Abstract
Background
Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) has high accuracy and a low complication rate; therefore, it has been widely used as a useful tool for diagnosis of and to determine treatment strategies for pancreatic tumors. Recently, reports of the recurrence of needle tract seeding after EUS-FNA are emerging.
Case presentation
An 83-year-old woman was referred to our hospital to undergo further examination of her pancreatic tumor. Multidetector computed tomography (MDCT) revealed a 25-mm-diameter mass in the pancreatic body. She underwent EUS-FNA (transgastric, 22-G needle, 2 passes) and was subsequently diagnosed with adenocarcinoma. Distal pancreatosplenectomy followed by adjuvant chemotherapy with S-1 for 6 months was performed. The level of carbohydrate antigen 19–9 gradually increased 22 months after surgery, and MDCT, which was performed 3 months later, revealed a 23-mm low-density mass in the stomach and paragastric lymph node swelling. Gastroendoscopy revealed a submucosal tumor, and endoscopic ultrasound revealed a hypoechoic mass in the submucosa of the gastric wall. Partial gastrectomy with lymph node resection was performed. The pathological findings showed adenocarcinoma extending from the subserosa to the submucosa and lymph node metastasis, consistent with a tumor recurrence from the resected pancreatic tumor. She received adjuvant chemotherapy with S-1; recurrence was not observed for 5 months, at the time of this writing.
Conclusion
It is important to pay careful attention to the development of needle tract seeding in patients with pancreatic cancer diagnosed by EUS-FNA. This is the first case of needle tract seeding with lymph node metastasis, highlighting the need for caution and providing novel insight in the postoperative follow-up of patients with pancreatic body/tail cancer.
Keywords: Pancreatic cancer, Endoscopic ultrasound-guided fine needle aspiration, Needle tract seeding, Recurrence, Lymph node metastasis
Background
Endoscopic ultrasound-guided fine needle aspiration (EUS-FNA) is a minimally invasive sampling technique. Because of its high accuracy [1] and low complication rate [2], EUS-FNA is widely used as a useful tool to diagnose and determine the treatment strategies for pancreatic tumors. However, clinical concerns about peritoneal dissemination or needle tract seeding associated with puncture exist. Although several