Abstract
Study Design:
Literature review.
Objective:
To conduct a literature review of studies reporting the incidence of pars interarticularis defects in athletes of specific sports, in order to allow more targeted prevention and treatment strategies to be implemented for the groups at highest risk.
Methods:
Electronic searches were performed using PubMed, Ovid Medline, EMBASE, Google Scholar, Cochrane Database of Systematic Reviews, and Cochrane Database of Controlled Trials from their dates of inception to September 2017, with the following keywords: “spondylolysis,” “sports,” “low back pain,” and “pars defects.”
Results:
A total of 509 total articles were retrieved, of which 114 were used in the final review. The incidence of pars interarticularis defects was found to be highest in diving (35.38%), cricket (31.97%), baseball/softball (26.91%), rugby (22.22%), weightlifting (19.49%), sailing (17.18%), table tennis (15.63%), and wrestling (14.74%). Only 5 studies reported the management instituted for their participants, and these were all case reports. Of 74 players with spondylolysis in these studies, 70 (94.59%) underwent conservative treatment and 4 (5.41%) underwent surgical treatment. 61 (82.43%) returned to their previous level of play, 6 (8.11%) retired, and the disposition of the final 7 was not reported.
Conclusion:
The current medical literature provides good evidence that the incidence of pars interarticularis defects is higher in the athletic population, with the highest incidence in diving. There remains no gold standard protocol for the management of pars interarticularis defects. Further research is required to compare conservative therapy to surgical therapy and to compare the various surgical techniques to each other.
Keywords: spondylolysis, incidence, athletes, sports, review, low back pain, prevalence
Introduction
Pars interarticularis defects relate to spondylolysis and/or spondylolisthesis of the spinal vertebra. The pars interarticularis is the segment of bone bounded by the lamina, pedicle, inferior articular process, and superior articular process of each vertebra (Figures 1 and 2). Pars interarticularis defects begin as stress reactions (pre-lytic stage), then progress to acute fractures (spondylolysis) and eventually chronic fractures.1 Complete fractures of the pars interarticularis may lead to anterolisthesis of the affected vertebra relative to the vertebra immediately inferior to it2 (spondylolisthesis), at which point neurological symptomatology may occur.
Figure 1.
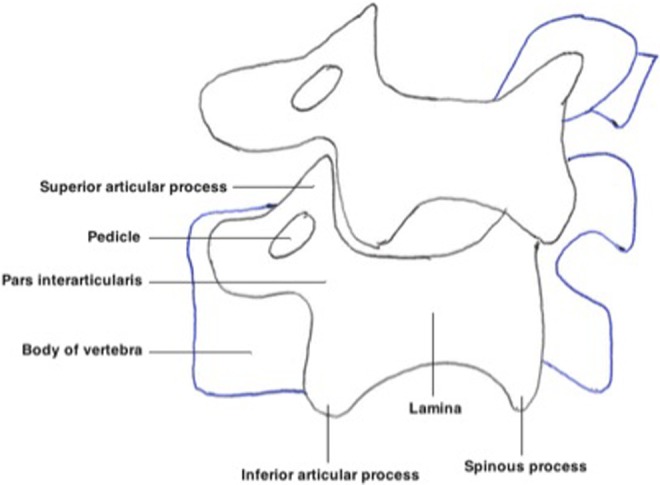
Diagrammatic representation of 2 lumbar vertebra. The pars interarticularis is the region between the lamina, pedicle, superior articular process, and inferior articular process of each vertebra. Each vertebra resembles a “Scotty dog,” with defect across the pars interarticularis producing the “Scotty dog collar” sign.
Figure 2.
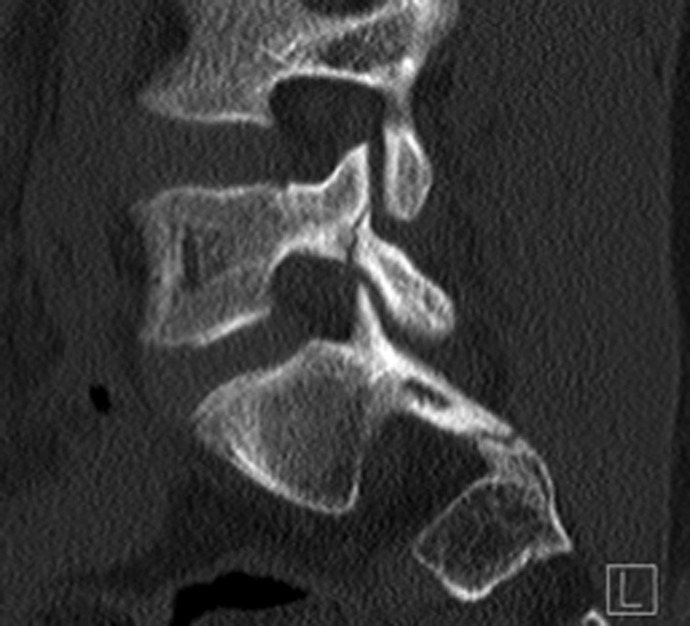
X-ray of the lumbar spine (lateral view) showing a spondylolytic defect.
The patient with lumbar spondylolysis typically complains of progressive back pain in the lumbar region, exacerbated by extension or twisting of the spine.3 Radicular pain and urinary disturbances are uncommon unless nerve root compression has occurred as a result of spondylolisthesis. A social history indicates previous or current athletic activity in 93% of spondylolysis patients.4 There may be a family history of spondylolysis, spondylolisthesis, or spina bifida occulta.5 On examination, there may be loss of lumbar lordosis, as well as restricted lumbar flexion and extension. Paraspinal muscle spasm and tenderness often occurs.6 The pathognomonic sign is the one-legged hyperextension test (stork test), but this test is not sensitive7 or specific8 enough to be relied on for assessment. If spondylolisthesis is present, hamstring tightness leads to shortened stride with hip and knee flexion.9 There may also be lumbar hyperlordosis leading to the appearance of excessive abdominal convexity.10,11 Neurological signs are rare, occurring only if nerve root compression has developed.6,12
Spondylolysis is most commonly bilateral13 (Figure 3), possibly because unilateral spondylolysis increases stress on the contralateral pedicle.14 The majority of spondylolysis occurs in L5, followed by L4, then combined L4-L5 involvement (Table 1).15-21 Furthermore, the severity of spondylolysis varies with location. Sixty-three percent of L5 spondylolysis exhibits terminal-stage defects despite young skeletal age, while most L3/L4 spondylolysis exhibits early-stage defects.4
Figure 3.
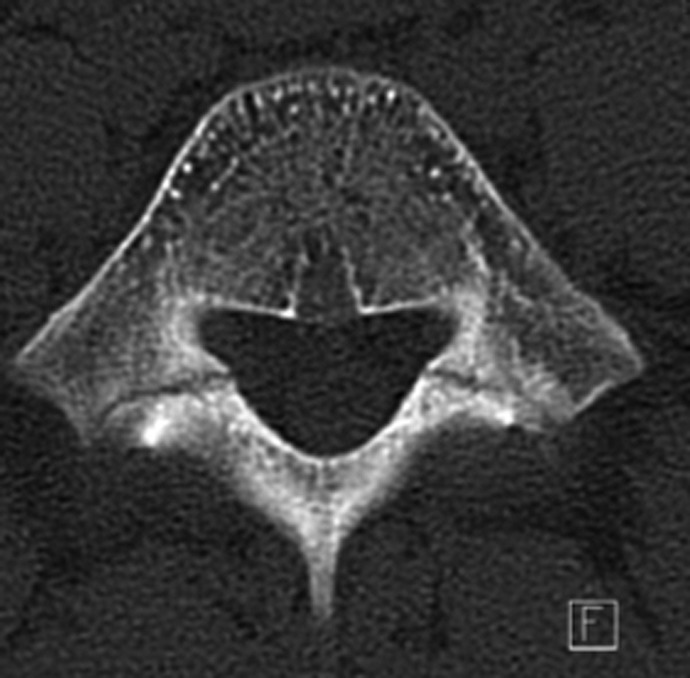
X-ray of the lumbar spine (axial view) showing bilateral spondylolytic defects. This radiograph is from one of the author’s patients.
Table 1.
Proportion of Spondylolysis Occurring at Specific Lumbar Levels.a
| Lumbar Level of Spondylolysis | Incidence (%) |
|---|---|
| L1 | 0-5 |
| L2 | 0-5 |
| L3 | 0-5 |
| L4 | 5-23 |
| L5 | 71-95 |
a The majority of lumbar spondylolysis occurs at L5 (71%-95%) followed by L4 (5%-23%). Spondylolysis at L1-L3 is rare (0%-5% each).
The incidence of spondylolysis has been shown to be 6% in the general adult population.17 The incidence is significantly higher in the athletic population, with studies showing as many as 52% of athletes with low back pain suffering spondylolysis and 60% with low back pain suffering a pars interarticularis defect of any grade.7 Other studies show that spondylolysis and spondylolisthesis constitute 47% of low back pain in adolescent athletes.22 Athletic participation is indeed a well-known risk factor for the development of pars interarticularis defects, but studies on the incidence of pars interarticularis defects often have 1 of 3 limitations: (a) small sample sizes; (b) the athletes being studied are from the same sporting institutions, the sporting styles of which may independently contribute to pars interarticularis defects; or (c) the studies measure incidence in a small number of sports. As such, this article aims to systematically review the current literature on the incidence of pars interarticularis defects in athletes, with detailed knowledge about particularly high-risk sports allowing the development of more targeted and effective prevention and treatment strategies in the future.
