Abstract
Objectives
To examine co-occurring mental health problems among a population-based sample of high school students in Ontario, Canada, to understand their prevalence, associated risk factors, and relationship with mental health service access and utilization.
Methods
The data were derived from the 2013 Ontario Student Drug Use and Health Survey, a biennial survey of students attending publicly funded Ontario schools, from a subsample of students who completed both the internalizing and substance use portions of the survey (n = 2945). Rates of co-occurring problems were calculated for the previous 12 months. Service use for students with co-occurring problems was also calculated for the past 12 months. Odds ratios were estimated using binary logistic regression models correcting for the survey design.
Results
In an adjusted model, youth with internalizing symptoms were 2.40 times more likely and youth with substance use problems were 2.24 times more likely to have accessed mental health services during the past 12 months than youth without these problems. Youth with co-occurring internalizing and substance use problems were 6.74 times more likely (95% CI 4.66–9.76, p < 0.001) to have accessed mental health services during the past year compared with youth without co-occurring problems, but only 52.8% of youth with co-occurring problems (95% CI 45.6–59.9%) used mental health services.
Conclusions
The findings suggest that just over half of Ontario students in grades 9 through 12 who have co-occurring internalizing and substance use problems are utilizing mental health services. Further research should examine the factors related to service use in this population in order to better inform policy and program development.
Keywords: Adolescents, Health services, Substance-related disorders, Depression
Résumé
Objectifs
Examiner les troubles de santé mentale concomitants dans un échantillon populationnel d’élèves du secondaire en Ontario, au Canada, pour comprendre la prévalence de ces troubles, les facteurs de risque associés et leurs liens avec l’accès et le recours aux services de santé mentale.
Méthode
Nos données sont dérivées du Sondage sur la consommation de drogues et la santé des élèves de l’Ontario de 2013, une enquête bisannuelle auprès des élèves fréquentant l’école publique dans la province; elles proviennent d’un sous-échantillon d’élèves ayant rempli à la fois les parties du sondage sur l’intériorisation et sur la consommation de substances (n = 2 945). Les taux de problèmes concomitants ont été calculés pour les 12 mois antérieurs. L’utilisation des services par les élèves présentant des problèmes concomitants a aussi été calculée pour les 12 mois antérieurs. Les rapports de cotes ont été estimés au moyen de modèles de régression logistique binaires après correction du plan de sondage.
Résultats
Selon un modèle ajusté, les jeunes présentant des symptômes d’intériorisation étaient 2,40 fois plus susceptibles, et les jeunes présentant des problèmes de consommation de substances, 2,24 fois plus susceptibles, d’avoir eu accès à des services de santé mentale au cours des 12 mois antérieurs que les jeunes ne présentant pas de tels problèmes. Les jeunes ayant des problèmes concomitants d’intériorisation et de consommation de substances étaient 6,74 fois plus susceptibles (IC de 95 % : 4,66-9,76, p < 0,001) d’avoir eu accès à des services de santé mentale au cours de l’année antérieure que les jeunes sans problèmes concomitants, mais seulement 52,8 % des jeunes ayant des problèmes concomitants (IC de 95 % : 45,6 %-59,9 %) avaient utilisé des services de santé mentale.
Conclusions
Ces résultats indiquent qu’un peu plus de la moitié des élèves de l’Ontario de la 9e à la 12e année ayant des problèmes concomitants d’intériorisation et de consommation de substances ont recours aux services de santé mentale. Il faudrait pousser la recherche pour examiner les facteurs liés à l’utilisation des services dans cette population afin d’éclairer l’élaboration des politiques et des programmes.
