Abstract
Psychotic disorders have varied clinical presentations, diagnostic stability is poor, and other mental disorders often co-occur with the conditions. To improve the clinical and pathophysiological utility of classification systems for psychosis, it is necessary to consider how symptoms may reflect dimensions of psychopathology that extend beyond the boundaries of traditional diagnostic classifications. We examined personality deviation as a means for explaining symptom variation across individuals with serious mental illness. Participants (N=312) with psychosis, first-degree biological relatives, and healthy controls underwent comprehensive clinical evaluations that included symptom ratings and Diagnostic Statistical Manual (DSM) consensus diagnoses. They completed the Personality Inventory for DSM-5 (PID-5), which provides multidimensional assessment of personality disturbances and characterizes psychosis-relevant phenomena, and the Schizotypal Personality Questionnaire (SPQ), a widely accepted measure of schizotypal traits. PID-5 was comparable to SPQ in differentiating between participants with and without psychosis. Greater psychotic symptomatology and higher scores on the SPQ Cognitive-Perceptual dimension were associated with higher scores on PID-5 Psychoticism. Facet-level traits showed diverse associations with existing clinical syndromes, suggesting they have utility for quantifying separable symptom dimensions that cut across existing disorders. Yet, the patient groups were similar across four of the five PID-5 personality trait domains indicating shared patterns of personality expression that challenge existing categorical delineations.
Keywords: psychosis, personality, HiTOP, PID-5, psychopathology, assessment
Dimensional models of psychopathology are becoming more prevalent in mental health research, in part due to the need to better explain symptoms that transgress traditional diagnostic categories. Psychotic psychopathology, for instance, may be better articulated by dimensional models that provide a quantitative framework for the diversity of syndromes within the psychosis spectrum as well as subtle psychosis-like experiences in the general population. Perhaps the most influential dimensional model is the recent Hierarchical Taxonomy of Psychopathology (HiTOP), which uses empirically-derived trait dimensions to parse symptom heterogeneity within existing disorders and clinical phenomena that cut across diagnostic boundaries. Dimensional and trait-based appraisal of psychotic psychopathology has potential to enhance the clinical utility of assessments by quantifying severity in specific domains and offering more personalized characterizations than categorical diagnoses. Moreover, trait dimensions may better capture the gradation of risk for psychosis that is apparent across healthy, at risk, and clinical samples. In the present study we assess personality and symptomatology in persons with psychotic clinical disorders and persons with heightened genetic liability for the disorders, to test the extent to which HiTOP can explain variation in psychotic psychopathology and be used to capture risk for severe mental illness (1,2).
Serious Mental Illness (SMI) within a Dimensional Framework
Chronic psychotic symptoms are typically associated schizophrenia spectrum disorders (commonly, schizophrenia and schizoaffective disorder), and bipolar disorder. Taken together, these diagnoses contain four broad domains of symptoms: positive symptoms (“psychosis” i.e., hallucinations, delusions), negative symptoms (i.e., decreased motivation, poverty of speech, reduced emotional expression), disorganized speech or behavior, and mood episodes (i.e. mania, hypomania, depression, or mixed). Positive symptoms are not obligatory within bipolar I disorder criteria, but one study estimates that half of people with the diagnosis experience psychosis (3) and the three factor solution of symptoms that is empirically supported in schizophrenia (4) has also been replicated in bipolar disorder (5). In addition, many individuals’ diagnoses shift within bipolar and schizophrenia spectrum disorders, particularly persons with short-duration expression of symptoms (e.g., Schizophreniform) or nonspecific disorders (e.g., Psychosis NOS; Addington, Chaves, & Addington, 2006; Salvatore et al., 2009). Thus, over a lifetime, individuals with different diagnoses may have experienced highly similar symptoms. The overlap and instability of psychotic disorders suggests that symptoms shared across diagnoses may reflect common underlying features, such as personality diatheses.
Evidence of a continuum reflecting a broad range of psychotic experiences contravenes conventional diagnostic classifications of disorders (7). Many subclinical features of severe mental illness, including psychotic-like experiences, occur in the general population, making psychiatrically unaffected persons an informative group in studies of personality. Psychotic-like experiences have been observed in the general population at substantially higher rates than the prevalence of severe mental illnesses such as schizophrenia spectrum disorders and bipolar affective disorder (8,9). Those who report psychotic-like phenomena are more likely to develop a psychotic disorder, but the majority do not (10). Considering the severity and type of clinical symptomatology within the psychosis spectrum and how it relates to dimensions of personality will help determine how clinical and subclinical psychosis conforms to HiTOP structure. A HiTOP conceptualization of psychotic psychopathology may also be a means of characterizing genetic liability for severe mental illness, as well as normative variation in psychotic-like phenomena.
HiTOP Model: Implications for SMI
HiTOP is a dimensional framework that has been introduced as an alternative to the Diagnostic and Statistical Manual of Mental Disorders, Fifth edition (DSM-5; 11) for classifying psychopathology (12). It is a dimensional and data-driven structure, thus reflecting the natural occurrence of psychopathology. Importantly, HiTOP addresses the issues of comorbidity and heterogeneity. The model presents higher-order dimensions of symptoms and personality. Specified symptoms form components that are subordinate to syndromes, subfactors and spectra, respectively. The personality traits align as more extreme expressions of the Five-Factor Model of normative personality (FFM; 12). The current study aims to demonstrate the close link between personality and psychosis using measures that fit within the HiTOP model.
Scales that have been specifically developed to assess extreme ranges of personality have been sensitive to experiences of persons with psychotic disorders. The Schizotypal Personality Questionnaire (SPQ; 13) measures trait-level propensity toward schizotypal characteristics. It has proven an effective tool to quantify traits common to psychotic disorders, encapsulated by Cognitive-Perceptual, Social-Interpersonal, and Disorganization dimensions. The three factors are elevated in first-degree relatives of persons with schizophrenia, and differentiate between schizophrenia spectrum disorders, bipolar disorder and unipolar depression (14,15). Importantly, the SPQ scales largely fit in the FFM via an expanded conceptualization of the fifth trait, Openness. Extending Openness to include unusual behaviors, speech, perceptions and beliefs better represents positive symptoms and disorganization within the psychotic spectrum (16,17). To comprehensively measure personality deviation in the psychotic spectrum, we require a tool that combines the specificity of the SPQ with the broad perspective of the FFM.
In the current study, we explore maladaptive expressions of all five personality traits in those with severe mental illness and family members using the Personality Inventory for DSM-5 (PID-5). The PID-5 was developed as a clinical tool to assess a broad range of maladaptive personality traits, including expression that does not meet formal diagnostic criteria for a personality disorder. It aligns with clinically observed personality expression articulated in “Section 3: Emerging Measures and Models” of the DSM-5 (18). PID-5 is reliable with good convergent and discriminant validity in healthy (18–20), clinical (21,22) and cross-cultural (19,23,24) samples. The PID-5 captures five broad trait domain factors that show continuity with the FFM (25–28): Negative Affect (FFM analogue: Neuroticism), Antagonism (FFM analogue: Agreeableness), Disinhibition (FFM analogue: Conscientiousness), Detachment (FFM analogue: Extraversion) and Psychoticism (FFM analogue: Openness)1.
An additional benefit of the PID-5 is that it forms a hierarchical structure in which each of the five trait domains is superordinate to five trait facets that illuminate fine-grained features. Phenotypes common across psychotic illnesses are likely to be observed at a higher-order domain level and may tap vulnerability for psychotic psychopathology (29). Examining a lower level of the personality, such as the 25 facets, may afford better differentiation of clinical phenomena (17,28,30). A predominant focus on domain-level effects may be why several studies have shown limited sensitivity to different symptom components and differentiation of psychiatric patients and relatives (16,31). For instance, the paradoxical association between the Openness and Intellect aspects is a compelling demonstration of the importance of subordinate hierarchical levels (32). The present work considers the PID-5 at domain and facet levels in an effort to demonstrate their utility. We expect that the domain level will highlight broad dimensions that are shared across psychosis, whereas narrower facets will differentiate syndromes and familial risk.
Clinical populations, including mood, anxiety, posttraumatic stress disorder, addictions disorders, and personality disorders, have been widely characterized by the PID-5 (e.g., 23,33–36). Applications within psychotic populations have been more limited, likely due to difficulties in recruiting participants with bipolar or schizophrenia spectrum disorders based on comparatively low base rates. Most studies using the PID-5 have examined the structure of psychopathology in Cluster A (i.e., schizoid, schizotypal and paranoid) personality disorders or psychotic disorders as a broad group (37–39). These approaches strongly support the inclusion of a fifth factor in measures of maladaptive personality. They are a natural point from which to examine patterns of personality evident in persons experiencing psychosis. One recent study found that persons with a psychotic condition had higher PID-5 Psychoticism, lower Detachment, Negative Affect, and Disinhibition, and equivalent Antagonism as compared to an affected psychiatric control group, suggesting PID-5 is sensitive in differentiating psychosis from other forms of psychopathology (40).
