Abstract
Significant shifts or discontinuities in symptom course can mark points of transition and reveal important change processes. The authors investigated 2 patterns of change in depression—the rapid early response and a transient period of apparent worsening that the authors call a depression spike. Participants were 29 patients diagnosed with major depressive disorder who enrolled in an open trial of an exposure-based cognitive therapy. Hierarchical linear modeling revealed an overall cubic shape of symptom change and that both the rapid response and spike patterns predicted lower posttreatment depression. Patients wrote weekly narratives about their depression. Early narratives of rapid responders were coded as having more hope than those of nonrapid responders. The narratives of patients with a depression spike had more cognitive–emotional processing during this period of arousal than those without a spike. Findings are discussed in the context of cognitive–emotional processing theories in depression and anxiety disorders.
Keywords: rapid response, depression spike, emotional processing, cognitive therapy, depression
A common assumption in psychotherapy research is that change is gradual and linear. Analyses often focus on group averages and pre-to-post change, with less emphasis on the rich information available in individual time course data. With the resurgence of interest in process research, a number of researchers have begun studying what happens between the beginning and end of therapy and nonlinear patterns of change. Analyses of the shape of symptom change can reveal whether change is gradual and monotonic or perhaps discontinuous and punctuated by substantial shifts in symptoms. Discontinuities in symptom ratings can be particularly informative because they mark points of transition and highlight segments of therapy in which important change processes can be isolated (A. M. Hayes, Laurenceau, & Cardaciotto, in press; A. M. Hayes, Laurenceau, Feldman, Strauss, & Cardaciotto, in press; Tang & DeRubeis, 1999).
Using individual time course data, we studied two types of discontinuity—a rapid early response1 and a spike (transient period of disturbance and apparent worsening)—in the course of an affectively charged cognitive therapy for depression. In this article, we review literature that suggests these two patterns might be useful markers of transition and predictors of treatment outcome. We then examined whether two cognitive variables, hope and cognitive–emotional processing, were associated with these points of transition. We illustrate how the analysis of discontinuities and patient narratives can be coupled to provide a unique window into the process of cognitive and emotional change across the course of therapy.
Rapid Early Response Pattern
In an influential article on patterns of change in eight clinical trials of cognitive therapy for depression, Ilardi and Craighead (1994) documented that the majority of symptom change occurred in the early sessions, after which there was little change. Group mean symptom time courses in each of the studies were used to calculate the percentage of change in depressive symptoms across the earliest sessions. Most of the total improvement occurred by the third week, with 60%–80% of the total decrease in depression occurring by Week 4 (Session 8, with two sessions per week). The pattern of findings was similar for the Beck Depression Inventory (BDI; Beck & Steer, 1987) and the Hamilton Rating Scale for Depression (Hamilton, 1960).
A rapid response also has been observed in pill placebo conditions (Grilo, Masheb, & Wilson, 2006; Stewart et al., 1998), behavioral family therapy and a nondirective support condition (Renaud et al., 1998), psychodynamic therapy (Crits-Christoph et al., 2001), and pharmacotherapy (Grilo et al., 2006). The rapid response predicts better outcomes in depression (e.g., Ilardi & Craighead, 1999; Renaud et al., 1998; Santor & Segal, 2001) and in difficult-to-treat clinical disorders, such as bulimia (e.g., Grilo et al., 2006; Wilson, Fairburn, Agras, Walsh, & Kraemer, 2002) and alcohol abuse (Breslin, Sobell, Sobell, Buchan, & Cunningham, 1997).
These findings are provocative and highlight the need to identify factors that predict early symptom reduction. Ilardi and Craighead (1994) proposed that hope might facilitate early change, as this variable is a potent process of change across psychotherapies (Frank, 1968; Grencavage & Norcross, 1990; Howard, Moras, Brill, Martinovich, & Lutz, 1996; Snyder, Ilardi, Michael, & Cheavens, 2000). Indeed, hopelessness does decrease early in cognitive therapy for depression (for a review, see Kuyken, 2004) and in behavioral activation therapy (Jacobson et al., 1996), and such change predicts better outcomes. The specific connection between hope and the rapid response is not yet clear, but early interventions such as providing a coherent treatment rationale, increasing engagement with the environment, and teaching skills to manage one’s emotions might engender hope in a disorder characterized by a crisis of hope (Snyder et al., 2000).
The Spike Pattern: Increased Variability and Disturbance Before Change
Another pattern of change receiving attention in dynamical systems theory, life transition research, and in exposure treatments for anxiety disorders is the opposite of a sudden improvement—a transient period of disturbance. The study of dynamical systems across a number of sciences is revealing an important marker of transition, called critical fluctuations (Kelso, 1995; Schiepek, Eckert, & Weihrauch, 2003; van der Maas & Molenaar, 1992), which appear as transient spikes and reflect system destabilization. When challenges to the current steady state of a system cannot be assimilated, system behavior often changes in nonlinear ways characterized by disturbance and increased variability before reorganization. This destabilization looks like a period of worsening but also opens the system to new information and exploration of potentially more adaptive associations and configurations. There is then an oscillation between old, less viable patterns and new, emerging patterns, until the system settles into a new dynamically stable state and variability decreases (Kelso, 1995; Thelen & Smith, 1994).
Critical fluctuations precede a range of developmental transitions, including motor, cognitive, and linguistic development (van Geert & van Dijk, 2002), as well as change in cognitive, affective, interpersonal, and personality dynamics in social and personality psychology (Vallacher, Read, & Nowak, 2002). A period of disturbance and emotional distress also can catalyze transformational change, such as dramatic shifts in meaning, life transition, posttraumatic growth (Baumeister, 1991; Linley & Joseph, 2004; Tedeschi & Calhoun, 2004), and even recovery from long-term substance abuse (W. R. Miller & C’de Baca, 2001). Evidence is accumulating to suggest that periods of disturbance are markers of system transition in a range of psychological phenomena and can reveal processes that facilitate and underlie the transition.
The Spike Pattern in Psychotherapy
A number of psychotherapy researchers have hypothesized that variability and destabilization before transition represents a general principle of change that can be applied to psychotherapy (Caspar & Berger, 2006; A. M. Hayes, Laurenceau, & Feldman, in press; A. M. Hayes & Strauss, 1998; Mahoney, 1991; Schiepek et al., 2003; Strauss et al., 2006). The clearest example of disturbance before change in psychotherapy occurs in exposure therapy for anxiety disorders, which is based on the assumption that anxiety must be increased to decrease it (Lang, 1984; Foa & Kozak, 1986; Foa, Huppert, & Cahill, 2006). Exposure interventions are designed to activate the fear network, decrease avoidance, and increase exposure to corrective information. This facilitates adaptive processing of disturbing emotional material (emotional processing). Exposure creates disturbance that is associated with physiological arousal (e.g., Lang, Melamed, & Hart, 1970) and “anxiety spikes” (Heimberg & Becker, 2002) during the exposure exercises and with a curvilinear (concave down) pattern of change over the course of therapy (Nishith, Resick, & Griffin, 2002).
Although exposure techniques have not been applied directly to the treatment of depression, the principles of exposure and disturbance before change have been hypothesized to apply. More than 2 decades ago, Rachman (1980) speculated that the principles of exposure and emotional processing might apply to the treatment of depression. Teasdale (1999) later presented an eloquent theoretical account of emotional processing in depression, and Moses and Barlow (2006) have highlighted important points of overlap in the psychopathology and treatment of anxiety disorders and depression. As with anxiety disorders, depression can be associated with avoidant emotion regulation styles, such as experiential avoidance (avoidance of disturbing emotions and experiences), hopelessness, disengagement and emotional blunting, and thought suppression (Alloy & Clements, 1998; Beevers, Wenzlaff, Hayes, & Scott, 1999; Grosse Holtforth, Grawe, Egger, & Berking, 2005; S. C. Hayes, Wilson, Gifford, Follette, & Strosahl, 1996; Rottenberg, 2005). Chronic avoidance of disturbing material can be associated with a rebound and intrusions of such material and with rumination (Lyubomirsky, & Nolen-Hoeksema, 1993; Wenzlaff & Luxton, 2003). Vacillation between avoidance and rumination can inhibit healthy processing of emotions and experiences (Brewin, Dalgleish, & Joseph, 1996; Greenberg, 2002; Greenberg & Watson, 2005) and maintain a perseverative loop that Teasdale and Barnard (1993) aptly call the depressive interlock. Thus, important tasks when treating depression are to reduce avoidance and rumination and to facilitate the therapeutic processing of disturbing emotions, cognitions, and other experiences. We construe these tasks as falling into the domain of exposure and creating disturbance to induce change.
Behavioral activation therapy is showing promise as a therapy that increases engagement with the environment and decreases patterns of avoidance and rumination, without addressing directly the cognitive content of depression or facilitating the processing of emotional material (Dimidjian et al., 2006). Mindfulness-based cognitive therapy (Segal, Williams, & Teasdale, 2002) reduces relapse by teaching participants to move into rather than away from negative emotions and to use acceptance-based strategies to engage but not become entangled in the disturbing material. These therapies for depression can be construed as applying some principles of exposure to reduce avoidance and increase the flow of new and corrective information. Although the form of the specific techniques differs from those used in exposure therapies for anxiety disorders, the function of the techniques is similar (A. M. Hayes, Beevers, Feldman, Laurenceau, & Perlman, 2005; A. M. Hayes & Feldman, 2004; Hopko, Lejeuz, Ruggiero, & Eifert, 2003).