Mots-clés: Adolescents, Services de santé, Troubles liés à une substance, Dépression
Introduction
An estimated 23.4% of Canadians aged 9–19 years are living with mental illness (Mental Health Commission of Canada 2013), with anxiety and mood disorders presenting as the most prevalent in adolescents (Mann et al. 2011). National surveys estimate the prevalence of severe substance use disorders (SUDs) among adolescents is between 2% and 5% (Sterling et al. 2010). Despite the common co-occurrence of mental illness and SUDs, relatively little is known about youth living with co-occurring problems. Based on surveys conducted in the general population, it is estimated that among youth with a current SUD, approximately 65–75% also have co-occurring mental health disorders. The rates are even higher if youth with only psychiatric symptoms (not meeting the threshold for diagnosis) are included (Diamond et al. 2006). Co-occurring problems in youth are associated with academic problems, relationship difficulties, and higher rates of suicide attempts and completions (Cummings et al. 2014). Youth with co-occurring problems also have greater severity of disorders, poorer prognoses, increased treatment challenges, and greater unmet needs for treatment compared to individuals with either type of disorder alone (Cummings et al. 2014; Lundkvist-Houndoumadi and Thastum 2017; Urbanoski et al., 2007). Nevertheless, very little is known about this group with respect to the nature of the care these youth receive.
While it is well established that externalizing disorders such as Attention Deficit Hyperactivity Disorder (ADHD), Conduct Disorder, and Oppositional Defiant Disorder frequently co-occur with SUDs (Dirks et al. 2017; Miranda et al. 2016; Ottosen et al. 2016; van Emmerik-van Oortmerssen et al. 2014), relatively less attention has been paid to the co-occurrence between SUD and internalizing problems such as depression and anxiety. It has been estimated that up to 24–50% of youth with SUDs also have depression (Hersh et al. 2014; Kaminer 2016); these disorders are associated in both the general population and clinical samples (Hersh et al. 2014; Kaminer 2016). While SUDs also appear to co-occur with anxiety disorders (Kaminer 2016), the association across the class of disorders is weaker (Essau et al. 2018), likely because youth with certain anxiety disorders (e.g., separation anxiety disorder) are likely to initiate substance use later compared to children with other anxiety disorders (e.g., generalized anxiety disorder). These previous research findings suggest that the co-occurrence of depression, anxiety, and substance use needs to be further examined.
While the negative impact of co-occurring problems on treatment efficacy has been well described (Cheung et al. 2010), very little is known about the effect of comorbidity on service use among youth. Limited studies of co-occurring problems in youth, as well as research in adults suggest that while people with co-occurring problems use more mental health services, they are more likely to report unmet need (Urbanoski et al., 2007). In a study of the general population in Ontario, unmet needs were also found to be higher among adolescents and females, with acceptability barriers as a contributing factor, with a preference to self-manage their problems as a result of their attitudes towards mental illness and health care providers (Andrade et al. 2014). Given the significant burden of mental illness and substance use disorders on adolescents in Canada, there is a need to examine adolescents’ patterns of service utilization and their unmet need for services. Therefore, the purpose of this study is to examine co-occurring internalizing symptoms and substance use problems among a population-based sample of Ontario students in order to understand their prevalence, associated risk factors, and relationship with mental health service access and utilization.
Methods
Survey and participants
The data used in this study were derived from the 2013 cycle of the Ontario Student Drug Use and Health Survey (OSDUHS), a biennial survey of students attending publicly funded schools in Ontario, Canada. In this study, we focus on a subpopulation within the OSDUHS dataset, specifically analyzing the results of students who completed both the internalizing and substance use portions of the survey (n = 2945). The 2013 cycle of the questionnaire was administered between November 2012 and June 2013. Four classes from each grade were selected at random (one in each of grades 9 to 12). To maximize data collection, two questionnaires, randomly distributed in a classroom, were employed, one of which contained the substance use and mental health indicators used in the current study. Students completed the questionnaires anonymously. Permission from each randomly selected school was first requested. Subsequently, all students under the age of 18 were required to have received signed parental consent, and all students were required to provide signed assent before they could participate. The OSDUHS protocol was approved by the Research Ethics Board of the Centre for Addiction and Mental Health. Further information on the OSDUHS is available in Boak et al. (2013).
Measures
The survey collected demographic data, including age, sex (0 = female, 1 = male), and birthplace of participants (0 = born outside Canada, 1 = born in Canada). Household data such as rural/urban residence (0 = attend school in town with less than 10,000 people, 1 = attend school in town with more than 10,000 people) and family structure (0 = live with both parents, 1 = split time between two homes) were also collected and examined.
