Abstract
Objectives
International data suggest the prevalence of severe obesity in young children may be increasing, yet no Canadian data are available. The objectives of this study were to examine definitions of severe obesity and to evaluate associated risk factors among young children in Ontario.
Methods
A cross-sectional study was conducted in children 17 to 24 months of age using two Ontario data sources: TARGet Kids! (n = 3713) and BORN Ontario (n = 768). Body mass index z score (zBMI) definitions were adapted from the World Health Organization (WHO) (z score > 3) and the US Centers for Disease Control (CDC) (> 120% of the 95th percentile) and applied to define severe obesity in young children. Multinomial logistic regression was used to evaluate associations between demographic and pregnancy risk factors and zBMI categories.
Results
A total of 1.1% (95% CI, 0.8–1.4) of children met the adapted WHO definition of severe obesity compared to 0.3% (95% CI, 0.2–0.6) using the CDC definition. Median neighbourhood household income (OR = 0.80, 95% CI, 0.69–0.93) and maternal pre-pregnancy BMI (OR = 1.08, 95% CI, 1.01–1.15) were associated with severe obesity in unadjusted analyses. After adjustment for potential confounders, the OR for the association between maternal pre-pregnancy BMI and severe obesity was 1.04 (95% CI, 0.94–1.15).
Conclusion
More than 1% of Ontario children met the adapted WHO definition of severe obesity in very early childhood. Modifiable risk factors were identified. Future studies are needed to understand the terminology, prevalence, and risk factors for severe obesity in young children across Canada.
Electronic supplementary material
The online version of this article (10.17269/s41997-018-0065-2) contains supplementary material, which is available to authorized users.
Keywords: Obesity; Obesity, morbid; Obesity, pediatric; Obesity, childhood onset; Body mass index
Résumé
Objectifs
Selon les données internationales, la prévalence de l’obésité sévère chez les jeunes enfants pourrait être en hausse, mais il n’existe pas de données canadiennes à ce sujet. Nous avons voulu examiner les définitions de l’obésité sévère et évaluer les facteurs de risque associés chez les jeunes enfants en Ontario.
Méthode
Nous avons mené une étude transversale auprès d’enfants de 17 à 24 mois à l’aide de deux sources de données ontariennes : TARGet Kids! (n = 3713) et BORN Ontario (n = 768). Nous avons adapté les définitions du score-z de l’indice de masse corporelle (IMC) de l’Organisation mondiale de la santé (OMS) (score-z > 3) et des Centers for Disease Control américains (CDC) (>120% du 95e centile) et nous les avons appliquées pour définir l’obésité sévère chez les jeunes enfants. Par régression logistique multinomiale, nous avons évalué les associations entre les facteurs de risque démographiques et liés à la grossesse et les catégories du score-z de l’IMC.
Résultats
Un total de 1,1% (IC de 95% : 0,8–1,4) des enfants répondaient à la définition de l’obésité sévère adaptée de celle de l’OMS, et 0,3% (IC de 95% : 0,2–0,6) répondaient à la définition adaptée de celle des CDC. Le revenu médian des ménages selon le quartier (rapport de cotes [RC] = 0,80, IC de 95% : 0,69–0,93) et l’IMC maternel avant la grossesse (RC = 1,08, IC de 95% : 1,01–1,15) étaient associés à l’obésité sévère dans nos analyses non ajustées. En tenant compte des facteurs confusionnels possibles, le RC de l’association entre l’IMC maternel avant la grossesse et l’obésité sévère était de 1,04 (IC de 95% : 0,94–1,15).
Conclusion
Plus de 1% des enfants ontariens répondent à la définition de l’obésité sévère de l’OMS pour les très jeunes enfants. Nous avons repéré des facteurs de risque modifiables. Il faudrait pousser la recherche pour comprendre la terminologie, la prévalence et les facteurs de risque de l’obésité sévère chez les jeunes enfants à l’échelle du Canada.
Mots-clés: Obésité, Obésité morbide, Obésité pédiatrique, Indice de masse corporelle
Introduction
Obesity in children is a global concern and the prevalence has increased substantially in recent decades (Wang & Lobstein, 2006; Rokholm et al., 2010). In Canada, 13% of children and adolescents 5–17 years of age have obesity in accordance with definitions set by the World Health Organization (WHO) (Roberts et al., 2012). Emerging evidence suggests that combined child overweight and obesity levels may have stabilized in several countries, including Canada (Rokholm et al., 2010; Rodd & Sharma, 2016), but more concerning is the rise of severe obesity around the world (Skinner et al., 2016; Garnett et al., 2016; Skelton et al., 2009). In 2014, 8.7% of American children and adolescents aged 2–19 years of age had severe obesity, an increase of 3.8% from 1999 (Skinner et al., 2016).
Risk factors in early childhood that are associated with later childhood obesity include higher maternal pre-pregnancy BMI, prenatal tobacco exposure, maternal excess gestational weight gain, high birthweight, gestational diabetes, and low socio-economic status (Woo Baidal et al., 2016). However, these risk factors have not been investigated in young children with severe obesity. Children with severe obesity are most likely to have severe obesity as adults (Kelly et al., 2013), and adult severe obesity is associated with higher risk of type 2 diabetes, hypertension, asthma, poor cardiometabolic outcomes, lower education attainment, and poor mental health, but these findings are inconsistent (Koebnick et al., 2010; Andreyeva et al., 2004; Tjepkema, n.d.). Understanding how these risk factors are comparable across categories of increased weight status is important to identify children at the highest risk for poor lifelong health outcomes.
