Abstract
Purpose
To report the outcomes of medical and surgical management for congenital aniridia-associated keratopathy (AAK) over a long follow-up period.
Design
Retrospective, comparative case series
Methods
Medical records of patients diagnosed with congenital aniridia were retrospectively reviewed. Age, gender, ethnicity, follow-up time, AAK stage, non-corneal abnormalities, ocular surgeries, and complications were recorded. The visual acuity equivalent (VAE), approximate Early Treatment Diabetic Retinopathy Study (appETDRS) letter score, was calculated using recorded Snellen visual acuities.
Results
Ninety-two eyes of 47 patients (31 females) with mean age of 48.0±18.0 years, and mean follow-up of 78.6±42.2 months were included. At the initial visit, 12 eyes (13%) were classified as stage I AAK, 33 eyes (35.9%) stage II, 25 eyes (27.2%) stage III, 17 eyes (18.5%) stage IV and 5 eyes (5.4%) stage V. Limbal stem cell transplantation (LSCT) and Boston Keratoprosthesis (KPro) were frequently performed on eyes with stages III-V. These advanced corneal surgeries significantly improved the median (95% CI) of calculated appETDRS scores from 2(0–20) to 26(15–41) (Snellen, 20/20000 to 20/300, P=0.0004). Patients with earlier stages (I-II) of AAK were managed medically and had stable visual acuity through their final visits (appETDRS, 26(20–35) to 35(26–35), Snellen, 20/300 to 20/200,P>0.05). The appETDRS VAE was significantly improved from 20(0–35) to 30(20–55), Snellen 20/400 to 20/250, following LSCT (P=0.021) and from 2(0–20) to 2(0–41) after KPro, same 20/20000 Snellen VAE, but with improved 95% CI after follow-up (P=0.019).
Conclusions
With proper characterization and staging of AAK, individualized medical and advanced surgical interventions preserves and improves visual acuity.
Keywords: Congenital aniridia, Corneal disease, Limbal stem cell deficiency, Limbal stem cell transplantation, Boston Keratoprosthesis, Visual acuity
Introduction
Congenital aniridia is a condition which manifests as a constellation of ophthalmic findings of varying severities including keratopathy, foveal hypoplasia, nystagmus, cataract, glaucoma, and iris hypoplasia.1 This condition has been found to be associated with dominantly-inherited mutations or deletions involving the PAX6 gene. Aniridia-associated keratopathy (AAK), characterized by progressive corneal pannus and opacification, can be seen in up to 80% of patients in varying degrees of severity.1, 2 Signs of keratopathy can appear as early as the first decade of life, though the median age of diagnosis is 33 years.3 Besides, glaucoma, AAK is the most common cause of progressive vision loss in aniridia. AAK begins with conjunctivalization and vascularization of the peripheral cornea, with slow, progressive encroachment onto the central cornea. These findings are a direct result of the loss of function of the limbal epithelial stem cells.4 In vivo confocal microscopy studies in aniridic patients have shown a strong correlation between the morphology of the palisades of Vogt (POV) and the stage of AAK. The progressive morphologic degradation of POV correlates with the loss of normal limbal and corneal epithelial phenotypes5 In addition to the abnormalities of the limbal stem cell/niche in AAK, many studies have demonstrated corneal epithelial cell dysfunction as a result of abnormal differentiation 4, defective cell adhesion,6 increased sensitivity to oxidative stress,7 and impaired wound healing.8, 9
Clinically, patients with AAK experience recurrent erosions, corneal ulceration, chronic pain, and eventually, loss of vision.10 Patients with AAK often have concomitant meibomian gland dysfunction, tear film insufficiency and decreased corneal sensitivity all of which are correlated with the severity of the corneal disease.11
Traditionally, management of early AAK has been supportive, while reserving penetrating keratoplasty for severe stromal scarring12 The outcomes of keratoplasty alone for AAK are poor,13 though they may still be helpful adjunctive procedures for restoring corneal clarity. Current methods such as limbal stem cell transplantation (LSCT), including keratolimbal allograft (KLAL) transplantation and living-related conjunctival-limbal allograft (lr-CLAL) transplantation, as well as Boston Keratoprosthesis (KPro) implantation have been demonstrated to be effective treatments for AAK.10, 14, 15 In contrast to penetrating keratoplasty, LSCT addresses the underlying pathophysiology of AAK, while KPro circumvents it.
Studies detailing the outcomes of these different strategies at the different stages of AAK are limited. In this study, the charts of patients diagnosed with AAK and managed at a tertiary care academic center were reviewed and analyzed, focusing on management, complications, visual outcomes. The results of this study led to the development of an evidence-based algorithm based on the stage of keratopathy to guide management of patients with AAK.
Patients and Methods
In this retrospective cohort study (comparative case series), the clinical charts of 47 patients (92 eyes) diagnosed with congenital aniridia by the cornea service at the Illinois Eye and Ear Infirmary (Chicago, IL) from 2005 to 2018 were reviewed. The diagnosis of congenital aniridia was established based on the clinical presentation including but not limited to: foveal hypoplasia, absence or hypoplasia of the iris, and nystagmus.16 The study was approved by Institutional Review Board (IRB) of College of Medicine, University of Illinois at Chicago.
The recorded data included demographic information, clinical examination data (including visual acuity, corneal pathology), surgical interventions, medications, and side effects. The severity of AAK was staged (Summarized in Table S1 in supplementary materials) as defined by Holland et al.3, 17 Stage I consists of abnormal peripheral corneal epithelium, manifested by increased uptake of fluorescein (late staining); Stage II is characterized by centripetal extension of epithelial changes; Stage III is characterized by central corneal epithelial changes and peripheral superficial neovascularization; Stage IV consists of abnormal epithelium over the entire cornea with sub-epithelial fibrosis; Stage V, the most advanced, describes abnormal epithelium over the entire cornea with deep and permanent stromal scarring.
