Summary
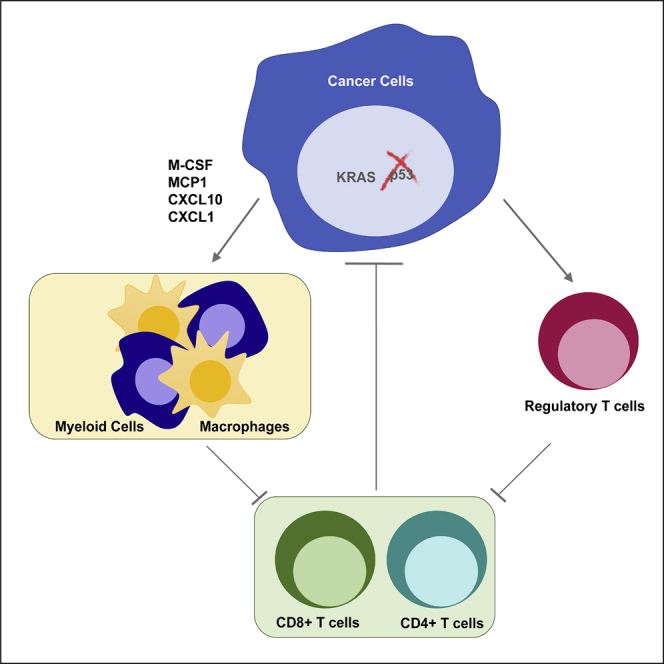
Loss of p53 function contributes to the development of many cancers. While cell-autonomous consequences of p53 mutation have been studied extensively, the role of p53 in regulating the anti-tumor immune response is still poorly understood. Here, we show that loss of p53 in cancer cells modulates the tumor-immune landscape to circumvent immune destruction. Deletion of p53 promotes the recruitment and instruction of suppressive myeloid CD11b+ cells, in part through increased expression of CXCR3/CCR2-associated chemokines and macrophage colony-stimulating factor (M-CSF), and attenuates the CD4+ T helper 1 (Th1) and CD8+ T cell responses in vivo. p53-null tumors also show an accumulation of suppressive regulatory T (Treg) cells. Finally, we show that two key drivers of tumorigenesis, activation of KRAS and deletion of p53, cooperate to promote immune tolerance.
Keywords: p53, Kras, tumor, myeloid cells, T cell response
Graphical Abstract
Highlights
-
•
Tumor-specific loss of p53 delays tumor rejection in immune-competent hosts
-
•
p53 loss increases myeloid infiltration through enhanced cytokine secretion
-
•
The increase in Treg cells in response to loss of p53 is independent of Kras mutation
-
•
Kras mutations coordinate with p53 loss to regulate myeloid recruitment
TP53 is one of the most frequently mutated genes in cancer; however, its significance in controlling tumor-immune crosstalk is not fully understood. Blagih et al. highlight a key role for tumor-associated loss of p53, a common oncogenic event, in regulating myeloid and T cell responses.
Introduction
There is strong evidence that cancer cells have the potential to be recognized by the immune system but that they can mobilize various mechanisms of immune evasion and escape, such as upregulation of immune checkpoint proteins to dampen T cell effector responses (Ribas and Wolchok, 2018). Current human studies have shown durable and complete responses to immune checkpoint blockades in a number of tumors; however, for reasons that are not completely clear, a sizable proportion of cancers fail to respond. It is apparent that the constellation of oncogenic events that leads to full neoplastic transformation can influence the effector function of the immune response in several ways. Oncogenic RAS can promote expression of various cytokines (Ancrile et al., 2008) that result in an inflammatory response, which is thought to promote cancer progression. RAS signaling also increases tumor cell expression of PD-L1 (Coelho et al., 2017), thereby suppressing activated T cells, and increases secretion of granulocyte-macrophage colony-stimulating factor (GM-CSF) to promote pancreatic neoplasia (Bayne et al., 2012, Pylayeva-Gupta et al., 2012). The co-activation of KRAS and MYC in lung tumors restructures macrophage and T cell responses in a CCL9 and interleukin-23 (IL-23)-dependent manner (Kortlever et al., 2017). Loss of PTEN, another common oncogenic event, results in resistance to PD-1 blockade in both melanoma and uterine leiomyosarcoma (George et al., 2017, Peng et al., 2016), while β-catenin signaling in melanoma was shown to limit T cell infiltration (Spranger et al., 2015).
p53 is best understood as a tumor suppressor (Hollstein et al., 1991). However, in the immune compartment, p53 also functions as a negative regulator of autoimmunity by supporting regulatory T (Treg) cells, through directly upregulating Foxp3 and promoting STAT5 activity, and restricting STAT3 in the pro-inflammatory helper T cells (T helper 17 [Th17] cells) (Kawashima et al., 2013, Okuda et al., 2003, Park et al., 2013, Watanabe et al., 2014, Zhang et al., 2011). Expression of p53 in macrophages leads to both an inflammatory response through co-operation with nuclear factor κB (NF-κB) and an anti-inflammatory response through STAT1 inhibition (Lowe et al., 2014, Yoon et al., 2015, Zheng et al., 2005). In the context of cancer, activation of p53 in the tumor stromal compartment has been shown to promote a tumor-restricting immune response. Induction of p53 in hepatic stellate cells (HSCs) results in senescence and the senescent-associated-secretory phenotype (SASP) that drives M1-macrophage polarization and limits cancer progression (Lujambio et al., 2013). Conversely, HSCs lacking p53 induce the differentiation of macrophages toward the tumor-promoting M2 state (Lujambio et al., 2013). Stromal loss of p53 changes the cytokine secretion pattern to promote myeloid-derived suppressor cells (MDSCs), thereby accelerating tumor growth (Guo et al., 2013). Interestingly, activation of p53 in the tumor microenvironment using local injection of the MDM2 inhibitor Nutlin selectively eradicated tumors that were rich in leukocytes. This response was dependent on stromal-p53 expression (Guo et al., 2017). These studies show that p53 levels in the stroma shape the inflammatory responses that influence tumor progression.
Despite the clear role of p53 in immune regulation, relatively few studies have examined how p53 status of the cancer cells affects the immune response in vivo. Reactivation of p53 in established liver cancers induced senescence and SASP, which promoted polymorphonuclear (PMN) infiltration and tumor regression (Xue et al., 2007). Futher studies showed that the induction of p53-dependent senescence in hepatocellular carcinomas was accompanied by the elimination of the tumor cells through a mechanism dependent on natural killer (NK) cells (Iannello et al., 2013). In silico correlations between the retention of wild-type (WT) p53 expression and immune infiltration in breast and head and neck cancers have also been noted (Siemers et al., 2017). However, a recent study of a PTEN-driven prostate cancer model indicated that concomitant loss of p53 enhanced tumor infiltration of CD11b+Gr1+ PMN cells. The recruitment of this myeloid population was through increased CXCL17 secretion by p53-null prostate cancer cells, and their role in promoting tumor development was associated with the expansion of immunosuppressive Treg cells (Bezzi et al., 2018). Similar findings were observed in mouse models of breast cancers, where loss of p53 increased frequencies of circulating and tumor neutrophils through unchecked WNT signaling, resulting in enhanced metastasis (Wellenstein et al., 2019).
In this study, we show that tumor-specific loss of p53 expression in both autochthonous lung and pancreatic tumor models correlates with changes in the tumor microenvironment. Using KRAS-driven pancreastumor-derived cancer cells as a model of p53 loss, we demonstrate that p53 deletion can promote immune tolerance through the recruitment of both myeloid cells and Treg cells. The enrichment of these suppressive populations results in enhanced protection of p53-null cancer cells from immune-mediated elimination. Furthermore, concomitant activation of KRAS and loss of p53 coordinate to promote immune tolerance.
Results
Loss of Trp53 Promotes Myeloid Recruitment in the Tumor Microenvironment
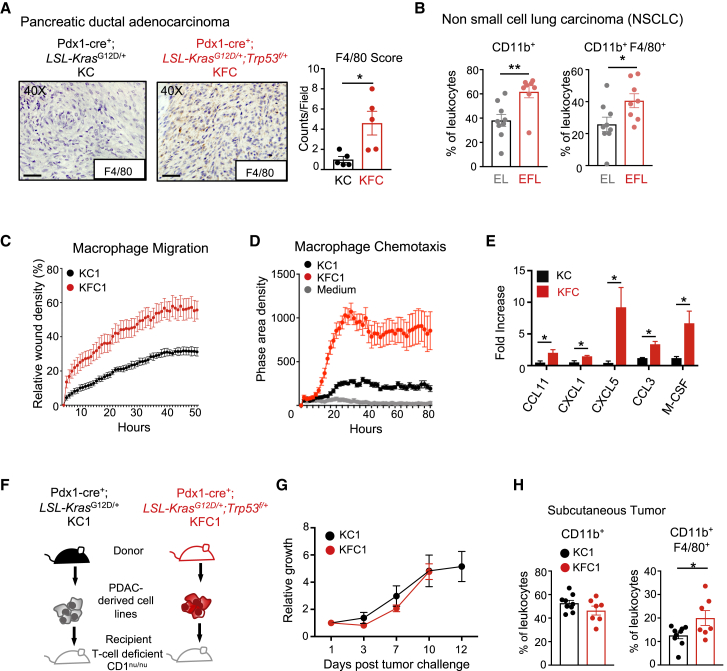
Tumor growth involves a complex interaction between stromal cells (of mesenchymal and immune origin) and cancer cells. Numerous studies have shown a role for macrophages in supporting cancer progression (Cassetta and Pollard, 2018, Noy and Pollard, 2014, Prenen and Mazzone, 2019, Qian and Pollard, 2010), and so we examined whether loss of p53 in autochthonous mouse models of pancreatic and lung cancers could influence myeloid cell recruitment to the tumor microenvironment (TME). Immunohistochemistry (IHC) sections were analyzed for F4/80+ immune cells in pancreatic tumors derived at equivalent endpoints from a pancreatic ductal adenocarcinoma cell (PDAC) model driven by pancreas-specific mutations in KRASG12D with either wild-type p53 (KC model; Pdx1-cre; LSL-KrasG12D/+) or one floxed Trp53 allele (KFC model; Pdx1-cre; LSL-KrasG12D/+; Trp53fl/+) (Tan et al., 2014) (Figure 1A, left). Tumors derived from KFC pancreatic tumors revealed increased macrophage F4/80+ staining (Figure 1A, right). We also examined an epidermal growth factor receptor (EGFR)-driven model of lung cancer with (ROSA26tTA-LSL-EGFRL858R, EL) and without p53 (Rosa26tTA-LSL-EGFRL858R;Trp53fl/fl, EFL). Tumors excised at similar endpoints were digested and stained for flow cytometry to detect CD11b+ and F4/80+ tumor immune infiltrates. Frequencies of CD11b+ myeloid-derived cells were significantly increased in EGFR-driven tumors null for p53, which were also enriched in CD11b+F4/80+ macrophages (Figure 1B).
Figure 1.
Cancer-Specific p53 Loss Increases Macrophage Infiltration, Chemokine Secretion, and Migration
(A) Immunohistochemical stain for F4/80 expression in pancreatic tumor sections from Pdx1-Cre;KrasLSL-G12D/+ (KC) (left) and Pdx1-Cre;KrasLSL-G12D/+;Trp53fl/+ (KFC) (right) mice. F4/80+ expression was evaluated based on color intensity per section. Scale bar at 1 μm. Each point on the graphs represents one mouse; cohort size n = 5, the means are represented as ± SEM.
(B) Lung tumors induced by adenoviral Cre were assessed by flow cytometry for CD11b+ and F4/80+ cell infiltrates from mice bearing the following genotypes: ROSA26tTA-LSLEGFRL858R (EL) (gray) and Rosa26tTA-LSLEGFRL858R;Trp53fl/fl (EFL) (red). Cohort sizes n = 8–9; the means are represented as ±SEM.
(C and D) Migration and chemotaxis assays using IncuCyte technology with bone-marrow-derived macrophages (BMDMs) cultured in the presence of conditioned media from PDAC-derived cell lines from KC1 (black) and KFC1 (red) tumors. The means are represented as ±SD of technical replicates (n = 6–8).
(C) Scratch-wound assay performed on BMDMs to measure wound closure.
(D) Chemotaxis assay of BMDMs migrating toward conditioned media of KC1 or KFC1 cancer cells.
(E) Luminex cytokine array performed on three independent KC and KFC cell lines derived from mouse PDACs. Values are represented as fold change in concentration compared to one of the PDAC-derived KC cell lines (KC1), and the means are represented as ± SEM.
(F) Schematic representation of the experimental design. Pancreatic derived cancer cell lines (KC1 and KFC1) were transduced with a near-infrared plasmid (iRFP) and subcutaneously injected into CD1nu/nu recipient mice.
(G) Growth curve represented as fold increase in iRFP fluorescence measured in real time by the Pearl imager over 12 days for KC1 (black circle) and KFC1 (red circle) cell lines injected into CD1nu/nu recipient mice (cohort size n = 5 per genotype). Two-way ANOVA was used for statistical analysis and the means are represented as ±SEM.
(H) Flow cytometry analysis of individual tumor digests for immune infiltrates expressing CD11b+ and F4/80+ surface markers. The means are represented as ±SEM, with cohort sizes n = 7–9.
Student’s unpaired t test was performed when not otherwise indicated, and p values are ∗p < 0.05 and ∗∗p < 0.01. See also Figure S1.
To gain insight into the interplay between macrophages and the p53 status of cancer cells, we isolated primary cancer cells from three independent KC and KFC tumors. KC-tumor-derived cells lines retained p53 expression and activity, showing growth inhibition in response to the p53 activator Nutlin, while cell lines derived from KFC tumors did not express p53 and were resistant to Nutlin treatment (Figures S1A and S1B). Previous studies have also shown that KFC tumors undergo loss of heterozygosity and become p53 null during tumor development (Tan et al., 2014). Reexpression of p53 in tumors can induce their ability to produce various inflammatory cytokines (Iannello et al., 2013), prompting us to examine whether conditioned media from the KC- and KFC-tumor derived cells could impact macrophage surface activation markers: major histocompatibility complex (MHC) class I, MHC class II, PD-L1, and CD80. In comparison to untreated bone-marrow-derived macrophages (BMDMs), conditioned media from all PDAC cell lines induced expression of all the activation markers to similar levels (Figure S1C), although this was not affected by p53 status. As both our autochthonous models (pancreas and lung) displayed a p53-associated change in macrophage infiltration, we examined the effect of conditioned medium on BMDM migration and chemotaxis. Interestingly, BMDMs exposed to conditioned media from KFC-derived cell lines displayed increased migration, demonstrated by enhanced wound healing and chemotaxis, compared to conditioned media from KC cell lines (Figures 1C, 1D, S1D, and S1E).
