INTRODUCTION
The South has an excessive HIV burden and is now the epicenter of HIV in the U.S.1–3 Despite being home to only one-third of the U.S. population, 45% of all people living with HIV are in the South.3 Under- and late HIV testing are key contributors to the ongoing HIV epidemic in the South.4 In Houston, where this study was conducted, 19% of those living with HIV are unaware (Amber L. Harbolt, personal communication, April 1, 2019). Further, one in five people diagnosed with HIV in Houston receive an AIDS diagnosis within 3 months, highlighting late diagnoses following years of missed testing opportunities.5 Rates of late HIV diagnoses in Houston are particularly high for African American and Hispanic patients.6 Earlier HIV diagnosis benefits both the community and the individual. The sooner patients are diagnosed and put on antiretroviral therapy (ART), the better their health outcomes. Early diagnosis and ART treatment also has been proven to reduce onward HIV transmission.7–11
Because of the benefits of routine HIV testing and evidence that it was being underperformed – only 37% of US adults in 2005 reported having been tested12 – the U.S. Centers for Disease Control and Prevention (CDC) issued updated HIV screening recommendations in 2006. Specifically, the CDC recommended routine HIV screening for all patients aged 13-64 unless HIV prevalence is documented to be under 0.1% in the patient population.13 In 2008, because of the high HIV prevalence in Houston,14 the Harris Health System (Harris Health), Houston’s largest public safety net healthcare system, adopted the new HIV screening recommendations and implemented its own local initiative: Routine Universal Screening for HIV (RUSH). The goal of the RUSH program was to gradually test all Harris Health patients for HIV and link those diagnosed with HIV to appropriate care. The program implemented an opt-out model, testing all patients ages 16 and older in need of a blood draw, unless they specified that they did not wish to be tested for HIV. At emergency centers, HIV tests were pre-selected in standard order sets; at clinics, providers were encouraged to order HIV tests, received annual trainings, and were given feedback on their HIV testing performance. Patients were informed of the RUSH program in the consent form for medical care given at the time of check-in. Additionally, signs describing the RUSH program were displayed in the registration, waiting, phlebotomy, and treatment areas. The RUSH program began in the two Harris Health hospital-based emergency centers in late 2008 and early 2009 and then gradually expanded to all 15 Harris Health outpatient clinics. Notably, in 2013, after the RUSH program had already launched, another national agency, the U.S. Preventive Services Task Force (USPSTF), gave a Grade A recommendation for routine HIV screening for all patients aged 15-65.15
Many studies to date have focused on opt-out HIV testing initiatives within emergency departments or other limited clinical sites; these studies have not explicitly compared the impact of national HIV testing guidelines relative to their local initiatives.16–18 The objective of this study was to review HIV testing in Harris Health from 2004 to 2016 to determine if HIV testing among the outpatient population served by Harris Health was impacted by implementation of the system-wide RUSH program, national HIV screening recommendations, or both.
METHODS
Setting
This study took place in Harris Health, which provides 165,000 emergency visits and 1.9 million outpatient clinic visits per year to 300,000 unique patients.19,20 The majority of Harris Health patients are African American (25.4%) or Hispanic (58.9%) and uninsured (60.2%).21
Data Collection
We abstracted HIV testing data for 2004 to 2016 from the electronic medical record (EMR) for all outpatient clinic patients ages 18-64. This date range was selected to include HIV testing for two years prior to the 2006 CDC HIV screening recommendations through 2016, which is three years following the 2013 USPSTF HIV screening recommendations. The data abstracted were HIV test date and past testing history in Harris Health back to 2002, the earliest laboratory data imported into the EMR.
The study was approved by the Baylor College of Medicine Institutional Review Board and the Harris Health System Office of Research & Sponsored Programs. A waiver of individual consent was granted.
Analysis
Statistical analyses were conducted using Stata 12 (Statacorp, College Station, TX). First, we extracted the number of HIV tests performed each year. Next, we calculated HIV testing rates for each year by determining what proportion of patients seen at the outpatient clinics were tested (1) during that year (annual testing rate) and (2) at any time previously in Harris Health (ever tested rate). We used a series of spline analyses to determine if implementation of the RUSH program in emergency centers or outpatient clinics or release of CDC or USPSTF screening recommendations – heretofore referred to as “milestones” – influenced HIV testing. This type of linear regression analysis is also frequently referred to as an interrupted time series analysis in the literature.22,23 The annual testing rates were split into two groups (prior to and after each milestone) and a linear regression was fit with terms for the pre-intervention slope, the post-intervention slope, and the difference between trend lines for the year of the intervention itself. We then identified the milestone(s) that led to a statistically significant difference in the pre-versus post-milestone slopes.