For the purpose of this study, patients managed by medical treatments (mainly those in lower AAK stages), are grouped under no advanced corneal surgeries (“No-Surgery”). The medical management of No-Surgery patients primarily included administration of non-preservative artificial tears, autologous serum tears, and scleral contact lenses. Limbal stem cell transplantation (LSCT) and Boston Keratoprosthesis (KPro) are grouped under the advanced corneal surgery group for management of higher stages of aniridic keratopathy. Visual acuities at the initial visit and subsequent follow-up visits were recorded. Improvement in visual acuity was defined as a final recorded best corrected visual acuity (BCVA) greater than the visual acuity at the initial visit.
Visual Acuity Equivalents and Statistical Analysis
The data are presented as mean±standard deviation (SD), number (percentage) and/or median (95% CI). For statistical analysis and comparison, BCVA was converted into approximate Early Treatment Diabetic Retinopathy Study (ETDRS) letter scores (appETDRS score) to represent visual acuity equivalent (VAE). The appETDRS score was used for ease of statistical analysis. Approximate ETDRS Letter Score (appETDRS Score) was converted by applying 85+50×log (Snellen Fraction), which was rounded to the nearest ETDRS Letter Score as described earlier.18 Subsequently, results were converted back to Snellen equivalent for ease of comprehension (The conversion of visual acuities between Snellen and appETDRS VAEs is summarized in Table S1 in supplementary materials).
Statistical analyses were performed using GraphPad Prism version 8.0.0 for Windows, GraphPad Software (San Diego, CA, USA; www.graphpad.com). Mean differences were statistically analyzed using paired and independent T-tests and one-way ANOVA with Tukey post-hoc. Chi-square test was used for qualitative data. Ordinal data (e.g. appETDRS Score) was analyzed using non-parametric tests including Mann-Whitney U test and Kruskal-Wallis test with Dunn-Bonferroni post-hoc for independent measures, and Wilcoxon for repeated/paired measures. P-values less than 0.05 were statistically significant.
Results
Demographics, Staging, and Interventions
Ninety-two eyes of 47 patients (two eyes were excluded due to enucleation) with diagnosis of congenital aniridia and aniridia-associated keratopathy were enrolled in this study. The mean follow-up was 78.6±42.2 (range, 10 to 156) months. Demographic data is summarized in Table 1. Thirty-one patients (65.9%) were female, and 16 patients (34.1%) were male. The mean age of patients was 48.0±18.0 (range, 11 to 90) years. The majority of cases had Stage II (35.9%) and Stage III (27.2%) aniridic keratopathy. Moreover, the percentage of Stage I among enrolled eyes was 13%, Stage IV was 18.5% and stage V was 5.4%. The most prevalent non-corneal pathologies were glaucoma and cataract (63% and 54.3%, respectively).
Table 1:
Demographic data and ocular manifestations of enrolled cases.*
| Patients (No) | 47 |
| Eyes (No) | 92 |
| Age (years, mean±SD) | 48.0±18.0 |
| Follow up (months, mean±SD) | 78.6±42.2 |
| Gender (No. (%)) | |
| Male | 16 (34.1) |
| Female | 31 (65.9) |
| Race (No. (%)) | |
| African-American | 10 (21.3) |
| White | 29 (61.7) |
| Hispanic | 2 (4.2) |
| Other | 6 (12.8) |
| Aniridia-Associated Keratopathy Stage at First Visit (Eye No. (%)) | |
| Stage I | 12 (13) |
| Stage II | 33 (35.9) |
| Stage III | 25 (27.2) |
| Stage IV | 17 (18.5) |
| Stage V | 5 (5.4) |
| Non-Corneal Pathologies Recorded during Follow up (Eye No. (%)) | |
| Aniridia Fibrosis Syndrome | 5 (5.4) |
| Glaucoma | 58 (63) |
| Angle Closure Glaucoma | 2 (2.2) |
| Ocular Hypertension | 3 (3.3) |
| Uncontrolled Glaucoma (Vision Loss owing to Glaucoma) | 1 (1.7) |
| Cataract | 58 (54.3) |
| Subluxation of the Lens | 2 (2.2) |
| Central Retinal Vein Occlusion | 1 (1.1) |
| Proliferative Vitreoretinopathy | 1 (1.1) |
| Diabetic Retinopathy | 1 (1.1) |
| Vitreous Hemorrhage | 1 (1.1) |
Data are presented as mean±SD, and/or Number (percentage).
Table 2 summarizes surgical procedures and post-operative complications during management of aniridic keratopathy, glaucoma, lens, and retinal pathologies. Most surgical interventions for AAK included LSCT and/or KPro. LSCT had a failure rate of 42.3%, and these required subsequent repeat LSCT and/or KPro. Retroprosthetic membranes formed in 40.9% of eyes managed with KPro. Penetrating keratoplasty (PKP) was performed in a subset of patients to improve corneal transparency after LSCT (n=5 eyes) and for other indications (n=3 eyes). Four eyes had a history of PKP prior to presentation. Fifty percent of the corneal transplants failed, requiring subsequent repeat-PKP, LSCT and/or KPro procedures. Fifty-eight out of 92 eyes developed glaucoma requiring intraocular pressure-lowering topical agents in 54 eyes and implantation of glaucoma shunts in 24 eyes. Fifty-eight eyes had lens pathology including cataract formation and crystalline lens subluxation which was managed most commonly by cataract removal and IOL placement (48 eyes). Pars-plana vitrectomy was performed in 13 eyes.