To explore the basis of this difference in the activity of the conditioned media, we analyzed cytokine secretion from three independently derived p53WT KC and p53-null KFC tumor-derived cell lines. Out of the 35 cytokines tested by a cytokine Luminex array, 20 were detectable and only 5 (CCL11, CXCL1, CXCL5, CCL3, and macrophage colony-stimulating factor [M-CSF]) were elevated in the three KFC cell lines (Figure 1E). While these myeloid-attracting and differentiating cytokines were elevated, T-cell-associated cytokines were not dependent on p53 expression (Figure S1F). Taken together, these results indicate that the KFC tumors secrete cytokines that have a myeloid-macrophage stimulating effect.
To understand the consequences of the p53 status of our tumor-derived cell lines on the myeloid compartment in vivo, we used a T-cell-deficient CD1nu/nu subcutaneous tumor model. In order to track accurately and in an unbiased fashion in vivo tumor growth, KC and KFC cells were engineered to express near-infrared fluorescent protein (iRFP) (Hock et al., 2014, Shcherbakova and Verkhusha, 2013) (Figure 1F). While the initial GEMM KC and KFC tumors arise at different rates, cells derived from these tumors grew at similar rates in CD1nu/nu recipients, as assessed by in vivo real-time imaging of the tumors (Figures 1G, S1G, and S1H). Flow cytometry analysis of tumor digests at endpoint revealed no changes in total frequency of CD11b+ myeloid infiltration; however, CD11b+F4/80+ macrophages were enhanced in KFC tumors, as seen in the autochthonous mouse models (Figures 1H and S1I). These results demonstrate that p53 ablation in the tumor can influence the TME independently of tumor growth.
p53 Deletion Delays Tumor Rejection and Promotes Myeloid-Associated Cytokines
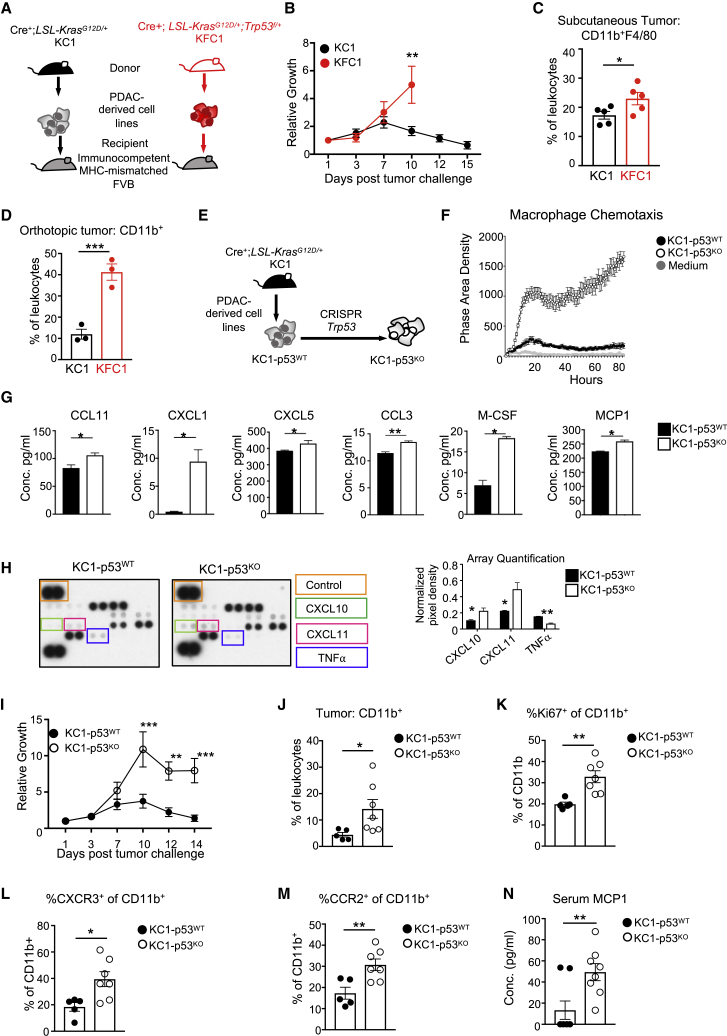
Loss of p53 in the tumor-derived cell lines did not accelerate subcutaneous tumor growth in athymic recipients, despite the increase of CD11b+F4/80+ infiltrates in the TME. We therefore turned to examine the effect of p53 loss in an immunocompetent model. Since our tumor-derived cells originated from mice of a mixed background, we used a tumor rejection model that has been previously employed to explore contributions of tumor-associated genetic alterations on a complete immune response (Chang et al., 2015, Dunn et al., 2005). Mixed strain KC- and KFC-derived cells were injected subcutaneously into pure FVB recipient mice, an immunocompetent MHC-mismatched strain (Figure 2A). The p53WT KC1 cells followed the expected growth kinetics of initial expansion until day 7, followed by progressive rejection. Surprisingly, the p53-null KFC1 cells continued to grow until the point where ethical considerations determined the termination of the study (Figure 2B). A similar pattern of delayed rejection in p53-null cells was seen in two further independently derived KFC cells (Figures S2A and S2B). Further examination of the tumor digests taken from these mice at day 7 showed an increase in F4/80+ macrophages in p53-null (KFC1) tumors (Figure 2C). In order to confirm that the p53-dependent effect on tumor-associated myeloid cells was not site specific, we performed pancreatic orthotopic injections of KC1 and KFC1 cell lines in FVB mice. In line with the genetic tumor models and the subcutaneous models (Figures 1A, 1H, and 2C), p53-null orthotopic tumors displayed increased myeloid infiltration (Figure 2D).
Figure 2.
Tumor Regression, Cytokine Production, and Myeloid Infiltration Are Influenced by p53
(A) Schematic representation of the experimental design. KC1 and KFC1 pancreatic-tumor-derived cell lines expressing iRFP were subcutaneously implanted into FVB, MHC-mismatched recipient mice.
(B) Growth curve of KC1 (black circle) and KFC1 (red circle) cell lines injected into five FVB recipient mice per genotype. Tumor growth is measured as an increase in iRFP signal compared to the original fluorescence count on day 1 using the Pearl imager. Two-way ANOVA was used for statistical analysis, and the means are represented as ±SEM.
(C) Individual tumors were harvested on day 7 post-injection and digested into single cells. Flow cytometry analysis was performed to measure F4/80+ immune tumor infiltrates, and the means are represented as ±SEM.
(D) KC1 (black circle) and KFC1 (red circle) cells were orthotopically injected into the pancreas of FVB recipients (cohort size n = 3 per genotype). Graph shows percentage of pancreatic CD11b+ infiltrates 7 days post-operation, and the means are represented as ±SEM.
(E) Schematic representation of the experimental design. KC1 PDAC cells were deleted for Trp53 by CRISPR, generating an isogenic pair (KC1-p53WT and KC1-p53KO).
(F) A chemotaxis assay performed on BMDMs migrating towards KC1-p53WT or KC1-p53KO conditioned medium, or culture medium. The extent of BMDM migration was calculated as phase area density of technical replicate wells (n = 8) and the means are represented as ±SD.
(G) Enzyme-linked absorbent assays (ELISAs) were performed with conditioned medium collected from KC1-p53WT (black) and KC1-p53KO (white) cells. ELISAs from left to right are CCL11, CXCL1, CXCL5, CCL3, M-CSF, and MCP1. Concentration was measured as pg/mL and the means are represented as ±SD.
(H) Cytokine array of conditioned media from KC1-p53WT (left) and KC1-p53KO (right) cell lines. (Left) Boxed duplicate dots show changes in CXCL10 (green), CXCL11 (pink), TNF-α (blue), with a positive invariant control (orange). (Right) pixel quantification of each dot normalized to the positive control and the means are represented as ± SD.
(I) 6 mice were injected with either the KC1-p53WT (black circle) or the KC1-p53KO (open circle) cells. The growth curve was measured by in vivo imaging of iRFP using the Pearl imager and graph shows fold increase in fluorescence from day 1 post-injection. Two-way ANOVA was used for statistical analysis, and the means are represented as ± SEM.
(J–M) Tumors derived from KC1-p53WT (n = 5) or KC1-p53KO cells (n = 7) were digested into single-cells at day 3 post-injection. Digests were analyzed for infiltrating myeloid populations by flow cytometry. Graphs show tumors from individual mice, and the means are represented as ±SEM.
(J) Flow cytometry analysis showing frequencies of tumor-infiltrating CD11b+ myeloid cells in mice harboring KC1-p53WT (black circles) or KC1-p53KO (open circles) tumors.
(K) Frequency of proliferating intratumoral CD11b+ populations measured by Ki67 staining.
(L) Frequency of CXCR3 expression on infiltrating CD11b+ cells.
(M) Percentage of CD11b+ cells within tumor digests expressing surface CCR2.
(N) Serum collected at endpoint (day 14) from FVB mice injected with the KC1-p53WT cell line (n = 8) or the KC1-p53KO cell line (n = 8) and analyzed for circulating levels of MCP1 by ELISA. The means are represented as ±SEM.
Student’s unpaired t test was applied to experiments unless otherwise indicated and p values are ∗p < 0.05, ∗∗p < 0.01. See also Figure S2.
One potential caveat with tumors arising in genetically engineered mice is that additional genetic alterations acquired during tumor development may also contribute to tumor-immune interactions. To test directly the effect of p53 loss, we used gene editing to delete p53 from two KC-p53WT cell lines (KC1 and KC2), generating matched isogenic cell lines named KC1-p53KO and KC2-p53KO (Figure 2E). BMDM chemotaxis assays using conditioned media from KC1-p53WT and KC1-p53KO PDAC cell lines confirmed our previous findings that KFC-p53KO conditioned media enhanced BMDM migration (Figure 2F). ELISAs for CCL11, CXCL1, CXCL5, CCL3, M-CSF, and MCP1 (Figure 2G) showed that as seen in the tumor-derived KFC cell lines, p53 loss increased production of these cytokines (Figures 2G and S2C). Additionally, we performed an unbiased analysis of 62 cytokines in conditioned media from KC1-p53WT and KC1-p53KO cells, which further revealed increased CXCL10 and 11, and decreased tumor necrosis factor α (TNF-α) secretion (Figure 2H). Of note, CXCL10 and 11 uniquely bind to the CXCR3 receptor. Our results show that cancer cells deficient for p53 increase the production of chemokines involved in myeloid recruitment and macrophage differentiation.
Turning back to the in vivo rejection model, we found that the isogenic p53KO cells displayed delayed rejection kinetics, similar to PDAC cells that lost p53 during tumor development (Figures 2I and S2D). At an early time point (3 days post-injection), CD11b+ myeloid cells were enriched in p53-deleted tumors in comparison to their parental p53WT controls (Figure 2J), although this difference was lost by day 7 (Figure S2E). Next, we looked more closely for potential in vivo consequences of the changes in cytokine secretion detected in vitro. M-CSF is a key driver of myeloid differentiation and proliferation, and we detected a 2-fold increase of proliferating CD11b+Ki67+ myeloid cells in p53KO tumors (Figures 2K and S2F), correlating with enhanced M-CSF production by these cells. We also probed for myeloid cells expressing CXCR3 (the receptor for CXCL9-11) and CCR2 (one of the receptors for CCL11 and uniquely a receptor for MCP1) (Martinelli et al., 2001) within our tumor digests. Interestingly, both CXCR3+ and CCR2+ infiltrating CD11b+ myeloid cells were significantly enhanced within KC1-p53KO tumors (Figures 2L, 2M, and S2G), correlating with increased production of the cytokines for these receptors by the p53-deleted tumor cells. We further confirmed an increase in intra-tumoral CD11b+ cells expressing CXCR3 in the second isogenic tumor pair at day 3 (Figure S2H). Systemic cytokine changes were also observed in tumor-bearing mice. At endpoint (day 14 post-tumor challenge), mice harboring p53-null tumors displayed significantly increased serum levels of MCP1 (Figure 2N). In conclusion, data from both GEMM-derived cells and the isogenic pairs show that loss of p53 in tumor cells promotes the production of cytokines involved in myeloid recruitment and homeostasis.
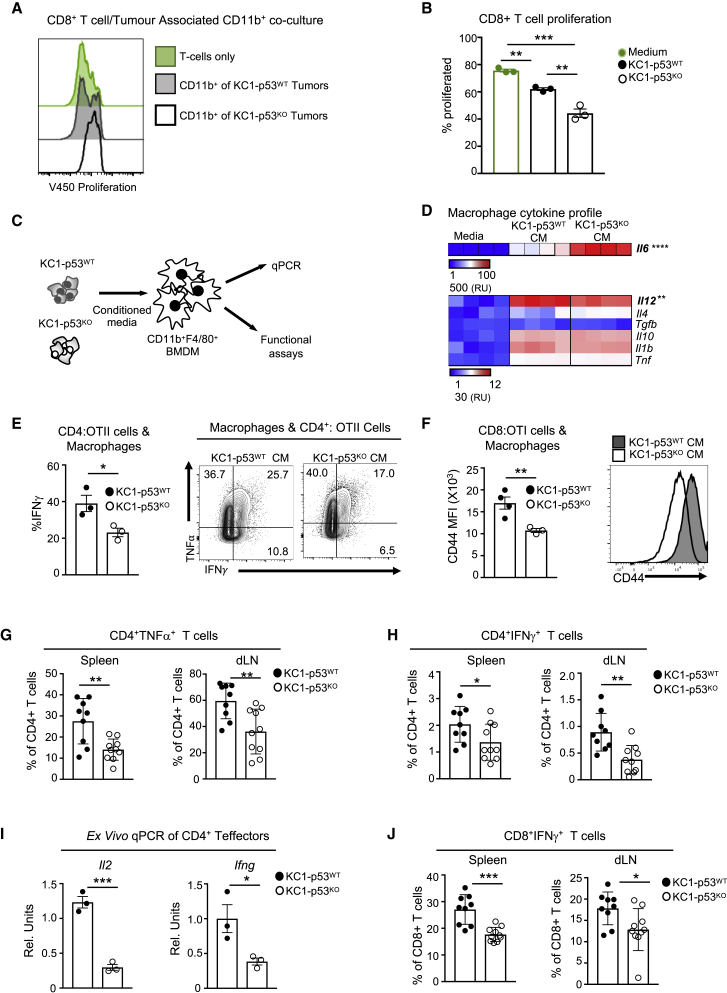
p53-Null Tumors Reeducate Myeloid Cells to Attenuate T Cell Responses
Our observation that loss of p53 affects tumor growth in immunocompetent, but not athymic, mice indicated that an intact T cell response is required for the rejection of p53-expressing cells. To test whether the CD11b+ cells found in the KC1-p53KO tumors were immune suppressive, we isolated CD11b+ cells from the tumors at day 3 and co-cultured them with preactivated T cells stained with the v450 proliferation dye. While the myeloid cells derived from both tumors attenuated T cell proliferation, the myeloid cells isolated from KC1-p53KO tumors more robustly inhibited CD4+ and CD8+ T cell proliferation (Figures 3A, 3B, S3A, and S3B). These observations were confirmed in the second pair of isogenic cells (Figures S3C and S3D).
Figure 3.
