Abstract
Background:
For the surgical treatment of traumatic hollow viscus injuries, laparoscopy offers a potentially less morbid approach to open exploration among appropriately selected patients. This study aimed to evaluate utilization trends and efficacy of laparoscopy in the management of pediatric abdominal trauma.
Study Design:
To gain both study granularity and power, our institutional trauma registry (2005-2017) and the National Trauma Data Bank (NTDB; 2010-2015) identified patients <18 years who required celiotomy for abdominal trauma. Injury mechanisms, patient characteristics, and hospital courses were compared between open and laparoscopic approaches. Unadjusted and adjusted statistical analyses were performed.
Results:
Overall, data were similar among 393 institutional and 11,399 NTDB patients undergoing laparoscopic (n=88, 22%; n=1,663, 16%) or open (n=305, 78%; n=9,736, 85%) surgery for abdominal trauma. In both registries, laparoscopy was more commonly employed in younger (institutional p=0.026; NTDB p<0.001) female (p=0.019; p<0.001) patients having lower injury severity (p<0.001) and blunt injuries (p=0.031; p<0.001). Laparoscopy associated with fewer complications overall when adjusting for demographics and injury severity [institutional OR 0.25 (0.08 – 0.75), p=0.013; NTDB OR 0.69 (0.55 – 0.88), p=0.002]. An increase in utilization of MIS for pediatric abdominal trauma was detected over time (NTDB: r=0.88, p=0.02).
Conclusion:
For the management of pediatric abdominal trauma, laparoscopy was employed typically in younger, more stable, and female patients sustaining blunt injuries. Appropriately selected patients have similar or better outcomes to patients treated with laparotomy, with no increase in adverse events or missed injuries. Increased utilization of laparoscopy to manage abdominal trauma in children suggests greater acceptance of this approach.
Level of Evidence:
Level III
Keywords: pediatric trauma, laparoscopy, intestinal injuries, National Trauma Data Bank
1. Introduction
Pediatric abdominal trauma is a common problem having diverse mechanisms, presentations, and injury patterns. In the typical context of multi-system trauma among children, the gastrointestinal tract remains the most common site of initially undiagnosed and potentially fatal injuries if missed (1). Due to the physiologic reserve of children and often concomitant distracting injuries, hollow viscus injuries can manifest subtly over time. Criteria and opinions vary on the optimal timing and approach to diagnose and/or treat gastrointestinal injuries. Given the rising popularity of MIS across surgical specialties, laparoscopy is gaining traction in the definitive management of abdominal trauma among both adults and children. Laparoscopy appears to be an effective tool for resolving diagnostic uncertainty in a hemodynamically stable child having a concerning exam and equivocal imaging in the context of blunt or penetrating abdominal trauma (2, 3). If a laparotomy is nontherapeutic, the morbidity has been reported as high as 41.3%, and the associated costs are increased 1.78-fold when compared to a diagnostic laparoscopy (4–6). Therefore, the minimally invasive approach is an appealing alternative to open exploration in appropriately selected patients.
The use of laparoscopy in abdominal trauma with the intent to treat, not solely diagnose, a hollow viscus injury is less well studied, particularly in children (Figure 1). Our group has examined previously the use of therapeutic laparoscopy in children having isolated traumatic bowel injuries and found a trend towards improved outcomes. However, that prior study appeared early in the experience of applying laparoscopy to highly selected pediatric patients sustaining blunt focal abdominal trauma only and was limited by small sample size and only a few surgeons having experience (7). Similarly, other retrospective studies have indicated a likely benefit to therapeutic laparoscopy but incompletely characterized the indications and patient selection, outcomes, and national trends when utilizing MIS (8–14). An appropriately matched cohort study of substantial size and power comparing the open and MIS approach to abdominal trauma in children has not been published to date.
Figure 1. Therapeutic laparoscopy for pediatric abdominal trauma.
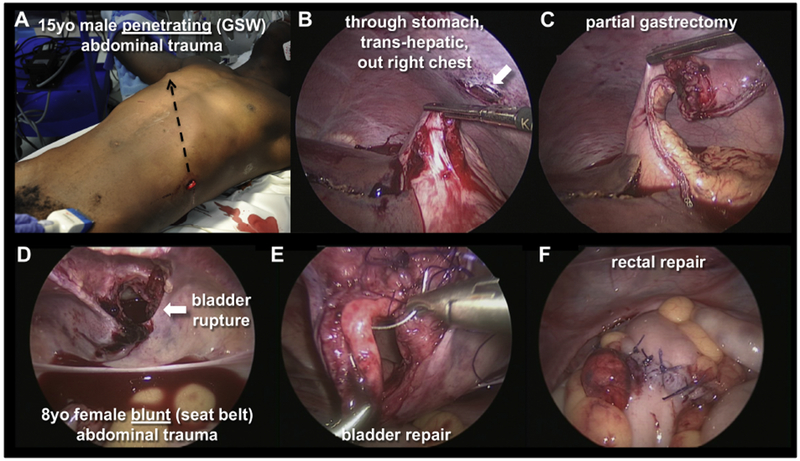
(A-C) 15 YO male with penetrating abdominal trauma (gunshot wound) traversing through-and-through stomach, trans-hepatically, and out right chest (A, black, dashed arrow indicates trajectory; B, white arrow indicates exit wound through right chest). Partial gastrectomy was completed laparoscopically (C). (D-F) 8 YO female with blunt abdominal trauma due to a seat belt injury. Bladder repair (E) and rectal repair (F) completed laparoscopically.
This study sought to characterize the use of laparoscopy for definitive management in pediatric abdominal trauma, evaluating indications and patient selection as well as outcomes and trends in the use of MIS over time. Patient data were queried from both the National Trauma Data Bank (NTDB) and our institutional trauma registry to attain both power and granularity in the analysis (15). We hypothesized that the use of laparoscopy to treat pediatric abdominal trauma in appropriately selected patients would associate with equivalent or improved outcomes to the standard of laparotomy. Specifically, we speculated that therapeutic laparoscopy would be associated with improved outcomes, including shortened length of stay and reduced complications when compared to laparotomy in comparable patients, and that missed injuries would not be exacerbated. Furthermore, we hypothesized that use of laparoscopy in pediatric abdominal trauma has increased over time as surgeons have become increasingly facile with minimally invasive techniques.
2. Materials and Methods
The Vanderbilt Institutional Review Board approved all aspects of this study (#162129).