reports have indicated that preoperative EUS-FNA for pancreatic cancer does not affect postoperative survival or peritoneal recurrence [3, 4], emerging cases of needle tract seeding after EUS-FNA have been recently highlighted. Herein, we report a case of tumor seeding of pancreatic cancer after distal pancreatosplenectomy following EUS-FNA, and we review the literature related to needle tract seeding after EUS-FNA.
Case presentation
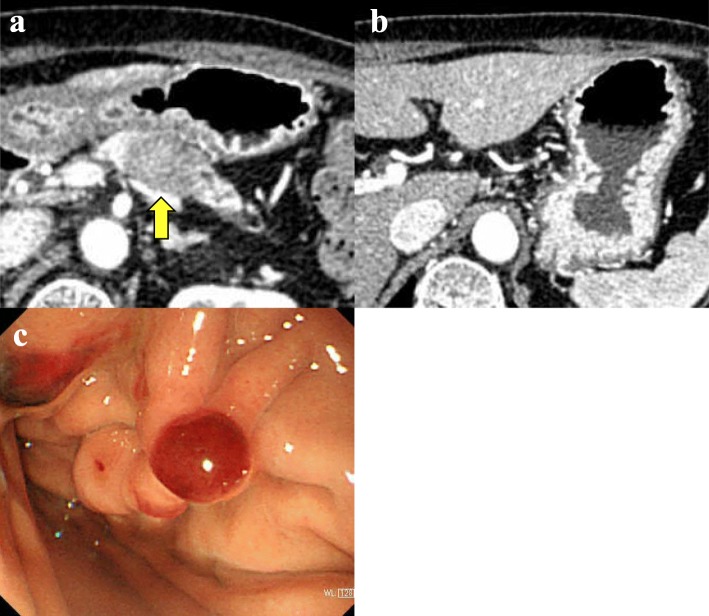
An 83-year-old woman with a pancreatic mass identified on abdominal ultrasonography during a medical examination was referred to our hospital. Multidetector computed tomography (MDCT) revealed a 25-mm-diameter low-density mass in the body of the pancreas with dilatation of the main pancreatic duct (Fig. 1a). The carbohydrate antigen 19–9 (CA19–9) level was significantly higher (286 U/mL) than the normal range. To examine the pathological diagnosis, EUS-FNA of the pancreatic tumor was performed using a 22-G needle (SonoTip® 22G, Medicos-Hirata, Tokyo, Japan) passed twice through the gastric wall. During the procedure, early complications were not observed. Subsequently, the patient was diagnosed with adenocarcinoma. Considering that metastatic disease was not observed and her condition was good for her age, she underwent distal pancreatosplenectomy with lymphadenectomy (i.e., anterior radical antegrade modular pancreatosplenectomy). Based on the intraoperative findings, peritoneal dissemination was not observed, and the peritoneal washing cytology was negative for carcinoma cells (CY0). The pancreatic tumor did not invade the gastric wall. The pathological findings resulted in a diagnosis of invasive ductal carcinoma (tub2, Pbt, pTS2 [32 × 25 × 20 mm], infiltrative type, int, INFb, ly3, v2, ne1, pT3, pCH0, pDU0, pS1, pRP1, pPV1sp, pA0, pPL1, pOO0, pN1b [10/20] [#11], pM0, pStage IIB) (according to the 7th edition of the Japanese Pancreas Society classification) with R0 resection (pT2N2M0 pStage III, according to the 8th edition of tumor-node-metastasis (TNM) classification by the American Joint Committee on Cancer/Union for International Cancer Control). According to the pathological examination, there was an invasion on the serosal side of the anterior pancreatic tissue, but not on the stomach. She received adjuvant chemotherapy containing S-1 for 6 months.
Fig. 1.
