Abstract
Tarlov cysts are extradural meningeal cysts with collections of cerebrospinal fluid within the nerve sheath. These cysts are uncommon but tend to present more often in women. Symptomatic Tarlov cysts can lead to a variety of neurologic symptoms and painful conditions, including chronic pelvic pain. There is no consensus regarding the best treatment for symptomatic cysts. Surgical management has high rates of complication, including chronic pain, but better long-term results for symptom and cyst resolution. We describe a patient who developed worsening pelvic pain and lumbar radiculopathy after surgical management of her Tarlov cysts. Medication failed to relieve the pain, as did a variety of other procedures, before the patient ultimately received significant pain relief from high-frequency spinal cord stimulation. This case may provide guidance for physicians when managing patients suffering from symptomatic Tarlov cysts, or worsening pain symptoms after surgical management of these cysts.
Keywords: Pelvic pain, Chronic pain, Tarlov cyst, Spinal cord stimulator
Highlights
-
•
Tarlov cysts are an uncommon condition that presents more often in women.
-
•
Symptomatic cysts can lead to neurologic symptoms and painful conditions including chronic pelvic pain.
-
•
Surgery for symptomatic cysts is associated with high complication rates.
-
•
Patients who develop pain after Tarlov cyst surgery may benefit from spinal cord stimulation.
-
•
Spinal cord stimulation can be beneficial for chronic pelvic pain.
1. Introduction
Tarlov cysts are perineural fluid-filled sacs that are usually found in the lumbosacral spine around the junction of peripheral nerve roots and the respective dorsal root ganglia. The cysts are extradural meningeal cysts with collections of cerebrospinal fluid (CSF) within the nerve root sheath [1]. Tarlov cysts are found in roughly 1%–5% of the general population. [2,3]. Interestingly, some studies have demonstrated that women account for 59%–70% of cases [2,4]. Symptomatic Tarlov cysts are rare but can sometimes grow in size and compress adjacent nerve root structures, leading to localized or radicular pain, bowel and bladder symptoms, or other neurological sequelae. The most common presenting symptoms are back pain, pelvic pain, perineal pain, lumbar radiculopathy, or bowel/bladder symptoms. These are generally exacerbated by maneuvers that raise the CSF pressure such as standing, coughing, sneezing, or straining to void or defecate. Diagnosis is generally done with imaging and magnetic resonance imaging (MRI) is the modality of choice.
Tarlov cysts were first described by Tarlov in 1938 as an incidental finding during an autopsy [5]. Since then a variety of surgical and non-surgical interventions have been described for the treatment of Tarlov cysts. Unfortunately, there is a high rate of complications associated with surgical treatment of these cysts including hemorrhage, neurological deficit, CSF leak, infection, chronic pain, and cyst recurrence. A systematic review of surgical and non-surgical management of Tarlov cysts demonstrated a 21% and 12.47% complication rate respectively. There was a higher rate of transient sciatica, CSF-related complications, and bladder/bowel complications. Interestingly, both groups reported symptomatic improvement in 83.5% of patients. Transient exacerbation of symptoms and cyst recurrence was noted to be higher in non-surgically managed groups, suggesting surgical management is associated with higher postprocedural complication rates but better long-term efficacy for symptoms and cyst resolution [6]. Given the rarity of the condition and the high complication rates associated with surgical management, there is currently no consensus regarding the best treatment for patients who are symptomatic.
We describe a patient who had a longstanding history of chronic pelvic pain secondary to multiple sacral Tarlov cysts. She underwent surgery for her condition, but it worsened her symptoms and the patient ultimately obtained relief with the use of a high-frequency spinal cord stimulator (SCS).