Methods
Data Sources
The authors performed a comprehensive search of the published medical literature, using the following electronic databases from their dates of inception to September 2017: PubMed, Ovid Medline, EMBASE, Google Scholar, Cochrane Database of Systematic Reviews, and Cochrane Database of Controlled Trials. Searches were performed with the following terms as MeSH headings and keywords, with Boolean operations, including “AND” and “OR”: “spondylolysis,” “sports,” “low back pain,” and “pars defects.” Synonyms were used to identify the remainder of relevant studies. Citations and abstracts were retrieved. A hand search of the bibliographies was also performed to identify relevant articles missed by the electronic search. Two independent researchers performed the literature search.
Study Selection Criteria
Articles were included in the current review if their primary subject matter was the classification, epidemiology, risk factors, diagnosis, or management of pars interarticularis defects, or if they discussed pars interarticularis defects in athletic populations. Articles were excluded if the athletic population was not a significant focus of the article, or if they discussed the total incidence of spinal disorders without providing statistics specifically on pars interarticularis defects. Articles were also excluded if they were not in English, unless the statistics from such articles were recounted in other English articles, in which case they were included in the current review. The articles were reviewed for inclusion or exclusion independently by 2 of the authors, and disputes were resolved by group consensus.
Results
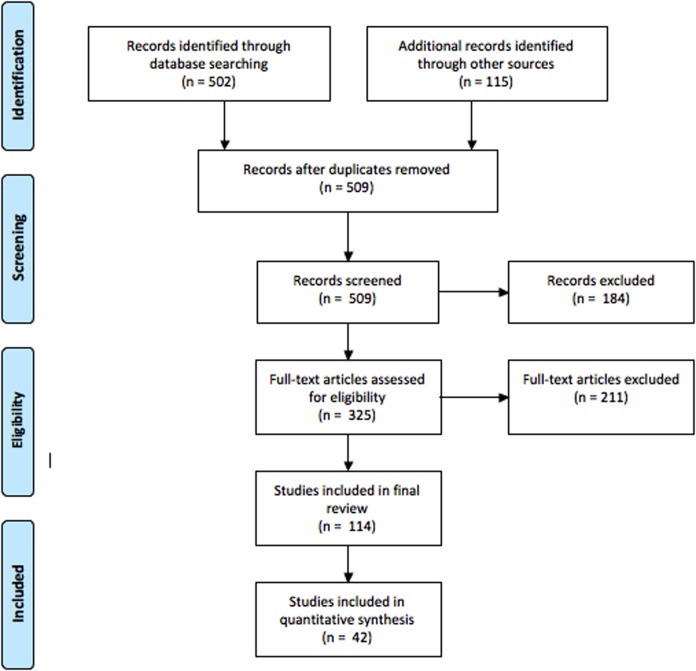
A total of 502 articles were retrieved from database searches, and 115 were retrieved from the reference lists of articles (n = 617). There were 108 duplicate articles, 37 articles not in English, 77 irrelevant articles, 68 articles outside the scope of the current review, 1 commentary, and 1 opinion article (n = 325). Of the 325 remaining articles, 114 were required for the current review with quantitative data collected from 42 articles (Figure 4).
Figure 4.
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.23 A total of 504 original articles were retrieved. A total of 114 articles were used in the final review with quantitative data retrieved from 42 of these articles.
Epidemiology
The incidence of spondylolysis in neonates is zero,17,24 4.4% in 6-year-olds, and 6% in adults.17 The incidence in athletic populations is considerably higher (Table 2). Approximately 75% of spondylolysis will develop into spondylolisthesis.17
Table 2.
Incidence of Pars Interarticularis Defects by Sport.
| Sport | Sample Size | Athletes With at Least One Pars Interarticularis Defect | |
|---|---|---|---|
| n | % | ||
| Archery | |||
| Rossi et al26 | 26 | 0 | 0 |
| Soler et al27 | 44 | 1 | 2.27 |
| Total | 70 | 1 | 1.43 |
| Badminton | |||
| Kobayashi et al31 | 3 | 2 | 66.66 |
| Soler et al27 | 38 | 2 | 5.26 |
| Total | 41 | 4 | 9.76 |
| Baseball | |||
| Rossi et al26 | 21 | 1 | 4.76 |
| Kobayashi et al31 | 60 | 37 | 61.67 |
| Kobayashi et al31,a | 3 | 0 | 0 |
| Kono et al36 | 91 | 14 | 15.38 |
| Akimoto et al37 | 143 | 18 | 12.59 |
| Hasegawa et al59 | 95 | 22 | 23.16 |
| Matsumoto et al60 | 40 | 11 | 27.5 |
| Wakitani et al61 | 71 | 38 | 53.52 |
| Total | 524 | 141 | 26.91 |
| Basketball | |||
| Kono et al36 | 66 | 9 | 13.64 |
| Rossi et al26 | 174 | 17 | 9.77 |
| Kobayashi et al31 | 30 | 15 | 50 |
| Soler et al27 | 288 | 19 | 6.6 |
| Akimoto et al37 | 96 | 11 | 11.46 |
| Total | 654 | 71 | 10.86 |
| Baton twirling | |||
| Kobayashi et al31 | 1 | 0 | 0 |
| Bobsledding | |||
| Rossi et al26 | 36 | 5 | 13.88 |
| Rossi et al26,b | 25 | 2 | 8 |
| Soler et al27 | 15 | 3 | 20 |
| Total | 76 | 10 | 13.16 |
| Boxing | |||
| Rossi et al26 | 27 | 3 | 11.11 |
| Soler et al27 | 21 | 3 | 14.29 |
| Total | 48 | 6 | 12.5 |
| Canoeing | |||
| Rossi et al26 | 69 | 8 | 11.59 |
| Soler et al27 | 162 | 10 | 6.17 |
| Total | 231 | 18 | 7.79 |
| Cricket (fast bowling) | |||
| Crewe et al41 | 46 | 15 | 32.61 |
| Ranson et al34 | 28 | 12 | 42.86 |
| Hardcastle et al42 | 22 | 12 | 54.54 |
| Engstrom et al43 | 51 | 18 | 35.29 |
| Foster et al44 | 82 | 9 | 10.98 |
| Annear et al45 | 20 | 9 | 45 |
| Elliott et al46 | 20 | 11 | 55 |
| Total | 269 | 86 | 31.97 |
| Cycling | |||
| Rossi et al26 | 95 | 13 | 13.68 |
| Soler et al27 | 175 | 11 | 6.29 |
| Total | 270 | 24 | 8.89 |
| Diving | |||
| Rossi et al26 | 57 | 23 | 40.35 |
| Soler et al27 | 8 | 0 | 0 |
| Total | 65 | 23 | 35.38 |
| Equestrian | |||
| Rossi et al26 | 83 | 5 | 6.02 |
| Soler et al27 | 16 | 0 | 0 |
| Total | 99 | 5 | 5.05 |
| Fencing | |||
| Rossi et al26 | 143 | 19 | 13.28 |
| Soler et al27 | 56 | 6 | 10.71 |
| Total | 199 | 25 | 12.56 |
| Football (American) | |||
| Jones et al51 | 104 | 5 | 4.81 |
| Rossi et al26 | 400 | 65 | 16.25 |
| McCarroll et al52 | 145 | 22 | 15.2 |
| Soler et al27 | 13 | 0 | 0 |
| Semon et al53 | 58 | 12 | 20.69 |
| Iwamoto et al54 | 742 | 77 | 10.38 |
| Ferguson et al55 | 12 | 6 | 50 |
| Abe et al56 | 210 | 42 | 20 |
| Total | 1720 | 229 | 13.32 |
| Golf | |||
| Rossi et al26 | 38 | 2 | 5.26 |
| Soler et al27 | 52 | 1 | 1.92 |
| Total | 90 | 3 | 3.33 |
| Gymnastics | |||
| Rossi et al26 | 673 | 112 | 16.64 |
| Mohriak et al62 | 18 | 1 | 5.56 |
| Kobayashi et al31 | 5 | 2 | 40 |
| Toueg et al11 | 92 | 6 | 6.52 |
| Sward et al32 | 52 | 8 | 15.38 |
| Toueg et al63 | 93 | 6 | 6.45 |
| Soler et al27 | 235 | 33 | 14.04 |
| Bennett et al64 | 13 | 4 | 30.77 |
| Kono et al36 | 49 | 4 | 8.16 |
| Akimoto et al37 | 61 | 5 | 8.2 |
| Jackson et al65 | 100 | 11 | 11 |
| Total | 1391 | 192 | 13.80 |
| Handball | |||
| Rossi et al26 | 42 | 3 | 7.14 |
| Kobayashi et al31 | 1 | 0 | 0 |
| Soler et al27 | 67 | 5 | 7.46 |
| Total | 110 | 8 | 7.27 |
| Hockey (ice and field) | |||
