Abstract
Hypercalcemia of malignancy frequently manifests as paraneoplastic syndrome in patients with solid tumors. A 71-year-old man was diagnosed with stage IIIB lung squamous cell carcinoma. Laboratory examination revealed high serum calcium concentration with elevated serum parathyroid hormone-related protein (PTHrP) and 1,25-dihydroxyvitamin D3 levels. As the patient did not respond to the initial treatment with calcitonin, extracellular fluid infusion, and chemotherapy, systemic prednisolone was administered additionally. Thus, the levels of serum calcium normalized and PTHrP and 1,25-dihydroxyvitamin D3 decreased simultaneously. To our knowledge, this is the first case report on the successful treatment of hypercalcemia of malignancy caused by PTHrP and 1,25-dihydroxyvitamin D3 cosecretion in a patient with lung cancer.
1. Introduction
Hypercalcemia is a relatively common finding in cases of paraneoplastic syndrome. Hypercalcemia of malignancy (HCM) occurs in up to 20 to 30% of patients with cancer [1]. It can be classified into the following four types: caused by local osteolytic hypercalcemia, secretion of parathyroid hormone- (PTH-) related protein (PTHrP), secretion of 1,25-dihydroxyvitamin D3 (calcitriol), and ectopic hyperparathyroidism. PTHrP derived from solid tumors, especially squamous cell carcinoma, is a well-known mediator of HCM. However, calcitriol is rarely secreted from these tumors. Only few previous reports have described elevated levels of both blood serum PTHrP and calcitriol in patients with solid tumors [2–6]. Here, we report the case of a patient with squamous cell lung cancer, who developed hypercalcemia caused by cosecretion of PTHrP and calcitriol, which was improved by corticosteroids.
2. Case Presentation
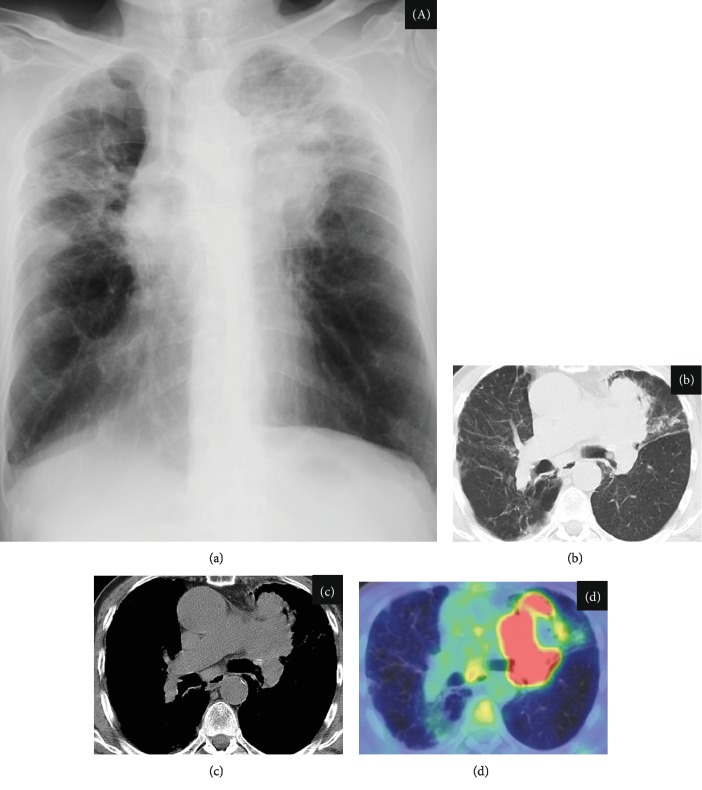
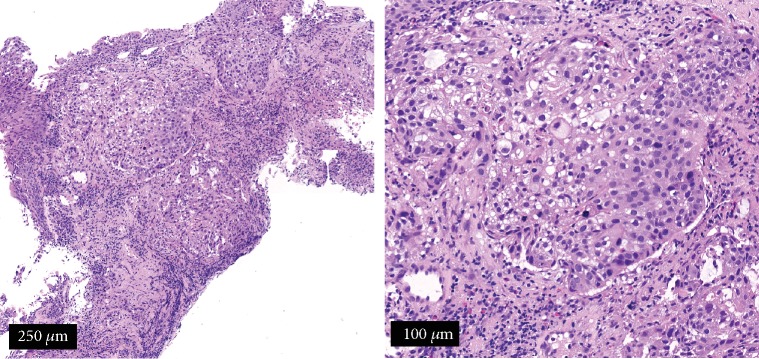
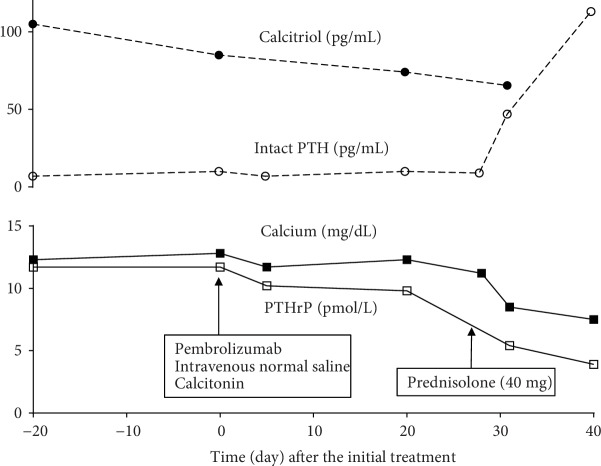
The patient was a 71-year-old man who presented with nausea, fatigue, and anorexia. He was referred to our hospital for investigation of these symptoms and abnormalities; as such, chest radiography was performed (Figure 1(a)). Laboratory examination revealed an elevated blood serum calcium level (12.3 mg/dL, serum albumin level 3.2 g/dL) and normal creatinine level, which did not indicate dehydration and renal dysfunction (Table 1). He did not take any hypercalcemia-inducing agents such as thiazide diuretics, theophylline, lithium, osteoporosis therapeutic drugs, and vitamin D supplements. Serum PTHrP level was elevated (11.7 pmol/L (reference value < 1.1 pmol/L)), although