Images prior to the initial operation for pancreatic cancer. a Computed tomography revealed a low-density mass in the body of the pancreas (arrow). b Lymph node swelling around the stomach before surgery was not observed. c The puncture site of fine needle aspiration
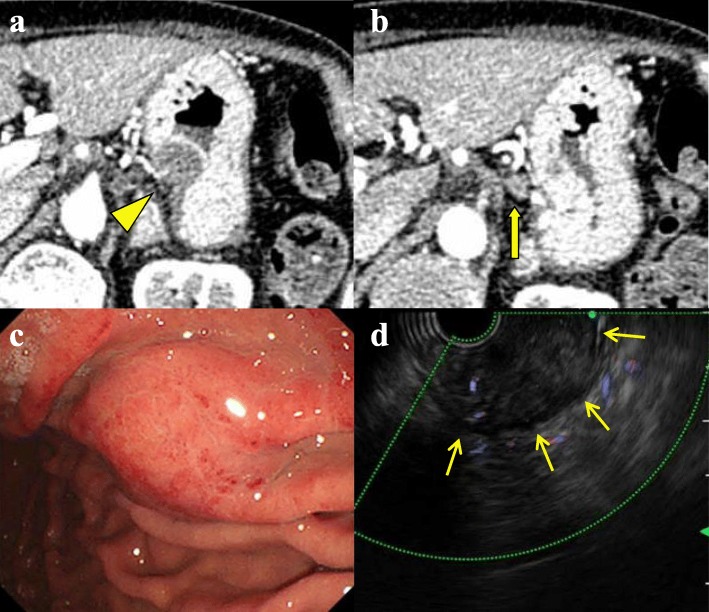
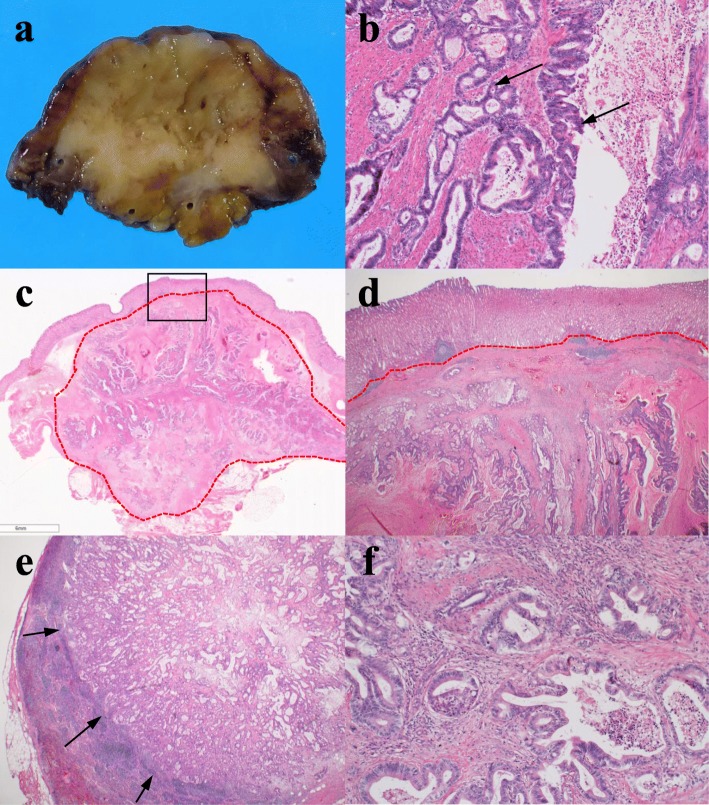
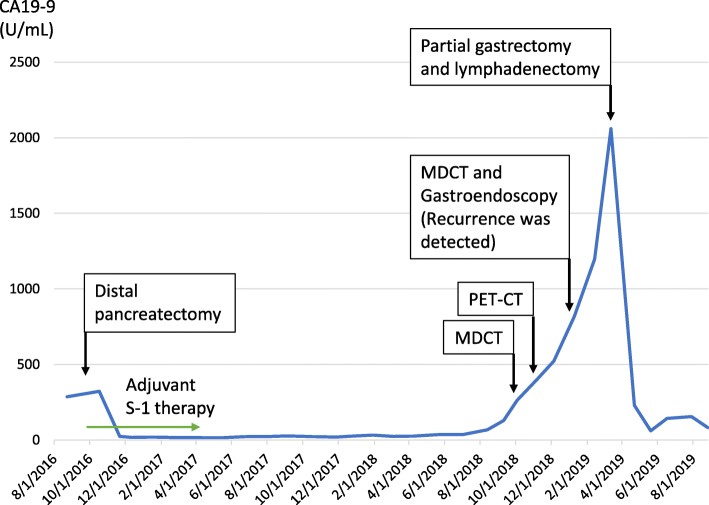
Twenty-two months after surgery, the CA19–9 level increased, but both MDCT and positron emission tomography did not show an evidence of recurrence. Three months later, during a careful follow-up, MDCT revealed a 23-mm low-density mass in the gastric body wall (Fig. 2a) with paragastric lymph node swelling (Fig. 2b). Gastroendoscopy revealed a 10-mm submucosal tumor in the posterior wall of the middle gastric body (Fig. 2c), and endoscopic ultrasound revealed a hypoechoic mass in the submucosa (Fig. 2d). Adenocarcinoma was detected on EUS-FNA, and the gastric mass was diagnosed as a metastasis of pancreatic cancer caused by needle tract seeding. Partial gastrectomy and lymph node resection were performed. Using an electrosurgical knife, all layers of the stomach located with the gastric tumor was resected with a certain margin, and the only hard and swollen lymph nodes were resected. Regarding the intraoperative findings, other metastases or peritoneal disseminations were not observed, and the cytology for ascites was negative. A 25-mm white mass was observed in the resected specimen (Fig. 3a), and histopathological examination indicated adenocarcinoma, extending from the submucosa to the subserosa in the gastric wall (Fig. 3b–d), and paragastric lymph node metastasis (Fig. 3e). She was diagnosed with metastasis of the previous pancreatic cancer derived from needle tract seeding (Fig. 3f). The postoperative course was uneventful, and recurrence was not observed for 5 months, at the time of this writing. The timeline of the treatment for this patient is described in Fig. 4.
Fig. 2.
Images at the detection of needle tract seeding in the gastric wall. a Twenty-five months after initial pancreatectomy, computed tomography revealed a 23-mm-diameter low-density mass in the wall of the gastric body (arrow head). b A lymph node around the stomach was swollen (arrow). c Gastroendoscopy revealed an approximately 10-mm-diameter submucosal tumor in the posterior gastric wall. d Endoscopic ultrasound revealed a hypoechoic mass in the submucosa (arrows)
Fig. 3.
