Abstract
Background
Exercise is gaining extreme relevancy as a new therapeutic intervention for Parkinson's disease (PD). However, the frequent misuse of the concepts exercise, physiotherapy, and physical activity limits the possibility of summarizing research findings. This review aims to clarify these concepts and summarize the evidence on exercise in PD.
Methods
We critically appraised physical activity–related concepts and conducted a systematic review of clinical trials evaluating exercise interventions in PD. Additionally, we discussed the implications for PD clinical practice and research.
Results
Exercise is a subset of physical activity, and a major component of physiotherapy for PD management, having as the main goal to improve physical fitness. The appraisal of the 83 identified clinical trials found high variability in exercise interventions. Multimodal exercise was the most studied, and 60 minutes, two times/week for 12 weeks, the most reported prescription parameters.
Conclusion
The best available evidence recommends increasing physical activity levels in PD. Exercise and physiotherapy programs seem the most efficacious strategies to achieve this goal. As a result of the heterogeneity in the type and manner exercise is prescribed, it is not possible to propose strong recommendations for exercise in PD. We believe that, in addition to the clarification of concepts here presented, a collaborative and rigorous work of different areas of knowledge is needed.
Keywords: physical activity, exercise, physiotherapy, Parkinson's disease
Today, Parkinson's disease (PD) treatment is still focused on symptomatic control, primarily involving dopaminergic medications, which are not effective for the entire spectrum of PD symptoms.1, 2, 3 Because of the benefits of improving the physical functioning of PD patients and the potential positive influence on disease progression, physiotherapy and exercise have been proposed as adjuvants to pharmacological treatment in PD.2, 3, 4
In recent years, several studies have been published exploring the benefits of physical activity (PA), exercise, and physiotherapy in PD. However, despite representing different concepts, they have been frequently used interchangeably, hindering the interpretation of results and the possibility of synthesizing and critically evaluating research findings.5, 6, 7 Furthermore, the level of standardization of the interventions and the methodological quality of the trials are usually low, frequently leading to conflicting or inconclusive results, which hamper the possibility of generating recommendations based on high levels of evidence.2, 8, 9
In order to improve the available evidence and establish its real efficacy, we believe that exercise in PD should be approached as a therapeutic intervention and prescribed with the same rigor as pharmacological interventions. For this to happen, collaboration between the fields of movement disorders and sports science is needed. In this article, we aim to: (1) clarify PA‐related concepts, so that all researchers use the same terminology and the synthesis and interpretation of study results will be possible; (2) summarize the published evidence about exercise prescription in PD; and (3) extend and adapt the current knowledge of sports science to PD, providing recommendations that help health professionals in their clinical practice. In order to fully address these aims, we begin our review by examining the current knowledge of sports science, specifically the PA‐related concepts and the basic notions of exercise prescription and applying these to the Parkinson's field. We used the results of our systematic review to provide an overview of the state of art of exercise prescription in PD. We end this review discussing safety issues and delineating possible ways to improve the evidence of exercise prescription in PD.
Clarifying Concepts
How Are Physical Fitness, Physical Function, and PA Related?
According to the International Classification of Functioning, Disability and Health (ICF) model, physical fitness belongs to the domain “body functions and structures.” Its changes over time are reflected in physical function, which belongs to the ICF domain “activity” (Table 1). Physical function could be approached from two different, but complementary, perspectives (Fig. 1): as the subject's ability and best performance in a functional task, physical performance, or as the subject's usual PA in real life.
Table 1.
PA‐related concepts definitions
| Concept | Definition |
|---|---|
| Physical fitness or physical capacity | Set of attributes that people have or achieve. Can be either health‐ or skill‐related.5, 10, 24 |
| Physically fit | The ability to perform moderate‐to‐vigorous levels of PA without undue fatigue and the capability of maintaining this capacity throughout life.5, 25 It positively correlates with physical function.5, 10 |
| Physical function | The ability to carry out activities that involve bodily movement, ranging from basic self‐care tasks to social activities, that require a combination of skills.9 Can be approached as an individual's physical behavior in real life, “physical activity,” or as the ability of the person to perform a specific task, “physical performance.”9 |
| Physical performance | The ability to perform specific functional tests or tasks.9 |
| Physical activity | Any bodily movement produced by skeletal muscles that results in energy expenditure.5, 9, 10 |
| Exercise | A subset of PA, characterized by: (1) being planned, structured, and involving repetitive bodily movements; (2) not following a conservative energy consumption approach; and (3) always intended to improve or maintain one or more components of physical fitness, even if the participant is not continuously aware of it.5, 10 |
Figure 1.
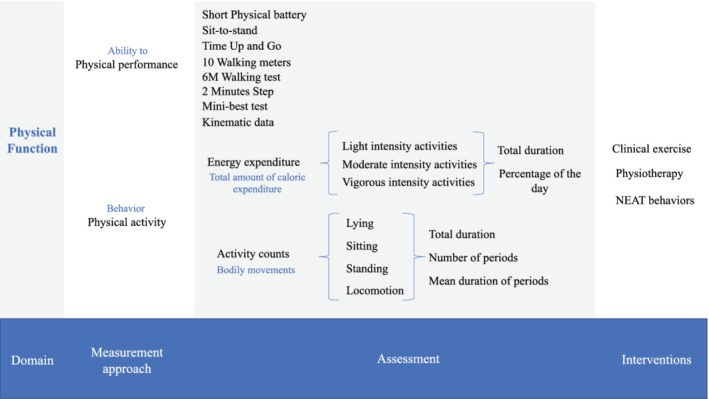
Physical function: included domains, detection and intervention.
