Abstract
Purpose
The aim of this retrospective study was to evaluate the correlation between D-dimer levels in positive thromboembolic thoracic computed tomography (CT) with the diameter of the pulmonary trunk and to study the relation between the D-dimer and the uni- or bilateralism of the lesions and the presence of pulmonal trunk involvement. We also analysed gender-specific differences in patients with and without dilatation of the pulmonal trunk.
Material and methods
A total of 100 acute care patients (50 men and 50 women) with positive thromboembolic multiple detector computed tomography of the thorax, performed on two modern CT scanners, were retrospectively studied. All thoracic CTs were evaluated by two expert radiologists, with attention paid to the diameter of the pulmonary trunk and the correlation of D-dimer level with the uni-or bilateralism of the lesions. We also analysed sex-specific correlations. All patients underwent multislice computed tomography-examination after applying 70 ml iodinated non-ionic contrast media. Graphpad Prism 8.1.1 software was used for statistical data.
Results
The “strongest” weak correlation resulted between D-dimer levels and the axial diameter of the pulmonal trunk. Considering the correlation between the axial diameter of the pulmonal trunk and gender-related distributions, we found that female patients had higher axial diameters than men. Another weak relationship, almost zero, was found between the D-dimer level and gender. Regarding the correlation between the uni- or bilateralism of thromboembolism and the D-dimer levels, we also found a weak correlation.
Conclusions
This retrospective study showed that D-dimer levels, the diameter of the pulmonal trunk, the location, and gender-related distributions have almost no correlation and are not significantly predictive in imaging.
Keywords: mediastinum, acute pulmonary embolism, multi detector computed tomography (MDCT)
Introduction
Acute pulmonal embolism (PE) is a very common diagnosis in acute care and can cause diverse symptoms, ranging from mild respiratory distress to sudden death. In acute care units the annual incidence rate is from 0.2 to 0.8 /1000 [1,2]. Today, pulmonary angio-computed tomography (CT) after contrast administration is the gold standard method. The aim of the diagnosis of acute pulmonary embolism is to have the dose of the contrast agent adapted to the body weight, with the associated improved resolution of the smaller lung vessels [3].
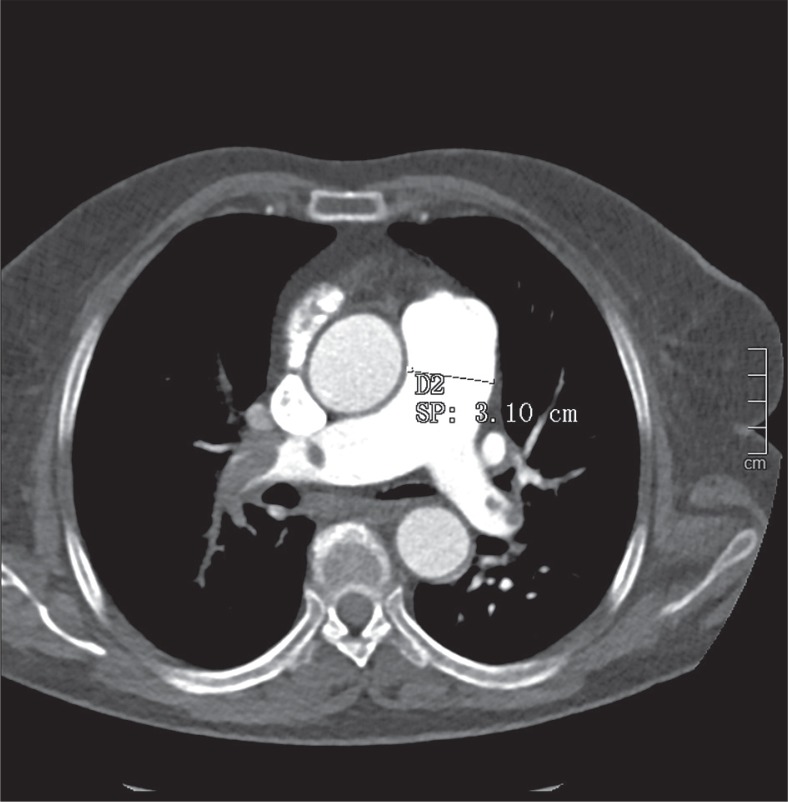
In this retrospective single centre study, we tried to ascertain if there is a correlation between D-dimer levels in positive acute thromboembolic thoracic CT and the axial diameter of the pulmonary trunk (Figure 1), and if there is a cut-off D-dimer level regarding the uni-or bilateralism of the lesions and with the presence of pulmonal trunk involvement.