Table 2:
Performed procedures and observed complications/side effects for management of aniridia-related pathologies during follow up period.*
| Pathology (Intervention Required) | Intervention | Frequency within Pathology (No. (%)) | Observed Complications/Side Effects in Follow-up | Frequency in Performed Procedures (No. (%)) | |
|---|---|---|---|---|---|
| Aniridia-Associated Keratopathy (N=92 eyes) | Limbal Stem Cell Transplantation | 26 (28.3) | Failure/rejection (repeat LSCT or KPro required) | 11 (42.3) | |
| Boston Keratoprosthesis | 22 (23.9) | Retroprosthetic membrane | 9 (40.9) | ||
| Extrusion of KPro | 4 (18.2) | ||||
| PKP | Performed before first visit to the referral center | 4 (4.3) | Failure (necessity for LSCT, repeat-LSCT, or KPro), total 6 (50%) of PKPs | 2 (66.6), required KPro | |
| Concurrent/after LSCT | 5 (5.4) | 3 (60), required repeat-LSCT | |||
| Performed independently | 3 (3.3) | 1 (33.3), required LSCT and KPro | |||
| Keratectomy | 4 (4.4) | - | |||
| AMT | 3 (3.3) | - | |||
| Tarsorrhaphy | 1 (1.1) | - | |||
| Glaucoma (N=58 eyes) | Glaucoma Shunt Placement | 24 (41.3) | Hypotony | 1 (4.1) | |
| Glaucoma Drop Administration | 54 (93.1) | - | |||
| Diode and/or SLT Treatment | 7 (12.1) | Aniridia Fibrosis Syndrome | 2 (28.5) | ||
| Lens Pathology (N=58 Eyes) | Cataract Surgery with IOL Placement | 48 (81.1) | Complication(s) required IOL exchange/removal | 5 (10.6) | |
| Lensectomy | 3 (5.2) | - | |||
| YAG Laser Capsulotomy | 3 (5.1) | - | |||
| Retinal Pathology (N=16 Eyes) | Pars Plana Vitrectomy/Retinal Detachment Repair | 13 (81.2) | Suprachoroidal hemorrhage | 2 (15.4) | |
| Scleral Reinforcement | 3 (18.8) | - | |||
Data are presented as Number (percentage).
Abbreviations: LSCT, Limbal Stem Cell Transplantation; KPro, Keratoprosthesis; PK, Penetrating Keratoplasty; AMT, Amniotic Membrane Transplantation; SLT, Selective Laser Trabeculoplasty; IOL, Intra-Ocular Lens.
Advanced Corneal Surgeries Improve Visual Acuity in Congenital AAK
Table 3 shows the outcomes following major corneal surgeries (LSCT and KPro), including the preservation and/or improvement of visual acuity in eyes with AAK. Overall, the median visual acuity was improved at the last follow-up visit compared to first visit in all enrolled eyes (appETDRS Score, 20 (5–30) versus 26 (20–35); ie. Snellen 20/400 to 20/300, respectively, P<0.0001). Forty-two eyes (45.7%) out of all 92 enrolled eyes had improvement in their visual acuity at final follow-up. Fifty-one eyes were managed medically during the follow-up time with no advanced corneal surgery; while, 41 eyes underwent advanced corneal surgeries (LSCT and KPro) to improve their visual acuity. Patients who underwent advanced corneal surgeries on at least one eye were typically older in age. The mean age in patients with advanced corneal surgeries and with no advanced corneal surgery was 53.0±17.2 (range, 20 to 90) and 44.0±17.8 (range, 11 to 90) years at last follow-up, respectively (P=0.016). The mean age of patients at first advanced corneal surgery was 44.5±17.5 (range, 10 to 82) years. The prevalence of glaucoma in patients whom required advanced corneal surgeries was significantly higher than that of patients with no advanced surgery (P<0.0001); however, the distribution of patients requiring cataract surgery was similar across both groups (P=0.692).
Table 3:
Comparing the effects of individualized interventions on BCVA in congenital aniridia-associated keratopathy.*
| No Advanced Corneal Surgery (N=51 eyes) | Patients with Advanced Corneal Surgeries (LSCT and/or KPro, N=41 eyes) | Total | P-value (between cases with no-surgery and total of those with advanced surgeries) | P-value (between cases with no-surgery and sub-groups of advanced surgeries) | |||||
|---|---|---|---|---|---|---|---|---|---|
| Total | Sub-Groups | ||||||||
| LSCT (N=19 eyes) | LSCT-KPro (N=7 eyes) | KPro (N=15 eyes) | |||||||
| Age at Last Follow-up (years, mean±SD) | 44.0±18.0 | 53.0±17.2 | 56.4±14.4 | 44.6±19.5 | 52.5±18.9 | 48.0±18.0 | 0.016 (Independent T-Test ) | 0.045 (One-way ANOVA Test) | |
| Age at First Advanced Corneal Surgery (years, mean±SD) | - | 44.5±17.5 | 48.3±13.4 | 33.1±20.5 | 45.1±19.5 | - | - | - | |
| Follow-up (months, mean±SD) | 65.3±43.7 | 95.2±34.1 | 99.9±33.2 | 96.8±45.5 | 88.4±30.6 | 78.6±42.2 | 0.001 (Independent T-Test) | 0.006 (One-way ANOVA Test) | |
| Glaucoma (No. (%)) | Yes | 24 (47.1) | 34 (82.9) | 16 (84.2) | 6 (85.7) | 12 (80) | 58 (63) | <0.0001 (Chi-Square test) | 0.005 (Chi-Square test) |
| No | 27 (52.9) | 7 (17.1) | 3 (15.8) | 1 (14.3) | 3 (20) | 34 (37) | |||