Also consistent with the spirit of exposure, cognitive and emotion theorists in depression emphasize the importance of fully activating the cognitive, affective, behavioral, and somatic components of the depressive network, increasing tolerance to avoided emotions and thought, and increasing exposure to corrective information to facilitate cognitive restructuring and emotional processing (Beck, Freeman, Davis, & Associates, 2004; Greenberg & Safran, 1987; Guidano, 1991; A. M. Hayes et al., 2005; Ingram, Miranda, & Segal, 1998; Moses & Barlow, 2006; Power & Brewin, 1997; Samoilov & Goldfried, 2000; Teasdale, 1999). Schema-focused therapies (e.g., Beck et al., 2004; Young, Klosko, & Weishaar, 2003) and emotion-focused therapy for depression (Greenberg & Watson, 2005) apply these principles directly. Interventions of this sort challenge existing patterns of functioning in an affectively charged context and are consistent with the more general notion in dynamical systems and life transition research that creating disturbance can catalyze change. As such, they are likely to produce spike patterns of symptom change similar to those in exposure therapies for anxiety disorders. Such nonlinear patterns have not been examined in these affectively charged therapies for depression. In addition, the efficacy of behavioral activation therapy raises questions about whether facilitating this type of disturbance adds anything to the recovery process in depression (Longmore & Worrell, 2007).
The hypothesized mechanism of change in exposure and exposure-like interventions is increasing understanding and tolerance of one’s emotions and coming to new meanings, which has been referred to as emotional processing (Foa & Kozak, 1986; Lang, 1984; Teasdale, 1999), cognitive–emotional processing (Rachman, 2001), and experiencing (Greenberg, 2002; Klein, Mathieu-Coughlan, & Kiesler, 1986). We use the term cognitive–emotional processing to capture the combination of affective engagement and arousal, cognitive analysis, and meaning making.
Given the convergence across dynamical systems, life transition, and psychotherapy research on increased disturbance as an important marker of system transition, we examined the spike pattern (operationalized as a transient increase in depression) as a predictor of change in depression. We developed a therapy that distills and integrates components from behavioral activation, mindfulness-based, schema-focused, and emotion-focused therapies for depression with principles of exposure from the treatment of anxiety disorders. Because we use exposure as the central organizing principle, we consider this an exposure-based therapy. It is important to be clear that this is not a pure exposure therapy, and the content and specific intervention strategies differ somewhat from exposure for specific anxiety disorders. However, we apply the principles of exposure in that the therapy is designed to first decrease hopelessness, avoidance, and rumination (inhibitors of change) and then to promote activation and disturbance of the depressive network to facilitate cognitive–emotional processing.
We expected a rapid early response that was associated with hope, as patients learned stress management skills and increased approach behaviors and tolerance of negative emotions. During the exposure-activation phase of therapy, we predicted a spike in depression scores akin to anxiety spikes (Heimberg & Becker, 2002), as the depressive network was activated and corrective information was introduced. Consistent with theories of change in exposure therapies for anxiety disorders, cognitive–emotional processing was predicted to occur during this period of disturbance. We expected the rapid response and spike patterns to appear cubic in form across the course of therapy and to predict better treatment outcomes.
Method
Participants
All participants were recruited from the general phone line of a university-based clinic for the community. Callers who described symptoms of depression and who were interested in participating in the study were invited for an intake interview. All signed informed consent forms that were approved by the university’s internal review board, and informed consent was obtained before the initial intake interview. Prior to enrollment, participants were administered the Structured Clinical Interview for DSM-IV (First, Spitzer, Gibbon, & Williams, 1995). Those who met criteria for major depressive disorder and not for bipolar disorder, psychotic disorder, borderline personality disorder, current substance abuse, or imminent suicidality were included in the study. Those who were not included were referred back to the general clinic for treatment.
The sample was 66% female and was ethnically diverse (39% White, 51% Hispanic/Latino, 2% Asian American, 2% African American, and 6% other or mixed heritage). The mean age was 36.69 (SD = 11.33; range = 16 to 58). Most participants had some college education (90%) and were not married or cohabiting (73%). The median number of previous depressive episodes was 2.5. Nine of the 33 participants (27%) had been taking antidepressant medication for at least 6 months and did not discontinue the medication. Those receiving medication scored somewhat lower on pretreatment depression scores on the Modified Hamilton Rating Scale for Depression (MHRSD) than those not on medication, but this difference was not statistically significant, pretreatment MHRSD: F(1, 28)= 3.31, p = .08. Pretreatment depression scores did not differentiate those with and without a rapid response or a depression spike ( ps >.60). Those with and without medication also did not differ significantly on depression at Session 5, midtreatment, posttreatmant, or on any of the narrative coding variables (all ps < .20).
Of the 33 participants enrolled in therapy, 29 completed at least 12 of the 20 sessions and were considered completers. Those who completed 12 sessions attended at least 4 of the exposure-activation sessions and therefore, we reasoned, received an adequate dose to examine spikes and the cognitive–emotional processing variable. Four (12%) did not complete the therapy (all discontinued before Session 8). Of the noncompleters, 2 moved, 1 had a difficult pregnancy and could not attend therapy, and 1 discontinued for unknown reasons.
Therapists
Therapists were 16 masters-level doctoral students in clinical psychology at the University of Miami and two PhD-level therapists. All therapists received weekly individual and biweekly group supervision. Approximately half of the therapists were women (55%), and therapists varied in ethnicity (75% White, 20% Hispanic/Latino, and 5% Asian American).
Exposure-Based Cognitive Therapy (EBCT)
This therapy and the outcome data are described in more detail in previous reports (A. M. Hayes & Harris, 2000; A. M. Hayes et al., 2005), but we provide an overview of the content of the therapy to make clear how it was designed to induce a depression spike. The focus of the present report is on the process of change rather than on the efficacy of the therapy. EBCT consists of 20 to 24 sessions in three phases. Throughout the course of therapy, patients write narratives about their depression for 20 min each week before their next therapy session. This expressive writing task is designed to facilitate exposure to and processing of emotional material between sessions, as well as to assess the impact of sessions each week. By putting their experiences into words, patients can experience their emotions more deeply and evaluate and make meaning of them between sessions (cf. Greenberg & Angus, 2004; Pennebaker, 1997).
The goal of the stress management phase (Sessions 1–8) is to increase the resources and motivation for change and teach healthy lifestyle habits that can increase resilience after the depressive episode. Healthy habits related to sleep, eating, physical and social activity, emotion regulation, and problem solving are introduced. These skills take a while to incorporate into one’s life, so they are taught early and addressed throughout the course of therapy. Patients learn to identify avoidance and rumination and use breathing techniques and basic principles from mindfulness meditation (Segal et al., 2002) to disengage from these patterns. Meditation exercises are introduced gradually in the last four sessions of this phase to prepare patients to approach the disturbing emotions and thoughts in the exposure-activation phase of therapy. No direct cognitive change or affectively charged interventions are introduced in this early phase of therapy. This design begins to address Tang and DeRubeis’s (1999) argument that the rapid response is due to cognitive interventions introduced as early as Session 2 in most trials of cognitive therapy. This period of healthy lifestyle skills training also provided a within-subject contrast for the subsequent and more turbulent exposure-activation phase of therapy.
The exposure-activation phase of therapy (Sessions 9ȃ18) involves directly activating the depressive network by having patients describe in session the feelings of hopelessness and core negative view of self that arose during their most recent episode. They also reread the narratives that they wrote about their depression in the early weeks of therapy. Patients then explore the historical antecedents of their negative self-concept, which often increases the affective charge of the sessions. These exercises are designed to activate the depressive network of negative thoughts, affect, behavior, and even somatic responses. In this context, the negative beliefs are explored and questioned, inconsistent information is generated, and exercises are introduced to increase inconsistency and dissonance.
Of the exposure therapies for anxiety disorders, EBCT is most similar to those for posttraumatic stress disorder (Cohen, Mannarino, & Deblinger, 2006; Foa & Rothbaum, 1997; Levitt & Cloitre, 2005; Resick & Schnicke, 1993). Patients are encouraged to approach previously avoided material without engaging in strategies to reduce the negative affect and are guided to explore disturbing thoughts and feelings, consider inconsistent information, and develop new meaning. In depression, emotional processing cannot occur until hopelessness, avoidance, and rumination are reduced, which are goals of the first phase of therapy. Patients are guided to tolerate what Taylor and Rachman (1991) called a fear of sadness and to approach and explore core themes of hopelessness, defectiveness, and failure related to their depression. EBCT does not involve identifying specific automatic thoughts or cognitive distortions, and this approach includes less direct disputation and challenge of depressive thoughts than standard cognitive therapy for depression (Beck, Rush, Shaw, & Emery, 1979). Rather, EBCT involves more guided exploration of the depressive material as in schema-based cognitive therapies for personality disorders (Beck et al., 2004; Young, Klosko, & Weishaar, 2003), therapies that are also designed to facilitate broad-based change in maladaptive cognitive-affective-behavioral-somatic patterns. EBCT is affectively charged and teaches the functional aspects of emotions, but it is different from emotion-focused therapy for depression (Greenberg & Watson, 2005) in that it also teaches healthy lifestyle skills, specific emotion regulation skills to reduce avoidance and rumination, mindfulness meditation, and includes some direct cognitive change methods.
