Abstract
Objective
For patients who belonged to physician rosters at a family medicine practice in the core of Calgary, Canada, we compared primary care utilization for those who were stably housed and those experiencing homelessness.
Methods
This retrospective chart review accessed electronic medical record data for rostered patients who visited their family physician between July 1, 2015 and August 31, 2016. We assessed the association between homelessness status (defined as having been sheltered in overnight shelters and/or emergency/provisional housing during the study period) and the rate of visits to primary care (defined as the count of visits associated with a patient accounting for the length of the patient’s relationship with their family physician) using multivariate negative binomial regression.
Results
We analyzed 1013 patients belonging to three family physician rosters, of whom 112 experienced homelessness during the study period (11.1%). The mean number of visits for patients who experienced homelessness was 9.6 (SD 10.5), compared to 4.2 (SD 3.6) visits for stably housed patients (p < 0.0001). The rate of accessing primary care for patients experiencing homelessness was 2.02 times greater than the rate for stably housed individuals (rate ratio [RR] 2.02, 95% confidence interval [95% CI] 1.74–2.35; p < 0.0001).
Conclusion
In the context of an inner-city primary care clinic in Calgary, Canada, homelessness status is associated with an increased rate of visits to primary care. This work has implications for public health and health systems decision-makers involved in developing equitable health policy, as well as for frontline care providers who serve this vulnerable population.
Keywords: Primary care, Health service utilization, Vulnerable populations, Homelessness, Social determinants of health, Health equity
Résumé
Objectif
Chez les patients inscrits d’un cabinet de médecine familiale du centre-ville de Calgary (Canada), nous avons comparé l’utilisation des soins primaires par les patients ayant un logement stable et les patients sans domicile fixe.
Méthode
Pour l’examen rétrospectif des dossiers médicaux, nous avons accédé aux données du dossier médical électronique des patients inscrits ayant visité leur médecin de famille entre le 1er juillet 2015 et le 31 août 2016. Nous avons évalué les associations entre l’itinérance (définie comme étant le logement dans des centres d’accueil de nuit, des maisons de refuge ou des logements provisoires durant la période de l’étude) et le taux de consultations en soins primaires (défini comme étant le nombre de consultations associées à un patient, compte tenu de la durée de la relation du patient avec son médecin de famille) selon un modèle de régression binomiale négative multivarié.
Résultats
Nous avons analysé 1013 patients figurant sur les listes de trois médecins de famille; 112 de ces patients (11,1%) étaient itinérants durant la période de l’étude. Le nombre moyen de consultations des patients itinérants était de 9,6 (écart-type de 10,5), contre 4,2 consultations (écart-type de 3,6) pour les patients ayant un logement stable (p < 0,0001). Le taux d’accès aux soins primaires des patients itinérants était 2,02 fois plus élevé que celui des personnes ayant un logement stable (rapport de taux [RT] 2,02, intervalle de confiance de 95% [IC de 95%] 1,74–2,35; p < 0,0001).
Conclusion
Dans le contexte d’une clinique de soins primaires située dans un quartier déshérité du centre-ville de Calgary (Canada), l’itinérance est associée à un taux accru de consultations en soins primaires. L’étude a des conséquences pour les décideurs de la santé publique et du système de santé qui participent à l’élaboration de politiques de santé équitables, ainsi que pour les dispensateurs de soins de première ligne qui servent cette population vulnérable.