| Cataract Surgery (No. (%)) | Yes | 27 (52.9) | 20 (48.8) | 8 (42.1) | 5 (71.4) | 5 (33.3) | 47 (51.1) | 0.692 (Chi-Square test) | 0.351 (Chi-Square test) |
| No | 24 (47.1) | 21 (51.2) | 11 (57.9) | 2 (28.6) | 10 (66.7) | 45 (48.9) | |||
| Aniridia- Associated Keratopathy Stage (No. (%)) | I | 12 (23.5) | 0 | 0 | 0 | 0 | 12 (13) | <0.0001 (Mann-Whitney U test) | <0.0001 (Kruskal-Wallis Test) |
| II | 30 (58.8) | 3 (7.3) | 2 (10.5) | 1 (14.3) | 0 | 33 (35.9) | |||
| III | 6 (11.8) | 19 (46.3) | 13 (68.4) | 4 (57.1) | 2 (13.3) | 25 (27.2) | |||
| IV | 2 (3.9) | 15 (36.6) | 4 (21.1) | 1 (14.3) | 10 (66.7) | 17 (18.5) | |||
| V | 1 (2) | 4 (9.8) | 0 | 1 (14.3) | 3 (20) | 5 (5.4) | |||
| BCVA at First Visit | |||||||||
| Snellen Equivalent (No. (%)) | ≥20/100 | 9 (17.6) | 3 (7.3) | 3 (15.8) | 0 | 0 | 12 (13) | 0.005 (Mann-Whitney U test) | 0.005 † (Kruskal-Wallis Test) |
| ≥20/400 | 28 (54.9) | 13 (31.7) | 7 (36.8) | 2 (28.6) | 4 (26.7) | 41 (44.6) | |||
| ≥20/1500 | 1 (2) | 2 (4.9) | 1 (5.3) | 0 | 1 (6.7) | 3 (3.3) | |||
| ≥20/20000 | 12 (23.9) | 23 (56.1) | 8 (42.1) | 5 (71.4) | 10 (66.7) | 35 (38) | |||
| LP | 1 (2) | 0 | 0 | 0 | 0 | 1 (1.1) | |||
| appETDRS VAE (Median (95% CI)) | 26 (20–35) | 2 (0–20) | 20 (0–35) | 2 (0–35) | 2 (0–20) | 20 (5–30) | 0.002 (Mann-Whitney U test) | 0.003 † (Kruskal-Wallis Test) | |
| BCVA at Last Visit | |||||||||
| Snellen Equivalent (No. (%)) | ≥20/100 | 11 (21.6) | 8 (19.5) | 5 (26.3) | 1 (14.3) | 2 (13.3) | 19 (20.7) | 0.069 (Mann-Whitney U test) | 0.031‡ (Krnskal-Wallis Test) |
| ≥20/400 | 26 (51) | 18 (43.9) | 11 (57.9) | 3 (42.9) | 4 (26.7) | 44 (47.8) | |||
| ≥20/1500 | 4 (7.8) | 2 (4.9) | 1 (5.3) | 0 | 1 (6.7) | 6 (6.5) | |||
| ≥20/20000 | 9 (17.6) | 4 (9.8) | 1 (5.3) | 1 (14.3) | 2 (13.3) | 13 (14.1) | |||
| LP | 0 | 4 (9.8) | 0 | 2 (28.6) | 2 (13.3) | 4 (4.3) | |||
| NLP | 1 (2) | 5 (12.2) | 1 (5.3) | 0 | 4 (26.7) | 6 (6.5) | |||
| appETDRS VAE (Median (95% CI)) | 35 (26–35) | 26 (15–41) | 30 (20–55) | 41 (0–55) | 2 (0–41) | 26 (20–35) | 0.396 (Mann-Whitney U test) | 0.178 (Krnskal-Wallis Test) | |
| Change in Visual Acuity (No. (%)) | |||||||||
| Impairment | 12 (23.5) | 14 (34.1) | 5 (26.3) | 3 (42.9) | 6 (40) | 26 (28.3) | 0.494 (Mann-Whitney U test) | 0.663 (Krnskal-Wallis Test) | |
| Stable | 20 (39.2) | 4 (9.8) | 2 (10.5) | 0 | 2 (13.3) | 24 (26.1) | |||
| Better | 19 (37.3) | 23 (56.1) | 12 (63.2) | 4 (57.1) | 7 (46.7) | 42 (45.7) | |||
Data are presented as mean±SD, Number (Percentage) and/or Median (95% CI).
Significant difference between No-Advanced Surgery and KPro groups (Dunn-Bonferroni post-hoc test, P<0.05). No significant difference between other groups.
Significant difference between LSCT and KPro groups (Dunn-Bonferroni post-hoc test, P<0.05). No significant difference between other groups.
Abbreviations: LSCT, Limbal Stem Cell Transplantation; KPro, Keratoprosthesis; BCVA, Best Corrected Visual Acuity; appETDRS VAE, Approximate Early Treatment Diabetic Retinopathy Study Letter Score Visual Acuity Equivalent.
The median (95% CI) appETDRS Score VAE for eyes with major corneal surgeries was 2 (0–20) (Snellen 20/20000) at presentation, which was significantly poorer than that of eyes not requiring major corneal surgeries (appETDRS Score, 26 (20–35); i.e. Snellen 20/300 P=0.002). However, advanced corneal surgeries led to a significant improvement of BCVA in these eyes by last follow-up (appETDRS Score 26 (15–41); i.e. Snellen 20/300, P=0.0004). Furthermore, no significant difference in BCVA between the two groups was found at last follow-up (P=0.396, Table 3).
Individualized Treatment Plans Result in Significant Improvements in Visual Acuity in Patients with AAK
As presented in Table 3, the procedures for management of AAK were categorized into (1) eyes that did not require LSCT or KPro surgery (No-Surgery), (2) eyes that underwent primary LSCT, including those who required repeat LSCT (LSCT), (3) eyes that underwent primary LSCT followed by a KPro (LSCT-KPro), and (4) eyes with primary KPro implantation, including those requiring repeat KPro (KPro). The stage of AAK at initial visit was significantly higher in eyes that underwent LSCT and/or KPro compared to eyes with no advanced corneal surgery (P<0.0001). The BCVA (appETDRS score) was significantly different at first visit between eyes that did not require advanced corneal surgery and those who eventually underwent LSCT and/or KPro surgeries (P=0.003). Glaucoma was more prevalent in cases managed with LSCT and/or KPro (P=0.005). Rates of cataract surgery were similarly distributed through advanced surgery-type groups (P=0.351).