the intact PTH level was low (7 pg/mL (reference value 10-65 pg/mL)). Surprisingly, the serum calcitriol level was elevated (105 pg/mL (reference value 20-40 pg/mL)) although 25-OH vitamin D3 level was low (16 ng/mL (reference value > 20 ng/mL)). Integrated computed tomography and 18F-2-deoxy-2-fluoro-D-glucose (FDG) positron emission tomography (PET/CT) showed uptake of FDG by a left pulmonary hilar lesion and both ipsilateral mediastinal and subcarinal lymph nodes, because of which lung cancer with metastasis to the lymph nodes was highly suspected (Figures 1(b)–1(d)). No other organs, including the bone, liver, and bilateral adrenal glands, showed FDG uptake. Head magnetic resonance imaging revealed no metastatic lesions. Based on the results of a bronchoscopic examination showing proliferation of large polygonal atypical cells with intercellular bridges in the bronchial submucosa (Figure 2), the patient was diagnosed with stage IIIB lung squamous cell carcinoma (55% of tumor cells were positive for programmed cell death-ligand 1 expression). Lymphoma, granulomatous disease, and mycobacterial or fungal infections were ruled out based on the results of histopathological analysis. Pembrolizumab (200 mg/body every 3 weeks) was administered as the first-line treatment. In addition to anticancer treatment, calcitonin and intravenous 0.9% normal saline were first administered. Despite initial treatment for HCM, hypercalcemia did not improve. On day 28 from the initial treatment of HCM, systemic prednisolone (40 mg/day) was additively administered. Serum calcium level rapidly decreased thereafter and normalized (serum calcium 8.5 mg/dL, serum albumin 3.1 g/dL) on day 31. Serum PTHrP and calcitriol levels decreased simultaneously (PTHrP: 5.4 pmol/L; calcitriol: 65.4 pg/mL) in response to systemic prednisolone. Serum intact PTH levels were elevated to the normal range (47 pg/mL), indicating improvement of the negative feedback circuit to regulate serum calcium levels. However, lung cancer gradually progressed during two cycles of pembrolizumab, suggesting an inadequate therapeutic response to this immunotherapy. Respiratory failure developed, and the patient died on day 58. Figure 3 shows the clinical course of this patient.
Figure 1.
Chest radiography and F-2-deoxy-2-fluoro-D-glucose positron emission tomography/computed tomography (PET/CT) findings. (a) Chest radiography demonstrating a mass-like lesion on the left upper lung field and (b–d) PET/CT showing uptake of FDG by a left pulmonary hilar lesion mass and subcarinal lymph nodes.