Mots-clés: Soins primaires, Utilisation des services de santé, Populations vulnérables, Personnes sans domicile fixe, Déterminants sociaux de la santé, Équité en santé
Introduction
Despite recognition of stable housing as a human right and determinant of health, homelessness is endemic in Canada (World Health Organization. Health and human rights, 2016; World Health Organization, 2013; The Homeless Hub, 2016a). Degrees of homelessness exist, where individuals may (1) experience absolute homelessness, sleeping in locations not intended for human habitation; (2) make use of emergency shelters, such as those providing habitation overnight or as a respite from domestic violence; (3) be provisionally accommodated; or (4) be considered at risk of becoming homeless (The Homeless Hub, 2012). Individuals who experience homelessness face marked disparities in health compared to those with residential stability (Fazel et al., 2014). An international estimate of average life expectancy for individuals facing homelessness is 42–52 years, while life expectancy for housed individuals is 80 years (O’Connell, 2005). Individuals experiencing homelessness also face higher rates of non-communicable diseases compared to those with stable housing (Wright & Tompkins, 2006; O’Carroll & O’Reilly, 2008). Further, individuals experiencing homelessness face difficulty accessing health services despite having high and complex health needs (Robertson & Cousineau, 1986; Silvestrini et al., 2016). Specific to the Canadian context, studies have robustly characterized ambulatory, emergency, and inpatient health service utilization among cohorts of individuals facing homelessness and housing instability, documenting challenges in access to care and unmet medical needs (Stergiopoulos et al., 2016; Jaworsky et al., 2016). Recent scholarship has demonstrated that when complex populations including individuals of lower socio-economic status do gain access to the health system, they represent very high users of health services (Rosella et al., 2014). Taken together, these findings speak to the various facets that must be considered by the medical, social services, and public health sectors in taking action on improving health for individuals experiencing homelessness.
Primary healthcare plays a key role in the healthcare system toward improved health outcomes and reduced care costs (World Health Organization, 2008; Starfield et al., 2005). In the vein of designing strategies to mitigate the adverse impacts of the social determinants of health, further primary care utilization studies can offer valuable insight. Most medical care is delivered through family medicine, where in many countries, primary care constitutes an individual’s first-point-of-contact with the healthcare system (World Health Organization, 2008; Starfield et al., 2005). Variations in patient-provider relationships exist within family medicine, where a consistent, long-term relationship with a family physician has the strongest potential to promote health and well-being (College of Family Physicians of Canada, 2012). The practice of family physicians rostering patients to become registered within their practice and establish a long-term commitment to the patient-physician relationship is gaining traction in Canada and is recommended by the College of Family Physicians of Canada (College of Family Physicians of Canada, 2012). Rostering confers significant advantages for patient-centered care by treating the family medicine practice as a “medical home” from which specialty care, social services, and public health interventions might be centrally coordinated. A recent study using population administrative data in Ontario, Canada, demonstrated positive impacts of family medicine rostering on reduced utilization of hospital care (Tiagi & Chechulin, 2014). For vulnerable populations including individuals who face homelessness, previous studies have demonstrated that registration with a family physician for this population confers benefits, including increased access to needed hospital and specialist care (Shortt et al., 2008; Elwell-Sutton et al., 2016). For individuals experiencing homelessness, a study of primary care utilization once individuals have gained access to family medicine and become rostered with a primary care physician has not occurred. This work seeks to augment the scholarship on care utilization for individuals facing homelessness, with the objective of elucidating the relationship between homelessness status and frequency of visits to rostered primary care providers.
Methods
Setting
This study took place in Calgary, Alberta, Canada. Calgary, with 1.2 million residents, is Canada’s fourth largest city and has been characterized as having low population density relative to the three larger Canadian cities of Toronto, Vancouver, and Montreal (Calgary Economic Development, 2016; Alberta Health Services, 2016). Calgary has a large population of individuals experiencing homelessness, which has been estimated at 3222 in 2016 (The Homeless Hub. Calgary, 2016b). Homelessness-oriented health and social services in Calgary are administered by a breadth of organizations and levels of government, which include Alberta Health, the provincial health ministry; Alberta Health Services, which is the centralized health services administration organization in the province; the City of Calgary; and a number of non-profit agencies (Calgary Homeless Foundation, 2016).
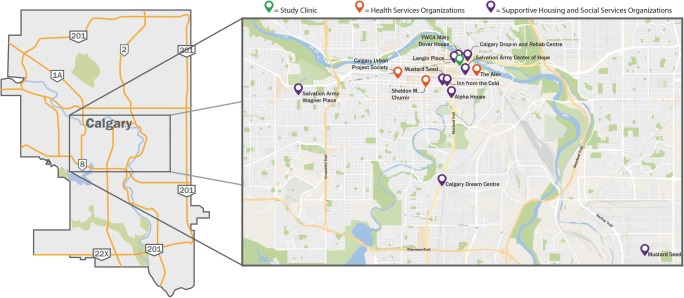
The community primary care clinic that contributed data to this study is uniquely situated to offer health services to marginalized populations in Calgary, with its position depicted visually within Calgary in Fig. 1. This clinic was not developed with a mandate to serve marginalized groups either exclusively or primarily and therefore does not provide the same degree of supports that other homeless-dedicated health facilities would have, such as case manager/social workers or mental health and addiction medical primary care or specialist providers. In contrast, the Calgary Urban Project Society (CUPS) primary care clinic and Sheldon Chumir Health Centre are examples of facilities in Calgary’s inner city that offer such dedicated health and social supports for the marginalized groups. The clinic under study is geographically situated in a convenient location relative to housing facilities, social services, and health service agencies designed to cater to marginalized groups and thus rosters several such patients. In Alberta, the majority of primary care clinics utilize fee-for-service remuneration; a small number of clinics (five) in the province are remunerated via capitation models (Government of Alberta, 2017).
