Abstract
Context
Slips, trips, and falls are leading causes of musculoskeletal injuries in firefighters. Researchers have hypothesized that heat stress is the major contributing factor to these fireground injuries.
Objective
To examine the effect of environmental conditions, including hot and ambient temperatures, and exercise on functional and physiological outcome measures, including balance, rectal temperature, and perceived exertion.
Design
Randomized controlled clinical trial.
Setting
Laboratory environmental chamber.
Patients or Other Participants
A total of 13 healthy, active career firefighters (age = 26 ± 6 years [range = 19–35 years], height = 178.61 ± 4.93 cm, mass = 86.56 ± 16.13 kg).
Intervention(s)
Independent variables consisted of 3 conditions (exercise in heat [37.41°C], standing in heat [37.56°C], and exercise in ambient temperature [14.24°C]) and 3 data-collection times (preintervention, postintervention, and postrecovery). Each condition was separated from the others by at least 1 week and lasted a maximum of 40 minutes or until the participant reached volitional fatigue or a rectal temperature of 40.0°C.
Main Outcome Measure(s)
Firefighting-specific functional balance performance index, rectal temperature, and rating of perceived exertion.
Results
Exercise in the heat decreased functional balance, increased rectal temperature, and altered the perception of exertion compared with the other intervention conditions.
Conclusions
A bout of exercise in a hot, humid environment increased rectal temperature in a similar way to that reported in the physically active population and negatively affected measures of functional balance. Rather than independently affecting balance, the factors of exercise and heat stress appeared to combine, leading to an increased likelihood of slips, trips, and falls.
Keywords: balance, tactical athletes, heat stress
Key Points
Heat stress from the environment combined with exercise decreased functional balance in firefighters.
Rectal temperature was elevated by a bout of exercise in a hot, humid environment and was not effectively decreased using the recovery procedures for firefighters.
Trained career firefighters demonstrated high levels of perceived exertion while exercising in a hot, humid environment.
Musculoskeletal injuries (MSIs) due to overexertion, slips, trips, and falls are a leading cause of lost duty days in the fire service.1,2 These injuries can occur in a variety of occupational environments that are broadly categorized into fireground (eg, vehicle fires, wildfires, structural fires) and nonfireground (eg, medical emergencies, vehicle accidents, natural disasters) environments. Most firefighter injuries occur in the fireground category.2 This is a complex environment in which firefighters are exposed to strenuous exercise and extreme heat, as well as environmental hazards, such as falling debris, reduced visibility, and smoke accumulation.
The number of fireground injuries in the United States has declined on average from approximately 60 922 per year in the 1980s to approximately 49 685 per year in the 1990s, approximately 39 054 per year in the early 2000s, and an average of 30 096 per year from 2010 to 2015. In 2015, a total of 29 130 fireground injuries were recorded by the National Fire Protection Association (NFPA).2 Whereas the number of injuries per year has declined, the injury rate has remained relatively unchanged since 1981, ranging between 22.6 and 25.6 injuries per 1000 fires.2 In contrast, the injury rate for nonfire incidents has been reduced from 1.24 to 0.44 per 1000 incidents since 1981.2 The leading causes of fireground injuries were slips, trips, and jumps, which accounted for 27.2% of all fireground injuries (7923 injuries). Slips, trips, and falls often produce more severe injuries (eg, strains, sprains, and fractures),3 which result in the highest incidence rates of missed work days4 and high medical and compensation costs.5 Therefore, these injuries are very costly to firefighters' health and wellness, to fire-service readiness, and monetarily.
Environmental heat stress is considered the primary cause of muscle fatigue and overexertion in the fire service.1 Overexertion and bodily reactions accounted for 20% of all nonfatal firefighting injuries between 2003 and 2014.6 According to the National Institute for Occupational Safety and Health,7 individuals who are exposed to extreme heat or work in a hot, humid environment are at risk for heat stress. Researchers1 indicated that environmental heat stress can lead to loss of functional balance, resulting in slips, trips, and falls. This conclusion was based on previous studies in which investigators showed that heat exposure promoted dehydration and fatigue, increased cardiovascular strain, and impaired cognitive function.1 Whereas heat stress contributes to injury in the fire service, it is also important to understand the contribution of fatigue from physical activity to balance impairments and the resulting MSIs so that targeted interventions can be developed to combat the combined risk factors that contribute to injury at the fireground.
Investigators8–10 reported that aerobic and anaerobic exercise could reduce postural control, alter mechanics, and lead to disruptions in balance. Exercise fatigue can reduce postural stability by causing changes in the center of pressure away from more stable positions. Changes caused by exercise fatigue can also modify joint kinematics, reducing the ability to detect and respond to slips, and decrreasing control over body dynamics when exposed to challenging postural positions.9–11 The negative effects of fatiguing exercise on postural control and balance seem to subside within 10 to 15 minutes after cessation of exercise.8,10,11 Importantly, these studies were conducted in nonfirefighter populations that did not use personal protective equipment (PPE), which may exacerbate the effect of exercise on balance.