How to Define PA and Exercise?
PA is defined as any bodily movement produced by skeletal muscles that results in energy expenditure. It is a behavior reflex of subjects’ physical function and can be divided in to exercise or nonexercise activity thermogenesis (NEAT; or lifestyle forms of PA).5, 10, 11
Exercise is characterized by: (1) being planned, structured, and being an activity involving repetitive bodily movements; (2) not following a conservative energy consumption approach; and (3) always being intended to improve or maintain one or more components of physical fitness, even if the participant is not continuously aware of it.5, 11 NEAT is defined as all energy expenditure excluding sleeping, eating, and activity not intended to constitute a structured period of exercise.12
PA levels are usually expressed in activity counts or energy expenditure estimates.10 Activity counts report the total duration, number of periods, and mean duration of lying down, sitting, standing, and periods of locomotion.5 Energy expenditure can be measured in kilocalories (kcal) or through metabolic equivalent of task (MET; 1 MET represents the expenditure of 1 kcal/kg per hour = consumption of 3.5 mL of O2/kg per hour, equivalent to the energy expenditure at rest). In this context, energy expenditure results from total duration and the percentage of the day spent on light‐ (1.5–3.0 METs), moderate‐ (3.0–5.9 METs), and vigorous‐intensity (≥6 METs) activities. NEAT behaviors are associated with light‐intensity activities, whereas exercise training is usually associated with moderate‐ or vigorous‐intensity activities.
Higher levels of PA positively correlate with physical fitness and functional independence.5, 13, 14 It decreases the risk of falling and fractures and delays all‐cause mortality.15 It also improves self‐control, self‐image, and cognitive function and empowers older people to remain active in the community.10, 15, 16
How Does Exercise Relate to Physiotherapy?
Physiotherapy is a nonpharmacological therapeutic intervention that uses a holistic patient‐centered approach, which aims to restore and maximize the quality of movement and functional independence, while supporting patient self‐management and participation.17, 18 Exercise is one of the most common interventions in physiotherapy programs. It is prescribed with the aim of improving disease symptoms and functioning problems, as well as slowing functional deterioration and, in some cases, disease progression. Besides exercise‐based programs in the clinic, physiotherapists also prescribe home‐based exercise programs according to the specific needs of patients and encourage them to increase their daily levels of physical activity.4, 17, 18
In PD management, physiotherapy is mainly an exercise‐based intervention that addresses five core areas: physical fitness, transfers, manual activities, balance, and gait.18
Exercise as a Therapeutic Intervention
Exercise as a therapeutic intervention (or clinical exercise) is the application of the body of knowledge of sports science involving physiological, metabolic, and structural responses and prescribing principles to short‐ and long‐term PA with clinical relevance to the management of health conditions.19, 20 Clinical exercise is becoming extremely relevant as a new efficacious therapeutic intervention in multiple medical fields. Besides helping in disease management, clinical exercise also improves physical fitness and is associated with other general health benefits, including the improvement of cardio‐ and cerebrovascular health, reduction of osteoporosis and age‐related sarcopenia, improvement in psychological and autonomic disorders, and as having a general anti‐inflammatory effect.14, 21
In PD, clinical exercise has been recommended as an adjunct to pharmacological interventions for the management of symptoms unresponsive to pharmacological and surgical therapeutic approaches. Today, it is also recognized as one of the most promising therapeutic interventions for delaying disease progression.6, 9, 22
Exercise Prescription
How to Prescribe Clinical Exercise
To achieve exercise benefits, supercompensation—described as the adaptive response following a controlled application of stress on the body and its subsequent regeneration—should be reached during training.23 In order to optimize this process, and simultaneously avoid injury, the principles of prescription and training should be followed. In this review, we will focus on the principle of prescription, the FITT (frequency, intensity, type, and time) principle, and on the five major principles of training with clinical impact: specificity, overload, progression, variance, and reversibility.24
The specificity principle indicates that the effects of training derived from an exercise program be specific to the exercise performed and the muscles involved, which requires a clearly predefined aim of training.24 According to the overload principle, during exercise the body has to work at a higher intensity than normal to improve fitness. If not achieved, supercompensation may not occur, or an overload of stress may be induced, increasing the risk of injury.24 The principle of progression refers to the need to adapt the overload level, through short increases in one or more components of the FITT principle. Contrariwise, once the training stimulus is removed, fitness levels will eventually return to baseline (principle of reversibility).11, 25 Last, the principle of variance highlights the need to vary the type of exercise in order to ensure that exercise remains interesting over time and, consequently, that the subject is compliant.11
Table 2 summarizes the American College of Sports Medicine (ACSM) guidelines for exercise prescription in healthy adults and elderly and for promoting bone health. These guidelines take into account the new recommendation from the 2018 physical activity guidelines for Americans. These are extendable, according to the authors, to chronic diseases, such as PD.14, 24, 26, 27
Table 2.