The current study is a natural extension of this work, in which we provide a more detailed clinical characterization and explicitly contrast diagnoses within the psychotic spectrum. An inconsistency to address is that, when compared to controls, persons with psychosis have generally shown higher Neuroticism, the normative FFM equivalent of Negative Affect (41). Including controls and relatives alongside psychiatric groups will allow us to extend Ohi and colleagues’ findings to the maladaptive range of personality. The clarity and detail with which PID-5 examines personality related to psychotic phenomena lends the current study particular strength in examining personality and symptom patterns in schizophrenia, bipolar disorder, and relatives.
Psychosis Vulnerability within a Dimensional Framework
The inclusion of relatives and persons with a spectrum of severe psychopathology is a unique aspect of the current work. Dimensions of personality appear to tap neurobiological and genetic bases for individuals differences related to psychopathology in addition to describing patterns of behavior, emotion, and thinking (42,43). Genetic liability is partly shared across schizophrenia and bipolar disorder (44,45). First-degree relatives are at increased risk for psychotic illness, meaning that schizophrenia confers familial risk for bipolar disorder and vice versa (46). Relatives of persons with psychotic disorders demonstrate attenuated versions of the patterns of probands across symptom, cognitive, and electrophysiology domains (29,47–52). Subclinical psychotic experiences are elevated in relatives, even those who never develop a psychiatric disorder (53–55). Given these patterns, it follows that trait elevations evident in individuals with psychosis and first-degree biological relatives may reflect a common etiology. Indeed, there is already some evidence suggesting that maladaptive trait expression reflects variation in shared genetic risk across psychotic disorders (15,50). An important next step is to demonstrate how genetic liability for severe mental illness relates to personality at the domain and facet level. We carry out the present analysis to provide insight into the etiology that may underlie maladaptive personality traits and, to our knowledge, be the first to demonstrate such a pattern using the PID-5.
In the present study, we provide a comprehensive overview of the connection between personality and psychopathology across patients with severe mental illness, first-degree biological relatives, and psychiatrically unaffected individuals using the PID-5 and SPQ. We investigate how well the measures characterize personality domains and facets across the spectrum of clinical and subclinical symptoms in schizophrenia spectrum disorders, bipolar I disorder and persons with familial liability for psychosis. Diagnostic groups are used as a heuristic to demonstrate that traits are elevated across people who have what were traditionally thought of as distinct disorders and among those who have no formal diagnosis but who nonetheless share genetic risk. We hypothesize that the PID-5 will perform as well as SPQ in differentiating those with psychiatric disorders from controls. The trait domain level is expected to highlight the shared vulnerability across the psychotic spectrum. Negative Affect and Disinhibition are expected to be elevated in schizophrenia and bipolar disorder, consistent with FFM studies linking elevated Neuroticism and Extraversion to general risk for psychopathology; Negative Affect is expected to be associated with symptoms of depression and anxiety. Additionally, the Psychoticism factor is expected to be elevated in both schizophrenia and bipolar clinical groups, and strongly correlated with positive symptoms. We expect the facets will parse selective symptom components observed more frequently in schizophrenia (i.e., Anhedonia and Suspiciousness) or bipolar disorder (i.e., Emotionally Liability). At the facet level we expect similarities to meld subclinical and clinical trait levels, with elevations among relatives following the respective diagnostic group (i.e., relatives of bipolar patients showing a muted version of the elevations in bipolar patients).
Methods
Participants
Persons with bipolar affective or schizophrenia spectrum disorders, first-degree biological relatives, and healthy controls were recruited as participants. Stable psychiatric outpatients were recruited from the Minneapolis Veterans Affairs Health Care System (VAHCS) and community mental health centers. A family pedigree was completed by relatives and patients; the pedigree was also used as a recruitment tool to identify relatives for participation. All potential participants were screened via telephone; those that met study criteria were invited to participate in person. Informed consent was completed in accordance with the Declaration of Helsinki and approved by the Minneapolis VAHCS and University of Minnesota Institutional Review Boards.
All participants were native English speakers, 18 to 60 years old, with normal or corrected hearing and vision, and intelligence quotient greater than 70. Patients and controls were excluded for substance abuse or dependence within the past six months, electroconvulsive therapy (ECT), epilepsy, diagnosed seizure disorder, history of stroke, neurological condition, other uncontrolled medical conditions likely to affect brain functioning (e.g., untreated thyroid condition), and head injury resulting in fractured skull or loss-of-consciousness for more than 30 minutes. Controls had no history of primary psychotic disorder, hypomania, anti-psychotic medication use, current or past depressive episodes, ADHD or learning disability, or family history of bipolar or psychotic disorder.
Participants underwent a structured clinical interview (SCID; 56) for Diagnostic and Statistical Manual of Mental Disorders, Fourth edition, Text Revision (DSM-IV-TR; 57). Relatives and controls additionally completed the Structured Interview for Schizotypy to assess for Cluster A personality disorders and traits (58). The clinical interviewer rated current symptomatology of all participants using the 24-item version of the Brief Psychiatric Rating Scale (BPRS; 59). Participants with schizophrenia or bipolar diagnoses were additionally rated on the Scale for the Assessment of Negative Symptoms (SANS; 60) and the Scale for the Assessment of Positive Symptoms (SAPS; 61). Final diagnoses were determined by two clinical staff (doctoral-level psychologists or trained advanced graduate students) who reviewed all clinical interview materials for each participant and reached a unanimous consensus for all diagnoses (62); thus, while no diagnostic reliability was not quantified, agreement was maximized within the clinical team. An estimate of full-scale intelligence quotient was measured using the Block Design and Vocabulary subtests (63) of the Wechsler Adult Intelligence Scale, Third Edition (WAIS-III; 64).
Three hundred twelve participants met inclusion criteria: 86 persons with schizophrenia spectrum disorders (SZ), 57 persons with bipolar affective disorders (BP), 77 relatives of schizophrenia probands (R-SZ), 24 relatives of bipolar probands (R-BP), and 68 healthy controls (HC). Bipolar spectrum diagnoses included Bipolar I Disorder (n=56; 17 with psychotic features) and Bipolar Disorder NOS (n=1, with psychotic features). Schizophrenia spectrum diagnoses included Schizophrenia (n=70), and Schizoaffective disorder (n=15), Delusional disorder (n=1), and Psychosis NOS (n=1). Forty-eight R-SZ had no history of any psychiatric diagnosis, while 14 R-BP were unaffected. Cluster A personality disorders or traits were present in 14 R-SZ, and 3 R-BP.
Questionnaire Procedures
Participants completed the Personality Inventory for DSM-5 (PID-5; 11) as part of a larger research protocol. The PID-5 contains 220 items. Participants responded on a scale of 0 (Very False or Often False) to 3 (Very True or Often True). Partial raw scores were prorated for missing data. Two subjects missed 10 items (4.5%); seven participants missed 1 or 2 items (<1%). The items form five personality trait domains (Negative Affect, Detachment, Antagonism, Disinhibition, and Psychoticism) superordinate to 25 personality trait facets. The trait domains were calculated so that every facet contributed to a domain estimate, in accordance with empirically derived factors (65).
Participants also completed the Schizotypal Personality Questionnaire (SPQ; 13). The SPQ contains 74 items for which participants responded True or False. The questionnaire forms a three factor structure: Cognitive-Perceptual, Social-Interpersonal, and Disorganization (15,66). Factors were calculated as sum scores, prorated for any missing items. A single participant was excluded from SPQ analysis due to 19 missing items (26%). Another 31 participants were excluded because all items were scored 0. Thirteen participants who completed the PID-5 questionnaire failed to complete the SPQ. Thus, the SPQ analysis contains 267 participants.
Statistical Analysis
All statistical tests were carried out in SPSS (Version 20). First, five mixed multilevel models tested between-group differences in the PID-5 trait domains. Each domain was modeled as a separate dependent variable, with Šidák corrections for multiple comparisons: α<.01 (67). Group was the fixed independent variable; age and gender were also entered as predictors. Family membership was modeled as a random effect using intraclass correlations (ICC) in all analyses. Second, mixed multilevel models quantified the extent to which the five BPRS symptom domains, entered as simultaneously, predicted each PID-5 domains. Covariates (age, gender), random effects (family), and p-statistic threshold (α<.01) were equivalent in design to the between-group PID-5 trait domain analyses. Third, mixed level models tested between-group effects on PID-5 facets, with age and gender as covariates (Šidák correction: α<.002). ICC calculations were not made at the facet level given the null contribution in trait domain analysis.