2.1. Patient Selection
To attain both power and granularity in this study, patient data were acquired respectively from the NTDB and our institutional trauma registry. Among patients registered in the NTDB from 2010-2015 (i.e., the last 6 years available at time of study), those 18 years and younger who received an abdominal operation were selected using the International Classification of Disease, 9th Revision (ICD-9) procedure codes for exploratory laparotomy (54.11), laparoscopy (54.21), and other laparotomy (54.19). In this context, 11,399 patients met inclusion criteria. Our institutional trauma registry was queried from 2005-2017 applying the same criteria, and 393 patients met inclusion criteria. Demographic as well as preoperative and postoperative outcome data were collected for each cohort.
This analysis examined only the first abdominal operation performed on each patient during their hospital stay. Among the institutional cohort, this intervention was determined directly from a detailed chart review; among the NTDB, this operation was determined from the procedure codes associated with the shortest time from admission to procedure. In both cohorts, patients were classified as receiving laparotomy, laparoscopy, or laparoscopy converted to laparotomy based on the first abdominal operation. Conversions were handled according to the specific intent of each analysis as indicated throughout the text. For analyses assessing patient and trauma characteristics associated with operative approach, conversions were included in the laparoscopy group. For the analysis of postoperative outcome variables, conversions were excluded from analysis due to inability to assess reason for conversion.
Operations were characterized as therapeutic if any intervention was performed beyond simple diagnostic exploration. In the institutional database, this distinction was determined directly from review of the medical record and operative reports. In the NTDB, operations having additional procedure codes beyond the exploratory laparotomy and/or laparoscopy (54.11, 54.21, and 54.19) were determined to be therapeutic. In order to achieve an analysis that was simple and consistent with the aims of this study, a therapeutic determination was only made in NTDB patients for whom their first abdominal operation was also their first overall operation (48.6% of the total cohort, n = 5,540). Patients who had another operation preceding the first abdominal operation (e.g., craniotomy, orthopedic repair, etc.) were excluded from this subgroup analysis.
Patient and trauma characteristics considered in this study included age, gender, injury severity score (ISS), Glasgow Coma Score (GCS), mechanism of injury, systolic blood pressure, and pulse. Outcome variables of interest included operative time, estimated blood loss (EBL), length of stay (LOS), ICU days, ventilator days, all complications (including missed injuries requiring a subsequent intervention), small bowel obstruction, and vital status at discharge. A determination of the hospital type in which patients were operated on (pediatric versus adult) was made based on the attending surgeon in the institutional cohort and on a unique facility code variable in the NTDB.
2.2. Statistical Analysis
Data for each cohort were summarized using the median and interquartile range. The Wilcoxon rank sums test was applied to two-group continuous variables (Kruskal-Wallis for more than two groups), and the Pearson chi-squared test was applied to categorical variables. A Pearson correlation coefficient was used to assess trends in use of laparoscopy over time. Univariate and multivariate logistic regression were applied to assess patient and trauma characteristics associated with operative approach including age at injury, gender, mechanism of injury, injury severity score, Glasgow Coma Score, pulse, and systolic blood pressure. Unadjusted outcomes were compared between operative approaches using Wilcoxon rank sums test for continuous variables and Pearson chi-squared test for categorical variables. Linear and logistic regression were employed to assess operative outcomes between approaches while adjusting for age, gender, mechanism of injury, injury severity score, systolic blood pressure, heart rate, and Glasgow Coma Score. Due to a smaller sample size in the institutional cohort, a propensity score was assigned based on the previously mentioned variables and regression analyses were subsequently completed with adjustment for the propensity score. Subgroup analyses were performed to assess operative outcomes for patients undergoing therapeutic operations only. Statistical significance was set at p<0.05.
3. Results
3.1. Demographics and Cohorts
Institutional and NTDB data were first compared to ensure our institution resembled the national experience before analyzing more granular details (Table 1). Indeed, the institutional (n=393) and the NTDB cohorts (n=11,399) were generally similar for the data analyzed (Table 1). Although the Vanderbilt Trauma Registrar reports cases to the NTDB, the potential for duplicated cases between data sets was only 3.4%. Notable differences in demographics and trauma type included gender, race, mechanism of injury, and injury severity score. Institutional patients were 69% male and 65% white compared to 75% male and 48% white in the NTDB (p=0.029 for gender and p<0.001 for race, Table 1), although notably race was not reported for 20% of NTDB patients. The institutional cohort included a higher proportion of patients presenting with blunt trauma compared to the NTDB (63% versus 50%, p<0.001). ISS was higher in the institutional (17.0 [9.0, 27.5]) compared to the NTDB cohort (14.0 [9.0, 26.0], p<0.001; Table 1). Vital signs and GCS on admission, length of stay, and vital status at discharge appeared clinically comparable between cohorts (Table 1). Laparoscopy was utilized more frequently in the institutional cohort, with 16% of institutional cases completed laparoscopically (73% of which were therapeutic) versus 12% of NTDB cases (64% of which were determined confidently to represent therapeutic interventions; p<0.001, Table 1).
Table 1.