Tumoral Loss of p53 Promotes Suppressive Myeloid Lineages and Reduces T Cell Activation
(A) CD11b+ cells isolated from individual KC1-p53WT (gray shade) and KC1-p53KO (black line) tumors 3 days post-injection and co-cultured with pre-activated CD8+ T cells stained with V450 proliferation dye. Cells were analyzed after 48 h. T cell proliferation in the absence of CD11b+ cells is denoted in green.
(B) Graph displays percent proliferation of CD8+ T cells with tumor-derived CD11b+ cells isolated from individual KC1-p53WT (black) or KC1-p53KO (white) tumors or in the absence of CD11b+ cells (green). Each dot represents CD11b+ cells derived from a pool of two tumors per genotype and means are represented as ±SEM.
(C) Schematic representation of the experimental design. BMDMs activated with conditioned media (CM) from KC1-p53WT or KC1-p53KO cells and screened for cytokine expression by qPCR and functional assays.
(D) mRNA expression of T-cell-polarizing cytokines expressed by BMDMs incubated in the presence of IMDM (medium), or KC1-p53WT, or KC1-p53KO conditioned media. Red indicates higher and blue lower expression levels, where each lane represents BMDMs derived from individual mice; the means are represented as ±SEM.
(E and F) Incubation of BMDMs with conditioned media, followed by a 2-h pulse of ovalbumin and co-cultured with CD4+OTII or CD8+OTI cells, respectively. Graphs show one of three experiments and display technical replicates (n = 3-4); means are represented as ±SD.
(E) OTII CD4+ T cells restimulated with OVA 323-339 peptide after co-culture with BMDMs educated by KC1-p53WT CM (closed circles) or KC1-p53KO CM (open circles). Representative flow cytometry plot (right) of restimulated OTII T cells followed by intracellular cytokine staining (ICS) for IFN-γ and TNF-α after 4 days of differentiation.
(F) CD8+OTI cells activated by BMDMs pulsed with OVA and measured by flow cytometry for surface expression of CD44, shown as mean fluorescence intensity (MFI). Left graph represents technical replicates for CD44 MFI, and on the right, the histogram shows CD44 surface expression.
(G–J) Analysis of CD4+ and CD8+ T cells in the periphery of FVB recipients injected with KC1-p53WT (black) or KC1-p53KO (white) cell lines. Graphs show biological replicates and the means are represented as ±SEM.
(G and H) Intracellular cytokine flow cytometry analysis of spleen and draining lymph nodes of FVB mice bearing KC1-p53WT and KC1-p53KO tumors (n = 9–10 FVB per genotype), 7 days post injection. Graphs illustrate (G) CD4+ T cells expressing TNF-α and (H) CD4+ T cells producing IFN-γ upon ex vivo restimulation with PMA, ionomycin, and GolgiStop (n = 9–10 per genotype).
(I) CD4+ T cells isolated from KC1-p53WT and KC1-p53KO tumor-bearing FVB mice and cell sorted for CD4+ CD25− populations. qPCR was performed on RNA isolated from ex vivo sorted CD4+ CD25− T cells and tested for Il2 and Ifng mRNA. The means are represented as ±SEM, and each point represents two pooled mice (cohort size n = 6 per genotype).
(J) Ex vivo restimulation of spleen and dLN from tumor bearing FVB mice to detect CD8+T cells producing IFN-γ. The means are represented as ±SEM (cohort size n = 9–10 per genotype).
Unpaired t tests were performed on all data except for multiple comparisons, where Tukeys’s multiple comparisons test was used. p values are ∗p < 0.05, ∗∗p < 0.01, and ∗∗∗p < 0.001. See also Figure S3.
Cancer cells have been shown to influence the crosstalk between myeloid cells and T lymphocytes (Cooks et al., 2018), so we examined the effect of conditioned media from KC1-p53WT and KC1-p53KO cells on BMDM-dependent T-cell-activating functions (Figure 3C). Focusing on cytokines involved in CD4+ T helper and CD8+ cytotoxic T lymphocyte (CTL) differentiation, we found only two of the seven cytokines showed significantly changed mRNA expression in response to KC1-p53KO conditioned media; namely, a strong increase in expression of Il6, a T helper 1 (Th1) cell antagonist, and a subtler decrease in expression of Il12, a Th1-cell- and CTL-promoting cytokine (Figure 3D). These changes predict that BMDMs conditioned by KC1-p53KO media would show impaired polarization of CD4+ Th1 cells and CTL activation (Athie-Morales et al., 2004, Dodge et al., 2003, Wu et al., 2015). To verify this hypothesis, we co-cultured BMDMs pulsed with the model antigen ovalbumin (OVA) with T cell receptor (TCR)-transgenic CD4+ or CD8+ T cells recognizing the OVA peptides (OTII [CD4+] or OTI [CD8+] T cells). BMDMs educated by KC1-p53KO conditioned media and loaded with OVA peptide were less effective in differentiating Th1 cells, as demonstrated by reduced interferon-γ (IFN-γ)+TNF-α+-producing OTII CD4+ T cells (Figure 3E). Furthermore, CTL activation was compromised by KC1-p53KO-instructed BMDMs, as shown by the weaker expression of the activation marker CD44 on CD8+ OTI cells (Figure 3F). Led by our mouse data, we stratified pancreatic cancer patients from The Cancer Genome Atlas (TCGA) dataset according to a designed gene list based on classical MDSC markers, including ITGAM (CD11b) and CXCL10 (Figure S3E). Patients with a high MDSC signature displayed statistically lower overall survival (Figure S3F). Interestingly, patients with a high MDSC gene signature trended toward an enrichment of TP53 mutations compared to the low-MDSC-signature population (Figure S3G). Taken together, these data demonstrate that p53 deletion in cancer cells creates a tumor-promoting environment through remodeling myeloid-T cell crosstalk.
Encouraged by our in vitro and ex vivo results, we assessed T cell activity in mice bearing GEMM-derived or isogenic p53WT and p53-null tumors. Ex vivo restimulation of the spleen and tumor draining lymph node (dLN) on day 7, when tumors were of equivalent sizes, revealed a reduction in anti-tumor T cell responses (as measured by CD4+ Th1 TNF-α+ and IFN-γ+ cells) in mice bearing p53-null tumors from either isogenic (Figures 3G, 3H, and S3H) or the GEMM-derived lines (Figures S3I and S3J). Furthermore, sorted CD4+CD25− T cells from mice bearing KC1-p53KO tumors expressed less Il2 and Ifng mRNA than CD4+CD25−T cells from KC1-p53WT recipients (Figure 3I), suggesting an overall lack of CD4+ T cell activation. Impaired CD8+ CTL IFN-γ+ production further demonstrated weakened T cell responses in mice carrying p53-null tumors (Figures 3J and S3K–S3M). Overall, our data suggest that p53 deletion in cancer cells undermines T cell effector responses, at least in part through co-opting myeloid cell functions.
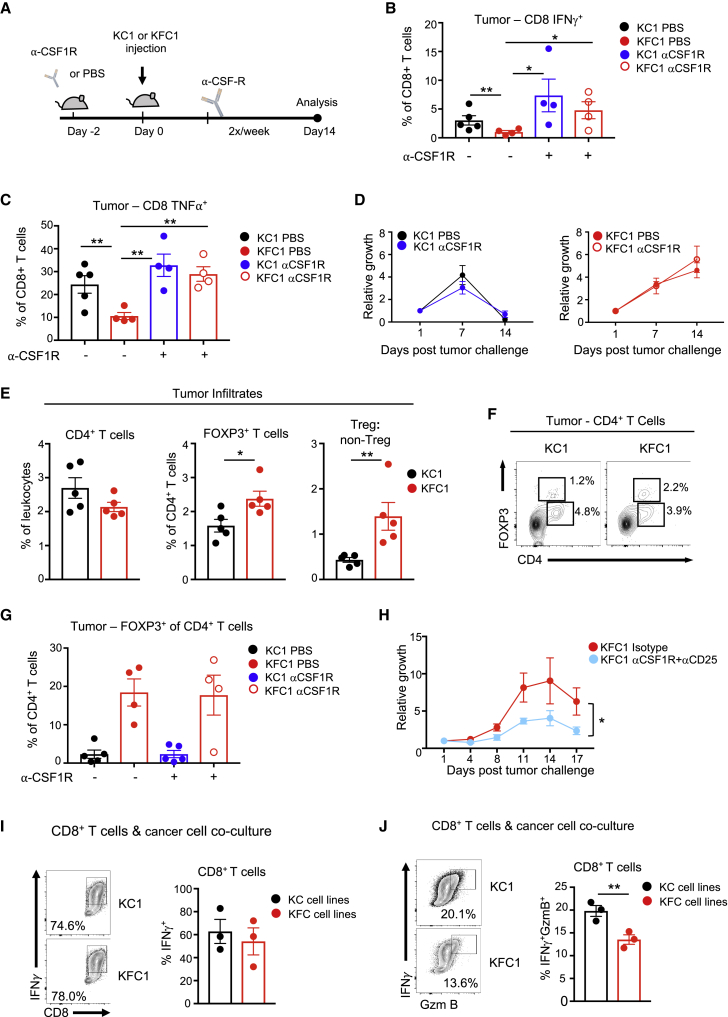
Combination Therapy of CSF1R and CD25 Blockade Attenuates p53-Null Cancer Cells
Our in vitro data suggested that the dampened T cell responses seen in mice bearing p53KO tumors may be a consequence of pro-tumorigenic myeloid cells responding to elevated M-CSF from p53-ablated cancer cells (Figure 2G). To test the contribution of M-CSF production by p53-null cells to the modulation of the T cell response in vivo, we treated immunocompetent mice challenged with either p53WT or p53-null tumor cells with neutralizing antibodies against CSF1R, the receptor for M-CSF (Figure 4A). CSF1R specificity was confirmed by showing the expected compensatory increase in serum M-CSF levels in treated mice (Bartocci et al., 1987), with no change in serum granulocyte colony-stimulating factor (G-CSF) (Figures S4A and S4B). Subcutaneous tumors were harvested at day 7, and effector function of infiltrating CD4+ and CD8+ T cells was assessed. Consistent with results from spleen and dLN of tumor-bearing mice, vehicle-treated, p53-null tumors contained less activated effector CD4+ and CD8+ T cells secreting IFN-γ and TNF-α (Figures 4B, 4C, and S4C–S4E). CSF1R blockade restimulated T cell function in p53-null tumors to levels seen in p53-WT tumors (Figures 4B, 4C, and S4C–S4E) but did not change the rate of rejection of tumors of either genotype (Figure 4D). Furthermore, T cell reactivation in p53-null tumors was irrespective of absolute tumor size, as confirmed by in vivo imaging of the tumors (Figure S4F). These data suggest that inhibition of M-CSF signaling that is induced by p53-deleted cells can reactivate T cell function within the tumor but fails to promote rejection when used as a monotherapy.
Figure 4.
CSF1R Blockade Increases the Activation of Intratumoral T Cells in p53-Null Tumors but Depends on Treg Cell Depletion for Regression
(A) Scheme of CSF1R blockade administration and subcutaneous growth in FVB mice.
(B and C) Isolated tumors at day 7 from mice injected with PBS (untreated) or CSF1R neutralizing antibody (treated), digested and ex vivo restimulated with PMA, ionomycin, and GoligStop. Each point represents one individual tumor (cohort size n = 4–5), and the means are represented as ±SEM. (B) CD8+ IFN-γ+ and (C) CD8+ TNF-α+ in KC1 control (black circles), KC1 treated (blue), KFC1 (red), and KFC1 treated (red open circles) mice.
(D) Subcutaneous growth of KC1 PDAC tumors treated with PBS (black line) or anti-CSF1R (blue) and KFC1 PDAC tumors treated with PBS (red) or anti-CSF1R (red open circle) in FVB recipients (cohort size n = 5 per condition). The means are represented as ±SEM.
(E) Tumors were processed and stained for CD4+ infiltrates and expression of FOXP3. Graph on the right shows the ratio of Treg cell/non-Treg populations in tumor infiltrating CD4+ cells. The means are represented as ±SEM with cohort sizes n = 5.
(F) Representative flow cytometry plots of CD4 and FOXP3 expressing T cells in individual tumors of each genotype.
(G) Flow cytometry analysis of tumor digests for CD4+ FOXP3+ T cell infiltration in tumors of untreated and treated mice, where each point represents one tumor. Means are represented as ±SEM, with sample sizes n = 4-5.
(H) Growth curve using in vivo imaging of the KFC1 tumors treated with isotype control (red) (n = 5) or with αCD25 treatment followed by αCSF1R treatment (blue) (n = 5) over 17 days post-tumor challenge. Graph shows relative growth compared to day 1 measured by in vivo fluorescence. Two-way ANOVA was used for statistical analysis and the means are represented as ±SEM.
(I and J) Flow cytometry analysis of in-vitro-activated CD8+ T cells cocultured with individually derived PDAC cell lines.
(I) IFN-γ production of restimulated CD8+ T cells with independent KC (KC1-3) or KFC (KFC1-3) PDAC cell lines shown as a representative flow cytometry plot (left) and as a graph showing biological replicates (right). Means are represented as ±SEM.
(J) IFN-γ+GzmB+-producing CD8+ T cells assessed by restimulation and ICS. Representative flow cytometry plot of restimulated and stained CD8+ T cells (left). Each dot on the graph (right) represents one co-culture of pre-activated CD8+ T cells with KC (black) (KC1-3) or KFC (red) (KFC1-3) cell lines. The means are represented as ±SEM. Co-culture experiments represent one of three independent experiments.
An unpaired Student’s t test was applied unless otherwise indicated. p values are ∗p < 0.05 and ∗∗p < 0.01. See also Figure S4.
The failure of CSF1R blockade to promote tumor rejection prompted us to investigate other mechanisms of immune suppression that may reflect additional effects of tumor cells on T cell function. One essential immunosuppressive population that is at the epicenter of T cell immune tolerance are Treg cells (Sakaguchi et al., 2008), which are currently being targeted for cancer immunotherapies (Tanaka and Sakaguchi, 2017). Flow cytometry analysis of the original untreated tumors showed an accumulation of Treg cells within p53-null tumors with no changes in CD4+ T cell frequencies (Figure 4E). Tumors deleted for p53 were biased toward Treg cells, as assessed by the Treg cell/non-Treg cell ratio of CD4+ T cell infiltrates (Figures 4E and 4F). The inability of CSF1R blockade to reduce intra-tumoral Treg cell frequencies (Figure 4G) led us to perform a double blockade targeting both CSF1R and Treg cells using αCD25 to eradicate Treg cells. This method is well established to effectively deplete Treg cells (Onizuka et al., 1999, Setiady et al., 2010, Shimizu et al., 1999), although various studies have shown that CD25 blockade alone does not effectively block the growth of established tumors (Arce Vargas et al., 2017, Onizuka et al., 1999). Using a combined treatment of αCD25 for 3 days prior to tumor challenge followed by an αCSF1R regime, we were able to attenuate the growth of the p53-null tumors in FVB recipients (Figure 4H). These intervention data suggest that immunotherapy for p53-compromised tumors requires targeting both the myeloid and Treg cell compartments for a positive outcome.