Table 1.
Results of laboratory tests conducted on admission.
| Value | Reference value | ||
|---|---|---|---|
| Peripheral blood | |||
| White blood cells | 11,900 | /μL | 3,900-9,800 |
| Neutrophils | 85.8 | % | |
| Lymphocytes | 8.5 | % | |
| Basophils | 0.5 | % | |
| Eosinophils | 0.8 | % | |
| Monocytes | 4.4 | % | |
| Hemoglobin | 11.8 | g/dL | 13.5-17.6 |
| Hematocrit | 36.8 | % | 39.8-51.8 |
| Platelets | 413,000 | /μL | 131,000-362,000 |
| Blood biochemistry | |||
| Total bilirubin | 0.59 | mg/dL | 0.2-1.2 |
| Aspartate transaminase | 25 | U/L | 9.0-30 |
| Alanine transaminase | 17 | U/L | 4.0-35 |
| Lactate dehydrogenase | 197 | U/L | 80-260 |
| Alkaline phosphatase | 282 | U/L | 106-345 |
| γ-Glutamyl transpeptidase | 59 | U/L | 16-84 |
| Total protein | 7.5 | g/dL | 6.5-8.2 |
| Albumin | 3.2 | g/dL | 3.9-4.9 |
| Urea nitrogen | 16.4 | mg/dL | 8.0-20 |
| Creatinine | 0.94 | mg/dL | 0.6-1.1 |
| Sodium | 143 | mEq/L | 132-148 |
| Potassium | 4.2 | mEq/L | 3.6-5.0 |
| Chloride | 105 | mEq/L | 96-110 |
| Calcium | 12.3 | mg/dL | 8.2-10.2 |
| Phosphorus | 2.6 | mg/dL | 2.3-4.3 |
| Intact PTH | 7 | pg/mL | 10-65 |
| PTHrP | 11.7 | pmol/L | <1.1 |
| Calcitriol | 105 | pg/mL | 20-40 |
| 25-OH vitamin D3 | 16 | ng/mL | >20 |
| Urine | |||
| pH | 5.5 | 5.0-9.0 | |
| Occult blood | (-) | ||
| Sugar | (-) | ||
| Protein | (-) | ||
| Urea nitrogen | 312 | mg/dL | 650-1,300 |
| Creatinine | 69.9 | mg/dL | 50-150 |
| Sodium | 38 | mEq/L | 70-250 |
| Potassium | 37.7 | mEq/L | 25-100 |
| Chloride | 41 | mEq/L | 70-250 |
| Calcium | 22.2 | mg/dL | 50-300 |
| Phosphorus | 36.8 | mg/dL | <500 |
PTH: parathyroid hormone; PTHrP: parathyroid hormone-related protein; calcitriol: 1,25-dihydroxyvitamin D3.
Figure 2.
Pathological analysis of a transbronchial lung biopsy specimen using hematoxylin and eosin staining. Proliferation of large polygonal atypical cells with intercellular bridges is seen in the bronchial submucosa, suggesting squamous cell carcinoma. (a) Scale bar represents 250 μm; (b) scale bar represents 100 μm.
Figure 3.
Clinical course of the present case. Calcitriol: 1,25-dihydroxyvitamin D3; PTH: parathyroid hormone; PTHrP: parathyroid hormone-related protein.
3. Discussion
To our knowledge, this is a rare case with cosecretion of PTHrP and calcitriol in lung cancer. There are only five previous reports of the cosecretion of PTHrP and calcitriol in cases of solid tumors including ovarian carcinoma, pancreatic neuroendocrine tumor, renal cell carcinoma, seminoma, and lung cancer [2–6], which are summarized in Table 2. In the previous report on lung cancer, the histological type was squamous cell carcinoma [6], as in our case. The patient could not receive systemic prednisolone because of rapid tumor progression with no improvement of hypercalcemia. However, systemic prednisolone could be effective for HCM induced by cosecretion of PTHrP and calcitriol in other cases with solid tumors. In summary, this is the first report of the successful treatment of HCM caused by cosecretion of PTHrP and calcitriol in a patient with lung cancer.
Table 2.