Despite the potential importance of severe obesity, there is no harmonized definition or national data about the prevalence and risk factors of severe obesity in very young Canadian children (Shields & Tremblay, 2010). WHO growth reference standards are recommended for child growth monitoring in Canada and they define severe obesity as BMI z-score (zBMI) > 3 for children 5 to 19 years of age (WHO, 2006). In the US, the Centers for Disease Control and Prevention (CDC) recommends using > 120% of the 95th percentile to define severe obesity in children 2 to 20 years of age (Flegal et al., 2009). However, there is no recommended definition of severe obesity for children < 2 years of age by either organization.
Early childhood is a critical period for growth monitoring and children less than 2 years of age are frequently seen by their primary care providers (Morinis et al., 2012). Few studies have examined severe obesity in this age group and there may be opportunities for intervention if obesity is identified early. There are no national data on BMI for children less than 2 years of age; recent surveys such as the Canadian Health Measures Survey have only included children 3 years of age and older (Rodd & Sharma, 2016).
Given the lack of harmonized criteria for severe obesity and the lack of data in Canada on the prevalence of severe obesity in very early childhood, the primary objective of this study was to compare the prevalence of severe obesity, using WHO (primary) and CDC (secondary) defined cut-offs, in children 17 to 24 months of age, from two Ontario data sources. To be consistent with definitions of severe obesity in older children, the WHO cutoff of zBMI > 3 and the CDC definition of > 120% of the 95th percentile were used to define severe obesity. Our secondary objective was to evaluate associations between select demographic and pregnancy characteristics with overweight, obesity, and severe obesity in young children.
Methods
Study design and data sources
A cross-sectional analysis was conducted using two Ontario data sources: The Applied Research Group for Kids (TARGet Kids!) and Better Outcomes Registry & Network (BORN) Ontario.
TARGet Kids! is an ongoing, primary care practice-based research network in the Greater Toronto Area. The network consists of 11 pediatric and family physician primary care practices in the Toronto area and has been described previously (Carsley et al., 2015). Data were collected by trained research assistants and abstracted from records of children less than 6 years of age at scheduled well-child visits between 2009 and 2016 (Anderson et al., 2017).
BORN Ontario is a population-based, maternal child health registry, collecting pregnancy, birth, and early newborn data for all babies born in the province of Ontario. BORN recently piloted a project to build a repository of data for children in primary care at the enhanced 18-month well-baby visits from 12 family health teams in Ontario, including Toronto, Fenelon Falls, Petrolia, Chatham, Burlington, Hamilton, Kingston, St. Thomas, and London. Data from the electronic medical record systems from these primary care practices were uploaded to the BORN information system (BIS) for visits that took place between 2014 and 2016 for children 17 to 24 months of age and linked to other pregnancy and demographic variables contained in the BIS. The collection sites for TARGet Kids! and BORN were mutually exclusive, ensuring that all children in these two cohorts were unique.
Inclusion/exclusion criteria
Children whose information was contained in TARGet Kids! and BORN data repositories, and who were 17 to 24 months of age, were eligible to participate. In both TARGet Kids! and BORN data sets, children born < 32 weeks gestational age were excluded. Consistent with the TARGet Kids! study protocol, TARGet Kids! children were excluded if they had severe developmental delay, health conditions affecting growth, any acute or chronic illness (other than asthma), or if their families were unable to complete English questionnaires (Carsley et al., 2015).
This study was approved by the Research Ethics Boards at The Hospital for Sick Children, St. Michael’s Hospital, and the Children’s Hospital of Eastern Ontario. Consent was obtained from parents of all participating children in TARGet Kids!. For BORN data, informed consent was not required since this was a secondary analysis of de-identified data in a prescribed registry under the Personal Health Information Protection Act (PHIPA).
Outcome measurement
The primary outcome, severe obesity, was measured in both TARGet Kids! and BORN, using length and weight to determine BMI. At TARGet Kids!, anthropometric measurements were collected by trained research assistants. Weight was measured using a precision digital scale (SECA, Germany) to the nearest 0.01 kg; length was measured using a length board to the nearest 0.1 cm. Additional routine data were abstracted from electronic medical records (EMRs) for participating children between 17 and 24 months of age, who were not measured by a research assistant. This was done to supplement records of children from TARGet Kids! who did not attend a scheduled 18-month well-child visit but did visit their physician practice when they were between 17 and 24 months of age. At BORN, anthropometric measurements were collected in primary care clinics by clinicians and were later extracted from the EMRs and linked to other covariate data using BIS records (Ontario’s Enhanced 18-Month Well-Baby Visit Electronic Medical Record (EMR) Integration and Repository Project, 2013).
BMI was calculated by dividing weight by height squared. zBMI, standardized by age and sex, was determined using WHO growth references (WHO, 2006). The growth references were selected as they are meant to reflect optimal growth in children < 5 years and recommended for this age group in Canada (Marchand, 2010). BMI-for-age was used as the primary outcome instead of weight-for-length as we have previously shown high agreement between the two measures and BMI is the standard measure used in all other age groups (Furlong et al., 2016).