Figure 1.
An example of measuring the pulmonal trunk
Today’s clinicians use diagnostic scores to identify risk stratification like the classic Wells score (WS), modified WS, simplified WS, revised Geneva score (GS), simplified GS, and the YEARS score. In our Institution clinicians use clinical signs and measurement of the D-dimer level in peripheric blood to confirm the suspicion of acute PE. D-dimer is a fibrin cleavage product that results from cleavage of cross-linked fibrin by factor XIIIa. Its low-level plasma expression expresses the control of haemostasis by coagulation factors and fibrinolytic system. Increased D-dimer values serve as activation markers of haemostasis, a condition that is present in any thrombotic process. Normal values preclude significant activation. The exact quantification of D-dimer levels has an important role in guiding therapy [4]. But which levels of D-dimer are pathologic? The D-dimer level has a low specificity but a very high sensitivity. It can be elevated in many other pathologies, after surgery, but also after bone fractures or infections. Many previous studies have shown that the D-dimer test is highly sensitive (> 95%) in acute deep venous thrombosis or pulmonary embolism [5]. In our hospital levels under 500 ng/ml fibrinogen equivalent units (FEU) are considered normal.
Another key in the pathophysiology of acute PE is the dilatation of the main pulmonal trunk (MPA). In a study from 2012 [6] the authors found no correlation in women between age and MPA in a healthy reference group. But which clinical significance has the dilatation of the MPA? There are many other causes of MPA dilatation, such as pulmonary arterial hypertension, Eisenmenger syndrome, high altitude, congenital cardiac shunting, pulmonal valvular stenosis, congenital, infectious, rheumatologic/vasculitis, connective tissue diseases, and idiopathic or traumatic causes. The most common cause is pulmonary hypertension (PH). Increased intrapulmonary pressures lead to vascular thickening and dilation with increased vascular wall shear stress, as well as increased collagen and elastin deposition in the adventitia layer of the pulmonal trunk. The continuous high pressure in the MPA causes cell activation and vascular remodelling in hypoxia-induced PH [7]. Another key in understanding pulmonal thromboembolism is to analyse the correlation between MPA-dilatation and the side involvement, i.e. if there is a predilection of involving the right or the left side in trunk dilation and non-trunk dilatation.
Material and methods
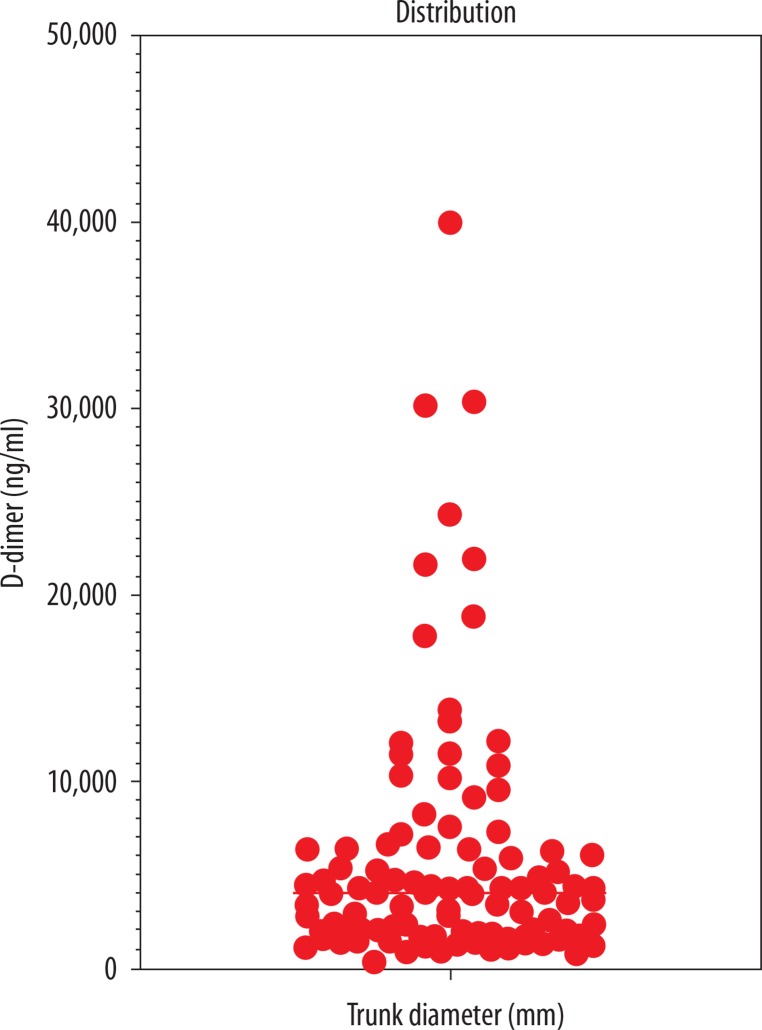