Finally, we examined the consequences of direct interactions between CD8+ cytotoxic T lymphocytes (CTLs) and cancer cells. CTL cytotoxic function is elicited by IFN-γ and granzyme B (GzmB) production and can be affected by cancer cells (Fischer et al., 2007). CTLs co-cultured with KC-p53WT and KFC-p53KO cells were equally capable of secreting IFN-γ (Figure 4I). However, co-culture with KFC-p53KO cells clearly impaired CTL GzmB production upon restimulation (Figure 4J).
Tumor cells can evade CTL responses through downregulation of MHC class I surface expression (McGranahan et al., 2017), although this was not observed in the p53-null PDAC-tumor-derived cells (Figure S4G). In order to assess if loss of p53 in cancer cells influences their ability to present endogenous peptides, we introduced the model antigen, OVA, into the isogenic PDAC cell lines. Co-culturing of peptide-stimulated OTI cells with KC1p53WT-mOVA and KC1p53KO-mOVA increased cell death in both PDAC cell lines, as marked by increased propidium-iodide-positive cells. However, loss of p53 did not lead to an increased resistance to OTI killing by MHC class I (Figure S4H). Taken together, these results indicate that immune evasion in response to loss of p53 reflects both an accumulation of suppressive Treg cells and inhibition of T cell cytotoxic functions.
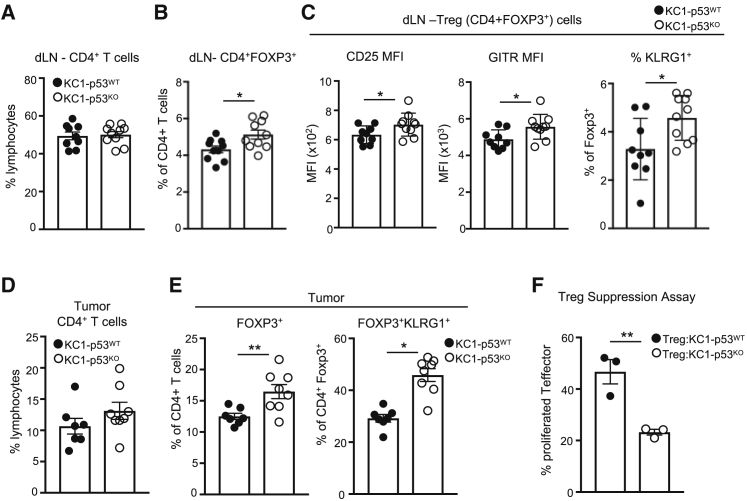
CancerCell-Associated Loss of p53 Selects for Suppressive Regulatory T Cell Lineages
Our observation that targeting Treg cells in parallel with CSF1R was critical in reducing tumor growth of p53-null cells prompted us to examine the effect of the p53 status of cancer cells on regulatory T cells more closely. Treg cells have different degrees of suppressive abilities, which can be phenotypically identified through surface expression of CLTA-4, KLRG1, and GITR and high expression of CD25 (Arpaia et al., 2015). Mice bearing KFC1 p53-null tumors displayed increased systemic presence of CD4+FOXP3+CTLA-4+ T cells in the spleen and dLN (Figures S5A and S5B), suggesting a greater suppressive immune response. To determine whether the skewing toward more suppressive Treg cells depended on the site of the tumor, we orthotopically implanted KC1 and the KFC1 cell lines into the pancreata of FVB recipients. Tumors of both genotypes were detected in the pancreas at day 7 (Figure S5C) with a strong accumulation of highly suppressive Treg KLRG1+ cells in p53-null pancreatic tumors (Figure S5D).
To validate the p53 specificity of these Treg cell responses, we turned again to the isogenic KC1-p53WT and KC1-p53KO cells. Identical CD4+ T cell frequencies were present in the tumor dLN of both KC1-p53WT and KC1-p53KO recipients (Figure 5A). However, the proportion of FOXP3+ (Treg) cells present within the CD4+ population was enhanced in mice bearing KC1-p53KO cancer cells (Figure 5B). Phenotypic characterization of these Treg cells revealed an increase in the proportion expressing markers of suppression (high CD25, GITR, and KLRG1 expression) (Figures 5C and S5E). In addition, while p53 status did not affect total CD4+ T cell frequency in the tumor (Figure 5D), KC1-p53KO tumors accumulated more FOXP3+ Treg cells, especially those with KRLG1 surface expression (Figure 5E). Consistent with these data, ex vivo Treg cell suppression assays of CD4+CD25+ Treg cells sorted from tumor-bearing mice showed that Treg cells isolated from KC1-p53KO recipients were more efficient at inhibiting the proliferation of CD4+CD25− T cells in vitro (Figures 5F and S5F). Both our in vivo characterization and ex vivo functional assays highlight the relationship between tumor p53 loss and the local and systemic accumulation of regulatory T cell responses.
Figure 5.
p53 Loss Increases Intratumoral and Systemic Suppressive Treg Cell Lineages
(A–E) Flow cytometry analysis of tumors from FVB mice injected with the isogenic cells lines KC1-p53WT (black circles) and KC1-p53KO (open circles) and analyzed 7 days post-injection. Cohort sizes n = 7–10, the means are represented as ±SEM.
(A) CD4+ T cell frequencies in the dLN from KC1-p53WT KC1-p53KO recipients.
(B) Intracellular staining of FOXP3 and CD4 surface expression in T cells within the dLN.
(C) The mean fluorescence intensity (MFI) of CD25 and GITR and the frequency of KLRG1 surface expression within Treg cell populations in tumor dLN.
(D) Frequencies of CD4+ T cell infiltration in KC1-p53WT KC1-p53KO tumors.
(E) Intracellular staining for FOXP3 in tumor-infiltrating CD4+T cells (left) and surface expression of KLRG1 within the CD4+FOXP3+ T cell population (right).
(F) Ex vivo Treg suppression assay of sorted CD4+CD25+ Treg cells from mice (cohort size n = 6) injected with KC1-p53WT (black circles) and KC1-p53KO (open circles) cell lines. Data show percentage of proliferating co-cultured CD4+CD25− T cells that were stained with v450 proliferation dye. Each point represents CD4+CD25+ Treg cells from two pooled recipient FVB mice, and the means are represented as ±SEM.
An unpaired Student’s t test was used for statistics with p values of ∗p < 0.05 and ∗∗p < 0.01. See also Figure S5.
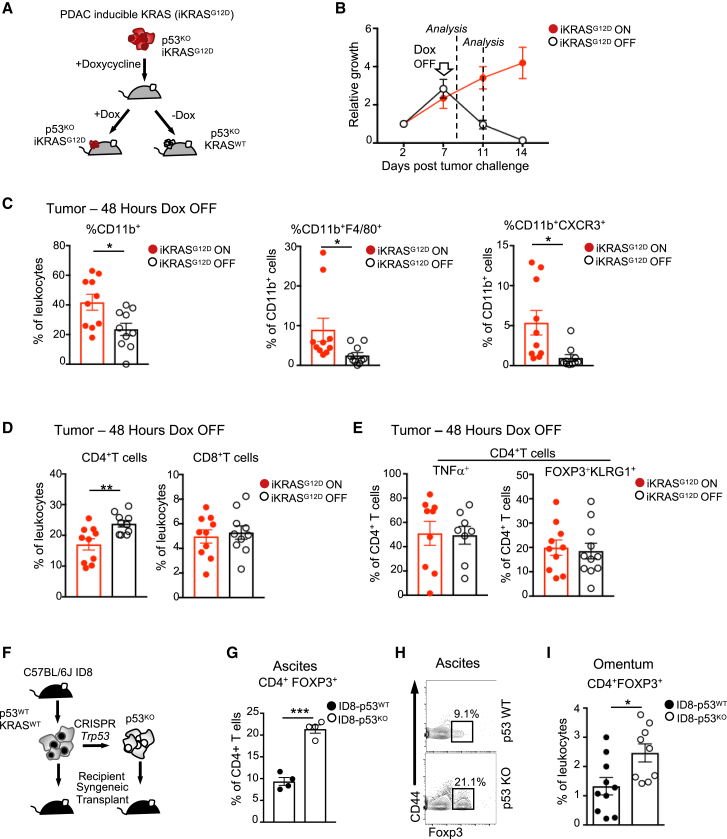
KRAS Mutations Coordinate with p53 Loss for Myeloid, but Not Treg, Cell Recruitment
In humans, nearly 90% of pancreatic cancer patients show mutations in KRAS (cBioportal) (Cerami et al., 2012), and our autochthonous models were based on mutations in KRAS or in upstream signaling receptors (EGFR). Recent work has shown that activating KRAS mutations can drive an immunosuppressive response in cancer cells through increased PD-L1 expression (Coelho et al., 2017). In order to examine the role of KRAS activation in promoting tumor tolerance in the context of p53 loss, we used previously described doxycycline (Dox)-inducible KRASG12D-driven p53-null PDAC mouse cells (Ying et al., 2012) (Figure 6A). Tumors were initiated for 7 days in FVB recipient mice treated with Dox to drive mutant KRAS expression before either maintaining Dox treatment (iKRASG12D-ON) or removing Dox (iKRASG12D-OFF). Despite the lack of p53 in all of these tumor cells, removal of Dox resulted in complete eradication of the tumor within 7 days (Figure 6B). We evaluated early and late tumor-associated immune infiltrates at 48 h and 5 days post-Dox withdrawal. Within 48 h of Dox removal, iKRASG12D-OFF tumors displayed reduced frequencies of CD11b+ cells, especially those positive for F4/80 and CXCR3 expression (Figure 6C), with a modest influx of CD4+ T cells but no changes in CD8+ T cell frequencies (Figure 6D). At this time point, iKRASG12D-ON and iKRASG12D-OFF tumors showed no difference in CD4+ T effector cells or CD4+FOXP3+KLRG1+ suppressive Treg cells (Figure 6E).
Figure 6.
KRAS Coordinates with p53 Loss for the Recruitment of Myeloid, but Not Treg, Cells
(A) Schematic representation of the inducible iKrasG12D/+;Trp53f/f PDAC cell model (iKRASG12D).
(B) Growth kinetics of the iKRASG12D cell line (red circles) expressing iRFP subcutaneously injected into FVB recipients. Doxycycline (Dox) was maintained (red circles) or removed at day 7 (open circles) to modulate mutant KRAS expression. Tumor growth was measured using in vivo imaging using the Pearl imager and expressed relative to initial iRFP fluorescence at day 1 post-injection. Cohort sizes n = 10 and the means are represented as ±SEM.
(C–E) Analysis of individual tumor infiltrates of myeloid and T cell subsets 48 h post-Dox withdrawal. Cohort sizes n = 8−12 and the means are represented as ±SEM.
(C) Analysis of CD11b+, CD11b+F4/80+, and CD11b+CXCR3+ tumor-associated myeloid cells analyzed by flow cytometry (open circles Dox OFF and red circles Dox ON).
(D) Flow cytometry analysis of CD4+ and CD8+ T cell infiltrate frequencies.
(E) Analysis of intra-tumoral CD4+ T cell post ex vivo restimulation for expression of TNF-α+ (left) and CD4+FOXP3+KLRG1+ (right).
(F) Schematic representation of experimental design. C57Bl6/J-derived ID8 ovarian cancer cell lines were deleted of Trp53 using CRISPR/Cas9 and injected intraperitoneally into syngeneic recipients.
(G–I) Flow cytometry analysis of ascites and omentum at equivalent endpoints from mice bearing ID8-p53WT (black circles) and ID8-p53KO (open circles) tumors.
(G) CD4+FOXP3+ Treg cells in the ascites. Cohort size n = 4; means are represented as ±SEM.
(H) Representative plot of CD4+ T cells expressing FOXP3 and CD44.
(I) CD4+FOXP3+ T cells in tumor-immune infiltrates in the omentum Cohort size n = 9–10; means are represented as ±SEM.
A two-way ANOVA was used to analyze in vivo growth kinetics, and an unpaired Student’s t test was used for all bar graphs. p values are ∗p < 0.05, ∗∗p < 0.01, and ∗∗∗p < 0.001. See also Figure S6.
Evaluation of peripheral T cells in recipient mice 5 days after Dox removal showed a significant increase of pro-inflammatory CD4+ and CD8+ T cells in the spleen and a trend toward an increase in the dLNs under iKRASG12D-OFF conditions (Figures S6A and S6B). There was no overall change in suppressive Treg cell populations (Figure S6C). These data suggest that KRAS inactivation in part reactivates T cell effector immune responses but has no impact on the accumulation of regulatory T cells. To further explore the cooperation between p53 loss and KRAS activation, we turned to a previously described model of isogenic C57Bl6/J ID8 ovarian cancer cells with and without p53, which are WT for KRAS (Walton et al., 2016). These cells were injected into the peritoneum of syngeneic C57Bl6/J mice (Figure 6F), and as we previously published, there was a skewing toward PMN cells present in the ascites of mice carrying p53KO tumors (Walton et al., 2016). Interestingly, while there was no change in the total frequency of CD4+ T cells (Figures S6D and S6E), the ascites from mice injected with ID8 p53KO cells showed a 2-fold increase of regulatory T cells (Figures 6G and 6H) and a preferential skewing toward Treg cells, as illustrated by the FOXP3+ to FOXP3− ratio (Figure S6F). A major site of ovarian cancer spread is to the omental fat or the omentum (Worzfeld et al., 2017). Processing and staining of omental tumors for flow cytometry revealed enriched populations of regulatory T cells present in p53-ablated lesions (Figure 6I). These results further support a model in which p53 loss in tumors promotes Treg cell infiltration.
Discussion
In this study, we showed that p53-deficient tumors can re-orchestrate the innate immune response through suppression of effector CD4+ and CD8+ T cells, which reflected an increase in the inhibitory actions of myeloid suppressor cells and regulatory T cells, accompanied by a direct impairment of GzmB in CD8+ T cells. Other studies have shown that mutations in p53 correlate with reduced GzmB in gastric cancers (Jiang et al., 2018) and a CSF1 (M-CSF) response signature in breast cancers (Beck et al., 2009). Somatic changes in the tumor can also induce systemic changes beyond the tumor microenvironment, and we showed dampened local and systemic T cell effector function in mice harboring p53-deficient tumors, seen as decreased IFN-γ and TNF-α production (Figure 3). We propose that these weakened T cell responses are partially mediated by suppressive myeloid cells derived from the tumor as well as through Treg cell suppressive functions. Conditioned media from p53-null cancer cells alters the cytokine profile of BMDMs, which in turn influences CTL and Th1 cell differentiation (Figure 3). These observations are consistent with previous publications showing that tumor-derived CD11bGr+ cells promote the de novo differentiation of Treg cells in prostate cancer models and reduce circulating IFN-γ-producing T cells in B cell malignancies (Bezzi et al., 2018, Christopoulos et al., 2011). Systemic changes were also seen in p53-deficient breast cancer models, which also showed an increase in MCP1 serum levels similar to those seen in our p53-null tumor-bearing mice (Wellenstein et al., 2019).