Pathological findings of the resected tumor. a Macroscopic image of the resected gastric tumor showed a white hard tumor. b Columnar epithelium with atypical nuclei spread in the gastric wall while forming a ductal structure (arrows). These were similar to the histological findings of the previously resected pancreatic cancer. c Adenocarcinoma was mainly located from the subserosa to the muscularis propria in the gastric wall, with invasion in the submucosa (within dotted line). d An enlargement within the square of (c). The mucosal layer was preserved. e No. 3 lymph node metastasis was observed in the adenocarcinoma (arrows). f Primary pancreatic cancer. From these pathological findings, the submucosal tumor in the gastric wall was diagnosed as arising from needle tract seeding derived from pancreatic cancer
Fig. 4.
Treatment timeline of the patient
Discussion
In this report, we described a case of pancreatic cancer recurrence in the gastric wall due to needle tract seeding after distal pancreatectomy following EUS-FNA. To the best of our knowledge, this is the first report of a gastric submucosal tumor arising from needle tract seeding along with paragastric lymph node metastasis. Since the first case was reported by Hirooka et al. in 2003, a total of 18 cases including the present case have been described, and 13 cases were reported within the last 5 years (Table 1) [5–21]. Among these cases, there was no pancreatic tumor located in the head of the pancreas. This might be because the EUS-FNA had been performed through the duodenum for pancreatic head lesions, and the site of puncture would have been resected simultaneously with the primary lesion during pancreatoduodenectomy.
Table 1.
Characteristics of reported needle tract seeding of pancreatic cancer after EUS-FNA
| No. | Details of pancreatic cancer | Interval from FNA (months) | Details of needle tract seeding | Outcomes | ||||
|---|---|---|---|---|---|---|---|---|
| Location, Size (mm) | Initial therapy | Symptom | Elevated CA19–9 | Size (mm) | Treatment | |||
| 1 | Pb, 20 | DP + Partial Gx | 1 | No | NA | micro | Partial Gx | Died 25 months after surgery |
| 2 | Pt, 8 | DP | 21 | Yes | + | 50 | ChemoTx | Died 12 months after diagnosis |
| 3 | Pt, 28 | DP | 14 | Yes | + | 40 | Unknown | Unknown |
| 4 | Pb, NA | Central pancreatectomy+Adj CRT, gefitinib | 36 | No | NA | 45 | Total Gx | Died with metastasis of melanoma |
| 5 | Pb, 20 | DP | 22 | NA | – | NA | Unknown | Unknown |
| 6 | Pb, 20 | DP | 8 | No | + | 12 | Partial Gx | Alive 27 months without recurrence after Gx |
| 7 | Pb, 25 | DP + Adj S-1 | 28 | No | + | 32 | Subtotal Gx | Unknown |
| 8 | Pb, 25 | DP | 19 | No | + | 20 | Partial Gx | Alive 16 months without recurrence after Gx |
| 9 | NA, NA | DP | 6 | No | NA | NA | Distal Gx+Adj S-1 | Re-recurrence at 21 months after Gx |
| 10 | Pbt, NA | Radiation therapy | 7 | No | NA | NA | Unknown | Unknown |
| 11 | NA, 30 | ChemoTx | 3 | No | NA | 24 | ChemoTx | Died 29 months after initial EUS-FNA |
| 12 | Pb, 30 | DP + Adj S-1 | 8 | No | + | 12 | Partial Gx+Adj GEM | Alive 18 months without recurrence after Gx |
| 13 | Pb, 10 | DP + Adj S-1 | 22 | Yes | NA | NA | Partial Gx | Unknown |
| 14 | Pt, 37 | DP + Adj GEM/S-1 | 24 | No | NA | 20 | Partial Gx | Unknown |
| 15 | Pb, 35 | ChemoTx | 8 | No | NA | NA | DP + Partial Gx | Unknown |
| 16 | Pb, 15 | DP + Partial Gx | 1 | No | + | micro | Partial Gx | Died 18 months after surgery |
| 17 | Pb, 34 | DP + Partial Gx | 4 | No | NA | micro | Partial Gx | Alive 18 months after surgery |
| Our case | Pb, 32 | DP + Adj S-1 | 25 | No | + | 25 | Partial Gx + lymph node | Alive 5 months without recurrence after Gx |
EUS-FNA Endoscopic-ultrasound-guided fine needle aspiration, CA19–9 carbohydrate antigen 19–9, Pb Pancreatic body, Pt Pancreatic tail, Pbt Pancreatic body and tail, NA Not applicable, DP Distal pancreatectomy, Adj Adjuvant, ChemoTx Chemotherapy, CRT Chemoradiation therapy, GEM Gemcitabine, Gx Gastrectomy