In this retrospective study, we considered 100 patients who underwent thoracic computed tomography angiography (CTA) with contrast administration at our Institution in the period January 2015 – January 2019 after admission to the Emergency Department. All patients presented clinical signs of PE and underwent D-dimer examination levels in acute care. The range of blood D-dimer levels were between 300 and 39.958 ng/ml (Figure 2). The diameter of the main pulmonary artery (MPA) ranged from 21 to 50 mm. We considered a normal reference of 29 mm in men and 27 mm in women [6]. Retrospectively we also analysed whether there were other associated reasons for high D-dimer levels.
Figure 2.
The distribution shows that the most D-dimer levels are in the range under 10,000 ng/ml
All of the authors confirm that the research was performed according to the principles of the Declaration of Helsinki. Informed consent was not obtained.
Imaging protocol
Multiple detector computed tomography (MPCT) scans were performed in our department with two multislice CT-scanners. All the examinations were performed on a dual-source CT scanner (Somatom Definition Flash; Siemens Healthcare, Forchheim, Germany and Somatom Drive; Siemens Healthcare, Forchheim, Germany) with patients lying supine on the table with their arms at the side of their body, with spiral acquisition. Scanning parameters are given in Table 1. Thoracic CTAs were obtained after intravenous administration of 70 ml of 350 mg iodine/ml iodinated contrast material (Iobitridol, Xenetix 350, Guerbet, France) at a flow rate of 4 ml/s, followed by a 50-ml saline flush through an 18-gauge catheter placed in an antecubital vein using an automatic power injector (Medrad Stellant, Bayer); a bolus-tracking technique was adopted, with the region of interest (ROI) placed in the pulmonal trunk (threshold 100 Hounsfield units [HU]). We analysed only axial images with a slice thickness of 1 mm.
Table 1.
Scanning and reconstruction parameters for pulmonal computed tomography angiography
| Factor | SOMATOM definition flash | SOMATOM definition drive |
|---|---|---|
| Scanning technique | Spiral | Spiral |
| Scan direction | Craniocaudal | Craniocaudal |
| kVp | Care kV (ref. kV 120) | Care kV (ref. kV 120) |
| Care-DOSE reference | 170 mA | 150 mA |
| Collimation | 128 × 0.6 mm | 128 × 0.6 mm |
| Rotation time | 0.28 sec | 0.28 sec |
| Pitch | 2.2 | 2.5 |
Interpretation
Two radiologists with approximately 10 years of experience retrospectively analysed the CTA scans, measuring the axial diameter of the pulmonal trunk at level of pulmonal artery bifurcation. We selected this method because of its fast and daily feasibility in routine praxis.
Statistical analysis
All statistical calculations were performed using Graphpad Prism 8.1.1 software. To calculate the correlations, we used Pearson (r) and the Spearman (p) correlation statistic methods.