The CDC cutoff of > 120% of the 95th percentile and WHO cut-off of zBMI > 3, applied to the age and sex standardized zBMI scores from WHO growth reference charts were used to estimate prevalence of severe obesity (Shields & Tremblay, 2010; Flegal et al., 2009). For our secondary objective, to remain consistent with WHO weight terminology used in older children (5 to 19 years), children were classified into four growth categories: zBMI ≤ 1, 1 < zBMI ≤ 2, 2 < zBMI ≤ 3, and zBMI > 3, which we termed severe obesity.
Exposure measurement
Select demographic and pregnancy variables were evaluated as potential risk factors for severe obesity. Data on exposure variables were collected from parent-reported questionnaires at TARGet Kids! and abstracted from BIS linked birth records, census data, and prenatal visit data for BORN. Demographic variables included child age and sex, maternal ethnicity, and median neighbourhood household income. Maternal ethnicity was categorized as Caucasian, Black, Asian, and Other, representing smaller groups. Maternal ethnicity was not collected for all mothers from BORN, as this measure was only available for mothers who had prenatal screening records. Median after-tax neighbourhood household income was obtained at the dissemination area level by linking to the postal code conversion file (PCCF) from Statistics Canada (Postal Code OM Conversion File (PCCF), 2016).
Pregnancy variables included gestational age, birthweight, maternal pre-pregnancy BMI, presence of gestational diabetes and/or hypertension, parity, and in utero smoke exposure from smoking in the household. Gestational age was categorized as term (≥ 37 weeks) or preterm (< 37 weeks). Birthweight was categorized as low (< 2.5 kg), normal (2.5–4.0 kg) and high (> 4.0 kg). Parity was categorized as nulliparous (0) and multiparous (≥ 1). Smoke exposure in utero was a self-reported measure, defined as either the mother or another member of the household smoking during the mother’s pregnancy.
Data cleaning
Outlier values for child height and weight measurements were identified using WHO Field Tables (2006—birth to 60 months) (WHO, 2006). For zBMI scores above 5.0 or below −5.0, child weight and height measurements were noted. At TARGet Kids!, these outliers were reviewed to determine whether they were values appropriate for age and sex according to the WHO field tables, and were reviewed directly in the original charts before determining whether they were to be excluded. For BORN data, children with outlier zBMI scores of above 5.0 or below −5.0, which were outside the age-appropriate height and weight measurement ranges from WHO field tables (WHO, 2006), were removed since we were unable to review the heights and weights directly.
Statistical analysis
Data were analyzed using SAS 9.4 and R 3.3.2. Descriptive statistics including means and standard deviations and frequency distributions were reported for all continuous and categorical variables, respectively, in the two datasets separately (data not shown) and pooled together.
To evaluate the associations between demographic and pregnancy-related variables and increased weight status, multinomial logistic regression for all five weight categories using WHO weight definitions were modeled with a zBMI of less than 1 as the reference category. For all regression analysis, the data from TARGet Kids! and BORN were pooled. Multiple imputation was conducted using the mice package in R prior to regression modeling (Groothuis-Oudshoorn & Van Buuren, 2011). Odds ratios and 95% CI were obtained for the association between each exposure variable and obesity category using unadjusted multinomial regression models. Using adjusted multinomial logistic regression, we then examined three key risk factors (maternal pre-pregnancy BMI, birthweight, and smoke exposure in utero) in separate models that were each adjusted for income, ethnicity, parity, and other hypothesized confounders as relevant to each model. Statistical significance was defined as p < 0.05 and all tests were two-sided.
Results
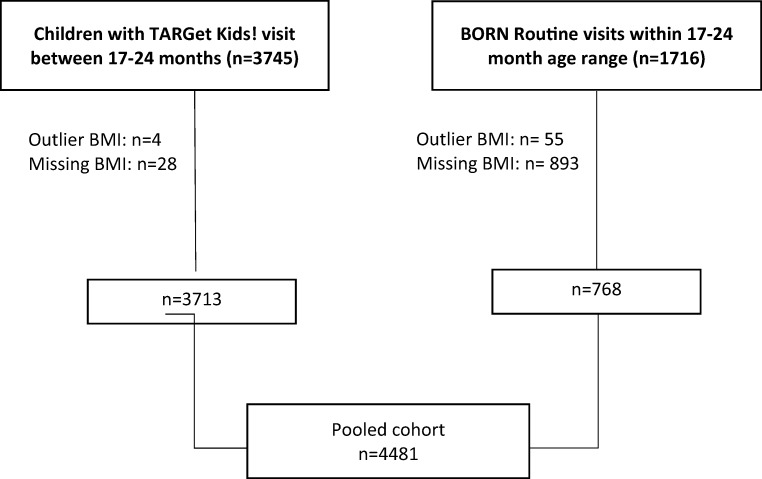
The pooled cohort of TARGet Kids! and BORN children included 4481 children aged 17 to 24 months (see Study Flow Diagram, Fig. 1). Demographic and pregnancy characteristics of the TARGet Kids! and BORN cohorts are presented in Table 1, as unique and pooled cohorts. In the pooled cohort, 46.9% of the children were female with a mean age of 19.9 (SD 2.5) months, and the average median neighbourhood household income was $54,756 (SD 26,180). Missing values were high in the gestational age and birthweight variables for TARGet Kids! and in the maternal ethnicity variable for BORN (Table 1), limiting our ability to compare the two cohorts. The zBMI, adjusted for age and sex, was 0.26 (SD 1.1) in the pooled cohort.