The third phase of the therapy (Sessions 19–posttreatment) is the consolidation and positive growth phase. Applying Bouton’s (2004) principles on the importance of strengthening new, adaptive learning that can compete with the old, maladaptive patterns, this phase includes exercises to solidify the new learning related to one’s hope and view of self. Patients are guided to actively develop a more balanced view of the self that includes both positive and negative characteristics, and they complete exercises to clarify their sense of meaning and purpose. After depression, there is often a fear of positive experiences, hope, and a positive view of self because of the potential disappointment that can follow. Patients learn to tolerate and reinforce positive material and maintain steadiness in the face of difficulties and positive experiences. They look to the future and set realistic goals for the upcoming months. In addition, the signs of relapse and relevant relapse prevention strategies are reviewed.
Measures
The MHRSD (I. W. Miller, Bishop, Norman, & Maddever, 1985) is a 25-item interview-based measure of depression severity. The MHRSD contains 17 items that assess the same symptoms as the original Hamilton Rating Scale for Depression (Hamilton, 1960). It correlates highly with the original scale and has acceptable reliability and validity (I. W. Miller et al., 1985). Items are summed to determine depression severity. The 17-item MHRSD was used to be consistent with other outcomes studies on the treatment of depression. The MHRSD includes items that assess anxiety and physiological arousal that are especially relevant to the assessment of depression spikes. The Hamilton depression scales have been used to study the rapid response and show similar patterns of results as the BDI (Ilardi & Craighead, 1994). Because the MHRSD was administered biweekly across the course of therapy, therapists administered the interview. An independent clinical assessor rated 20% of the tapes for each patient to assess interrater agreement on the MHRSD. Total scores were used in all analyses, and agreement between raters on total scores was high (intraclass correlation [ICC] = .92). Depression was assessed at the beginning of the session.
Narratives and Coding
Narratives.
Patients were asked to write narratives about their depression each week for 20 min before they arrived for their next appointment (Bolger, Davis, & Rafaeli, 2003; Pennebaker, 1997). They were asked to write about “their deepest thoughts and feelings related to their depression.” These narratives were designed to capture the impact of the therapy sessions over the week and also to facilitate processing over the course of therapy. All narratives were coded, but for the present study, we report the content of those that preceded the rapid early response and those that were written at the peak amplitude of the depression spike.
Coders.
The coders were three doctoral-level clinical psychology graduate students and one bachelor-level research assistant. The second author, Greg C. Feldman, was one of the coders but was blind to patient outcomes. Coders were trained to criterion with practice coding for approximately 10 hr. After reaching criterion agreement (ICC ≥.80), two coders rated each narrative. Coders were paired with each other an equal number of times. Weekly to biweekly meetings were held to review discrepancies and prevent rater drift.
Coding of narratives.
The Change and Growth Experiences Scale (CHANGE; A. M. Hayes, Feldman, & Goldfried, 2006) was used to code the content of the weekly narratives. CHANGE can be used to code narratives or therapy sessions. The coding system includes a range of variables that assess cognitive, affective, behavioral, somatic, and interpersonal aspects of functioning, as well as avoidance and cognitive–emotional processing. The variables relevant to the present study are hope and cognitive–emotional processing. Each variable is coded on a scale from 0 to 3 (0 = not present or very low, 1 = low, 2 = medium, 3 = high). Variables are not mutually exclusive and can co-occur. Intraclass correlations revealed that interrater agreement on all coding categories was good to excellent (ICC = .73 to .84). Because agreement was good, the ratings were averaged. Averaged ratings were used in the analyses.
Hope is the extent to which the person describes an expectation that the future will be better and progress can be made on problem areas, as well as a commitment to change. (Examples of Level 3: “I am beginning to see a way out of this black hole. I think I will make it.” and “At times I feel as if I am sinking, but today I can see my way out.”)
Cognitive–emotional processing is exploring and questioning issues and material related to depression, with some insight or perspective shift. Significant insight or a perspective shift often has emotional and behavioral manifestations. This category is designed to capture concepts that have been labeled as emotional processing, meaning making, benefit finding, cognitive change, and schema change. Thus, it contains aspects of both cognitive and affective change. However, affective arousal without some insight or perspective shift is not considered processing. Rumination, worry, and other perseverative thoughts are also not considered processing. An example of Level 3 processing is
I have been spending so much time trying to run away from myself that I have lost my compass. I have ended up with a man who is not good for me and in a job that is below me. I put up with the hurt because I thought I did not deserve better. It had eroded my spirit. I felt like a dead person. That realization makes me feel nauseous and disgusted, but I am now discovering my strength and potential. I had no idea what I was capable of.
In this example, there is disturbance manifested by affective arousal and even nausea, but there is also significant insight and a shift in perspective.
Overview of Analyses
In the first set of analyses, we examined the shape of change in depression symptoms assessed by the MHRSD. Hierarchical linear modeling (HLM; Raudenbush, Bryk, Cheong, & Congdon, 2004) was used to test linear, quadratic, and cubic patterns of symptom change. Hierarchical linear modeling considers both within-subject and between-subject variance in outcome and can be used to provide an overall picture of the shape of within-person symptom change over treatment.
In the second set of analyses, we examined the individual trajectories of depression symptoms to classify patients with and without a rapid early response and depression spike. We examined the rapid response and depression spike in hierarchical regression analyses as predictors of posttreatment depression, after controlling statistically for pretreatment depression. The phase design of the therapy allowed us to study the rapid response in the stress management phase (Sessions 1–8), the depression spike in the exposure-activation phase (Sessions 9–18), and depression in the consolidation and positive growth phase (Sessions 19–posttreatment).
The third set of analyses focused on understanding patient processes associated with the rapid early response and the depression spike by examining the content of the patient narratives written near these periods of transition. One-way analyses of variance were conducted to compare nonrapid and rapid responders on the extent of hope and cognitive–emotional processing in the narratives that immediately preceded Session 5. One-way analyses of variance also were conducted to compare those with and without a depression spike on the extent of hope and cognitive–emotional processing in the narratives that occurred at the peak of the depression spike (or at the median session of the spike, Session 11, for those without a spike).
In a previous report on this therapy (A. M. Hayes et al., 2005), the highest level of processing (peak processing) predicted more improvement in posttreatment depression, controlling statistically for depression at the beginning of the exposure phase (midtreatment). Therefore, in the present study, we examined whether depression spikes predicted the peak level of processing. To explore the possibility that peak processing might mediate the association between depression spikes and improvement in depression, spike status (presence or absence) and peak processing scores were entered simultaneously in a regression equation as predictors of postreatment depression, controlling statistically for midtreatment depression.
Results
The Shape of Change
As reported elsewhere (A. M. Hayes et al., 2005), hierarchical linear modeling analyses revealed that this therapy was associated with a significant linear decrease in depression, and analyses of change in pre–post BDI and MHDRS scores suggested large effect sizes. The focus of the present study is on the shape and process of change rather than on treatment outcome. We hypothesized that the overall shape of change would be cubic, that is, that there would be an early decrease in depression in the stress management phase of therapy, a period of increased disturbance during the exposure-activation phase, and a subsequent decrease in the consolidation phase. Linear, quadratic, and cubic parameters are typically highly correlated at the within-person level, so we generated normalized orthogonal polynomial coefficients to address the within-person multicollinearity between these terms (Hedeker, 2004). As predicted, there was not only a significant linear decrease in symptoms but also a significant cubic pattern of change (Table 1). The cubic pattern of change suggested that there might be a rapid early response and a subsequent period of disturbance marked by transient spikes in depression scores.
Table 1.
Parameter Estimates for Change in Depression (MHRSD) Symptoms Over Time
| Fixed effect | Coefficient | SE | t (28) |
|---|---|---|---|
| Intercept | 11.17 | 1.03 | 10.81*** |
| Linear MHRSD slope | −9.62 | 1.36 | −7.08*** |
| Quadratic MHRSD slope | −1.01 | 1.50 | −0.67 |
| Cubic MHRSD slope | −2.73 | 0.99 | −2.76** |
Note. MHRSD = Modified Hamilton Rating Scale for Depression, which was assessed biweekly across the course of therapy. Parameters are based on normalized orthogonal polynomial coefficients.
p < .01
p < .001
Rapid Early Response
We plotted and examined individual trajectories of depression scores over the course of therapy. Adapting the criteria of Ilardi and Craighead (1994), we classified patients as having a rapid early response if the MHRSD scores at Session 5 represented 60% or more of the total change from pretreatment to posttreatment for that individual. A graphic depiction of a rapid response is shown in Figure 1. The mean depression levels at pretreatment, Session 5, and posttreatment (see Table 2) suggest that 69% of the total change in depression occurred for the sample by Session 5 (pretreatment to Session 5 change = 8.51 MHRSD points, total change = 12.31 points). As displayed in Table 2, 41% of the patients had a rapid response. One-way analyses of variance revealed that nonrapid and rapid responders did not differ significantly at pretreatment depression, but rapid responders had significantly lower MHRSD scores at each assessment thereafter. However, chi-square analyses suggest that the two groups did not differ significantly on the number of patients who achieved remission (MHRSD ≤ 7 at posttreatment).
Figure 1.