Summary of cases presenting cosecretion of PTHrP and calcitriol in solid tumors.
| Author | Age | Sex | Primary tumor | Histological type | Tx of HCM | Sx | CTx | RTx | Course of the tumor | Outcome of HCM | Effective Tx of HCM |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Hoekman et al. [2] | 70 | F | Ovarian carcinoma | Adenocarcinoma | Pamidronate | Yes | No | No | Resection | Improvement | Operation |
| Hydrocortisone | |||||||||||
| Van den Eynden et al. [3] | 59 | M | Pancreatic neuroendocrine tumor | Neuroendocrine tumor | Pamidronate | Yes | Yes | No | Reduction | Improvement | Chemotherapy |
| Zoledronic acid | |||||||||||
| Shivnani et al. [4] | 57 | M | Renal cell carcinoma | Clear cell | Pamidronate | No | Yes | No | Progression | Improvement | Prednisolone |
| Prednisolone | |||||||||||
| Rodriguez-Gutierrez et al. [5] | 35 | M | Seminoma | Seminoma | Calcitonin | No | Yes | No | Reduction | Improvement | Chemotherapy |
| Nemr et al. [6] | 60 | M | Lung cancer | Squamous | Calcitonin | No | No | No | Progression | No improvement | None |
| Zoledronic acid | |||||||||||
| Furosemide | |||||||||||
| Ogawaa | 71 | M | Lung cancer | Squamous | Prednisolone | No | Yes | No | Progression | Improvement | Prednisolone |
| Calcitonin |
CTx: chemotherapy; HCM: hypercalcemia of malignancy; RTx: radiation therapy; Sx: surgery; Tx: treatment. aPresent case.
The mechanism of independently elevated PTHrP and calcitriol productions remains poorly understood. PTHrP secreted from solid tumors binds to the PTH-1 receptor causing hypercalcemia [7]. However, unlike PTH, it does not elicit calcitriol synthesis [8]. 1-α-Hydroxylase, an enzyme converting 25-OH vitamin D3 to calcitriol, normally expresses in the kidney. Previous report demonstrated that its expression in alveolar macrophages was higher in the lung cancer patients than in the healthy group [9]. Additionally, a human small cell lung cancer cell line constitutively expressed this enzyme [10]. These findings might explain the possible mechanism of PTHrP and calcitriol cosecretion in patients with lung cancer.
Hypercalcemia with an elevated calcitriol level has been reported in patients with some granulomatous diseases including sarcoidosis, tuberculosis, fungal infection, and lymphoma [11]. In our case, histopathological examination suggested no complications with these diseases. Thus, we concluded lung cancer as the cause of elevated serum calcitriol.
Treatment using extracellular fluid infusion, calcitonin, and chemotherapy was initially introduced in our case. Previous reports indicated that combined extracellular fluid infusion and calcitonin worked rapidly (within several hours) in some cases [12]. However, this therapy was not effective without responsiveness of the lung cancer to chemotherapy, which strongly suggested the necessity of an additive therapeutic drug.
In a case of metastatic renal cell carcinoma, prednisolone was chosen for the treatment of HCM, with beneficial effects [4]. Similarly, in our case, hypercalcemia showed a good response to systemic prednisolone as an add-on agent, possibly through steroid-mediated suppressive effects on the expression of enzymes necessary for PTHrP and calcitriol synthesis.
In four previous reports, bisphosphonates were selected for treating HCM due to cosecretion of PTHrP and calcitriol [2–4, 6], although hypercalcemia was not unaltered in the patients. Bisphosphonates were consequently unnecessary in our case because prednisolone therapy in addition to calcitonin and extracellular fluid infusion was sufficient to normalize the serum calcium levels. However, recurrence of HCM might be observed during initial therapy using prednisolone, though long-term observation was impossible due to the rapid tumor progression. Bisphosphonates could possibly be beneficial as additive agents in this situation [13, 14].
In summary, caution must be exercised by clinicians when patients with lung cancer show hypercalcemia with elevated serum levels of both PTHrP and calcitriol. Early introduction of prednisolone as an optimal therapeutic strategy should be recommended for patients with HCM induced by cosecretion of PTHrP and calcitriol.
Conflicts of Interest
The authors have no conflicts of interest to report.