Results
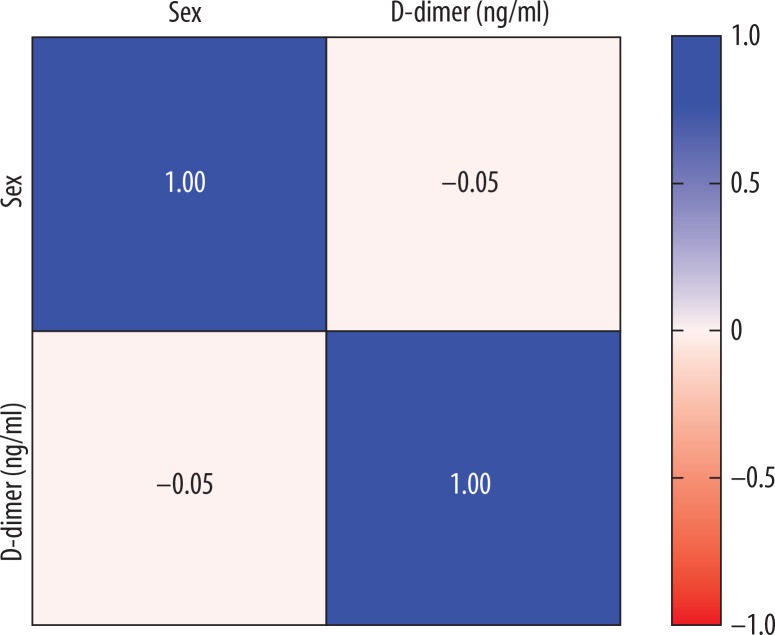
Considering the correlation between D-dimer levels and the axial diameter of the pulmonal trunk, we found a weak correlation, with a Pearson correlation r value of 0.2141 (Table 2). Using the Spearman correlation, we also found a weak value (p = 0.2871). The relationship between the D-dimer level and gender (Figure 3) gave a negative Pearson score of –0.05 (almost zero correlation).
Table 2.
Pearson correlation
| Pearson correlation r | Trunk diameter (mm) vs. D-dimer (ng/ml) |
|---|---|
| r | 0.2141 |
Figure 3.
Correlation between sex and D-dimer levels
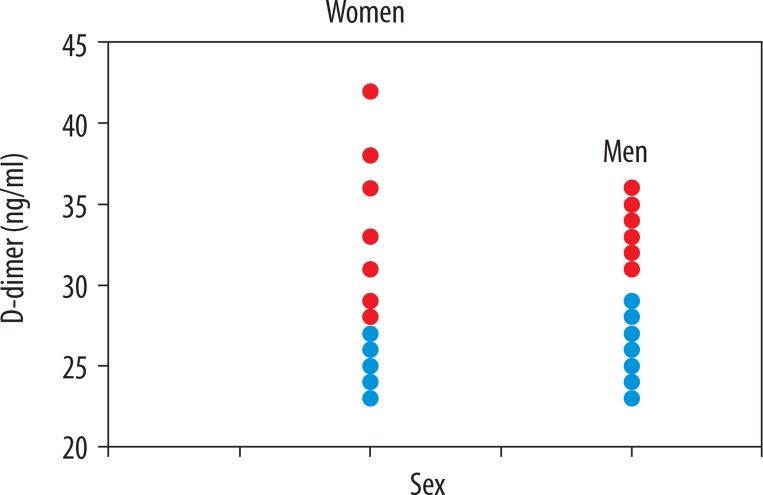
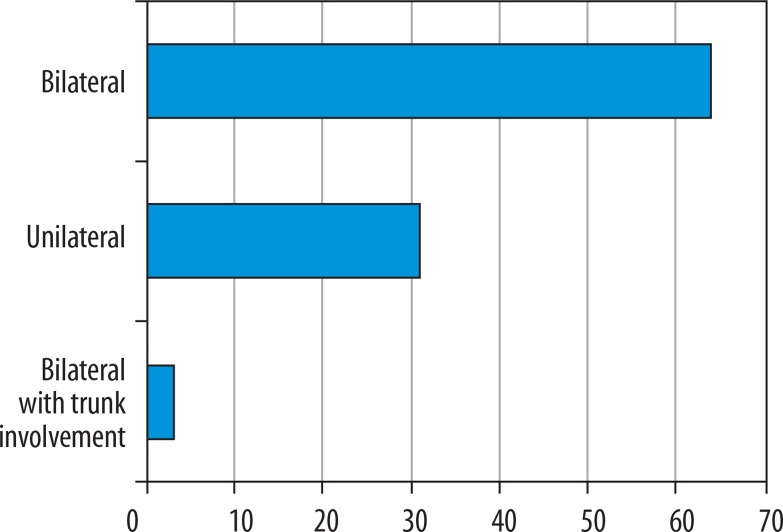
Considering the correlation between the axial diameter of the pulmonal trunk and gender-related distributions (Figure 4), we found that female patients had higher axial diameters (58.3% above 27 mm) in PE versus male patients (46% above 29 mm), which means that women have a higher risk of developing pulmonal hypertension in PE than men [8]. Hormonal influence must be considered in the pathophysiology of trunk dilatation. Considering the correlation between the location (uni- or bilateralism) and the D-dimer levels, we found a weak correlation with a Pearson value of 0.2572 and a Spearman value of 0.2789. 64% of the study population had bilateral pulmonal involvement, 31% had unilateral involvement, and only 3% had a bilateral PE with trunk involvement (Figure 5). In the search for associated diseases or conditions that could lead to an increase in D-dimer levels, we found neoplastic diseases in 11 patients (11%) (four patients with a non-surgically treated lung tumour in chemotherapy and one in immunotherapy, one patient with a cerebral neoplasm in follow-up after surgical therapy and chemotherapy, and five patients with a recent diagnosis of an adenocarcinoma of the colon). In 35 patients (35%) we found a coexisting chronic atrial fibrillation. Twenty-six patients (26%) showed renal pathologies like mild chronic renal failure. In nine patients (9%) there was a chronic congestive cardiac failure. Associated deep vein thrombosis was found in 46 patients (46%). This indicates the presence of coexisting and overlapping conditions in these patients, which also increase D-dimer levels (Tables 3 and 4).