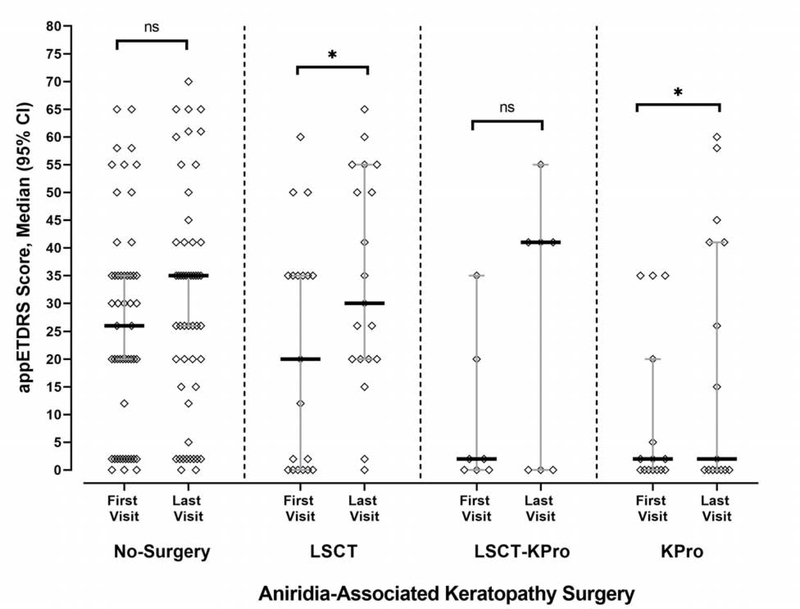
As it is shown in Figure 1, median appETDRS score VAE (95% CI) was 26 (20–35) (Snellen 20/300) in the 51 eyes with no advanced corneal surgery. The BCVA in these eyes did not significantly change during follow-up (appETDRS VAE (95% CI), 35 (26–35); i.e., Snellen 20/200, P=0.092). However, performing LSCT (with repeated limbal stem cell transplantation if needed) on 19 eyes significantly improved the BCVA during follow-up time (appETDRS VAE (95% CI), 20 (0–35) improved to 30 (20–55), Snellen, 20/400 to 20/250; P=0.021). Similarly, intervention with KPro significantly improved the BCVA as recorded at first visit and last follow-up visit (appETDRS VAE (95% CI), first visit, 2 (0–20), last visit, 2 (0–41), P=0.019, Figure 1).– Before KPro, 66.7% of patients had 20/20000 to 20/1500 vision, 26.7% patients had between 20/400 and 20/100 vision and no patients had 20/100 or better; meanwhile after KPro, 26.7% patients had at least 20/100 vision and 6.7% had 20/100 to 20/400 (see Table 3).
Figure 1:
The effects of individualized advanced corneal surgeries on BCVA changes in management of AAK. The median visual acuity (appETDRS Score visual acuity equivalents) was significantly improved after performing limbal stem cell transplantation (LSCT) and Boston Keratoprosthesis (KPro). The visual acuity in patients with no surgical management was not significantly changed during the follow-up time. Although, the overall median (95% CI) visual acuity in cases managed by both LSCT followed by KPro (LSCT-KPro group) was improved, the difference was not significant. The data were analyzed using Wilcoxon test. *, P<0.05; ns, not significant.
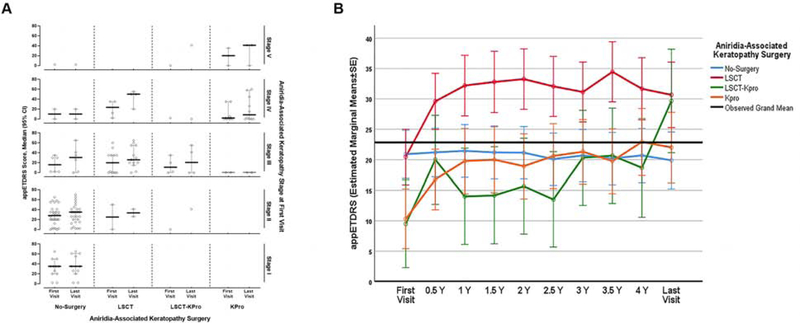
Figure 2A shows the relationship among AAK stages with procedures performed and the resultant visual acuity (represented in appETDRS score VAEs (95% CI)). The median aniridic keratopathy stages for eyes managed with no surgery, LSCT, or only with KPro were II, III and IV, respectively. The medical and surgical management according to the stage of corneal pathology at first visit resulted in preservation or improvement in visual acuity (Figure 2A).
Figure 2:
(A) Advanced corneal surgeries were significantly more prevalent in higher stages of aniridic keratopathy (Kruskal-Wallis tests, P<0.0001). KPro was the preferred first performed advanced surgery in stages IV and V. Meanwhile, LSCT was preferred for stages III and IV. In general, an improvement in visual acuity was observed in all management regardless of the stage of AAK. (B) Outlining the changes in appETDRS visual acuity equivalents of enrolled cases through follow up in different time points. There is an initial improvement in BCVA in the first 6 to 12 months after advanced surgical interventions followed by stable visual acuity up to the last follow-up visit.
Moreover, tracking the visual acuities throughout the follow-up period in different time-point visits demonstrates that there is an initial improvement in BCVA in the first 6 to 12 months as a result of the advanced surgical interventions, followed by stability that is usually maintained until the last follow-up visit (Figure 2B).
Discussion
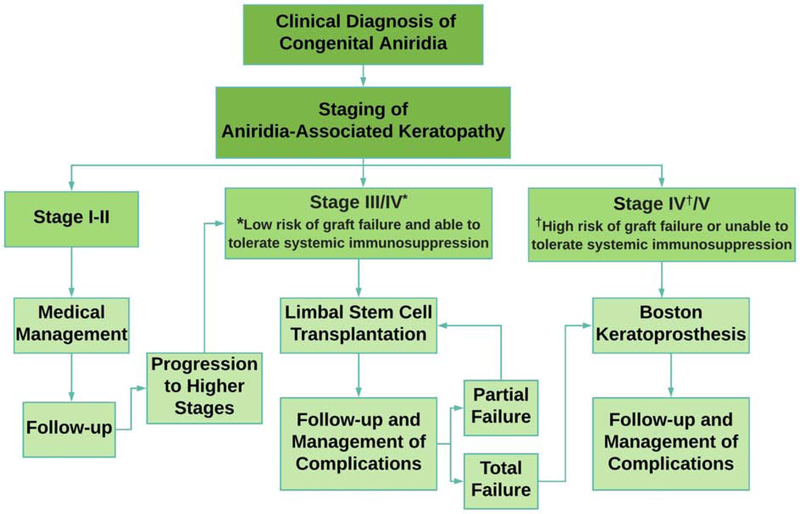
In this retrospective cohort study, we analyzed the visual outcomes of AAK based on the staging of the corneal disease in each eye regardless of the stage of the fellow eye. In general, low AAK stages were managed medically, whereas higher AAK stages were treated with advanced corneal surgeries including limbal stem cell transplantation and Boston Keratoprosthesis. Our results show that the keratopathy stage-based management strategies preserved or improved the visual acuity, and this improvement was maintained throughout the follow-up period. This observation led to the recommendation of an algorithm for management of AAK according to the primary stage of corneal pathology (Figure 2).