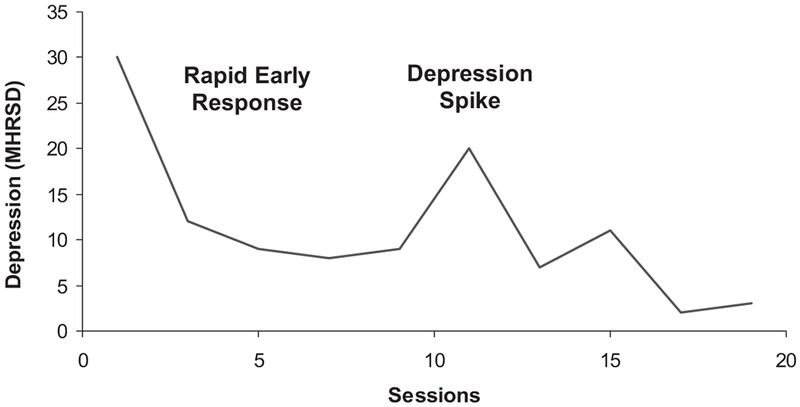
Modified Hamilton Rating Scale for Depression (MHRSD) scores for case example administered biweekly across the course of therapy. This case illustrates the rapid early response and depression spike patterns.
Table 2.
Summary of Rapid Early Response and Depression Spike Categorizations
| Variable | Nonrapid responder M (% or SD) |
Rapid responder M (% or SD) |
F or χ2 | p |
|---|---|---|---|---|
| n | 17 (59%) | 12 (41%) | ||
| Pre MHRSD | 19.30 (4.71) | 18.83 (7.02) | 0.05 | .83 |
| Session 5 MHRSD | 13.53 (6.40) | 7.17 (4.71) | 8.55 | .007 |
| Mid MHRSD | 15.29 (7.61) | 8.00 (4.59) | 8.72 | .04 |
| Post MHRSD | 8.05 (6.48) | 5.00 (2.83) | 4.44 | .045 |
| Number remitted (MHRSD ≤ 7) | 12/17 (71%) | 10/12 (83%) | χ2 = 0.18 | .67 |
| Early hope | .97 (0.99) | 1.75 (0.81) | 5.02 | .03 |
| Early cognitive/emotional processing | .73 (0.68) | 1.06 (0.95) | 1.15 | .30 |
| No depression spike M (% or SD) |
Depression spike M (% or SD) |
|||
| n | 11 (38%) | 18 (62%) | ||
| Pre MHRSD | 19.73 (7.16) | 18.72 (4.73) | 0.21 | .65 |
| Session 5 MHRSD | 13.18 (6.87) | 9.50 (6.04) | 2.29 | .14 |
| Mid MHRSD | 13.37 (7.45) | 11.61 (7.51) | 0.37 | .55 |
| Post MHRSD | 10.82 (7.56) | 4.83 (2.47) | 9.77 | .004 |
| Number remitted (MHRSD ≤ 7) | 5/11 (45.5%) | 17/18 (94.4%) | χ2 = 6.55 | .009 |
| Magnitude of increase | 1.90 (2.39) | 10.00 (3.61) | 43.27 | <.001 |
| Number of spikes | 0–3 | |||
| Median session first spike | 11 | |||
| Number of sessions completed | 20.91 (4.46) | 22.27 (3.14) | 0.94 | .34 |
| Hope at spike | 0.95 (0.93) | 0.67 (0.79) | 0.80 | .38 |
| Cognitive/emotional processing at spike | 0.23 (0.41) | 1.19 (0.86) | 12.10 | .002 |
| Peak processing | 1.46 (0.97) | 2.53 (0.58) | 13.73 | .001 |
Note. Analyses of variance were used to compare dimensional variables and chi-square for categorical variables. MHRSD = Modified Hamilton Rating Scale for Depression; Mid MHRSD = assessment after the stress management phase of therapy; peak processing = the highest level of processing.
Depression Spikes
When defining a depression spike, it is important to capture a fluctuation that is meaningful and does not represent random variation or a loss of treatment effect. We used the 7-point criterion that Tang and DeRubeis (1999) used in their classification of the sudden gain, which is a large decrease in depression symptoms (BDI ≥ 7 points) that does not reverse (increase by ≥ 50% of the gain). These authors used BDI scores, but the Hamilton depression scales also have been used to study rapid response and sudden gain patterns with similar results (Ilardi & Craighead, 1994; Vittengl, Clark, & Jarrett, 2005). In the present study, patients were classified as having a depression spike if their MHRSD scores in the exposure-activation phase increased by seven points or more and decreased by that much in the same phase of therapy. This pattern is depicted in Figure 1. The depression spike is similar to Heimberg and Becker’s (2002) anxiety spike and is the conceptual opposite of Tang and DeRubeis’s sudden gain.
Also shown in Table 2, 62% had a depression spike in the exposure-activation phase. In contrast, 35% (10 of 29) of the patients had a spike in the stress-management phase. In the early sessions, 9 (31%) patients had one spike, and 1 (4%) had two spikes. In the exposure-activation phase, 11 patients (37.9%) had no spikes, 13 (44.8%) had one spike, 4 (13.8%) had two spikes, and 1 (3.5%) had three spikes. A paired-sample t test showed that more spikes occurred in the exposure-activation phase than in the earlier phase, t(28) = 2.58, p = .02. The median session of the exposure-activation phase spike was Session 11. The mean magnitude of the increase for those with spikes in that period was 10 points (SD = 3.61, range = 7 to 17 points). One-way analyses of variance showed that those with and without a spike in the exposure-activation phase did not differ significantly on depression scores at the beginning or midpoint of therapy. However, those with depression spikes in the exposure-activation phase reported less depression at the end of therapy. Chi-square analyses showed that significantly more patients with a spike than without achieved remission of depression (MHRSD ≤ 7). All but 1 of those with spikes remitted. Those with and without spikes did not differ in the number of sessions completed.
Rapid Early Response and Depression Spikes as Predictors of Posttreatment Depression
Using hierarchical regression analyses, pretreatment depression scores were entered in Step 1 of the equation, and rapid response and depression spike (exposure-activation phase only) classifications were entered simultaneously in Step 2 as predictors of posttreatment depression. As seen in Table 3, having a rapid response and a depression spike contributed uniquely to the prediction of depression at the end of therapy. The results were similar when we examined continuous measures of early depression response (depression scores at Session 5) and the number of spikes (range = 0 to 3) as predictors of treatment outcome. In contrast, as seen in Table 4, spikes in the stress-management phase were associated with higher depression scores at the end of this phase (midtreatment) and were not associated with posttreatment outcome.
Table 3.
Summary of Hierarchical Regression Analyses of Symptom Patterns Predicting Posttreatment Depression Symptoms, Controlling for Pretreatment Symptoms
| Variable | B | SE | β | t | 95% CI for B | R2Δ | FΔ | df |
|---|---|---|---|---|---|---|---|---|
| Step 1 | .08 | 2.26 | 1, 28 | |||||
| Pre MHRSD | 0.28 | 0.19 | .28 | 1.50 | −0.10, 0.67 | |||
| Step 2 | .35 | 7.66 | 1, 26 | |||||
| Pre MHRSD | 0.23 | 0.15 | .22 | 1.47 | −0.09, 0.54 | |||
| Rapid response | −3.77 | 1.74 | −.33 | −2.17* | −7.35, −0.19 | |||
| Depression spike | −5.45 | 1.77 | −.47 | −3.08** | −9.10, −1.81 | |||
| Step 1 | .08 | 2.26 | 1, 28 | |||||
| Pre MHRSD | 0.28 | 0.19 | .28 | 1.50 | −0.10, 0.67 | |||
| Step 2 | .32 | 6.76 | 1, 26 | |||||
| Pre MHRSD | 0.12 | 0.16 | .12 | 0.72 | −0.22, 0.45 | |||
| Session 5 MHRSD | 0.37 | 0.15 | .42 | 2.58* | 0.08, 0.67 | |||
| Number of spikes | −2.31 | 1.14 | −.33 | −2.02* | −4.67, 0.05 |
Note. Depression spikes occur in the exposure–activation phase of therapy. MHRSD = Modified Hamilton Rating Scale for Depression.
p < .05.
p < .01.
Table 4.
Intercorrelations and Descriptive Statistics of Rapid Early Response, Depression Spikes, Narrative Coding, and Depression Scores
| Variable | 1 | 2 | 3 | 4 | 5 | 6 | 7 | 8 | 9 | 10 | 11 | 12 |
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Rapid response | — | |||||||||||
| 2. Session 5 MHRSD | −.49** | — | ||||||||||
| 3. Early hope | .40* | −.42* | — | |||||||||
| 4. Early processing | .20 | −.23 | .25 | — | ||||||||
| 5. Early depression spike | −.04 | .07 | .13 | .08 | — | |||||||
| 6. Exposure phase depression spike | .08 | −.28 | .07 | .15 | .17 | — | ||||||
| 7. Hope at spike | −.20 | −.11 | .08 | .01 | .03 | −.17 | — | |||||
| 8. Processing at spike | .17 | −.42* | .17 | .09 | .03 | .56** | .14 | — | ||||
| 9. Peak processing | .12 | −.27 | .28 | .23 | .25 | .58*** | .02 | .48** | — | |||
| 10. Pre MHRSD | −.04 | .26 | −.22 | .02 | .23 | −.09 | −.21 | −.18 | −.06 | — | ||
| 11. Mid MHRSD | −.49** | .73*** | −.49** | −.39* | .38* | −.12 | .12 | −.12 | −.02 | .30 | — | |
| 12. Post MHRSD | −.38* | .53** | −.45* | −.23 | .07 | −.52** | .11 | −.33 | −.37* | .28 | .52** | — |
| M | 10.90 | 1.36 | 0.83 | 1.09 | 1.10 | 2.12 | 19.41 | 12.28 | 7.10 | |||
| (SD) | 0, 1 | (6.50) | (1.03) | (0.77) | 0, 1 | 0, 1 | (0.99) | (0.98) | (0.91) | (5.79) | (7.40) | (5.73) |
Note. MHRSD = Modified Hamilton Rating Scale for Depression; Mid MHRSD = assessment after the stress management phase of therapy; Hope and processing at spike = hope and processing in the essays at the peak of the depression spike; Peak processing = the highest level of processing.
p < .05.
p < .01.
p < .001.