It is important to note that unlike the response to reexpression of p53 in p53-null cancers, the p53-expressing cells in our study did not undergo senescence and maintained proliferative ability that was similar to the p53-null cells both in vitro and in vivo (Figure 1). Recent studies have attributed changes in cytokine profiles to oncogenic drivers, such as mutation in KRAS, MYC, and loss of PTEN (Coelho et al., 2017, Kortlever et al., 2017, Peng et al., 2016, Pylayeva-Gupta et al., 2012). Our data suggest that one consequence of p53 loss is enhanced secretion of cytokines involved in myeloid recruitment and proliferation. Our work suggests the loss of p53 in tumors has a complex effect on cytokine secretion of both tumor and macrophage populations, ultimately affecting the T cell response. These observations complement recent work showing that an increase in WNT secretion in response to p53 loss in breast cancer cells can stimulate systemic inflammation and drive metastasis (Wellenstein et al., 2019). The complexity of the immune response to p53 loss is further highlighted by a recent study showing that loss of p53 in a prostate cancer model increases expression of CXCL17 and CXCL5 and consequent attraction of tumor-promoting Gr-1+CD11b+ cells (Bezzi et al., 2018). Consistent with our study, loss of p53 in the prostate model also led to an increased expression of CXCL9 and CXCL10 (Bezzi et al., 2018). Although we were unable to identify any changes in the intrinsic ability of p53-null cancer cells to present antigen, previous studies have shown p53-dependent alterations in antigen presentation (Wang et al., 2013, Zhu et al., 1999), and it remains possible that cell-intrinsic changes also play a role in the immune response to p53 loss.
Although blockade of the M-CSF receptor, CSF1R, produced a positive effect in allowing infiltration of T cell effector function in the p53-null tumors, this was not sufficient for rejection. This observation dovetails with a previous study targeting CSF1R with PD-L1 in an orthotopic pancreatic model (with mutations in KRAS and loss of INK) to increase the efficacy of PD-L1 blockade (Zhu et al., 2014). Blocking CSF1R by chemical targeting in the p53R172H Kras pancreatic mouse model has shown a 2-week increase in survival and, as we also showed, an increase in T cell effector function (Candido et al., 2018). In addition, macrophage depletion with clodronate and CSF1R inhibition did not provide therapeutic benefit to primary tumors in the KPC pancreatic cancer model, similar to our results (Griesmann et al., 2017). Given the complexity of the immune modulatory response to loss of p53, it is not surprising that reversal of only one part of the response is insufficient to fully regain tumor rejection, since CD11b+ and Treg cell populations remained enriched in p53-null tumors. By targeting both suppressive populations through double blockade with anti-CSF1-R and anti-CD25, we were able to diminish the growth of p53-null tumors in an MHC-mismatched recipient. Indeed, our data show that the enhanced Treg cell infiltration into p53-null tumors is not prevented by CSF1R blockade, highlighting the importance of a combination immunotherapy.
MSDCs and Treg cells are two major immune-suppressive populations hijacked by many cancer cells. MDSCs arise and expand under pathological conditions, especially during cancer. Naturally occurring Treg cells are a heterogeneous population, with different surface markers predicting suppressive capacity (Cheng et al., 2012). In both our subcutaneous and orthotopic models, we detect an enrichment of KLRG1+ and CLTA4+ Treg cells in p53-null tumor-bearing mice. KLRG1+ Treg cells are considered a highly suppressive and terminally differentiated population of Treg cells that arise during tissue repair, such as influenza-induced lung injury, and help in tissue regeneration (Arpaia et al., 2015). Consistently, Treg cells isolated from recipients harboring p53-deficient tumors displayed increased suppressive capacity compared to their WT counterparts, dovetailing with a similar observation in PTEN- and p53-null prostate tumors (Bezzi et al., 2018).
Pancreatic and lung tumors harboring mutations in KRAS also frequently acquire mutations in p53. While loss of p53 permits the proliferation of mutant-KRAS-expressing cells, which would otherwise undergo senescence, our data also demonstrate cooperation between KRAS and p53 mutations in allowing cancer cells to evade the immune response. Previous studies on pancreatic cancer have focused on the effects of mutant KRAS in pancreatic ductal epithelial cells (PDECs) and in combination with mutant p53 in PDAC models, where GM-CSF was a contributing factor for neutrophil recruitment to the tumor (Bayne et al., 2012, Pylayeva-Gupta et al., 2012). Interestingly, while neutrophils were enriched in orthotopically implanted KRASG12D PDECs, there was no change in Treg cell infiltration (Pylayeva-Gupta et al., 2012), supporting our observation that p53 plays a more important role in modulating Treg cells in cancer. The selection for suppressive Treg cells seems to depend predominantly on p53 loss rather than the coordinated overexpression of mutant KRAS, as demonstrated by the iKRAS system and the ID8 ovarian cancer model. Moreover, a recent study analyzing lung cancer patients treated with PD-L1 blockade reported that patients harboring both KRAS and TP53 mutations were resistant to immunotherapy through a mechanism that was independent of PD-L1 expression levels (Skoulidis et al., 2018). Hence, understanding how different oncogenic drivers interact to promote immune tolerance will be required to understand how best to apply immunomodulatory therapies in cancer.
STAR★Methods
Key Resources Table
| REAGENT or RESOURCE | SOURCE | IDENTIFIER |
|---|---|---|
| Antibodies | ||
| FITC anti-mouse KRLG1 | TONBO biosciences | Cat# 35-5893; RRID:AB_2621718 |
| FITC anti-mouse IFN gamma | TONBO Biosciences | Cat# 35-7311-U100; RRID:AB_2621724 |
| FITC anti-mouse CD4 | TONBO Biosciences | Cat# 35-0031-U100; RRID:AB_2621665 |
| FITC anti-mouse CD8a | BioLegend | Cat# 100706; RRID:AB_312745 |
| FITC anti-mouse FOXP3 | eBioscience | Cat# 11-5773-82; RRID:AB_465243 |
| PE anti-mouse CTLA-4 | eBioscience | Cat# 12-1522-82; RRID:AB_465243 |
| PE anti-mouse F4/80 | eBioscience | Cat# 12-4801-82; RRID:AB_465923 |
| PE anti-mouse CD4 | BioLegend | Cat# 100407; RRID:AB_312692 |
| PE anti-mouse CD8a | eBioscience | Cat# 12-0081-81; RRID:AB_465529 |
| PE anti-mouse FOXP3 | TONBO bioscience | Cat# 50-5773-U100; RRID:AB_2621797 |
| PE anti-mouse CD274 | eBioscience | Ca# 12-5982-81; RRID:AB_466088 |
| PE anti-human/mouse CD44 | eBioscience | Cat# 12-0441-81; RRID:AB_465663 |
| PerCP-Cy5.5 anti-mouse Ki67 | BioLegend | Cat# 652424; RRID:AB_2629531 |
| PerCP-Cy5.5 anti-mouse Ly6G | BioLegend | Cat# 127616; RRID:AB_1727563 |
| PeCy7 anti-mouse Granzyme B | eBioscience | Cat# 25-8898-80; RRID:AB_10853338 |
| PeCy7 anti-mouse GITR | BD Pharmigen | Cat# 558140; RRID:AB_647252 |
| PeCy7 anti-mouse CD11b | BD Pharmigen | Cat# 552850; RRID:AB_394491 |
| PeCy7 anti-mouse NKp46 | eBioscience | Cat# 25-3351-82; RRID:AB_394491 |
| PeCy7 anti-mouse CD8a | eBioscience | Cat# 25-0081-81; RRID:AB_469583 |
| PeCy7 anti-mouse CD4 | TONBO bioscience | Cat# 60-0041-U100; RRID:AB_469583 |
| PeCy7 anti-mouse CD80 | eBioscience | Cat# 25-0801-82; RRID:AB_2573370 |
| eFluor450 anti-mouse IL-2 | eBioscience | Cat# 48-7021-82; RRID:AB_1944462 |
| vFluor450 anti-mouse CD4 | TONBO bioscience | Cat# 75-0042-U100; RRID:AB_2621928 |
| eFluor450 anti-mouse CD8a | eBioscience | Cat# 48-0081-82; RRID:AB_1272198 |
| BV605 anti-mouse Ly6C | BioLegend | Cat# 128036; RRID:AB_2562353 |
| BV605 anti-mouse CXCR3 | BioLegend | Cat# 126523; RRID:AB_2561353 |
| BV650 anti-mouse CD8a | eBioscience | Cat# 100555; RRID:AB_2561353 |
| BV650 anti-mouse CD4 | BioLegend | Cat# 100555; RRID:AB_2562529 |
| BV650 anti-mouse CD11b | BioLegend | Cat# 101259; RRID:AB_2566568 |
| BV711 anti-mouse CD11b | BioLegend | Cat# 101242; RRID:AB_2563310 |
| BV711 anti-mouse CD4 | BioLegend | Cat# 100557; RRID:AB_2562607 |
| BV711 anti-mouse CD8a | BioLegend | Cat# 100759; RRID:AB_2563510 |
| BV785 anti-mouse MHCII I-A/I-E | BioLegend | Cat# 107646; RRID:AB_313317 |
| BV785 anti-mouse B220 | BioLegend | Cat# 103246; RRID:AB_2563256 |
| APC anti-mouse CD4 | eBioscience | Cat# 17-0042-82; RRID:AB_469323 |
| APC anti-mouse FOXP3 | eBioscience | Cat# 20-0191-U100; RRID:AB_2621561 |
| APC anti-mouse MHCI H-2Kd,H-2Dd | eBioscience | Cat# 17-5998-82; RRID:AB_2573250 |
| APC anti-mouse TNF alpha | eBioscience | Cat# 506308; RRID:AB_315429 |
| APC anti-mouse CD25 | eBioscience | Cat# 20-0251-U100; RRID:AB_2621567 |
| APC anti-mouse CD86 | eBioscience | Cat# 17-0862-81; RRID:AB_469418 |
| AlexaFluor647 anti-mouse CCR2 (CD192) | BioLegend | Cat# 150604; RRID:AB_2566140 |
| Vinculin mouse monoclonal | Santa Cruz Biotechnology | Cat# SC-73614; RRID:AB_1131294 |
| p53 mouse monoclonal antibody | Cell Signaling Technology | Cat# 2524; RRID:AB_331743 |
| InVivoPlus mouse IgG2a isotype control | BioXCell | Cat# BP0085; RRID:AB_1107771 |
| InVivo monoclonal anti mouse CSF1R | BioXCell | Cat#BE0213; RRID:AB_466565 |
| InVivo monoclonal anti-CD25 | BioXCell | Cat# BE0012; RRID:AB_1107619 |
| Anti-mouse CD28 Functional grade purified | eBioscience | Cat# 16-0281-86; RRID:AB_468923 |
| Anti-mouse CD3e Functional grade purified | eBioscience | Cat# 16-0031-86; RRID:AB_468849 |
| IRDye® 800CW Donkey anti-mouse | Li-Cor | Cat# 926-32212; RRID:AB_621847 |
| IRDye® 680LT Donkey anti-Rabbit | Li-Cor | Cat# 926-68023; RRID:AB_10706167 |
| Chemicals, Peptides, and Recombinant Proteins | ||
| Recombinant Murine Il-2 | Peprotech | Cat# 212-12 |
| Ovalbumin peptide 257-364 | Francis Crick Institute | N/A |
| Ovalbumin peptide 323-339 | Francis Crick Institute | N/A |
| Recombinant Murine M-CSF | Peprotech | Cat# 315-02 |
| Critical Commercial Assays | ||
| Mouse M-CSF ELISA Kit | RayBio ® | Cat# ELM-MCSF |
| Mouse G-CSF ELISA Kit | RayBio ® | Cat# ELM-GCSF |
| Mouse CXCL1/KC ELISA Kit | OriGene Techologies, Inc | Cat# EA100460 |
| Mouse Cytokine Array Panel A - Proteome Profiler | R&D systems ® | Cat# ARY006 |
| Mouse CCL2 Uncoated ELISA Kit | Invitrogen | Cat# 99-7391-22 |
| Mouse MIP1 alpha (CCL3) Uncoated ELISA Kit | Theromo Fisher Scientific | Cat# 88-56013-22 |
| Mouse LIX ELISA Kit | RayBio ® | Cat# ELM-LIX |
| ProcartaPlex Mouse Cytokine & Chemokine Panel 1 (26 plex) | Invitrogen eBioscience | EPX260-26088-901 |
| LEGEND MAX Mouse CCL11 ELISA Kit | BioLegend | Cat# 4438907 |
| High capacity cDNA reversts transcription kit | AppliedBiosystems | Cat# 4368814 |
| RNeasy ® Mini Kit | QIAGEN | Cat# 157029548 |
| RNase Free and DNase set | QIAGEN | Cat# 79254 |
| Deposited Data | ||
| PAAD - TCGA | TCGA | https://gdac.broadinstitute.org/; RRID:SCR_003193 |
| Experimental Models: Cell Lines | ||
| Phoenix-ECO | ATCC® | Cat# CRL-3214; RRID:CVCL_H717 |
| KC1 Pdx1-cre; LSL-KRasG12D | Beatson Institute for Cancer Research | N/A |
| KC3 Pdx1-cre; LSL-KRasG12D | Beatson Institute for Cancer Research | N/A |
| KC3 Pdx1-cre; LSL-KRasG12D | Beatson Institute for Cancer Research | N/A |
| KFC1 Pdx1-cre; LSL-KrasG12D; Trp53fl/+ | Beatson Institute for Cancer Research | N/A |
| KFC2 Pdx1-cre; LSL-KrasG12D; Trp53fl/+ | Beatson Institute for Cancer Research | N/A |
| KFC3 Pdx1-cre; LSL-KrasG12D; Trp53fl/+ | Beatson Institute for Cancer Research | N/A |
| ID8 | Walton et al., 2016 | N/A |
| ID8-p53KO | Walton et al., 2016 | N/A |
| iKRAS;p53f/+ | Ying et al., 2012 | N/A |
| Experimental Models: Organisms/Strains | ||
| C57Bl6/J mice females (6-10weeks) | Charles River Laboratories | CR: 632 |
| CD1 nude- Crl:CD1-Foxn1nu./nu. females (6-10weeks) | Charles River Laboratories | CR: 087 |
| FVB/NCrl females (6-10weeks) | Charles River Laboratories | CR: 207 |
| Oligonucleotides | ||
| Primers for qPCR T cell cytokines See Table 1 | This paper | N/A |
| Trp53 gRNA/Cas9 | Walton et al., 2016 | N/A |
| Recombinant DNA | ||
| pBABE-iRFP plasmid | Hock et al., 2014 | N/A |
| pCl-neo-mOVA | Yang et al., 2010 | Addgene Cat# 25099; RRID:Addgene_25099 |
| MIGR1 | Pear et al., 1998 | Addgene Cat# 27490; RRID:Addgene_27490 |
| Software and Algorithms | ||
| ImageJ | Schneider et al., 2012 | https://imagej.nih.gov/ij/; RRID:SCR_001935 |
| Image Studio v5 | Li-Cor | N/A |
| FlowJo version 9.0 | FlowJo | https://www.flowjo.com/solutions/flowjo/downloads; RRID:SCR_008520 |
| survival package version 2.41-3 | https://cran.r-project.org/web/packages/surviva/index.html | |
| R version 3.4.3 | RStudio | http://www.R-project.org; RRID:SCR_000432 |
| Prism Version 7 | GraphPad | https://www.graphpad.com/scientific-software/prism/; RRID:SCR_002798 |
Lead Contact and Materials Availability
Further information and requests for resources and reagents should be directed to and will be fulfilled by the Lead Contact Karen H Vousden (karen.vousden@crick.ac.uk). All unique/stable reagents generated in this study are available from the Lead Contact with a completed MTA.