Fig. 1.
Map of Calgary, Alberta, Canada, illustrating the geographic location of the family medicine clinic under study relative to housing organizations and social support organizations
Study design and data source
We undertook a retrospective chart review to elicit the association between homelessness status and the frequency of visits to primary care at the clinic under study. The dataset used to explore the study objective was created by abstracting data from the clinic’s electronic medical record, HealthQuest (Microquest, 2017). Patients whose records were eligible to enter the cohort were those rostered to primary care physicians at the clinic. The rostering process occurred independently of this study as part of routine clinical care. Rostering at this clinic entails verbal affirmation from the patient when medical office administrative staff would inquire whether the patient considered themselves to be a patient belonging to a family physician’s roster (i.e., medical office administration would ask “do you consider Dr. [surname] to be your family physician?”).
Our research team initially intended to abstract data for all physicians practicing at the clinic. However, we carried out a statistical power calculation based on abstraction of one physician’s patient panel and determined that this preliminary abstraction and data analysis constituted a sufficient sample size to explore the association of interest at α = 0.05 and β = 0.20 (data not shown). To account for variations between physician practice styles, we abstracted data from patient panels belonging to three primary care physicians practicing at the clinic who consented to have their patient panels abstracted. The family physician to whom the roster belonged was responsible for deriving the homelessness status variable for each patient in their roster. Three physicians’ rosters were included in this study. At the time of the study, five physicians were practicing at the clinic.
Study measures
This study investigated the relationship between homelessness status, serving as the study’s primary predictor, and the rate of visits to primary care, serving as the study’s primary outcome. Homelessness status was defined as whether the patient had been sheltered at overnight shelters and/or emergency/provisional housing at any point during the study interval (July 1, 2015 to July 25, 2016). This was a derived binary variable created by the research team’s family physicians who were familiar with the social and medical histories of their rostered patients. The primary study outcome, rate of visits to primary care, was defined as the count of visits associated with a patient accounting for the length of that patient’s relationship with their primary care physician. Length of relationship was estimated as a number of days, using the date that a patient joined the physician roster subtracted from the date of data query (July 25, 2016). Other variables abstracted included birthdate to calculate age on the date of data query, sex, and primary care physician to whom the patient was registered to (rostered).
Statistical analysis
Descriptive statistics were generated to characterize study variables, using means and standard deviations for continuous variables and frequencies and proportions for categorical variables. To compare measures between groups, we used t tests for continuous variables and chi-squared tests for categorical variables. We used negative binomial regression to elucidate the relationship between current homelessness status and the rate of visits to primary care, a count outcome. We initially considered the use of a Poisson regression model to explore this association but did not proceed since the variance of the primary study outcome was far greater than the mean which precludes the use of this method. We used multivariate methods to estimate the magnitude of the impact of homelessness status on primary care visit frequency, where we adjusted for patient age, sex, and physician. We also generated by-sex associations adjusted for age and physician. Data analysis took place using SAS Statistical Software, Version 9.4 (Cary, NC).
Ethics
This study received ethical approval from the Conjoint Health Research Ethics Board at the University of Calgary (REB 16-1329).