Narrative Codings Associated With the Rapid Early Response and Depression Spike
Because the rapid response and exposure-activation phase depression spikes predicted posttreatment outcome, we studied the narratives in the vicinity of these transition points. Table 4 summarizes the intercorrelations between the rapid response, depression spike, coding variables, and depression and also provides the descriptive statistics for these variables.
Rapid early response.
The narratives immediately before Session 5 were coded to capture what patients were writing about early in therapy. The Week 4 narratives were written when the healthy lifestyle skills were introduced. Mindfulness meditation had not yet been introduced. As shown in Table 2, rapid responders expressed more hope in these early narratives than did nonrapid responders, but these groups did not differ in cognitive–emotional processing.
Depression spike.
The exposure-activation phase was expected to be associated with a transient worsening of depressive symptoms and with more processing. We identified the sessions during which the depression spike occurred for each person. When patients had more than one spike, the narratives were sampled from the week at which depression scores were the highest (peak magnitude) in the first of the spikes. For those with a depression spike (n = 18), the median session of the spike was Session 11. For those without a spike (n = 11), the narrative from the median spike session (11) was sampled to maintain consistency. The median session falls in the period of therapy when therapists were activating the depressive network. Table 2 shows that those with depression spikes had narratives coded with higher cognitive–emotional processing than those without spikes, but the two groups did not differ in hope. The rapid response was not associated with later spikes, but it is interesting to note that less depression at Session 5 was associated with more processing at the spike (see Table 4).
Depression Spikes and Peak Levels of Processing
In an earlier study with this sample, A. M. Hayes et al. (2005) reported that the highest level of processing achieved during or after the exposure-activation phase of therapy (peak processing) predicted depression levels at the end of treatment, controlling statistically for midtreatment depression. Depression spikes in the present study tended to occur by Session 11, and the median peak processing scores occurred later at around Session 14. The peak levels of processing always followed the spike. We therefore examined whether depression spikes predicted later peak levels of processing in the narratives. Depression spikes were not only associated with more processing at the height of the disturbance, but a regression analysis showed that spikes also predicted the highest levels of processing that patients reached, β = 0.58, t(28) = 3.71, p = .001.
As seen in Table 4, depression spikes and peak processing scores were significantly correlated, and both were also significantly associated with posttreatment depression, thus meeting Baron and Kenny’s (1986) criteria to test for mediation. Peak processing was examined as a mediator of the association between spikes and outcome. In a hierarchical regression analysis, midtreatment depression scores were entered in Step 1, and depression spike and peak processing scores were entered simultaneously in Step 2 as predictors of posttreatment depression. Peak processing remained a significant predictor of outcome, β = −0.39, t(26) = −2.21, p = .04, confidence interval (CI) = −4.37 to −0.15, whereas spikes no longer did, β = −0.17, t(26) = −0.97, p = .34, CI = −3.70 to 1.33. This suggests that the association between depression spikes and outcome is mediated in part by peak level of processing in the narratives (Baron & Kenny, 1986; Holmbeck, 1997).
Discussion
We investigated two types of change in an EBCT for depression by intensively sampling patient process variables and studying individual-level trajectories of depression symptoms. As hypothesized, there was an overall cubic pattern of change in depression symptoms, which suggested an early decline in symptoms, a period of transient worsening of symptoms (i.e., a depression spike), and a further decrease in symptoms. Analyses of individual trajectories revealed that 41% of the sample experienced a rapid response, and 62% experienced at least one depression spike in the exposure-activation phase of therapy. Both patterns uniquely predicted less depression at the end of therapy, as did continuous measures of these two patterns— depression level at Session 5 and the number of depression spikes. In addition, the depression spike predicted the highest (peak) level of processing achieved. This transient symptom exacerbation was only associated with improvement when it occurred in the exposure-activation phase. Depression spikes that occurred earlier were instead associated with worse depression at midpoint and did not predict posttreatment outcomes.
The narratives that occurred in the segments of therapy during the rapid response and depression spike revealed that rapid responders expressed more hope in Session 4 narratives than did nonrapid responders. Those with depression spikes wrote narratives at the height of the arousal that were characterized by more cognitive–emotional processing than did those without a spike. Depression spikes also predicted the peak levels of processing, and the association between the spikes and outcome seemed to be mediated in part by the peak processing scores.
Our findings suggest two patterns of change: one that involves a steep decline of symptoms early in treatment (rapid response) and is associated with hope, and one that involves an increase in symptoms followed by a further decrease (depression spike) that is associated with more cognitive–emotional processing. Greenberg (2002) summarizes two types of change that provide a framework for understanding these two patterns. First-order change involves symptom reduction, improved coping, support, and stress reduction. Second-order change involves change in core cognitive-affective-behavioral-somatic patterns and a fundamental shift in perspective (Greenberg, 2002, p. 177), similar to the transformational change described in dynamical system theory, posttraumatic and adversarial growth, and dramatic life transition.
Indeed, the goals of the stress-management phase of EBCT are to stabilize rather than destabilize patients and are similar to those of first-order change. The skills are designed to energize and strengthen patients and reduce processes that inhibit change (hopelessness, avoidance, and rumination). As Ilardi and Craighead (1999) proposed, we found that early expressions of hope differentiated the narratives of the rapid and nonrapid responders. Neither hope nor the rapid response was associated with pretreatment levels of depression, which suggests that those who expressed more hope were not simply those who were less depressed at intake. Hope, which includes both the motivation for change and the belief that one can effect change (Snyder et al., 2000), occurred before direct cognitive change and affectively charged interventions were introduced. This design addresses to some extent the argument that the rapid response in cognitive therapy is due to early cognitive change interventions (Tang & DeRubeis, 1999). However, incorporating healthy lifestyle habits into one’s life is likely to involve some cognitive change, even if specific cognitive change interventions have not yet been introduced.
These findings are consistent with Howard et al.’s (1996) generic model of change in psychotherapy that includes remoralization, a facet of hope, in the first few sessions of most therapies. Change in hope also occurs early in cognitive therapy for depression (e.g., DeRubeis et al., 1990; Kuyken, 2004; Rush, Kovacs, Beck, Weissenburger, & Hollon, 1981). Jacobson et al. (1996) reported similar findings in behavioral activation therapy for depression, which like EBCT, does not include direct cognitive change interventions in the early sessions.
The consistent finding of early symptom reduction, even in intractable problems such as bulimia and substance abuse, is provocative. On one hand, as much as 60%–80% of the total symptom change occurs by Session 4 for a number of clinical disorders (e.g., Ilardi & Craighead, 1999; Grilo et al., 2006) and by about Session 5 with another early pattern of change, the sudden gain (Tang & DeRubeis, 1999; Tang, DeRubeis, Beberman, & Pham, 2005). On the other hand, the response rates for the best available treatments for depression are about 60%, and the relapse rates are still disturbingly high (Hollon, Thase, & Markowitz, 2002; Westen & Morrison, 2001). A consensus in the treatment of depression is that current treatments are not of sufficient duration and that more attention needs to be paid to the prevention of relapse and recurrence (Hollon et al., 2002). There is also increasing evidence that depression is more recurrent and chronic than previously realized (Judd et al., 1998). It is hard to imagine a four-session therapy for depression, which a literal interpretation of the rapid response and sudden gain research may imply. Moreover, most studies of the rapid response report that at least half of the patients do not experience a rapid response, and Vittengl et al. (2005) reported that as many as 24% to 47% of patients who experience a sudden gain have a later reversal (loss of ≥ 50% of the gain). Thus, we believe there is room for important symptom change after the early response and that this might be the second-order change described by Greenberg (2002).
Second-order change is likely to be more destabilizing than first-order change. The exposure-activation phase of EBCT was disturbing in that 62% of the sample experienced at least one period of transient symptom exacerbation (depression spike), and some as many as three spikes. Yet, as predicted, this turbulent period was associated with more cognitive–emotional processing in the narratives and with better posttreatment outcomes. Neither having a depression spike during the exposure-activation phase nor higher levels of processing was associated with levels of depression at intake or at midtreatment, but those with less depression at Session 5 had more processing in the narratives at the spike. This early change might facilitate later processing, but this is not yet clear, as the rapid response was not associated with later processing. Consistent with recent research on experiential therapy for depression (Missirlian, Toukmanian, Warwar, & Greenberg, 2005; Pos, Greenberg, Goldman, & Korman, 2003), it was arousal and processing later in therapy, rather than early on, that was most strongly associated with improvement at the end of therapy. This pattern of activation and processing is similar to that described in exposure therapies for anxiety disorders (Heimberg & Becker, 2002; Nishith et al., 2002) and in natural recovery from trauma (Gilboa-Schechtman & Foa, 2001).