2. Case Description
The patient was a 66-year-old woman with a longstanding history of chronic pelvic pain secondary to multiple large Tarlov cysts affecting the S1-S4 nerve roots. She had attempted medication management with acetaminophen, NSAIDs, and neuropathic pain medications. She had also undergone a series of epidural steroid injections and a trial of superior hypogastric plexus blocks but obtain minimal relief with these. She ultimately had surgery for the removal of the Tarlov cysts as well as sacral lamina reconstruction (Fig. 1). However, the patient's surgery resulted in worsening of her chronic pelvic pain, and also produced new-onset back pain and lumbar radiculopathy down both legs. The patient reported constant debilitating back and pelvic pain with intermittent stabbing and burning pain in her legs. Her worsening symptoms were uncontrolled with continued medication management as well as a repeat series of epidural steroid injections.
Fig. 1.

Lumbosacral MRI demonstrating post-surgical changes after the patient's initial surgery.
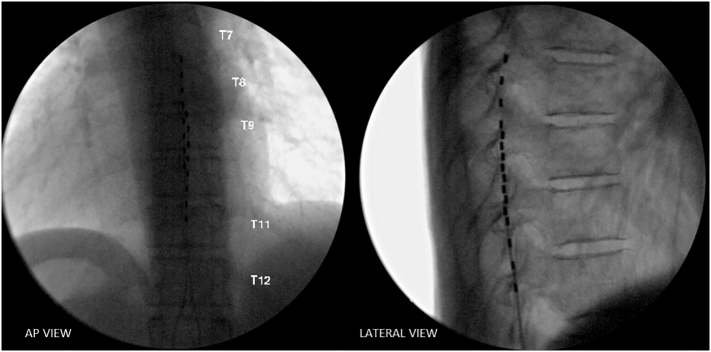
Given that the patient's worsening symptoms were unrelieved with both medication management and interventional pain procedures, we tried high-frequency spinal cord stimulation for her worsening pain and new-onset radiculopathy. The patient was counseled regarding the risks and benefits of the procedure and elected to proceed. A spinal cord stimulator lead was introduced into the epidural space and advanced to the superior endplate of T8. A second lead was placed at the superior endplate of T9 (Fig. 2).
Fig. 2.
Fluoroscopic imaging demonstrating SCS lead placement in the posterior epidural space at the superior levels of T8 and T9.
The patient presented for follow-up after the procedure and reported significant improvement in her symptoms. She noted that the use of SCS had resulted in a 90% improvement of her back pain, a 95% improvement in her pelvic pain, and >50% improvement in her radiculopathy. Additionally, she reported she was much more active and was able to decrease her medication use with the pain relief she obtained from spinal cord stimulation.
3. Discussion
Tarlov cysts can be a challenging condition to recognize and diagnose given the rarity of the condition. Although these cysts most commonly affect the sacral nerve roots, they have been found in lumbar, thoracic, and cervical regions as well. The condition is generally asymptomatic. However, a small percentage of patients may demonstrate symptoms related to nerve root compression. Tarlov cysts tend to expand over time and can cause nerve root irritation, leading to pain or other neurological disturbances.
There is no consensus on the optimal management of symptomatic Tarlov cysts. Percutaneous cyst drainage is a nonsurgical intervention has been used to treat this condition [3]. This treatment is only temporary though, as cysts tend to gradually reform and symptoms recur. In addition to percutaneous drainage, one study has demonstrated that cyst aspiration with the placement of fibrin glue can prevent recurrence of the cysts. However, these patients are also at significant risk for postprocedural aseptic meningitis [7].
Surgical treatment of symptomatic cysts varies and can involve complete cyst removal with excision of the affected posterior root and ganglion, decompressive laminectomy, cyst wall resection, and cyst fenestration [[8], [9], [10], [11]]. The success and complication rates vary greatly by procedure. Again, there is no consensus regarding when surgical management for Tarlov cysts is warranted, though one study suggested that cysts larger than 1.5 cm with associated radicular pain or bowel/bladder dysfunction may benefit the most from surgical intervention [10].
We recommend that patients presenting with symptomatic Tarlov cysts diagnosed by imaging should initially undergo conservative management with medication management, including acetaminophen, nonsteroidal anti-inflammatory drugs, and neuropathic pain medications such as gabapentin. Additionally, patients may respond to interventional pain procedures such as epidural steroid injections. Surgery should be reserved for patients who fail conservative management, given the high complication rates.