Patient and trauma characteristics of institutional and NTDB cohorts
| Institutional (n = 393) | NTDB (n = 11,399) | p-value | |
|---|---|---|---|
| Age at injury (years) | 15.9 [9.1, 17.7] | 16.0 [11.0, 17.0] | 0.476 |
| Gender | |||
| Male | 271 (69%) | 8,527 (75%) | 0.029 |
| Female | 122 (31%) | 2,868 (25%) | |
| Race | |||
| White | 254 (65%) | 5,453 (48%) | <0.001 |
| Black | 110 (28%) | 3,370 (30%) | |
| Asian | 2 (1%) | 160 (1%) | |
| American Indian | 1 (0%) | 94 (1%) | |
| Other/Unknown | 24 (6%) | 2,322 (20%) | |
| Mechanism of Injury | |||
| Blunt | 246 (63%) | 5,715 (50%) | <0.001 |
| Penetrating | 121 (31%) | 5,003 (44%) | |
| Other/Unspecified | 24 (6%) | 606 (5%) | |
| Injury Severity Score | 17.0 [9.0, 27.5] | 14.0 [9.0, 26.0] | < 0.001 |
| ED Pulse (beats per minute) | 106.0 [88.0, 125.0] | 104.0 [87.0, 124.0] | 0.300 |
| ED Systolic Blood Pressure (mmHg) | 118.0 [106.0, 130.0] | 121.0 [105.0, 137.0] | < 0.001 |
| ED Respiratory Rate (breaths per min) | 20.0 [18.0, 24.0] | 20.0 [18.0, 24.0] | 0.265 |
| ED Temperature (F) | 98.2 [97.6, 98.6] | 98.1 [97.0, 98.6] | < 0.001 |
| ED Glasgow Coma Score | 15.0 [14.0, 15.0] | 15.0 [14.0, 15.0] | 0.930 |
| Time to Incision (hours) | 2.5 [0.9, 5.5] | 2.0 [1.0, 4.8] | 0.238 |
| Operative Approach | |||
| MIS | 64 (16%) | 1,363 (12%) | <0.001 |
| Open | 305 (78%) | 9,736 (85%) | |
| Conversion | 24 (6%) | 300 (3%) | |
| Length of Stay (days) | 6.0 [4.0, 10.8] | 7.0 [4.0, 13.0] | 0.025 |
| ICU days | 0 [0, 4] | 1 [0, 5] | < 0.001 |
| Ventilator days | 0 [0, 2] | 0 [0, 2] | 0.052 |
| Vital status at discharge | |||
| Alive | 357 (91%) | 10,217 (90%) | 0.221 |
| Deceased/Expired | 36 (9%) | 1,099 (10%) | |
| Not Known/Recorded | 0 | 83 (1%) | |
NTDB, National Trauma Data Bank; ED, emergency department; ICU, intensive care unit; F, Fahrenheit
3.2. Operative indications and procedures
Operative indications and procedural data were collected for the institutional database. CT scans were performed preoperatively in 81% of patients overall. Indications for operation after imaging included evidence of intra-abdominal injury (45%), free fluid (45% of patients), pneumoperitoneum (17%), and evolving clinical concerns (21%, Table 2). No significant differences in indication between operative approaches was detected. The most commonly performed procedures were small bowel repair (34% of patients), large bowel repair (24%), and splenectomy or splenorrhaphy (18%, Table 2). Regarding procedures performed, significant differences were observed between operative approaches for: splenorrhaphy/splenectomy (22% of laparotomies vs. 2% of laparoscopies vs. 0% of conversions; p < 0.001); small bowel repair (36% vs. 13% vs. 67%, respectively; p < 0.001); and hepatorrhaphy (12% vs. 0% vs. 0%, respectively; p = 0.003, Table 2). No statistically significant differences were detected between operative approaches for other procedures, and statistical relationships were maintained with a binary comparision of laparotomy to laparoscopy (exclusing conversions). Of the 24 cases that were converted from laparoscopy to laparotomy, the most common reason was for repair of injuries more easily fixed via celiotomy (15 patients, 63%), followed by inadequate visualization of structures (8 patients, 33%). One patient (4%) was converted for both of these reasons.
Table 2.
Injury and Operative Data (Institutional)
| Combined (N = 393) | Laparotomy (N = 305) | Laparoscopy (N = 64) | Conversion (N = 24) | Binary p-value** | Overall p-value | |
|---|---|---|---|---|---|---|
| CT performed pre-op | ||||||
| No | 75 (19%) | 61 (20%) | 14 (22%) | 0 (0%) | 0.735 | 0.046 |
| Yes | 318 (81%) | 244 (80%) | 50 (78%) | 24 (100%) | ||
| Indication* | ||||||
| Intra-abdominal free fluid (imaging) | 176 (45%) | 137 (45%) | 28 (44%) | 11 (46%) | 0.864 | 0.980 |
| Intra-abdominal free air (imaging) | 67 (17%) | 50 (16%) | 11 (17%) | 6 (25%) | 0.876 | 0.558 |
| Intra-abdominal injury (imaging) | 175 (45%) | 141 (46%) | 24 (38%) | 10 (42%) | 0.202 | 0.424 |
| Concern for intra-abdominal injury | 84 (21%) | 68 (22%) | 12 (19%) | 4 (17%) | 0.531 | 0.693 |
| Other | 5 (1%) | 3 (1%) | 2 (3%) | 0 (0%) | 0.178 | 0.323 |
| Procedures performed* | ||||||
| Small bowel repair | 135 (34%) | 111 (36%) | 8 (13%) | 16 (67%) | <0.001 | < 0.001 |
| Large bowel repair | 93 (24%) | 76 (25%) | 9 (14%) | 8 (33%) | 0.061 | 0.092 |
| Splenorrhaphy/splenectomy | 69 (18%) | 68 (22%) | 1 (2%) | 0 (0%) | <0.001 | < 0.001 |
| Chest tube | 37 (9%) | 36 (12%) | 0 (0%) | 1 (4%) | 0.004 | 0.009 |
| Hepatorrhaphy | 36 (9%) | 36 (12%) | 0 (0%) | 0 (0%) | 0.004 | 0.003 |
| Gastrorrhaphy | 29 (7%) | 25 (8%) | 3 (5%) | 1 (4%) | 0.335 | 0.512 |
| Vascular repair | 27 (7%) | 26 (9%) | 1 (2%) | 0 (0%) | 0.052 | 0.053 |
| Partial pancreatectomy | 22 (6%) | 21 (7%) | 1 (2%) | 0 (0%) | 0.102 | 0.114 |
| Mesenteric repair | 20 (5%) | 15 (5%) | 2 (3%) | 3 (13%) | 0.534 | 0.196 |
| Diaphragmatic repair | 20 (5%) | 17 (6%) | 3 (5%) | 0 (0%) | 0.776 | 0.483 |
| Kidney repair/nephrectomy | 14 (4%) | 14 (5%) | 0 (0%) | 0 (0%) | 0.081 | 0.123 |
| Bladder repair | 14 (4%) | 12 (4%) | 2 (3%) | 0 (0%) | 0.758 | 0.593 |
| Cholecystectomy | 6 (2%) | 6 (2%) | 0 (0%) | 0 (0%) | 0.258 | 0.415 |
| Appendectomy | 5 (1%) | 5 (2%) | 0 (0%) | 0 (0%) | 0.302 | 0.482 |
| Salpingo/oophorectomy | 1 (0%) | 1 (0%) | 0 (0%) | 0 (0%) | 0.646 | 0.865 |
| Other | 126 (32%) | 96 (31%) | 25 (39%) | 5 (21%) | 0.240 | 0.237 |
| Indication for conversion | ||||||
| Injury repair | -- | -- | -- | 15 (63%) | -- | -- |
| Inadequate visualization | -- | -- | -- | 8 (33%) | ||
| Both | -- | -- | -- | 1 (4%) | ||
Some patients had multiple indications or procedures performed
Binary p-value compares laparotomy vs. laparoscopy
3.3. Patient and trauma characteristics by approach
3.3.1. Institutional cohort
Among the institutional cohort, a laparoscopic, relative to open, approach was associated with younger age (10.7 years [7.5, 14.8] versus 16.7 years [10.5, 18.0], p<0.001), female gender (41% versus 28% female, p=0.023), blunt mechanism of injury (71% versus 61%,p=0.001), and a lower ISS (10.0 [7.0, 17.5] versus 18.0 [10.0, 33.0], p<0.001; Table 3). Laparoscopy was significantly more likely to be performed at our pediatric compared to adult hospital, with 89% of these procedures being performed at our ACS-verified Level I Pediatric Trauma Center (p<0.001), which could account for patient age differences. Interestingly, laparoscopy was associated with an increased time to procedure from arrival (4.5 hours [3.0, 11.9] versus 1.5 hours [0.8,4.4], p<0.001; Table 3).