The optimal treatment and long-term prognosis of needle tract seeding are still unknown. In general, it is rare to resect recurrent lesions in patients with postoperative pancreatic cancer since the median survival time from the detection of recurrence to death is 3–10 months [22, 23]. However, a recent systematic review, which analyzed the data of 301 postoperative patients with isolated recurrence of pancreatic cancer, showed that the median overall survival was 26.0 months (range, 0–112 months), and median disease-free survival was 14.2 months (range, 4–29 months) after the resection of recurrence sites [24]. Although these findings were analyzed in a heterogeneous and limited number of patients, these data showed that some patients may benefit from surgery. This suggests that surgery may contribute to the improvement in the prognosis in the case of gastric wall recurrence due to needle tract seeding considering that there are no other recurrent lesions. To improve the outcomes of patients with needle tract seeding by surgical procedures, early detection of recurrence is significantly crucial. Based on a review of the literature, subjective symptoms are clinically insignificant in establishing the diagnosis because 14 of the 17 patients (82.4%) were asymptomatic at the time of recurrence detection. In contrary, increased CA19–9 levels were observed in 8 of the 9 cases (88.9%). Therefore, CA19–9 might be useful for the early detection of recurrence due to needle tract seeding during the postoperative follow-up of patients.
Although several reports have suggested that the translocation of malignant cells is associated with EUS-FNA [18, 25], the developmental process of needle tract seeding is unclear. Because the number of reports is significantly small, it remains unknown whether tumor factors or fine needle aspiration procedure factors such as needle size, the number of puncture sites, and the number of needle passes are significantly associated on the occurrence of needle tract seeding. In addition, needle tract seeding of pancreatic cancer will be considered a significantly important problem in the future. A randomized controlled trial that compared neoadjuvant chemotherapy using gemcitabine and S-1 with upfront surgery (Prep-02/JSAP05) demonstrated the significant survival benefits of neoadjuvant chemotherapy for patients with resectable pancreatic cancer [26]. Considering this result, neoadjuvant chemotherapy can be considered a potentially beneficial treatment for pancreatic cancer, and simultaneously, the pathological diagnosis obtained by EUS-FNA is essential before performing an initial treatment. Hence, a prospective cohort study comprising a large sample size is required to confirm the detailed clinical characteristics of needle tract seeding.
In conclusion, patients with pancreatic body or tail cancer diagnosed by EUS-FNA should pay careful attention on the occurrence of needle tract seeding and lymph node metastasis. Further cumulative cases are required to elucidate the accurate frequency, optimal treatment, and long-term outcomes.
Acknowledgments
None.
Abbreviations
- CA19–9
Carbohydrate antigen 19–9
- EUS-FNA
Endoscopic-ultrasound-guided fine needle aspiration
- MDCT
Multidetector computed tomography
Authors’ contributions
NS gathered the patient’s data and wrote the manuscript. NS, MO, and TS performed the surgery. MO treated the patient with adjuvant chemotherapy and performed follow-up. EN and TM were responsible for the pathological diagnosis of the case. RM and NK performed EUS-FNA. HY, KF, TT, SKuboki, DS, SKagawa, and MO discussed and analyzed the data with NS and ST and assisted in writing the manuscript. All authors approved the final manuscript.
Funding
The authors received no financial support for the preparation of this case report.
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.
Ethics approval and consent to participate
The Ethics Committees of Chiba University, Graduate School of Medicine approved the content of this manuscript (#3032), and the patient provided written informed consent before surgery.
Consent for publication
Written informed consent was obtained from the patient for the publication of this case report and any accompanying images.