We would also like to comment on the success of spinal cord stimulation in this patient. SCS has been proven to be effective for treating intractable neuropathic pain such as lumbar radiculopathy and post-laminectomy syndrome [[12], [13], [14]]. There is also growing evidence that SCS can even be helpful for treating debilitating chronic visceral pelvic pain [15]. We believe this case is of importance as it describes the complicated management of patients with symptomatic Tarlov cysts who ultimately fail to respond to conservative therapy. We also describe the use of SCS in this patient and the benefit it can provide for patients who are suffering from severe radiculopathy after surgery as well as those with chronic pelvic pain (Fig. 3).
Fig. 3.
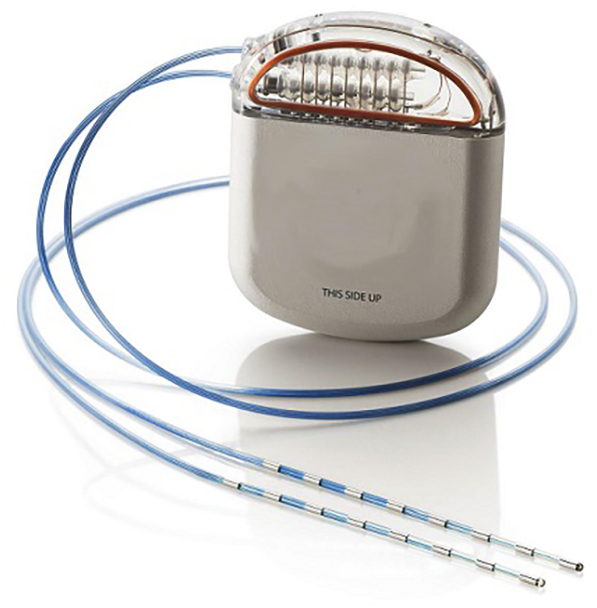
An example of an implantable high-frequency spinal cord stimulator system showing the percutaneous leads and implantable pulse generator.
4. Conclusion
Tarlov cysts are an uncommon condition that present more often in women. This condition rarely becomes symptomatic, producing a variety of neurologic symptoms and painful conditions. Given the rarity of the condition and the high complication rates associated with surgery, there is no clear treatment algorithm for symptomatic patients. These cysts can be managed conservatively or surgically; surgical management has higher complication rates but better long-term results for symptom and cyst resolution. Patients who develop new or worsening pain after Tarlov cyst surgery may benefit from spinal cord stimulation. This case may provide guidance for physicians managing patients suffering from symptomatic Tarlov cysts, or worsening pain symptoms after surgical management of these cysts.
Acknowledgments
Contributors
Jamal Hasoon contributed to the drafting, literature review, and critical revision of the article.
Amnon A. Berger contributed to the drafting, literature review, and critical revision of the article.
Ivan Urits contributed to review and critical revision of the article.
Vwaire Orhurhu contributed to review and critical revision of the article.
Omar Viswanath contributed to review and critical revision of the article.
Musa Aner provided supervision, and contributed to review and critical revision of the article.
Conflict of Interest
The authors declare that they have no conflict of interest regarding the publication of this case report.
Funding
No funding from an external source supported the publication of this case report.
Patient Consent
Obtained.
Provenance and Peer Review
This case report was peer reviewed.