Improvements in firefighter PPE have effectively reduced the risk of injury due to exposure to chemicals and extreme heat12; however, PPE has been reported to negatively affect balance.13,14 The negative effect of PPE on balance may be linked to substantial alterations in center of mass, gait mechanics, and functional balance among firefighters.1,15
Much of the literature on exertional heat illnesses related to sport participation has established a consensus and recommendation for whole-body cooling to lower the rectal temperature of the patient as fast as possible at the site.16 In the fire service, the likelihood of returning to live fire suppression after a recovery protocol is high; therefore, the use of whole-body cooling is not likely or practical.17 Regardless of the return to activity, the NFPA18 advised in standard 1584 that all firefighters use passive- or active-cooling methods, replace fluids, remove PPE, and rest for a minimum of 10 minutes after live fire suppression and continuous firefighting activity. Various methods of recovery, including passive (eg, removing protective clothing and equipment)19,20 and active (forearm immersion, oscillating fans)21,22 techniques have been assessed, with positive and negative recovery outcomes. The 10- to 20-minute recovery period for firefighters is insufficient for restoring or reducing rectal temperature and heart rate.22,23 Whether a recovery period for firefighters improves functional measures of performance before continuing sustained fire activities is unknown.
In much of the research conducted with firefighters, the interaction of heat stress and exercise on balance has been examined, rather than the relative contributions of each factor.1 Therefore, the purpose of our study was to determine the individual and combined effects of exercise and environmental temperature on functional balance and whether functional balance is restored during a 20-minute recovery period. We hypothesized that exercise in a hot, humid environment would produce greater functional-balance deficits than exercise in ambient temperatures and standing in the heat. We also proposed that the 20-minute recovery protocol would not return rectal temperature and perceived exertion measures to baseline values.
METHODS
Design
This study was a randomized, controlled trial with a 3 × 3 repeated-measures, single-cohort design. The independent variables were intervention with 3 levels (exercise in heat, standing in heat, and exercise in ambient temperature) and time with 3 levels of measurement (preintervention, postintervention, and postrecovery). The dependent variables were functional balance, rectal temperature, and rating of perceived exertion (RPE).
Participants
A convenience sample of participants was recruited by telephone, e-mail, and face-to-face solicitation from local fire stations in a midsize town (approximate population = 60 000) in the southeastern United States. Fifteen career firefighters began the study, and 13 male career firefighters (age = 26 ± 6 years [range = 19–35 years], height = 178.61 cm ± 4.93 cm, mass = 86.56 kg ± 16.13 kg, experience = 7 ± 6 years) completed all 3 interventions. We excluded 1 volunteer who had personal time constraints and 1 volunteer who was unable to complete the postintervention functional-balance assessment because of signs and symptoms of exertional heat exhaustion. Firefighters completed a health-history questionnaire and were included if they were not on restricted duty in the fire department at the time of the study, were not taking any medications that put them at a higher risk for dehydration, were not prone to dehydration, and had not been hospitalized for dehydration in the 6 months before the study. Participants provided written informed consent, and the study was approved by the institutional review boards at Indiana State University and Auburn University.
Intervention
Each of the 3 randomized conditions lasted a maximum of 40 minutes and was completed in an environmental chamber (Espec North America Inc, Hudsonville, MI) that continuously regulated the temperature and relative humidity. For the heat conditions, the chamber was set to 46.1°C with 40% humidity. For the ambient-temperature condition, the chamber was set to 18.3°C with 40% humidity. During testing, the temperature and humidity in the environmental chamber remained constant and consistent. Testing occurred midday in October in the southeastern United States. We captured the wet-bulb globe temperature (WBGT; QUESTemp 32 Thermal Environment Monitor; 3M, St Paul, MN) during each minute of the condition. Participants completed the 3 conditions at least 7 days apart to avoid any acclimatization. For the exercise-in-heat (WBGT = 37.41°C ± 1.28°C) and exercise-in-ambient-temperature (WBGT = 14.24°C ± 0.45°C) conditions, a treadmill was set at an incline of 2.5% and speed of 4.5 km/h. For the standing-in-heat condition (WBGT = 37.56°C ± 0.65°C), participants stood upright during testing. The WBGT for the 2 heat conditions was selected as an accurate, yet conservative, temperature for the testing that was similar to the temperatures used in previous research24–26 on the fire service. During the intervention, participants were restricted from consuming water as they would be during a firefighting run (or job-related task). The intervention was considered complete when participants reached a rectal temperature of 40°C, volitional fatigue, or the 40-minute time limit. We chose the maximum time of 40 minutes because it corresponds to the maximum time a firefighter is expected to work without a break according to NFPA standard 1584.18
After completing the intervention and the associated firefighter functional-balance test, participants had a 20-minute recovery period. Recovery included removing the jacket, hood, helmet, gloves, and self-contained breathing apparatus pack and lowering the trousers to the boots. Participants sat in front of fans and were provided unlimited chilled or room-temperature water, which was also consistent with NFPA standard 1584.18 Figure 1 depicts the recovery protocol.
Figure 1.
Recovery protocol using isolated electric fans and cold-water consumption. The research team member monitored core temperature during the 20-minute period.