ACSM endurance and resistance training guidelines for healthy and older adults (or persons with certain chronic diseases, including PD patients) and for promoting bone health
| Healthy Adults (1) | Older Adults (2) | Bone Health | |
|---|---|---|---|
| Endurance exercise training |
Moderate‐intensity: ≥30 min × d–1, ≥5 d × wk–1 ➔ ≥150 min × wk–1 Energy expenditure: 3.0 to 5.9 METs Vigorous‐intensity: ≥20 min × d–1, ≥3 d × wk–1 ≥75 min × wk–1 Energy expenditure: ≥6 METs Combination of moderate‐ and vigorous‐intensity: 10 MET × h × wk–1 Weekly recommendation: 1,000 kcal×wk–1 |
≥60% of pretraining VO2max ≥3 d × wk–1 |
Exercise type: a combination of weight‐bearing activities (tennis; stair climbing; jogging, at least intermittently during walking), activities that involve jumping (volleyball, basketball), and resistance exercise that targets all major muscle groups Intensity: moderate to high, in terms of bone‐loading forces Frequency: 3 to 5 times per week Duration: 30 to 60 min × d–1 |
| Resistance exercise training |
Frequency: ≥2 to 3 d × wk–1 Repetitions: 2 to 4 sets per muscle group Rest period between sessions: 48 to 72 hours Muscle strength: Resistance: 60% to 80% of 1 RM (novice and intermediate trainers: 60%–70% of 1 RM) Repetitions: 8 to 12 per set (the needed to induce muscle fatigue, but not exhaustion) Rest intervals: 2 to 3 minutes
Muscle endurance: Resistance: 50% of 1 RM Repetitions: 15 to 25 per set Duration: not more than 2 sets |
Start from: Resistance: 40% to 50% of 1 RM Repetitions: 10 to 20 per set Progress: adopting healthy adults’ regimen
Power development: Resistance: 20% to 50% of 1 RM Repetitions: 8 to 12 repetitions Duration: 3 sets |
Exercise type: weight lifting Frequency: 2 to 3 times per week |
Which Type of Exercise?
According to the ACSM, exercise can be divided into endurance, resistance, flexibility, balance, and multicomponent training.9, 14, 27, 28 All increase metabolic, physical, and mechanical demands, leading to increased stress on various tissues and biological functions. When the appropriate type of exercise is performed at a proper intensity and adequate duration and frequency, supercompensation is achieved resulting in improved physical fitness and function.13 Because of a combination of genetic and lifestyle factors, there is wide variability in subjects’ responses to exercise. An individualized exercise prescription, taking into account an evaluation of fitness levels, subjects’ personal factors, environmental conditions, and including all exercise components, should be considered.14, 26
Endurance Training
Definition
Endurance exercise training (EET) is defined as a type of exercise in which the body's large muscles move in a rhythmic manner for sustained periods.26
Health‐Related Benefits
EET is associated with several health benefits. The most studied are the cardiovascular effects, including: (1) a lower heart rate at rest and at any submaximal exercise workload; (2) lower blood pressure rises during submaximal exercise; (3) improvements in the oxygen delivery and extraction capacities of the trained muscle groups; and (4) reduction of atherogenic risk factors and in large elastic artery stiffness, improved endothelial and baroreflex function, and increased vagal tone.26 EET has also positive effects on metabolic function (enhanced glycemic control, augmented clearance of postprandial lipids, and preferential utilization of fat during submaximal exercise), in cognitive performance (reduces the risk of cognitive decline, dementia), mood (depression and anxiety), and in bone health (attenuates age‐related decline of bone mass density, reducing the risk of fracture).26, 29, 30 In elderly or adults with clinically significant chronic conditions or functional impairments, EET influences subjects’ self‐concept and self‐esteem through the increase of psychosocial control, self‐efficacy, and perceived competency.26 In PD, EET seems to have positive results on physical fitness, balance, gait speed, motor function, quality of life, and rate of falls, benefits that are preserved for 2 to 6 months after cessation of the exercise program.9 Evidence suggests that the exercise level required to obtain benefits in cardiorespiratory fitness and cardiometabolic health is higher than the exercise level required to maintain those benefits. While many physiological changes occur as soon as 1 or 2 weeks following cessation of exercise training, maintaining a reduced level of exercise only has a modest influence on VO2max over periods of several months.14
Resistance Exercise
Definition
Resistance exercise training (RET) refers to activities where muscles work or hold against an applied force or weight to improve muscular fitness (i.e., functional parameters of strength, endurance, and power).14, 26 Changes are measured using a variety of methods, with the most common in older adults being 1‐RM (repetition maximum‐effort) or 3‐RM performance compared with isometric or isokinetic measures.26 RET can be performed through dynamic exercises based on concentric and eccentric muscle contractions, simultaneously targeting multiples of the major muscle groups or single‐joint exercises that isolate functionally important muscle groups.14 To optimize the effects of exercise, the following indications should be kept in mind: (1) RET should use the correct form and technique during the full range of motion of the joint; (2) repetitions should be made in a controlled manner, using proper breathing techniques (i.e., exhalation during the concentric phase and inhalation during the eccentric phase avoiding the Valsalva maneuver); (3) antagonist muscles (e.g., the abdominals and lumbar extensors) should be trained to avoid muscular imbalances; (4) rest periods between sessions of 48 to 72 hours should be included to promote the cellular/molecular adaptations associated with muscle hypertrophy and strength; and (5) training exclusively featuring eccentric contractions should be avoided because it can severely damage muscles and is associated with serious complications.14 Subjects with increased risk of falls should focus on power development (i.e., the force or torque of a muscular contraction multiplied by its velocity measured through isokinetic, isotonic, stair climbing, and vertical jumping protocols). Power seems to be more strongly associated with functional performance and to suffer a more rapid age‐related deterioration loss than strength.14, 26 RET interruption leads to a fast loss of improvements in muscle strength and power. Therefore, in order to be beneficial, at least a single session per week of moderate‐ to hard‐intensity resistance exercise should be maintained.14, 27