Fig. 1.
Flow diagram for cohort selection for TARGet Kids! and BORN data sources
Table 1.
Comparison of socio-demographic and maternal pregnancy variables in TARGet Kids! and BORN for children 17 to 24 months of age in Ontario
| Variable | TARGet Kids! (n=3713*) |
BORN (n=768) |
Pooled (n=4481† ) |
|---|---|---|---|
| Mean (SD) | Mean (SD) | Mean (SD) | |
| Age (months) | 20.2 (2.6) | 18.9 (1.2) | 19.9 (2.5) |
| zBMI‡ | 0.24 (1.1) | 0.37 (1.3) | 0.26 (1.1) |
| Median neighbourhood household income | 59,342 (26,271) | 33,468 (10,610) | 54756 (26,180) |
| N missing | 301 | 33 | 334 |
| Maternal Pre-Pregnancy BMI | 23.6 (4.5) | 25.4 (6.1) | 24.1 (5.0) |
| N missing | 1828 | 154 | 1982 |
| N (%) | N (%) | N (%) | |
| Sex | |||
| Male | 1962 (52.8) | 416 (54.2) | 2378 (53.1) |
| Female | 1751 (47.2) | 352 (45.8) | 2103 (46.9) |
| Gestational age at birth | |||
| ≥ 37 weeks | 2194 (59.1) | 669 (87.1) | 2863 (63.9) |
| <37 weeks | 283 (7.6) | 49 (6.4) | 332 (7.4) |
| Missing | 1236 (33.3) | 50 (6.5) | 1286 (28.7) |
| Birthweight | |||
| ≤ 2500g | 339 (9.1) | 31 (4.0) | 370 (8.3) |
| 2501-4000g | 2438 (65.7) | 603 (78.5) | 3041 (67.9) |
| ≥ 4001g | 304 (8.2) | 78 (10.2) | 382 (8.5) |
| Missing | 632 (17.0) | 56 (7.3) | 688 (15.3) |
| Maternal Ethnicity | |||
| Caucasian | 2331 (62.8) | 291 (37.9) | 2622 (58.5) |
| Black | 156 (4.2) | 18 (2.3) | 174 (3.9) |
| Asian | 556 (15.0) | 54 (7.0) | 610 (13.6) |
| Other | 358 (9.6) | 12 (1.6) | 370 (8.3) |
| Missing | 312 (8.4) | 393 (51.2) | 705 (15.7) |
| Gestational diabetes | |||
| No | 3270 (88.1) | 665 (86.6) | 3935 (87.8) |
| Yes | 176 (4.7) | 48 (6.2) | 224 (5.0) |
| Missing | 267 (7.2) | 55 (7.2) | 322 (7.2) |
| Gestational hypertension | |||
| No | 3234 (87.1) | 677 (88.1) | 3911 (87.3) |
| Yes | 194 (5.2) | 42 (5.5) | 236 (5.3) |
| Missing | 285 (7.7) | 49 (6.4) | 334 (7.4) |
| Smoke Exposure in utero§ | |||
| Yes | 58 (1.6) | 40 (5.2) | 98 (2.2) |
| No | 3313 (89.2) | 678 (88.3) | 3991 (89.1) |
| Missing | 342 (9.2) | 50 (6.5) | 392 (8.7) |
| Parity | |||
| 0 | 1501 (40.4) | 343 (44.7) | 1844 (41.2) |
| ≥1 | 1983 (53.4) | 365 (47.5) | 2348 (52.4) |
| Missing | 229 (6.2) | 60 (7.8) | 289 (6.4) |
* Of the 3713 subjects in TARGet Kids! cohort, 2331 are from NHQ visits and 1382 are from retrospective visits
† Pooled data sets consist of 3713 TARGet Kids! children and 768 BORN children
‡ Subjects with ZBMIs higher than +5.0 or lower than -5.0 were removed from analysis in the TARGet Kids! after review of original records and analysis without review in BORN cohort
§ Smoke exposure in utero was a self-reported measure, defined as either the mother or another member of the household smoking during the mother’s pregnancy
For our primary objective, a comparison of the prevalence of children meeting the definitions of severe obesity, and all other weight categories, is presented in Table 2 using both the WHO and CDC cutoffs for the pooled cohort. Based on the WHO definition, 47 (1.1%, 95% CI: 0.8–1.4) children were defined as zBMI > 3, whereas only 15 (0.3%, 95% CI: 0.2–0.6) of children met the CDC cutoff of > 120% of the 95th percentile. When the weight categories were evaluated separately for TARGet Kids! and BORN, we observed that the BORN cohort had a higher prevalence of children with zBMI > 3 (2.5%) in comparison to TARGet Kids! cohort (0.8%) (Supplemental Table 1).
Table 2.