Experimental Model and Subject Details
Mice
The mouse models of pancreatic ductal adenocarcinomas were generated using Pdx1-Cre; LSL-KrasG12D/+; Trp53+/+ and Pdx1-Cre; LSL-KrasG12D/+; Trp53fl/+ as previously published (Morton et al., 2010). The mouse model of non-small cell lung carcinomas was based on the tetracycline inducible EGFR-L858R [Tg(tet-O-EGFR∗L858R)56Hev] from the Mouse Repository of the National Cancer Institute. The R26tTA and Trp53fl/fl mice were obtained from the Jackson laboratory. Mice were crossed to generate Rosa26tTaLSL tet(O)EGFRL858R and Rosa26tTaLSL tet(O)EGFRL858R Trp53flox/flox mice and all backcrossed to C57Bl6/J background. Adenoviral Cre (Viral Vector Core, University of Iowa, USA) was delivered via intratracheal intubation (single dose, 2.5x107 virus particles in 50 μl). FVB (male and females) and CD1nu/nu (females) were purchased from Charles River, and OTI and OTII mice were purchased from Jax and maintained at the Beatson Institute for Cancer Research and the Francis Crick Institute animal facilities. All animals used ranged from 10-30 weeks of age and littermates of the same sex were randomly assigned to experimental groups.
Animal experiments were subject to ethical review by the Francis Crick Animal Welfare and Ethical Review Body and regulation by the UK Home Office project license P8AA77917 and P319AE968 or at the BICR reviewed and approved by the University of Glasgow and UK Home Office for the project license (70/8645). All mice were housed under conditions in line with the Home Office guidelines (UK). Mice were housed from 3-5 per cage and were kept in a 12-hour day/night cycle starting at 7:00 until 19:00. Food and water were available ad libitum and rooms were kept at 21°C at 55% humidity. All procedures were performed following the Animals (scientific procedures) Act 1986 and the EU Directive 2010.
Cell lines and transfection
Phoenix-ECO (ATCC® CRL-3214™) were purchased from the ATCC. PDAC cells from Pdx1-Cre; LSL-KrasG12D/+; Trp53+/+ and Pdx1-Cre; LSL-KrasG12D/+; Trp53fl/+ mice were derived as previously described (Tan et al., 2014). Cell lines used (KCs and KFCs) were tested for genetic background purity by the Charles River Genetic Testing Services. After a 384 SNP panel batch analysis (MB-160318AJ), cell lines derived from tumors were deemed mismatched (e.g., B6N 73%–78.9%, FVB 46.7%–59.8%, 129S4SvJae 60.3%–71.7%). ID8 isogenic ovarian cancer cells were previously described (Walton et al., 2016). iKRAS cell line was gifted by RA DePinho and were maintained in DMEM, 10% FBS and 2μg/ml of doxycycline (Ying et al., 2012). All other cell lines were maintained in DMEM, 10% FBS and penicillin-streptomycin and in 37°C, 5% CO2 humidified incubators.
Primary T cells and bone marrow were derived from C57Bl6/J mice (either male or female) held at the BICR or Francis Crick institute and aged between 10-30 weeks.
Mouse Cancer Orthotopic Models
The pancreatic orthotopic model protocol was described by Kim et al. (2009). Briefly, pancreatic cancer cells were surgically implanted into the pancreas of recipient mice (500,000 cells in 25μl of Matrigel, BD-Biosciences). For the ovarian ID8 cancer model, 5x106 cells were injected intraperitoneally (IP) in 6-8-week-old female C57Bl6/J mice (Charles River Laboratories, UK). The development of ascites and other symptoms were diagnosed as previously described (Walton et al., 2016).
Tumor Challenge and Rejection Models
PDAC derived cells expressing iRFP were subcutaneously injected into the left flank of FVB mice at 1x106 cells/mouse. Growth was monitored by in vivo imaging and mice were taken at humane endpoint as dictated by the UK Home Office and the animal license. Allograft growth in CD1nu/nu mice was performed by unilateral flank injections of 1x106 per mouse. Growth was measured by in vivo imaging and humane endpoints were respected. All in vivo antibodies were purchased from Bio-X-Cell. Anti-CSF1R (clone AFS98) was used at a concentration of 300μg/mouse and administered twice a week. Anti-CD25 (PC-61.5.3) was used three days prior to tumor challenge and used at 400μg/mouse. Isotype control used was IgG2a (C1.18.4) and 200μg/mouse was used as a control.
Method Details
T cell and CD11b+ cell purification, macrophage differentiation, and cell culture
CD8+ T cells and CD4+ T cells were isolated from spleens and peripheral lymph nodes, prepared into single cell suspensions and lysed for red blood cells (10x RBC lysis buffer, Biolegend). Negative isolation kits and positive isolation kits (CD11b+ cells) were purchased from StemCell Technologies and isolation was performed following manufacture’s procedures. T cells were activated and cultured as previously described (Jones et al., 2007) using plate-bound anti-CD3 and anti-CD28 antibodies.
Isolation of intratumoral CD11b+ cells was performed on tumors digested using the tumor preparation protocol (see below). CD11b+ cells were isolated from tumor single cell suspensions using positive isolation kits from StemCell Technologies, following the manufacturer’s protocol.
Macrophages were differentiated from bone marrow flushed using PBS, a 1mL syringe and a 25G needle. Bone marrow was collected, lysed for red blood cells (10x RBC lysis buffer, Biolegend), and plated on non-TC treated plates at 5x106 cells/10cm dish and 20ng/ml of M-CSF (Peprotech).
Cell culture of pancreatic ductal adenocarcinoma cells (PDACs) and ID8 cell lines were maintained in DMEM supplemented with 10% FBS and Pen/Strep.
Treg and CD11b suppression assays
CD4+CD25+ and CD4+CD25- T cells were isolated by performing CD4+ T cell negative isolation by STEMCELL technology kits and sorted by flow cytometry (FACS Aria Sorter) (CD4-FITC and CD25-APC). Briefly, ratios of 1:1 (Treg:Teffector) to 1:32 were generated in the presence of irradiated splenocytes and activated with 1μg/ml of αCD3 for 3 days (Collison and Vignali, 2011).
CD11b+ cells were isolated by positive selection from digested tumors (see above). T cells were stained with V450 dye and plate-bound activated with a-CD3 (5μg/ml) and a-CD28 (2μg/ml) for 24 hours. After 24 hours, T cells were co-cultured with isolated tumor-associated CD11b+ cells at a ratio of 1:4 in a 24 well plate for a further 2 days and proliferation was assessed using a the eBioscience live/dead fixable viability dye, APC-Cy7, and flow cytometry. Isolated CD11b+ intratumoral cells were plated 8 hours prior to co-culture at 0.5x106 cells per 24 well plate (Corning). Plate-bound activated T cells were plated 24 hours post-activation at 0.75x106 cells per 24 well plate.
Flow cytometry
Single cell suspensions were stained for surface markers in PBS for 20 minutes at 4°C. Intracellular proteins (i.e., cytokines, FOXP3, and Ki67) were assessed using the FOXP3/Transcription staining buffer set (eBioscience, San Diego, CA) and following manufacturer’s instructions. Cells were permeabilized for 30 minutes and stained for intracellular proteins for 1 hour at 4°C. All fluorochromes were purchased from Biolegened and eBioscienes. Ex vivo re-stimulation was performed using PMA (Sigma-Aldrich), ionomycin (Sigma-Aldrich), and Golgi Stop (BD Biosciences) for 4 hours as previously described (Kornete et al., 2012). For OTI and OTII peptide re-stimulation, peptides OVA257-264 and OVA323-339, were incubated with transgenic T cells at 10μg/ml with Golgi Stop (BD Biosciences) for 6 hours followed by surface staining and ICS. Dead cells were distinguished using the fixable viability dye efluor780® from eBioscience. Single cell suspensions were fixed and permeabilized using the FOXP3 Transcription staining buffer set. Samples were acquired on the BD LSRFortessa™ and on the BD FACSymphony™. Flow cytometry data was analyzed using FlowJo (TreeStar).
Extracellular Cytokine Measurements
ELISA kits were purchased from R&D systems for M-CSF, CXCL1, CCL11, and G-CSF. ELISAs for MCP1, CCL3 and CXCL5 were purchased from Life Technologies, Invitrogen. All ELISAs and cytokine arrays were performed on conditioned media (cells were plated at 1x106 cells/10cm dish) harvested after 24 hours. Cytokine arrays were purchased from R&D systems ® (Mouse cytokine panel array A) and performed on conditioned media from cells prepared as for ELISAs. Cytokines were detected following the manufacture’s procedures and using chemiluminescence (read at 450nm). Pixels from cytokine array data were analyzed using ImageJ software. The Luminex cytokine array used in this study was the Invitrogen eBioscience ProcartaPlex Mouse Cytokine & Chemokine Panel 1 (26 plex) with 4 additional cytokines
Immunoblotting
Cells were lysed using RIPA buffer supplemented the 1%SDS and phosphatase inhibitors (La Roche Ltd), denatured at 95°C, and resolved on NuPAGE polyacrylamide pre-cast gels (ThermoFischer Scientific). Transfer of gels onto nitrocellulose membranes was performed using the iBlot2 (Invitrogen). Cells were probed for p53 with monoclonal anti-mouse p53 antibody from Cell Signaling Technologies (clone 1C12). Vinculin (H10, Santa Cruz Biotechnologies) was detected as a loading control. Secondary antibodies were purchased from LiCOR IRDye 800CW and 700CW.
In Vivo Imaging
Mice were anesthetized with isoflurane and imaged using the Pearl Imager by LiCOR. iRFP fluorescence was excited using the 685nm laser and emission was detected in the 700nm channel (730nm). Fluorescence was analyzed using the Image Studio v5 from LiCOR.
Co-Culture Assays
Activated T cells and PDACS
Primary T cells were activated with plate-bound anti-CD3 (5μg/ml) and anti-CD28 (2μg/ml) for 24 hours. Activated T cells were then co-cultured with adherent PDAC cells in 24 well plates or 96 well plates. PDACs were plated at 20 000 cells/well with 1x106 T cells (24 well plate) or 10,000 PDAC cells/well with 200,000 T cells (96 well plate) and co-incubated for 2 days. T cells were re-stimulated with PMA, ionomycin and GolgiStop (BD Biosciences) for 4 hours prior to ICS. Intracellular cytokines probed by ICS and flow cytometry were Granzyme B, IFNγ and TNFα.
BMDMs and Transgenic T cells
0.3x106 BMDMs pulsed with 10μg/ml of ovalbumin (Sigma-Aldrich) for 1 hour, washed and naive OTI or OTII cells were added to the culture at 1x106 cells/well. T cells were kept in co-culture for 3-4 days followed by OVA257-264 and OVA323-339 re-stimulation at 10μg/ml in the presence of a Golgi blocker (GolgiStop, BD Bioscience), surface staining, ICS and acquired by flow cytometry.
OTI and PDAC-mOVA cell viability
Splenocytes from OT1 TCR transgenic mice were stimulated in vitro with 10μg/ml of SIINFEKL (OVA257-264) for 48 hours. Cells were spun down using Lympholyte M (Cedarlane) following the manufacturer’s instructions. Activated CD8+OT1 cells were co-cultured in a 24 well plate (Corning) at 0.5x106 cells to 200,000 PDAC-mOVA isogenic cells. Cells were stained with propidium iodide for cell viability and acquired on the BDLSRFortessa™.
Tissue collection, Immunohistochemistry (IHC) and scoring
Tissue was collected and fixed in 10% neutral buffered formalin (NBF). Samples were replaced with 70% ethanol after 48hours, embedded in paraffin blocks, and processed by standard histological techniques. Sections were cut at 5μM. IHC and H&E was performed as previously published (Myant et al., 2013). F480 antibody was purchased from eBioscience (rat anti-mouse F4/80 Cat. No 14-4801-82; RRID:AB_467558). Scoring of tumor sections for individual markers was performed by counting 30 fields using QuPath open source digital software (Bankhead et al., 2017) and set as an average per field.
Tumor Preparation and Serum Collection
Tumors
Tumors were carefully excised from the animals and kept in ice cold medium till processing. Tumors were minced into small (about 1mm) pieces and digested in digestion buffer containing: collagenase 0.012%, dispase, 0.1mg/ml DNase I, 1% FBS in Krebs Ringer Bicarbonate Buffer (KRB) for 45-60 min at 37°C with gentle oscillation. The digestion was stopped by the addition of at least 10 volume of ice cold DMEM supplemented with 10% FBS. The solution was filtered through a 100 μm cell strainer and the isolated cells were precipitated by centrifugation at 300 X g for 5 min, washed with PBS before further processing.
Serum
Serum was collected by cardiac puncture into EDTA coated tubes. Blood was spun in 1.5mL Eppendorf tubes at 2000xg for 15 minutes at 4°C. Serum was collected in upper phase and stored at −80°C.
RNA extraction and QPCR
Total RNA was extracted using RNeasy® columns (QIAGEN) from at least 3 technical replicates per sample according to manufacturer instructions. Genomic DNA was removed using on column DNA digestion (QIAGEN). cDNA was generated using the High-Capacity cDNA reverse transcription kit (Thermofisher) according to manufacturer’s instructions. Power up ™ SYBR® Green Master MIX (Applied Biosystem) was used to perform QPCR with the following primers:
Table 1
| Gene and accession number | Forward primer | Reverse primer |
|---|---|---|
| Il-6 | tcctaccccaatttccaatgctc | ttggatggtcttggtccttagcc |
| Tnf-α | CCCCAAAGGGATGAGAAGTT | CTCCTCCACTTGGTGGTTTG |
| IL-12b | CTGCTGCTCCACAAGAAGGA | ACGCCATTCCACATGTCACT |
| Il-1β | GCAACTGTTCCTGAACTCAACT | TCTTTTGGGGTCCGTCAACT |
| cyc | ATGGTCAACCCCACCGTGT | TTTCTGCTGTCTTTGGAACTTTGTC |
Gene expression values were calculated according to Pfaffl method (Pfaffl, 2001) and expressed as relative units compared to the control group
Scratch-Wound and Migration Assays
Scratch-wound Assay
BMDMs were differentiated with 10ng/ml M-CSF and re-plated onto Imagelock 96 well plates. Scratches were made using the Essenbio scratch making tool. Wound closure was monitored in real-time using IncuCyte™ Live-Cell Analysis System and analyzed using IncuCyte S3 software.