Internalizing symptoms were measured by psychological distress, suicide ideation, and suicide attempts. Psychological distress in the past 12-month period was measured using the Kessler 6-item Psychological Distress Scale (K6) (Cronbach’s Alpha = 0.89) (Kessler et al. 2002). The K6 scale measures symptoms of anxiety and depression, with a score of 8 or higher indicating moderate levels of psychological distress in the past 12 months (Boak et al. 2013; Galea et al. 2007). Students were also asked whether they had seriously considered attempting suicide (0 = no suicide ideation, 1 = suicide ideation) and whether they had actually attempted suicide (0 = no suicide attempts, 1 = suicide attempt). For the multivariate analyses, students were deemed to have internalizing symptoms if they met the criteria for psychological distress measured by the Kessler scale, and/or they reported suicide ideation or a suicide attempt during the past 12 months (0 = no internalizing symptoms, 1 = internalizing symptoms).
Substance-related problems were measured in the OSDUHS using several different validated measures. The OSDUHS includes the Alcohol Use Disorders Identification Test (AUDIT), which was developed by the World Health Organization (Saunders et al. 1993). The AUDIT assesses hazardous and harmful drinking. Hazardous drinking refers to an established pattern of drinking that increases the likelihood of future medical and physical problems (e.g., accidents), whereas harmful drinking refers to a pattern of drinking that is already causing damage to one’s health (e.g., alcohol-related injuries). Those with a score of 8 or more (out of 40) are considered to be drinking at a hazardous or harmful level (Cronbach’s Alpha = 0.84). The “CRAFFT” screener assesses drug use problems experienced by students (Knight et al. 1999). The six items pertain to problems experienced during the past month. A total score of 2 or more (out of 6) problems is used to identify adolescents who have a drug use problem (Cronbach’s Alpha = 0.77). Finally, The Severity of Dependence Scale (SDS) is a validated 5-item scale used to screen for cannabis dependence in adolescent populations (Martin et al. 2006). Each item was scored on a 4-point scale; those with a score of 4 or more (out of 15) are considered to have a potential cannabis dependence problem (Cronbach’s alpha = .81). For the multivariate analyses, students were deemed to have a substance use problem if they met the criteria for hazardous drinking, and/or a drug use problem (0 = no substance use problem, 1 = substance use problem). Students were considered to have a co-occurring mental health internalization and substance use problem if they met the criteria for internalizing symptoms and the criteria for substance use problem.
To measure service use, the OSDUHS includes three questions related to mental health service utilization. The students were asked about seeing a doctor, nurse, or counselor about emotional or mental health problems, having been prescribed medicine to treat anxiety or depression, and having entered a treatment program for drug or alcohol use problems in the past 12 months. Students were considered to have utilized services if they responded positively to any one of the above three questions (0 = did not access mental health services, 1 = accessed mental health services). Furthermore, the OSDUHS asks about feeling the need for help for mental health or emotional problems and compares this to actual mental health service use in the past 12 months to measure unmet mental health service need.
Analytic strategy
A stratified (region and school type), two-stage (school, class) cluster sample design was used, which is representative of Ontario students in grade 9 through grade 12. Post-stratification weights were calculated for the sex-by-grade distributions within each regional stratum separately to ensure that the respondents in each region were proportionate to the population structure. Because the sampling design employs complex sampling methods and unequal probabilities of selection, all confidence intervals (CIs) were corrected for characteristics of the sampling design (i.e., stratification, clustering, and weighting) using Stata 13.1 and applying Taylor series methods. The analysis was based on a design with 19 strata (region × school type), and 181 primary sampling units (schools). All analyses examined the random half-sample of the students who were asked about their substance use. In order to maximize comparability among the different multivariate models, listwise deletion was not used, and all multivariate models were nested with the same sample size (n = 2945) using the markout add-on command available in Stata (Long and Freese 2014). All estimates utilized the weighted data, and all multivariate analyses used binary logistic regression models correcting for the survey design. These binary logistic regression models were assessed at the p < 0.05 level of significance. A more detailed description of the inclusion/exclusion criteria and sampling procedures and weighting of the data can be found in a previous publication (Boak et al. 2013).