Results
Cohort characterization
We studied a cohort of patients rostered to family medicine physicians, who presented to an inner-city community primary care clinic in Calgary, Canada, between July 1, 2015 and August 30, 2016 (Table 1). The study analyzed data from 1013 patients rostered to three family physicians. Of the cohort, 112 patients (11.1%) were characterized as experiencing homelessness at any point during the specified study period where 901 were considered stably housed (88.9%). The cohort was 51% female (n = 521) and 49% male (n = 492). Patients who experienced homelessness during the study period were 73.2% male, while stably housed patients were 45.5% male (p < 0.0001). Among the three physician rosters studied, there was a variation in the proportion of patients experiencing homelessness, where one roster had 4% and the others saw 12% and 15%. The mean number of visits to the primary care clinic under study was 4.8 (SD 5.1) for the full cohort, where the mean count of visits between patients experiencing homelessness (mean 9.6, SD 10.5) and patients who were stably housed (mean 4.2, SD 3.6) was significantly different (p < 0.0001) (Table 2). The average number of days since patients in the cohort had been rostered to family medicine was 263 (SD 107). The mean rate of visiting primary care for this patient population was 7.6 visits per year (SD 7.7), where the rate varied between patients who had experienced homelessness during the study period (mean 14.6, SD 14.1) and patients who were stably housed (mean 6.7, SD 5.9) (p < 0.0001).
Table 1.
Cohort demographics
| Full cohort, N = 1013 | Patients stably housed, N = 901 | Patients experiencing homelessness, N = 112 | p value | |
|---|---|---|---|---|
| Patients belonging to all physicians | 1013 | 901 (88.9) | 112 (11.1) | |
| Patients in physician 1’s roster | 427 | 375 (87.8) | 52 (12.2) | < 0.0001 |
| Patients in physician 2’s roster | 250 | 239 (95.6) | 11 (4.4) | |
| Patients in physician 3’s roster | 336 | 287 (85.4) | 49 (14.6) | |
| Age, years (mean, SD) | 38.7 (16.5) | 37.2 (16.3) | 50.6 (13.3) | < 0.0001 |
| Age category (n, row %) | ||||
| < 45 years old | 678 | 644 (95.0) | 34 (5.0) | < 0.0001 |
| 45–60 years old | 215 | 167 (77.7) | 48 (22.3) | |
| > 60 years old | 120 | 90 (75.0) | 30 (25.0) | |
| Gender (n, row %) | ||||
| Female | 521 | 491 (94.2) | 30 (5.8) | < 0.0001 |
| Male | 492 | 410 (83.3) | 82 (16.7) | |
Table 2.
Characterization of visits to primary care for patients included in the study cohort
| Full cohort, N = 1013 | Patients stably housed, N = 901 | Patients experiencing homelessness, N = 112 | p value | |
|---|---|---|---|---|
| Number of visits (mean, SD) | 4.8 (5.1) | 4.2 (3.6) | 9.6 (10.5) | < 0.0001 |
| Length of relationship (mean, SD) [days since joining roster] | 263 (107) | 262 (106) | 272 (110) | < 0.0001 |
| Rate of visits (mean, SD) [number of visits/years rostered] | 7.6 (7.7) | 6.7 (5.9) | 14.6 (14.1) | < 0.0001 |
| High user, top 5% of patient rates (n, %) | ||||
| Non-high user | n = 962 (95.0%) | n = 874 (90.9%) | n = 88 (9.15%) | < 0.0001 |
| High user | n = 51 (5.0%) | n = 27 (52.9%) | n = 24 (47.1%) | |
We conducted an analysis of the top 5% of the patient cohort with the highest rates of visiting primary care, representing 51 patients of the 1013 patients in the full cohort (Table 2). Of these high users of primary care, 47.1% had experienced homelessness during the study period (n = 24), whereas 9.15% of those not in the top 5% had experienced homelessness.
Impact of homeless status on rostered primary care utilization
Our analyses found strong associations when comparing the rate of visits to primary care between patients experiencing homelessness and stably housed patients using negative binomial regression methods (Table 3). For the total cohort, the multivariate adjusted model indicated that the rate of homeless individuals accessing primary care physicians was 2.02 times greater than the rate for stably housed individuals (rate ratio [RR] 2.02, 95% confidence interval [95% CI] 1.74–2.35; p < 0.0001) when adjusted for age, sex, and including family physician as a variable in the model. We also characterized the relationship between homelessness status and the frequency of accessing primary care health services according to sex. When stratified by sex, the rate of accessing primary care health services was 2.05 times greater for men experiencing homelessness compared to those who were stably housed (RR 2.05, 95% CI 1.69–2.50, p < 0.0001). For females, our analyses indicated a rate ratio of 1.55 (95% CI 1.21–1.98, p < 0.0001) when comparing women who faced homelessness or were housed in shelters during the study period compared to women who were stably housed.