Table 3.
Patient and trauma characteristics by initial operative approach
| INSTITUTION | NTDB | |||||
|---|---|---|---|---|---|---|
| Laparotomy (n = 305) | Laparoscopy* (n = 88) | p-value | Laparotomy (n = 9,736) | Laparoscopy* (n = 1,663) | p-value | |
| Age at injury (years) | 16.7 [10.5, 18.0] | 10.7 [7.5, 14.8] | < 0.001 | 16 [12, 18] | 14 [8, 17] | < 0.001 |
| Gender | ||||||
| Male | 219 (72%) | 52 (59%) | 0.023 | 7,360 (76%) | 1,167 (70%) | < 0.001 |
| Female | 86 (28%) | 36 (41%) | 2,374 (24%) | 494 (30%) | ||
| Race | ||||||
| White | 191 (63%) | 63 (72%) | 0.314 | 4.590 (47%) | 863 (52%) | 0.002 |
| Black | 89 (29%) | 21 (24%) | 2,924 (30%) | 446 (27%) | ||
| Asian | 1 (0%) | 1 (1%) | 138 (1%) | 22 (1%) | ||
| American Indian | 1 (0%) | 0 | 76 (1%) | 18 (1%) | ||
| Other/Unknown | 21 (7%) | 2 (2%) | 2,008 (20%) | 314 (19%) | ||
| Mechanism of Injury | ||||||
| Blunt | 184 (61%) | 62 (71%) | 0.001 | 4,853 (50%) | 862 (52%) | < 0.001 |
| Penetrating | 106 (35%) | 15 (17%) | 4,374 (45%) | 629 (38%) | ||
| Other/Unspecified | 14 (5%) | 10 (11%) | 509 (6%) | 172 (10%) | ||
| Location of operation | ||||||
| Children’s hospital | 116 (38%) | 78 (89%) | < 0.001 | 2,692 (28%) | 641 (39%) | < 0.001 |
| Adult hospital | 189 (62%) | 10 (11%) | 7,044 (72%) | 1,022 (61%) | ||
| Injury Severity Score | 18.0 [10.0, 33.0] | 10.0 [7.0, 17.5] | < 0.001 | 16 [9, 27] | 9 [4, 16] | < 0.001 |
| ED Pulse (beats per minute) | 107 [88.5, 128] | 104 [88, 117] | 0.230 | 104 [86, 125] | 102 [87, 119] | < 0.001 |
| ED Systolic Blood Pressure (mmHg) | 118.0 [102.0, 130.0] | 118.0 [109.5, 126.0] | 0.952 | 120 [104, 138] | 122 [110, 136] | < 0.001 |
| ED Respiratory Rate (breaths per minute) | 20 [17, 24] | 21 [18, 25] | 0.082 | 20 [18, 24] | 20 [18, 24] | 0.252 |
| ED Temperature (F) | 98.1 [97.5, 98.8] | 98.2 [97.7, 98.5] | 0.653 | 97.9 [97.0, 98.6] | 98.2 [97.5, 98.8] | < 0.001 |
| ED Glasgow Coma Score | 15 [11, 15] | 15 [15, 15] | 0.003 | 15 [14, 15] | 15 [15, 15] | < 0.001 |
| Time to Incision (hours) | 1.5 [0.8, 4.4] | 4.5 [3.0, 11.9] | < 0.001 | 1.8 [1,4] | 4 [2, 16.4] | < 0.001 |
Includes laparoscopy converted to laparotomy
NTDB, National Trauma Data Bank; ED, emergency department
Univariate and multivariate logistic regression were employed to assess which patient or trauma characteristics significantly predicted operative approach among the institutional cohort. In univariate analysis, laparoscopy was associated with younger patients (OR 0.89 [95% CI, 0.85 – 0.93], p<0.001), female gender (1.76 [1.08 – 2.89],p=0.02), blunt injury (2.38 [1.29 – 4.39],p=0.005), lower ISS (0.94 [0.92 – 0.96], p<0.001), and higher GCS (1.11 [1.03 – 1.19],p=0.003). Presenting ED pulse and SBP did not significantly associate with operative approach in the univariate analysis and thus were excluded from the multivariate analysis. In multivariate analysis, age (0.94 [0.87 – 0.99], p<0.026), female gender (1.99 [1.12 – 3.55], p=0.019), blunt mechanism (2.27 [1.08 – 4.78], p=0.031), and ISS (0.94 [0.91 – 0.97], p<0.001), but not GCS (1.00 [0.96 – 1.05], p=0.934), remained significant predictors of operative approach.
3.3.2. NTDB cohort
In the NTDB, similar trends were observed. A laparoscopic approach was associated with younger patients (14 years [8, 17] versus 16 years [12, 18],p<0.001), females (30% versus 24% female, p<0.001), blunt injury (52% versus 50%, p<0.001), and lower ISS (9 [4, 16] versus 16 [9, 27], p<0.001; Table 3). As in the institutional cohort, pediatric hospitals attempted a significantly greater percentage of cases laparoscopically (641 of 3,333 cases; 19%) compared to adult trauma centers (1,022 of 8,066 cases; 13%; p<0.001). Laparoscopy was again associated with an almost identically increased time to procedure (4 hours [2, 16.4] versus 1.8 hours [1, 4],p<0.001; Table 3).
Univariate and multivariate regression analyses showed laparoscopy to be significantly associated with younger age (adjusted OR 0.95 [0.94 – 0.96], p<0.001), female gender (1.36 [1.19 – 1.55], p<0.001), blunt injury (1.53 [1.34 – 1.75], p<0.001), lower ISS (0.94 [0.94 – 0.95], p<0.001), lower pulse (0.99 [0.97 – 0.99] per 5-unit change, p<0.001) and higher SBP (1.02 [1.01 – 1.03] per 5-unit change, p<0.001). Again, GCS was significant in univariate (1.09 [1.08 – 1.11],p<0.001) but not multivariate (1.00 [0.99 – 1.03],p=0.58) analysis. Of note, odds ratios for presenting pulse and SBP were very close to 1.00, indicating that these variables are likely not clinically significant despite being statistically significant.