Firefighter-Specific Functional-Balance Testing
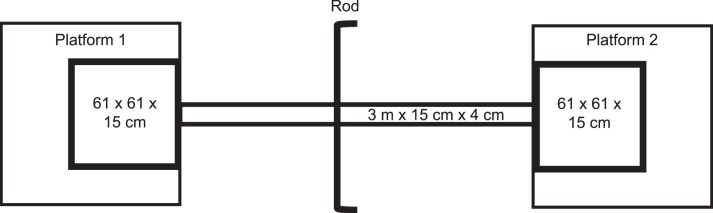
Participants completed a firefighter-specific functional-balance test in full firefighting turnout gear and PPE at preintervention, postintervention, and postrecovery. Their turnout gear and PPE included boots, trousers, jacket, hood, helmet, gloves, and self-contained breathing apparatus pack (mass = 22.7 kg ± 0.69 kg). During the study, the self-contained breathing apparatus was not connected to a full face mask and not delivering air. The firefighter functional-balance test was developed and validated specifically for firefighters.15 Participants began the test on a 15-cm-high platform, stepped down onto a 15-cm-wide narrow plank, and walked to another 15-cm-high platform (Figure 2). They were instructed to turn around in the designated space on the second platform and walk back across the plank to finish on the first platform. To increase the difficulty of the task, participants completed this balance test while maneuvering under a rod positioned at 75% of their height (Figure 2). For each trial, they completed the balance test 2 times without the obstacle and 4 times with the obstacle, followed by 2 more times without the obstacle. We recorded the time (in seconds) on a stopwatch (Sportline Inc, Yonkers, NY) from when the participants stepped off the first platform to the time they returned to the first platform and turned around. In addition to recording the time, we recorded minor and major errors for each trial. A minor error consisted of foot or hand contact with the ground, hand contact on the platform, stepping outside the designated space on the platform on the turn, stepping outside the designated space on the platform due to being unable to stop, or hitting the obstacle. The only major error was knocking off the obstacle rod. We monitored and recorded the errors on either side of the functional-balance test setup. Figure 3 shows a participant going under the obstacle rod in various manners during the test. The following formula, which was similar to that used in previous research,13,15 was used to calculate performance index (PI) for each trial of the test:
 |
Figure 2.
Functional-balance test.
Figure 3.
Participants completed the functional-balance test obstacle trial using different approaches as seen in the A, side shuffle, and B, forward minisquat maneuver.
A higher PI score indicated worse functional balance, and a lower PI score indicated better functional balance.
Physiological Measures
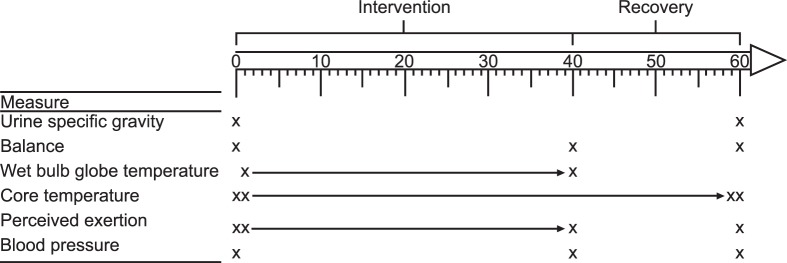
The mass of participants was recorded on their entry to the facility before and after they donned their full turnout gear and PPE. Rectal temperature and RPE were recorded at the completion of each firefighter functional-balance test, each minute of the environmental intervention, and each minute of the recovery period (Figure 4). To capture rectal temperature, participants wore rectal thermistors (Doric Series 400; VAS Engineering, San Diego, CA) that were self-inserted to a depth of 10 cm, which was marked on the flexible probe with a piece of tape and were read by a digital thermometer (Doric 450 Series model 450TH; VAS Engineering) throughout the test condition. Perceived exertion was measured using the Borg RPE scale.24 A digital handheld “pen” refractometer (model PEN-Urine SG; ATAGO, Tokyo, Japan) was used to assess urine specific gravity before and after the trial to ensure euhydration and the safety of the participants.
Figure 4.
The study design. Urine specific gravity was measured at the beginning and end of the trial. Balance and blood pressure were assessed preintervention, postintervention, and postrecovery. Wet-bulb globe temperature was measured each minute throughout the intervention. Core temperature was recorded during each minute of the intervention and recovery. Perceived exertion was measured throughout the entire intervention and after the last baseline assessment.
Statistical Analysis
Data were transferred into a custom spreadsheet (Excel 2010; Microsoft Corp, Redmond, WA). Measures of central tendency were performed for demographic and variable measures. A 3 × 3 repeated-measures analysis of variance was conducted on the main outcome measures of PI, rectal temperature, and perceived exertion for the 3 conditions (exercise in heat, exercise in ambient temperature, and standing in heat) at 3 times (preintervention, postintervention, and postrecovery). Follow-up 1-way analysis of variance and pairwise comparisons with the Holm sequential Bonferroni adjustments were completed. Data were analyzed using SPSS (version 24; IBM Corp, Armonk, NY). We set the α level a priori at .05.
RESULTS
The descriptive data collected for each main outcome measure are reported in the Table.
Table.