Health‐Related Benefits
RET is associated with significantly better cardiometabolic risk factor profiles, lower risk of developing functional limitations, and lower all‐cause mortality. It is correlated with effective increases in bone mass (bone mineral density and content) and strength of the specific stressed bones.14, 26 In older adults or those with functional limitations, RET has proved to be effective in reducing falls and fracture events.26, 29 Compared with other types of exercise, RET is more efficacious in slowing the loss of muscle strength and bone mass and decreasing the levels of energy‐absorbing soft tissue. It also favors positive changes in body composition, increasing fat‐free mass and decreased fat mass.14, 26 In PD, RET seems to improve muscle strength, balance, functional mobility, and quality of life with effects lasting for 12 weeks. However, study results are not consistent and should be interpreted with some caution.2, 9
Flexibility Exercise
Definition
Flexibility exercise training (FET) refers to activities that aim to preserve or extend the range of motion (ROM).26 FET could follow different methods: ballistic, static, dynamic stretching, and/or using proprioceptive neuromuscular facilitation (PNF). PNF may produce slightly larger gains in the flexibility of some joints compared with other techniques, but requires the assistance of a second person.14 A duration of 10 to 30 seconds per stretch, at the point of tightness or slight discomfort, is recommended. Older individuals may realize greater improvements in ROM with longer durations (30–60 seconds) of stretching.14 Repeating each flexibility exercise two to four times is effective. A series of exercises targeting the major muscle‐tendon units of the shoulder girdle, chest, neck, trunk, lower back, hips, posterior and anterior legs, and ankles are recommended.14 Joint range of motion improves gradually after approximately 3 to 4 weeks of regular stretching at a frequency of at least two to three times a week. Greater gains in joint range of motion are accrued with daily flexibility exercise.14 To optimize FET, this should be performed when the muscle temperature is elevated through light‐to‐moderate cardiorespiratory or muscular endurance exercise or passively through external methods, such as moist heat packs or hot baths. ROM improvements reverse within 4 to 8 weeks of cessation of stretching exercise.14
Health‐Related Benefits
Flexibility exercises may enhance postural stability and balance, particularly when combined with resistance exercise.14, 26 In PD, flexibility training has been used as part of multimodal training or used as the intervention of the control group in clinical trials. Research is needed to understand its role in PD.2, 9
Balance and Multicomponent Exercise
Definition
Balance exercise training refers to a combination of activities designed to increase lower body strength and reduce the likelihood of falling.26 Multicomponent exercise training (also called neuromotor or multimodal training) is the combination of the previously mentioned types of exercise with the training of different motor skills, such as balance, coordination, gait, and agility, and proprioceptive training.14, 27
Health‐Related Benefits
Balance training is a critical component of training programs for older adults or individuals at increased risk and fear of falling. Multicomponent training is beneficial as part of a comprehensive exercise program for older persons, especially to improve balance, agility, and muscle strength, and it also contributes to reducing the risk of falls.14, 26, 29 In PD, it is infrequent that balance and multicomponent exercise are addressed exclusively as exercise programs; they rather form part of a physiotherapy therapeutic intervention. The available evidence reports that balance training improves PD patients’ mobility and postural stability.2
Where Are We in Exercise Prescription in PD?
Today, there is a strong consensus that clinical exercise in PD improves symptom management, physiological and structural brain function, and there is a strong belief in its impact in delaying disease progression.31 However, the way that exercise interventions have been conceptualized in PD is not systematically detailed or robustly established, which affects the possibility of summarizing research findings. In order to cover this evidence gap, we retrieved the data of the current standards of exercise prescription in clinical studies involving patients with PD through a systematic review. PubMed, PEdro, and the Cochrane Library electronic databases were searched from their inception to July 2019. The following keywords were used in combination in the search strategy: Parkinson's disease, exercise, therapeutic exercise, and physical activity. Hand searching was also performed to identify further qualifying studies from reference lists of relevant studies. A detailed description of the methods, methodological quality analysis, and characteristics of the included studies are presented in Supporting Information Appendix S1.
Exercise Prescription General Data
Of the 1,118 records retrieved, 83 studies were included in this review; all were published between 1986 and 2019.
One hundred three exercise interventions were found. Of these, 38% (n = 39) concern multimodal exercise interventions, 28% (n = 29) endurance training, 20% (n = 21) resistance training, 11% (n = 11) balance training, and 3% (n = 3) flexibility training (Fig. 2).
Figure 2.
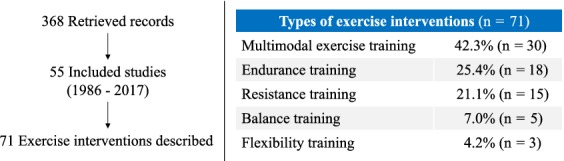
Type of exercise interventions in the included studies.