Last, PID-5 and SPQ schizotypy scales were entered into separate stepwise logistic regressions predicting psychotic diagnostic status (Bipolar I Disorder with psychotic features or Schizophrenia spectrum disorders). In the PID-5 model, Psychoticism facets were entered into the first step; the remaining schizotypy facets (Restricted Affectivity, Withdrawal, and Suspiciousness) were added in step two. For SPQ, the Cognitive-Perceptual factor was entered in the first step, followed by Social-Interpersonal and Disorganized factors in step two. Models were compared using Cox & Snell R2 estimates and classification accuracy. Between groups effects were also measured for SPQ factors using a mixed multilevel model with age and gender as covariates (Šidák correction: α<.017).
Results
Initially, we compared basic demographic and clinical characteristics of participants (see Table 1). Current symptoms, as assessed by total score on the BPRS, were lowest in R-SZ and CON, intermediate in R-BP and BP, and highest in SZ (F(4,307)=41.76, p<.001). SANS and SAPS, which were collected only for persons with schizophrenia or bipolar affective disorders, revealed higher positive (F(139)=25.49, p<.001) and negative symptoms (F(139)=8.76, p<.01) amongst SZ. Age was comparable across all five participant groups (F(4,307)=1.94, p=.10). The ratio of male versus female participants differed across the groups (χ2 =21.63, p<.05) due to the larger number of males amongst SZ and BP, and fewer females amongst R-SZ.
Table 1.
Clinical and Demographic Characteristic
| CON | R-BP | R-SZ | BP | SZ | Statistic | |
|---|---|---|---|---|---|---|
| N (% Male) | 68 (57%) | 24 (58%) | 77 (38%) | 57 (72%) | 86 (69%) | χ2 =21.63, p<.05 |
| Mean Age (SD) | 44.66 (11.32) | 42.92 (12.44) | 47.78 (13.57) | 48.47 (11.05) | 44.83 (10.22) | F4,307=1.94, p=.10 |
| BPRS - Mean (SD) | ||||||
| Sum Total | 27.89 (4.47)bcde | 34.56 (8.92)a | 31.96 (7.32)a | 36.03 (7.65)ac | 44.85 (11.92)abcd | F4,307=41.76, p<.001 |
| Positive | 1.02 (0.09) | 1.20 (0.50) | 1.18 (0.49) | 1.20 (0.31) | 2.38 (1.27) | - |
| Negative | 1.07 (0.21) | 1.33 (0.47) | 1.15 (0.34) | 1.28 (0.42) | 1.58 (0.78) | - |
| Disorganization | 1.24 (0.33) | 1.57 (0.59) | 1.53 (0.55) | 1.71 (0.57) | 2.00 (0.71) | |
| Depression/Anxiety | 1.39 (0.55) | 1.97 (0.79) | 1.86 (0.91) | 2.21 (1.17) | 2.27 (1.09) | - |
| Activation/Mania | 1.17 (0.38) | 1.38 (0.68) | 1.19 (0.41) | 1.45 (0.76) | 1.34 (0.54) | - |
|
SAPS/SANS –
Mean (SD) |
||||||
| Positive Sx | - | - | - | 0.81 (1.71) | 3.29 (3.37) | F139=25.49, p<.001 |
| Negative Sx | - | - | - | 2.23 (2.16) | 3.61 (2.97) | F139=8.76, p<.01 |
= differed from CON;
= differed from R-BP;
= differed from R-SCZ;
= differed from BP;
=differed from SCZ
Note. Participants consisted of individuals with a schizophrenia spectrum disorder (SZ) and their first-degree relatives (R-SZ), individuals with bipolar affective disorder (BP) and their first-degree relatives (R-BP), and healthy controls (CON). All participants were rated on current symptoms by the clinical interviewer using the Brief Psychiatric Rating Scale (BPRS); BPRS Sum Total scores range 24–168, and factor scores range from 1 (Not Present) to 7 (Extremely Severe). SZ and BP were also rated on the Scale of Negative Symptoms (SANS) and Scale of Positive Symptoms (SAPS), which are scored on a range of 0 (None) to 4 (Marked). Across both clinical measures, the groups demonstrated the expected spectrum of symptoms: CON showed minimal current symptoms, relative groups had slightly higher symptom levels, and patients had the highest levels within the sample. Positive symptoms consistently differentiated SZ from other participants; however, the two psychiatric groups were comparably elevated in mood symptoms. Values are listed as means with standard deviations in parentheses, except where noted for gender proportions.
PID-5 Domains
In a broad sense, the domain level results were as expected: SZ and BP were elevated and CON at lower levels of maladaptive personality domains on average, while relative groups fell in between (see Figure 1). All five domains had significant effects of group after corrections for age and gender [Negative Affect: F(4,307)=20.67, p<.01; Detachment: F(4,307)=28.83, p<.01; Antagonism: F(4, 307)=4.09, p<.01; Disinhibition: F(4,307)=15.30, p<.01; Psychoticism: F(4,307)=42.85, p<.01]. Psychoticism set SZ apart from all other participants. The two groups experiencing psychotic disorders, BP and SZ, had similarly elevated Negative Affect, Detachment and Disinhibition. Both psychiatric groups were more elevated than their respective relatives in Negative Affect, Detachment, and Disinhibition. Thus, the relative groups diverged from the patient groups more in some domains than others. The relatives never significantly differed from one another at the domain level.
Figure 1.
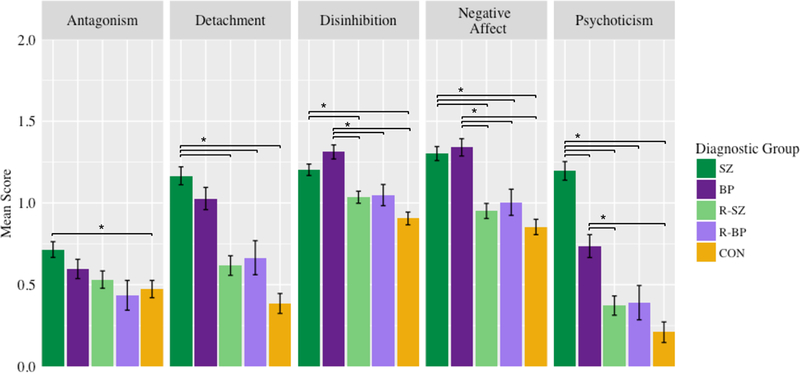
Group differences in PID-5 domains. from mixed multilevel analyses of the five PID-5 personality trait domains. PID-5 mean scores are reported on a scale from 0 (Very False or Often False) to 3 (Very True or Often True). Significant post-hoc group comparisons are notated by brackets. Error bars denote standard errors for all domains.
For the most part, age and gender did not contribute significantly to the personality domains. Younger age was associated with higher Disinhibition (F(304)=13.17, p<0.01); given the comparable age across all groups, the effects of age should not affect the interpretation of the current findings. Consistent with recent findings (40), Antagonism was comparable across most the groups. Females reported lower levels of Antagonism than males (F(197)=7.40, p<0.01) suggesting the maladaptive range of Agreeableness is more informative to gender differences in presentation than to diagnosis or familial risk within the psychotic spectrum. Family membership, as assessed by ICC, contributed minimally to the findings across all domains, demonstrating the effects were not driven by family clusters.
Five mixed models tested the direct relationship between the BPRS symptom factors and each PID-5 domain after controlling for family cluster, age, and gender (see Table 2). Positive symptoms predicted the largest increases in Psychoticism. Depression/Anxiety symptoms were most notably associated with higher Detachment and Negative Affect. Disorganization predicted smaller increases in Detachment and Negative Affect. Neither Negative symptoms nor Mania symptoms were associated with any of the PID-5 domains. The results provide evidence that PID-5 Psychoticism is capturing clinically relevant aspects of severe mental illness within the intended domains.
Table 2.