It is important to note, however, that it is critical to consider the patient’s resources for undergoing this type of change and the timing of destabilizing interventions (Wiser & Arnow, 2001). For example, patients in the midst of significant negative life events, psychosis, suicidality, homicidality, or the symptoms of borderline personality disorder do not have the resources to undergo this sort of destabilizing change. First-order, incremental change can be very useful here, with a focus on stabilization rather than destabilization.
Rachman (1980) and Teasdale (1999) speculated some time ago that the principles of exposure and emotional processing might apply to the treatment of depression. Moses and Barlow (2006) pointed to the substantial overlap between the etiology and treatment of anxiety and depression, and they encouraged more research on common principles across these disorders. The present study is perhaps a step in this endeavor. We identified two patterns of symptom change in EBCT—an early decrease in depression symptoms associated with hope and a transient spike in depression symptoms associated with cognitive–emotional processing. The latter type of change looks remarkably similar to that in exposure therapies for anxiety disorders and in other types of change studied in dynamical systems, life transition, and posttraumatic growth research.
Limitations and Future Directions
The depression spike was associated with cognitive–emotional processing and is consistent with the proposition that affective arousal is important in second-order change. A next step is to investigate whether this sort of change facilitates a reconfiguration of the depressive network or the development of a new, more positive network that competes with the depressive network (Bouton, 2004; Foa et al., 2006; Teasdale, 1999), which has implications for relapse prevention. The third phase of EBCT is designed to develop and elaborate positive network elements related to hope, a sense of meaning and purpose, and a positive view of self. It is also designed to exercise and strengthen the hyporesponsive positive affect system (Watson, 2002). Facilitating this type of change might increase resilience in the face of challenge and reduce the risk of relapse and recurrence. An important test of whether inducing disturbance adds to the change process (Longmore & Worrell, 2007) will be to compare the process of change and long-term outcomes in EBCT with a therapy that facilitates more gradual and linear change, such as behavioral activation therapy (Martell, Addis, & Jacobson, 2001).
The design of this study allowed us to examine patterns of change in depression and the content of patient narratives in particular phases of treatment. In a sense, the phase design provides a within-person comparison condition, a strategy used by Tang and DeRubeis (1999) in their research on the sudden gain pattern of change. Because this was the first open trial in the treatment development process, we are developing measures of therapist adherence and competence but do not yet have data to support that the interventions were indeed delivered when intended and that the interventions actually constitute exposure. However, the data suggest that depression spikes occurred in the exposure-activation phase, as expected, and that cognitive–emotional processing occurred during this phase.
The frequent assessment of depression and the narrative methodology provided a window into the change process that is not possible with a simple pre-mid-posttreatment assessment design. A cubic pattern of change could be investigated, and individual symptom trajectories could be examined to reveal the rapid response and depression spike patterns. The narratives took only 20 min of patient time each week but provide a wealth of information on what is changing as patients go through the course of therapy. This method might capture “life as it is lived” (Bolger et al., 2003) more than self-report measures of automatic thought and dysfunctional attitudes that are not specific to the person and are often administered infrequently. The CHANGE coding system (A. M. Hayes et al., 2006) can quantify the content of the narratives and provide idiographic data. The frequent assessment and use of the narrative method allowed us to map the narrative content onto the indicators of transition—the rapid response and the depression spike—to begin to uncover what might be changing at these points.
A significant improvement in the study design would be to include multimethod measures of the change process, such as laboratory tasks from cognitive and affective science (e.g., Atchley, Ilardi, & Enloe, 2003; Gotlib & Neubauer, 2000; Nandrino, Dodin, Martin, & Henniaux, 2004). These measures could be conducted during the hypothesized periods of transition to track components of the depressive network and of a more adaptive, competing network (cf. Bouton, 2004; Foa et al., 2006). Physiological measures could be added during the exposure-activation phase to serve as a manipulation check of whether this phase is associated with arousal, as is the case in exposure therapies for anxiety disorders.
In conclusion, this study is part of a program of research on the roles of destabilization and cognitive–emotional processing in the treatment of depression. The sample size is small in this development phase, but we include intensive analyses of the change process and the use of individual- and group-level data. The therapy was delivered in a university-based clinic, so it is not clear whether the findings will generalize to other treatment settings and to samples that were excluded in this trial. The findings must be considered preliminary because this study did not include a control condition, and it is possible that a cubic shape of change may reflect the natural course of depression. This study sets the stage for the essential next step, a randomized clinical trial that includes a comparison group that promotes gradual linear change, assessment of depressive and competing networks, and the study of the processing of events and emotions over the follow-up period. There is much work to do, but it is an exciting time when general principles of change can be identified, especially principles that reflect the complex, nonlinear ways that patients might change in psychotherapy.
Acknowledgments
This research was conducted in part when Adele M. Hayes was at the University of Miami. This study was supported in part by National Institute of Mental Health Grant R21-MH62662 awarded to Adele M. Hayes. We thank William Galyardt, David Greenawalt, Melanie Harris, Jose Sandoval, Jennifer Strauss, and Barbara Wolfsdorf, and our research and therapist teams. We also thank all of the participants in this study.
Contributor Information
Adele M. Hayes, University of Delaware
Greg C. Feldman, Simmons College
Christopher G. Beevers, University of Texas at Austin
Jean-Philippe Laurenceau, University of Delaware.
LeeAnn Cardaciotto, University of Delaware.
Jamie Lewis-Smith, University of Miami.
References
- Alloy LB, & Clements CM (1998). Hopelessness theory of depression: Tests of the symptom component. Cognitive Therapy and Research, 22, 303–335. [Google Scholar]
- Atchley RA, Ilardi SS, & Enloe A (2003). Hemispheric asymmetry in the lexical processing of emotion: The effect of current and past depression. Brain and Language, 84, 105–119. [DOI] [PubMed] [Google Scholar]
- Baron RM, & Kenny DA (1986). The moderator-mediator variable distinction in social psychological research: Conceptual, strategic and statistical considerations. Journal of Personality and Social Psychology, 51, 1173–1182. [DOI] [PubMed] [Google Scholar]
- Baumeister RF (1991). Meanings of life. New York: Guilford Press. [Google Scholar]
- Beck AT, Freeman A, Davis DD, & Associates. (2004). Cognitive therapy of personality disorders. New York: Guilford Press. [Google Scholar]
- Beck AT, Rush AJ, Shaw BF, & Emery G (1979). Cognitive therapy of depression. New York: Wiley. [Google Scholar]
- Beck AT, & Steer RA (1987). Beck Depression Inventory: Manual. San Antonio, TX: Psychological Corporation. [Google Scholar]
- Beevers CG, Wenzlaff RM, Hayes AM, & Scott WD (1999). Depression and the ironic effects of thought suppression: Therapeutic strategies for improving mental control. Clinical Psychology: Science and Practice, 6, 133–148. [Google Scholar]
- Bolger N, Davis A, & Rafaeli E (2003). Diary methods: Capturing life as it is lived. Annual Review of Psychology, 54, 579–616. [DOI] [PubMed] [Google Scholar]
- Bouton ME (2004). Context and behavioral processes in extinction. Learning and Memory, 11, 485–494. [DOI] [PubMed] [Google Scholar]
- Breslin FC, Sobell MB, Sobell LC, Buchan G, & Cunningham CJ (1997). Toward a stepped care approach to treating problem drinkers: The predictive utility of within-treatment variables and therapist prognostic ratings. Addiction, 92, 1479–1489. [PubMed] [Google Scholar]
- Brewin CR, Dalgleish T, & Joseph S (1996). A dual representation theory of posttraumatic stress disorder. Psychological Review, 103, 670–686. [DOI] [PubMed] [Google Scholar]