| Rossi et al26 | 170 | 13 | 7.64 |
| Soler et al27 | 106 | 3 | 2.83 |
| Donaldson et al25 | 25 | 11 | 44 |
| Suzuki et al28 | 63 | 10 | 15.87 |
| Total | 364 | 37 | 10.16 |
| Javelin | |||
| Schmitt et al66 | 21 | 14 | 66.67 |
| Martial arts | |||
| Rossi et al26 | 64 | 10 | 15.62 |
| Kobayashi et al31 | 3 | 1 | 33.33 |
| Kobayashi et al31 | 2 | 1 | 50 |
| Soler et al27 | 43 | 4 | 9.3 |
| Kono et al36 | 38 | 4 | 10.53 |
| Akimoto et al37,c | 40 | 5 | 12.5 |
| Akimoto et al37,d | 49 | 5 | 10.2 |
| Kuroki et al67 | 21 | 7 | 33.33 |
| Total | 260 | 37 | 14.23 |
| Motorcycling | |||
| Rossi et al26 | 8 | 0 | 0 |
| Mountaineering | |||
| Soler et al27 | 63 | 1 | 1.59 |
| Paddleball | |||
| Soler et al27 | 20 | 2 | 10 |
| Pole vaulting | |||
| Rebella et al68 | 135 | 4 | 2.96 |
| Rowing | |||
| Maurer et al69 | 22 | 6 | 27.27 |
| Rossi et al26 | 246 | 19 | 7.72 |
| Soler et al27 | 77 | 13 | 16.88 |
| Total | 345 | 38 | 11.01 |
| Rugby | |||
| Rossi et al26 | 65 | 7 | 10.76 |
| Kobayashi et al31 | 5 | 1 | 20 |
| Soler et al27 | 40 | 2 | 5 |
| Abe et al56 | 169 | 52 | 30.77 |
| Total | 279 | 62 | 22.22 |
| Sailing | |||
| Rossi et al26 | 128 | 22 | 17.18 |
| Shooting | |||
| Rossi et al26 | 76 | 8 | 10.52 |
| Soler et al27 | 81 | 4 | 4.94 |
| Total | 157 | 12 | 7.64 |
| Skating (ice) | |||
| Rossi et al26 | 42 | 3 | 7.14 |
| Skating (roller) | |||
| Soler et al27 | 7 | 0 | 0 |
| Skiing | |||
| Rossi et al26 | 154 | 25 | 16.23 |
| Rossi et al26,e | 18 | 2 | 11.11 |
| Soler et al27 | 77 | 6 | 7.79 |
| Total | 249 | 33 | 13.25 |
| Soccer | |||
| Kobayashi et al31 | 47 | 25 | 53.19 |
| Sward et al32 | 31 | 2 | 6.45 |
| Soler et al27 | 55 | 1 | 1.82 |
| Murase et al70 | 160 | 14 | 8.75 |
| Kono et al36 | 264 | 23 | 8.71 |
| Akimoto et al37 | 320 | 28 | 8.75 |
| Kyo et al71 | 37 | 18 | 48.65 |
| Matsumoto et al60 | 60 | 19 | 31.67 |
| Total | 974 | 130 | 13.35 |
| Sumo | |||
| Nakagawa72 | 37 | 5 | 13.51 |
| Swimming | |||
| Rossi et al26,f | 307 | 34 | 11.07 |
| Kobayashi et al31 | 1 | 1 | 100 |
| Engstrom et al.43 | 20 | 4 | 20 |
| Soler et al27 | 176 | 18 | 10.23 |
| Soler et al27,g | 11 | 1 | 9.09 |
| Kono et al36 | 55 | 10 | 18.18 |
| Akimoto et al37 | 117 | 12 | 10.26 |
| Total | 687 | 80 | 11.64 |
| Table tennis | |||
| Rossi et al26 | 1 | 0 | 0 |
| Kobayashi et al31 | 4 | 3 | 75 |
| Kono et al36 | 25 | 3 | 12 |
| Akimoto et al37 | 34 | 4 | 11.76 |
| Total | 64 | 10 | 15.63 |
| Tennis | |||
| Rossi et al26 | 306 | 36 | 11.76 |
| Kobayashi et al31 | 10 | 4 | 40 |
| Sward et al32 | 30 | 3 | 10 |
| Soler et al27 | 91 | 1 | 1.1 |
| Maquirriain et al33 | 139 | 3 | 2.16 |
| Alyas et al73 | 33 | 9 | 27.27 |
| Rajeswaran et al35 | 98 | 29 | 29.59 |
| Kono et al36 | 53 | 8 | 15.09 |
| Akimoto et al37 | 67 | 9 | 13.43 |
| Total | 827 | 102 | 12.33 |
| Track and field | |||
| Rossi et al26 | 353 | 61 | 17.28 |
| Rossi et al26,h | 54 | 11 | 20.37 |
| Kobayashi et al31 | 13 | 4 | 30.77 |
| Soler et al27 | 685 | 61 | 8.91 |
| Kono et al36 | 144 | 19 | 13.19 |
| Akimoto et al37 | 206 | 23 | 11.17 |
| Soler et al27,i | 9 | 0 | 0 |
| Soler et al27,j | 90 | 7 | 7.78 |
| Total | 1554 | 186 | 11.97 |
| Volleyball | |||
| Rossi et al26 | 150 | 16 | 10.66 |
| Kobayashi et al31 | 12 | 1 | 8.33 |
| Soler et al27 | 70 | 7 | 10 |
| Külling et al12 | 29 | 6 | 20.69 |
| Akimoto et al37 | 53 | 2 | 3.77 |
| Total | 314 | 32 | 10.19 |
| Weight lifting | |||
| Rossi et al26 | 112 | 25 | 22.32 |
| Kotani et al74 | 26 | 8 | 30.77 |
| Soler et al27 | 85 | 11 | 12.94 |
| Granhed et al75 | 13 | 2 | 15.38 |
| Total | 236 | 46 | 19.49 |
| Wrestling | |||
| Rossi et al26 | 80 | 20 | 25 |
| Soler et al27 | 143 | 16 | 11.19 |
| Sward et al32 | 30 | 2 | 6.67 |
| Granhed et al75 | 32 | 4 | 12.5 |
| Total | 285 | 42 | 14.74 |
a Softball.
b Luge, not bobsledding.
c Judo.
d Kendo.
e Water skiing.
f Synchronized swimming and water polo.
g Synchronized swimming.
h Pentathlon/triathlon.
i Pentathlon.
j Triathlon.
Hockey
The incidence of pars defects in hockey players has been reported as 2.83% to 44%,25-28 with spondylolisthesis occurring in 15.9% of this population.29 The majority of players affected are forwards, with a greater proportion of spondylolysis ipsilateral to their handedness.25 Defense players more commonly present with spondylolysis contralateral to their handedness.25 This difference may be accounted for by the different spinal motions required of players in different positions. Forward players are required to shoot the puck on the side of their handedness, leading to ipsilateral spondylolysis. Defense players are required to quickly twist and turn in both directions while defending against players of the opposing team, leading to contralateral spondylolysis.
Tennis
Pars defects are more common in elite tennis players than the nonathletic population,30 with spondylolysis occurring in 1.1% to 40%26,27,31-37 of this population due to the excessive forces placed on the lumbar spine during the service game.38 The topspin serve puts players at a greater risk of lumbar injury than the flat or slice serves,38-40 since it involves a racquet head more posterior and more medial to the shoulder compared with the flat and slice serves.39
Diving
Pars defects in athletic divers have a reported incidence of 0% to 40.35%,26,27 with the incidence of 0% likely due to the small sample size studied (n = 8).27 Divers reach speeds of 51 km/h before entering the water, then decelerate to 33 km/h on impact with the water, exerting a strong physical force on their lumbar spines.3 Divers with low back pain have a larger trunk extension angle than those without low back pain. Trunk extension angle corresponds to the shoulder flexion angle, so having a flexible shoulder can decrease the trunk extension angle in divers, thereby decreasing the risk of low back pain.3 These results may apply to other sports involving compound movements such as gymnastics and throwing sports.