Descriptive Analysis and Pairwise Comparisons (N = 13)
|
Main Outcome Measure |
Condition |
Time |
Mean ± SD |
Condition − Condition = Mean Difference (95% Confidence Interval) |
| Performance index, points | ||||
| Exercise in heat | Preintervention | 8.24 ± 1.66 | Preintervention − postintervention = −1.86 (−2.78, −0.96)a | |
| Postintervention | 10.10 ± 2.00 | Preintervention − postrecovery = 0.38 (−0.31, 1.06) | ||
| Postrecovery | 7.86 ± 1.64 | Postintervention − postrecovery = 2.24 (1.51, 2.96)a | ||
| Exercise in ambient temperature | Preintervention | 8.74 ± 2.74 | Preintervention − postintervention = −0.15 (−0.66, 0.43) | |
| Postintervention | 8.89 ± 2.95 | Preintervention − postrecovery = 0.42 (−0.17, 1.00) | ||
| Postrecovery | 8.32 ± 2.54 | Postintervention − postrecovery = 0.57 (0.13, 0.94)a | ||
| Standing in heat | Preintervention | 8.32 ± 1.43 | Preintervention − postintervention = −0.13 (−0.64, 0.38) | |
| Postintervention | 8.45 ± 1.65 | Preintervention − postrecovery = 0.57 (0.06, 1.07)a | ||
| Postrecovery | 7.75 ± 1.63 | Postintervention − postrecovery = 0.70 (0.41, 0.98)a | ||
| Rectal temperature, °C | ||||
| Exercise in heat | Preintervention | 37.52 ± 0.20 | Preintervention − postintervention = −1.75 (−2.19, −1.32)a | |
| Postintervention | 39.27 ± 0.65 | Preintervention − postrecovery = −0.87 (−1.21, −0.54)a | ||
| Postrecovery | 38.39 ± 0.53 | Postintervention − postrecovery = 0.88 (0.54, 1.21)a | ||
| Exercise in ambient temperature | Preintervention | 37.44 ± 0.43 | Preintervention − postintervention = −0.91 (−1.18, −0.64)a | |
| Postintervention | 38.35 ± 0.50 | Preintervention − postrecovery = −0.16 (−0.60, 0.27) | ||
| Postrecovery | 37.60 ± 0.79 | Postintervention − postrecovery = 0.75 (0.48, 1.01)a | ||
| Standing in heat | Preintervention | 37.58 ± 0.25 | Preintervention − postintervention = −0.52 (−0.70, −0.34)a | |
| Postintervention | 38.10 ± 0.35 | Preintervention − postrecovery = −0.02 (−0.48, −0.34) | ||
| Postrecovery | 37.60 ± 0.77 | Postintervention − postrecovery = 0.50 (0.14, 0.86)a | ||
| Rating of perceived exertion, points | ||||
| Exercise in heat | Preintervention | 7.62 ± 1.33 | Preintervention − postintervention = −9.76 (−11.94, −7.60)a | |
| Postintervention | 17.38 ± 3.29 | Preintervention − postrecovery = −1.46 (−2.43, −0.49)a | ||
| Postrecovery | 9.08 ± 1.66 | Postintervention − postrecovery = 8.30 (6.51, 10.11)a | ||
| Exercise in ambient temperature | Preintervention | 8.54 ± 2.03 | Preintervention − postintervention = −1.92 (−2.23, −1.02)a | |
| Postintervention | 10.46 ± 2.26 | Preintervention − postrecovery = 0.23 (−0.73, 1.91) | ||
| Postrecovery | 8.31 ± 1.70 | Postintervention − postrecovery = 2.15 (1.38, 2.92)a | ||
| Standing in heat | Preintervention | 8.46 ± 1.85 | Preintervention − postintervention = −2.77 (−4.78, −0.76)a | |
| Postintervention | 11.23 ± 4.42 | Preintervention − postrecovery = 0.46 (−0.45, 1.37) | ||
| Postrecovery | 8.00 ± 1.68 | Postintervention − postrecovery = 3.23 (1.42, 5.05)a | ||
Difference (P ≤ .05).
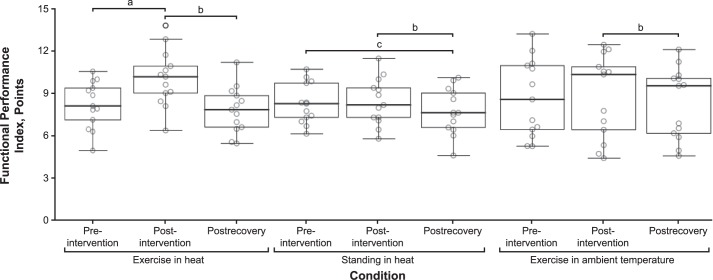
Performance Index
When comparing all conditions, we did not identify differences at preintervention. We found a condition-by-time interaction effect (F4,48 = 9.86, P < .001, ηp2 = 0.45). We observed a main effect of time (F2,24 = 20.77, P < .001, ηp2 = 0.63) but not condition (F2,24 = 0.79, P = .46, ηp2 = 0.06). Follow-up pairwise comparisons among conditions revealed several differences that are summarized in the Table and Figure 5.
Figure 5.
Functional-balance test performance index (errors and time) for each intervention at each data-point measurement. Boxes indicate the first and third quartiles. a Difference between preintervention and postintervention measures (P ≤ .05). b Difference between postintervention and postrecovery measures (P ≤ .05). c Difference between preintervention and postrecovery measures (P ≤ .05).
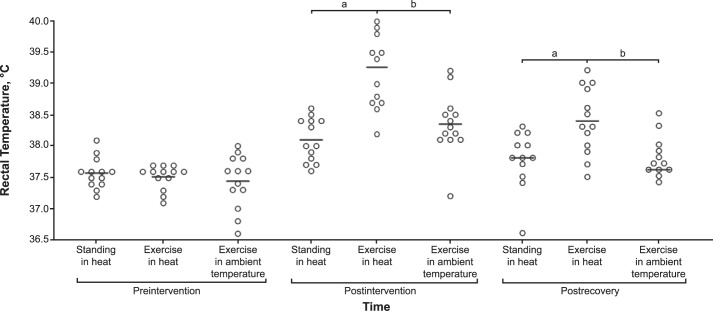
Rectal Temperature
A condition-by-time interaction effect was present (F4,48 = 8.69, P < .001, ηp2 = 0.42). We also noted main effects of condition (F2,24 = 59.03, P < .001, ηp2 = 0.83) and time (F2,24 = 9.89, P < .001, ηp2 = 0.45). Follow-up pairwise comparisons for condition and time revealed several differences that are summarized in the Table.