Comparison of zBMI categories using CDC and WHO weight category definitions in pooled TARGet Kids! and BORN for children 17 to 24 months of age
| WHO*† | Prevalence (95% CI) | CDC† | Prevalence (95% CI) |
|---|---|---|---|
| zBMI ≤ 1 | 75.4% (74.1–76.6) | < 85th percentile | 74.1% (72.8–75.4) |
| 1 < zBMI ≤ 2 | 18.4% (17.3–19.6) | 85th to 95th percentile | 13.7% (12.7–14.7) |
| 2 < zBMI ≤ 3 | 5.1% (4.5–5.8) | 95th to ≤ 120% of 95th percentile | 11.9% (11.0–12.9) |
| zBMI > 3 | 1.1% (0.8–1.4) | >120% of 95th percentile | 0.3% (0.2–0.6) |
*Definitions of zBMI categories for children 5–19 years of age were applied since no definition of severe obesity currently exists for children <2 years of age
†Detailed definitions for the weight categories and percentile ranges for individual TARGet Kids! and BORN can be found in Supplemental Table 1
For our secondary objective, multinomial logistic regression models, using WHO defined weight categories as dependent variables, are presented in Table 3 (unadjusted) and Table 4 (adjusted). When the analyses were conducted separately for TARGet Kids! and BORN, the results appeared similar for both groups, although many estimates had wide confidence intervals due to small sample size (data not shown). In the unadjusted models with TARGet Kids! and BORN data pooled (Table 3), median neighbourhood household income (per $10,000) was associated with decreased odds of zBMI > 3, (OR = 0.8, 95% CI: 0.69–0.93). Maternal pre-pregnancy BMI (per kg/m2) was associated with increased odds of zBMI > 3 (OR = 1.08, 95% CI, 1.01–1.15). High birthweight (> 4.0 kg) (OR = 1.67, 95% CI: 1.30–2.15; OR = 1.81, 95% CI: 1.21–2.72) and the presence of smoke exposure in utero (OR = 1.86, 95% CI, 1.16–2.98; OR = 3.21, 95% CI, 1.70–6.08) were significantly associated with increased weight status categories, 1 < zBMI ≤ 2 and 2 < zBMI ≤ 3, respectively.
Table 3.
Multinomial logistic regression unadjusted analysis of pooled BORN and TARGet Kids! cohorts
| Weight status* (Ref = zBMI ≤ 1) | ||||||
|---|---|---|---|---|---|---|
| 1 < zBMI ≤ 2 | 2 < zBMI ≤ 3 | zBMI > 3 | ||||
| Variable | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Age (months) | 1.03 | 1.00–1.06 | 0.98 | 0.92–1.03 | 0.91 | 0.79–1.04 |
| Sex | ||||||
| Female vs Male | 0.91 | 0.78–1.06 | 0.67 | 0.51–0.88 | 0.73 | 0.41–1.32 |
| Median neighbourhood household income (per $10,000) | 0.96 | 0.93–0.99 | 1.00 | 0.95–1.05 | 0.80 | 0.69–0.93 |
| Maternal pre-pregnancy BMI (per kg/m2) | 1.05 | 1.03–1.07 | 1.04 | 1.01–1.08 | 1.08 | 1.01–1.15 |
| Gestational age | ||||||
| < 37 weeks vs ≥ 37 weeks | 0.88 | 0.65–1.20 | 1.18 | 0.74–1.87 | 1.43 | 0.55–3.71 |
| Birthweight | ||||||
| Low vs normal | 0.81 | 0.60–1.08 | 0.68 | 0.39–1.19 | 0.28 | 0.04–2.04 |
| High vs normal | 1.67 | 1.30–2.15 | 1.81 | 1.21–2.72 | 1.33 | 0.46–3.82 |
| Maternal ethnicity | ||||||
| Non-caucasian vs caucasian | 0.74 | 0.61–0.89 | 1.03 | 0.75–1.41 | 1.30 | 0.63–2.66 |
| Parity | ||||||
| Nulliparous vs multiparous | 0.84 | 0.71–0.98 | 0.66 | 0.49–0.88 | 0.75 | 0.39–1.44 |
| Gestational diabetes | ||||||
| Yes vs No | 0.91 | 0.64–1.30 | 0.85 | 0.44–1.63 | 1.40 | 0.43–4.58 |
| Gestational hypertension | ||||||
| Yes vs No | 1.03 | 0.73–1.43 | 1.01 | 0.55–1.84 | 0.88 | 0.21–3.66 |
| Smoke exposure in utero | ||||||
| Yes vs No | 1.86 | 1.16–2.98 | 3.21 | 1.70–6.08 | 2.75 | 0.65–11.66 |
*Weight status is categorized using WHO weight category definitions only
Table 4.