Chemoattraction assays
BMDMs at 5000 cells per chamber were plated in the upper chamber of an IncuCyte™ ClearView 96-well Cell Migration plate (Essen BioScience). Conditioned medium from different PDAC cell lines was placed in the bottom chamber. The Incucyte ZOOM® live-cell imaging system was used to measure cell migration.
Plasmids, stable expression and CRISPR/CAS9
Plasmids for iRFP (Hock et al., 2014) were transfected into Phoenix-ECO (ATCC® CRL-3214) using GeneJuice® Transfection reagents (Merk Milipore). PDAC cell lines were transduced with viral media and pBABE-iRFP selected for by puromycin (Sigma-Aldrich) at a concentration of 2.5μg/ml. Plasmid positive cells were cultured in selection media for 7 days. CRISPR/CAS9 methods were employed for genetic deletion of the Trp53 gene as previously described (Walton et al., 2016). Retroviral introduction of ovalbumin sequence for membrane bound ovalbumin (mOVA) was cloned out of the pCl-neo-mOVA plasmid (Addgene No 25099) (Yang et al., 2010) and into the MSCV-based MIGR1 (Addgene 27490) vector (Pear et al., 1998). Phoenix-EC (ATCC ® CRL-3214) were used for virus production and PDAC cells were virally transduced three consecutive days. mOVA expressing cells were selected by cell sorting for GFP expression.
Bioinformatics Analysis of TCGA datasets
Survival curves & gene expression: SEM normalized data was downloaded from the TCGA firehose website [ https://gdac.broadinstitute.org/]. Top (high group) and bottom (low group) quartiles pancreatic adenocarcinoma samples for MDSC-signature ranked expression were compared using the survival package version 2.41-3 (https://cran.r-project.org/web/packages/survival/index.html) in R version 3.4.3 (http://www.R-project.org) and the level of statistical significance determined by the log rank test. Expression data from PAAD patients with a mutation in TP53 was compared to those without a mutation using DESEQ2 (Love et al., 2014). Boxplots show the log2 expression values of selected genes grouped by their TP53 mutation status, with the adjusted p value determined by the Wald test.
Quantification and Statistical Analysis
Data are presented as mean ± SD for technical replicates, or mean ± SEM for biological replicates. Data was analyzed using the unpaired Student t test when comparing two conditions. One-way ANOVA with a Tukey’s multiple comparisons test was performed on comparisons of more than two conditions as well as in vivo growth studies. Two-way Anova was performed on the in vivo tumor growth studies with treatments and different p53 alterations. Statistical significance is indicated in all figures by the following annotations: ∗ p < 0.05; ∗∗p < 0.01;∗∗∗p < 0.005. GraphPad Prism 7 was used for statistical analysis and graph generation.
Data and Code Availability
This study did not generate any unique datasets or code
Acknowledgments
We would like to thank the histology team at the Beatson Institute for Cancer Research and the animal facilities at the Francis Crick and Beatson Institutes. J.B. was funded by a Canadian Institute of Health Research (CIHR) postdoctoral grant. J.B.W. was funded by the Marsh Rivkin Center for Ovarian Cancer. S.H. and E.G. were funded by a European Research Council (ERC) THESEUS grant. We would like to acknowledge and thank the Pear lab and Castro lab for donating their plasmids to Addgene (Pear et al., 1998, Yang et al., 2010). This work was funded by Cancer Research UK grants C596/A10419 and C596/A26855, and supported by the Francis Crick Institute, which receives its core funding from Cancer Research UK (FC001557), the UK Medical Research Council (FC001557), and the Wellcome Trust (FC001557), and the CRUK Beatson Institute, which receives its core funding from Cancer Research UK grant C596/A17196. C.S. is Royal Society Napier Research Professor. This work was supported by the Francis Crick Institute, which receives its core funding from Cancer Research UK (FC001169 and FC001202), the UK Medical Research Council (FC001169 and FC001202), and the Wellcome Trust (FC001169 and FC001202). C.S. is funded by Cancer Research UK (TRACERx, PEACE, and CRUK Cancer Immunotherapy Catalyst Network), the CRUK Lung Cancer Centre of Excellence, the Rosetrees Trust, NovoNordisk Foundation (ID16584), and the Breast Cancer Research Foundation (BCRF). This research is supported by a Stand Up To Cancer‐LUNGevity-American Lung Association Lung Cancer Interception Dream Team translational research grant (SU2C-AACR-DT23-17). Stand Up To Cancer is a program of the Entertainment Industry Foundation. Research grants are administered by the American Association for Cancer Research, the Scientific Partner of Stand Up To Cancer. C.S. receives funding from the ERC under the European Union’s Seventh Framework Programme (FP7/2007-2013) consolidator grant (FP7-THESEUS-617844); European Commission ITN (FP7-PloidyNet 607722); an ERC advanced grant (PROTEUS) from the ERC under the European Union’s Horizon 2020 research and innovation program (grant agreement 835297); and Chromavision from the European Union’s Horizon 2020 research and innovation program (grant agreement 665233).
Author Contributions
The study was conceived and designed by J.B., F.Z., S.H., E.G., M.H., K.B., and K.H.V. Investigations were conducted by J.B., F.Z., M.H., S.P., A.H., S.H., J.B.W., S.M., M.Y., and J.P.M. Bioinformatics analysis was carried out by P.C. The manuscript was written by J.B., F.Z., and K.H.V., and all authors contributed to the review of the paper.
Declaration of Interests
K.H.V. is on the board of directors and shareholder of Bristol Myers Squibb, a shareholder of GRAIL, and on the science advisory board of PMV Pharma, RAZE Therapeutics, and Ludwig Cancer. She is a co-founder and consultant of Faeth Therapeutics, funded by Khosla Ventures. She has been in receipt of research funding from Astex Pharmaceuticals and AstraZeneca and contributed to CRUK Cancer Research Technology filing of patent application WO/2017/144877. C.S. receives grant support from Pfizer, AstraZeneca, BMS, Roche-Ventana, and Boehringer-Ingelheim; has consulted for Pfizer, Novartis, GlaxoSmithKline, MSD, BMS, Celgene, AstraZeneca, Illumina, Genentech, Roche-Ventana, GRAIL, Medicxi, and the Sarah Cannon Research Institute; is an advisor for Dynamo Therapeutics; is a shareholder of Apogen Biotechnologies, Epic Bioscience, and GRAIL; and has stock options in and is co-founder of Achilles Therapeutics. I.A.M. is on the advisory boards for Clovis Oncology, Tesaro, AstraZeneca, Roche, and Carrick Therapeutics and is in receipt of research funding from AstraZeneca.
Published: January 14, 2020
Footnotes
Supplemental Information can be found online at https://doi.org/10.1016/j.celrep.2019.12.028.
Supplemental Information
References
- Ancrile B.B., O’Hayer K.M., Counter C.M. Oncogenic ras-induced expression of cytokines: a new target of anti-cancer therapeutics. Mol. Interv. 2008;8:22–27. doi: 10.1124/mi.8.1.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arce Vargas F., Furness A.J.S., Solomon I., Joshi K., Mekkaoui L., Lesko M.H., Miranda Rota E., Dahan R., Georgiou A., Sledzinska A., Melanoma TRACERx Consortium. Renal TRACERx Consortium. Lung TRACERx Consortium Fc-optimized anti-CD25 depletes tumor-infiltrating regulatory T cells and synergizes with PD-1 blockade to eradicate established tumors. Immunity. 2017;46:577–586. doi: 10.1016/j.immuni.2017.03.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Arpaia N., Green J.A., Moltedo B., Arvey A., Hemmers S., Yuan S., Treuting P.M., Rudensky A.Y. A distinct function of regulatory T cells in tissue protection. Cell. 2015;162:1078–1089. doi: 10.1016/j.cell.2015.08.021. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Athie-Morales V., Smits H.H., Cantrell D.A., Hilkens C.M. Sustained IL-12 signaling is required for Th1 development. J. Immunol. 2004;172:61–69. doi: 10.4049/jimmunol.172.1.61. [DOI] [PubMed] [Google Scholar]
- Bankhead P., Loughrey M.B., Fernández J.A., Dombrowski Y., McArt D.G., Dunne P.D., McQuaid S., Gray R.T., Murray L.J., Coleman H.G. QuPath: open source software for digital pathology image analysis. Sci. Rep. 2017;7:16878. doi: 10.1038/s41598-017-17204-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bartocci A., Mastrogiannis D.S., Migliorati G., Stockert R.J., Wolkoff A.W., Stanley E.R. Macrophages specifically regulate the concentration of their own growth factor in the circulation. Proc. Natl. Acad. Sci. USA. 1987;84:6179–6183. doi: 10.1073/pnas.84.17.6179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bayne L.J., Beatty G.L., Jhala N., Clark C.E., Rhim A.D., Stanger B.Z., Vonderheide R.H. Tumor-derived granulocyte-macrophage colony-stimulating factor regulates myeloid inflammation and T cell immunity in pancreatic cancer. Cancer Cell. 2012;21:822–835. doi: 10.1016/j.ccr.2012.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Beck A.H., Espinosa I., Edris B., Li R., Montgomery K., Zhu S., Varma S., Marinelli R.J., van de Rijn M., West R.B. The macrophage colony-stimulating factor 1 response signature in breast carcinoma. Clin. Cancer Res. 2009;15:778–787. doi: 10.1158/1078-0432.CCR-08-1283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bezzi M., Seitzer N., Ishikawa T., Reschke M., Chen M., Wang G., Mitchell C., Ng C., Katon J., Lunardi A. Diverse genetic-driven immune landscapes dictate tumor progression through distinct mechanisms. Nat. Med. 2018;24:165–175. doi: 10.1038/nm.4463. [DOI] [PubMed] [Google Scholar]
- Candido J.B., Morton J.P., Bailey P., Campbell A.D., Karim S.A., Jamieson T., Lapienyte L., Gopinathan A., Clark W., McGhee E.J. CSF1R+ macrophages sustain pancreatic tumor growth through T Cell suppression and maintenance of key gene programs that define the squamous subtype. Cell Rep. 2018;23:1448–1460. doi: 10.1016/j.celrep.2018.03.131. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cassetta L., Pollard J.W. Targeting macrophages: therapeutic approaches in cancer. Nat. Rev. Drug Discov. 2018;17:887–904. doi: 10.1038/nrd.2018.169. [DOI] [PubMed] [Google Scholar]
- Cerami E., Gao J., Dogrusoz U., Gross B.E., Sumer S.O., Aksoy B.A., Jacobsen A., Byrne C.J., Heuer M.L., Larsson E. The cBio cancer genomics portal: an open platform for exploring multidimensional cancer genomics data. Cancer Discov. 2012;2:401–404. doi: 10.1158/2159-8290.CD-12-0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chang C.H., Qiu J., O’Sullivan D., Buck M.D., Noguchi T., Curtis J.D., Chen Q., Gindin M., Gubin M.M., van der Windt G.J. Metabolic competition in the tumor microenvironment is a driver of cancer progression. Cell. 2015;162:1229–1241. doi: 10.1016/j.cell.2015.08.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cheng G., Yuan X., Tsai M.S., Podack E.R., Yu A., Malek T.R. IL-2 receptor signaling is essential for the development of Klrg1+ terminally differentiated T regulatory cells. J. Immunol. 2012;189:1780–1791. doi: 10.4049/jimmunol.1103768. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Christopoulos P., Pfeifer D., Bartholomé K., Follo M., Timmer J., Fisch P., Veelken H. Definition and characterization of the systemic T-cell dysregulation in untreated indolent B-cell lymphoma and very early CLL. Blood. 2011;117:3836–3846. doi: 10.1182/blood-2010-07-299321. [DOI] [PubMed] [Google Scholar]
- Coelho M.A., de Carne Trecesson S., Rana S., Zecchin D., Moore C., Molina-Arcas M., East P., Spencer-Dene B., Nye E., Barnouin K. Oncogenic RAS signaling promotes tumor immunoresistance by stabilizing PD-L1 mRNA. Immunity. 2017;47:1083–1099.e1086. doi: 10.1016/j.immuni.2017.11.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Collison L.W., Vignali D.A. In vitro Treg suppression assays. Methods Mol. Biol. 2011;707:21–37. doi: 10.1007/978-1-61737-979-6_2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cooks T., Pateras I.S., Jenkins L.M., Patel K.M., Robles A.I., Morris J., Forshew T., Appella E., Gorgoulis V.G., Harris C.C. Mutant p53 cancers reprogram macrophages to tumor supporting macrophages via exosomal miR-1246. Nat. Commun. 2018;9:771. doi: 10.1038/s41467-018-03224-w. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dodge I.L., Carr M.W., Cernadas M., Brenner M.B. IL-6 production by pulmonary dendritic cells impedes Th1 immune responses. J. Immunol. 2003;170:4457–4464. doi: 10.4049/jimmunol.170.9.4457. [DOI] [PubMed] [Google Scholar]
- Dunn G.P., Bruce A.T., Sheehan K.C., Shankaran V., Uppaluri R., Bui J.D., Diamond M.S., Koebel C.M., Arthur C., White J.M., Schreiber R.D. A critical function for type I interferons in cancer immunoediting. Nat. Immunol. 2005;6:722–729. doi: 10.1038/ni1213. [DOI] [PubMed] [Google Scholar]
- Fischer K., Hoffmann P., Voelkl S., Meidenbauer N., Ammer J., Edinger M., Gottfried E., Schwarz S., Rothe G., Hoves S. Inhibitory effect of tumor cell-derived lactic acid on human T cells. Blood. 2007;109:3812–3819. doi: 10.1182/blood-2006-07-035972. [DOI] [PubMed] [Google Scholar]
- George S., Miao D., Demetri G.D., Adeegbe D., Rodig S.J., Shukla S., Lipschitz M., Amin-Mansour A., Raut C.P., Carter S.L. Loss of PTEN is associated with resistance to anti-PD-1 checkpoint blockade therapy in metastatic uterine leiomyosarcoma. Immunity. 2017;46:197–204. doi: 10.1016/j.immuni.2017.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griesmann H., Drexel C., Milosevic N., Sipos B., Rosendahl J., Gress T.M., Michl P. Pharmacological macrophage inhibition decreases metastasis formation in a genetic model of pancreatic cancer. Gut. 2017;66:1278–1285. doi: 10.1136/gutjnl-2015-310049. [DOI] [PubMed] [Google Scholar]