Rates of co-occurring problems were calculated for the previous 12 months. Chi-square tests were conducted to examine the data for differences between males and females with co-occurring problems. Service use for students with co-occurring problems was also calculated for the past 12 months. Odds ratios were calculated using binary logistic regression models correcting for the survey design.
Results
Rates of co-occurring internalizing symptoms and substance use problems
Table 1 presents the percentage of participants who met the criteria for internalizing symptoms, substance use problems, and co-occurring internalizing symptoms and substance use problems. Nearly one third of the participants met criteria for internalizing symptoms (31.2%; 95% CI 28.0–34.7%). Over one quarter (27.6%; 95% CI 24.8–30.6%) of students reported having substance use problems related to at least one substance. Overall, 12.0% (95% CI 10.0–14.3%) of the sample reported both internalizing symptoms and substance use problems. Rates of co-occurring problems increased significantly from grades 9 to 12, with 7.5% of grade 9 students meeting criteria for co-occurring problems compared to 14.2% of grade 12 students (p < 0.001).
Table 1.
Demographic and clinical profiles of study population (n = 2945)
| Indicator | Total (SD or 95% CI) | |
|---|---|---|
| Demographics | ||
| Age (mean in years) | 16.01 (15.93–16.10) | |
| Sex (% female) | 50.8% (47.7–53.8%) | |
| Nationality (% born in Canada) | 83.9% (80.0–87.1%) | |
| Location of residence (% rural) | 17.8% (8.1–34.7%) | |
| Living situation (% who spend their time living in ≥ 2 households) | 11.5% (9.9–13.2%) | |
| Substance use problems | ||
| Cannabis dependence | 2.5% (1.7–3.6%) | |
| Drug use problem | 17.0% (14.6–19.7%) | |
| Hazardous/harmful drinking | 19.9% (17.8–22.1%) | |
| Overall substance use problems | 27.6% (24.8–30.6%) | |
| Internalizing symptoms | ||
| Elevated psychological distress | 28.2% (25.3–31.4%) | |
| Suicide ideation | 14.0% (12.1–16.1%) | |
| Suicide attempt | 3.8% (2.9–4.9%) | |
| Overall internalizing symptoms | 31.2% (28.0–34.7%) | |
| Co-occurring problems | ||
| Overall co-occurring problems | 12.0% (10.0–14.3%) | |
Youth with internalizing symptoms, substance use problems, or both had an approximately even sex distribution, a mean age of 16.01 (95% CI 15.93–16.10) years, resided in predominately urban areas (82.2%), and mostly lived in only one household (88.5%).
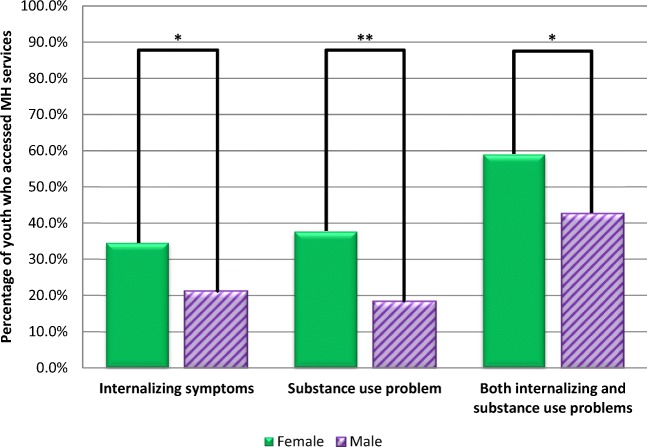
Mental health service access
Table 2 presents the percentage of youth with internalizing symptoms, substance use problems, and co-occurring problems who accessed mental health services during the past 12 months. Fewer youth with substance use problems accessed mental health services (24.2%; 95% CI 15.3–35.9%) than youth with internalizing symptoms (29.4%; 95% CI 23.1–36.7%) or co-occurring problems (52.8%; 95% CI 45.6–59.9%). Mean number of mental health visits by the youth in these groups followed the same pattern (0.70 times, 1.28 times, and 2.73 times, respectively). In each group, more females accessed services than males (Fig. 1). The difference in the proportion of youth with co-occurring problems accessing services from grade 9 through 12 was not statistically significant. A small percentage of youth with substance use problems reported need for mental health services (16.1%; 95% CI 12.0–21.3%), which was less than the percentage who actually accessed services. On the contrary, both youth with internalizing symptoms and co-occurring problems exhibited a higher self-reported need for mental health services (59.7%; 95% CI 53.4–65.6%; and 65.9%; 95% CI 60.7–70.9%; respectively) than actual services accessed. Therefore, the unmet mental health service need for youth with internalizing symptoms and co-occurring problems (40.6% and 27.6%, respectively) was higher than the unmet need for those with substance use problems (9.2%).