Multinomial logistic regression adjusted analysis of pooled BORN and TARGet Kids! cohorts
| Weight status§ (Ref = zBMI ≤ 1) | ||||||
|---|---|---|---|---|---|---|
| 1 < zBMI ≤ 2 | 2 < zBMI ≤ 3 | zBMI > 3 | ||||
| Variable | OR | 95% CI | OR | 95% CI | OR | 95% CI |
| Maternal pre-pregnancy BMI (kg/m2)* | 1.04 | 1.02–1.07 | 1.02 | 0.97–1.07 | 1.04 | 0.94–1.15 |
| Birthweight† | ||||||
| Low vs normal | 0.74 | 0.44–1.24 | 0.47 | 0.17–1.33 | 0.74 | 0.09–5.96 |
| High vs normal | 1.52 | 1.03–2.24 | 1.11 | 0.53–2.28 | N/R | N/R |
| Smoke exposure in utero‡ | ||||||
| Yes vs no | 1.39 | 0.74–2.61 | 2.65 | 1.09–6.45 | 3.95 | 0.87–17.84 |
*Adjusted for median neighbourhood household income, maternal ethnicity, parity, and smoke exposure in utero
†Adjusted for median neighbourhood household income, maternal ethnicity, parity, smoke exposure in utero, and maternal pre-pregnancy BMI
‡Adjusted for median neighbourhood household income, maternal ethnicity, and parity
§Child weight status was categorized using WHO weight category definitions only
In our adjusted models of maternal pre-pregnancy BMI, birthweight, and smoke exposure in utero, none of the associations with severe obesity were statistically significant (Table 4). However, increased maternal pre-pregnancy BMI and high birthweight (> 4.0 kg) were risk factors for children with 1 < zBMI ≤ 2 and children with a zBMI between 2 and 3 had over 2 times more odds of being exposed to smoking in utero (OR = 2.65, 95% CI, 1.09–6.45).
Discussion
To our knowledge, this is one of the first studies that has investigated the prevalence of severe obesity and potential risk factors in young Canadian children. The results of our study suggest that in children 17–24 months of age in Ontario, the prevalence of severe obesity is approximately 1%, although estimates varied between WHO and CDC cutoffs. The WHO definition recognizes a larger proportion of children to fit the severe obesity category in comparison to CDC. Weight terminology for children 0–5 years old is not consistent with that of older children; for example, in children under 5 years of age zBMI > 2 and ≤ 3 is termed overweight, whereas for children over 5 years of age this zBMI category is considered obese. These definitions are misleading and are challenging to use when evaluating weight categories among children of all ages. We propose that consistent terminology should be used for all age groups and the WHO definition of zBMI > 3 should be used to estimate severe obesity in young children in Canada. A less conservative estimate recognizes more children with extreme weight issues and the WHO definition parallels with the use of WHO growth recommendations for other age groups in Canada.
Given the paucity of Canadian data in this age group, we were unable to directly compare our estimates to national surveys (Roberts et al., 2012; Rodd & Sharma, 2016; Shields & Tremblay, 2010). However, our prevalence estimates were similar to those observed in a study of children 0–2 years of age using primary care electronic medical records in Ontario (Biro et al., 2016). The prevalence of severe obesity observed in our study was substantially lower than US estimates of 2.07% for children aged 2–4 years (Pan et al., 2012) and 4.6–6.4% for youth aged 2 to 19 years old (using the CDC > 120% of the 95th percentile) (Skinner et al., 2016; Koebnick et al., 2010). This difference is likely related, at least in part, to the younger age group in our study. Different classification systems have been used to define severe obesity internationally, which also limits our ability to compare prevalence estimates (Valerio et al., 2013).
Lower median neighbourhood household income and high maternal BMI were both associated with a child zBMI > 3 in our unadjusted model. This is consistent with literature suggesting these are risk factors for overweight and obesity in young children (Woo Baidal et al., 2016). However, it has not been established that these are risk factors for severe obesity. High birthweight was significantly associated with 1 < zBMI ≤ 2 and 2 < zBMI ≤ 3 in our unadjusted analyses; after adjustment for potential confounders, this association was only statistically significant for 1 < zBMI ≤ 2 although all ORs were > 1.0. This is consistent with previous studies that have found high birthweight is associated with excess weight and obesity later in childhood (Yu et al., 2011).
Other socio-demographic and pregnancy risk factors that we evaluated were not associated with severe obesity, but we did observe trends across high zBMI categories. For example, smoke exposure during pregnancy was positively associated with 2 < zBMI ≤ 3, with children being at almost 3 times greater risk if they had been exposed to smoking in utero (Table 4). This is consistent with previous reports that linked smoke exposure to excess weight (Oken et al., 2008). Our ability to compare weight status according to ethnicity was limited by the data collection differences between the two cohorts, with more limited ethnicity categories in BORN data.
Our study addresses a gap in Canadian data on severe obesity in young children. Given that no population-based national surveys in Canada provide BMI distributions for this young age group, we combined data from two existing Ontario data sources from primary care. Data from TARGet Kids! and BORN may not be generalizable to all children in Ontario or Canada, but our large sample size can provide at least some description of this issue. Multiple methods of recruitment such as active voluntary recruitment and passive extraction from EMRs also generate diversity in the child data. Pregnancy characteristics such as the prevalence of gestational hypertension and diabetes were similar for TARGet Kids! and BORN and in line with provincial estimates (Maternal Hypertension in Canada, 2014; Maternal Diabetes in Canada, 2014). Further, children in this cohort represented a diverse ethnic background and income gradient.