Table 3.
Negative binomial regression for rostered primary care utilization, comparing patients stably housed and those experiencing homelessness
| Estimate, unadjusted | Estimate, adjusted for physician | Estimate, adjusted for physician and demographics | |
|---|---|---|---|
| Total cohort | β 0.82 (95% CI 0.67, 0.95), RR 2.25 (95% CI 1.95, 2.59) p < 0.0001 | β 0.77 (95% CI 0.63, 0.91), RR 2.15 (95% CI 1.87, 2.59), p < 0.0001 | β 0.70 (0.55, 0.85), RR 2.01 (95% CI 1.73, 2.34)*, p < 0.0001 |
| Females only | β 0.48 (95% CI 0.23, 0.73), RR 1.61 (95% CI 1.26, 2.08), p < 0.0001 | β 0.45 (95% CI 0.21, 0.70), RR 1.57 (95% CI 1.23, 2.01), p = 0.0003 | β 0.53 (95% CI 0.27, 0.79), RR 1.70 (95% CI 1.31, 2.21)†, p = 0.0004 |
| Males only | β 0.87 (95% CI 0.70, 1.06), RR 2.41 (95% CI 2.00, 2.89), p < 0.0001 | β 0.85 (95% CI 0.67, 1.04), RR 2.34 (95% CI 1.95, 2.82), p < 0.0001 | β 0.67 (95% CI 0.46, 0.87), RR 1.95 (95% CI 1.59, 2.40)†, p < 0.0001 |
*Adjusted for continuous age, gender, and physician roster
†Adjusted for continuous age and physician roster
Discussion
Our work indicates that for a population accessing rostered primary care in the core of Calgary, Canada, individuals who experienced homelessness had an increased rate of visits to primary care providers compared to patients who were stably housed. The large and significant magnitude of these associations persisted upon multivariate adjusting of the model for patient age, sex, and family physician. Upon stratifying the results by sex, we found that the effect size of the impact of homelessness status on the rate of accessing primary care health services was larger for male patients than for female patients.
Acknowledging that this investigation lacked information regarding diagnoses and chief complaints, on the basis of our findings in conjunction with existing literature, we hypothesize that the mechanism by which individuals who experience homeless visit primary care at an increased rate compared to stably housed patients is complex (Fransham & Dorling, 2018; Hwang & Burns, 2014). For individuals facing homelessness, what would be relatively straightforward primary care concerns for stably housed patients may manifest as an urgent or emergency health issue in this complex population, often at great cost to the healthcare system (Fleisch & Nash, 2017). Notably, disadvantaged populations face barriers and challenges in their interactions with the health system that may translate to having to access their primary care provider more often than stably housed patients. We hypothesize that such challenges may include struggles with compliance and adherence to medications or health regimes, requiring clarification or additional visits to replace lost or stolen prescriptions, medications, or health supports. As well, primary care may be the sole access point to the health system for many patients, where specialist or mental health services may be difficult to access. Such poor access to non-primary care might occur as a result of these facilities being located in inconvenient areas for an individual who relies on transit or walking, limited patient ability to navigate the health system, and the limited length of time that specialist referrals remain active (i.e., if a patient does not follow up to schedule or does not attend the appointment, the referral is closed). Additionally, supporting optimal health of the homeless and precariously housed may require the family physician to provide assistance navigating the often-complex network of social supports and administrative tasks required to support their patients’ needs. Finally, challenges to optimal health literacy may compound all of these barriers (Glazier, 2007; Schillinger et al., 2017). However, we advocate that further work to illuminate causal inferences between homelessness and high rates of visiting primary care would be a worthy next step to build on this study’s findings.
We also noted sex-specific differences in the association between homelessness status and accessing primary care, where the magnitude of the relationship between the rate of visits to primary care and homelessness is greater for males than for females. We note that the smaller rate ratio observed for women may stem from the propensity for females to seek health services more frequently than male patients regardless of homelessness status, where these gender differences have been consistent and well characterized in previous studies (Bertakis et al., 2000; de Moraes et al., 2017).