Volleyball
A total of 3.77% to 20.69% of beach volleyball players suffer from spondylolysis.12,26,27,31,37 This increased prevalence is due to the powerful overhead hitting motion that volleyball players employ during serve or smash movements, causing malalignment of the shoulders relative to the hips. When this is combined with repetitive lumbar hyperextension to increase the force exerted on the ball, spondylolysis occurs.12
Cricket
The incidence of spondylolysis in cricket players is 10.98% to 55%.34,41-46 L5 is the most commonly affected spinal level, with L4 and L3 less commonly affected.45,47 Defects tend to arise contralateral to the bowling arm, perhaps explaining why such defects are more common on the left than the right.42,47 Spondylolisthesis occurs commonly in bilateral pars defects of these athletes, but is rare in unilateral defects.48 This occurs primarily due to the bowling movement, which requires lumbar flexion, hyperextension, and lateral rotation. Also, reaction forces from the ground on the front foot and back foot, transmitted through the lumbar spine during delivery, are significantly higher than body weight.45,48 A mixed front-and-side bowling style provides a higher risk of spondylolysis than front-only and side-only bowling styles, due to higher degrees of these lumbar movements.42,46,49,50
Rugby, American Football and Other Contact Sports
Spondylolysis occurs in 0% to 50% of American football players26,27,51-56 and 5% to 30.77% of rugby players.26,27,31,56 The lower limit of 0% for American football can be attributed to the small sample size studied (n = 13).27 These contact sports are different from noncontact sports such as gymnastics, because collision exerts an extra axial loading force on the spine that is not present in noncontact sports. Also, locking of the lumbosacral spine (which physiologically protects the spine) cannot adequately occur in contact sports since there are multiple concurrent forces on the athlete as they compete for possession of the ball.57 In rugby, lumbar spinal injuries occur most commonly in defensive players due to the axial loading forces during defensive tackles. The scrum and spear tackle also exert further axial and rotational forces which ultimately increase the incidence of pars defects in this athletic population.58
Classification
The currently accepted classification system for spondylolysis (Table 3) (type IIa spondylolisthesis) is based on the progression of pathological changes that occur in pars interarticularis defects. Radiological magnetic resonance imaging (MRI) changes are grouped in 5 grades (grades 0-4).1 Grade 0 is a normal pars interarticularis, with no evidence of stress reaction. Grade 1 refers to T2 signal abnormalities of the pars interarticularis but not of the adjacent pedicle or articular process, representing a bone marrow stress reaction (edema) without cortical disruption. Grade 2 refers to T2 signal abnormalities and thinning, fragmentation or irregularity of the pars interarticularis on T1 or T2 image, representing incomplete pars interarticularis fractures that have not yet caused cortical disruption. Grade 3 refers to complete unilateral or bilateral cortical disruption (spondylolysis) with T2 signal abnormalities, representing acute complete fractures of the pars interarticularis. Grade 4 involves cortical disruption without abnormal T2 signals, representing old pars interarticularis fractures that have not united.76
Table 3.
Classification of Pars Interarticularis Defects (Type IIa Spondylolisthesis) by Radiological and Pathological Features.a
| Grade | Radiological Change | Pathological Change |
|---|---|---|
| 0 | Nil | Nil |
| 1: Stress reaction | T2 signal abnormalities, with no pars defect on T1/T2 images | Bone marrow edema |
| 2: Incomplete fracture | T2 signal abnormalities, with thinning, fragmentation, or irregularity of the pars interarticularis on T1 or T2 images | Bone marrow oedema with pars defect (incomplete fracture), but spondylolysis (cortical disruption) has not yet occurred |
| 3: Complete fracture | Cortical disruption on T1/T2 images, with T2 signal abnormalities present | Cortical disruption (spondylolysis) has occurred and bone marrow edema is present, but reunion is still possible |
| 4: Chronic complete fracture | Cortical disruption on T1/T2 images, with no T2 signal abnormalities present | Complete pars interarticularis fracture that has never reunited, with no associated bone marrow edema |
a Spondylolysis is characterized by cortical disruption (grade 3 and 4 defects). Grade 1 and 2 defects are prespondylolytic.
The 5 grades of radiological changes can be used in various combinations to produce classifications of varying categories. Currently, most classifications use a 5-category system (grade 0, grade 1, grade 2, grade 3, grade 4), but the most reliable is likely to be a 3-category system (grade 0, grades 1-3, grade 4).1 In any case, the classification used must achieve adequate accuracy while still being able to differentiate between the various stages of pars interarticularis damage.
The currently accepted classification of spondylolisthesis (Table 4) is based on etiology: type I (dysplastic), type II (isthmic), type III (degenerative), type IV (traumatic), type V (pathologic), and type VI (postsurgical).2 Dysplastic spondylolisthesis occurs due to a congenital defect in the neural arch. Isthmic spondylolisthesis occurs due to a defect in the pars interarticularis, and has 3 subtypes: type IIa (spondylolytic, occurring due to stress fractures of the pars, such as by repetitive hyperextension and twisting), type IIb (repeated microtrauma occurs to the pars; as it heals, nonlinear forces cause the pars to elongate and thin, making it susceptible to future fracture), and type IIc (acute traumatic fracture of the pars). Degenerative spondylolisthesis occurs due to progressive degeneration of the facet joint complex (eg, capsule, ligaments). Traumatic spondylolisthesis is caused by acute spinal trauma, which leads to a posterior column fracture, but not pars fracture. Pathologic spondylolisthesis occurs due to a pathological process such as infection, malignancy, or endocrine disorder. Postsurgical spondylolisthesis occurs due to postsurgical lumbar instability. The focus of this review is pars interarticularis defects in athletes (type IIa spondylolisthesis).
Table 4.
Classification of Spondylolisthesis by Etiology.a
| Type | Etiology | Pathogenesis |
|---|---|---|
| I | Dysplastic | Congenital defect in the neural arch |
| II | Isthmic | Pars interarticularis defect |
| IIa | Stress fracture of the pars (spondylolysis) | |
| IIb | Repeated microtrauma and nonlinear forces cause elongation of the pars | |
| IIc | Acute traumatic fracture of the pars | |
| III | Degenerative | Degeneration of the facet joint complex (capsule, ligaments) |
| IV | Traumatic | Acute traumatic fracture of posterior column, but not the pars |
| V | Pathologic | Infection, neoplasm, endocrine disorder, or other pathology causes vertebral instability |
| VI | Postsurgical | Postsurgical lumbar instability |
a Pars interarticularis defects in athletes correspond to type IIa spondylolisthesis.
Spondylolisthesis may also be classified into developmental and acquired causes.77,78 Developmental spondylolisthesis corresponds to the dysplastic and isthmic etiologies. Acquired spondylolisthesis corresponds to the traumatic, pathologic and postsurgical etiologies.
Risk Factors
Known risk factors for pars interarticularis defects include childhood/adolescence, male sex, race, particular sports, and other lifestyle choices that lead to repetitive hyperextension and rotation of the lumbar spine.24,79-81 Possible risk factors include family history and spina bifida occulta.4,5
Spondylolysis is more common in children since their bones are still in the growth stages, with weaker osteochondral junctions and thinner cortices. Children also participate more frequently in physical activity than adults, not allowing sufficient time for recovery from microtrauma.79 Another reason that children develop pars defects more commonly than adults is that children can develop injuries due to unaccustomed loads. In other words, a child who is an expert at soccer may be injured playing a sport they are not accustomed to (eg, tennis), even if tennis presents similar loading forces on the body. Contrastingly, adults do not often develop injuries from unaccustomed loads.82 Males develop spondylolysis more commonly than females with a ratio of 2:1,24,80 but females are more likely to develop severe spondylolisthesis.83 Incidence in white males is 6.4%, black males is 2.8%, white females is 2.3%, and black females is 1.1%.24 Eskimos have the highest incidence,81 supporting a genetic predisposition to spondylolysis.5 Spondylolysis occurs more commonly in athletes81 due to repetitive hyperextension and twisting movements of the lumbar spine, as previously mentioned.
Family history and spina bifida occulta (SBO) are possible risk factors for pars defects. Sixty-three percent of L5 spondylolysis exhibits terminal-stage defects despite young skeletal age, while most L3/L4 spondylolysis exhibits early-stage defects.4 This suggests that certain risk factors (possibly genetic) predispose to L5 spondylolysis, but not to spondylolysis at other lumbar levels. Another possibility could be the fact that L5 experiences more stress than other lumbar levels. Of the patients studied by Sakai et al,4 93% of L5 spondylolysis patients suffered from SBO, while 0% of the L3/L4 spondylolysis patients suffered from SBO. This indicates a strong correlation between L5 spondylolysis and SBO, either due to a common genetic predisposition, with autosomal dominant inheritance84,85 or because SBO directly predisposes to spondylolysis. This is supported by Yamada et al,5 who studied 3 brothers—2 of whom were twins—who all developed lumbar spondylolysis and concomitant SBO. It is postulated that defective osteogenesis during the growth period leads to both SBO and spondylolysis.4
Athletes have been shown to have larger sacrohorizontal angles (angle between the lumbar vertebra and upper end-plate of the sacrum) than nonathletes,32 leading to increased lumbar lordosis. Increased lumbar lordosis increases the risk of pars interarticularis defects due to greater shear and compressive forces on the lumbar spine.86,87 Lumbar lordosis may also be increased during adolescence, when rapid bone growth causes tightness of the iliopsoas and thoracolumbar fascia.19,88 Additionally, specific sporting positions may be associated with a higher body mass index, such as defensive players in rugby, and higher body mass index is associated with increased lumbar lordosis.89,90
Investigations
Imaging modalities are the mainstay of diagnosis in pars defects since clinical assessment is unreliable,8 but there is no universally agreed algorithm for the diagnostic workup.91 A trial of conservative management may be attempted before undertaking any imaging investigations, if the lower back pain is of recent onset and there is insufficient clinical suspicion for spondylolysis.92 Oblique and lateral X-rays of the lumbar spine may be performed as an initial investigation, with lucency of the pars interarticularis indicating a pars defect. The pathognomonic sign on oblique lumbar X-ray is the “Scotty dog collar” sign (the “Scotty dog” is the appearance of the normal spine, and the “collar” indicates the nondisplaced pars fracture).93 Computed tomography (CT), MRI, and single photon emission computed tomography (SPECT) are all more sensitive than X-ray8 and allow greater appreciation of the spinal anatomy, but their exact role in the diagnostic workup remains debated. Generally, early-stage disease is best detected by SPECT, but MRI has an increasingly positive role in this area.93 CT is excellent for assessing more progressive disease, determining fracture size and extent, and providing a baseline on which to assess adequacy of healing.93 In all cases, a high index of suspicion is required to detect less common types of pars defects, such as unilateral spondylolysis, spondylolysis of the upper lumbar vertebra (L1-L3), multilevel spondylolysis, and early stage lesions in which cortical disruption has not yet occurred.94,95
Management
There is no gold standard protocol for the management of pars interarticularis defects. Further studies are required to compare conservative therapy to surgical therapy, and to compare Buck’s repair with Scott’s wiring technique, Morscher technique and other novel surgical techniques involved in these defects. The literature summatively suggests a mean return-to-play time of 3.7 months for conservative therapy, and 7.9 months for operative therapy.96
Only 5 studies in this review reported the management instituted for their participants,25,42,43,52,65 and these were all case series (Table 5). Of 74 players with spondylolysis in these studies, 70 (94.59%) underwent conservative treatment and 4 (5.41%) underwent surgical treatment. Sixty-one (82.43%) returned to their previous level of play, 6 (8.11%) retired,25,42 and the disposition of the final 7 was not reported.42
Table 5.