- Guo G., Marrero L., Rodriguez P., Del Valle L., Ochoa A., Cui Y. Trp53 inactivation in the tumor microenvironment promotes tumor progression by expanding the immunosuppressive lymphoid-like stromal network. Cancer Res. 2013;73:1668–1675. doi: 10.1158/0008-5472.CAN-12-3810. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo G., Yu M., Xiao W., Celis E., Cui Y. Local activation of p53 in the tumor microenvironment overcomes immune suppression and enhances antitumor immunity. Cancer Res. 2017;77:2292–2305. doi: 10.1158/0008-5472.CAN-16-2832. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hock A.K., Lee P., Maddocks O.D., Mason S.M., Blyth K., Vousden K.H. iRFP is a sensitive marker for cell number and tumor growth in high-throughput systems. Cell Cycle. 2014;13:220–226. doi: 10.4161/cc.26985. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hollstein M., Sidransky D., Vogelstein B., Harris C.C. p53 mutations in human cancers. Science. 1991;253:49–53. doi: 10.1126/science.1905840. [DOI] [PubMed] [Google Scholar]
- Iannello A., Thompson T.W., Ardolino M., Lowe S.W., Raulet D.H. p53-dependent chemokine production by senescent tumor cells supports NKG2D-dependent tumor elimination by natural killer cells. J. Exp. Med. 2013;210:2057–2069. doi: 10.1084/jem.20130783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jiang Z., Liu Z., Li M., Chen C., Wang X. Immunogenomics analysis reveals that TP53 mutations inhibit tumor immunity in gastric cancer. Transl. Oncol. 2018;11:1171–1187. doi: 10.1016/j.tranon.2018.07.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Jones R.G., Bui T., White C., Madesh M., Krawczyk C.M., Lindsten T., Hawkins B.J., Kubek S., Frauwirth K.A., Wang Y.L. The proapoptotic factors Bax and Bak regulate T cell proliferation through control of endoplasmic reticulum Ca(2+) homeostasis. Immunity. 2007;27:268–280. doi: 10.1016/j.immuni.2007.05.023. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kawashima H., Takatori H., Suzuki K., Iwata A., Yokota M., Suto A., Minamino T., Hirose K., Nakajima H. Tumor suppressor p53 inhibits systemic autoimmune diseases by inducing regulatory T cells. J. Immunol. 2013;191:3614–3623. doi: 10.4049/jimmunol.1300509. [DOI] [PubMed] [Google Scholar]
- Kim M.P., Evans D.B., Wang H., Abbruzzese J.L., Fleming J.B., Gallick G.E. Generation of orthotopic and heterotopic human pancreatic cancer xenografts in immunodeficient mice. Nat. Protoc. 2009;4:1670–1680. doi: 10.1038/nprot.2009.171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kornete M., Sgouroudis E., Piccirillo C.A. ICOS-dependent homeostasis and function of Foxp3+ regulatory T cells in islets of nonobese diabetic mice. J. Immunol. 2012;188:1064–1074. doi: 10.4049/jimmunol.1101303. [DOI] [PubMed] [Google Scholar]
- Kortlever R.M., Sodir N.M., Wilson C.H., Burkhart D.L., Pellegrinet L., Brown Swigart L., Littlewood T.D., Evan G.I. Myc cooperates with Ras by programming inflammation and immune suppression. Cell. 2017;171:1301–1315.e1314. doi: 10.1016/j.cell.2017.11.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Love M.I., Huber W., Anders S. Moderated estimation of fold change and dispersion for RNA-seq data with DESeq2. Genome Biol. 2014;15:550. doi: 10.1186/s13059-014-0550-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lowe J.M., Menendez D., Bushel P.R., Shatz M., Kirk E.L., Troester M.A., Garantziotis S., Fessler M.B., Resnick M.A. p53 and NF-κB coregulate proinflammatory gene responses in human macrophages. Cancer Res. 2014;74:2182–2192. doi: 10.1158/0008-5472.CAN-13-1070. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lujambio A., Akkari L., Simon J., Grace D., Tschaharganeh D.F., Bolden J.E., Zhao Z., Thapar V., Joyce J.A., Krizhanovsky V., Lowe S.W. Non-cell-autonomous tumor suppression by p53. Cell. 2013;153:449–460. doi: 10.1016/j.cell.2013.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Martinelli R., Sabroe I., LaRosa G., Williams T.J., Pease J.E. The CC chemokine eotaxin (CCL11) is a partial agonist of CC chemokine receptor 2b. J. Biol. Chem. 2001;276:42957–42964. doi: 10.1074/jbc.M103933200. [DOI] [PubMed] [Google Scholar]
- McGranahan N., Rosenthal R., Hiley C.T., Rowan A.J., Watkins T.B.K., Wilson G.A., Birkbak N.J., Veeriah S., Van Loo P., Herrero J. Allele-specific HLA loss and immune escape in lung cancer evolution. Cell. 2017;171:1259–1271.e1211. doi: 10.1016/j.cell.2017.10.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Morton J.P., Timpson P., Karim S.A., Ridgway R.A., Athineos D., Doyle B., Jamieson N.B., Oien K.A., Lowy A.M., Brunton V.G. Mutant p53 drives metastasis and overcomes growth arrest/senescence in pancreatic cancer. Proc. Natl. Acad. Sci. USA. 2010;107:246–251. doi: 10.1073/pnas.0908428107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myant K.B., Cammareri P., McGhee E.J., Ridgway R.A., Huels D.J., Cordero J.B., Schwitalla S., Kalna G., Ogg E.L., Athineos D. ROS production and NF-κB activation triggered by RAC1 facilitate WNT-driven intestinal stem cell proliferation and colorectal cancer initiation. Cell Stem Cell. 2013;12:761–773. doi: 10.1016/j.stem.2013.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Noy R., Pollard J.W. Tumor-associated macrophages: from mechanisms to therapy. Immunity. 2014;41:49–61. doi: 10.1016/j.immuni.2014.06.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Okuda Y., Okuda M., Bernard C.C. Regulatory role of p53 in experimental autoimmune encephalomyelitis. J. Neuroimmunol. 2003;135:29–37. doi: 10.1016/s0165-5728(02)00428-9. [DOI] [PubMed] [Google Scholar]
- Onizuka S., Tawara I., Shimizu J., Sakaguchi S., Fujita T., Nakayama E. Tumor rejection by in vivo administration of anti-CD25 (interleukin-2 receptor alpha) monoclonal antibody. Cancer Res. 1999;59:3128–3133. [PubMed] [Google Scholar]
- Park J.S., Lim M.A., Cho M.L., Ryu J.G., Moon Y.M., Jhun J.Y., Byun J.K., Kim E.K., Hwang S.Y., Ju J.H. p53 controls autoimmune arthritis via STAT-mediated regulation of the Th17 cell/Treg cell balance in mice. Arthritis Rheum. 2013;65:949–959. doi: 10.1002/art.37841. [DOI] [PubMed] [Google Scholar]
- Pear W.S., Miller J.P., Xu L., Pui J.C., Soffer B., Quackenbush R.C., Pendergast A.M., Bronson R., Aster J.C., Scott M.L., Baltimore D. Efficient and rapid induction of a chronic myelogenous leukemia-like myeloproliferative disease in mice receiving P210 bcr/abl-transduced bone marrow. Blood. 1998;92:3780–3792. [PubMed] [Google Scholar]
- Peng W., Chen J.Q., Liu C., Malu S., Creasy C., Tetzlaff M.T., Xu C., McKenzie J.A., Zhang C., Liang X. Loss of PTEN promotes resistance to T cell-mediated immunotherapy. Cancer Discov. 2016;6:202–216. doi: 10.1158/2159-8290.CD-15-0283. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfaffl M.W. A new mathematical model for relative quantification in real-time RT-PCR. Nucleic Acids Res. 2001;29:e45. doi: 10.1093/nar/29.9.e45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Prenen H., Mazzone M. Tumor-associated macrophages: a short compendium. Cell. Mol. Life Sci. 2019;76:1447–1458. doi: 10.1007/s00018-018-2997-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pylayeva-Gupta Y., Lee K.E., Hajdu C.H., Miller G., Bar-Sagi D. Oncogenic Kras-induced GM-CSF production promotes the development of pancreatic neoplasia. Cancer Cell. 2012;21:836–847. doi: 10.1016/j.ccr.2012.04.024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Qian B.Z., Pollard J.W. Macrophage diversity enhances tumor progression and metastasis. Cell. 2010;141:39–51. doi: 10.1016/j.cell.2010.03.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ribas A., Wolchok J.D. Cancer immunotherapy using checkpoint blockade. Science. 2018;359:1350–1355. doi: 10.1126/science.aar4060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sakaguchi S., Yamaguchi T., Nomura T., Ono M. Regulatory T cells and immune tolerance. Cell. 2008;133:775–787. doi: 10.1016/j.cell.2008.05.009. [DOI] [PubMed] [Google Scholar]
- Schneider C.A., Rasband W.S., Eliceiri K.W. NIH Image to ImageJ: 25 years of image analysis. Nature Methods. 2012;9:671–675. doi: 10.1038/nmeth.2089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Setiady Y.Y., Coccia J.A., Park P.U. In vivo depletion of CD4+FOXP3+ Treg cells by the PC61 anti-CD25 monoclonal antibody is mediated by FcgammaRIII+ phagocytes. Eur. J. Immunol. 2010;40:780–786. doi: 10.1002/eji.200939613. [DOI] [PubMed] [Google Scholar]
- Shcherbakova D.M., Verkhusha V.V. Near-infrared fluorescent proteins for multicolor in vivo imaging. Nat. Methods. 2013;10:751–754. doi: 10.1038/nmeth.2521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shimizu J., Yamazaki S., Sakaguchi S. Induction of tumor immunity by removing CD25+CD4+ T cells: a common basis between tumor immunity and autoimmunity. J. Immunol. 1999;163:5211–5218. [PubMed] [Google Scholar]
- Siemers N.O., Holloway J.L., Chang H., Chasalow S.D., Ross-MacDonald P.B., Voliva C.F., Szustakowski J.D. Genome-wide association analysis identifies genetic correlates of immune infiltrates in solid tumors. PLoS ONE. 2017;12:e0179726. doi: 10.1371/journal.pone.0179726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Skoulidis F., Goldberg M.E., Greenawalt D.M., Hellmann M.D., Awad M.M., Gainor J.F., Schrock A.B., Hartmaier R.J., Trabucco S.E., Gay L. STK11/LKB1 mutations and PD-1 inhibitor resistance in KRAS-mutant lung adenocarcinoma. Cancer Discov. 2018;8:822–835. doi: 10.1158/2159-8290.CD-18-0099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Spranger S., Bao R., Gajewski T.F. Melanoma-intrinsic β-catenin signalling prevents anti-tumour immunity. Nature. 2015;523:231–235. doi: 10.1038/nature14404. [DOI] [PubMed] [Google Scholar]
- Tan E.H., Morton J.P., Timpson P., Tucci P., Melino G., Flores E.R., Sansom O.J., Vousden K.H., Muller P.A. Functions of TAp63 and p53 in restraining the development of metastatic cancer. Oncogene. 2014;33:3325–3333. doi: 10.1038/onc.2013.287. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tanaka A., Sakaguchi S. Regulatory T cells in cancer immunotherapy. Cell Res. 2017;27:109–118. doi: 10.1038/cr.2016.151. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walton J., Blagih J., Ennis D., Leung E., Dowson S., Farquharson M., Tookman L.A., Orange C., Athineos D., Mason S. CRISPR/Cas9-mediated Trp53 and Brca2 knockout to generate improved murine models of ovarian high-grade serous carcinoma. Cancer Res. 2016;76:6118–6129. doi: 10.1158/0008-5472.CAN-16-1272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang B., Niu D., Lai L., Ren E.C. p53 increases MHC class I expression by upregulating the endoplasmic reticulum aminopeptidase ERAP1. Nat. Commun. 2013;4:2359. doi: 10.1038/ncomms3359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Watanabe M., Moon K.D., Vacchio M.S., Hathcock K.S., Hodes R.J. Downmodulation of tumor suppressor p53 by T cell receptor signaling is critical for antigen-specific CD4(+) T cell responses. Immunity. 2014;40:681–691. doi: 10.1016/j.immuni.2014.04.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wellenstein M.D., Coffelt S.B., Duits D.E.M., van Miltenburg M.H., Slagter M., de Rink I., Henneman L., Kas S.M., Prekovic S., Hau C.S. Loss of p53 triggers WNT-dependent systemic inflammation to drive breast cancer metastasis. Nature. 2019;572:538–542. doi: 10.1038/s41586-019-1450-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Worzfeld T., Pogge von Strandmann E., Huber M., Adhikary T., Wagner U., Reinartz S., Müller R. The unique molecular and cellular microenvironment of ovarian cancer. Front. Oncol. 2017;7:24. doi: 10.3389/fonc.2017.00024. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu W., Dietze K.K., Gibbert K., Lang K.S., Trilling M., Yan H., Wu J., Yang D., Lu M., Roggendorf M. TLR ligand induced IL-6 counter-regulates the anti-viral CD8(+) T cell response during an acute retrovirus infection. Sci. Rep. 2015;5:10501. doi: 10.1038/srep10501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xue W., Zender L., Miething C., Dickins R.A., Hernando E., Krizhanovsky V., Cordon-Cardo C., Lowe S.W. Senescence and tumour clearance is triggered by p53 restoration in murine liver carcinomas. Nature. 2007;445:656–660. doi: 10.1038/nature05529. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yang J., Sanderson N.S., Wawrowsky K., Puntel M., Castro M.G., Lowenstein P.R. Kupfer-type immunological synapse characteristics do not predict anti-brain tumor cytolytic T-cell function in vivo. Proc. Natl. Acad. Sci. USA. 2010;107:4716–4721. doi: 10.1073/pnas.0911587107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ying H., Kimmelman A.C., Lyssiotis C.A., Hua S., Chu G.C., Fletcher-Sananikone E., Locasale J.W., Son J., Zhang H., Coloff J.L. Oncogenic Kras maintains pancreatic tumors through regulation of anabolic glucose metabolism. Cell. 2012;149:656–670. doi: 10.1016/j.cell.2012.01.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yoon K.W., Byun S., Kwon E., Hwang S.Y., Chu K., Hiraki M., Jo S.H., Weins A., Hakroush S., Cebulla A. Control of signaling-mediated clearance of apoptotic cells by the tumor suppressor p53. Science. 2015;349:1261669. doi: 10.1126/science.1261669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang S., Zheng M., Kibe R., Huang Y., Marrero L., Warren S., Zieske A.W., Iwakuma T., Kolls J.K., Cui Y. Trp53 negatively regulates autoimmunity via the STAT3-Th17 axis. FASEB J. 2011;25:2387–2398. doi: 10.1096/fj.10-175299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zheng S.J., Lamhamedi-Cherradi S.E., Wang P., Xu L., Chen Y.H. Tumor suppressor p53 inhibits autoimmune inflammation and macrophage function. Diabetes. 2005;54:1423–1428. doi: 10.2337/diabetes.54.5.1423. [DOI] [PubMed] [Google Scholar]
- Zhu K., Wang J., Zhu J., Jiang J., Shou J., Chen X. p53 induces TAP1 and enhances the transport of MHC class I peptides. Oncogene. 1999;18:7740–7747. doi: 10.1038/sj.onc.1203235. [DOI] [PubMed] [Google Scholar]
- Zhu Y., Knolhoff B.L., Meyer M.A., Nywening T.M., West B.L., Luo J., Wang-Gillam A., Goedegebuure S.P., Linehan D.C., DeNardo D.G. CSF1/CSF1R blockade reprograms tumor-infiltrating macrophages and improves response to T-cell checkpoint immunotherapy in pancreatic cancer models. Cancer Res. 2014;74:5057–5069. doi: 10.1158/0008-5472.CAN-13-3723. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
This study did not generate any unique datasets or code