RESULTS
The number of Harris Heath outpatient clinic patients who were tested for HIV each year increased across all sites during the study period, starting with 12,078 patients in 2004 and rising to 77,567 by 2016. The number of unique patients visiting Harris Health outpatient clinics also increased, from 114,000 in 2004 to 219,000. Except for a transient decrease in 2015, we found that annual testing rates increased from 10.5% in 2004 to 35.4% in 2016. Additionally, ever tested rates increased each year, from 15.3% in 2004 to 75.9% in 2016 (see Fig. 1).
FIGURE 1. HIV Testing for Harris Health Outpatient Clinic Patients, Houston, TX, 2004-2016.
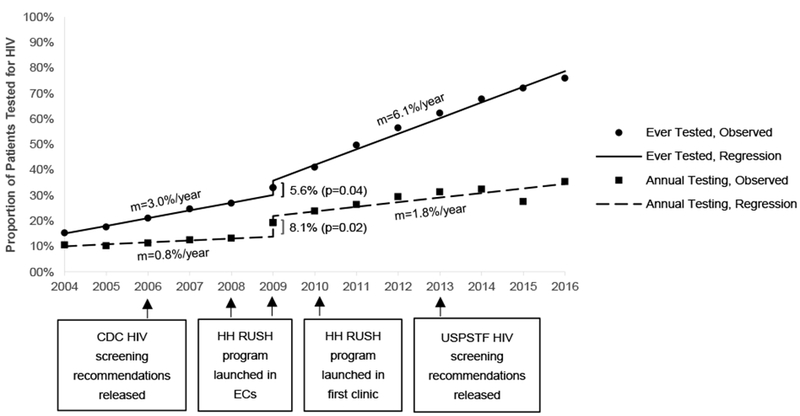
Proportion of Harris Health (HH) outpatient clinic patients who received an HIV test in a given year (annual testing) or at any time since 2002 (ever tested). Data fitted with linear regression models containing splines. The included splines reflect the only significant jumps in the annual HIV testing rate and ever HIV tested rate, which were observed in 2009, coinciding with the implementation of the RUSH program in the emergency centers. m=slope; CDC=Centers for Disease Control and Prevention; HIV=Human Immunodeficiency Virus; RUSH=Routine Universal Screening for HIV; EC=Emergency Center; USPSTF=U.S. Preventive Services Task Force
We next examined whether HIV testing changed following any of the milestones. The spline analysis revealed a significant jump in the annual HIV testing rate in 2009 (8.1%, P=0.019), coinciding with the implementation of the RUSH program in the emergency centers. No significant increases in annual HIV testing rates were observed corresponding with any other milestones. The spline analysis found that the ever tested rate also had a significant jump of 5.6% in 2009 (P=0.035). No significant increases in ever HIV tested rates were observed corresponding with any other milestones. Accordingly, Figure 1, which displays the proportion of Harris Health outpatient clinic patients who received an HIV test in a given year or at any time since 2002, only includes the regressions containing a spline at 2009, the year in which a significant jump in both measures of HIV testing was observed.
DISCUSSION
There have been many missed opportunities for HIV testing in healthcare settings – the primary site of HIV testing in the United States.24 In Texas, the majority of patients who have never been tested have had a routine doctor visit within the past year, indicating the importance of promoting routine HIV testing within healthcare settings.25
Our study found significantly increased HIV annual testing and ever tested rates for Harris Health patients aged 18-64 from 2004 to 2016. Among Harris Health outpatient clinic patients, rates of annual HIV testing more than tripled (10.5% to 35.4%), and rates of ever HIV tested more than quintupled (15.3% to 75.9%). In contrast, national rates of ever receiving an HIV test remained relatively constant over that time period, suggesting that the increase in testing in Harris Health was the result of local changes.26 It is notable that there was a decrease in the annual testing rate in 2015. This is likely due to reorganization and re-staffing within Harris Health, further highlighting the impact of local policy and procedures on testing rates. Our previous work in our Harris Health System has shown that a disruption in local procedures can adversely impact HIV testing rates.27
A limitation of this study is the potential that HIV testing was influenced by factors outside of the local RUSH program. It is possible that during the 2004-2016 time period other city, county, state, or national initiatives may have increased the acceptability of HIV testing among patients or the frequency with which providers offered HIV testing. Future studies could include a comparator health care system in an attempt to discern this possibility.