While a large sample size is a strength of this study, the low proportion of children with severe obesity limits the power of our multinomial logistic regression modeling. Many of the observed ORs for severe obesity were consistent in magnitude with the categories for overweight and obesity but they were not statistically significant at p < 0.05. Multiple imputation was used to reduce bias from missing data, however, the relatively high proportion of missing data for variables such as maternal pre-pregnancy BMI, maternal ethnicity and smoke exposure in utero may be due to reporting bias. Further, although the prevalence of many characteristics were similar in BORN and TARGet Kids!, there were other variables such as smoke exposure in utero where the prevalence was quite different. If children with severe obesity and exposed to smoke exposure in utero were less likely to participate in this study, it may result in selection bias.
While BMI data validity was assessed in the TARGet Kids! data through original chart review, this was not possible in BORN data, potentially excluding some subjects with severe obesity inappropriately as outliers. Other data issues include lack of standardized methods of height and weight measurement in primary care, for example, the use of a length board compared to standing height. Measuring length is the recommended method of measurement for children under 2.
Conclusion
In Ontario, severe obesity is present in approximately 1% of young children, demonstrating the need for recognition and further characterization of risk factors for severe obesity, and strategies and resources to prevent and manage severe obesity. It is important to note that our interpretations are based on an inferred definition of severe obesity, given to children 17 to 24 months old, based on available definitions for older children. Consistent weight status definitions do not exist for children at this young age, but the need for it is evident. As there is a lack of national child growth monitoring in Canada, especially for very young children, we propose the WHO definition be used with Canadian data to remain consistent with existing growth guidelines in our country. Our study highlights the importance of a standardized definition of severe obesity in young children and reiterates the need for population-based surveillance.
Electronic supplementary material
(DOCX 15 kb)
Acknowledgements
We thank all of the participating families for their time and involvement in TARGet Kids! and are grateful to all practitioners who are currently involved in the TARGet Kids! practice-based research network.
Funding
Funding for this study was received from the Canadian Institutes of Health Research.
Compliance with ethical standards
Conflict of interest
JLM received an unrestricted research grant for a completed investigator-initiated study from the Dairy Farmers of Canada (2011–2012) and Ddrops provided non-financial support (vitamin D supplements) for an investigator-initiated study on vitamin D and respiratory tract infections (2011–2015). PCP received unrestricted research grants for completed investigator-initiated studies from Danone Institute of Canada (2002–2004 and 2006–2009), Dairy Farmers of Ontario (2008–2010), and Mead Johnson Nutrition provided non-financial support (Fer-In-Sol® liquid iron supplement) (2011–2017) for an ongoing investigator-initiated trial of iron deficiency in young children that was funded by Canadian Institutes of Health Research (FRN # 115059). These agencies had no role in the design, collection, analyses or interpretation of the results of this study or in the preparation, review, or approval of the manuscript. All other authors declare they have no conflicts of interest.
References
- Andreyeva T, Sturm R, Ringel JS. Moderate and severe obesity have large differences in health care costs. Obesity Research. 2004;12(12):1936–1943. doi: 10.1038/oby.2004.243. [DOI] [PubMed] [Google Scholar]
- Anderson LN, Ball GDC, Birken CS, et al. The team to address bariatric care in Canadian children (Team ABC3): team grant research proposal. BMC Research Notes. 2017;10(1):1–15. doi: 10.1186/s13104-016-2345-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Biro S, Barber D, Williamson T, Morkem R, Khan S, Janssen I. Prevalence of toddler, child and adolescent overweight and obesity derived from primary care electronic medical records: an observational study. CMAJ Open. 2016;4(3):E538–E544. doi: 10.9778/cmajo.20150108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carsley S, Borkhoff CM, Maguire JL, et al. Cohort profile: the applied research group for Kids (TARGet Kids!) International Journal of Epidemiology. 2015;44(3):776–788. doi: 10.1093/ije/dyu123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flegal KM, Wei R, Ogden CL, Freedman DS, Johnson CL, Curtin LR. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. The American Journal of Clinical Nutrition. 2009;90(4):1314–1320. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- Furlong K. R., Anderson L. N., Kang H., Lebovic G., Parkin P. C., Maguire J. L., OConnor D. L., Birken C. S. BMI-for-Age and Weight-for-Length in Children 0 to 2 Years. PEDIATRICS. 2016;138(1):e20153809–e20153809. doi: 10.1542/peds.2015-3809. [DOI] [PubMed] [Google Scholar]
- Garnett SP, Baur LA, Jones AMD, Hardy LL. Trends in the prevalence of morbid and severe obesity in Australian children aged 7–15 years, 1985–2012. PLoS One. 2016;11(5):1–7. doi: 10.1371/journal.pone.0154879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Groothuis-Oudshoorn, K., & Van Buuren, S. (2011). Mice: multivariate imputation by chained equations in R. Journal of Statistical Software, 45(3).
- Kelly Aaron S., Barlow Sarah E., Rao Goutham, Inge Thomas H., Hayman Laura L., Steinberger Julia, Urbina Elaine M., Ewing Linda J., Daniels Stephen R. Severe Obesity in Children and Adolescents: Identification, Associated Health Risks, and Treatment Approaches. Circulation. 2013;128(15):1689–1712. doi: 10.1161/CIR.0b013e3182a5cfb3. [DOI] [PubMed] [Google Scholar]
- Koebnick C, Smith N, Coleman KJ, et al. Prevalence of extreme obesity in a multiethnic cohort of children and adolescents. Journal of Pediatrics. 2010;157(1):26–31. doi: 10.1016/j.jpeds.2010.01.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marchand V. Promoting optimal monitoring of child growth in Canada: using the new World Health Organization growth charts. Paediatrics & Child Health. 2010;15(2):77–79. doi: 10.1093/pch/15.2.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Maternal Diabetes in Canada. Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/publications/healthy-living/maternal-diabetes-canada.html. Published 2014. Accessed August 28, 2016.