3.4. Outcomes based on operative approach
3.4.1. Institutional cohort
Comparing all laparoscopic (n=64) to open (n=305) operations in the institutional cohort, laparoscopy was associated with decreased EBL (15 ml [10, 25] versus 300 ml [100, 1000], p<0.001), shorter length of stay (3 days [2, 5] versus 6 days [4, 12], p<0.001), decreased ICU days (0 days [0, 0] versus 1 day [0, 4],p<0.001), and decreased mortality at discharge (2% versus 11%,p=0.015; Table 4). No specific complication reached a statistically significant difference between approaches, but overall complications were reduced in the laparoscopic group (8% versus 33%, p<0.001; Table 4). These differences likely associate with use of laparoscopy for less severely injured and more stable patients. Therefore, regression analyses were completed controlling for age, gender, MOI, ISS, SBP, heart rate, and GCS. In the adjusted analysis, operative time, EBL, length of stay, ICU days, ventilator days, and vital status lost statistical significance despite trends remaining in favor of laparoscopy. However, laparoscopy was still associated with decreased overall complications (adjusted OR 0.25 [95% CI, 0.08 – 0.75], p=0.013), including decreased incidence of small bowel obstruction (SBO, OR 0.03 [95% CI, 0.02 – 0.06], p<0.001). However, with an overall SBO rate of just 4% (14 of 369 patients), the OR cannot be reliably interpreted in this context. It is possible that a larger sample size would provide a more clinically meaningful OR.
Table 4.
Operative outcomes by approach - all cases
| INSTITUTION | NTDB | |||||
|---|---|---|---|---|---|---|
| Laparotomy (n = 305) | Laparoscopy (n = 64) | p-value | Laparotomy (n = 9,736) | Laparoscopy (n = 1,363) | p-value | |
| Operating time | 100 [65, 147] | 85 [64, 127] | 0.216 | -- | -- | -- |
| Estimated Blood Loss (ml) | 300 [100, 1000] | 15 [10, 25] | < 0.001 | -- | -- | -- |
| Therapeutic operation | ||||||
| Yes | 295 (97%) | 47 (73%) | < 0.001 | 3,968 (83%) | 402 (64%) | < 0.001 |
| No | 10 (3%) | 17 (27%) | 818 (17%) | 230 (36%) | ||
| Length of Hospital Stay (days) | 6 [4, 12] | 3 [2, 5] | < 0.001 | 7 [4, 13] | 4 [2, 8] | < 0.001 |
| ICU Days | 1 [0, 4] | 0 [0, 0] | < 0.001 | 2 [0. 51 | 0 [0, 2] | < 0.001 |
| Ventilator Days | 0 [0, 2] | 0 [0, 0] | < 0.001 | 0 [0, 2] | 0 [0, 0] | < 0.001 |
| Any Hospital Complication | ||||||
| No | 205 (67%) | 59 (92%) | < 0.001 | 7,852 (81%) | 1,250 (92%) | < 0.001 |
| Yes | 100 (33%) | 5 (8%) | 1,884 (19%) | 113 (8%) | ||
| Missed Injury/Re-exploration | ||||||
| No | 295 (97%) | 64 (100%) | 0.142 | -- | -- | -- |
| Yes | 10 (3%) | 0 | -- | -- | ||
| Surgical Site Infection | ||||||
| No | 11 (4%) | 0 | 0.123 | 9,401 (97%) | 1,357 (100%) | < 0.001 |
| Yes | 294 (96%) | 64 (100%) | 335 (3%) | 6 (0%) | ||
| Postoperative ileus | ||||||
| No | 285 (93%) | 63 (98%) | 0.117 | -- | -- | -- |
| Yes | 20 (7%) | 1 (2%) | -- | -- | ||
| Small Bowel Obstruction | ||||||
| No | 235 (77%) | 45 (70%) | 0.161 | -- | -- | -- |
| Yes | 13 (4%) | 1 (2%) | -- | -- | ||
| No long-term follow-up | 57 (19%) | 18 (28%) | -- | -- | ||
| Vital status at discharge | ||||||
| Alive | 270 (89%) | 63 (98%) | 0.015 | 8,573 (88%) | 1,346 (99%) | < 0.001 |
| Dead | 35 (11%) | 1 (2%) | 1,091 (11%) | 6 (0%) | ||
Excludes conversions
Institutional hospital complications include: missed injury or re-exploration, unplanned return to OR, surgical site infection, other local infection, bacteremia, fungemia, or ileus
NTDB hospital complications include: abdominal compartment syndrome, abdominal fascia left open, acute renal failure, acute respiratory distress syndrome, base deficit, bleeding, cardiac arrest with CPR, coagulopathy, coma, decubitus ulcer, surgical site infection, drag or alcohol withdrawal syndrome, deep vein thrombosis, extremity compartment syndrome, graft/prosthesis/flap failure, elevated intracranial pressure, myocardial infarction, pneumonia, pulmonary embolism, stroke, systemic sepsis, unplanned intubation, or wound disruption
Comparing outcomes from institutional cases that were therapeutic (n=295 laparotomy, 47 laparoscopy), laparoscopy was associated with decreased EBL (15 ml [10, 25] versus 300 ml [100, 1000], p<0.001), decreased length of stay (3.5 days [2, 5] versus 6 days [4, 12], p<0.001), decreased ICU days (0 days [0, 0] versus 1 day [0, 4],p<0.001), and decreased mortality at discharge (2% versus 12%, p=0.048; Table 5). Again, while no specific complication reached statistical difference between the two groups, overall complications were lower in the laparoscopic group (11% versus 34%, p=0.001, Table 5). No significant difference in operative time between approaches was detected (p=0.572, Table 5).
Table 5.