Figure 4.
Correlation between diameter and gender. The red points indicate trunk dilatation, the blue ones indicate the normal range diameters
Figure 5.
Distribution of location of the pulmonal embolism
Table 3.
The study parameters
| D-dimer(ng/ml) | Location | Gender | Trunk-diameter(mm) |
|---|---|---|---|
| 1393 | Bilateral | M | 25 |
| 2238 | Bilateral | F | 38 |
| 5308 | Unilateral | F | 24 |
| 1940 | Bilateral | M | 26 |
| 1981 | Unilateral | M | 24 |
| 2356 | Bilateral | M | 23 |
| 30,388 | Bilateral | F | 25 |
| 5170 | Unilateral | M | 25 |
| 1492 | Bilateral | F | 24 |
| 6415 | Unilateral | F | 26 |
| 4259 | Bilateral | M | 31 |
| 17,803 | Bilateral with trunk involvement | F | 42 |
| 1378 | Unilateral | M | 24 |
| 916 | Bilateral | F | 24 |
| 7597 | Bilateral | F | 33 |
| 1654 | Unilateral | F | 25 |
| 1845 | Bilateral | M | 23 |
| 18,836 | Bilateral | M | 31 |
| 4870 | Bilateral | M | 24 |
| 10,374 | Unilateral | M | 27 |
| 21,965 | Bilateral | F | 26 |
| 13,858 | Unilateral | M | 24 |
| 2040 | Bilateral | F | 27 |
| 1095 | Unilateral | M | 25 |
| 3349 | Bilateral | F | 29 |
| 1315 | Unilateral | F | 24 |
| 11,519 | Unilateral | F | 29 |
| 39,958 | Bilateral | F | 31 |
| 4022 | Bilateral | F | 23 |
| 1511 | Bilateral | F | 24 |
| 1893 | Bilateral | F | 24 |
| 6281 | Bilateral | F | 28 |
| 2376 | Bilateral | M | 24 |
| 30,167 | Bilateral | M | 25 |
| 2052 | Bilateral | M | 25 |
| 2122 | Bilateral | M | 24 |
| 12,174 | Bilateral | F | 26 |
| 13,267 | Bilateral | M | 31 |
| 1286 | Bilateral | F | 31 |
| 6506 | Bilateral | M | 24 |
| 950 | Unilateral | F | 26 |
| 4766 | Bilateral | F | 24 |
| 1602 | Bilateral | F | 25 |
| 12,135 | Bilateral | M | 25 |
| 2410 | Bilateral | M | 33 |
| 1721 | Unilateral | M | 23 |
| 4318 | Bilateral | M | 24 |
| 4518 | Bilateral | M | 24 |
| 1602 | Bilateral | M | 26 |
| 4400 | Bilateral | F | 31 |
| 4649 | Unilateral | F | 28 |
| 6378 | Bilateral | F | 25 |
| 1621 | Bilateral | M | 25 |
| 24,340 | Bilateral | M | 31 |
| 6411 | Bilateral | F | 26 |
| 4318 | Unilateral | M | 32 |
| 4343 | Bilateral | F | 26 |
| 3519 | Unilateral | M | 27 |
| 1386 | Unilateral | M | 28 |
| 3038 | Bilateral | M | 29 |
| 2628 | Bilateral | F | 26 |
| 6109 | Unilateral | F | 27 |
| 1131 | Bilateral | F | 26 |
| 848 | Unilateral | M | 23 |
| 10,890 | Bilateral with trunk involvement | M | 36 |
| 11,451 | Bilateral | M | 33 |
| 1351 | Unilateral | M | 28 |
| 21,662 | Bilateral | M | 26 |
| 6689 | Bilateral | F | 36 |
| 4400 | Unilateral | F | 25 |
| 4400 | Unilateral | M | 25 |
| 2028 | Bilateral | M | 34 |
| 300 | Unilateral | M | 28 |
| 9200 | Bilateral with trunk involvement | M | 29 |
| 10,230 | Bilateral | F | 25 |
| 9615 | Bilateral | F | 25 |
| 1200 | Bilateral | F | 26 |
| 7200 | Bilateral | F | 36 |
| 4000 | Bilateral | F | 27 |
| 4300 | Bilateral | M | 24 |
| 4100 | Bilateral | M | 24 |
| 5902 | Bilateral | F | 31 |
| 4100 | Bilateral | M | 28 |
| 3125 | Bilateral | F | 36 |
| 4807 | Unilateral | M | 35 |
| 5386 | Bilateral | F | 31 |