Studies in Which Treatment Modality and Return-to-Play Time Were Reported.a
| No. of Athletes With Pars Defects | Conservative Therapy | Surgical Therapy | Returned to Previous Level of Play | Retired | |
|---|---|---|---|---|---|
| Donaldson et al25 | 11 | 11 | 0 | 10 | 1 |
| Hardcastle et al42 | 12 | 9 | 3 | Not reported | 5 |
| Engstrom et al43 | 18 | 18 | 0 | 18 | 0 |
| McCarroll et al52 | 22 | 21 | 1b | 22 | 0 |
| Jackson et al65 | 11 | 11 | 0 | 11 | 0 |
| Total | 74 | 70 | 4 | 61 | 6 |
a Five studies reported treatment modality for participants found to have spondylolytic defects.
b Intervertebral disc surgery, not pars interarticularis surgery.
Conservative Therapy
Management of pars interarticularis defects typically begins with rest, orthosis, and physical therapy97; transcutaneous electrical stimulation has also been described.98,99 The orthosis prevents hyperextension and twisting of the spine, while physical therapy strengthens and stretches the muscles of the trunk and lower limbs.100 Specific physical therapies include foam rolling, isometric strengthening exercises and exercises aimed at stretching the iliopsoas, piriformis, rectus femoris, and spinal erector muscles.86 Conservative management is effective for unilateral and bilateral lesions, allowing 90% of patients to return to baseline activity levels within 6 months.101 Unilateral lesions are the most likely to heal with conservative treatment, followed by bilateral lesions then pseudobilateral lesions (asymmetrical tracer uptake), but this is a radiological distinction since nonunion appears to have no effect on the overall outcome and ability to resume sport.101 At 11-year follow-up, only 22% of athletes are limited by pars defects treated conservatively,102 with limitation defined as any alteration to recreational activity.
Orthoses (Braces)
There are 2 types of orthoses: (a) thoracolumbosacral orthoses and (b) lumbosacral orthoses. For each of these, they may be flexible orthoses which simply decrease the activity of the adjacent paraspinal and abdominal muscle, or they may be rigid orthoses which restrict movement primarily in the sagittal plane, thus preventing hyperextension of the spine. Rigid thoracolumbosacral orthoses are thus more commonly used20,96,103 since they theoretically allow greater spinal rest and bony healing, but data suggests equally effective results and similar return-to-play time with lumbosacral orthoses.96
Surgical Therapy
Surgical intervention is indicated if there is failure of conservative treatment after 6 months, persistent back pain after 9 to 12 months, or pars pseudoarthrosis (nonunion after 9-12 months).97 104,105 Spondylolisthesis more than 50% in those who have not reached skeletal maturity, neurological deficit and radiculopathy are relative indications for surgical management.104 There are several methods of surgical management. A Buck’s repair involves screw fixation of the pars interarticularis.106 Variations include the Scott wiring technique107 and the Morscher technique108 (Table 6). Minimally invasive techniques have also recently been described, with quicker postoperative recovery but greater technical difficulty.97,109-112 Currently, there are no randomized controlled trials comparing different techniques of pars repair.
Table 6.
Buck’s Repair, Scott’s Wiring Technique, and Morscher Technique Are Used for Surgical Fixation of Pars Defects.
| Buck’s repair | Screw fixation of the pars interarticularis to compress the defect |
| Scott’s wiring technique | A wire is passed through the transverse processes of the vertebrae, then wrapped around the spinous processes. This stabilizes the defect and allows bony repair |
| Morscher technique | Bone graft fills the defect then screws are inserted into the superior articular processes. A hook hangs over the lamina and is secured by a lock |
Comparison of surgical outcomes is difficult as surgeons use various intraoperative and postoperative regimens in treating pars defects. Most surgeons immobilize patients for 3 months postoperatively in a rigid lumbosacral orthosis, then allow graduated return to activity.104, 113 Most surgeons allow resumption of sport after 6 months postoperatively in noncontact sports, and 12 months postoperatively in contact sports, although some surgeons advise patients to never recommence contact sports.104, 113 Approximately 50% of surgeons advise patients never to recommence collision.113 In all cases, patients must be fully rehabilitated before returning to athletic activity. This involves no pain with sport-specific activity, as well as full strength and range of motion. Naturally, some athletic activities can never be recommenced using these criteria since they require extreme ranges of motion that cannot be recommenced after surgery, such as dancers who require lumbar hyperextension for their vocation.112, 113 The main factors ultimately influencing return to athletic activity are symptomaticity and time from surgery; it is unclear whether radiographic appearance is one of the least important104,112,113 or most important factors112,114 influencing return to athletic activity.
Prevention
Prevention of pars defects by targeting modifiable risk factors may be an important adjunct against this disorder. For example, notifying cricketers of the increased risk using a mixed front-and-side action or tennis players of the increased risk using a topspin serve may lead to decreased incidence of pars defects. Coaches should also be trained in the provision of safe training routines, and high-risk maneuvers should be reserved for competitive play and not employed during training sessions.
Limitations
This study elucidated several areas of weakness in the current literature on pars interarticularis defects in athletes. Specifically, there were multiple differences in the study protocols of the 42 articles from which quantitative data was collected. The studies were always retrospective or prospective cohort studies; performing a randomized controlled trial for this clinical question would be unethical and practically impossible, since it would involve preventing certain individuals from performing physical activity for several years. Furthermore, there was considerable heterogeneity in the populations selected for testing with some studies only considering athletes of a particular sex, professional level or age. A number of studies only considered symptomatic patients whereas others studied all patients regardless of their symptomaticity. The imaging modalities used to detect pars interarticularis defects were also inconsistent, with some studies only using X-ray or CT imaging, which is inferior to MRI for detecting prelytic lesions. Finally, in athletes in whom more than one defect was detected the defect of highest grade was counted, such that the present study does not differentiate between patients with single and multiple defects. Future studies on this topic would benefit from prospectively using highly sensitive imaging (MRI) to detect all lesions in a symptomatic population of well-defined athletic experience so that better comparisons can be made between sports subtypes.