References
- 1.Stewart A. F. Clinical practice. Hypercalcemia associated with cancer. New England Journal of Medicine. 2005;352(4):373–379. doi: 10.1056/NEJMcp042806. [DOI] [PubMed] [Google Scholar]
- 2.Hoekman K., Tjandra Y. I., Papapoulos S. E. The role of 1,25-dihydroxyvitamin D in the maintenance of hypercalcemia in a patient with an ovarian carcinoma producing parathyroid hormone-related protein. Cancer. 1991;68(3):642–647. doi: 10.1002/1097-0142(19910801)68:3<642::aid-cncr2820680334>3.0.co;2-a. [DOI] [PubMed] [Google Scholar]
- 3.Van den Eynden G. G., Neyret A., Fumey G., et al. PTHrP, calcitonin and calcitriol in a case of severe, protracted and refractory hypercalcemia due to a pancreatic neuroendocrine tumor. Bone. 2007;40(4):1166–1171. doi: 10.1016/j.bone.2006.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Shivnani S. B., Shelton J. M., Richardson J. A., Maalouf N. M. Hypercalcemia of malignancy with simultaneous elevation in serum parathyroid hormone-related peptide and 1,25-dihydroxyvitamin D in a patient with metastatic renal cell carcinoma. Endocrine Practice. 2009;15(3):234–239. doi: 10.4158/EP.15.3.234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Rodríguez-Gutiérrez R., Zapata-Rivera M. A., Quintanilla-Flores D. L., et al. 1,25-dihydroxyvitamin D and PTHrP mediated malignant hypercalcemia in a seminoma. BMC Endocrine Disorders. 2014;14(1) doi: 10.1186/1472-6823-14-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Nemr S., Alluri S., Sundaramurthy D., Landry D., Braden G. Hypercalcemia in lung cancer due to simultaneously elevated PTHrP and ectopic calcitriol production: first case report. Case Reports in Oncological Medicine. 2017;2017:3. doi: 10.1155/2017/2583217.2583217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Esbrit P., Egido J. The emerging role of parathyroid hormone-related protein as a renal regulating factor. Nephrology, Dialysis, Transplantation. 2000;15(8):1109–1111. doi: 10.1093/ndt/15.8.1109. [DOI] [PubMed] [Google Scholar]
- 8.Horwitz M. J., Tedesco M. B., Sereika S. M., Hollis B. W., Garcia-Ocaña A., Stewart A. F. Direct comparison of sustained infusion of human parathyroid hormone-related protein-(1-36) [hPTHrP-(1-36)] versus hPTH-(1-34) on serum calcium, plasma 1,25-dihydroxyvitamin D concentrations, and fractional calcium excretion in healthy human volunteers. The Journal of Clinical Endocrinology and Metabolism. 2003;88(4):1603–1609. doi: 10.1210/jc.2002-020773. [DOI] [PubMed] [Google Scholar]
- 9.Yokomura K., Suda T., Sasaki S., Inui N., Chida K., Nakamura H. Increased expression of the 25-hydroxyvitamin D3-1α-hydroxylase gene in alveolar macrophages of patients with lung cancer. The Journal of Clinical Endocrinology and Metabolism. 2003;88(12):5704–5709. doi: 10.1210/jc.2003-030537. [DOI] [PubMed] [Google Scholar]
- 10.Mawer E. B., Hayes M. E., Heys S. E., et al. Constitutive synthesis of 1,25-dihydroxyvitamin D3 by a human small cell lung cancer cell line. The Journal of Clinical Endocrinology and Metabolism. 1994;79(2):554–560. doi: 10.1210/jcem.79.2.8045976. [DOI] [PubMed] [Google Scholar]
- 11.Tebben P. J., Singh R. J., Kumar R. Vitamin D-mediated hypercalcemia: mechanisms, diagnosis, and treatment. Endocrine Reviews. 2016;37(5):521–547. doi: 10.1210/er.2016-1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Maier J. D., Levine S. N. Hypercalcemia in the intensive care unit: a review of pathophysiology, diagnosis, and modern therapy. Journal of Intensive Care Medicine. 2013;30(5):235–252. doi: 10.1177/0885066613507530. [DOI] [PubMed] [Google Scholar]
- 13.Hoff A. O., Toth B. B., Altundag K., et al. Frequency and risk factors associated with osteonecrosis of the jaw in cancer patients treated with intravenous bisphosphonates. Journal of Bone and Mineral Research. 2008;23(6):826–836. doi: 10.1359/jbmr.080205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Mhaskar R., Kumar A., Miladinovic B., Djulbegovic B. Bisphosphonates in multiple myeloma: an updated network meta-analysis. Cochrane Database of Systematic Reviews. 2017;(12, article CD003188) doi: 10.1002/14651858.CD003188.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]