Exercise frequency varied from three times/day to weekly sessions, with two sessions/week being the most used frequency (43%; n = 36 studies). Interventions lasted from 2 to 96 weeks; 12 weeks was the most frequent duration (28%; n = 23). The duration of exercise sessions varied between 20 and 120 minutes, with 60 minutes being the most common duration (54%; n = 45 studies).
In 16% (n = 13) studies, the dropout rate was higher than 20%. The main causes of attrition were symptom burden and clinical deterioration. Pooled results from studies that reported one or more dropouts (61%; n = 51) showed a higher dropout rate among the control groups (odds ratio = 0.85; 95% confidence interval = [0.68, 1.05]); however, the results were not statistically significant (Supporting Information Appendix S1). The most used comparators were other interventions (57%; n = 47), usual care/no intervention (37%; n = 31).
Endurance Training
Ninety‐seven percent (n = 28) of the studies reported exercise prescription according to the FITT principle. The most used methods to measure exercise intensity level were heart rate (Hrmax; 39%; n = 11), heart rate reserve (HRR; 21%; n = 6), maximum speed (21%; n = 6) and rate of perceived exertion using the Borg scale (Borg Rating of Perceived Exertion; 18%; n = 5). The majority of the interventions tested were of moderate intensity, that is, Hrmax ranging from 60% to 80% or from 60% to 70% of the HRR.
Resistance Training
Fifty‐eight percent (n = 12) of the included resistance exercise studies reported exercise prescription according to the FITT principle. One‐repetition maximum‐effort protocol (1 RM) was the most used method to measure exercise intensity level (64%; n = 9), ranging 30% to 90% of 1 RM.
Are Clinical Exercise Programs Always the Answer?
Although the ultimate goal is that patients engage in exercise programs and become physically active subjects (i.e., those who comply with the recommended levels of PA), the one‐size‐fits = all messaging strategies do not always work, and some additional preceding steps may be needed.32
Most PD patients spend a considerable portion of their day in sedentary behaviors.27, 32 Replacing sitting time by small amounts of light‐intensity or, ideally, moderate‐intensity PA may provide significant protective health benefits.27, 32 Therefore, in low‐fit, sedentary patients, the first step may be to move more and sit less throughout the day, promoting all possible forms of PA.32 This includes little changes in the daily routine, such as parking farther away from a destination and walking, climbing stairs, doing housework, or gardening.11, 27
Walking is usually a good first moderate‐intensity activity given that it does not involve special skills, equipment, or environment.27 As patients become fitter, additional benefits may be obtained with longer duration, frequency, or by substituting moderate‐ with higher‐intensity PA. If possible, patients should engage in multicomponent exercise programs, including endurance, resistance, and balance exercises, which are very important in sedentary people with decreased autonomy and at a high risk of falls.11, 27
A fundamental objective of exercise prescription is to promote a change in personal health behaviors. In order to do this, attention should be given to: (1) discussing goals with patients; (2) teaching patients to self‐monitor activity and progress; (3) providing information and giving feedback about progress; and (4) educating patients about the behaviors that will help them progress toward reaching their goals.11, 32
Is It Enough to Engage in Clinical Exercise Programs?
According to 2018 physical activity guidelines,27 even among those considered active subjects (i.e., who comply with the weekly recommendations of PA), the majority spend a high percentage of the day in sedentary behaviors (i.e., any waking behavior characterized by an energy expenditure ≤1.5 METs while in a seated or reclining posture).27, 33 According to a 2011 systematic review on sedentary behavior and subsequent health outcomes, sedentary behavior may be a risk factor, independent of PA, for multiple adverse health outcomes in adults.32 The 2018 physical activity guidelines state that even when the recommended levels are not achieved, some PA may result in fitness and health benefits, particularly in sedentary individuals.14, 26 Therefore, it is recommended to not only increase levels of physical activity by engaging in exercise programs, but also to reduce sedentary time by increasing standing and light‐intensity ambulatory activities (e.g., incidental movements, lifestyle‐embedded activities).27, 33 For those who for some reason (e.g., physical impairments, financial, or logistic issues) cannot engage in exercise programs, an increase in NEAT behaviors should be recommended.
Are Exercise and Increases in PA Well Tolerated and Safe?