Operative outcomes by approach – therapeutic cases only
| INSTITUTION | NTDB | |||||
|---|---|---|---|---|---|---|
| Laparotomy (n = 295) | Laparoscopy (n = 47) | p-value | Laparotomy (n = 3,968) | Laparoscopy (n = 402) | p-value | |
| Operating time | 101 [66, 148] | 88 [72, 130] | 0.572 | -- | -- | -- |
| Estimated Blood Loss (ml) | 300 [100, 1000] | 15 [10, 25] | < 0.001 | -- | -- | -- |
| Length of Hospital Stay (days) | 6 [4, 12] | 3.5 [2, 5] | < 0.001 | 7 [4, 13] | 3 [2, 7] | < 0.001 |
| ICU Days | 1 [0, 4] | 0 [0, 0] | < 0.001 | 1 [0, 4] | 0 [0, 1 | < 0.001 |
| Ventilator Days | 0 [0, 2] | 0 [0, 0] | < 0.001 | 0 [0, 1] | 0 [0, 0] | < 0.001 |
| Any Hospital Complication | ||||||
| No | 195 (66%) | 42 (89%) | 0.001 | 3,276 (83%) | 387 (96%) | < 0.001 |
| Yes | 100 (34%) | 5 (11%) | 692 (17%) | 15 (4%) | ||
| Missed Injury/Re-exploration | ||||||
| No | 285 (97%) | 47 (100%) | 0.200 | -- | -- | |
| Yes | 10 (3%) | 0 | -- | -- | ||
| Surgical Site Infection | ||||||
| No | 284 (96%) | 47 (100%) | 0.178 | 3,817 (96%) | 402 (100%) | <0.001 |
| Yes | 11 (4%) | 0 | 151 (4%) | 0 (0%) | ||
| Postoperative ileus | ||||||
| No | 275 (93%) | 46 (98%) | 0.217 | -- | -- | -- |
| Yes | 20 (7%) | 1 (2%) | -- | -- | ||
| Small Bowel Obstruction | ||||||
| No | 228 (77%) | 34 (72%) | 0.469 | -- | -- | -- |
| Yes | 12 (4%) | 1 (2%) | -- | -- | ||
| No long-term follow-up | 55 (19%) | 12 (26%) | -- | -- | ||
| Vital status at discharge | ||||||
| Alive | 261 (88%) | 46 (98%) | 0.048 | 3,558 (90%) | 392 (100%) | < 0.001 |
| Dead | 34 (12%) | 1 (2%) | 381 (10%) | 1 (0%) | ||
Excludes conversions
Institutional hospital complications include: missed injury or re-exploration, unplanned return to OR, surgical site infection, other local infection, bacteremia, fungemia, or ileus
NTDB hospital complications include: abdominal compartment syndrome, abdominal fascia left open, acute renal failure, acute respiratory distress syndrome, base deficit, bleeding, cardiac arrest with CPR, coagulopathy, coma, decubitus ulcer, surgical site infection, drag or alcohol withdrawal syndrome, deep vein thrombosis, extremity compartment syndrome, graft/prosthesis/flap failure, elevated intracranial pressure, myocardial infarction, pneumonia, pulmonary embolism, stroke, systemic sepsis, unplanned intubation, or wound disruption
Similarly, after controlling for age, gender, MOI, ISS, SBP, heart rate, and GCS with a propensity score, laparoscopy was associated with a decreased incidence of SBO (OR 0.04 [95% CI, 0.02 – 0.08], p<0.001). No significant difference between approaches was observed for all complications (0.36 [0.12 – 1.09], p=0.07). However, there was a trend towards decreased complications with therapeutic laparoscopy. Again, no significant difference was observed in operative time (18.0 min difference [95% Cl on β, −46.7 – 9.5], p=0.20), EBL (415 ml difference [95% Cl on beta, −1,303 – 471.8], p=0.35), length of stay (4.0 day difference [95% Cl on beta, −9.1 – 1.2], p=0.13), or vital status (OR 0.0005 [0 – 1.4e19], p=0.77) between therapeutic laparoscopy and therapeutic laparotomy in this controlled subgroup analysis.
3.4.2. NTDB Cohort
In the NTDB, comparing all laparoscopic (n=1,363) versus open (n=9,736) cases, laparoscopy was associated with decreased length of stay (4 days [2, 8] versus 7 days [4, 13], p<0.001), decreased ICU days (0 days [0, 2] versus 2 days [0, 5], p<0.001), fewer hospital complications (8% versus 19%, p<0.001), and decreased mortality (<1% versus 11%,p<0.001; Table 4).
Interestingly, regression analyses controlling for age, gender, MOI, ISS, SBP, heart rate, and GCS demonstrated a significant association between laparoscopy and increased ICU days (0.75-day difference [95% Cl on β, 0.28 – 1.21 ], p=0.002). However, since an ICU stay after laparoscopy was a relatively rare occurrence (i.e., ICU days = 0), this result is likely skewed by a few outlying events. As with the institutional cohort, laparoscopy was associated with decreased hospital complications (adjusted OR 0.69 [0.55 – 0.88], p=0.002). Specifically, laparoscopy was associated with decreased odds of SSI (adjusted OR 0.16 [0.07 – 0.39], p<0.001). Though laparoscopy was also significantly associated with decreased mortality in the controlled analysis (OR 0.08 [95% CI, 0.03 – 0.19], p<0.001), a low overall mortality rate and a 0% morality rate in the laparoscopy likely contribute to a statistical difference in the absence of a true clinical difference.
For NTDB cases in which presence or absence of a therapeutic intervention could be assessed (n=402 laparoscopic, 3,968 open), laparoscopy was associated with decreased length of stay (3 days [2, 7] versus 7 days [4, 12], p<0.001), decreased ICU days (0 days [0, 1] versus 1 day [0, 4], p<0.001), decreased hospital complications (4% versus 17%, p<0.001) and decreased mortality (<1% versus 10%, p<0.001; Table 5). When controlling for age, gender, MOI, ISS, SBP, heart rate, and GCS, laparoscopy continued to associate with decreased length of stay (1.6 days [95% Cl on β, −2.8 – −4.0], p=0.009) and decreased hospital complications (OR 0.41 [0.23 – 0.74], p=0.003).
3.5. Laparoscopy utilization over time
In the institutional cohort, the percentage of all cases completed laparoscopically appeared to increase overtime, although the relationship was not statistically significant (r=0.36, p=0.22 Figure 2A). Similarly, for therapeutic cases at our institution, the percentage of cases completed laparoscopically appeared to increase over time, but the relationship also was not statistically significant (r=0.23, p=0.45; Figure 2B). Among all cases registered in the NTDB, a statistically significant increase in utilization of MIS for pediatric abdominal trauma (r=0.88, p=0.02), however, among clear therapeutic cases completed laparoscopically over time, only a trend in this approach was detected (r=0.26, p=0.66; Figure 2).
Figure 2. Utilization of laparoscopy to treat pediatric abdominal trauma over time.