Table 2.
Mental health service need and access among Ontario secondary students with internalizing symptoms, substance use problems, and co-occurring problems
| 12-month service history | Internalizing symptoms | Substance use problems | Both internalizing symptoms and substance use problems |
|---|---|---|---|
| Self-reported need for MH services | 59.7% (95% CI 53.4–65.6%) | 16.1% (95% CI 12.0–21.3%) | 65.9% (95% CI 60.7–70.9%) |
| Actual MH services accessed | 29.4% (95% CI 23.1–36.7%) | 24.2% (95% CI 15.3–36.0%) | 52.8% (95% CI 45.6–59.9%) |
| Unmet MH service need | 40.6% (95% CI 34.9–46.7%) | 9.2% (95% CI 6.4–13.3%) | 27.6% (95% CI 22.3–33.5%) |
| Mean number of MH visits | 1.28 (95% CI 0.93–1.63) | .70 (95% CI 0.36–1.04) | 2.73 (95% CI 2.15–3.31) |
MH mental health; n = 2945
Fig. 1.
Sex differences in mental health service access for youth with internalizing, substance use, and comorbid problems. MH mental health;*p < 0.05; **p < 0.01
Table 3 presents the results from a binary logistic regression model, estimating mental health service access during the past year. In model 1, which examined demographic variables, sex and living situation were the only significant predictors of accessing mental health services after adjusting for the other variables. Males were 49% less likely than females to report accessing mental health services during the past year (p < 0.001), and youth who split their time between two or more homes were 1.92 times more likely to access mental health services than those living in one household (p < 0.001). In model 2, which examined clinical variables, each of internalizing problems (OR = 2.68, p < 0.001), substance use problems (OR = 2.04, p < 0.01), and co-occurring problems (OR = 7.20, p < 0.001) significantly predicted the likelihood of youth having used mental health services. In model 3, the full model, youth with internalizing symptoms were 2.40 times more likely than youth without co-occurring problems to have accessed mental health services, and youth with substance use problems were 2.37 times more likely than youth without co-occurring problems to have accessed mental health services during the past 12 months. Youth with co-occurring problems were 6.74 times more likely (95% CI 4.66–9.76, p < 0.001) than students without co-occurring problems to have accessed mental health services during the past year.
Table 3.