Competing interests
The authors declare that they have no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Eloubeidi MA, Varadarajulu S, Desai S, Shirley R, Heslin MJ, Mehra M, et al. A prospective evaluation of an algorithm incorporating routine preoperative endoscopic ultrasound-guided fine needle aspiration in suspected pancreatic cancer. J Gastrointest Surg. 2007;11(7):813–819. doi: 10.1007/s11605-007-0151-x. [DOI] [PubMed] [Google Scholar]
- 2.Jenssen C, Alvarez-Sánchez MV, Napoléon B, Faiss S. Diagnostic endoscopic ultrasonography: assessment of safety and prevention of complications. World J Gastroenterol. 2012;18(34):4659–4676. doi: 10.3748/wjg.v18.i34.4659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Ngamruengphong S, Xu C, Woodward TA, Raimondo M, Stauffer JA, Asbun HJ, et al. Risk of gastric or peritoneal recurrence, and long-term outcomes, following pancreatic cancer resection with preoperative endosonographically guided fine needle aspiration. Endoscopy. 2013;45(8):619–626. doi: 10.1055/s-0033-1344216. [DOI] [PubMed] [Google Scholar]
- 4.Kim SH, Woo YS, Lee KH, Lee JK, Lee KT, Park JK, et al. Preoperative EUS-guided FNA: effects on peritoneal recurrence and survival in patients with pancreatic cancer. Gastrointest Endosc. 2018;88(6):926–934. doi: 10.1016/j.gie.2018.06.024. [DOI] [PubMed] [Google Scholar]
- 5.Hirooka Y, Goto H, Itoh A, Hashimoto S, Niwa K, Ishikawa H, et al. Case of intraductal papillary mucinous tumor in which endosonography-guided fine-needle aspiration biopsy caused dissemination. J Gastroenterol Hepatol. 2003;18:1323–1324. doi: 10.1046/j.1440-1746.2003.03040.x. [DOI] [PubMed] [Google Scholar]
- 6.Paquin SC, Gariépy G, Lepanto L, Bourdages R, Raymond G, Sahai AV. A first report of tumor seeding because of EUS-guided FNA of a pancreatic adenocarcinoma. Gastrointest Endosc. 2005;61(4):610–611. doi: 10.1016/S0016-5107(05)00082-9. [DOI] [PubMed] [Google Scholar]
- 7.Chong A, Venugopal K, Segarajasingam D, Lisewski D. Tumor seeding after EUS-guided FNA of pancreatic tail neoplasia. Gastrointest Endosc. 2011;74(4):933–935. doi: 10.1016/j.gie.2010.10.020. [DOI] [PubMed] [Google Scholar]
- 8.Ahmed K, Sussman JJ, Wang J, Schmulewitz N. A case of EUS-guided FNA-related pancreatic cancer metastasis to the stomach. Gastrointest Endosc. 2011;74(1):231–233. doi: 10.1016/j.gie.2010.10.008. [DOI] [PubMed] [Google Scholar]
- 9.Katanuma A, Maguchi H, Hashigo S, Kaneko M, Kin T, Yane K, et al. Tumor seeding after endoscopic ultrasound-guided fine-needle aspiration of cancer in the body of the pancreas. Endoscopy. 2012;44(Suppl 2):E160–E161. doi: 10.1055/s-0031-1291716. [DOI] [PubMed] [Google Scholar]
- 10.Minaga K, Kitano M, Yamashita Y. Surgically resected needle tract seeding following endoscopic ultrasound-guided fine-needle aspiration in pancreatic cancer. J Hepatobiliary Pancreat Sci. 2015;22(9):708–709. doi: 10.1002/jhbp.269. [DOI] [PubMed] [Google Scholar]
- 11.Tomonari A, Katanuma A, Matsumori T, Yamazaki H, Sano I, Minami R, et al. Resected tumor seeding in stomach wall due to endoscopic ultrasonography-guided fine needle aspiration of pancreatic adenocarcinoma. World J Gastroenterol. 2015;21(27):8458–8461. doi: 10.3748/wjg.v21.i27.8458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sakurada A, Hayashi T, Ono M, Ishiwatari H, Ogino J, Kimura Y, et al. A case of curatively resected gastric wall implantation of pancreatic cancer caused by endoscopic ultrasound-guided fine-needle aspiration. Endoscopy. 2015;47(Suppl 1 UCTN):E198–E199. doi: 10.1055/s-0034-1377592. [DOI] [PubMed] [Google Scholar]
- 13.Iida T, Adachi T, Ohe Y, Nakagaki S, Yabana T, Kondo Y, et al. Re-recurrence after distal gastrectomy for recurrence caused by needle tract seeding during endoscopic ultrasound-guided fine-needle aspiration of a pancreatic adenocarcinoma. Endoscopy. 2016;48(Suppl 1):E304–E305. doi: 10.1055/s-0042-116431. [DOI] [PubMed] [Google Scholar]