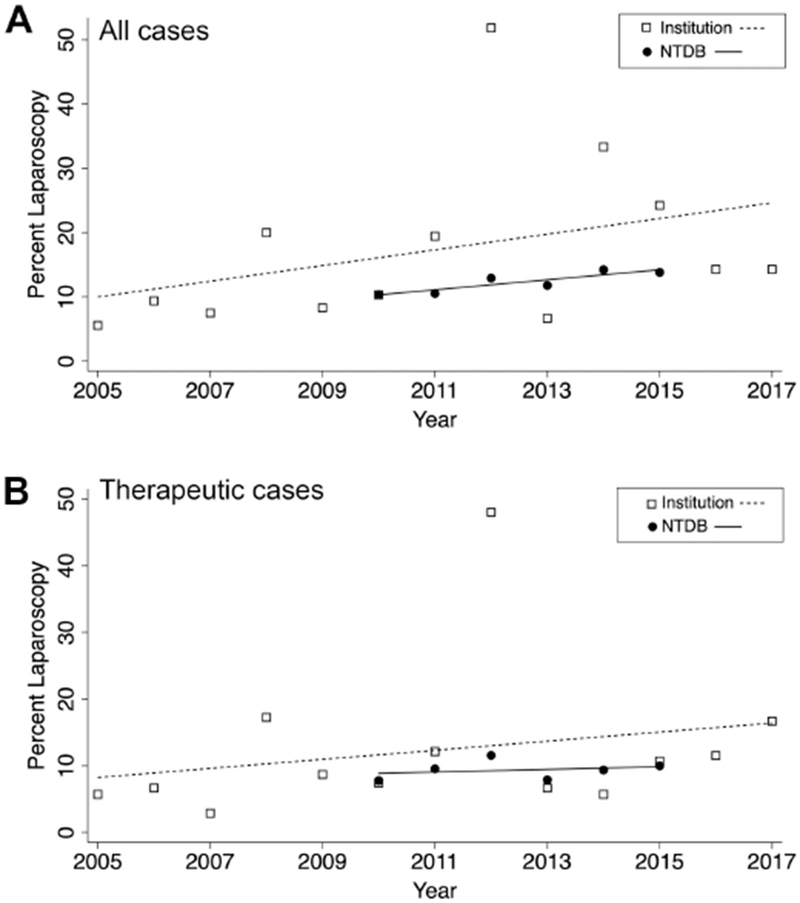
(A) Percentage of all operations for pediatric abdominal trauma completed over time. Institutional data represented by hollow squares with corresponding linear fit represented by dashed line (r=0.36, p=0.22). NTDB data represented by solid circles with corresponding linear fit represented by solid line (r=0.88, p=0.02). (B) Percentage of therapeutic operations for pediatric abdominal trauma completed over time. Institutional data represented by hollow squares with corresponding linear fit represented by dashed line (r=0.23, p=0.45). NTDB data represented by solid circles with corresponding linear fit represented by solid line (r=0.26, p=0.66).
4. Discussion
Parallel analysis of a busy ACS-verified Level 1 Pediatric Trauma Center and the NTDB demonstrated foremost that laparoscopy in the therapeutic management of pediatric abdominal trauma is safe and efficacious in appropriately selected patients. Laparoscopy was typically used in younger, more stable, female patients sustaining blunt mechanisms of injury and by pediatric surgeons. Hollow viscus perforation or devascularization were the most common injury patterns repaired laparoscopically, whereas liver and kidney injuries were always repaired with a laparotomy. However, a wide variety of injuries were successfully repaired laparoscopically, including splenic, gastric, pancreatic, diaphragmatic, vascular, and bladder injuries. When adjusting for age, gender, MOI, ISS, SBP, heart rate, and GCS, laparoscopy associated with fewer complications, including SBO in the institutional cohort and SSI in the NTDB cohort. Our data indicate an increase in the use of therapeutic laparoscopy over time.
Several smaller retrospective studies with cohort sizes between 23 and 200 patients suggested that the use of laparoscopy in pediatric abdominal trauma also may be safe and appropriate in hemodynamically stable patients, and can reduce unnecessary laparotomies (9, 11, 13, 14). The power provided through our dual analysis of the largest reported institutional cohort and the NTDB offers persuasive evidence that the trends seen both in the current and previous studies are indeed valid. In all levels of our analysis, significant or near-significant findings in the institutional database were consistently significant in the larger national database. Furthermore, the safety of laparoscopy in pediatric abdominal trauma among appropriately selected patients is supported through this study. In no instance did an outcome measure reach significance in favor of laparotomy in either unmatched or matched analyses, with the sole exception of ICU days in the NTDB, as discussed above. Even operative time, while apparently longer for laparoscopy, did not reach statistical significance in the institutional cohort. Moreover, therapeutic laparoscopy was shown in this study to be associated with fewer complications, even after adjusting for injury severity and demographics. The feared complication of missing an injury while operating laparoscopically did not occur in our large institutional cohort.
Given the demonstrated safety of therapeutic laparoscopy in this study, the physiologic characteristics associated with the MIS approach to treat abdominal trauma are indicative of accurate patient selection criteria. More specifically, patients who were younger, more stable, female, and presenting with a blunt mechanism of injury, emerged as more likely to be treated with MIS, and may well represent the ideal candidate. However, highly selected older males sustaining penetrating injuries were managed successfully with laparoscopy in our institution as well (Figure 1A–C). Notably, no obvious clinical reason explained why female patients would be favored over male patients in selection for a minimally invasive procedure. Although gender associated independently with laparoscopy in multivariate analysis after controlling for injury severity, the authors postulate that gender may somehow represent a surrogate for injury complexity. In other words, it is possible that female patients tended to be less severely injured or sustained less violent mechanisms. Indeed, further study is required to determine if laparoscopy is more or less safe for specific subgroups, such as male patients, older patients, and patients with penetrating mechanisms. Nonetheless, physiologic stability using age-specific parameters should always govern the decision for the optimal surgical approach to the injured abdomen of a child.
In addition to demonstrating the safety and efficacy of therapeutic laparoscopy in pediatric abdominal trauma, its growing application in this context also points to a shift in surgeon mindset. Though not reaching strict statistical significance, parallel trends detected in both our own center and in the NTDB indicate that surgeons are utilizing laparoscopy for the treatment of hollow viscus injuries in children with an increasing frequency over the last 10-15 years. We argue that, given the safety of the procedure in appropriately selected patients, increased surgical training in and clinical practice with MIS should yield greater confidence and experience to consider its use in pediatric abdominal trauma. One important consideration for surgeons hesitant to adopt laparoscopy in the minimally invasive context is the potential to delay definitive repair, particularly in cases that ultimately require conversion to an open procedure. Notably, among the 24 conversions that occurred at our hospital, for which complete records are available, none of the patients apparently suffered from delays in treatment.
This study has several limitations that temper broad generalizations and conclusions. As previously stated, appropriate patient selection is essential to the use of laparoscopy in any age abdominal trauma. Clearly not every patient is a candidate for MIS, and less stable patients and those having extensive, catastrophic abdominal injuries require open surgery, given the lengthier time to complete an MIS case, difficulty of vascular control with laparoscopy, inability to aspirate blood or succus while maintaining adequate iatrogenic pneumoperitoneum, and poor visibility with ileus. Moreover, operating with one’s hands is simply faster than with 5 mm instruments when time is essential. Therefore, randomization to generate level 1 evidence is highly impractical for the protean presentations the injured child experiences. Although less invasive, laparoscopy is not without risks, and prolonged insufflation is associated with compromised venous return, increased CO2 and acidosis, increased operative time, and reduced urine output after this approach (16–18).