Aniridic patients may gradually develop vision loss from glaucoma, cataract, or aniridia-associated keratopathy. In this study, we found that prevalence of glaucoma and cataract are 63% and 54.3%, respectively (Table 1), which is consistent with previous studies.19, 20 Our data also shows that patients who require advanced corneal surgery have a significantly higher association with developing glaucoma or experiencing glaucomatous progression than those who do not require advanced corneal surgery.
The eyes treated with medical management (fifty-one eyes) had a higher prevalence of lower keratopathy stages (stages I, II) than those underwent advanced corneal surgeries (forty-one eyes, stages III, IV and V). Medical management involved minimally invasive treatments (preservative-free artificial tears, autologous serum tears and scleral contact lenses) to promote a healthier ocular surface environment and necessitated frequent follow-up to monitor for progression. Thirty-nine out of 51 eyes with medical management had stable or improved visual acuity at last follow-up.
In stage III/IV of AAK, limbal stem cell transplantation was generally performed. This addresses the underlying stem cell deficiency in AAK and aims to prevent stromal scarring. Limbal stem cell transplantation includes living-related conjunctival-limbal allograft (lr-CLAL) transplantation (3 eyes in this study) or keratolimbal allograft (KLAL) transplantation (16 eyes in this study). Our current preference is to perform lr-CLAL owing to lower risk of failure/rejection with proper immunosuppression. PKP was performed in 5 eyes following LSCT to remove stromal scarring.
In stage IV of AAK, limbal stem cell transplantation (with subsequent PKP in cases of severe corneal scarring) is preferred over KPro as an optical procedure if the case is deemed to have a low risk for limbal graft failure. According to recent studies, ocular surface inflammation, severe dry eye, ocular surface exposure, and inability to take long-term systemic immunosuppressive are risk factors that lead to graft failure.10, 21–27 In this study, 73.7% cases managed with limbal stem cell transplantation had improved or stable visual acuity at the last visit (Table 3). However, 42.3% of LSCTs failed or had rejection over the course of follow-up and required subsequent repeat LSCT or placement of a KPro. Our results had overall lower visual acuity improvement and a higher rate of limbal graft failure/rejection compared to study by Holland et al,26 that aniridic patients with at least 5 years of follow-up had a 73.1% rate of success of LSCT with one procedure and 81.4% success with repeat LSCT. Of note, this study looked only at LSCT treatment and looked predominantly at patients with stage IIa LSCD, while our institution performs LSCT for stage III-IV LSCD. Moreover, evaluating each eye independently from the other eye is a limitation of this study which should be considered in further studies.
For high-risk stage IV cases and patients who are unable to tolerate systemic immunosuppression (due to advanced age or systemic co-morbidities), Boston Keratoprosthesis is preferred over LSCT. Patients with high risk for LSCT failure mainly include those with prior graft failures (PKP or LSCT) who have already been sensitized immunologically. For stage V, we generally prefer KPro since LSCT alone cannot restore vision and they will require additional keratoplasty procedure that can increase the risk of rejection/failure. Nonetheless, this is not an absolute indication and LSCT combined with PKP may be considered as an alternative KPro in stage V patients with no prior transplants or tube shunts (given the high likelihood of recurrent endothelial failure in patients with tube shunt). Several studies demonstrated reasonable success and long-term retention of primary KPro in patients with limbal stem cell deficiency, with approximately 80% retention and good visual acuity at 3 to 5 years.28–30 In general, eyes without preoperative cicatricial diseases, such as aniridia, had lower complication rates than those with cicatricial diseases. Previous studies showed that primary KPro implantation achieved better visual outcomes at long term follow-up compared to KPro implantation after corneal transplantation.28, 31, 32 In these studies, there was also no significant difference between retention time and postoperative complications between these two groups.28, 31, 32 Based on our data and supported by the aforementioned studies, patients with high-grade AAK should be considered for primary KPro implantation. Previous studies reported various improvements in final visual acuity, ranging from 43.5% to 87.5%, while the KPro retention rate ranged from 76.9% to 100%.14, 15, 33, 34 It seems that the discrepancies in reports correspond to differences in follow-up times (from 1.4 to 4.5 years). In our study, 60% of eyes experienced improvement of visual acuity following primary KPro implantation. Admittedly, these results are affected by a selection bias because higher stage AAK is designated to have KPro, leaving these patients with the largest potential for improvement. Although the Boston Keratoprosthesis has advantages, there are also significant associated complications such as retroprosthetic membrane, glaucoma, corneal melt, and endophthalmitis.
The results of this study show that nine (40%) of the 22 KPro cases developed retroprosthetic membranes, and four (18.2%) had KPro extrusion. Due to the higher risk of complications that may lead to vision loss in KPro patients, we reserve this procedure for the more advanced stages of AAK in which other forms of therapy are likely to fail. Shah et al reported that twenty-six percent of aniridic eyes (12 out of 46 eyes) experienced new onset or progression of glaucoma after KPro implantation, 6 of which required glaucoma device implantation.34 Both newly diagnosed and progression of glaucoma after KPro implantation should be closely monitored and managed. Recent studies suggest that patients with moderate to advanced glaucoma undergoing KPro should also receive surgical intervention prior to, at the same time, or within three months after implantation. This led to significantly better visual acuity at 3 years without an associated increase in postoperative complications.35, 36 In our institution, all aniridic patients without a functioning glaucoma valve receive glaucoma drainage implant surgery prior or at the time of KPro surgery. With careful monitoring and proper interventions, many of the KPro complications can be successfully managed.