The main concerns related to the practice of physical exercise are musculoskeletal injuries and cardiovascular risks. Musculoskeletal concerns should be approached by tailoring the exercise to each patient's limitations, ideally by a health care professional and by following crucial aspects of exercise prescription (warming up, cooling down, using the proper training technique, and gradual progression).14
Regarding cardiovascular risks, the fear of these events comes from the existence of exertion‐related symptoms that occur in pathological states (e.g., exertion angina or exertion dyspnea), but also from exercise as a trigger for potentially fatal cardiovascular events. These events are more frequent in patients with coronary disease or structural heart disease, even though they are very rare, leading to 1 death in 396,000 patient‐hours of exercise in previously healthy individuals34 and 1 cardiovascular event/per 60,000 patient‐hours of exercise in those with cardiovascular disease in a cardiac rehabilitation setting.35 Thus, physical exercise seems to be safe, but risk minimization requires: screening assessments, education about prodromal signs and symptoms of cardiovascular disease, consultation with a health professional, and exercise stress testing (if medically indicated). PD patients, especially beginner exercisers, may benefit from a consultation with an exercise expert. Not all patients will benefit from cardiac stress testing. There is no evidence suggesting its use as a diagnostic tool for cardiovascular disease in asymptomatic individuals at low risk of coronary artery disease or before activities like walking.12, 14
Implications for PD Clinical Practice
The majority of PD patients fail to meet the daily‐recommended level of 30 minutes of activity per day.36 Recent studies show that PD patients spent 75% of all awake time in sedentary behaviors, 18% in low levels of PA, and 6% in a combination of moderate and vigorous levels of PA. Compared to healthy controls matched for age, PD patients were approximately 30% less physically active, accentuating the difference with disease progression.16
Increasing PA levels through a more active lifestyle and/or engaging exercise or physiotherapy programs has been shown to have positive effects in PD patients’ physical fitness (e.g., cardiovascular endurance, muscular strength, or balance) and cognitive and physical function. In addition, it seems to have a disease‐modifying effect that needs to be confirmed.6, 16, 37
Therefore, because of its extensive benefits, health professionals should make PA counseling a part of routine patient visits.12, 13 Increasing NEAT behaviors, through the adoption of a more active lifestyle (e.g., not parking the car very close to the place of destination, gardening, climbing stairs, and implementing 2‐minute breaks during long periods of seated activities) should be recommended to all PD patients. For those who are capable and who have the necessary logistic conditions, participation in individualized and/or community exercise programs should be suggested.6, 16, 18, 27, 37 The ParkFit study36 tested a multifaceted behavioral change program, designed to increase the level of physical activity of PD patients. Although the authors refer the need for more robust interventions to promote PAs in daily life, patients spent almost 1.5 hours/week extra on PA, compared with baseline.36 Therefore, the incorporation of established counseling strategies and techniques from individual behavioral programs seems promising.12, 13
Implications for PD Research
Similarly to pharmacological therapeutic interventions, clinical exercise should be recommended according to exercise prescribing principles. Although the number of trials on exercise is considerably growing, their methodological quality is still unsatisfactory (Supporting Information Appendix S1).8 By not being an industry‐sponsored pharmacological intervention, its development program has been driven mainly by investigator‐initiated trials without clear recommendations about the best type of exercise and the most appropriate intensity, frequency, and duration.31
In order to clarify the real effects of exercise as a therapeutic intervention and to optimize its use in managing PD, the knowledge and rigor of a formal drug development program should be used in clinical exercise research. In order to improve this field, we suggest that the following questions be first addressed: (1) What is the most appropriate study design to conduct trials on exercise in PD (patient population, study design–parallel, delayed‐start, washout, best sham‐intervention/comparator, and recommended outcomes); (2) what is the most adequate clinical exercise intervention to be tested and applied in PD (type of intervention, intensity, and duration); and (3) how to optimally deal with factors related to exercise interventions like adherence, persistence, and adverse effects.
Conclusion
Physical health‐related quality of life could be improved by increasing levels of PA. This could be reached simply by adopting a more active lifestyle (i.e., increasing the daily level of NEAT behaviors), engaging in an exercise program, or through a multimodal physiotherapy intervention.6, 9, 18
The weekly recommended level of PA for PD patients is 150 minutes of moderate‐intensity PA or 75 minutes of vigorous‐intensity PA. However, the majority of PD patients are not capable of achieving these recommendations.
Exercise programs are the easiest and most efficacious strategy for achieving these levels of activity. Similarly to pharmacological therapeutic interventions, these should be prescribed and performed based on the FITT principle of prescribing exercise.
Nonetheless, exercise programs are not the only way of increasing PA levels. In the case of more advanced PD patients with higher levels of sedentary behaviors, the increase in PA levels should be made through increasing NEAT behaviors (like small incidental repeated movements) that, although apparently inconsequential, are important to both balance and muscle and maintaining energy function. Even for active PD patients, this is also an important recommendation in order to reduce the time spent in sedentary behaviors.
Because of the good safety profile, easy access, and low cost of exercise interventions, the confirmation of both symptomatic and disease‐modifying effects of exercise in this field could have a profound societal impact. In the absence of other disease‐modifying interventions and when some of the existent pharmacological interventions are associated with the presence of motor and nonmotor complications, this type of approach could be extremely useful.38 In order to clarify the benefits of exercise and inform health professionals on critical factors in exercise prescription in PD, the following questions need to be addressed: How should the FITT principle be applied to the different stages of PD; how should safety and adherence issues be dealt with; and what is the optimal duration of exercise programs?
Author Roles
(1) Research Project: A. Conception, B. Organization, C. Execution; (2) Statistical Analysis: A. Design, B. Execution, C. Review and Critique; 3. Manuscript Preparation: A. Writing of the First Draft, B. Review and Critique.
R.B.M.: 1A, 1B, 1C, 2A, 2B, 2C, 3A, 3B
A.R.: 1A, 1B, 1C, 2A, 2B, 3B
D.C.: 1C, 2C, 3B
A.C.C.: 2C, 3B
D.G.: 2C, 3B
M.V.: 1A, 2C, 3C
M.T.: 1A, 2C, 3C
F.S.: 1A, 2C, 3C
J.J.F.: 1A, 1B, 2A, 2C, 3B
Disclosures
Ethical Compliance Statement: We confirm that we have read the Journal's position on issues involved in ethical publication and affirm that this work is consistent with those guidelines. The authors confirm that the approval of an institutional review board or a patients informed consent were not required for this work based on the submission type.