| 8258 | Bilateral | F | 31 |
| 3402 | Unilateral | F | 24 |
| 4000 | Bilateral | M | 31 |
| 1030 | Unilateral | M | 26 |
| 3464 | Bilateral | F | 27 |
| 3719 | Bilateral | M | 23 |
| 3015 | Bilateral | M | 25 |
| 7314 | Bilateral | F | 26 |
| 2807 | Unilateral | F | 24 |
| 5355 | Unilateral | F | 23 |
| 1785 | Unilateral | M | 25 |
| 1646 | Unilateral | F | 25 |
| 2839 | Bilateral | F | 27 |
| 2060 | Unilateral | M | 28 |
Table 4.
Minimum values, 25% percentile, median, 75% percentile and maximum values
| Factor | Trunk diameter(mm) | D-dimer(ng/ml) |
|---|---|---|
| Total number of patients | 100 | 100 |
| Minimum value | 23 | 300 |
| 25th percentile | 24 | 1904.75 |
| Median | 26 | 4061 |
| 75th percentile | 29 | 6483.25 |
| Maximum value | 42 | 39,958 |
Conclusions
The clinical presentation of acute PE is varied. The most frequent clinical symptoms are chest pain, tachycardia, hypotension, dyspnoea, cough, and haemoptysis [9]. But what can a radiologist expect from the CT examination? Can there be any correlation between clinical and radiological parameters? In this retrospective study we tried to find correlations between different radiological and clinical parameters in the imaging “outcome’, i.e whether parameters like D-dimer, diameter of MPA, uni- or bilateralism of PE, and gender-related factors are radiologically significant. Considering that not every centre has a dual-source CT, we analysed parameters that are simple in their clinical and radiological evaluation. Assuming D-dimer levels under 500 ng/ml to be negative, we found one of 100 patients (1%) with a D-dimer-level of 300 ng/ml with PE.
A study from 2014 [10] proposed an age-adjusted D-dimer cut-off, but the results were not satisfactory. In other studies several scores for quantification of the clot were proposed, such as the CT severity score and CT obstruction index developed by Mastora et al. and Qanadli et al., respectively, but these are not routinely used in clinical practice [11,12].
The different correlation types show low correlation statistical data. The “strongest” weak correlation was between D-dimer levels and the axial diameter of the pulmonal trunk. Considering the correlation between the axial diameter of the pulmonal trunk and gender-related distributions, we found that female patients had higher axial diameters than men. We confirmed that women have a higher risk of developing pulmonal hypertension in PE than men [8].
Another weak relationship (almost zero) was found between D-dimer level and gender. Regarding the correlation between uni- or bilateralism of thromboembolism and the D-dimer levels, we found a weak correlation. The limitations of this retrospective study are, in our opinion, the use of only one clinical parameter like the D-dimer level to assess acute PE. We did not include diagnostic scores to identify risk stratification, such as the classic Wells score (WS), modified WS, simplified WS, revised Geneva score (GS), simplified GS, and the YEARS score.