Preintervention rectal temperatures did not differ for any condition. The mean rectal temperature for the exercise-in-heat condition was greater than that for the standing-in-heat (mean difference = 1.169°, P < .001; 95% confidence interval [CI] = 0.708, 1.630) and the exercise-in-ambient-temperature (mean difference = 0.923°, P = .02; 95% CI = 0.178, 1.668) conditions at postintervention. We did not observe a difference between the standing-in-heat and the exercise-in-ambient-temperature conditions (P = .45). For measures collected postrecovery, rectal temperatures were higher for the exercise-in-heat than the standing-in-heat (mean difference = 0.792°, P = .005; 95% CI = 0.242, 1.342) and the exercise-in-ambient-temperature (mean difference = 0.792°, P = .045; 95% CI = 0.016, 1.569) conditions. The rectal temperatures for each condition at each time are provided in Figure 6.
Figure 6.
Rectal temperature data depicting no difference at the preintervention measure and an elevated rectal temperature after recovery for the exercise-in-heat condition. The horizontal bar indicates the median. a Difference between the standing-in-heat and exercise-in-heat conditions (P ≤ .05). b Difference between the exercise-in-heat and exercise-in-ambient-temperature conditions (P ≤ .05).
Rating of Perceived Exertion
We found a condition-by-time interaction effect (F4,48 = 65.97, P < .001, ηp2 = 0.70). Main effects were demonstrated for condition (F2,24 = 67.92, P < .001, ηp2 = 0.85) and time (F2,24 = 7.05, P = .004, ηp2 = 0.89). Follow-up pairwise comparisons for condition and time yielded several differences that are summarized in the Table and Figure 7.
Figure 7.
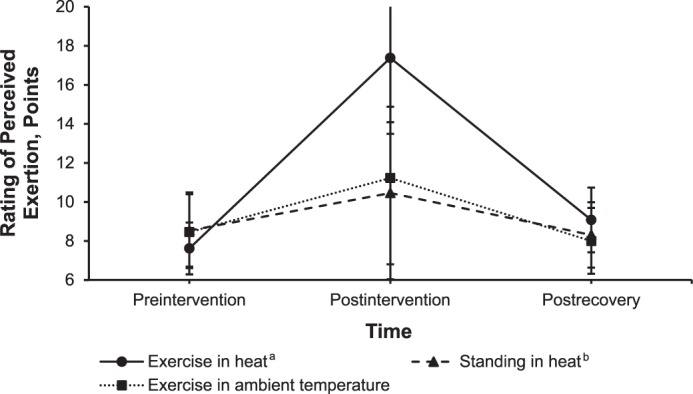
Rating of perceived exertion using the Borg scale24 throughout the study interventions. a Difference between estimated marginal means for the exercise-in-heat and standing-in-heat conditions (P ≤ .05). b Difference between estimated marginal means for the standing-in-heat and exercise-in-ambient-temperature conditions (P ≤ .05).
DISCUSSION
We examined the separate and combined effects of environmental heat and exercise on functional-balance PI, rectal temperature, and RPE. We hypothesized that the combined effects of environmental heat and exercise would lead to poorer scores on the functional-balance test, higher rectal temperatures, and higher levels of RPE. We also proposed that the current NFPA recovery protocol would be ineffective for returning firefighters to baseline measures of functional balance, rectal temperature, and RPE.
Performance Index
The PI was negatively affected by a bout of exercise, regardless of the environmental condition tested. The exercise-in-heat condition resulted in worse PI scores than the standing-in-heat condition. These findings suggested that a combination of exercise and a hot, humid environment may contribute to decreases in balance during firefighting operations and may help explain why most reported injuries during fireground operations are due to slips, trips, falls, and jumps.3
These data also help describe the relationships among heat stress, activity, fatigue, and measures of balance in firefighters. Researchers1 have suggested that the primary source of fatigue and the link between firefighting tasks and MSIs is heat stress. Others27 have demonstrated that fatigue due to activity diminished dynamic balance in firefighters in a nonthermoregulated environment. Our results suggested that it is not the factors of activities and heat stress independently that affect balance, leading to an increased likelihood of slips, trips, and falls, but rather the combination of the 2 factors. Our findings also indicated that both modifiable and nonmodifiable factors specific to the fire service may contribute to the MSIs incurred during slips, trips, falls, and jumps.3
Whereas the environment in which firefighters work cannot be changed, possible solutions could be implemented to offset the decreased balance that we and other researchers13 have found. Two potential avenues for developing a solution could be (1) alternating and improving firefighter PPE and (2) implementing fire service physical-training programs that focus on neuromuscular control. Substantial research has been conducted to improve the design of the current firefighter PPE to account for the demands of long operations in potentially hot, humid environments and the movement demands of a firefighter in today's complex fire-and-rescue environments. Clinicians also may be able to address the challenge of decreased balance and neuromuscular control after firefighting operations by incorporating firefighting-specific programs for developing balance and neuromuscular control. Balance training in other physically active populations has been shown to improve outcomes such as postural sway, functional movements, neuromuscular control, and agility.28 Given the unique nature of the fire service and the addition of a substantial external load, current programs developed for other populations may not be appropriate for firefighters. Investigators should examine whether currently available program options are appropriate for the fire service.