Conclusion
The current medical literature provides good evidence that the incidence of pars interarticularis defects is higher in the athletic population, with the highest incidence in diving, cricket, and baseball/softball. There remains no gold standard protocol for the management of pars interarticularis defects. Further studies are required to compare conservative therapy (rest, orthosis, physical therapy) to surgical therapy, and to compare Buck’s repair with Scott’s wiring technique, Morscher technique, and other novel surgical techniques involved in these defects.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Hollenberg GM, Beattie PF, Meyers SP, Weinberg EP, Adams MJ. Stress reactions of the lumbar pars interarticularis: the development of a new MRI classification system. Spine (Phila Pa 1976). 2002;27:181–186. doi:10.1097/00007632-200201150-00012 [DOI] [PubMed] [Google Scholar]
- 2. Wiltse LL, Newman PH, Macnab I. Classification of spondylolisis and spondylolisthesis. Clin Orthop Relat Res. 1976;(117):23–29. doi:10.1097/00003086-197606000-00003 [PubMed] [Google Scholar]
- 3. Narita T, Kaneoka K. The prevention of low back sisorders in divers In: Kanosue K, Ogawa T, Fukano M, Fukubayashi T, eds. Sports Injuries and Prevention. Tokyo, Japan: Springer; 2015:383–393 [Google Scholar]
- 4. Sakai T, Goda Y, Tezuka F, et al. Characteristics of lumbar spondylolysis in elementary school age children. Eur Spine J. 2016;25:602–606. doi:10.1007/s00586-015-4029-4 [DOI] [PubMed] [Google Scholar]
- 5. Yamada A, Sairyo K, Shibuya I, Kato K, Dezawa A, Sakai T. Lumbar spondylolysis in juveniles from the same family: a report of three cases and a review of the literature. Case Rep Orthop. 2013;2013:272514 doi:10.1155/2013/272514 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Vernese LF, Chu SK. Spondylolysis: assessment and treatment in youth athletes. Curr Phys Med Rehabil Rep. 2017;5:75–82. doi:10.1007/s40141-017-0151-z [Google Scholar]
- 7. Sundell CG, Jonsson H, Adin L, Larsén KH. Clinical examination, spondylolysis and adolescent athletes. Int J Sports Med. 2013;34:263–267. doi:10.1055/s-0032-1321723 [DOI] [PubMed] [Google Scholar]
- 8. Masci L, Pike J, Malara F, Phillips B, Bennell K, Brukner P. Use of the one-legged hyperextension test and magnetic resonance imaging in the diagnosis of active spondylolysis. Br J Sports Med. 2006;40:940–946. doi:10.1136/bjsm.2006.030023 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Oren JH, Gallina JM. Pars injuries in athletes. Bull Hosp Jt Dis (2013). 2016;74:73–81 [PubMed] [Google Scholar]
- 10. Samartzis D, Arnold PM. Spine in the Arts. The boxing boys of Akrotiri: early illustration of spondylolytic spondylolisthesis related to a sports injury. Spine J. 2007;7:254–255. doi:10.1016/j.spinee.2006.06.392 [DOI] [PubMed] [Google Scholar]
- 11. Toueg CW, Mac-Thiong JM, Grimard G, Poitras B, Parent S, Labelle H. Spondylolisthesis, sacro-pelvic morphology, and orientation in young gymnasts. J Spinal Disord Tech. 2015;28:E358–E364. doi:10.1097/BSD.0b013e3182956d62 [DOI] [PubMed] [Google Scholar]
- 12. Kulling FA, Florianz H, Reepschlager B, Gasser J, Jost B, Lajtai G. High prevalence of disc degeneration and spondylolysis in the lumbar spine of professional beach volleyball players. Orthop J Sports Med. 2014;2:2325967114528862 doi:10.1177/2325967114528862 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Nakayama T, Ehara S. Spondylolytic spondylolisthesis: various imaging features and natural courses. Jpn J Radiol. 2014;33:3–12. doi:10.1007/s11604-014-0371-4 [DOI] [PubMed] [Google Scholar]
- 14. Sairyo K, Katoh S, Sasa T, et al. Athletes with unilateral spondylolysis are at risk of stress fracture at the contralateral pedicle and pars interarticularis: a clinical and biomechanical study. Am J Sports Med. 2005;33:583–590. doi:10.1177/0363546504269035 [DOI] [PubMed] [Google Scholar]
- 15. Beutler WJ, Fredrickson BE, Murtland A, Sweeney CA, Grant WD, Baker D. The natural history of spondylolysis and spondylolisthesis: 45-year follow-up evaluation. Spine (Phila Pa 1976). 2003;28:1027–1035. doi:10.1097/01.BRS.0000061992.98108.A0 [DOI] [PubMed] [Google Scholar]
- 16. Standaert CJ, Herring SA. Spondylolysis: a critical review. Br J Sports Med. 2000;34:415–422. doi:10.1136/bjsm.34.6.415 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Fredrickson BE, Baker D, McHolick WJ, Yuan HA, Lubicky JP. The natural history of spondylolysis and spondylolisthesis. J Bone Joint Surg Am. 1984;66:699–707. [PubMed] [Google Scholar]
- 18. Congeni J, McCulloch J, Swanson K. Lumbar spondylolysis. A study of natural progression in athletes. Am J Sports Med. 1997;25:248–253. doi:10.1177/036354659702500220 [DOI] [PubMed] [Google Scholar]
- 19. McCleary MD, Congeni JA. Current concepts in the diagnosis and treatment of spondylolysis in young athletes. Curr Sports Med Rep. 2007;6:62–66. doi:10.1097/01.CSMR.0000306559.19088.6f [DOI] [PubMed] [Google Scholar]
- 20. Iwamoto J, Takeda T, Wakano K. Returning athletes with severe low back pain and spondylolysis to original sporting activities with conservative treatment. Scand J Med Sci Sports. 2004;14:346–351. doi:10.1111/j.1600-0838.2004.00379.x [DOI] [PubMed] [Google Scholar]
- 21. Morita T, Ikata T, Katoh S, Miyake R. Lumbar spondylolysis in children and adolescents. J Bone Joint Surg Br. 1995;77:620–625. doi:10.1302/0301-620x.77b4.7615609 [PubMed] [Google Scholar]
- 22. Micheli LJ, Wood R. Back pain in young athletes. Significant differences from adults in causes and patterns. Arch Pediatr Adolesc Med. 1995;149:15–18. doi:10.1001/archpedi.1995.02170130017004 [DOI] [PubMed] [Google Scholar]
- 23. Moher D, Liberati A, Tetzlaff J, Altman DG; PRISMA Group. Preferred Reporting Items for Systematic Reviews and Meta-Analyses: the PRISMA Statement. PLoS Med. 2009;6:e1000097 doi:10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Roche MB, Rowe GG. The incidence of separate neural arch and coincident bone variations; a survey of 4200 skeletons. Anat Rec. 1951;109:233–252. doi:10.1002/ar.1091090207 [DOI] [PubMed] [Google Scholar]
- 25. Donaldson LD. Spondylolysis in elite junior-level ice hockey players. Sports Health. 2014;6:356–359. doi:10.1177/1941738113519958 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Rossi F, Dragoni S. The prevalence of spondylolysis and spondylolisthesis in symptomatic elite athletes: radiographic findings. Radiography. 2001;7:37–42. doi:10.1053/radi.2000.0299 [Google Scholar]
- 27. Soler T, Calderon C. The prevalence of spondylolysis in the Spanish elite athlete. Am J Sports Med. 2000;28:57–62. doi:10.1177/03635465000280012101 [DOI] [PubMed] [Google Scholar]
- 28. Suzuki K. Medical check of lumbar spine in adolescent ice hockey players [in Japanese]. Rinshou Sports Igaku (Clinical Sports Medicine). 2002;19:1425–1430. [Google Scholar]
- 29. Sakai T, Sairyo K, Suzue N, Kosaka H, Yasui N. Incidence and etiology of lumbar spondylolysis: review of the literature. J Orthop Sci. 2010;15:281–288. doi:10.1007/s00776-010-1454-4 [DOI] [PubMed] [Google Scholar]
- 30. Abrams GD, Renstrom PA, Safran MR. Epidemiology of musculoskeletal injury in the tennis player. Br J Sports Med. 2012;46:492–498. doi:10.1136/bjsports-2012-091164 [DOI] [PubMed] [Google Scholar]
- 31. Kobayashi A, Kobayashi T, Kato K, Higuchi H, Takagishi K. Diagnosis of radiographically occult lumbar spondylolysis in young athletes by magnetic resonance imaging. Am J Sports Med. 2013;41:169–176. doi:10.1177/0363546512464946 [DOI] [PubMed] [Google Scholar]
- 32. Sward L, Hellstrom M, Jacobsson B, Peterson L. Spondylolysis and the sacro-horizontal angle in athletes. Acta Radiol. 1989;30:359–364. doi:10.3109/02841858909174697 [PubMed] [Google Scholar]
- 33. Maquirriain J, Ghisi JP. The incidence and distribution of stress fractures in elite tennis players. Br J Sports Med. 2006;40:454–459. doi:10.1136/bjsm.2005.023465 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Ranson CA, Burnett AF, Kerslake RW. Injuries to the lower back in elite fast bowlers: acute stress changes on MRI predict stress fracture. J Bone Joint Surg Br. 2010;92:1664–1668. doi:10.1302/0301-620X.92B12.24913 [DOI] [PubMed] [Google Scholar]
- 35. Rajeswaran G, Turner M, Gissane C, Healy JC. MRI findings in the lumbar spines of asymptomatic elite junior tennis players. Skeletal Radiol. 2014;43:925–932. doi: 10.1007/s00256-014-1862-1 [DOI] [PubMed] [Google Scholar]