Other drawbacks of this study are the exclusion of the age of the patients and the fact that a dilatation of MPA can have other causes, like cardiac shunts, arterial hypertension, Eisenmenger syndrome, high altitude, pulmonal valvular stenosis, infections, and connective tissue diseases, as well as idiopathic or traumatic causes. Another limitation is the absence of a control group and the presence of coexisting pathologies that increase D-dimer levels.
This retrospective study showed that D-dimer levels, the diameter of the pulmonal trunk, its location, and gender-related distributions have almost no correlation and are not significantly predictive in imaging.
Disclosure
The authors declared no conflicts of interest.
References
- 1.Konstantinides SV, Torbicki A, Agnelli G, et al. ; Task Force for the Diagnosis and Management of Acute Pulmonary Embolism of the European Society of Cardiology (ESC). 2014 ESC guidelines on the diagnosis and management of acute pulmonary embolism. Eur Heart J. 2014;35:3033–3069. doi: 10.1093/eurheartj/ehu283. [DOI] [PubMed] [Google Scholar]
- 2.Remy-Jardin M, Pistolesi M, Goodman LR, et al. Management of suspected acute pulmonary embolism in the era of CT angiography: a statement from the Fleischner Society. Radiology. 2007;245:315–329. doi: 10.1148/radiol.2452070397. [DOI] [PubMed] [Google Scholar]
- 3.Albrecht MH, Bickford MW, Nance JW, Jr, et al. State-of-the-art pulmonary CT angiography for acute pulmonary embolism. AJR Am J Roentgenol. 2017;208:495–504. doi: 10.2214/AJR.16.17202. [DOI] [PubMed] [Google Scholar]
- 4.Weitz JI, Fredenburgh JC, Eikelboom JW. A test in context: D-dimer. J Am Coll Cardiol. 2017;70:2411–2420. doi: 10.1016/j.jacc.2017.09.024. [DOI] [PubMed] [Google Scholar]
- 5.Pulivarthi S, Gurram MK. Effectiveness of D-dimer as a screening test for venous thromboembolism: an update. N Am J Med Sci. 2014;6:491–499. doi: 10.4103/1947-2714.143278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Truong QA, Massaro JM, Rogers IS, et al. Reference values for normal pulmonary artery dimensions by noncontrast cardiac computed tomography: the Framingham Heart Study. Circ Cardiovasc Imaging. 2012;5:147–154. doi: 10.1161/CIRCIMAGING.111.968610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Raymond TE, Khabbaza JE, Yadav R, Tonelli AR. Significance of main pulmonary artery dilation on imaging studies. Ann Am Thorac Soc. 2014;11:1623–1632. doi: 10.1513/AnnalsATS.201406-253PP. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Memon HA, Park MH. Pulmonary arterial hypertension in women. Methodist Debakey Cardiovasc J. 2017;13:224–237. doi: 10.14797/mdcj-13-4-224. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Moore AJE, Wachsmann J, Chamarthy MR, Panjikaran L, Tanabe Y, Rajiah P. Imaging of acute pulmonary embolism: an update. Cardiovasc Diagn Ther. 2018;8:225–243. doi: 10.21037/cdt.2017.12.01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Righini M, Van Es J, Den Exter PL, et al. Age-adjusted d-dimer cutoff levels to rule out pulmonary embolism: The adjust-pe study. JAMA. 2014;311:1117–1124. doi: 10.1001/jama.2014.2135. [DOI] [PubMed] [Google Scholar]
- 11.Mastora I, Remy-Jardin M, Masson P, et al. Severity of acute pulmonary embolism: evaluation of a new spiral CT angiographic score in correlation with echocardiographic data. Eur Radiol. 2003;13:29–35. doi: 10.1007/s00330-002-1515-y. [DOI] [PubMed] [Google Scholar]
- 12.Qanadli SD, El Hajjam M, Vieillard-Baron A, et al. New CT index to quantify arterial obstruction in pulmonary embolism: comparison with angiographic index and echocardiography. AJR Am J Roentgenol. 2001;176:1415–1420. doi: 10.2214/ajr.176.6.1761415. [DOI] [PubMed] [Google Scholar]