Factors associated with mental health service use in logistic regression models
| Variables | Model 1: socio-demographic model | Model 2: illness group model | Model 3: full multivariate model | ||||||
|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | p | AOR | 95% CI | p | AOR | 95% CI | p | |
| Age | 1.05 | 0.95–1.17 | NS | 0.98 | 0.87–1.10 | NS | |||
| Male sex | 0.51 | 0.40–0.64 | < 0.001 | 0.55 | 0.42–0.71 | < 0.001 | |||
| Born in Canada | 0.82 | 0.51–1.31 | NS | 0.75 | 0.45–1.23 | NS | |||
| Rural residence | 1.15 | 0.79–1.68 | NS | 1.17 | 0.79–1.72 | NS | |||
| Multiple households | 1.92 | 1.27–2.91 | < 0.001 | 1.61 | 1.04–2.50 | < 0.05 | |||
| No internalizing or substance use | REF | – | – | REF | – | – | |||
| Internalizing symptoms | 2.68 | 1.81–3.95 | < 0.001 | 2.40 | 1.61–3.57 | < 0.001 | |||
| Substance use problems | 2.04 | 1.23–3.38 | < 0.01 | 2.24 | 1.38–3.64 | < 0.01 | |||
| Co-occurring problems | 7.20 | 5.00–10.37 | < 0.001 | 6.74 | 4.66–9.76 | < 0.001 | |||
Multiple households = individuals who spend their time living in 2 or more households. OR adjusted odds ratio, CI confidence interval, Sig. statistical significance, NS non-significant
Model 1: F(5, 98) = 11.24; p < 0.001; model 2: F(3, 98) = 45.62; p < 0.001; model 3: F(8, 98) = 25.11; p < 0.001
Discussion
In this study, we aimed to better understand the prevalence and demographic factors associated with co-occurring internalizing symptoms and substance use problems among Ontario high school students, and examine their mental health service access and utilization. Among youth with co-occurring problems, about half did not access mental health services during the past year and more than 27% reported unmet need for care. The unmet need is even higher among youth with internalizing symptoms alone at 40%. Our findings suggest that mental health service use increased with comorbid illness, but remained low overall. We found higher rates of mental health service use among females and youth with each of internalizing symptoms and substance use problems as well as co-occurring problems. Whether someone was born in Canada or not did not predict mental health service utilization.
The sex difference towards increased mental health service use among female youth with internalizing symptoms has been established in other studies (Merikangas et al. 2011). However, this persistent gap in access to care among males should remind policy makers, researchers, and clinicians that there is an urgent need to implement sex-specific approaches in designing and promoting services.
Youth with internalizing symptoms and co-occurring problems exhibit higher self-reported need for mental health services than actual services accessed compared to youth with only substance use problems. It is plausible that youth with substance use problems use more services than they perceive they need because they do not view their substance use as problematic but are compelled to attend treatment by parents or conditions of the criminal justice system (i.e., court mandated treatment for driving under the influence) (Daley 2013). Youth with internalizing symptoms or co-occurring problems on the other hand have much greater perceived need than actual care received. Previous research has identified several barriers to access for youth in general, including physical location (storefront) and youth-friendliness of services (Hetrick et al. 2017). Research to improve care for specific subpopulations of youth has generally been lacking, with the exception of early psychosis intervention services. The success of early psychosis intervention programs is a good example of how health services research can aid in the development and implementation of systems of care for specific subpopulations. Therefore, more research is needed to better inform the development of services specific to youth with internalizing symptoms and co-occurring problems.
Our findings are limited by the design of the survey from which we drew our data. While the survey is weighted to be representative of Ontario youth, young people outside of the public school system are excluded. Self-report surveys are prone to response bias, including recall bias and social desirability bias. However, evidence suggests that data collected from youth through anonymous school-based surveys demonstrate higher validity than data collected through other methods (Brener et al. 2003; Deighton et al. 2013). Last, OSDUHS is a cross-sectional survey that does not allow for examination of symptoms and service use over time. Our findings of associations are correlational and do not necessarily imply causation.
Overall, the findings suggest that a large proportion of Ontario students in grades 9 through 12 have problematic internalizing symptoms and substance use, and less than half are utilizing mental health services. Furthermore, the rate of co-occurring problems increases by grade, with almost 15% of grade 12 students meeting criteria. Despite the significant burden associated with these problems, unmet mental health need among young people with internalizing symptoms and co-occurring problems remains high. Future research should examine the factors related to service use in this population in order to better inform policy and program development and address specific barriers for different subpopulations of youth.
Acknowledgements
We want to thank the research support from Ms. Lindsay Williams, Alisha Williams, Connor Ostoich, and Geneva Mason.
Funding
This work was supported by the Canadian Institutes of Health Research [grant number EKT-121928]. Dr. Cheung is supported by the Bell Canada Chair in Adolescent Mood and Anxiety Disorders and the Ontario Mental Health Foundation New Investigator Fellowship. Dr. Kozloff is supported by a NARSAD Young Investigator Grant from the The Brain and Behaviour Research Foundation.