Funding Sources and Conflicts of Interest: The authors report no sources of funding and no conflicts of interest.
Financial Disclosures for previous 12 months: D.C. has participated in educational meetings and/or attended conferences or symposia with Bristol‐Myers Squibb, Bayer, Boehringer Ingelheim, Daiichi Sankyo, Merck Serono, Ferrer, Pfizer, Novartis, and Roche. J.J.F. has consulted for Ipsen, GlaxoSmithKline, Novartis, Teva, Lundbeck, Solvay, Abbott, BIAL, Merck‐Serono, and Merz; has received research grants from GlaxoSmithKline, Grunenthal, Teva, and Fundação MSD; and has been employed by Laboratory of Clinical Pharmacology and Therapeutics of Lisbon.
Supporting information
Appendix S1. Methodology used in the systematic review and characteristics of intervention in the included studies.
Acknowledgments
UID/BIM/50005/2019, project funded by Fundação para a Ciência e a Tecnologia (FCT)/Ministério da Ciência, Tecnologia e Ensino Superior (MCTES) through Fundos do Orçamento de Estado. Fundação para a Ciência e a Tecnologia (FCT; SFRH/BD/120773/2016 to R.B.M.).
Relevant disclosures and conflicts of interest are listed at the end of this article.
References
- 1. Von Campenhausen S, Bornschein B, Wick R, et al. Prevalence and incidence of Parkinson's disease in Europe. Eur Neuropsychopharmacol 2005;15:473–490. [DOI] [PubMed] [Google Scholar]
- 2. Earhart GM, Falvo MJ. Parkinson disease and exercise. Compr Physiol 2013;3:833–848. [DOI] [PubMed] [Google Scholar]
- 3. Burgess S, Rassmusson X. Parkinson's narratives: onset experiences and perceived benefits of preferred physical activity. Adv Soc Sci Res J 2016;3:150–160. [Google Scholar]
- 4. Taylor NF, Dodd KJ, Shields N, et al. Therapeutic exercise in physiotherapy practice is beneficial: a summary of systematic reviews 2002–2005. Aust J Physiother 2007;53:7–16. [DOI] [PubMed] [Google Scholar]
- 5. Caspersen CJ, Powell KE, Christenson GM. Physical activity, exercise, and physical fitness: definitions and distinctions for health‐related research. Public Health Rep 1974;100:126–131. [PMC free article] [PubMed] [Google Scholar]
- 6. Lauzé M, Daneault JF, Duval C. The effects of physical activity in Parkinson's disease: a review. J Parkinsons Dis 2016;6:685–698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Bauman AE, Sallis JF, Dzewaltowski DA, et al. Toward a better understanding of the influences on physical activity: the role of determinants, correlates, causal variables, mediators, moderators, and confounders. Am J Prev Med 2002;23(2 Suppl):5–14. [DOI] [PubMed] [Google Scholar]
- 8. Abell B, Glasziou P, Hoffmann T. Exploration of the methodological quality and clinical usefulness of a cross‐sectional sample of published guidance about exercise training and physical activity for the secondary prevention of coronary heart disease. BMC Cardiovasc Disord 2017;17:153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Mak MK, Wong‐Yu IS, Shen X, et al. Long‐term effects of exercise and physical therapy in people with Parkinson disease. Nat Rev Neurol 2017;13:689–703. [DOI] [PubMed] [Google Scholar]
- 10. Van Lummel RC, Walgaard S, Pijnappels M, et al. Physical performance and physical activity in older adults: associated but separate domains of physical function in old age. PLoS One 2015;10:e0144048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. American College of Sports Medicine . ACSM's Guidelines for Exercise Testing and Prescription, 9th ed. Baltimore, MD: Wolters Kluwer Lippincott Williams & Wilkins; 2014. [Google Scholar]
- 12. Donnelly JE, Blair SN, Jakicic JM, et al. Appropriate physical activity intervention strategies for weight loss and prevention of weight regain for adults. Med Sci Sports Exerc 2009;41:459–471. [DOI] [PubMed] [Google Scholar]
- 13. Haskell WL, Montoye HJ, Orenstein D. Physical activity and exercise to achieve health‐related physical fitness components. Public Health Rep 1983;100:202–212. [PMC free article] [PubMed] [Google Scholar]
- 14. Garber CE, Blissmer B, Deschenes MR, et al. Quantity and quality of exercise for developing and maintaining cardiorespiratory, musculoskeletal, and neuromotor fitness in apparently healthy adults: guidance for prescribing exercise. Med Sci Sports Exerc 2011;43:1334–1359. [DOI] [PubMed] [Google Scholar]
- 15. Jantunen H, Wasenius N, Salonen MK, et al. Objectively measured physical activity and physical performance in old age. Age Ageing 2017;46:232–237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Benka Wallen M, Franzen E, Nero H, et al. Levels and patterns of physical activity and sedentary behavior in elderly people with mild to moderate Parkinson disease. Phys Ther 2015;95:1135–1141. [DOI] [PubMed] [Google Scholar]
- 17. World Confederation for Physical Therapy . Description of physical therapy. 2011. http://www.wcpt.org/sites/wcpt.org/files/files/PS_Description_PT_Sept2011_FORMATTED_edit2013.pdf. Accessed 12 January 2018.