- Caspar F, & Berger T (2006). Insight and cognitive psychology In Castonguay LG & Hill C (Eds.), Insight in psychotherapy (pp. 375–399). Washington, DC: American Psychological Association. [Google Scholar]
- Cohen JA, Mannarino AP, & Deblinger E (2006). Treating traumavand traumatic grief in children and adolescents. New York: Guilford Press. [Google Scholar]
- Crits-Christoph P, Connolly MB, Gallop R, Barber JP, Tu X, Gladis M, et al. (2001). Early improvement during manual-guided cognitive and dynamic psychotherapies predicts 16-week remission status. Journal of Psychotherapy Practice and Research, 10, 145–154. [PMC free article] [PubMed] [Google Scholar]
- DeRubeis RJ, Hollon SD, Evans MD, Garvey MJ, Grove WM, & Tuason VB (1990). How does cognitive therapy work? Cognitive change and symptom change in cognitive therapy and pharmacotherapy for depression. Journal of Consulting and Clinical Psychology, 58, 862–869. [DOI] [PubMed] [Google Scholar]
- Dimidjian S, Hollon SD, Dobson KS, Schmaling KB, Kohlenberg RJ, et al. (2006). Randomized trial of behavioral activation, cognitive therapy, and antidepressant medication in acute treatment of adults with major depression. Journal of Consulting and Clinical Psychology, 74, 658–670. [DOI] [PubMed] [Google Scholar]
- First MB, Spitzer RL, Gibbon M, & Williams JBW (1995). Structured Clinical Interview for DSM–IV Axis I Disorders: Patient Edition (SCID-I/P; Version 2.0). New York: Biometrics Research Department, New York State Psychiatric Institute. [Google Scholar]
- Foa EB, Huppert JD, & Cahill SP (2006). Emotional processing theory: An update In Rothbaum BO (Ed.), Pathological anxiety: Emotional processing in etiology and treatment (pp. 3–24). New York: Guilford Press. [Google Scholar]
- Foa EB, & Kozak MJ (1986). Emotional processing of fear: Exposure to corrective information. Psychological Bulletin, 99, 20–35. [PubMed] [Google Scholar]
- Foa EB, & Rothbaum BO (1997). Treating the trauma of rape. New York: Guilford Press. [Google Scholar]
- Frank J (1968). The role of hope in psychotherapy. International Journal of Psychiatry, 5, 383–395. [PubMed] [Google Scholar]
- Gilboa-Schechtman E, & Foa EB (2001). Patterns of recovery after trauma: Individual differences and trauma characteristics. Journal of Abnormal Psychology, 110, 392–400. [DOI] [PubMed] [Google Scholar]
- Gotlib IH, & Neubauer DL (2000). Information-processing approaches to the study of cognitive biases in depression In Johnson SL, Hayes AM, Field TM, Schneiderman N, & McCabe PM (Eds.), Stress, coping, and depression (pp. 117–143). Mahwah, NJ: Erlbaum. [Google Scholar]
- Greenberg LS (2002). Integrating an emotion-focused approach to treatment in psychotherapy integration. Journal of Psychotherapy Integration, 12, 154–189. [Google Scholar]
- Greenberg LS, & Angus L (2004). The contributions of emotion processes to narrative change in psychotherapy: A dialectical constructivist approach In Angus L & McLeod J (Eds.), Handbook of narrative psychotherapy (pp. 331–349). Thousand Oaks, CA: Sage. [Google Scholar]
- Greenberg LS, & Safran JD (1987). Emotion in psychotherapy: Affect, cognition, and the process of change. New York: Guilford Press. [Google Scholar]
- Greenberg LS, & Watson J (2005). Emotion-focused therapy of depression. Washington. DC: American Psychological Association. [Google Scholar]
- Grencavage LM, & Norcross JC (1990). Where are the commonalities among therapeutic common factors? Professional Psychology: Research and Practice, 5, 372–378. [Google Scholar]
- Grilo CM, Masheb RM, & Wilson TG (2006). Rapid response to treatment for binge eating disorder. Journal of Consulting and Clinical Psychology, 74, 602–613. [DOI] [PubMed] [Google Scholar]
- Grosse Holtforth M, Grawe K, Egger D, & Berking M (2005). Reducing the dreaded: Change of avoidance motivation in psychotherapy. Psychotherapy Research, 15, 261–271. [DOI] [PubMed] [Google Scholar]
- Guidano VF (1991). Affective change events in a cognitive therapy system approach In Safran JD & Greenberg LS (Eds.), Emotion, psychotherapy and change (pp. 50–80). New York: Guilford Press. [Google Scholar]
- Hamilton M (1960). Development of a rating scale for depression. Journal of Neurology, Neurosurgery, and Psychiatry, 23, 56–62. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM, Beevers C, Feldman G, Laurenceau J-P, & Perlman CA (2005). Avoidance and emotional processing as predictors of symptom change and positive growth in an integrative therapy for depression. International Journal of Behavioral Medicine, 12, 111–122. [DOI] [PubMed] [Google Scholar]
- Hayes AM, & Feldman GC (2005). Clarifying the construct of mindfulness in the context of emotion regulation and the process of change in therapy. Clinical Psychology: Science and Practice, 11, 255–262. [Google Scholar]
- Hayes AM, Feldman GC, & Goldfried MR (2006). The Change and Growth Experiences Scale: A measure of insight and emotional processing In Castonguay LG & Hill C (Eds.), Insight in psychotherapy (pp. 231–253). Washington, DC: American Psychological Association. [Google Scholar]
- Hayes AM, & Harris MS (2000). The development of an integrative treatment for depression In Johnson S, Hayes AM, Field T, Schneiderman N, & McCabe P (Eds.), Stress, coping, and depression (pp. 291–306). Mahwah, NJ: Erlbaum. [Google Scholar]
- Hayes AM, Laurenceau J-P, & Cardaciotto L (in press). Methods for capturing the process of change In Nezu AM & Nezu CM (Eds.), Evidence-based outcome research: A practical guide to conducting randomized clinical trials for psychosocial interventions. New York: Oxford University Press. [Google Scholar]
- Hayes AM, Laurenceau J-P, & Feldman GC, Strauss JL, & Cardaciotto LA (in press). Change is not always linear: The study of nonlinear and discontinuous patterns of change in psychotherapy. Clinical Psychology Review. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hayes AM, & Strauss JL (1998). Dynamic systems theory as a paradigm for the study of change in psychotherapy: An application to cognitive therapy for depression. Journal of Consulting and Clinical Psychology, 66, 939–947. [DOI] [PubMed] [Google Scholar]
- Hayes SC, Wilson KW, Gifford EV, Follette VM, & Strosahl K (1996). Emotional avoidance and behavioral disorders: A functional dimensional approach to diagnosis and treatment. Journal of Consulting and Clinical Psychology, 64, 1152–1168. [DOI] [PubMed] [Google Scholar]
- Hedeker D (2004). An introduction to growth modeling In Kaplan D (Ed.), The Sage handbook of quantitative methodology for the social sciences (pp. 215–234). Thousand Oaks, CA: Sage. [Google Scholar]
- Heimberg RG, & Becker RE (2002). Cognitive-behavioral group treatment for social phobia: Basic mechanisms and clinical applications. New York: Guilford Press. [Google Scholar]
- Hollon SD, Thase ME, & Markowitz JC (2002). Treatment and prevention of depression. Psychological Science in the Public Interest, 3, 39–77. [DOI] [PubMed] [Google Scholar]
- Holmbeck GN (1997). Toward terminological, conceptual, and statistical clarity in the study of mediators and moderators: Examples from the child-clinical and pediatric psychology literatures. Journal of Consulting and Clinical Psychology, 65, 599–610. [DOI] [PubMed] [Google Scholar]
- Hopko DR, Lejeuz CW, Ruggiero KJ, & Eifert GH (2003). Contemporary behavioral activation treatments for depression: Procedures, principles, and progress. Clinical Psychology Review, 23, 699–717. [DOI] [PubMed] [Google Scholar]
- Howard KI, Moras K, Brill PL, Martinovich Z, & Lutz W (1996). Evaluation of psychotherapy: Efficacy, effectiveness, and patient progress. American Psychologist, 51, 1059–1064. [DOI] [PubMed] [Google Scholar]
- Ilardi SS, & Craighead WE (1994). The role of nonspecific factors in cognitive–behavior therapy for depression. Clinical Psychology: Science and Practice, 1, 138–156. [Google Scholar]
- Ilardi SS, & Craighead WE (1999). Rapid early response and nonspecific factors in cognitive-behavior therapy for depression: A reply to Tang and DeRubeis. Clinical Psychology: Science and Practice, 6, 295–299. [Google Scholar]
- Ingram RE, Miranda J, & Segal ZV (1998). Cognitive vulnerability to depression. New York: Guilford Press. [Google Scholar]
- Jacobson NS, Dobson KS, Truax PA, Addis ME, Koerner K, Gollan JK, et al. (1996). A component analysis of cognitive–behavioral treatment for depression. Journal of Consulting and Clinical Psychology, 64, 295–305. [DOI] [PubMed] [Google Scholar]
- Judd LL, Akiskal HS, Maser JD, Zeller PH, Endicott J, Coryell W, et al. (1998). A prospective 12-year study of subsyndromal and syndromal depressive symptoms in unipolar major depressive disorders. Archives of General Psychiatry, 55, 694–700. [DOI] [PubMed] [Google Scholar]
- Kelso JAS (1995). Dynamic patterns. Cambridge, MA: MIT Press. [Google Scholar]
- Klein MH, Mathieu-Coughlan P, & Kiesler DJ (1986). The Experiencing Scales In Greenberg LS & Pinsof WM (Eds.), The psychotherapeutic process: A research handbook (pp. 21–71). New York: Guilford Press. [Google Scholar]
- Kuyken W (2004). Cognitive therapy outcome: The effects of hopelessness in a naturalistic outcome study. Behaviour Research and Therapy, 42, 631–646. [DOI] [PubMed] [Google Scholar]