Association Between Personality and Symptoms.
| Negative Affect | Detachment | Antagonism | Disinhibition | Psychoticism | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| β (SE) | 95% CI | β (SE) | 95% CI | β (SE) | 95% CI | β (SE) | 95% CI | β (SE) | 95% CI | |
| Age | 0.01 (0.02) | [−0.03, 0.05] | 0.01 (0.03) | [−0.04, 0.06] | −0.01 (0.02) | [−0.06, 0.04] | −0.05 (0.02) | [−0.08, −0.01] | −0.03 (0.03) | [−0.08, 0.02] |
| Gender | 0.02 (0.04) | [−0.07, 0.11] | −0.02 (0.05) | [−0.13, 0.08] | −0.23 (0.05) | [−0.33, −0.13] | −0.06 (0.04) | [−0.13, 0.01] | −0.12 (0.06) | [−0.23, −0.01] |
| BPRS | ||||||||||
| Positive Sx | 0.06 (0.02) | [0.01, 0.11] | 0.11 (0.03) | [0.05, 0.17] | 0.10 (0.03) | [0.04, 0.16] | 0.02 (0.02) | [−0.02, 0.07] | 0.31 (0.03) | [0.25, 0.38] |
| Negative Sx | 0.00 (0.02) | [−0.05, 0.04] | 0.06 (0.03) | [0.01, 0.11] | −0.02 (0.03) | [−0.07, 0.03] | 0.05 (0.02) | [0.01, 0.09] | 0.05 (0.03) | [−0.01, 0.11] |
| Disorganization | 0.08 (0.03) | [0.03, 0.13] | 0.12 (0.03) | [0.06, 0.19] | 0.04 (0.03) | [−0.02, 0.10] | 0.05 (0.02) | [0.00, 0.09] | 0.05 (0.03) | [−0.02, 0.11] |
| Depression/ Anxiety | 0.16 (0.03) | [0.11, 0.21] | 0.22 (0.03) | [0.16, 0.27] | 0.04 (0.03) | [−0.02, 0.09] | 0.08 (0.02) | [0.03, 0.12] | 0.13 (0.03) | [0.07, 0.20] |
| Mania | −0.02 (0.02) | [−0.07, 0.02] | −0.06 (0.03) | [−0.11, 0.00] | 0.01 (0.02) | [−0.04, 0.06] | 0.04 (0.02) | [0.00, 0.08] | −0.01 (0.03) | [−0.06, 0.05] |
Note. A series of mixed effects models considered the relationship between current symptoms, as measured by the Brief Psychiatric Rating Scale (BPRS), and maladaptive trait domains, as measured by the Personality Inventory for DSM-5 (PID-5). One of the most pronounced associations was between PID-5 Psychoticism and positive symptoms (i.e., hallucinations and delusions). Greater BPRS Depression/Anxiety symptoms predicted the largest changes in two PID-5 domains, Negative Affect and Detachment. Effect of family membership, included as a random effect in all models, was not significant for any of the PID-5 domain traits. Significant effects (p < .01) are noted in bold font.
PID-5 Facets
The third set of analyses investigated the 25 facets subordinate to the PID-5 trait domains. Twenty facets had statistically significant effects of group, which were explored by post-hoc comparisons (see Figure 2). Consistent with our hypothesis, Psychoticism differentiated BP and SZ patient groups at the trait domain and facet levels despite the overlap in presenting clinical symptomatology. SZ had exceptionally high Perceptual Dysregulation and Unusual Beliefs & Experiences as compared to all other groups. We also hypothesized that SZ would have particularly high Anhedonia and Suspiciousness, facets falling under the Detachment domain. Indeed, Suspiciousness was the only facet outside of the Psychoticism domain for which SZ had higher levels than all other groups.
Figure 2.
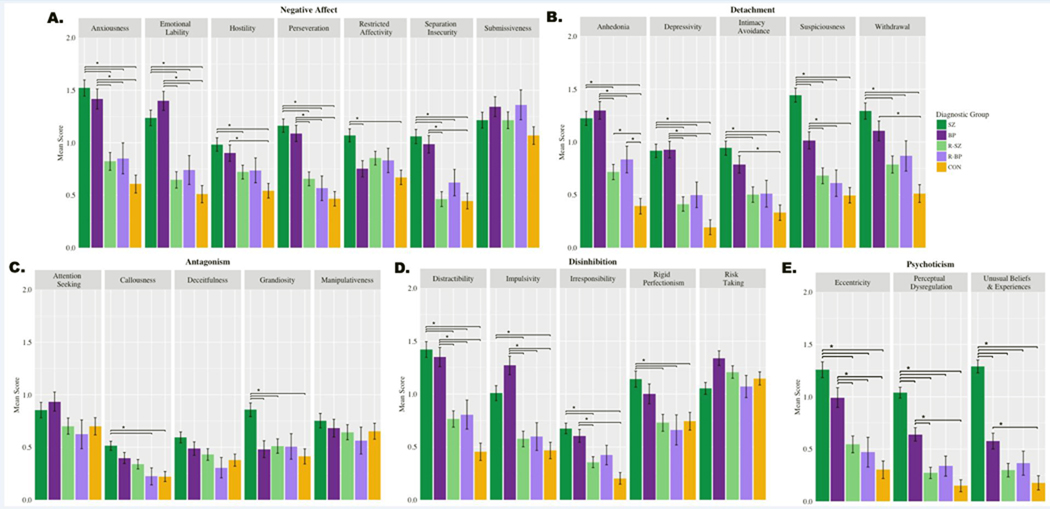
Group differences in PID-5 trait facets. Mixed multilevel models test between-group differences at the subordinate facet level of each of the five trait domains: (A) Negative Affect; (B) Detachment; (C) Antagonism; (D) Disinhibition; and (E) Psychoticism. PID-5 mean scores are reported on a scale from 0 (Very False or Often False) to 3 (Very True or Often True). Significant post-hoc group comparisons are notated by brackets. Facets without brackets did not reach significance in the mixed multilevel model analysis. Error bars denote standard errors.
SZ and BP had common elevations across the majority (16) of facets, reinforcing the relevance of a broad range of clinical and personality features to psychosis, including those that lie outside of positive symptoms. Both psychiatric groups differed from R-SZ, R-BP and CON in: four facets of Negative Affect (Emotional Liability, Anxiousness, Perseveration, Separation Insecurity); three facets of Detachment (Anhedonia, Depressivity, Suspiciousness); three facets of Disinhibition (Distractibility, Irresponsibility, Impulsivity); and two facets of Psychoticism (Perceptual Dysregulation, Unusual Beliefs & Experiences). Whereas SZ differed controls in all twenty facets showing group differences, BP were comparable to controls in four facets: Restricted Affectivity (Negative Affect), Rigid Perfectionism (Disinhibition), and Callousness and Grandiosity (Antagonism). R-SZ and R-BP were comparable to CON on all facets except Anhedonia. As observed at the domain level, the two relative groups did not differ from one another. Gender effects, with male participants’ scores exceeding women’s, were observed in all Antagonism facets, Risk Taking, Irresponsibility, and Restricted Affectivity. Effects of age were significant for Risk Taking, Irresponsibility, and Callousness.
SPQ
Lastly, we compared the ability of PID-5 schizotypy scales and SPQ to differentiate persons with clinically significant psychosis from those without a psychotic disorder (see Table 3). At the first step of each model, PID-5 Psychoticism facets accounted for slightly more variance (R2=.28) than the SPQ Cognitive-Perceptual factor (R2=.27). The full models were comparable (R2=.30), with SPQ accurately predicting the diagnostic status of 78.5% of participants and PID-5 classifying 77.5%.
Table 3.
Diagnostic Classification by Personality Measures: Comparing PID-5 and SPQ.
| b(SE) | p-value | OR | 95% CI | R2Δ | ||
|---|---|---|---|---|---|---|
| Model 1: PID-5 Schizotypy | ||||||
| Step 1 | .28 | |||||
| Eccentricity | −.58 | (.32) | .07 | .56 | [.30, 1.05] | |
| Perceptual Dysregulation | .42 | (.59) | .48 | 1.52 | [.48, 4.82] | |
| Unusual Beliefs | 1.72 | (.40) | < .001 | 5.56 | [2.53, 12.21] | |
| Step 2 | .02 | |||||
| Restricted Affectivity (lack) | .29 | (.32) | .36 | .75 | [.72, 2.51] | |
| Withdrawal | .30 | (.30) | .32 | 1.35 | [.75, 2.44] | |
| Suspiciousness | .65 | (.33) | .049 | 1.92 | [1.00, 3.67] | |
| Psuedo R2: | .30 | |||||
| Correct Classification %: | 77.5% | |||||
| Model 2: SPQ | ||||||
| Step 1 | .27 | |||||
| Cognitive-Perceptual | .21 | (.03) | < .001 | 1.24 | [1.16, 1.32] | |
| Step 2 | .03 | |||||
| Social-Interpersonal | .06 | (.03) | .02 | 1.07 | [1.01, 1.12] | |
| Disorganized | −0.17 | (.05) | .001 | .85 | [.76, .94] | |
| Psuedo R2: | .30 | |||||
| Correct Classification %: | 78.5% | |||||
Note. N = 298. Bolded effects are significant at p < .05. Abbreviations: PID-5 = Personality Inventory for DSM-5, SPQ = Schizotypal Personality Questionnaire. PID-5 Step 1 includes all facets within the Psychoticism trait domain. Step 2 includes Restricted Affectivity from the Negative Affect domain, and Withdrawal and Suspiciousness from the Detachment domain.