- 18. Keus S, Munneke M, Graziano M, et al. European Physiotherapy Guideline for Parkinson's Disease, 1st ed Nijmegen, The Netherlands: KNGF/ParkinsonNet; 2014. http://www.fizioterapeitiem.lv/attachments/article/307/4_eu_guideline_parkinson_201412-development.pdf. Accessed 23 October 2019. [Google Scholar]
- 19. McGough EL, Lin SY, Belza B, et al. A scoping review of physical performance outcome measures used in exercise interventions for older adults with Alzheimer disease and related dementias. J Geriatr Phys Ther 2019;42:28–47. [DOI] [PubMed] [Google Scholar]
- 20. Thompson PD, Franklin BA, Balady GJ, et al. Exercise and acute cardiovascular events: Placing the risks into perspective. Med Sci Sports Exerc 2007;39:886–897. [DOI] [PubMed] [Google Scholar]
- 21. Warburton DER, Nicol CW, Bredin SSD. Health benefits of physical activity: the evidence. CMAJ 2006;174:801–809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Keus SHJ, Munneke M, Graziano M. European physiotherapy guideline for parkinson's disease: information for neurologists. Mov Disord 2016;31:S589. [Google Scholar]
- 23. Gambetta VA. Athletic Development: The Art & Science of Functional Sports Conditioning, 1st ed. Champaign, IL: Human Kinetics; 2006. [Google Scholar]
- 24. SHAPE America—Society of Health and Physical Educators, Ayers SF, Sariscsany MJ. Physical Education for Lifelong Fitness: The Physical Best Teacher's Guide, 3rd ed Reston, VA: National Association for Sports and Physical Education; 2011. http://www.ode.state.or.us/teachlearn/subjects/pe/curriculum/fittprinciple.pdf. Accessed 13 January 2018. [Google Scholar]
- 25. Campbell KL, Neil SE, Winters‐Stone KM. Review of exercise studies in breast cancer survivors: attention to principles of exercise training. Br J Sports Med 2012;46:909–916. [DOI] [PubMed] [Google Scholar]
- 26. Chodzko‐Zajko WJ, Proctor DN, Fiatarone Singh MA, et al. Exercise and physical activity for older adults. Med Sci Sports Exerc 2009;41:1510–1530. [DOI] [PubMed] [Google Scholar]
- 27. Piercy KL, Troiano RP, Ballard RM, et al. The physical activity guidelines for Americans. JAMA 2018;320:2020–2028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. American College of Sports Medicine Position Stand . The recommended quantity and quality of exercise for developing and maintaining cardiorespiratory and muscular fitness, and flexibility in healthy adults. Med Sci Sport Exerc 1998;30:975–991. [DOI] [PubMed] [Google Scholar]
- 29. Kohrt WM, Bloomfield SA, Little KD, et al. Physical activity and bone health. Med Sci Sport Exerc 2004;36:1985–1996. [DOI] [PubMed] [Google Scholar]
- 30. Colberg SR, Albright AL, Blissmer BJ, et al. Exercise and type 2 diabetes: American College of Sports Medicine and the American Diabetes Association: joint position statement. Exercise and type 2 diabetes. Med Sci Sports Exerc 2010;42:2282–2303. [DOI] [PubMed] [Google Scholar]
- 31. Ramazzina I, Bernazzoli B, Costantino C. Systematic review on strength training in parkinson's disease: an unsolved question. Clin Interv Aging 2017;12:619–628. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. Thorp AA, Owen N, Neuhaus M, et al. Sedentary behaviors and subsequent health outcomes in adults: a systematic review of longitudinal studies, 1996–2011. Am J Prev Med 2011;41:207–215. [DOI] [PubMed] [Google Scholar]
- 33. Tremblay MS, Colley RC, Saunders TJ, et al. Physiological and health implications of a sedentary lifestyle. Appl Physiol Nutr Metab 2010;35:725–740. [DOI] [PubMed] [Google Scholar]
- 34. Thompson PD, Funk EJ, Carleton RA, et al. Incidence of death during jogging in Rhode Island from 1975 through 1980. JAMA 1982;247:2535–2538. [PubMed] [Google Scholar]
- 35. Franklin BA, Bonzheim K, Gordon S, et al. Safety of medically supervised outpatient cardiac rehabilitation exercise therapy. Chest 1998;114:902–906. [DOI] [PubMed] [Google Scholar]
- 36. van Nimwegen M, Speelman AD, Overeem S, et al. Promotion of physical activity and fitness in sedentary patients with Parkinson's disease: randomised controlled trial. BMJ 2013;346:f576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Dontje ML, de Greef MHG, Speelman AD, et al. Quantifying daily physical activity and determinants in sedentary patients with Parkinson's disease. Parkinsonism Relat Disord 2013;19:878–882. [DOI] [PubMed] [Google Scholar]
- 38. Ahlskog JE. Does vigorous exercise have a neuroprotective effect in Parkinson disease? Neurology 2011;77:288–294. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Appendix S1. Methodology used in the systematic review and characteristics of intervention in the included studies.