This work has several limitations to acknowledge. We drew on a limited sample to investigate the study association of interest, which limits generalizability of our findings. We were limited to the unique situation of the clinic under study as well as lack of coordination of primary care EMR data between clinics and were not able to include other clinics to contribute to a larger sample. Another limitation of this work relates to the lack of feasibility regarding the extraction of free-text clinical notes in the electronic medical record to abstract information, such as chief complaint, to provide greater depth to our study. The interface of the EMR requires manual extraction of free-text clinical notes from each patient encounter individually to obtain this data. We propose that exploring our study association with adjustment for comorbidity indices such as Aggregated Diagnosis Groups or Charlson Comorbidity Index would be valuable future directions to build on this work (Charlson et al., 2008). Another limitation relates to potential misclassification of patients according to homelessness status. There is difficulty inherent in accurately capturing an individual’s situation along the spectrum of experiencing absolute homelessness (sleeping in areas unfit for human habitation), residing in provisional housing or shelters, being at risk of becoming homeless, and being stably housed. We derived our homelessness status variable based on documented addresses for each patient and clinician knowledge of each patient’s social history, but acknowledge that more accurate methods to capture homelessness status might be to issue questionnaires during patient encounters to inform prospective studies. Finally, this study is limited in that we did not extract ICD-9 codes for all patient visits and were not able to adjust our results for a morbidity index. However, this study has strengths to note. To our knowledge, this is the first work to have conducted a comparison between homeless and non-homeless individuals and their rate of accessing primary care health services. We drew on the unique situation of the community primary care clinic under study and made use of point-of-care health administrative data to elucidate an association that most primary care settings are not positioned to provide. As such, we propose that this study provides an augmentation to the state of knowledge surrounding homelessness and the experience of individuals facing homelessness and seeking to access health services. Further, we were fortunate to have several family physicians as part of the research team who served as active participants in the research process and contributed perspectives observed from their work as front-line practitioners with the marginalized populations our work studied.
While we acknowledge many limitations in this work, we foresee that our findings have relevance for health decision-makers involved in designing solutions to reduce health disparities. For system planners and the public health community, we note implications in regard to limited data available to study the social determinants of health, especially for the most vulnerable segments of the population where the impacts of health disparities are most marked. This work was a pragmatic study that extracted elements readily available from a family medicine EMR, collected as part of routine clinical care. The social history variables, including housing status, implemented in this clinic are likely not standard across other electronic medical record systems, creating difficulty in developing a robust understanding of healthcare experiences for vulnerable populations. As such, the public health and epidemiology communities involved in designing and utilizing data capture systems might work together with clinical providers to develop data systems to be used in routine clinical care and social service provision. As well, we advocate that healthcare policy decision-makers should take heed of these results that demonstrate the disproportionate burden of visits to primary care that homeless patients represent in the total visits to family medicine physicians. The health policy landscape in Canada is shifting toward the consideration of alternate physician remuneration schemes where incentives might be implemented to promote high-quality, relationship-based primary care for complex populations. System planners and decision-makers involved in influencing these policies, too, should consider the responsibility of medicine and public health to support and promote equity of access to care and overall health for all Canadians regardless of socio-economic position. Finally, it is advantageous for population health practitioners and the frontline medical and social services communities to be aware of utilization patterns in primary care for vulnerable populations. The College of Family Physicians of Canada encourages the country’s primary care sector to implement rostered, relationship-based family medicine, acting as a coordinator between a patient’s primary care, specialty care, and public health and preventive medicine needs (The College of Family Physicians of Canada, 2011). As this model takes hold in Canada, there will be an increased requirement for medicine and public health professionals to collaborate in their shared goal of acting on the adverse impacts on the social determinants of health for those populations who face the greatest disparities, including those experiencing homelessness.
Compliance with ethical standards
This study received ethical approval from the Conjoint Health Research Ethics Board at the University of Calgary (REB 16-1329).
References
- Alberta Health Services (2016) Urban sprawl and health
- Bertakis KD, Azari R, Helms LJ, et al. (2000) Gender differences in the utilization of health care services. J Fam Pract. (Accessed March 7, 2017);49(2):147–52. Available at: http://www.ncbi.nlm.nih.gov/pubmed/10718692 (Accessed March 7, 2017). [PubMed]
- Calgary Economic Development (2016)Calgary Population Statistics. Available at: http://www.calgaryeconomicdevelopment.com/research-and-reports/demographics-lp/demographics/ (Accessed February 18, 2017).