- 14.Kita E, Yamaguchi T, Sudo K. A case of needle tract seeding after EUS-guided FNA in pancreatic cancer, detected by serial positron emission tomography/CT. Gastrointest Endosc. 2016;84(5):869–870. doi: 10.1016/j.gie.2016.01.060. [DOI] [PubMed] [Google Scholar]
- 15.Yamabe A, Irisawa A, Shibukawa G, Hoshi K, Fujisawa M, Igarashi R, et al. Rare condition of needle tract seeding after EUS-guided FNA for intraductal papillary mucinous carcinoma. Endosc Int Open. 2016;4(7):E756–E758. doi: 10.1055/s-0042-107072. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Minaga K, Kitano M, Enoki E, Kashida H, Kudo M. Needle-tract seeding on the proximal gastric wall after EUS-guided fine-needle aspiration of a pancreatic mass. Am J Gastroenterol. 2016;111(11):1515. doi: 10.1038/ajg.2016.307. [DOI] [PubMed] [Google Scholar]
- 17.Yasumoto M, Okabe Y, Ishikawa H, Kisaki J, Akiba J, Naito Y, et al. A case of gastric wall implantation caused by EUS-FNA 22 months after pancreatic cancer resection. Endosc Ultrasound. 2018;7(1):64–66. doi: 10.4103/eus.eus_58_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sakamoto U, Fukuba N, Ishihara S, Sumi S, Okada M, Sonoyama H, et al. Postoperative recurrence from tract seeding after use of EUS–FNA for preoperative diagnosis of cancer in pancreatic tail. Clin J Gastroenterol. 2018;11(3):200–205. doi: 10.1007/s12328-018-0822-z. [DOI] [PubMed] [Google Scholar]
- 19.Matsumoto K, Kato H, Tanaka N, Okada H. Preoperative detection of tumor seeding after endoscopic ultrasonography-guided fine needle aspiration for pancreatic cancer. Intern Med. 2018;57(12):1797–1798. doi: 10.2169/internalmedicine.0321-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Minaga K, Takenaka M, Katanuma A, Kitano M, Yamashita Y, Kamata K, et al. Needle tract seeding: an overlooked rare complication of endoscopic ultrasound-guided fine-needle aspiration. Oncology. 2017;93(Suppl 1):107–112. doi: 10.1159/000481235. [DOI] [PubMed] [Google Scholar]
- 21.Matsui T, Nishikawa K, Yukimoto H, Katsuta K, Nakamura Y, Tanaka S, et al. Needle tract seeding following endoscopic ultrasound-guided fine-needle aspiration for pancreatic cancer: a report of two cases. World J of Surgical Oncol. 2019;17(1):134. doi: 10.1186/s12957-019-1681-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Sperti C, Pasquali C, Piccoli A, Pedrazzoli S. Recurrence after resection for ductal adenocarcinoma of the pancreas. World J Surg. 1997;21(2):195–200. doi: 10.1007/s002689900215. [DOI] [PubMed] [Google Scholar]
- 23.Zhang Y, Frampton AE, Kyriakides C, Bong JJ, Habib N, Ahmad R, et al. Loco-recurrence after resection for ductal adenocarcinoma of the pancreas: predictors and implications for adjuvant chemoradiotherapy. J Cancer Res Clin Oncol. 2012;138(6):1063–1071. doi: 10.1007/s00432-012-1165-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moletta L, Serafini S, Valmasoni M, Pierobon ES, Ponzoni A, Sperti C. Surgery for recurrent pancreatic cancer: is it effective? Cancers (Basel) 2019;11(7):E991. doi: 10.3390/cancers11070991. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Levy MJ, Gleeson FC, Campion MB, Caudill JL, Clain JE, Halling K, et al. A prospective cytological assessment of gastrointestinal luminal fluid acquired during EUS: a potential source of false-positive FNA and needle tract seeding. Am J Gastroenterol. 2010;105(6):1311–1318. doi: 10.1038/ajg.2010.80. [DOI] [PubMed] [Google Scholar]
- 26.Unno M, Motoi F, Matsuyama Y, Satoi S, Matsumoto I, Aosasa S, et al. Randomized phase II/III trial of neoadjuvant chemotherapy with gemcitabine and S-1 versus upfront surgery for resectable pancreatic cancer (Prep-02/JSAP-05) J Clin Oncol. 2019;37(Suppl 4):189. doi: 10.1200/JCO.2019.37.4_suppl.189. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.