Short abstract
Background
Around a third of people with multiple sclerosis (MS) experience dysphagia. There is a need for disease-specific information on survival following placement of gastrostomy tube in people with MS.
Objective
We aimed to study survival following gastrostomy in patients with MS.
Methods
We reviewed medical records, home enteral feeding database and death certificates of people with MS who had gastrostomy from 2005 to 2017. Cox regression analysis was performed to identify independent predictors associated with mortality after gastrostomy.
Results
Median survival of 53 patients with MS after gastrostomy was 21.73 months. Median duration of hospital stay after gastrostomy was 14 days (IQR 5.25, 51.5). Survival at 30 days, 3 months, 1, 2, 5 and 10 years were 100% (53/53), 98.1% (52/53), 81.1% (43/53), 54.7% (29/53), 22.4% (11/49) and 6.8% (3/44), respectively. Of 53 patients, 24 died due to respiratory tract infection. Patients who had gastrostomy tube before 50 years of age survived longer (median 28.48 months) compared with those who had the gastrostomy after age 50 years (median 17.51 months) (p = 0.040).
Conclusion
Around 54% of patients with MS survived two or more years following gastrostomy. Younger patients had better survival. The most frequent cause of death was respiratory infection.
Keywords: Multiple sclerosis, gastrostomy, enteral nutrition, deglutition disorders, survival rate, mortality, dysphagia
Introduction
Around a third of people with multiple sclerosis (MS) experience dysphagia, which has a negative impact on quality of life and increases the risk of dehydration and aspiration.1,2 Insertion of a gastrostomy tube allows nutrition and hydration to be administered safely in people with dysphagia. Studies in motor neurone disease have identified that patients find the decision to place a gastrostomy tube a challenge, especially due to lack of disease-specific information.3 There is a paucity of studies describing the outcomes following placement of a gastrostomy tube in patients with MS. This service evaluation aims to describe outcomes for patients with MS following placement of gastrostomy tube.
Materials and methods
Design
We performed a descriptive retrospective case note review.
Participants
Patients diagnosed with MS who had a gastrostomy placed for home enteral feeding (HEF) in Sheffield from 2005 to 2017 were included. We reviewed all patients with MS who had a gastrostomy tube place between 2005 and 2017. The service evaluation was approved by The Clinical Effectiveness Unit of Sheffield Teaching Hospitals NHS Foundation Trust (CEU Registration Number: 8300).
Data collection
The data were retrieved from patients’ hospital medical records, the local HEF team database and certificates of cause of death obtained from Her Majesty’s General Register Office, Southport, United Kingdom. We collected the following data: indication for the gastrostomy tube placement, Expanded Disability Status Scale (EDSS)4 functional score at the time of gastrostomy tube placement, duration of hospital stay, discharge location, date of death and cause of death.
Statistical analyses
Descriptive statistics were performed. Continuous variables were reported using mean ± standard deviation (SD) for normally distributed or median (Inter Quartile Range (IQR) 25, IQR 75) for non-normally distributed variables for Kolmogorov–Smirnov and Shapiro–Wilk tests. Categorical variables are presented as number (percentage). Cumulative survival probability was calculated using the Kaplan–Meier method. Cox regression analysis was performed to identify independent predictors associated with mortality after gastrostomy placement. The results of the regression analysis are represented with odds ratios (ORs) and 95% confidence intervals (CIs). Statistical analyses were performed using SSPS Statistics version 18.0 (SPSS, Inc., Chicago, IL, USA). A p-value <0.05 was considered to be statistically significant.
Results
Fifty-three patients with MS had a gastrostomy tube placed between 2005 and 2017. Baseline characteristics of patients are shown in Table 1. On 31 July 2018, nine patients were alive. Median duration of hospital stay after gastrostomy tube insertion was 14 (IQR 5.25, 51.5) days. Twenty-eight patients (52.8%) were discharged back to their own home and 25 patients (47.2%) to a nursing home.
Table 1.
Clinical features, demographic characteristics and survival of people with MS who had a gastrostomy.