- Calgary Homeless Foundation (2016) People First Strategy. (Accessed February 19, 2017). Available at: http://calgaryhomeless.com/homelessness-in-calgary/people-first-strategy/ (Accessed February 19, 2017).
- Charlson Mary E., Charlson Robert E., Peterson Janey C., Marinopoulos Spyridon S., Briggs William M., Hollenberg James P. The Charlson comorbidity index is adapted to predict costs of chronic disease in primary care patients. Journal of Clinical Epidemiology. 2008;61(12):1234–1240. doi: 10.1016/j.jclinepi.2008.01.006. [DOI] [PubMed] [Google Scholar]
- College of Family Physicians of Canada (2012) Patient rostering in family practice. (Accessed April 2, 2018). Available at: http://www.cfpc.ca/uploadedFiles/Health_Policy/CFPC_Policy_Papers_and_Endorsements/CFPC_Policy_Papers/BestAdvice_RosteringFINALOct30.pdf (Accessed April 2, 2018).
- Elwell-Sutton T, Fok J, Albanese F, et al. Factors associated with access to care and healthcare utilization in the homeless population of England. J Public Heal. 2016;39(1):26–33. doi: 10.1093/pubmed/fdw008. [DOI] [PubMed] [Google Scholar]
- Fazel S, Geddes JR, Kushel M (2014) The health of homeless people in high-income countries: descriptive epidemiology, health consequences, and clinical and policy recommendations. Lancet (London, England). (Accessed February 19, 2017);384(9953):1529–40. Available at: http://linkinghub.elsevier.com/retrieve/pii/S0140673614611326 (Accessed February 19, 2017). [DOI] [PMC free article] [PubMed]
- Fleisch Sheryl B., Nash Robertson. Medical Care of the Homeless. Primary Care: Clinics in Office Practice. 2017;44(1):57–65. doi: 10.1016/j.pop.2016.09.009. [DOI] [PubMed] [Google Scholar]
- Fransham M, Dorling D. Homelessness and public health. BMJ. 2018 (Accessed April 2, 2018);360:k214. Available at: http://www.ncbi.nlm.nih.gov/pubmed/29378686 (Accessed April 2, 2018). [DOI] [PubMed]
- Glazier Richard. Balancing Equity Issues in Health Systems: Perspectives of Primary Healthcare. HealthcarePapers. 2007;8(sp):35–45. doi: 10.12927/hcpap.2007.19218. [DOI] [PubMed] [Google Scholar]
- Government of Alberta (2017) Blended Capitation Clinical ARP model. Available at: http://www.health.alberta.ca/professionals/ARP-Clinical-capitation.html (Accessed April 3, 2018).
- Hwang SW, Burns T (2014) Health interventions for people who are homeless. Lancet (London, England). (Accessed April 2, 2018);384(9953):1541–7. Available at: http://www.ncbi.nlm.nih.gov/pubmed/25390579 (Accessed April 2, 2018). [DOI] [PubMed]
- Jaworsky Denise, Gadermann Anne, Duhoux Arnaud, Naismith Trudy E., Norena Monica, To Matthew J., Hwang Stephen W., Palepu Anita. Residential Stability Reduces Unmet Health Care Needs and Emergency Department Utilization among a Cohort of Homeless and Vulnerably Housed Persons in Canada. Journal of Urban Health. 2016;93(4):666–681. doi: 10.1007/s11524-016-0065-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Microquest (2017) Healthquest Electronic Medical Record Software. Available at: http://www.microquest.ca/healthquest/Electronic-Records.aspx (Accessed February 19, 2017).