The greatest annual increase in HIV testing rates was seen in 2009 after the implementation of the RUSH program in emergency centers, suggesting that the program may have been causal in the increased HIV testing. In contrast, there was no significant increase in rates after the implementation of RUSH in clinics, likely because implementation occurred over an extended period of time. Significant changes in HIV testing rates were not apparent after the implementation of the CDC and USPSTF recommendations in 2006 and 2013, respectively. Our data demonstrate the importance of supplementing national recommendations with local programmatic and policy changes driven by local healthcare system leadership, a finding that should inform future practice. While this study showed a significant increase in HIV testing over time, especially after the implementation of our local RUSH program, future research should examine ongoing barriers to achieving universal HIV testing. This may be particularly important for populations facing HIV-related health inequities who rely on safety net healthcare services and are in urgent need of HIV testing.
Acknowledgments
Sources of Support: The HIV-related work was supported in part by the National Institute of Mental Health of the National Institutes of Health under Award Number K23MH094235 (Principal Investigator: Arya). This work was also supported in part by the Center for Innovations in Quality, Effectiveness and Safety (#CIN 13-413) of the Michael E. DeBakey Veterans Affairs Medical Center in Houston. The Harris Health RUSH program was supported by the Gilead HIV Focus Program, Texas Dept of State Health Services (2011-0351783, D-11-00102), and the CDC (PS07-768, PS10-10138, PS12-1201, PS07-768, PS10-1001, PS04-012).
Footnotes
Meetings at which parts of the data were presented: National Summit on HCV and HIV Diagnosis, Prevention, and Access to Care in Arlington, VA on June 4-6, 2015
Conflicts of Interest: The authors have no conflicts of interest or financial conflicts to disclose.
Contributor Information
Monisha Arya, Baylor College of Medicine, and Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center, Houston, TX.
Rachel Eileen Marren, School of Public Health, University of Washington, Seattle, WA.
Haley Gilbertson Marek, Baylor College of Medicine, Houston, TX.
Siavash Pasalar, Harris Health System, Houston, TX.
Vagish Hemmige, Baylor College of Medicine, Houston, TX.
Thomas P. Giordano, Baylor College of Medicine, and Center for Innovations in Quality, Effectiveness and Safety, Michael E. DeBakey VA Medical Center, Houston, TX.
REFERENCES
- 1.Reif SS, Whetten K, Wilson ER, et al. HIV/AIDS in the Southern USA: A disproportionate epidemic. AIDS Care. 2014;26(3):351–359. doi: 10.1080/09540121.2013.824535 [DOI] [PubMed] [Google Scholar]
- 2.Hess KL, Hu X, Lansky A, Mermin J, Hall HI. Lifetime risk of a diagnosis of HIV infection in the United States. Ann Epidemiol. 2017;27(4):238–243. doi: 10.1016/j.annepidem.2017.02.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Centers for Disease Control and Prevention (CDC). HIV in the United States by Geography. https://www.cdc.gov/hiv/pdf/statistics/cdc-hiv-geographic-distribution.pdf. Published November 2017. Accessed April 14, 2019.
- 4.Reif SR, Safley D, McAllaster C. A Closer Look: Deep South Has the Highest HIV-Related Death Rates in the United States. Southern HIV/AIDS Strategy Initiative; 2015. https://southernaids.files.wordpress.com/2011/10/a-closer-look-deep-south-has-the-highest-hiv-related-death-rates-in-the-united-states-final.pdf Accessed April 14, 2019.
- 5.Local Data: Houston. AIDSVu. https://aidsvu.org/state/texas/houston/ Published 2016. Accessed March 29, 2019.