Rectal Temperature
Our data on rectal temperature changes across conditions and times suggested that both individual and combined effects of environmental heat and exercise were present. The greatest change in rectal temperature (mean difference = 1.75°C; 95% CI = 1.197°C, 2.310°C) between preintervention and postintervention was during the exercise-in-heat condition followed by the exercise-in-ambient-temperature (mean difference = 0.91°C; 95% CI = 0.561°C, 1.255°C) and standing-in-heat (mean difference = 0.52°C; 95% CI = 0.294°C, 0.753°C) conditions. Whereas each component (environmental heat and exercise) had an effect in increasing rectal temperature, the combined effects led to a greater increase than simply the sum of the effects of environmental heat and exercise. Our results were similar to those of authors29–31 who reported increased rectal temperature in firefighters and other physically active individuals after activity in a variety of environmental conditions. The increase in rectal temperature could help explain why we saw decrements in the PI. After each condition, the range of mean rectal temperatures was from 38.10°C ± 0.35°C to 39.27°C ± 0.65°C, with the exercise-in-heat condition exhibiting the greatest increase in rectal temperature. Exertional heat exhaustion is often indicated by muscle weakness, fatigue, and a lack of coordination.16,32 The elevated rectal temperature and known physical and cognitive deficits associated with heat exhaustion may help explain the elevated functional-balance PI scores seen during this condition. The PI is a calculation of the time to complete the task, as well as the number of errors committed during the task. Therefore, if an individual is experiencing the signs and symptoms of heat exhaustion, we might expect PI scores to be negatively affected.
Given the unexpected nature of fire-service response, it is difficult to mitigate the negative effects of exertional heat illness through acclimatization. However, it may be possible to mitigate and prevent exertional heat illness by integrating cooling modalities into the firefighter PPE. Researchers should examine the feasibility of widespread integration of these cooling technologies into the PPE system.
Rating of Perceived Exertion
The RPE data suggested that all 3 conditions resulted in increased RPEs. Similar to the PI score and rectal temperature, the exercise-in-heat condition led to the greatest mean score increase (mean difference = 9.77 points; 95% CI = 7.005, 12.534), followed by the standing-in-heat (mean difference = 2.77 points; 95% CI = 0.210, 5.329) and the exercise-in-ambient-temperature (mean difference = 1.92 points; 95% CI = 0.768, 3.078) conditions. Examining the previously reported minimally important difference score for the Borg scale that we used to measure RPE, we determined that the difference in RPE between the standing-in-heat and the exercise-in-ambient-temperature conditions might not be clinically meaningful.33 The published minimally important difference for the Borg scale is 1 point, meaning that changes of less than 1 point may not be clinically meaningful in practice. For each condition, all participants started at an RPE score associated with the very, very light, or very light category anchor. During the postintervention measurements, participants reported scores associated with the very hard category anchor for the exercise-in-heat condition. For the postintervention measurements for the exercise-in-ambient-temperature and the standing-in-heat conditions, participants reported scores associated with the fairly light category anchor. They perceived that the exercise-in-heat condition was much more challenging than the other 2 conditions.
Improving a firefighter's RPE in uncomfortable and challenging conditions is of great importance. As the fireground becomes more complex, firefighters often must engage in multiple, complicated operations and tactics in a wide variety of conditions and situations. If their attention is drawn away from these essential tasks and toward the feeling of discomfort, their fireground effectiveness may decrease, placing them at an increased risk of injury or death due to mistakes and mishaps.34,35 Whether training in uncomfortable situations, such as those created in this study, translates to reduced cognitive load and better decision making at the fireground is unknown. Researchers should examine whether this relationship exists and whether it leads to a reduction in the risk of MSIs among firefighters.
Recovery Protocol
Our results also demonstrated that for all 3 conditions, the NFPA 1584 recovery protocol18 led to functional-balance PI scores that returned to near baseline. This suggests that the current standard for recovery effectively returns functional measures of balance to preactivity levels, regardless of the condition. Our data indicated that the recovery protocol effectively returned rectal temperature to baseline in a hot environment with no activity and an ambient environment with exercise but was ineffective in returning rectal temperature to near-baseline measures in the exercise-in-heat condition. This lack of cooling may be dangerous to firefighters who return to firefighting activities after a recovery period because they may perceive they are well and ready to reengage while their rectal temperature is still elevated, putting them at risk for a heat emergency upon reengaging. The decrease in functional measures for the exercise-in-heat condition may also be influenced by fatigue, which researchers have supported as a contributor to lower extremity injury36,37 and have identified in the fire service.27 These results are similar to previous work38 with tactical athletes in which rectal temperature remained elevated after treatment with a mist fan and cooling towels. Our RPE results again suggested that, whereas the NFPA 1584 recovery protocol18 may be appropriate for general activity or minimal activity in a hot environment, it may not be effective for firefighters exerting themselves in a hot, humid environment. The NFPA 1584 recovery protocol18 recommended that firefighters remove their turnout gear and PPE. This guideline was supported by Casa et al,16 who stated that removing clothing and equipment facilitated cooling because of evaporative properties. Investigators should examine alternatives to the current protocol that allow for a rapid return to service while still returning measures of physiological and functional performance to baseline.