- 36. Kono S. A study on the etiology of spondylolysis with reference to athletic activities. J Jpn Orthop Assoc. 1975;49:125–133. [Google Scholar]
- 37. Akimoto T. The etiology of spondylolysis with reference to athletic activities during growing period. Seikeigeka (Orthopaedics). 1979;30:638–646. [Google Scholar]
- 38. Mcanany S, Patterson D, Hecht AC. Spine injuries in tennis players In: Colvin AC, Gladstone JN, eds. The Young Tennis Player. Basel, Switzerland: Springer; 2016:121–134. [Google Scholar]
- 39. Sheets AL, Abrams GD, Corazza S, Safran MR, Andriacchi TP. Kinematics differences between the flat, kick, and slice serves measured using a markerless motion capture method. Ann Biomed Eng. 2011;39:3011–3020. doi:10.1007/s10439-011-0418-y [DOI] [PubMed] [Google Scholar]
- 40. Chow JW, Park SA, Tillman MD. Lower trunk kinematics and muscle activity during different types of tennis serves. Sports Med Arthrosc Rehabil Ther Technol. 2009;1:24 doi:10.1186/1758-2555-1-24 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Crewe H, Elliott B, Couanis G, Campbell A, Alderson J. The lumbar spine of the young cricket fast bowler: an MRI study. J Sci Med Sport. 2012;15:190–194. doi:10.1016/j.jsams.2011.11.251 [DOI] [PubMed] [Google Scholar]
- 42. Hardcastle P, Annear P, Foster DH, et al. Spinal abnormalities in young fast bowlers. J Bone Joint Surg Br. 1992;74:421–425. doi:10.1302/0301-620X.74B3.1587894 [DOI] [PubMed] [Google Scholar]
- 43. Engstrom CM, Walker DG. Pars interarticularis stress lesions in the lumbar spine of cricket fast bowlers. Med Sci Sports Exerc. 2007;39:28–33. doi:10.1249/01.mss.0000241642.82725.ac [DOI] [PubMed] [Google Scholar]
- 44. Foster D, John D, Elliott B, Ackland T, Fitch K. Back injuries to fast bowlers in cricket: a prospective study. Br J Sports Med. 1989;23:150–154. doi:10.1136/bjsm.23.3.150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Annear PT, Chakera TM, Foster DH, Hardcastle PH. Pars interarticularis stress and disc degeneration in cricket’s potent strike force: the fast bowler. Aust N Z J Surg. 1992;62:768–773. doi:10.1111/j.1445-2197.1992.tb06915.x [DOI] [PubMed] [Google Scholar]
- 46. Elliott BC, Hardcastle PH, Burnett AE, Foster DH. The influence of fast bowling and physical factors on radiologic features in high performance young fast bowlers. Sports Med Train Rehabil. 1992;3:113–130. doi:10.1080/15438629209517008 [Google Scholar]
- 47. Gregory PL, Batt ME, Kerslake RW. Comparing spondylolysis in cricketers and soccer players. Br J Sports Med. 2004;38:737–742. doi:10.1136/bjsm.2003.008110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Ranawat VS, Dowell JK, Heywood-Waddington MB. Stress fractures of the lumbar pars interarticularis in athletes: a review based on long-term results of 18 professional cricketers. Injury. 2003;34:915–919. doi:10.1016/S0020-1383(03)00034-2 [DOI] [PubMed] [Google Scholar]
- 49. Elliott BC. Back injuries and the fast bowler in cricket. J Sports Sci. 2000;18:983–991. doi:10.1080/026404100446784 [DOI] [PubMed] [Google Scholar]
- 50. Burnett A, Elliott B, Foster D, et al. The back breaks before the wicket: the young fast bowler’s spine. Sport Health. 1991;9:11–15. [Google Scholar]
- 51. Jones DM, Tearse DS, El-Khoury GY, Kathol MH, Brandser EA. Radiographic abnormalities of the lumbar spine in college football players: a comparative analysis. Am J Sports Med. 1999;27:335–338. doi:10.1177/03635465990270031101 [DOI] [PubMed] [Google Scholar]
- 52. McCarroll JR, Miller JM, Ritter MA. Lumbar spondylolysis and spondylolisthesis in college football players. A prospective study. Am J Sports Med. 1986;14:404–406. doi:10.1177/036354658601400513 [DOI] [PubMed] [Google Scholar]
- 53. Semon RL, Spengler D. Significance of lumbar spondylolysis in college football players. Spine (Phila Pa 1976). 1981;6:172–174. doi:10.1097/00007632-198103000-00012 [DOI] [PubMed] [Google Scholar]
- 54. Iwamoto J, Abe H, Tsukimura Y, Wakano K. Relationship between radiographic abnormalities of lumbar spine and incidence of low back pain in high school rugby players: a prospective study. Scand J Med Sci Sports. 2005;15:163–168. doi:10.1111/j.1600-0838.2004.00414.x [DOI] [PubMed] [Google Scholar]
- 55. Ferguson RJ, McMaster JH, Stanitski CL. Low back pain in college football linemen. J Sports Med. 1974;2:63–69. doi:10.1177/036354657400200201 [DOI] [PubMed] [Google Scholar]
- 56. Abe H. Spondylolysis in rugby and American football players. Jpn J Orthop Sports Med. 1990;9:109–114. [Google Scholar]
- 57. Castinel BH, Adam P, Prat C. A stress fracture of the lumbar spine in a professional rugby player. Br J Sports Med. 2007;41:337–338. doi:10.1136/bjsm.2006.032789 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58. Light DI, Kerr HA. Spine injuries in collision/heavy contact sports In: Micheli L, Stein C, O’Brien M, d’Hemecourt P, eds. Spinal Injuries and Conditions in Young Athletes. New York, NY: Springer; 2014:75–87. [Google Scholar]
- 59. Hasegawa A. Medical check of lumbar spine in baseball players in the national high school baseball championship [in Japanese]. Rinshou Sports Igaku (Clinical Sports Medicine). 2002;19:1431–1436. [Google Scholar]
- 60. Matsumoto M. Conservative treatment of lumbar disorders [in Japanese]. Rinshou Sports Igaku (Clinical Sports Medicine). 2006;23:1301–1309. [Google Scholar]
- 61. Wakitani S, Ochi T, Hirooka J, Yoneda M, Ono K. The study about lumbar spondylolysis found in professional baseball players. Cent Jpn J Orthop Traumatol. 1988;31:538–540. [Google Scholar]
- 62. Mohriak R, Silva PDV, Trandafilov M, Jr, et al. Spondylolysis and spondylolisthesis in young gymnasts. Rev Bras Ortop. 2010;45:79–83. doi:10.1016/S2255-4971(15)30221-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63. Toueg CW, Mac-Thiong JM, Grimard G, Parent S, Poitras B, Labelle H. Prevalence of spondylolisthesis in a population of gymnasts. Stud Health Technol Inform. 2010;158:132–137. doi:10.3233/978-1-60750-573-0-132 [PubMed] [Google Scholar]
- 64. Bennett DL, Nassar L, DeLano MC. Lumbar spine MRI in the elite-level female gymnast with low back pain. Skeletal Radiol. 2006;35:503–509. doi:10.1007/s00256-006-0083-7 [DOI] [PubMed] [Google Scholar]
- 65. Jackson DW, Wiltse LL, Cirincoine RJ. Spondylolysis in the female gymnast. Clin Orthop Relat Res. 1976;(117):68–73. doi:10.1097/00003086-197606000-00008 [PubMed] [Google Scholar]
- 66. Schmitt H, Brocai DR, Carstens C. Long-term review of the lumbar spine in javelin throwers. J Bone Joint Surg Br. 2001;83:324–327. doi:10.1302/0301-620X.83B3.11386 [DOI] [PubMed] [Google Scholar]
- 67. Kuroki T. Lumbar disorders of judo players. Jpn J Orthop Sports Med. 1994;14:387–390. [Google Scholar]
- 68. Rebella G. A prospective study of injury patterns in collegiate pole vaulters. Am J Sports Med. 2015;43:808–815. doi:10.1177/0363546514564542 [DOI] [PubMed] [Google Scholar]
- 69. Maurer M, Soder RB, Baldisserotto M. Spine abnormalities depicted by magnetic resonance imaging in adolescent rowers. Am J Sports Med. 2011;39:392–397. doi:10.1177/0363546510381365 [DOI] [PubMed] [Google Scholar]
- 70. Murase M. Clinical and radiological surveys of lumbar spondylolysis in young soccer players [in Japanese]. Nihon Seikeigeka Gakkai Zasshi. 1989;63:1297–1305. [PubMed] [Google Scholar]
- 71. Kyo M. Medical check of professional soccer team. Seikeigeka (Orthopaedics). 1995;46:243–247 [Google Scholar]
- 72. Nakagawa Y. Medical check of lumbar spine in college student sumo players [in Japanese]. Rinshou Sports Igaku (Clinical Sports Medicine). 2002;19:1445–1449. [Google Scholar]
- 73. Alyas F, Turner M, Connell D. MRI findings in the lumbar spines of asymptomatic, adolescent, elite tennis players. Br J Sports Med. 2007;41:836–841. doi:10.1136/bjsm.2007.037747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Kotani PT, Ichikawa N, Wakabayashi W, Yoshii BS, Koshimune M. Studies of spondylolysis found among weightlifters. Br J Sports Med. 1971;6:4–8. doi:10.1136/bjsm.6.1.4 [Google Scholar]
- 75. Granhed H, Morelli B. Low back pain among retired wrestlers and heavyweight lifters. Am J Sports Med. 1988;16:530–533. doi:10.1177/036354658801600517 [DOI] [PubMed] [Google Scholar]
- 76. Arendt EA, Griffiths HJ. The use of MR imaging in the assessment and clinical management of stress reactions of bone in high-performance athletes. Clin Sports Med. 1997;16:291–306. doi:10.1016/S0278-5919(05)70023-5 [DOI] [PubMed] [Google Scholar]