The group differences in SPQ factors was highly similar to that of the PID-5 Psychoticism domain. Mean scores were highest in SZ, followed by BP, R-BP, R-SZ and CON (see Figure 3). The Cognitive-Perceptual Factor appeared particularly sensitive to the SZ group. Social-Interpersonal elevations were largely shared by the two patient groups. Additionally, CON were significantly lower than all other groups on this factor. PID-5 Psychoticism correlation most strongly with SPQ Cognitive Perceptual (see Figure 3B; r = 0.80) and Disorganized (r = 0.67) factors. The Interpersonal Factor had the strongest relationship with PID-5 Detachment (r=0.75; correlation with Psychoticism r =g243 .48). Like the SPQ, PID-5 appears sensitive to schizotypal traits in psychiatric disorders within the psychotic spectrum, and in relatives of persons with severe mental illness.
Figure 3.
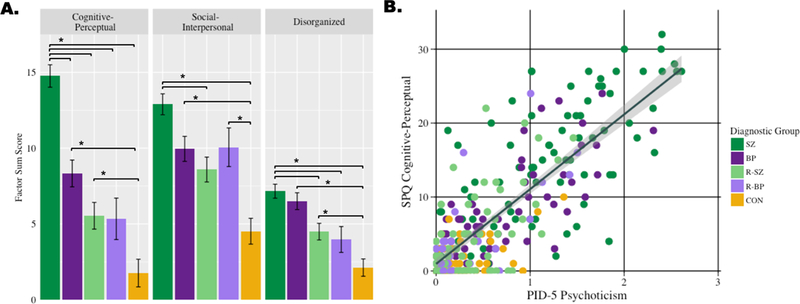
Individual and group differences in SPQ domains. Panel A: Group differences across the three factors of the Schizotypal Personality Questionnaire (SPQ). The SPQ is a well-established personality measure that has proved sensitive to both clinical and subclinical schizotypal traits. The results verify that the PID-5 sufficiently captures features of psychosis across the maladaptive level. Panel B: The SPQ Cognitive-Perceptual factor was strongly correlated with PID-5 Psychoticism, further supporting both measures as important to psychosis. SPQ factors are reported as sum scores that range from 0 to 33.
Discussion
The aim of this work was to demonstrate the utility of instruments such as the PID-5 to broadly assess traits in severe psychopathology, and the relationship to symptomatology. The results showcased the PID-5 as a comprehensive assessment tool that provides coverage of schizotypal dimensions, captures traits relevant to the psychotic spectrum, and quantifies the remaining four personality factors that have been well-represented in non-psychotic samples to-date. Three main methodological strengths maximized the value of the observations. First, by using an enriched sample of persons experiencing schizophrenia spectrum or bipolar disorders, we directly tested the association between symptoms and personality across diagnostic delineations. Second, we examined the full spectrum of maladaptive traits across two levels of the hierarchical structure of personality, with an instrument that offers detailed coverage of attributes associated with the core symptoms of psychosis (i.e., hallucinations, delusions, disorganization). Third, the inclusion of first-degree relatives was particularly novel within extant literature and may be helpful in identifying components of psychopathology with a common etiology.
Overwhelmingly, and in alignment with HiTOP theory, personality measures highlighted shared trait elevations across psychotic syndromes. Maladaptive ranges of personality, as indexed by PID-5 and SPQ, were most elevated in persons with schizophrenia or bipolar disorder. Psychoticism was the only domain to distinguish the psychiatric groups at the superordinate domain level. Participants with schizophrenia had elevated Psychoticism compared to all other groups. At the subordinate level, this was driven by the Perceptual Dysregulation and Unusual Beliefs & Experiences facets. We suspect that Suspiciousness follows a similar pattern because of cross-loadings on multiple personality domains including Psychoticism (29,65,68). A similar pattern was seen in the SPQ, particularly the Cognitive-Perceptual factor. In addition to illustrating group differences, PID-5 schizotypy scales and SPQ accurately classified the majority of participants based on psychotic diagnostic status. Of all PID-5 and SPQ schizotypy facets, PID-5 Unusual Beliefs and Experiences had the strongest predictive power (OR= 5.56), despite containing a mere eight items. Suspiciousness is also notable (OR= 1.92). When only considering positive schizotypy scales (i.e., PID-5 Eccentricity, Unusual Beliefs & Experiences, Perceptual Dysregulation, and SPQ Cognitive-Perceptual in Step 1 of regressions in Table 3) PID-5 performance is superior to SPQ, demonstrating the utility of PID-5 as a differential diagnosis tool.
Examining the structure of personality in scales with extensive coverage and in populations that endorse the extreme ends of the range may increase understanding of how the psychotic spectrum fits within maladaptive personality structures. The current findings can inform our understanding of the relationship between Psychoticism, in the maladaptive range of personality, and Openness, in the normative range. By including the extreme end of the domain, Psychoticism may be capturing variance that other indices omit, particularly that related to the aspect Openness-to-Experience. The high levels of Psychoticism within our sample suggest that the PID-5 highlights meaningful characteristics of severe mental illness. Furthermore, PID-5 captures the variability of individual scores across the sample. While persons with schizophrenia spectrum disorders represented the tail of the distribution on average, some endorsed low levels that overlapped with controls. Individual scores are particularly important to consider as we move toward measurement-based clinical care. Stable recovery, lack of insight, or comparing one’s self to peers with psychosis, could potentially explain the low Psychoticism scores in a portion of individuals with schizophrenia spectrum disorders.
No single study to-date has applied the PID-5 to multiple psychotic disorders and family members. The sample allowed us to consider how personality dimensions relate to both clinical presentation and shared risk. Our hypothesis with respect to personality in relatives met mixed findings. The relatives were intermediate to the patient groups and healthy controls, as we had predicted. More often than not, relatives of individuals with bipolar disorder were similar to those with bipolar disorder (16 of 25 facets) as compared to persons with schizophrenia and their relatives (6 of 25 facets). Neither the domain nor the facet level differentiated the two relative groups. As noted above, a limitation to the findings in relatives of persons with bipolar disorder may reflect general psychiatric distress more than familial liability for psychosis. Consistent with this theory, past work found that personality traits in persons at-risk for psychosis were highest in those expressing the highest current prodromal symptomatology (69). Alternatively, the similarities may reflect shared susceptibility across disorders, consistent with coaggregation of psychotic disorders within families (70).
Positive symptoms such as hallucinations and delusions do not account for the complete clinical picture of persons with psychosis, though they are central diagnostic criteria. Thus, it is not surprising that we saw personality overlap across disorders that share psychiatric features. High Negative Affect, Detachment, and Disinhibition in our psychiatric sample is consistent with high Neuroticism and low Extraversion and Conscientiousness observed in schizophrenia and a host of other psychiatric disorders (31,41). Our findings support the assumption that Negative Affect, Detachment, and Disinhibition may be general risk factors of psychopathology (31,71). As suggested by Carpenter (72), overlap between the patient groups may be due to features that are auxiliary to diagnostic criterion, such as general distress associated with having a mental illness. In the present investigation, Negative Affect and its facets all follow the pattern predicted by general distress: patients with schizophrenia and bipolar are higher than controls. The Psychoticism domain, in which we observed the greatest gap between BP and SZ, is minimally correlated with general distress (73), suggesting that the PID-5 captures variance uniquely associated with psychosis and shared characteristics.