| Total (N = 53) | |
|---|---|
| Age (years), mean ± SD | 55.4 ± 11.4 |
| Sex, n (%) | |
| - Male | 16 (30.2%) |
| - Female | 37 (69.8%) |
| Time from MS diagnosis to gastrostomy (years), mean ± SD | 17.8 ± 9.2 |
| Type of multiple sclerosis, n (%) | |
| - Relapsing–remitting MS | 1 (1.9%) |
| - Primary progressive MS | 5 (9.4%) |
| - Secondary progressive MS | 46 (86.8%) |
| - Unknown | 1 (1.9%) |
| EDSS score at time of gastrostomy, median (IQR), n (%) | 8.5 (8,8.9) |
| - 6 | 1 (1.9%) |
| - 7 | 1 (1.9%) |
| - 7.5 | 5 (9.4%) |
| - 8 | 18 (34%) |
| - 8.5 | 14 (26.4%) |
| - 9 | 7 (13.2%) |
| - 9.5 | 6 (11.3%) |
| - Unknown | 1 (1.9%) |
| Mobility status, n (%) | |
| - Bed bound | 22 (41.5%) |
| - Wheelchair bound | 28 (52.8%) |
| - Mobile with gait aid | 2 (3.8%) |
| - Unknown | 1 (1.9%) |
| Indication for gastrostomy | |
| - Swallowing difficulties | 29 (54.7%) |
| - Aspiration pneumonia or recurrent pneumonia | 14 (26.4%) |
| - Malnutrition or weight loss | 5 (9.4%) |
| - Unsafe swallow | 3 (5.7%) |
| - Prolonged intubation | 1 (1.9%) |
| - Unknown | 1 (1.9%) |
| Type of surgery | |
| -Emergency | 28 (52.8%) |
| -Elective | 24 (45.3%) |
| -Unknown | 1 (1.9%) |
| Location after discharge from hospital, n (%) | |
| -Own home | 28 (52.8%) |
| -Nursing home | 25 (47.2%) |
| Survival after gastrostomy | |
| 30 day | 53/53 (100%) |
| 3 months | 52/53 (98.1%) |
| 12 months | 43/53 (81.1%) |
| 24 months | 29/53 (54.7%) |
| 60 months | 11/49 (22.4%) |
| 120 months | 3/44 (6.8%) |
Median survival time was 21.73 (IQR 12.54, 39.67) months. Survival after gastrostomy is shown in Table 1. Cause of death as recorded in the Medical Certificates was respiratory tract infection (24), multiple sclerosis or frailty (14), osteomyelitis and pressure sore (1), urinary tract infection (1), intestinal obstruction (1), respiratory arrest following prolonged status epilepticus (1), asthma (1) and unknown (1).
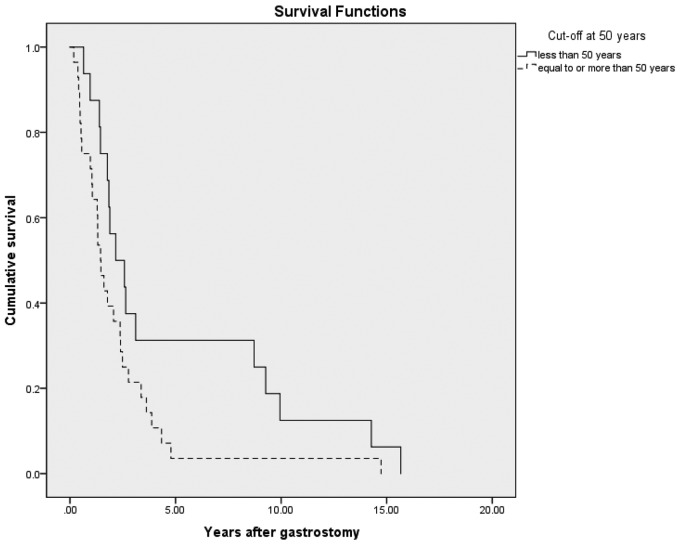
Patients who had gastrostomy tube before 50 years of age survived longer (median 28.48 months) compared with those who had the gastrostomy after age 50 years (median 17.51 months) (p = 0.040). Cox regression analysis showed that age more than 50 years at gastrostomy tube insertion was a significant predictor of shorter survival (OR 1.028) (1.001–1.057, 95% CI) (p = 0.044) (Figure 1). The duration of MS (p = 0.132), EDSS score (p = 0.647), type of MS (p = 0.668), gender (p = 0.098), mobility (p = 0.564), elective/emergency surgery (p = 0.841) and location after discharge from hospital (p = 0.479) did not predict survival after gastrostomy.
Figure 1.
Cox regression analysis comparing survival after gastrostomy for patients with MS of age more than 50 years and 50 years or less.
Y axis: Cumulative survival; X axis: Number of years after gastrostomy.
Discussion
This is the largest dataset on patients with MS on gastrostomy tube for HEF. A retrospective study and literature review about percutaneous endoscopic gastrostomy tube placement in neurodegenerative diseases showed that there were no studies that focused on the outcomes of patients with MS.5 Among 40 patients (13 with multiple sclerosis) the 30-day mortality was 3/40 (8%). The 30-day mortality after the gastrostomy placement in people with neurological disease is between 0% and 28%.5 Survival of patients with gastrostomy in our study at 30 days was 100%. The 3 months, 1 and 2 year values were also better than the survival reported in 500 patients with neurological disorders requiring gastrostomy. However, survival at 5 years in our study is 22.4%, which was less than the 32.2% reported in this cohort.6
More than 80% of patients with MS survived more than a year and more than 50% survived 2 years after gastrostomy. HEF is likely to extend the survival of people with dysphagia due to MS. Most frequent cause of death in our cohort was respiratory tract infection, which was similar to a previous study about mortality after gastrostomy in patients with neurological dysphagia.7 While gastrostomy may help meet patients’ nutritional requirements, it may not prevent aspiration pneumonia. Previous studies reported that older age was associated with poorer outcome following gastrostomy.5,8,9 We also noted that older age at the time of gastrostomy insertion was a significant predictor of shorter survival. In these studies the cut-off age for poor survival after gastrostomy for neurogenic dysphagia was 75 years.5,8,9 Our data found that the cut-off age for poor survival in patients with MS patient was 50 years. This could be because, unlike other neurodegenerative conditions causing dysphagia, MS is predominately a disease of young working-age adults. This may help clinicians in their discussions with patients with MS and their families about placement of a gastrostomy tube for HEF.