- Lang PJ (1984). Cognition in emotion: Concept and action In Izard CE, Kagan J, & Zajonc RB (Eds.), Emotions, cognition, and behavior (pp. 192–226). Cambridge, England: Cambridge University Press. [Google Scholar]
- Lang PJ, Melamed BG, & Hart J (1970). A psychophysiological analysis of fear modification using an automated desensitization procedure. Journal of Abnormal Psychology, 76, 220–234. [DOI] [PubMed] [Google Scholar]
- Levitt JT, & Cloitre M (2005). A clinician’s guide to STAIR/MPE: Treatment for PTSD related to childhood sexual abuse. Cognitive Behavioral Practice, 12, 40–52. [Google Scholar]
- Linley PA, & Joseph S (2004). Positive change following trauma and adversity: A review. Journal of Traumatic Stress, 17, 11–21. [DOI] [PubMed] [Google Scholar]
- Longmore RJ, & Worrell M (2007). Do we need to challenge thoughts in cognitive behavioral therapy? Clinical Psychology Review, 27, 173–187. [DOI] [PubMed] [Google Scholar]
- Lyubomirsky S, & Nolen-Hoeksema S (1993). Self-perpetuating properties of dysphoric rumination. Journal of Personality and Social Psychology, 65, 339–349. [DOI] [PubMed] [Google Scholar]
- Mahoney MJ (1991). Human change processes: The scientific foundations of psychotherapy. New York: Basic Books. [Google Scholar]
- Martell CR, Addis ME, & Jacobson NS (2001). Depression in context: Strategies for guided action. New York: W. W. Norton. [Google Scholar]
- Miller IW, Bishop SB, Norman WH, & Maddever H (1985). Modified Hamilton Rating Scale for Depression: Reliability and validity. Psychiatry Research, 14, 131–142. [DOI] [PubMed] [Google Scholar]
- Miller WR, & C’de Baca J (2001). Quantum change: When epiphanies and sudden insights transform ordinary lives. New York: Guilford Press. [Google Scholar]
- Missirlian TM, Toukmanian SG, Warwar SH, & Greenberg LS (2005). Emotional arousal, client perceptual processing, and working alliance in experiential psychotherapy for depression. Journal of Consulting and Clinical Psychology, 73, 861–871. [DOI] [PubMed] [Google Scholar]
- Moses EB, & Barlow DH (2006). A new unified treatment approach for emotional disorders based on emotion science. Current Directions in Psychological Science, 15, 146–150. [Google Scholar]
- Nandrino JL, Dodin V, Martin P, & Henniaux M (2004). Emotional information processing in first and recurrent major depressive episodes: An event-related potentials study. Journal of Psychiatric Research, 38, 475–484. [DOI] [PubMed] [Google Scholar]
- Nishith P, Resick PA, & Griffin MG (2002). Pattern of change in prolonged exposure and cognitive-processing therapy for female rape victims with posttraumatic stress disorder. Journal of Consulting and Clinical Psychology, 70, 880–886. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pennebaker JW (1997). Writing about emotional experiences as a therapeutic process. Psychological Science, 8, 162–166. [Google Scholar]
- Pos AE, Greenberg LS, Goldman RN, & Korman LM (2003). Emotional processing during experiential treatment of depression. Journal of Consulting and Clinical Psychology, 71, 1007–1016. [DOI] [PubMed] [Google Scholar]
- Power M, & Brewin CR (Eds.). (1997). The transformation of meaning in psychological therapies: Integrating theory and practice. Chichester, England: Wiley. [Google Scholar]
- Rachman S (1980). Emotional processing. Behaviour Research and Therapy, 18, 51–60. [DOI] [PubMed] [Google Scholar]
- Rachman S (2001). Emotional processing, with special reference to post-traumatic stress disorder. International Review of Psychiatry, 13, 164–171. [Google Scholar]
- Raudenbush S, Bryk A, Cheong YF, & Congdon R (2004). HLM 6: Hierarchical linear and nonlinear modeling. Lincolnwood, IL: Scientific Software International. [Google Scholar]
- Renaud J, Brent DA, Baugher M, Birmaher B, Kolko DJ, & Bridge J (1998). Rapid response to psychosocial treatment for adolescent depression: A two-year follow-up. Journal of the American Academy of Child & Adolescent Psychiatry, 37, 1184–1191. [DOI] [PubMed] [Google Scholar]
- Resick PA, & Schnicke MK (1993). Cognitive processing therapy for rape victims: A treatment manual. Newbury Park, CA: Sage. [Google Scholar]
- Rottenberg J (2005). Mood and emotion in major depression. Current Directions in Psychological Science, 14, 167–170. [Google Scholar]
- Rush AJ, Kovacs M, Beck AT, Weissenburger J, & Hollon SD (1981). Differential effects of cognitive therapy and pharmacotherapy on depressive symptoms. Journal of Affective Disorders, 3, 221–229. [DOI] [PubMed] [Google Scholar]
- Samoilov A, & Goldfried MR (2000). Role of emotion in cognitive–behavior therapy. Clinical Psychology: Science and Practice, 7, 373–385. [Google Scholar]
- Santor DA, & Segal ZV (2001). Predicting symptom return from rate of symptom reduction in cognitive-behavior therapy for depression. Cognitive Therapy and Research, 25, 117–135. [Google Scholar]
- Schiepek G, Eckert H, & Weihrauch S (2003). Critical fluctuations and clinical change: Data-based assessment in dynamic systems. Constructivism in the Human Sciences, 8, 57–84. [Google Scholar]
- Segal ZV, Williams JMG, & Teasdale JD (2002). Mindfulness-based cognitive therapy for depression: A new approach to preventing relapse. New York: Guilford Press. [Google Scholar]
- Snyder C, Ilardi S, Michael S, & Cheavens J (2000). Hope theory: Updating a common process for psychological change In Snyder CR & Ingram RE (Eds.), Handbook of psychological change: Psychotherapy processes and practices for the 21st century (pp. 128–153). New York: Wiley. [Google Scholar]
- Stewart JW, Quitkin FM, McGrath PJ, Amsterdam J, Fava M, Fawcett J, et al. (1998). Use of pattern analysis to predict differential relapse of remitted patients with major depression during 1 year of treatment with fluoxetine or placebo. Archives of General Psychiatry, 55, 334–343. [DOI] [PubMed] [Google Scholar]
- Strauss JL, Hayes AM, Johnson SL, Newman CF, Brown GK, Barber JP, et al. (2006). Early alliance, alliance ruptures, and symptom change in a nonrandomized trial of cognitive therapy for avoidant and obsessive–compulsive personality disorders. Journal of Consulting and Clinical Psychology, 74, 337–345. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tang TZ, & DeRubeis RJ (1999). Reconsidering rapid early response in cognitive–behavioral therapy for depression. Clinical Psychology: Science and Practice, 6, 283–288. [DOI] [PubMed] [Google Scholar]
- Tang TZ, DeRubeis RJ, Beberman R, & Pham T (2005). Cognitive changes, critical sessions, and sudden gains in cognitive–behavioral therapy for depression. Journal of Consulting and Clinical Psychology, 73, 168–172. [DOI] [PubMed] [Google Scholar]
- Taylor S, & Rachman SJ (1991). Fear of sadness. Journal of Anxiety Disorders, 5, 375–381. [Google Scholar]
- Teasdale JD (1999). Emotional processing, three modes of mind, and the prevention of relapse in depression. Behaviour Research and Therapy, 37, S53–S78. [DOI] [PubMed] [Google Scholar]
- Teasdale JD, & Barnard PJ (1993). Affect, cognition and change: Remodeling depressive thought. Hove, England: Erlbaum. [Google Scholar]
- Tedeschi RG, & Calhoun LG (2004). Posttraumatic growth: Conceptual foundations and empirical evidence. Psychological Inquiry, 15, 1–18. [Google Scholar]
- Thelen E, & Smith LB (1994). A dynamic systems approach to the development of cognition and action. Cambridge, MA: MIT Press. [Google Scholar]
- Vallacher RR, Read SJ, & Nowak A (2002). The dynamical perspective in personality and social psychology. Personality and Social Psychology Review, 6, 264–273. [Google Scholar]
- van der Maas H, & Molenaar P (1992). A catastrophe-theoretical approach to cognitive development. Psychological Review, 99, 395–417. [DOI] [PubMed] [Google Scholar]
- van Geert P, & van Dijk M (2002). Focus on variability: New tools to study intra-individual variability in developmental data. Infant Behavior mand Development, 25, 340–374. [Google Scholar]
- Vittengl JR, Clark LA, & Jarrett RB (2005). Validity of sudden gains in acute phase treatment of depression. Journal of Consulting and Clinical Psychology, 73, 173–182. [DOI] [PubMed] [Google Scholar]
- Watson D (2002). Positive affectivity: The disposition to experience pleasurable emotional states In Snyder CR & Lopez SJ (Eds.), The handbook of positive psychology (pp. 106–119). New York: Oxford University Press. [Google Scholar]
- Wenzlaff RM, & Luxton DD (2003). The role of thought suppression in depressive rumination Cognitive Therapy and Research, 27, 293–308. [Google Scholar]
- Westen D, & Morrison K (2001). A multidimensional meta-analysis of treatments for depression, panic, and generalized anxiety disorder: An empirical examination of the status of empirically supported therapies. Journal of Consulting and Clinical Psychology, 69, 875–899. [PubMed] [Google Scholar]
- Wilson GT, Fairburn CG, Agras WS, Walsh BT, & Kraemer H (2002). Cognitive–behavioral therapy for bulimia nervosa: Time course and mechanisms of change. Journal of Consulting and Clinical Psychology, 70, 267–274. [PubMed] [Google Scholar]
- Wiser S, & Arnow B (2001). Emotional experiencing: To facilitate or regulate? Journal of Clinical Psychology: In session, 57, 157–168. [DOI] [PubMed] [Google Scholar]
- Young JE, Klosko JS, & Weishaar ME (2003). Schema therapy: A practitioner’s guide. New York: Guilford Press. [Google Scholar]


