British Journal of Clinical Psychology, 44, 591–598. doi: 10.1348/014466505X64081 [DOI] [PubMed] [Google Scholar]
- Sutherland K, & Bryant RA (2008). Social problem solving and autobiographical memory in posttraumatic stress disorder. Behavior Research and Therapy, 46, 154–161. doi: 10.1016/j.brat.2007.10.005 [DOI] [PubMed] [Google Scholar]
- Sutin AR, & Robins RW (2007). Phenomenology of autobiographical memories: The Memory Experiences Questionnaire. Memory, 15, 390–314. doi: 10.1080/09658210701256654 [DOI] [PubMed] [Google Scholar]
- Tuerk PW, Yoder M, Grubaugh A, Myrick H, Hamner M, & Acierno R (2011). Prolonged exposure therapy for combat-related posttraumatic stress disorder: An examination of treatment effectiveness for veterans of the wars in Afghanistan and Iraq. Journal of Anxiety Disorders, 25, 397–403. doi: 10.1016/j.janxdis.2010.11.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tull MT, Jakupcak M, McFadden ME, & Roemer L (2007). The role of negative affect intensity and the fear of emotions in posttraumatic stress symptom severity among victims of childhood interpersonal violence. The Journal of Nervous and Mental Disease, 195, 580–587. doi: 10.1097/NMD.0b013e318093ed5f [DOI] [PubMed] [Google Scholar]
- Tull MT, & Roemer L (2003). Alternative explanations of emotional numbing of posttraumatic stress disorder: An examination of hyperarousal and experiential avoidance. Journal of Psychopathology and Behavioral Assessment, 25, 147–154. doi: 10.1023/A:1023568822462 [DOI] [Google Scholar]
- Waters TEA, Bohanek JG, Marin K, & Fivush R (2013). Null’s the word: A comparison of memory quality for intensely negative and positive events. Memory, 21, 633–645. doi: 10.1080/09658211.2012.745877 [DOI] [PubMed] [Google Scholar]
- Waters TEA, & Fivush R (2015). Relations between narrative coherence, identity, and psychological well-being in emerging adulthood. Journal of Personality, 83, 441–451. doi: 10.1111/jopy.12120 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weathers FW, Blake DD, Schnurr PP, Kaloupek DG, Marx BP, & Keane TM (2013). The Life Events Checklist for DSM-5 (LEC-5). Instrument available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Weathers FW, Litz BT, Keane TM, Palmieri PA, Marx BP, & Schnurr PP (2013). The PTSD Checklist for DSM-5 (PCL-5). Scale available from the National Center for PTSD at www.ptsd.va.gov. [Google Scholar]
- Weiss NH, Dixon-Gordon KL, Peasant C, & Sullivan TP (2018). An examination of the role of difficulties regulating positive emotions in posttraumatic stress disorder. Journal of Traumatic Stress, 31, 775–780. doi: 10.1002/jts.22330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Werner-Seidler A, & Moulds ML (2011). Autobiographical memory characteristics in depression vulnerability: Formerly depressed individuals recall less vivid positive memories. Cognition and Emotion, 25, 1087–1103. doi: 10.1080/02699931.2010.531007 [DOI] [PubMed] [Google Scholar]
- Wessling KS, Huber J, & Netzer O (2017). MTurk character misrepresentation: Assessment and solutions. Journal of Consumer Research, 44, 211–230. doi: 10.1093/jcr/ucx053 [DOI] [Google Scholar]
- Williams J, Ellis NC, Tyers C, Healy H, Rose G, & Macleod AK (1996). The specificity of autobiographical memory and imageability of the future. Memory & Cognition, 24, 116–125. doi: 10.3758/bf03197278 [DOI] [PubMed] [Google Scholar]
- Williams JM, & Broadbent K (1996). Autobiographical memory in suicide attempters. Journal of Abnormal Psychology, 95, 144–149. doi: 10.1037/0021-843X.95.2.144 [DOI] [PubMed] [Google Scholar]
- Williams JMG, Barnhofer T, Crane C, Hermans D, Raes F, Watkins E, et al. (2007). Autobiographical memory specificity and emotional disorder. Psychological Bulletin, 133, 122–148. doi: 10.1037/0033-2909.133.1.122 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wing JF, Schutte NS, & Byrne B (2006). The effect of positive writing on emotional intelligence and life satisfaction. Journal of Clinical Psychology, 62, 1291–1302. doi: 10.1002/jclp.20292 [DOI] [PubMed] [Google Scholar]
- Wortmann JH, Jordan AH, Weathers FW, Resick PA, Dondanville KA, Hall-Clark B, et al. (2016). Psychometric analysis of the PTSD Checklist-5 (PCL-5) among treatment-seeking military service members. Psychological Assessment, 28, 1392–1403. doi: 10.1037/pas0000260 [DOI] [PubMed] [Google Scholar]
- Zinbarg RE, Rekart KN, & Mineka S (2006). Autobiographical memory in dysphoric and non- dysphoric college students using a computerised version of the AMT. Cognition and Emotion, 20, 506–515. doi: 10.1080/02699930500341318 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.