Conclusion
Analysis of visual acuities and AAK stage-based treatments over a long follow-up period in patients with congenital aniridia led to the development of a data-supported algorithm for management of aniridic-associated keratopathy. In early stage AAK (Stages I and II), patients are best served by medical management and follow-up. With more severe presentations (Stages III, IV and V), LSCT and Boston KPro should be considered according to the clinical staging and evaluation of each individual eye (Figure 2). After performing advanced corneal surgeries, postoperative management is of paramount importance for long term success.
Supplementary Material
Figure 3:
Recommended algorithm developed based on the results of this study for the management of aniridia-associated keratopathy according to the stage of corneal pathology. Stage I-stage II is defined as abnormal peripheral epithelium with centripetal extension of changes. Stage III/stage IV (with low risk of limbal graft failure and able to tolerate systemic immunosuppression) is defined as central corneal epithelial changes with peripheral superficial neovascularization and limbal stem cell deficiency limited mostly to the surface. Stage IV (with high risk of limbal graft failure or unable to tolerate systemic immunosuppression)/stage V is defined as limbal stem cell deficiency with abnormal epithelium in entire cornea, subepithelial fibrosis, deep and permanent stromal scarring and/or significant endothelial dysfunction.
Acknowledgement
a. Funding/Support:
This work was supported by R01 EY024349 (ARD) and Core Grant for Vision Research EY01792 (MIR) from NEI/NIH; unrestricted grant to the department from Research to Prevent Blindness. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Biography
Ali R. Djalilian, MD, is a Professor of Ophthalmology at the University of Illinois Eye and Ear Infirmary, Chicago, Illinois. His clinical and research interests are in medical and surgical management of ocular surface disease including limbal stem cell deficiency and high risk keratoplasty.
Ghasem Yazdanpanah, MD, MPH is a research fellow and a bioengineering PhD candidate in University of Illinois Eye and Ear Infirmary. His clinical and research interest is ocular and orbital reconstruction by developing and applying translational strategies. His current research is focused on ocular surface and corneal stromal regeneration utilizing novel tissue engineering and drug delivery approaches such as biomaterial fabrication, additive bio-manufacturing and developing sustain-drug-release devices.
Aniridia-Associated Keratopathy (AAK), due to progressive loss of the limbal stem cells, is one of the major causes of vision loss in congenital aniridia. In this study, using long-term follow-up data in a referral center, the medical and surgical management of AAK and the outcomes are provided. Medical management is appropriate for early stages of AAK. Limbal stem cell transplantation and Boston Keratoprosthesis are the main surgical options for later stages of AAK.
Footnotes
b. Financial Disclosures:
Ali Djalilian has consulted for Novartis, Combangio, Dompé.
Mark I. Rosenblatt has consulted for Laurel Therapeutics, Silk Tears, Roche, AbbVie, Sarentis Therapeutics, PanOptica.
Elmer Y Tu has consulted for Kedrion, and Okogen.
Maria S Cortina has consulted for Eversight Eye bank, and Gore.
The following authors have no financial disclosures: Ghasem Yazdanpanah, Kelley J. Bohm, Omar M. Hassan, Faris I. Karas, Abdelrahman M. Elhusseiny, Manachai Nonpassopon, Muanploy Niparugs, and Joel Sugar.
All authors attest that they meet the current ICMJE criteria for authorship.
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Lee HJ, Colby KA. A review of the clinical and genetic aspects of aniridia. Semin Ophthalmol 2013;28(5–6):306–12. [DOI] [PubMed] [Google Scholar]
- 2.Eden U, Riise R, Tornqvist K. Corneal involvement in congenital aniridia. Cornea 2010;29(10):1096–102. [DOI] [PubMed] [Google Scholar]
- 3.Mayer KL, Nordlund ML, Schwartz GS, Holland EJ. Keratopathy in congenital aniridia. Ocul Surf 2003;1(2):74–9. [DOI] [PubMed] [Google Scholar]
- 4.Ramaesh T, Collinson JM, Ramaesh K, Kaufman MH, West JD, Dhillon B. Corneal abnormalities in Pax6+/− small eye mice mimic human aniridia-related keratopathy. Invest Ophthalmol Vis Sci 2003;44(5):1871–8. [DOI] [PubMed] [Google Scholar]
- 5.Eden U, Fagerholm P, Danyali R, Lagali N. Pathologic epithelial and anterior corneal nerve morphology in early-stage congenital aniridic keratopathy. Ophthalmology 2012;119(9):1803–10. [DOI] [PubMed] [Google Scholar]
- 6.Davis J, Duncan MK, Robison WG Jr., Piatigorsky J. Requirement for Pax6 in corneal morphogenesis: a role in adhesion. J Cell Sci 2003;116(Pt 11):2157–67. [DOI] [PubMed] [Google Scholar]
- 7.Ou J, Walczysko P, Kucerova R, et al. Chronic wound state exacerbated by oxidative stress in Pax6+/− aniridia-related keratopathy. J Pathol 2008;215(4):421–30. [DOI] [PubMed] [Google Scholar]
- 8.Collinson JM, Chanas SA, Hill RE, West JD. Corneal development, limbal stem cell function, and corneal epithelial cell migration in the Pax6(+/−) mouse. Invest Ophthalmol Vis Sci 2004;45(4):1101–8. [DOI] [PubMed] [Google Scholar]
- 9.Ramaesh T, Ramaesh K, Leask R, et al. Increased apoptosis and abnormal wound-healing responses in the heterozygous Pax6+/− mouse cornea. Invest Ophthalmol Vis Sci 2006;47(5):1911–7. [DOI] [PubMed] [Google Scholar]