An outstanding question within HiTOP has been the relationship between symptoms and personality. The link between the personality dimension Psychoticism and clinical Thought Disorder domain has been empirically demonstrated, as has the link between Negative Affect and Internalizing symptoms. The current analysis reproduced a clear relationship between Psychoticism and positive symptoms. This extends our between-groups analysis, showing that not only are people with primary psychotic disorders on average higher in Psychoticism, but the individual level of psychotic symptoms is tightly related to Psychoticism. Internalizing symptoms (i.e. BPRS Depression/Anxiety) significantly predicted Negative Affect scores. Surprisingly, Internalizing was associated more strongly with Detachment than Negative Affect. Quilty and colleagues found opposing relationships between personality and depression and mania symptoms. Depression was negatively associated with Extraversion, while mania was positively related to Extraversion (74). Our sample replicated the association between depression symptoms and Detachment, the maladaptive analogue of Extraversion, but not mania, which had a weak, non-significant negative correlation with Detachment. The negative symptom domains did not significantly predict any PID-5 trait domain. Neither mania nor negative symptoms has been well-characterized within the structure of psychopathology, leaving both as areas for future study. Understanding how negative symptoms fit within the taxonomy of mental illness could be especially relevant to advancing treatment for psychosis. Negative symptoms are one of the most enduring and refractory clinical components associated with psychosis, even within evidence-based practice (75).
HiTOP represents a pivotal change in theory and classification of psychopathology. However, it is largely consistent with how clinicians already understand and practice treatment, with cross-cutting symptoms as targets of evidence-based treatments (76). The symptom level provides greater reliability than diagnoses (77). Diagnostic interviews assign participants to discrete groups that may obscure the range of trait expression within each group. Presence of a psychotic disorder without a comorbid diagnosis, as required by many research protocols, is rare and does not reflect clinical presentations seen in treatment settings (78,79). Furthermore, the language of DSM (i.e., “not better explained by”) restricts how we represent shared symptom clusters and comorbidity in diagnostic assignments. Aligning clinical research and treatment with a common, empirically-established classification system will decrease the disconnect between development and application of psychiatric intervention.
We see two immediate areas in which future research of HiTOP can advance understanding of psychosis. First, our findings emphasize the importance of broadly assessing psychopathology across all five trait domains before honing in on specific facets or symptom clusters. All five domains were applicable to this specialized sample despite recruitment for participants with psychotic disorders. Yet, we have limited understanding of the relationship between Psychoticism and other traits, and the combined impact of multiple trait elevations on course of illness. Recent work has shown that Internalizing symptom domain (e.g., depression and anxiety) is more predictive of functional outcome in psychotic disorders than the Thought Disorder domain (80). Traits have been shown to interact to predict non-psychotic syndromes (81,82), and a similar process likely occurs in psychotic disorders. By broadening the focus of psychosis research, we can consider the interplay between traits. Second, further research can explore how dimensional assessments should inform treatment approaches. Select studies give promising demonstrations of the value of incorporating dimensional assessment in treatment planning. Baseline traits can be used to predict the effectiveness of treatment, or even be modified by effective treatment (81,83,84). A parallel line of work is reaching a better understanding of the reliability and meaning of individual scores. This can lead to clinically meaningful cutoffs on measures of the HiTOP model.
Conceptualizing mental illness through HiTOP is particularly important for severe mental illness given historical views of schizophrenia as intractable, permanent, and categorically different than other forms of mental illness. In fact, there are many evidence-based treatments for schizophrenia and bipolar disorder. Within the 21st century, there has been a push to understand risk factors of psychotic disorders and move toward early intervention, and even prevention. Our findings demonstrate that psychosis is not qualitatively different from other disorders, but rather overlaps on the majority of personality dimensions, which may suggest shared etiologic pathways and perhaps similar interventions to facilitate recovery. Dimensional models provide an empirically-based, quantitative framework for assessing the psychosis spectrum that can inform clinical assessment, intervention, and prevention.
Acknowledgments
This research was supported by Merit Review grants (#ICX000227A) to Dr. Scott Sponheim from the Veterans Health Administration Clinical Science Research and Development Program.
Robert F. Krueger’s efforts were supported in part by the U.S. National Institutes of Health (R01AG053217, U19AG051426) and by the Templeton Foundation. Thanks to the members of the CAB lab (http://cablab.umn.edu/) for their work in collecting the data included in this study. We also sincerely thank the research participants and their families for contributing to this research.
Footnotes
We recognize that the relationship between the normative personality factor Openness and maladaptive traits is an ongoing debate in contemporary models of personality. In particular, NEO Openness and PID-5 Psychoticism do not appear to be correlated (85,86). However, at the facet level of analysis, half the NEO-PI-R facets loaded positively on Psychoticism while the other half loaded negatively (22). DeYoung and colleagues (2012) describe this “paradoxical” relationship between the two subordinate aspects within the Openness domain. The lower-level normative facets/aspects, Openness-to-Experience and Intellect, both load positively on the Openness domain, yet the most extreme ends of Openness-to-Experience and Intellect are negatively correlated (32). Likewise, Openness-to-Experience has positively predicted Psychoticism, while Intellect has negatively predicted Psychoticism in a psychiatric sample (68). In normative and psychiatric samples, continuity between Psychoticism and the FFM appears to be strongest – yet paradoxical – at the subordinate Openness-to-Experience/Intellect level after shared variance has been extracted (22,32,68). We suspect this has been the reason for equivocal Openness findings in past studies of the psychotic spectrum, and feel that assessing the extreme ends of personality spectra at multiple levels of the hierarchy is particularly important with respect to psychotic disorders.
References
- 1.Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62(6):593–602. [DOI] [PubMed] [Google Scholar]
- 2.Salvatore P, Baldessarini RJ, Tohen M, Khalsa HK, Sanchez-Toledo JP, Zarate CA, et al. The McLean-Harvard First Episode Project: Two-year Stability of DSM-IV Diagnoses in 500 First-Episode Psychotic Disorder Patients. J Clin Psychiatry. 2009;70(4):458–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Perälä J, Suvisaari J, Saarni SI, Kuoppasalmi K, Isometsä E, Pirkola S, et al. Lifetime prevalence of psychotic and bipolar I disorders in a general population. Arch Gen Psychiatry. 2007. January 1;64(1):19–28. [DOI] [PubMed] [Google Scholar]
- 4.Peralta V, Cuesta MJ. Dimensional structure of psychotic symptoms: An item-level analysis of SAPS and SANS symptoms in psychotic disorders. Schizophr Res. 1999;38(1):13–26. [DOI] [PubMed] [Google Scholar]
- 5.Maziade M, Roy MA, Martinez M, Cliche D, Fournier J, Garneau Y, et al. Negative, psychoticism, and disorganized dimensions in patients with familial schizophrenia or bipolar disorder: continuity and discontinuity between the major psychoses. Am J Psychiatry. 1995;152(10):1458–63. [DOI] [PubMed] [Google Scholar]
- 6.Addington J, Chaves A, Addington D. Diagnostic stability over one year in first-episode psychosis. Schizophr Res. 2006;86(1–3):71–5. [DOI] [PubMed] [Google Scholar]