CONCLUSIONS
Functional balance was negatively affected by a bout of exercise in a hot, humid environment. Our findings indicated that neither exercise nor heat alone influenced balance but rather the combination of the 2 factors led to an increased likelihood of slips, trips, and falls. This observation is unique in the literature, as the exposure to heat itself as the factor has been identified as contributing to the high rates of MSI in firefighters during fireground activities. We also demonstrated that rectal temperature increased the most after the exercise-in-heat condition, a finding similar to that reported in a physically active population.29 Exertional heat exhaustion, indicated by elevated rectal temperatures combined with a higher RPE, could have affected the PI scores for functional balance, as the time to complete tasks may have changed because of the RPE. Finally, the NFPA18 standard 1584 was ineffective in returning core temperature to near-baseline levels in the exercise-in-heat condition, which is typical of live fire situations.
ACKNOWLEDGMENTS
This research was supported by the Graduate Student Research Fund from the Center of Research and Creativity at Indiana State University (Dr Winkelmann). We thank the project research assistants, including Sarah Gordon, Jordan Devine, Jess Nendze, and Bryce Munz. We also thank Chief Dow Sport, Chief John Lankford, and the City of Auburn Fire Department.
REFERENCES
- 1.Smith DL, Horn G, Goldstein E, et al. Champaign, IL: Firefighter Life Safety Research Center, Illinois Fire Service Institute, University of Illinois at Urbana-Champaign; 2019. Firefighter Fatalities and Injuries: The Role of Heat Stress and PPE. https://www.fsi.illinois.edu/documents/research/FFLSRC_FinalReport.pdf. Accessed January 15. [Google Scholar]
- 2.Haynes HJ, Molis JL. US firefighter injuries in 2014. Natl Fire Protect Assoc J. 2015. Nov–Dec.
- 3. Karter MJ., Jr Patterns of Firefighter Fireground Injuries Quincy, MA: National Fire Protection Association; 2012: 13 [Google Scholar]
- 4.Nonfatal occupational injuries and illnesses requiring days away from work, 2015. Bureau of Labor Statistics Web site. 2018. https://www.bls.gov/news.release/pdf/osh2.pdf. Accessed November 5.
- 5.Karter MJ., Jr Fire loss in the United States during 2011. Natl Fire Protect Assoc J. 2012. Sept–Oct. [PubMed]
- 6.Marsh SM, Gwilliam M, Konda S, Tiesman HM, Fahy R. Nonfatal injuries to firefighters treated in US emergency departments, 2003–2014. Am J Prev Med. 2018;55(3):353–360. doi: 10.1016/j.amepre.2018.04.051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.National Institute for Occupational Safety and Health (NIOSH) heat stress. Centers for Disease Control and Prevention Web site. 2018. https://www.cdc.gov/niosh/topics/heatstress/. Accessed November 5.
- 8.Fox ZG, Mihalik JP, Blackburn JT, Battaglini CL, Guskiewicz KM. Return of postural control to baseline after anaerobic and aerobic exercise protocols. J Athl Train. 2008;43(5):456–463. doi: 10.4085/1062-6050-43.5.456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lew FL, Qu X. Effects of multi-joint muscular fatigue on biomechanics of slips. J Biomech. 2014;47(1):59–64. doi: 10.1016/j.jbiomech.2013.10.010. [DOI] [PubMed] [Google Scholar]
- 10.Bryanton MA, Bilodeau M. Postural stability with exhaustive repetitive sit-to-stand exercise in young adults. Hum Mov Sci. 2016;49:47–53. doi: 10.1016/j.humov.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 11.Papa EV, Foreman KB, Dibble LE. Effects of age and acute muscle fatigue on reactive postural control in healthy adults. Clin Biomech (Bristol, Avon) 2015;30(10):1108–1113. doi: 10.1016/j.clinbiomech.2015.08.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Guidotti TL, Clough VM. Occupational health concerns of firefighting. Annu Rev Public Health. 1992;13(1):151–171. doi: 10.1146/annurev.pu.13.050192.001055. [DOI] [PubMed] [Google Scholar]
- 13.Punakallio A, Lusa S, Luukkonen R. Protective equipment affects balance abilities differently in younger and older firefighters. Aviat Space Environ Med. 2003;74(11):1151–1156. [PubMed] [Google Scholar]
- 14.Csiernik AJ, Winkelmann ZK, Eberman LE, True JR, Games KE. Personal protective equipment diminishes static and dynamic balance in firefighters [abstract] J Athl Train. 2017;52(suppl 6):S-38. [Google Scholar]
- 15.Hur P, Hsiao-Wecksler ET, Rosengren KS, Horn G, Smith DL. Effect of protective clothing and fatigue on functional balance of firefighters. J Ergon. 2013;S2(004) [Google Scholar]
- 16.Casa DJ, DeMartini JK, Bergeron MF, et al. National Athletic Trainers' Association position statement: exertional heat illnesses. J Athl Train. 2015;50(9):986–1000. doi: 10.4085/1062-6050-50.9.07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Barr D, Gregson W, Reilly T. The thermal ergonomics of firefighting reviewed. Appl Ergon. 2010;41(1):161–172. doi: 10.1016/j.apergo.2009.07.001. [DOI] [PubMed] [Google Scholar]
- 18.National Fire Protection Association. NFPA 1584: Standard on the Rehabilitation Process for Members During Emergency Operations and Training Exercises. Quincy, MA: National Fire Protection Association; 2008. [Google Scholar]