- Moraes Suzana Alves de, Lopes Daniele Almeida, Freitas Isabel Cristina Martins de. Sex-specific differences in prevalence and in the factors associated to the search for health services in a population based epidemiological study. Revista Brasileira de Epidemiologia. 2014;17(2):323–340. doi: 10.1590/1809-4503201400020004ENG. [DOI] [PubMed] [Google Scholar]
- O'Carroll A., O'Reilly F. Health of the homeless in Dublin: has anything changed in the context of Ireland's economic boom? The European Journal of Public Health. 2008;18(5):448–453. doi: 10.1093/eurpub/ckn038. [DOI] [PubMed] [Google Scholar]
- O’Connell JJ (2005) Premature mortality in homeless populations: a review of the literature
- Robertson MJ, Cousineau MR. Health status and access to health services among the urban homeless. Am J Public Heal. 1986;76:561–563. doi: 10.2105/AJPH.76.5.561. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rosella LC, Fitzpatrick T, Wodchis WP, et al. (2014) High-cost health care users in Ontario, Canada: demographic, socio-economic, and health status characteristics. BMC Health Serv Res. (Accessed May 16, 2018);14(1):532. Available at: http://bmchealthservres.biomedcentral.com/articles/10.1186/s12913-014-0532-2 (Accessed May 16, 2018). [DOI] [PMC free article] [PubMed]
- Schillinger Dean. Association of Health Literacy With Diabetes Outcomes. JAMA. 2002;288(4):475. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Shortt S.E.D., Hwang Stephen, Stuart Heather, Bedore Melanie, Zurba Nadia, Darling Margaret. Delivering Primary Care to Homeless Persons: A Policy Analysis Approach to Evaluating the Options. Healthcare Policy | Politiques de Santé. 2008;4(1):108–122. doi: 10.12927/hcpol.2008.20012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Silvestrini G, Federico B, Damiani G, et al. (2016) Healthcare utilization among urban homeless followed by an outpatient clinic: more intensive use by migrant groups. Eur J Public Health. (Accessed March 29, 2018);27(1):ckw108. Available at: http://www.ncbi.nlm.nih.gov/pubmed/28177446 (Accessed March 29, 2018). [DOI] [PubMed]
- Starfield B, Shi L, Macinko J (2005) Contribution of primary care to health systems and health. Milbank Q. (Accessed April 10, 2018);83(3):457–502. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16202000 (Accessed April 10, 2018). [DOI] [PMC free article] [PubMed]
- Stergiopoulos V, Gozdzik A, Misir V, et al. (2016) The effectiveness of a Housing First adaptation for ethnic minority groups: findings of a pragmatic randomized controlled trial. BMC Public Health. (Accessed April 2, 2018);16(1):1110. Available at: http://www.ncbi.nlm.nih.gov/pubmed/27769226 (Accessed April 2, 2018). [DOI] [PMC free article] [PubMed]
- The College of Family Physicians of Canada (2011) A vision for Canada: family practice: the patient’s medical home. Mississauga (Accessed April 2, 2018). Available at: http://www.cfpc.ca/A_Vision_for_Canada_Family_Practice_2011/ (Accessed April 2, 2018).
- The Homeless Hub (2012) Canadian definition of homelessness. (Accessed February 26, 2017). Available at: http://homelesshub.ca/homelessdefinition (Accessed February 26, 2017).
- The Homeless Hub (2016a) The state of homelessness in Canada. (Accessed February 19, 2017). Available at: http://homelesshub.ca/SOHC2016 (Accessed February 19, 2017).
- The Homeless Hub (2016b) Calgary Alberta. Canadian observatory on homelessness. Available at: http://homelesshub.ca/community-profiles/alberta/calgary
- Tiagi Raaj, Chechulin Yuriy. The Effect of Rostering with a Patient Enrolment Model on Emergency Department Utilization. Healthcare Policy | Politiques de Santé. 2014;9(4):105–121. doi: 10.12927/hcpol.2014.23809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- World Health Organization (2008) The World Health Report —primary health care (Now More Than Ever). WHO. World Health Organization; 2013 (Accessed April 10, 2018). Available at: http://www.who.int/whr/2008/en/ (Accessed April 10, 2018).
- World Health Organization (2013) Commission on Social Determinants of Health. WHO.
- World Health Organization (2016) Health and human rightsWorld Health Organization. World Health Organization
- Wright NMJ, Tompkins CNE (2006) How can health services effectively meet the health needs of homeless people? Br J Gen Pract. (Accessed November 28, 2016);56(525):286–93. Available at: http://www.ncbi.nlm.nih.gov/pubmed/16611519 (Accessed November 28, 2016). [PMC free article] [PubMed]