- 7.Eaton NR, Krueger RF, Docherty AR, Sponheim SR. Toward a model-based approach to the clinical assessment of personality psychopathology. J Pers Assess. 2014;96(3):283–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hanssen M, Bak M, Bijl R, Vollebergh W, Os J. The incidence and outcome of subclinical psychotic experiences in the general population. Br J Clin Psychol. 2005;44(2):181–91. [DOI] [PubMed] [Google Scholar]
- 9.Peters ER, Joseph SA, Garety PA. Measurement of delusional ideation in the normal population: Introducing the PDI (Peters et al. Delusions Inventory). Schizophr Bull. 1999;25(3):553–76. [DOI] [PubMed] [Google Scholar]
- 10.Bak M, Myin-Germeys I, Hanssen M, Bijl R. When does experience of psychosis result in a need for care? A prospective general population study. Schizophr Bull. 2003;29(2):349–58. [DOI] [PubMed] [Google Scholar]
- 11.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th Edition. 5th ed Arlington VA: American Psychiatric Association; 2013. [Google Scholar]
- 12.Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, et al. The Hierarchical Taxonomy of Psychopathology (HiTOP): A dimensional alternative to traditional nosologies. J Abnorm Psychol. 2017;126(4):454–77. [DOI] [PubMed] [Google Scholar]
- 13.Raine A The SPQ: A scale for the assessment of schizotypal personality based on DSM-III-R criteria. Schizophr Bull. 1991;17(4):555–64. [DOI] [PubMed] [Google Scholar]
- 14.Rossi A, Daneluzzo E. Schizotypal dimensions in normals and schizophrenic patients: A comparison with other clinical samples. Schizophr Res. 2002;54(1–2):67–75. [DOI] [PubMed] [Google Scholar]
- 15.Calkins ME, Curtis CE, Grove WM, Iacono WG. Multiple dimensions of schizotypy in first degree biological relatives of schizophrenia patients. Schizophr Bull. 2004;30(2):317–25. [DOI] [PubMed] [Google Scholar]
- 16.Wilson S, Sponheim SR. Dimensions underlying psychotic and manic symptomatology: Extending normal-range personality traits to schizophrenia and bipolar spectra. Compr Psychiatry. 2014;55(8):1809–19. [DOI] [PubMed] [Google Scholar]
- 17.Tackett JL, Quilty LC, Sellbom M, Rector NA, Bagby RM. Additional evidence for a quantitative hierarchical model of mood and anxiety disorders for DSM-V: The context of personality structure. J Abnorm Psychol. 2008;117(4):812–25. [DOI] [PubMed] [Google Scholar]
- 18.Wright AGC, Thomas KM, Hopwood CJ, Markon KE, Pincus AL, Krueger RF. The hierarchical structure of DSM-5 pathological personality traits. J Abnorm Psychol. 2012;121(4):951–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zimmermann J, Altenstein D, Krieger T, Holtforth MG, Pretsch J, Alexopoulos J, et al. The structure and correlates of self-reported DSM-5 maladaptive personality traits: Findings from two German-speaking samples. J Pers Disord. 2014;28(4):518–40. [DOI] [PubMed] [Google Scholar]
- 20.Hopwood CJ, Thomas KM, Markon KE, Wright AGC, Krueger RF. DSM-5 personality traits and DSM–IV personality disorders. J Abnorm Psychol. 2012;121(2):424–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bastiaens T, Claes L, Smits D, De Clercq B, De Fruyt F, Rossi G, et al. The construct validity of the Dutch personality inventory for DSM-5 personality disorders (PID-5) in a clinical sample. Assessment. 2016;23(1):42–51. [DOI] [PubMed] [Google Scholar]
- 22.Quilty L, Ayearst L, Chmielewski M. The psychometric properties of the Personality Inventory for DSM-5 in an APA DSM-5 field trial sample. Assessment. 2013;20(3):362–9. [DOI] [PubMed] [Google Scholar]
- 23.Bo S, Bach B, Mortensen E, Simonsen E. Reliability and hierarchical structure of DSM-5 pathological traits in a Danish mixed sample. J Pers Disord. 2016;30(1):112–29. [DOI] [PubMed] [Google Scholar]
- 24.Fossati A, Krueger RF, Markon KE, Borroni S, Maffei C. Reliability and validity of the personality inventory for DSM-5 (PID-5): Predicting DSM-IV personality disorders and psychopathy in community-dwelling Italian adults. Assessment. 2013. December;20(6):689–708. [DOI] [PubMed] [Google Scholar]
- 25.Thomas K, Yalch M, Krueger R. The convergent structure of DSM-5 personality trait facets and five-factor model trait domains. Assessment. 2013;20(3):308–11. [DOI] [PubMed] [Google Scholar]
- 26.Gore WL, Widiger TA. The DSM-5 dimensional trait model and five-factor models of general personality. J Abnorm Psychol. 2013;122(3):816–21. [DOI] [PubMed] [Google Scholar]
- 27.Griffin S a Samuel DB. A closer look at the lower-order structure of the Personality Inventory for DSM-5: Comparison with the Five-Factor Model. Personal Disord. 2014;5(4):406–12. [DOI] [PubMed] [Google Scholar]
- 28.DeYoung CG, Carey BE, Krueger RF, Ross SR. Ten aspects of the Big Five in the Personality Inventory for DSM–5. Personal Disord Theory, Res Treat. 2016;7(2):113–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tackett JL, Silberschmidt AL, Krueger RF, Sponheim SR. A dimensional model of personality disorder: Incorporating DSM Cluster A characteristics. Personal Disord Theory, Res Treat. 2009;S(1):27–34. [DOI] [PubMed] [Google Scholar]
- 30.Paunonen S V, Ashton MC. Big Five factors and facets and the prediction of behavior. J Pers Soc Psychol. 2001;81(3):524–39. [PubMed] [Google Scholar]
- 31.Malouff JM, Thorsteinsson EB, Schutte NS. The relationship between the Five-Factor Model of personality and symptoms of clinical disorders: A meta-analysis. J Psychopathol Behav Assess. 2005;27(2):101–14. [Google Scholar]
- 32.DeYoung CG, Grazioplene RG, Peterson JB. From madness to genius: The Openness/Intellect trait domain as a paradoxical simplex. J Res Pers. 2012;46(1):63–78. [Google Scholar]
- 33.Krueger RF, McGue M, Iacono WG. The higher-order structure of common DSM mental disorders: Internalization, externalization, and their connections to personality. Pers Individ Dif. 2001;30(7):1245–59. [Google Scholar]
- 34.Watson D, Stasik SM, Ro E, Clark LA. Integrating normal and pathological personality: Relating the DSM-5 trait-dimensional model to general traits of personality. Assessment. 2013;20(3):312–26. [DOI] [PubMed] [Google Scholar]
- 35.Few LR, Miller JD, Rothbaum AO, Meller S, Maples J, Terry DP, et al. Examination of the Section III DSM-5 diagnostic system for personality disorders in an outpatient clinical sample. J Abnorm Psychol. 2013;122(4):1057–69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.James LM, Anders SL, Peterson CK, Engdahl BE, Krueger RF, Georgopoulos AP. DSM-5 personality traits discriminate between posttraumatic stress disorder and control groups. Exp Brain Res. 2015;233(7):2021–8. [DOI] [PubMed] [Google Scholar]
- 37.Wright AGC, Simms LJ. On the structure of personality disorder traits: Conjoint analyses of the CAT-PD, PID-5, and NEO-PI-3 trait models. Personal Disord. 2014;5(1):43–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Markon KE. Modeling psychopathology structure: A symptom-level analysis of Axis I and II disorders. Psychol Med. 2010;40(2):273–88. [DOI] [PubMed] [Google Scholar]
- 39.Kotov R, Ruggero CJ, Krueger RF, Watson D, Yuan Q, Zimmerman M. New dimensions in the quantitative classification of mental illness. Arch Gen Psychiatry. 2011;68(10):1003–11. [DOI] [PubMed] [Google Scholar]
- 40.Bastiaens T, Smits D, De Hert M, Thys E, Bryon H, Sweers K, et al. The relationship between the Personality Inventory for the DSM-5 (PID-5) and the psychotic disorder in a clinical sample. Assessment. 2017;1–9. [DOI] [PubMed] [Google Scholar]
- 41.Ohi K, Shimada T, Nitta Y, Kihara H, Okubo H, Uehara T, et al. The Five-Factor Model personality traits in schizophrenia: A meta-analysis. Psychiatry Res. 2016;240:34–41. [DOI] [PubMed] [Google Scholar]
- 42.Allen T, DeYoung C. Personality neuroscience and the five factor model In: Widiger T, editor. Oxford Handbook of the Five Factor Model. 1st ed New York, NY: Oxford University Press; 2016. p. 319. [Google Scholar]
- 43.Krueger RF, Johnson W. Behavioral genetics and personality: A new look at the integration of nature and nurture In: John OP, Robins RW,Pervin LA, editors. Handbook of personality: Theory and research. 3rd ed New York, NY: Guilford Press; 2008. p. 287–310. [Google Scholar]
- 44.International Schizophrenia Consortium. Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature. 2009;460(7256):748–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Craddock N, O’Donovan MC, Owen MJ. Psychosis genetics: Modeling the relationship between schizophrenia, bipolar disorder, and mixed (or “schizoaffective”) psychoses. Schizophr Bull. 2009;35(3):482–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lichtenstein P, Yip B, Björk C, Pawitan Y. Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: A population-based study. Lancet. 2009;373(9659):234–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Iacono WG, Malone SM, McGue M. Substance use disorders, externalizing psychopathology, and P300 event-related potential amplitude. Int J Psychophysiol. 2003;48(2):147–78. [DOI] [PubMed] [Google Scholar]