Limitations
This was a retrospective medical records review. We did not evaluate patient-reported outcomes, the challenges patients faced with HEF and impact on quality of life. Around half (25/53) of our patients were discharged to a care home. We did not look into the reason for discharge to care home. Our data should not be interpreted as 50% of patients need care home due to gastrostomy tube placement. The goals of gastrostomy could be prevention of aspiration, improve nutrition and hydration and improve quality of life. The goal of gastrostomy was not explicitly stated in the medical records or our database. We also do not have data on people with MS who refused gastrostomy. Our data do not answer the question “Can gastrostomy extend survival, improve nutrition and prevent aspiration in MS patients who have indication for gastrostomy insertion?” A prospective study, with patients who refuse gastrostomy as control, may be helpful in answering these important questions.
Conclusion
Patients with MS survive 2 years and longer after placement of gastrostomy tube for HEF. The most common cause of death was respiratory infection. This information will help inform clinicians and patients with MS making decisions regarding gastrostomy tube placement. Further prospective research is required to evaluate the outcomes of patients with MS on HEF, particularly as the condition progresses.
Contributor Information
Lisa Grandidge, Princess Royal Spinal Injuries and Neurorehabilitation Centre, Northern General Hospital, Herries Road, Sheffield, UK.
Jessica Denning, Dietetic Department, Northern General Hospital, Herries Road, Sheffield, UK.
Krishnan Padmakumari Sivaraman Nair, Department of Neurology, Royal Hallamshire Hospital, Sheffield Teaching Hospitals NHS Foundation Trust, Sheffield, UK.
Conflicting of Interests
The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: Dr Chayaporn Chotiyarnwong was funded by a research fellowship from the Faculty of Medicine Siriraj Hospital, Mahidol University, Bangkok, Thailand. Other authors received no financial support for research, authorship or publication of this article.
ORCID iD
Krishnan Padmakumari Sivaraman Nair https://orcid.org/0000-0002-4004-2315
References
- 1.Guan XL, Wang H, Huang HSet al. Prevalence of dysphagia in multiple sclerosis: A systematic review and meta-analysis. Neurol Sci 2015; 36(5): 671–681. [DOI] [PubMed] [Google Scholar]
- 2.Marchese-Ragona R, Restivo DA, Marioni Get al. Evaluation of swallowing disorders in multiple sclerosis. Neurol Sci 2006; 27: S335–S337. [Google Scholar]
- 3.Stavroulakis T, Baird WO, Baxter SKet al. Factors influencing decision-making in relation to timing of gastrostomy insertion in patients with motor neurone disease. BMJ Support Palliat Care 2014; 4(1): 57–63. [DOI] [PubMed] [Google Scholar]
- 4.Kurtzke JF. Rating neurologic impairment in multiple sclerosis: An Expanded Disability Status Scale (EDSS). Neurology 1983; 33(11): 1444–1452. [DOI] [PubMed] [Google Scholar]
- 5.Sarkar P, Cole A, Scolding NJet al. Percutaneous endoscopic gastrostomy tube insertion in neurodegenerative disease: A retrospective study and literature review. Clin Endosc 2017; 50(3): 270–278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Kara O, Kizilarslanoglu MC, Canbaz Bet al. Survival after percutaneous endoscopic gastrostomy in older adults with neurologic disorders. Nutr Clin Pract 2016; 31(6): 799–804. [DOI] [PubMed] [Google Scholar]
- 7.Azzopardi N, Ellul P. Pneumonia and mortality after percutaneous endoscopic gastrostomy insertion. Turk J Gastroenterol 2013; 24(2): 109–116. [DOI] [PubMed] [Google Scholar]
- 8.Arora G, Rockey D, Gupta S. High In-hospital mortality after percutaneous endoscopic gastrostomy: Results of a nationwide population-based study. Clin Gastroenterol Hepatol 2013; 11(11): 1437–1444. [DOI] [PubMed] [Google Scholar]
- 9.Janes SE, Price CS, Khan S. Percutaneous endoscopic gastrostomy: 30-day mortality trends and risk factors. J Postgrad Med 2005; 51(1): 23–28; discussion 28–29. [PubMed] [Google Scholar]