- 10.Holland EJ, Djalilian AR, Schwartz GS. Management of aniridic keratopathy with keratolimbal allograft: a limbal stem cell transplantation technique. Ophthalmology 2003;110(1):125–30. [DOI] [PubMed] [Google Scholar]
- 11.Nishida K, Kinoshita S, Ohashi Y, Kuwayama Y, Yamamoto S. Ocular surface abnormalities in aniridia. Am J Ophthalmol 1995;120(3):368–75. [DOI] [PubMed] [Google Scholar]
- 12.Jabbehdari S, Rafii AB, Yazdanpanah G, Hamrah P, Holland EJ, Djalilian AR. Update on the Management of High-Risk Penetrating Keratoplasty. Curr Ophthalmol Rep 2017;5(1):38–48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kremer I, Rajpal RK, Rapuano CJ, Cohen EJ, Laibson PR. Results of penetrating keratoplasty in aniridia. Am J Ophthalmol 1993;115(3):317–20. [DOI] [PubMed] [Google Scholar]
- 14.Rixen JJ, Cohen AW, Kitzmann AS, Wagoner MD, Goins KM. Treatment of aniridia with Boston type I keratoprosthesis. Cornea 2013;32(7):947–50. [DOI] [PubMed] [Google Scholar]
- 15.Hassanaly SI, Talajic JC, Harissi-Dagher M. Outcomes following Boston type 1 keratoprosthesis implantation in aniridia patients at the University of Montreal. Am J Ophthalmol 2014;158(2):270–276 e1. [DOI] [PubMed] [Google Scholar]
- 16.Hingorani M, Hanson I, van Heyningen V. Aniridia. Eur J Hum Genet 2012;20(10):1011–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Ghahari E, Sharfi D, Holland EJ, Djalilian AR. Management of Limbal Stem Cell Deficiency In: Djalilian A, editor. Ocular Surface Disease: Springer, Cham, 2018:281–306. [Google Scholar]
- 18.Gregori NZ, Feuer W, Rosenfeld PJ. Novel method for analyzing snellen visual acuity measurements. Retina 2010;30(7):1046–50. [DOI] [PubMed] [Google Scholar]
- 19.Gramer E, Reiter C, Gramer G. Glaucoma and frequency of ocular and general diseases in 30 patients with aniridia: a clinical study. Eur J Ophthalmol 2012;22(1):104–10. [DOI] [PubMed] [Google Scholar]
- 20.Jastaneiah S, Al-Rajhi AA. Association of aniridia and dry eyes. Ophthalmology 2005;112(9):1535–40. [DOI] [PubMed] [Google Scholar]
- 21.Baradaran-Rafii A, Eslani M, Djalillian AR. Complications of keratolimbal allograft surgery. Cornea 2013;32(5):561–6. [DOI] [PubMed] [Google Scholar]
- 22.Cheung AY, Holland EJ. Keratolimbal allograft. Curr Opin Ophthalmol 2017;28(4):377–381. [DOI] [PubMed] [Google Scholar]
- 23.Han ES, Wee WR, Lee JH, Kim MK. Long-term outcome and prognostic factor analysis for keratolimbal allografts. Graefes Arch Clin Exp Ophthalmol 2011;249(11):1697–704. [DOI] [PubMed] [Google Scholar]
- 24.Ilari L, Daya SM. Long-term outcomes of keratolimbal allograft for the treatment of severe ocular surface disorders. Ophthalmology 2002;109(7):1278–84. [DOI] [PubMed] [Google Scholar]
- 25.Liang L, Sheha H, Tseng SC. Long-term outcomes of keratolimbal allograft for total limbal stem cell deficiency using combined immunosuppressive agents and correction of ocular surface deficits. Arch Ophthalmol 2009;127(11):1428–34. [DOI] [PubMed] [Google Scholar]
- 26.Movahedan A, Cheung AY, Eslani M, Mogilishetty G, Govil A, Holland EJ. Long-term Outcomes of Ocular Surface Stem Cell Allograft Transplantation. Am J Ophthalmol 2017;184(97–107. [DOI] [PubMed] [Google Scholar]
- 27.Solomon A, Ellies P, Anderson DF, et al. Long-term outcome of keratolimbal allograft with or without penetrating keratoplasty for total limbal stem cell deficiency. Ophthalmology 2002;109(6):1159–66. [DOI] [PubMed] [Google Scholar]
- 28.Kang KB, Karas FI, Rai R, et al. Five year outcomes of Boston type I keratoprosthesis as primary versus secondary penetrating corneal procedure in a matched case control study. PLoS One 2018;13(2):e0192381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Chang HY, Luo ZK, Chodosh J, Dohlman CH, Colby KA. Primary implantation of type I Boston keratoprosthesis in nonautoimmune corneal diseases. Cornea 2015;34(3):264–70. [DOI] [PubMed] [Google Scholar]
- 30.Aravena C, Bozkurt TK, Yu F, Aldave AJ. Long-Term Outcomes of the Boston Type I Keratoprosthesis in the Management of Corneal Limbal Stem Cell Deficiency. Cornea 2016;35(9):1156–64. [DOI] [PubMed] [Google Scholar]
- 31.Driver TH, Aravena C, Duong HNV, et al. Outcomes of the Boston Type I Keratoprosthesis as the Primary Penetrating Corneal Procedure. Cornea 2018;37(11):1400–1407. [DOI] [PubMed] [Google Scholar]
- 32.Fadous R, Levallois-Gignac S, Vaillancourt L, Robert MC, Harissi-Dagher M. The Boston Keratoprosthesis type 1 as primary penetrating corneal procedure. Br J Ophthalmol 2015;99(12):1664–8. [DOI] [PubMed] [Google Scholar]
- 33.Akpek EK, Harissi-Dagher M, Petrarca R, et al. Outcomes of Boston keratoprosthesis in aniridia: a retrospective multicenter study. Am J Ophthalmol 2007;144(2):227–231. [DOI] [PubMed] [Google Scholar]
- 34.Shah KJ, Cheung AY, Holland EJ. Intermediate-Term and Long-Term Outcomes With the Boston Type 1 Keratoprosthesis in Aniridia. Cornea 2018;37(1):11–14. [DOI] [PubMed] [Google Scholar]
- 35.Lenis TL, Chiu SY, Law SK, Yu F, Aldave AJ. Safety of Concurrent Boston Type I Keratoprosthesis and Glaucoma Drainage Device Implantation. Ophthalmology 2017;124(1):12–19. [DOI] [PubMed] [Google Scholar]
- 36.Lin M, Bhatt A, Haider A, et al. Vision retention in early versus delayed glaucoma surgical intervention in patients with Boston Keratoprosthesis type 1. PLoS One 2017;12(8):e0182190. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.