- 48.Snitz BE, MacDonald AW, Carter CS. Cognitive deficits in unaffected first-degree relatives of schizophrenia patients: A meta-analytic review of putative endophenotypes. Schizophr Bull. 2005;32(1):179–94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Narayan AJ, Allen TA, Cullen KR, Klimes-Dougan B. Disturbances in reality testing as markers of risk in offspring of parents with bipolar disorder: a systematic review from a developmental psychopathology perspective. Bipolar Disord. 2013;15(7):723–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Silberschmidt AL, Sponheim SR. Personality in relation to genetic liability for schizophrenia and bipolar disorder: Differential associations with the COMT Val108/158Met polymorphism. Schizophr Res. 2008;100(1–3):316–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Kang SS, Dionisio DP, Sponheim SR. Abnormal mechanisms of antisaccade generation in schizophrenia patients and unaffected biological relatives of schizophrenia patients. Psychophysiology. 2011;48(3):350–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Longenecker JM, Venables NC, Kang SS, McGuire KA, Sponheim SR. Brain responses at encoding predict limited verbal memory retrieval by persons with schizophrenia. Arch Clin Neuropsychol. 2018;33(4):477–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.van Os J, Linscott RJ, Myin-Germeys I, Delespaul P, Krabbendam L. A systematic review and meta-analysis of the psychosis continuum: Evidence for a psychosis proneness-persistence-impairment model of psychotic disorder. Psychol Med. 2009;39(2):179–95. [DOI] [PubMed] [Google Scholar]
- 54.Schürhoff F, Szöke A, Méary A, Bellivier F, Rouillon F, Pauls D, et al. Familial aggregation of delusional proneness in schizophrenia and bipolar pedigrees. Am J Psychiatry. 2003;160(7):1313–9. [DOI] [PubMed] [Google Scholar]
- 55.Varghese D, Saha S, Scott JD, Chan RCK, McGrath JJ. The association between family history of mental disorder and delusional-like experiences: A general population study. Am J Med Genet Part B Neuropsychiatr Genet. 2011;156(4):478–83. [DOI] [PubMed] [Google Scholar]
- 56.First M, Spitzer R, Gibbon M, Williams J. Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I). American Psychiatric Press, Inc. Washington, D.C; 1997. [Google Scholar]
- 57.American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, Text Revision (DSM-IV-TR) 4th ed. 2000. [Google Scholar]
- 58.Kendler K, Lieberman J, Walsh D. The Structured Interview for Schizotypy (SIS): A preliminary report. Schizophr Bull. 1989;15(4):559–71. [DOI] [PubMed] [Google Scholar]
- 59.Lukoff D, Liberman R, Nuechterlein K. Symptom monitoring in the rehabilitation of schizophrenic patients. Schizophr Bull. 1986;12(4):578–603. [DOI] [PubMed] [Google Scholar]
- 60.Andreasen NC. Scale for the Assessment of Negative Symptoms (SANS). Iowa City: University of Iowa; 1983. [Google Scholar]
- 61.Andreasen NC. Scale for the Assessment of Positive Symptoms (SAPS). Iowa City: University of Iowa; 1984. [Google Scholar]
- 62.Leckman JF. Best estimate of lifetime psychiatric diagnosis. Arch Gen Psychiatry. 1982;39(8):879–83. [DOI] [PubMed] [Google Scholar]
- 63.Brooker BH, Cyr JJ. Tables for clinicians to use to convert WAIS-R short forms. J Clin Psychol. 1986;42(6):982–6. [Google Scholar]
- 64.Wechsler D Wechsler Adult Intelligence Scale – Third Edition (WAIS–III). 3rd ed Wechsler D, editor. Psychological Corporation; 1997. [Google Scholar]
- 65.Krueger RF, Derringer J, Markon KE, Watson D, Skodol AE. Initial construction of a maladaptive personality trait model and inventory for DSM-5. Psychol Med. 2012;42(9):1879–90. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Raine A, Reynolds C, Lencz T, Scerbo A, Triphon N, Kim D. Cognitive-perceptual, interpersonal, and disorganized features of schizotypal personality. Schizophr Bull. 1994;20(1):191–201. [DOI] [PubMed] [Google Scholar]
- 67.Šidák Z Rectangular confidence regions for the means of multivariate normal distributions. J Am Stat Assoc. 1967;62(318):626–33. [Google Scholar]
- 68.Chmielewski M, Bagby RM, Markon K, Ring AJ, Ryder AG. Openness to Experience, Intellect, Schizotypal Personality Disorder, and Psychoticism: Resolving the controversy. J Pers Disord. 2014;28(4):483–99. [DOI] [PubMed] [Google Scholar]
- 69.Schultze-Lutter F, Klosterkötter J, Nikolaides A, Ruhrmann S. Personality dimensions in persons symptomatically at risk of psychosis: Pronounced but lacking a characteristic profile. Early Interv Psychiatry. 2015;9(3):242–7. [DOI] [PubMed] [Google Scholar]
- 70.Van Snellenberg JX, de Candia T, W B, WH B, TJ C, TA A, et al. Meta-analytic evidence for familial coaggregation of schizophrenia and bipolar disorder. Arch Gen Psychiatry. 2009;66(7):748. [DOI] [PubMed] [Google Scholar]
- 71.Jacobs N, van Os J, Derom C, Thiery E, Delespaul P, Wichers M. Neuroticism explained? From a non-informative vulnerability marker to informative person-context interactions in the realm of daily life. Br J Clin Psychol. 2011;50(1):19–32. [DOI] [PubMed] [Google Scholar]
- 72.Carpenter WT. Porous diagnostic boundaries: A new emphasis for the Bulletin. Schizophr Bull. 2014;40(1):1–2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Anderson JL, Sellbom M, Ayearst L, Quilty LC, Chmielewski M, Bagby RM. Associations between DSM-5 section III personality traits and the Minnesota Multiphasic Personality Inventory 2-Restructured Form (MMPI-2-RF) scales in a psychiatric patient sample. Psychol Assess. 2015;27(3):801–15. [DOI] [PubMed] [Google Scholar]
- 74.Quilty LC, Sellbom M, Tackett JL, Bagby RM. Personality trait predictors of bipolar disorder symptoms. Psychiatry Res. 2009;169(2):159–63. [DOI] [PubMed] [Google Scholar]
- 75.Aleman A, Lincoln TM, Bruggeman R, Melle I, Arends J, Arango C, et al. Treatment of negative symptoms: Where do we stand, and where do we go? Schizophr Res. 2017;186:55–62. [DOI] [PubMed] [Google Scholar]
- 76.Newby JM, McKinnon A, Kuyken W, Gilbody S, Dalgleish T. Systematic review and meta-analysis of transdiagnostic psychological treatments for anxiety and depressive disorders in adulthood. Clin Psychol Rev. 2015;40:91–110. [DOI] [PubMed] [Google Scholar]
- 77.Markon K, Chmielewski M, Miller C. The reliability and validity of discrete and continuous measures of psychopathology: a quantitative review. Psychol Bull. 2011;137(5):856–79. [DOI] [PubMed] [Google Scholar]
- 78.Buckley PF, Miller BJ, Lehrer DS, Castle DJ. Psychiatric comorbidities and schizophrenia. Schizophr Bull. 2009;35(2):383–402. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Merikangas KR, Akiskal HS, Angst J, Greenberg PE, Hirschfeld RMA, Petukhova M, et al. Lifetime and 12-month prevalence of bipolar spectrum disorder in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2007;64(5):543. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Longenecker J, George TP, Voore P, Bagby RM, McKenzie K, Pollock BG, et al. Cross-cutting symptom domains predict functioning in the psychotic spectrum. In: Canadian Psychiatric Association Conference 2018. [Google Scholar]
- 81.Allen TA, Carey BE, McBride C, Bagby RM, DeYoung CG, Quilty LC. Big Five aspects of personality interact to predict depression. J Pers. 2018;86(4):714–25. [DOI] [PubMed] [Google Scholar]
- 82.Naragon-Gainey K, Simms LJ. Three-way interaction of neuroticism, extraversion, and conscientiousness in the internalizing disorders: Evidence of disorder specificity in a psychiatric sample. J Res Pers. 2017;70:16–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Du L, Bakish D, Ravindran A V, Hrdina PD. Does fluoxetine influence major depression by modifying five-factor personality traits? J Affect Disord. 2002;71(1–3):235–41. [DOI] [PubMed] [Google Scholar]
- 84.Quilty LC, De Fruyt F, Rolland J-P, Kennedy SH, Rouillon PF, Bagby RM. Dimensional personality traits and treatment outcome in patients with major depressive disorder. J Affect Disord. 2008;108(3):241–50. [DOI] [PubMed] [Google Scholar]
- 85.Suzuki T, Samuel DB, Pahlen S, Krueger RF. DSM-5 alternative personality disorder model traits as maladaptive extreme variants of the five-factor model: an item-response theory analysis. J Abnorm Psychol. 2015;124(2):343–54. [DOI] [PubMed] [Google Scholar]
- 86.Wright ZE, Pahlen S, Krueger RF. Genetic and environmental influences on Diagnostic and Statistical Manual of Mental Disorders-Fifth Edition (DSM-5) maladaptive personality traits and their connections with normative personality traits. J Abnorm Psychol. 2017;126(4):416–28 [DOI] [PubMed] [Google Scholar]