References
- 1.Lucantoni C., Than K.D., Wang A.C., Valdivia-Valdivia J.M., Maher C.O., La Marca F., Park P. Tarlov cysts: a controversial lesion of the sacral spine. Neurosurg. Focus. 2011;31(6):E14. doi: 10.3171/2011.9.FOCUS11221. [DOI] [PubMed] [Google Scholar]
- 2.Park H.J., Jeon Y.H., Rho M.H., Lee E.J., Park N.H., Park S.I., Jo J.H. Incidental findings of the lumbar spine at MRI during herniated intervertebral disk disease evaluation. Am. J. Roentgenol. 2011;196(5):1151–1155. doi: 10.2214/AJR.10.5457. [DOI] [PubMed] [Google Scholar]
- 3.Paulsen R.D., Call G.A., Murtagh F.R. Prevalence and percutaneous drainage of cysts of the sacral nerve root sheath (Tarlov cysts) Am. J. Neuroradiol. 1994;15(2):293–297. [PMC free article] [PubMed] [Google Scholar]
- 4.Langdown A.J., Grundy J.R., Birch N.C. The clinical relevance of Tarlov cysts. Clin. Spine Surg. 2005;18(1):29–33. doi: 10.1097/01.bsd.0000133495.78245.71. [DOI] [PubMed] [Google Scholar]
- 5.Tarlov I.M. Perineurial cysts of the spinal nerve roots. Arch. Neurol. Psychiatr. 1938;40(6):1067–1074. [Google Scholar]
- 6.Sharma M., SirDeshpande P., Ugiliweneza B., Dietz N., Boakye M. A systematic comparative outcome analysis of surgical versus percutaneous techniques in the management of symptomatic sacral perineural (Tarlov) cysts: a meta-analysis. J. Neurosurg. Spine. 2019;30(5):623–634. doi: 10.3171/2018.10.SPINE18952. [DOI] [PubMed] [Google Scholar]
- 7.Patel M.R., Louie W., Rachlin J. Percutaneous fibrin glue therapy of meningeal cysts of the sacral spine. AJR Am. J. Roentgenol. 1997;168(2):367–370. doi: 10.2214/ajr.168.2.9016209. [DOI] [PubMed] [Google Scholar]
- 8.Caspar W., Papavero L., Nabhan A., Loew C., Ahlhelm F. Microsurgical excision of symptomatic sacral perineurial cysts: a study of 15 cases. Surg. Neurol. 2003;59(2):101–105. doi: 10.1016/s0090-3019(02)00981-3. [DOI] [PubMed] [Google Scholar]
- 9.Siqueira E.B., Schaffer L., Kranzler L.I., Gan J. CT characteristics of sacral perineural cysts: report of two cases. J. Neurosurg. 1984;61(3):596–598. doi: 10.3171/jns.1984.61.3.0596. [DOI] [PubMed] [Google Scholar]
- 10.Voyadzis J.M., Bhargava P., Henderson F.C. Tarlov cysts: a study of 10 cases with review of the literature. J. Neurosurg. Spine. 2001;95(1):25–32. doi: 10.3171/spi.2001.95.1.0025. [DOI] [PubMed] [Google Scholar]
- 11.Acosta F.L., Quinones-Hinojosa A., Schmidt M.H., Weinstein P.R. Diagnosis and management of sacral Tarlov cysts. Neurosurg. Focus FOC. 2003;15(2):1–7. doi: 10.3171/foc.2003.15.2.15. [DOI] [PubMed] [Google Scholar]
- 12.Cruccu G., Aziz T.Z., Garcia-Larrea L., Hansson P., Jensen T.S., Lefaucheur J.P., Simpson B.A., Taylor R.S. EFNS guidelines on neurostimulation therapy for neuropathic pain. Eur. J. Neurol. 2007;14(9):952–970. doi: 10.1111/j.1468-1331.2007.01916.x. [DOI] [PubMed] [Google Scholar]
- 13.Falowski S., Sharan A. A review on spinal cord stimulation. J. Neurosurg. Sci. 2012;56(4):287–298. [PubMed] [Google Scholar]
- 14.Wolter T. Spinal cord stimulation for neuropathic pain: current perspectives. J. Pain Res. 2014;7:651. doi: 10.2147/JPR.S37589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kapural L., Narouze S.N., Janicki T.I., Mekhail N. Spinal cord stimulation is an effective treatment for the chronic intractable visceral pelvic pain. Pain Med. 2006;7(5):440–443. doi: 10.1111/j.1526-4637.2006.00165.x. [DOI] [PubMed] [Google Scholar]