- Maternal Hypertension in Canada. Public Health Agency of Canada. https://www.canada.ca/en/public-health/services/publications/healthy-living/maternal-hypertension-canada.html. Published 2014. Accessed August 28, 2016.
- Morinis J, Maguire J, Khovratovich M, McCrindle BW, Parkin PC, Birken CS. Paediatric obesity research in early childhood and the primary care setting: The TARGet Kids! research network. International Journal of Environmental Research and Public Health. 2012;9(4):1343–1354. doi: 10.3390/ijerph9041343. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Oken E, Levitan EB, Gillman MW. Maternal smoking during pregnancy and child overweight: systematic review and meta-analysis. International Journal of Obesity. 2008;32:201–210. doi: 10.1038/sj.ijo.0803760. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ontario’s Enhanced 18-Month Well-Baby Visit Electronic Medical Record (EMR) Integration and Repository Project. BORN Ontario. https://www.bornontario.ca/en/partnership-projects/enhanced-18-month-well-baby-visit-project/. Published 2013. Accessed May 25, 2016.
- Pan L, Blanck HM, Sherry B, Dalenius K, Grummer-Strawn L. Trends in the prevalence of extreme obesity among US preschool-aged children living in low-income families, 1998-2010. JAMA. 2012;308(24):2563–2565. doi: 10.1001/jama.2012.108099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Postal Code OM Conversion File (PCCF), Reference Guide. Statistics Canada Catalogue no. 92–154-G. http://www.statcan.gc.ca/pub/92-154-g/92-154-g2016001-eng.htm. Published 2016. Accessed September 6, 2016.
- Roberts KC, Shields M, de Groh M, Aziz A, Gilbert JA. Overweight and obesity in children and adolescents: results from the 2009 to 2011 Canadian Health Measures Survey. Ottawa: Statistics Canada. https://www.statcan.gc.ca/pub/82-003-x/2012003/article/11706-eng.pdf. Published 2012. Accessed June 20, 2016. [PubMed]
- Rodd C, Sharma AK. Recent trends in the prevalence of overweight and obesity among Canadian children. CMAJ. 2016;188(13):E313–E320. doi: 10.1503/cmaj.150854. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rokholm B, Baker JL, Sorensen TIA. The levelling off of the obesity epidemic since the year 1999—a review of evidence and perspectives. Obesity Reviews. 2010;11(12):835–846. doi: 10.1111/j.1467-789X.2010.00810.x. [DOI] [PubMed] [Google Scholar]
- Shields M, Tremblay MS. Canadian childhood obesity estimates based on WHO, IOTF and CDC cut-points. International Journal of Pediatric Obesity. 2010;5(3):265–273. doi: 10.3109/17477160903268282. [DOI] [PubMed] [Google Scholar]
- Skinner AC, Perrin EM, Skelton JA. Prevalence of obesity and severe obesity in US children, 1999–2014. Obesity. 2016;24(5):1116–1123. doi: 10.1002/oby.21497. [DOI] [PubMed] [Google Scholar]
- Skelton JA, Cook SR, Auinger P, Klein JD, Barlow SE. Prevalence and trends of severe obesity among US children and adolescents. Academic Pediatrics. 2009;9(5):322–329. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tjepkema, M. Adult obesity in Canada: measured height and weight. Ottawa: Statistics Canada http://www.statcan.gc.ca/pub/82-620-m/2005001/pdf/4224906-eng.pdf. Published 2004. Accessed July 31, 2016.
- Valerio G, Maffeis C, Balsamo A, et al. Severe obesity and cardiometabolic risk in children: comparison from two international classification systems. PLoS One. 2013;8(12):6–13. doi: 10.1371/journal.pone.0083793. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wang Y, Lobstein T. Worldwide trends in childhood overweight and obesity. International Journal of Pediatric Obesity. 2006;1(1):11–25. doi: 10.1080/17477160600586747. [DOI] [PubMed] [Google Scholar]
- WHO Child Growth Standards based on length/height, weight and age. Acta Paediatr (Oslo, Norw 1992) Suppl. 2006;450:76–85. doi: 10.1111/j.1651-2227.2006.tb02378.x. [DOI] [PubMed] [Google Scholar]
- Woo Baidal JA, Locks LM, Cheng ER, Blake-Lamb TL, Perkins ME, Taveras EM. Risk factors for childhood obesity in the first 1,000 days. American Journal of Preventive Medicine. 2016;50(6):761–779. doi: 10.1016/j.amepre.2015.11.012. [DOI] [PubMed] [Google Scholar]
- Yu ZB, Han SP, Zhu GZ, et al. Birth weight and subsequent risk of obesity: a systematic review and meta-analysis. Obesity Reviews. 2011;12(7):525–542. doi: 10.1111/j.1467-789X.2011.00867.x. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 15 kb)