- 6.Houston Health Department. HIV Infection in Houston: An Epidemiological Profile, 2010 - 2014. Houston, TX; 2015. http://www.houstontx.gov/health/HIV-STD/HI_%20Epi_Profile_20160506_this.pdf Accessed March 29, 2019. [Google Scholar]
- 7.Marks G, Crepaz N, Senterfitt J, Janssen R. Meta-Analysis of High-Risk Sexual Behavior in Persons Aware and Unaware They are Infected With HIV in the United States. Jaids J Acquir Immune Defic Syndr. 2005;39(4):446–453. doi: 10.1097/01.qai.0000151079.33935.79 [DOI] [PubMed] [Google Scholar]
- 8.Hall H, Holtgrave D, Maulsby C. HIV transmission rates from persons living with HIV who are aware and unaware of their infection. AIDS. 2012;26(7):893–896. doi: 10.1097/QAD.0b013e328351f73f [DOI] [PubMed] [Google Scholar]
- 9.Colucci A, Balzano R, Camoni L, et al. Characteristics and behaviors in a sample of patients unaware of their infection until AIDS diagnosis in Italy: a cross-sectional study. AIDS Care. 2011;23(9):1067–1075. doi: 10.1080/09540121.2011.554525 [DOI] [PubMed] [Google Scholar]
- 10.Steward WT, Remien RH, Higgins JA, et al. Behavior Change Following Diagnosis with Acute/Early HIV Infection—A Move to Serosorting with Other HIV-Infected Individuals. The NIMH Multisite Acute HIV Infection Study: III. AIDS Behav. 2009;13(6):1054–1060. doi: 10.1007/s10461-009-9582-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Cohen MS, Chen YQ, McCauley M, et al. Prevention of HIV-1 Infection with Early Antiretroviral Therapy. N Engl J Med. 2011;365(6):493–505. doi: 10.1056/NEJMoa1105243 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2006:97 https://www.cdc.gov/brfss/annual_data/2006/pdf/codebook_06.pdf Accessed April 14, 2019. [Google Scholar]
- 13.Branson BM, Handsfield HH, Lampe MA, et al. Revised Recommendations for HIV Testing of Adults, Adolescents, and Pregnant Women in Health-Care Settings. MMWR. 2006;55(14):1–17. [PubMed] [Google Scholar]
- 14.Stein R, Xu S, Marano M, et al. HIV Testing, Linkage to HIV Medical Care, and Interviews for Partner Services Among Women — 61 Health Department Jurisdictions, United States, Puerto Rico, and the U.S. Virgin Islands, 2015. MMWR Morb Mortal Wkly Rep. 2017;66(41):1100–1104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Moyer VA. Screening for HIV: U.S. Preventive Services Task Force Recommendation Statement. Ann Intern Med. 2013;159(1):51–60. [DOI] [PubMed] [Google Scholar]
- 16.Henriquez‐Camacho C, Villafuerte‐Gutierrez P, Pérez‐Molina JA, et al. Opt-out screening strategy for HIV infection among patients attending emergency departments: systematic review and meta-analysis. HIV Med. 2017;18(6):419–429. [DOI] [PubMed] [Google Scholar]
- 17.Lin J, Mauntel-Medici C, Heinert S, et al. Harnessing the Power of the Electronic Medical Record to Facilitate an Opt-Out HIV Screening Program in an Urban Academic Emergency Department. JPHMP. 2017;23(3):264–268. [DOI] [PubMed] [Google Scholar]
- 18.Crumby NS, Arrezola E, Brown EH, Brazzeal A, et al. Experiences Implementing a Routine HIV Screening Program in Two Federally Qualified Health Centers in the Southern United States. Public Health Rep. 2016;131(Suppl 1):21–29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Harris Health System. Harris Health System 2017 Report to the Community. Houston, TX: https://www.harrishealth.org/SiteCollectionDocuments/annual-reports/ar-2017.pdf Accessed March 29, 2019. [Google Scholar]
- 20.Harris Health System. Harris Health System Bridge to 2020: Strategic Plan 2018-2020. Houston, TX: https://www.harrishealth.org/SiteCollectionDocuments/financials/strategic-plan-booklet-final.pdf Accessed March 29, 2019. [Google Scholar]
- 21.Harris Health System. Facts and Figures. Harris Health; https://www.harrishealth.org/about-us-hh/who-we-are/Pages/statistics.aspx Accessed March 29, 2019. [Google Scholar]
- 22.Nicholas G R, Goldsmith J. Using splines in regression. Nicholas Reich. http://nickreich.github.io/applied-regression-2016/assets/lectures/lecture10-splines/lecture10-splines.pdf. Published 2016. Accessed September 7, 2019.
- 23.Kontopantelis E, Doran T, Springate DA, et al. Regression based quasi-experimental approach when randomisation is not an option: interrupted time series analysis. BMJ. 2015;350:h2750. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Centers for Disease Control and Prevention (CDC). Behavioral Risk Factor Surveillance System Survey Data. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention; 2015. https://www.cdc.gov/brfss/annual_data/2015/pdf/codebook15_llcp.pdf Accessed April 14, 2019.
- 25.Van Handel M, Dietz P. Missed Opportunities for HIV Testing During Routine Doctor Visits, BRFSS, 2011-2013. In: Boston, MA; 2016. http://www.croiconference.org/sessions/missed-opportunities-hiv-testing-during-routine-doctor-visits-brfss-2011-2013 Accessed March 29, 2019. [Google Scholar]
- 26.Van Handel M, Branson BM. Monitoring HIV Testing in the United States: Consequences of Methodology Changes to National Surveys. Chuang J-H, ed. PLoS ONE. 2015;10(4). [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Medford-Davis LN, Yang K, Pasalar S, et al. Unintended adverse consequences of electronic health record introduction to a mature universal HIV screening program. AIDS Care. 2016;28(5):566–573. [DOI] [PubMed] [Google Scholar]