- 77. Logroscino G, Mazza O, Aulisa G, Pitta L, Pola E, Aulisa L. Spondylolysis and spondylolisthesis in the pediatric and adolescent population. Childs Nerv Syst. 2001;17:644–655. doi:10.1007/s003810100495 [DOI] [PubMed] [Google Scholar]
- 78. Marchetti PC, Bartolozzi P. Classification of spondylolisthesis as a guideline for treatment In: Bridwell KH, DeWald RL, Hammerberg KW, et al. eds. The Textbook of Spinal Surgery. Philadelphia, PA: Lippincott-Raven; 1997:1211–1254. [Google Scholar]
- 79. Jaimes C, Jimenez M, Shabshin N, Laor T, Jaramillo D. Taking the stress out of evaluating stress injuries in children. Radiographics. 2012;32:537–555. doi:10.1148/rg.322115022 [DOI] [PubMed] [Google Scholar]
- 80. Sakai T, Sairyo K, Takao S, Nishitani H, Yasui N. Incidence of lumbar spondylolysis in the general population in Japan based on multidetector computed tomography scans from two thousand subjects. Spine (Phila Pa 1976). 2009;34:2346–2350. doi:10.1097/BRS.0b013e3181b4abbe [DOI] [PubMed] [Google Scholar]
- 81. Simper LB. Spondylolysis in Eskimo skeletons. Acta Orthop Scand. 1986;57:78–80. doi:10.3109/17453678608993222 [DOI] [PubMed] [Google Scholar]
- 82. Huguenin L. Paediatric sports injuries. Aust Fam Physician. 2016;45:466–469. [PubMed] [Google Scholar]
- 83. Tallarico RA, Madom IA, Palumbo MA. Spondylolysis and spondylolisthesis in the athlete. Sports Med Arthrosc Rev. 2008;16:32–38. doi:10.1097/JSA.0b013e318163be50 [DOI] [PubMed] [Google Scholar]
- 84. Shahriaree H, Sajadi K, Rooholamini SA. A family with spondylolisthesis. J Bone Joint Surg Am. 1979;61:1256–1258. doi:10.1148/94.3.631 [PubMed] [Google Scholar]
- 85. Haukipuro K, Keranen N, Koivisto E, Lindholm R, Norio R, Punto L. Familial occurrence of lumbar spondylolysis and spondylolisthesis. Clin Genet. 1978;13:471–476. doi:10.1111/j.1399-0004.1978.tb01200.x [DOI] [PubMed] [Google Scholar]
- 86. Shurley JP, Newman JK. Spondylolysis in American football players: etiology, symptoms, and implications for strength and conditioning specialists. Strength Cond J. 2016;38:40–51. doi:10.1519/SSC.0000000000000244 [Google Scholar]
- 87. Alexander MJ. Biomechanical aspects of lumbar spine injuries in athletes: a review. Can J Appl Sport Sci. 1985;10:1–20. [PubMed] [Google Scholar]
- 88. d’Hemecourt PA, Gerbino PG, 2nd, Micheli LJ. Back injuries in the young athlete. Clin Sports Med. 2000;19:663–679. doi:10.1016/S0278-5919(05)70231-3 [DOI] [PubMed] [Google Scholar]
- 89. Guo JM, Zhang GQ, Alimujiang. Effect of BMI and WHR on lumbar lordosis and sacrum slant angle in middle and elderly women [in Chinese]. Zhongguo Gu Shang. 2008;21:30–31. [PubMed] [Google Scholar]
- 90. Bundy J, Hernandez T, Zhou H, Chutkan N. The effect of body mass index on lumbar lordosis on the Mizuho OSI Jackson spinal table. Evid Based Spine Care J. 2010;1:35–40. doi:10.1055/s-0028-1100891 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91. Duerson DH, Rodenberg RE, MacDonald J. Spondylolysis in the young athlete. Athletic Training Sports Health Care. 2016;8:5–7. doi:10.3928/19425864-20151119-05 [Google Scholar]
- 92. Ralston S, Weir M. Suspecting lumbar spondylolysis in adolescent low back pain. Clin Pediatr (Phila). 1998;37:287–293. doi:10.1177/000992289803700502 [DOI] [PubMed] [Google Scholar]
- 93. Syrmou E, Tsitsopoulos PP, Marinopoulos D, Tsonidis C, Anagnostopoulos I, Tsitsopoulos PD. Spondylolysis: a review and reappraisal. Hippokratia. 2010;14:17–21. [PMC free article] [PubMed] [Google Scholar]
- 94. Viana SL, Viana MA, de Alencar EL. Atypical, unusual, and misleading imaging presentations of spondylolysis. Skeletal Radiol. 2015;44:1253–1262. doi:10.1007/s00256-015-2138-0 [DOI] [PubMed] [Google Scholar]
- 95. Cardozo E, Chang RG, Sneag DB, Wyss J. Atypical location of low-back pain in a high school basketball player. Am J Phys Med Rehabil. 2015;94:e94–e95. doi:10.1097/PHM.0000000000000331 [DOI] [PubMed] [Google Scholar]
- 96. Panteliadis P, Nagra NS, Edwards KL, Behrbalk E, Boszczyk B. Athletic population with spondylolysis: review of outcomes following surgical repair or conservative management. Global Spine J. 2016;6:615–625. doi:10.1055/s-0036-1586743 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97. Gillis CC, Eichholz K, Thoman WJ, Fessler RG. A minimally invasive approach to defects of the pars interarticularis: restoring function in competitive athletes. Clin Neurol Neurosurg. 2015;139:29–34. doi:10.1016/j.clineuro.2015.08.024 [DOI] [PubMed] [Google Scholar]
- 98. Fellander-Tsai L, Micheli LJ. Treatment of spondylolysis with external electrical stimulation and bracing in adolescent athletes: a report of two cases. Clin J Sport Med. 1998;8:232–234. [DOI] [PubMed] [Google Scholar]
- 99. Stasinopoulos D. Treatment of spondylolysis with external electrical stimulation in young athletes: a critical literature review. Br J Sports Med. 2004;38:352–354. doi:10.1136/bjsm.2003.010405 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100. Kaneoka K. Low back disorders among athletes and its prevention In: Kanosue K, Ogawa T, Fukano M, Fukubayashi T, eds. Sports Injuries and Prevention. Tokyo, Japan: Springer; 2015:367–374 [Google Scholar]
- 101. Sys J, Michielsen J, Bracke P, Martens M, Verstreken J. Nonoperative treatment of active spondylolysis in elite athletes with normal X-ray findings: literature review and results of conservative treatment. Eur Spine J. 2001;10:498–504. doi:10.1007/s005860100326 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 102. Miller SF, Congeni J, Swanson K. Long-term functional and anatomical follow-up of early detected spondylolysis in young athletes. Am J Sports Med. 2004;32:928–933. doi:10.1177/0363546503262194 [DOI] [PubMed] [Google Scholar]
- 103. Blanda J, Bethem D, Moats W, Lew M. Defects of pars interarticularis in athletes: a protocol for nonoperative treatment. J Spinal Disord. 1993;6:406–411. doi:10.1097/00002517-199306050-00007 [DOI] [PubMed] [Google Scholar]
- 104. Radcliff KE, Kalantar SB, Reitman CA. Surgical management of spondylolysis and spondylolisthesis in athletes: indications and return to play. Curr Sports Med Rep. 2009;8:35–40. doi:10.1249/JSR.0b013e318194f89e [DOI] [PubMed] [Google Scholar]
- 105. Hardcastle PH. Repair of spondylolysis in young fast bowlers. J Bone Joint Surg Br. 1993;75:398–402. doi:10.1302/0301-620X.75B3.8496207 [DOI] [PubMed] [Google Scholar]
- 106. Buck JE. Direct repair of the defect in spondylolisthesis. Preliminary report. J Bone Joint Surg Br. 1970;52:432–437. [PubMed] [Google Scholar]
- 107. Nicol RO, Scott JH. Lytic spondylolysis. Repair by wiring. Spine (Phila Pa 1976). 1986;11:1027–1030. [DOI] [PubMed] [Google Scholar]
- 108. Morscher E, Gerber B, Fasel J. Surgical treatment of spondylolisthesis by bone grafting and direct stabilization of spondylolysis by means of a hook screw. Arch Orthop Trauma Surg. 1984;103:175–178. doi:10.1007/BF00435550 [DOI] [PubMed] [Google Scholar]
- 109. Sairyo K, Sakai T, Yasui N. Minimally invasive technique for direct repair of pars interarticularis defects in adults using a percutaneous pedicle screw and hook-rod system: technical note. J Neurosurg. 2009;10:492–495. doi:10.3171/2009.2.SPINE08594 [DOI] [PubMed] [Google Scholar]
- 110. Noggle JC, Sciubba DM, Samdani AF, Anderson DG, Betz RR, Asghar J. Minimally invasive direct repair of lumbar spondylolysis with a pedicle screw and hook construct. Neurosurg Focus. 2008;25:E15 doi:10.3171/FOC/2008/25/8/E15 [DOI] [PubMed] [Google Scholar]
- 111. Brennan RP, Smucker PY, Horn EM. Minimally invasive image-guided direct repair of bilateral L-5 pars interarticularis defects. Neurosurg Focus. 2008;25:E13 doi:10.3171/FOC/2008/25/8/E13 [DOI] [PubMed] [Google Scholar]
- 112. Bouras T, Korovessis P. Management of spondylolysis and low-grade spondylolisthesis in fine athletes. A comprehensive review. Eur J Orthop Surg Traumatol. 2015;25(suppl 1):S167–S175. doi:10.1007/s00590-014-1560-7 [DOI] [PubMed] [Google Scholar]
- 113. Rubery PT, Bradford DS. Athletic activity after spine surgery in children and adolescents: results of a survey. Spine (Phila Pa 1976). 2002;27:423–427. [DOI] [PubMed] [Google Scholar]
- 114. Sutton JH, Guin PD, Theiss SM. Acute lumbar spondylolysis in intercollegiate athletes. J Spinal Disord Tech. 2012;25:422–425. doi:10.1097/BSD.0b013e318236ba6c [DOI] [PubMed] [Google Scholar]