Regarding our subgroup analysis, we recognize the possible bias introduced by excluding patients who had other operations preceding their first abdominal operation in the therapeutic NTDB subgroup (see Methods). However, we feel that any such bias would be inconsequential to the reported outcomes and that the size of that subgroup is still sufficiently large for a well-powered analysis (N=5,540). Finally, although our retrospective study design and database analyses indeed lack the strength of a randomized trial, we do find merit in the observations given the similarities in both cohorts with respect to the typical patient characteristics having MIS and the beneficial outcomes. Surgeon judgement is paramount.
In our study, surgeon experience, bias, and training may contribute to an increase in therapeutic laparoscopy over time, and this variable is difficult to control for in the NTDB. However, given that a strong positive trend is seen in a national database with thousands of surgeons, it is more likely that the field is truly becoming more comfortable with this practice at least in pediatric abdominal trauma. Finally, despite our adjusting for injury severity, it is still possible that operative approach is simply a surrogate for patient stability, thereby weakening the findings of decreased complications and mortality in the laparoscopy group. Yet, in the experience and opinion of the authors, this study corroborates, in the context of pediatric abdominal trauma, a growing body of evidence demonstrating improved outcomes with minimally invasive surgery compared to open operations, as documented for other diseases and conditions.
5. Conclusion
After analyzing both a regional and national trauma database, therapeutic laparoscopy appears to be a safe and effective tool in the therapeutic management of pediatric abdominal trauma among appropriately selected patients. MIS for pediatric abdominal trauma is most commonly employed in younger, more stable, female patients suffering from a blunt mechanism and at a pediatric trauma center, is associated with similar or better outcomes as laparotomy in appropriately selected patients, and has increased in utilization over time.
Acknowledgements:
The authors would like to acknowledge the support of Monroe Carell, Jr. Children’s Hospital’s Surgical Outcomes Center for Kids.
Funding: This work was supported by CTSA award No. UL1 TR002243 from the National Center for Advancing Translational Sciences. Its contents are solely the responsibility of the authors and do not necessarily represent official views of the National Center for Advancing Translational Sciences or the National Institute of Health
Abbreviations
- NTDB
National Trauma Data Bank
- ED
emergency department
- ISS
injury severity score
- MOI
mechanism of injury
- GCS
Glasgow Coma Score
- OR
odds ratio
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
Meeting Presentations:
American College of Surgeons Clinical Congress. Boston, MA. October 2018.
American Academy of Pediatrics, Section on Surgery. Orlando, FL. November 2018.
References:
- 1.Lynch T, Kilgar J, Al Shibli A. Pediatric Abdominal Trauma. Current pediatric reviews. 2018;14(1):59–63 [DOI] [PubMed] [Google Scholar]
- 2.Sharp NE, Holcomb GW 3rd., The role of minimally invasive surgery in pediatric trauma: a collective review. Pediatr Surg Int. 2013. October;29(10):1013–8. [DOI] [PubMed] [Google Scholar]
- 3.Tharakan SJ, Kim AG, Collins JL, Nance ML, Blinman TA. Laparoscopy in Pediatric Abdominal Trauma: A 13-Year Experience. Eur J Pediatr Surg. 2016. October;26(5):443–8. [DOI] [PubMed] [Google Scholar]
- 4.Ross SE, Dragon GM, O’Malley KF, Rehm CG. Morbidity of negative coeliotomy in trauma. Injury. 1995. July;26(6):393–4. [DOI] [PubMed] [Google Scholar]
- 5.Renz BM, Feliciano DV. Unnecessary laparotomies for trauma: a prospective study of morbidity. J Trauma. 1995. March;38(3):350–6. [DOI] [PubMed] [Google Scholar]
- 6.Taner AS, Topgul K, Kucukel F, Demir A, Sari S. Diagnostic laparoscopy decreases the rate of unnecessary laparotomies and reduces hospital costs in trauma patients. J Laparoendosc Adv Surg Tech A. 2001. August;11(4):207–11. [DOI] [PubMed] [Google Scholar]
- 7.Streck CJ, Lobe TE, Pietsch JB, Lovvorn HN, 3rd. Laparoscopic repair of traumatic bowel injury in children. J Pediatr Surg. 2006. November;41(11):1864–9. [DOI] [PubMed] [Google Scholar]
- 8.Lin HF, Chen YD, Chen SC. Value of diagnostic and therapeutic laparoscopy for patients with blunt abdominal trauma: A 10-year medical center experience. PLoS One. 2018;13(2):e0193379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Feliz A, Shultz B, McKenna C, Gaines BA. Diagnostic and therapeutic laparoscopy in pediatric abdominal trauma. J Pediatr Surg. 2006. January;41(1):72–7. [DOI] [PubMed] [Google Scholar]
- 10.Pearson EG, Clifton MS. The Role of Minimally Invasive Surgery in Pediatric Trauma. Surg Clin North Am. 2017. February;97(1):75–84. [DOI] [PubMed] [Google Scholar]
- 11.Stringel G, Xu ML, Lopez J. Minimally Invasive Surgery in Pediatric Trauma: One Institution’s 20-Year Experience. JSLS. 2016. Jan-Mar;20(1). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Gaines BA, Rutkoski JD. The role of laparoscopy in pediatric trauma. Semin Pediatr Surg. 2010. November;19(4):300–3. [DOI] [PubMed] [Google Scholar]
- 13.Marwan A, Harmon CM, Georgeson KE, Smith GF, Muensterer OJ. Use of laparoscopy in the management of pediatric abdominal trauma. J Trauma. 2010. October;69(4):761–4. [DOI] [PubMed] [Google Scholar]
- 14.Alemayehu H, Clifton M, Santore M, et al. Minimally invasive surgery for pediatric trauma-a multicenter review. J Laparoendosc Adv Surg Tech A. 2015. March;25(3):243–7. [DOI] [PubMed] [Google Scholar]
- 15.American College of Surgeons Committee on Trauma. National Trauma Data Bank. 2010 – 2015 ed: American College of Surgeons. [Google Scholar]
- 16.Wedgewood J, Doyle E. Anaesthesia and laparoscopic surgery in children. Paediatr Anaesth. 2001. July;11(4):391–9. [DOI] [PubMed] [Google Scholar]
- 17.Fitzgerald SD, Andrus CH, Baudendistel LJ, Dahms TE, Kaminski DL. Hypercarbia during carbon dioxide pneumoperitoneum. American journal of surgery. 1992. January;163(1):186–90. [DOI] [PubMed] [Google Scholar]
- 18.Chang DT, Kirsch AJ, Sawczuk IS. Oliguria during laparoscopic surgery. J Endourol. 1994. October;8(5):349–52. [DOI] [PubMed] [Google Scholar]