References
- Andrade LH, Alonso J, Mneimneh Z, Wells JE, Al-Hamzawi A, Borges G, Kessler RC. Barriers to mental health treatment: results from the WHO world mental health surveys. Psychological Medicine. 2014;44(6):1303. doi: 10.1017/S0033291713001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boak, A., Hamilton, H., Adlaf, E., & Mann, R. (2013). Drug use among Ontario students, 1977–2013: detailed OSDUHS findings. Toronto, ON: Centre for Addiction and Mental Health. https://www.camh.ca/en/research/news_and_publications/ontario-student-drug-use-and-health-survey/Documents/2013%20OSDUHS%20Docs/2013OSDUHS_Detailed_ DrugUseReport.pdf.
- Brener ND, Billy JO, Grady WR. Assessment of factors affecting the validity of self-reported health-risk behavior among adolescents: evidence from the scientific literature. The Journal of Adolescent Health. 2003;33(6):436–457. doi: 10.1016/S1054-139X(03)00052-1. [DOI] [PubMed] [Google Scholar]
- Cheung A, Mayes T, Levitt A, Schaffer A, Michalak E, Kiss A, Emslie G. Anxiety as a predictor of treatment outcome in children and adolescents with depression. Journal of Child and Adolescent Psychopharmacology. 2010;20(3):211–216. doi: 10.1089/cap.2010.0006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cummings C, Caporino N, Kendall P. Comorbidity of anxiety and depression in children and adolescents: 20 years after. Psychological Bulletin. 2014;140(3):816–845. doi: 10.1037/a0034733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Deighton J, Tymms P, Vostanis P, Belsky J, Fonagy P, Brown A, Martin A, Patalay P, Wolpert M. The development of a school-based measure of child mental health. Journal of Psychoeducational Assessment. 2013;31(3):247–257. doi: 10.1177/0734282912465570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Diamond, G., Panichelli-Mindel, S. M., Shera, D., Dennis, M., Tiims F, & Ungemack, J. (2006). Psychiatric Syndromes in Adolescents with Marijuana Abuse and Dependency in Outpatient Treatment. Journal of Child & Adolescent Substance Abuse, 15(4), 37–54.
- Dirks H, Scherbaum N, Kis B, Mette C. ADHD in adults and comorbid substance use disorder: prevalence, clinical diagnostics and integrated therapy. Fortschritte der Neurologie-Psychiatrie. 2017;85(6):336–344. doi: 10.1055/s-0043-100763. [DOI] [PubMed] [Google Scholar]
- Essau CA, Lewinsohn PM, Lim JX, Ho MR, Rohde P. Incidence, recurrence and comorbidity of anxiety disorders in four major developmental stages. Journal of Affective Disorders. 2018;228:248–253. doi: 10.1016/j.jad.2017.12.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Galea S, Brewin CR, Gruber M, Jones RT, King DW, King LA, Kessler RC. Exposure to hurricane-related stressors and mental illness after Hurricane Katrina. Archives of General Psychiatry. 2007;64(12):1427–1434. doi: 10.1001/archpsyc.64.12.1427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hersh J, Curry JF, Kaminer Y. What is the impact of comorbid depression on adolescent substance abuse treatment? Substance Abuse. 2014;35(4):364–375. doi: 10.1080/08897077.2014.956164. [DOI] [PubMed] [Google Scholar]
- Hetrick SE, Bailey AP, Smith KE, Malla A, Mathias S, Singh SP, McGorry PD. Integrated (one-stop shop) youth health care: best available evidence and future directions. The Medical Journal of Australia. 2017;207(10):S5–S18. doi: 10.5694/mja17.00694. [DOI] [PubMed] [Google Scholar]
- Kaminer, Y. (2016). Youth substance abuse and co-occurring disorders. Washington, DC:American Psychiatric Association Publishing.
- Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand SL, Zaslavsky AM. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Medicine. 2002;32(6):959–976. doi: 10.1017/S0033291702006074. [DOI] [PubMed] [Google Scholar]
- Knight JR, Shrier LA, Bravender TD, Farrell M, Vander Bilt J, Shaffer HJ. A new brief screen for adolescent substance abuse. Archives of Pedicatrics and Adolescent Medicine. 1999;153(6):591–596. doi: 10.1001/archpedi.153.6.591. [DOI] [PubMed] [Google Scholar]
- Lundkvist-Houndoumadi, I., Thastum, M. (2017). Anxious Children and Adolescents Non-Responding to CBT: Clinical Predictors and Families' Experiences of Therapy. Clinical Psychology & Psychotherapy, 24(1), 82–93. [DOI] [PubMed]
- Long, S., & Freese, J. (2014). Regression models for categorical dependent variables using Stata. (3rd edition ed.). College Station, TX: Stata Press.
- Mann RE, Paglia-Boak A, Adlaf EM, Beitchman J, Wolfe D, Wekerle C, Rehm J. Estimating the prevalence of anxiety and mood disorders in an adolescent general population: an evaluation of the GHQ12. International Journal of Mental Health and Addiction. 2011;9(4):410–420. doi: 10.1007/s11469-011-9334-5. [DOI] [Google Scholar]
- Martin G, Copeland J, Gates P, Gilmour S. The Severity of Dependence Scale (SDS) in an adolescent population of cannabis users: Reliability, validity and diagnostic cut-off. Drug and Alcohol Dependence. 2006;83(1):90–93. doi: 10.1016/j.drugalcdep.2005.10.014. [DOI] [PubMed] [Google Scholar]
- Mental Health Commission of Canada (2013). Making the case for investing in mental health in Canada. Calgary, AB: Mental Health Commission of Canada, https://www.mentalhealthcommission.ca/ sites/default/files/2016-06/Investing_in_Mental_Health_FINAL_Version_ENG.pdf.
- Merikangas KR, He JP, Burstein M, Swendsen J, Avenevoli S, Case B, Olfson M. Service utilization for lifetime mental disorders in U.S. adolescents: results of the National Comorbidity Survey-Adolescent Supplement (NCS-A) Journal of the American Academy of Child and Adolescent Psychiatry. 2011;50(1):32–45. doi: 10.1016/j.jaac.2010.10.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Miranda A, Colomer C, Berenguer C, Roselló R, Roselló B. Substance use in young adults with ADHD: comorbidity and symptoms of inattention and hyperactivity/impulsivity. International Journal of Clinical and Health Psychology. 2016;16(2):157–165. doi: 10.1016/j.ijchp.2015.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ottosen C, Petersen L, Larsen JT, Dalsgaard S. Gender differences in associations between attention-deficit/hyperactivity disorder and substance use disorder. Journal of the American Academy of Child and Adolescent Psychiatry. 2016;55(3):227–234. doi: 10.1016/j.jaac.2015.12.010. [DOI] [PubMed] [Google Scholar]
- Saunders JB, Aasland OG, Babor TF, de la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption--II. Addiction. 1993;88(6):791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x. [DOI] [PubMed] [Google Scholar]
- Sterling S, Weisner C, Hinman A, Parthasarathy S. Access to treatment for adolescents with substance use and co-occurring disorders: challenges and opportunities. Journal of the American Academy of Child and Adolescent Psychiatry. 2010;49(7):637–646. doi: 10.1016/j.jaac.2010.03.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Urbanoski KA, Rush BR, Wild TC, Bassani DG, Castel S. Use of mental health care services by Canadians with co-occurring substance dependence and mental disorders. Psychiatric Services. 2007;58(7):962–969. doi: 10.1176/ps.2007.58.7.962. [DOI] [PubMed] [Google Scholar]
- van Emmerik-van Oortmerssen, K., Van de Glind, G., Koeter, M. W., Allsop, S., Auriacombe, M., Barta, C., et al. (2014). Psychiatric comorbidity in treatment-seeking substance use disorder patients with and without attention deficit hyperactivity disorder: results of the IASP study. Addiction, 109(2), 262–272. 10.1111/add.12370. [DOI] [PMC free article] [PubMed]