- 19.Hostler D, Reis SE, Bednez JC, Kerin S, Suyama J. Comparison of active cooling devices with passive cooling for rehabilitation of firefighters performing exercise in thermal protective clothing: a report from the Fireground Rehab Evaluation (FIRE) trial. Prehosp Emerg Care. 2010;14(3):300–309. doi: 10.3109/10903121003770654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Selkirk GA, McLellan TM. Physical work limits for Toronto firefighters in warm environments. J Occup Environ Hyg. 2004;1(4):199–212. doi: 10.1080/15459620490432114. [DOI] [PubMed] [Google Scholar]
- 21.Yeargin S, McKenzie AL, Eberman LE, Kingsley JD, Dziedzicki DJ, Yoder P. Physiological and perceived effects of forearm or head cooling during simulated firefighting activity and rehabilitation. J Athl Train. 2016;51(11):927–935. doi: 10.4085/1062-6050-51.10.09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Smith DL, Haller JM, Benedict R, Moore-Merrell L. Firefighter incident rehabilitation: interpreting heart rate responses. Prehosp Emerg Care. 2016;20(1):28–36. doi: 10.3109/10903127.2015.1037477. [DOI] [PubMed] [Google Scholar]
- 23.Horn GP, Gutzmer S, Fahs CA, et al. Physiological recovery from firefighting activities in rehabilitation and beyond. Prehosp Emerg Care. 2011;15(2):214–225. doi: 10.3109/10903127.2010.545474. [DOI] [PubMed] [Google Scholar]
- 24.Montain SJ, Sawka MN, Cadarette BS, Quigley MD, McKay JM. Physiological tolerance to uncompensable heat stress: effects of exercise intensity, protective clothing, and climate. J Appl Physiol (1985) 1994;77(1):216–222. doi: 10.1152/jappl.1994.77.1.216. [DOI] [PubMed] [Google Scholar]
- 25.Kim JH, Williams WJ, Coca A, Yokota M. Application of thermoregulatory modeling to predict core and skin temperatures in firefighters. Int J Ind Ergon. 2013;43(1):115–120. [Google Scholar]
- 26.Chou C, Tochihara Y, Ismail MS, Lee JY. Physiological strains of wearing aluminized and non-aluminized firefighters' protective clothing during exercise in radiant heat. Ind Health. 2011;49(2):185–194. doi: 10.2486/indhealth.ms1034. [DOI] [PubMed] [Google Scholar]
- 27.Games KE, Csiernik AJ, Winkelmann ZK, True JR, Eberman LE. Fatigue diminishes static and dynamic balance in firefighters [abstract] J Athl Train. 2017;52(suppl 6):S-151. [Google Scholar]
- 28.Zech A, Hübscher M, Vogt L, Banzer W, Hänsel F, Pfeifer K. Balance training for neuromuscular control and performance enhancement: a systematic review. J Athl Train. 2010;45(4):392–403. doi: 10.4085/1062-6050-45.4.392. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.DeMartini JK, Casa DJ, Belval LN, et al. Environmental conditions and the occurrence of exertional heat illnesses and exertional heat stroke at the Falmouth Road Race. J Athl Train. 2014;49(4):478–485. doi: 10.4085/1062-6050-49.3.26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Horn GP, Blevins S, Fernhall B, Smith DL. Core temperature and heart rate response to repeated bouts of firefighting activities. Ergonomics. 2013;56(9):1465–1473. doi: 10.1080/00140139.2013.818719. [DOI] [PubMed] [Google Scholar]
- 31.Williams-Bell FM, Aisbett B, Murphy BA, Larsen B. The effects of simulated wildland firefighting tasks on core temperature and cognitive function under very hot conditions. Front Physiol. 2017;8:815. doi: 10.3389/fphys.2017.00815. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kenefick RW, Sawka MN. Heat exhaustion and dehydration as causes of marathon collapse. Sports Med. 2007;37(4–5):378–381. doi: 10.2165/00007256-200737040-00027. [DOI] [PubMed] [Google Scholar]
- 33.Ries AL. Minimally clinically important difference for the UCSD Shortness of Breath Questionnaire, Borg scale, and visual analog scale. COPD. 2005;2(1):105–110. doi: 10.1081/copd-200050655. [DOI] [PubMed] [Google Scholar]
- 34.Aisbett B, Nichols D. Fighting fatigue whilst fighting bushfire: an overview of factors contributing to firefighter fatigue during bushfire suppression. Aust J Emerg Manage. 2007;22(3):31–39. [Google Scholar]
- 35.Robinson SJ, Leach J, Owen-Lynch PJ, Sünram-Lea SI. Stress reactivity and cognitive performance in a simulated firefighting emergency. Aviat Space Environ Med. 2013;84(6):592–599. doi: 10.3357/asem.3391.2013. [DOI] [PubMed] [Google Scholar]
- 36.Bagherian S, Rahnama N, Wikstrom EA, Clark MA, Rostami F. Characterizing lower extremity movement scores before and after fatigue in collegiate athletes with chronic ankle instability. Int J Athl Ther Train. 2018;23(1):27–32. [Google Scholar]
- 37.Nagle K, Johnson B, Brou L, Landman T, Sochanska A, Comstock RD. Timing of lower extremity injuries in competition and practice in high school sports. Sports Health. 2017;9(3):238–246. doi: 10.1177/1941738116685704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Sefton JM, McAdam JS, Pascoe DD, et al. Evaluation of 2 heat-mitigation methods in army trainees. J Athl Train. 2016;51(11):936–945. doi: 10.4085/1062-6050-51.10.13. [DOI] [PMC free article] [PubMed] [Google Scholar]