Abstract
Objectives
The objectives of this study were to explore the perspectives of older adults about the most important domains of aging well and to identify the social determinants of a person-centered index capturing these domains.
Methods
We conducted a mixed-methods study of 40 semi-structured interviews and epidemiological data from 670 older adults participating in the International Mobility in Aging Study (IMIAS) in Saint-Hyacinthe and Kingston. A composite index capturing the domains of aging well was constructed on the basis of findings from qualitative content analysis. Bivariate and multivariate regressions were carried out to examine the determinants of aging well, including economic determinants, health behaviours, health services, and the social environment.
Results
The qualitative results confirm the importance of symptomatic health conditions and psychosocial components. The index was computed as a continuous score (0 to 100) containing health components (ADL disability, mobility disability, pain, self-rated health, and cognitive function), and psychosocial components (mood, productive activities, social relations, life satisfaction, and self-mastery). Mean scores were 81 among Canadian older adults, and 83 and 79 for men and women respectively. Being male, having sufficient income, doing leisure physical activity, and feeling safe in one’s neighbourhood were all significantly associated with a higher score on the aging well index.
Conclusion
The composite index highlights important aspects of health and psychosocial well-being that could be augmented according to older adults themselves. Modifiable social determinants of aging well could guide social and health policies to maximize well-being in this population.
Electronic supplementary material
The online version of this article (10.17269/s41997-018-0114-x) contains supplementary material, which is available to authorized users.
Keywords: Aging, Mixed methods, Social determinants of health
Résumé
Objectifs
Les objectifs de cette étude étaient d’explorer la perspective de personnes âgées à propos des plus importants domaines de ce que signifie bien vieillir, ainsi que d’identifier les déterminants sociaux d’un index de bien vieillir centré sur la personne incluant ces domaines.
Méthodes
Nous avons effectué une étude à méthodes mixtes utilisant 40 entretiens semi-dirigés et des données épidémiologiques provenant de 670 personnes âgées ayant participé à l’étude internationale sur la mobilité au cours du vieillissement (IMIAS) au Canada, à Saint-Hyacinthe et à Kingston. Un index comprenant les domaines mentionnés par les participants au devis qualitatif a été construit à partir de mesures existantes. Des régressions bivariée et multivariée ont ensuite été estimées afin d’examiner les déterminants sociaux de l’index de bien vieillir, notamment les déterminants économiques, les comportements de santé, l’accès aux services de santé, et l’environnement social.
Résultats
Les résultats du devis qualitatif confirment l’importance de conditions de santé symptomatiques et de composantes psychosociales. Un index continu (0 à 100) a été développé, comprenant des domaines de la santé (incapacité dans les activités de la vie quotidienne, incapacité de mobilité, douleur, santé perçue et fonction cognitive) et psychosociaux (humeur, activités productives, relations sociales, satisfaction dans la vie et maitrise de soi). Les scores moyens étaient de 81 pour l’ensemble des répondants canadiens, ainsi que de 83 et 79 pour les hommes et les femmes, respectivement. Être un homme, avoir un revenu suffisant, faire des activités physiques comme loisir et se sentir en sécurité dans son quartier étaient des déterminants associés de manière statistiquement significative à un score plus élevé sur l’index de bien vieillir.
Conclusion
L’index proposé dans cette étude met en lumière des aspects importants de la santé et des domaines psychosociaux qui pourraient être améliorés selon la perspective de personnes âgées canadiennes. Les déterminants sociaux modifiables qui ont été identifiés pourraient guider des politiques sociales et de santé afin de maximiser le bien-être de cette population.
Mots-clés: Vieillissement, Méthodes mixtes, Déterminants sociaux de la santé
Introduction
Positive models of aging, including active, healthy, or successful aging, are increasingly receiving attention and stand in contrast to medicalized concepts like frailty, sarcopenia and disability. The most widely used definition of successful aging is “a low probability of disease and disease-related disability, high cognitive and physical functional capacity, and active engagement with life” (Rowe and Kahn 1997). Meanwhile, European scholars tend to define active aging as “a low probability of illness and disability, high physical fitness, high cognitive functioning, positive mood and coping with stress, and being engaged with life” (Fernández-Ballesteros et al. 2013). The WHO further created a policy framework that identified participation, health, and security as the three pillars of active aging (World Health Organization 2002).
Despite enduring interest and promise, there remain important challenges in defining and measuring successful aging consistently for research, clinical practice, and policy purposes. The terminology used is inconsistent, with authors either comparing similar models but labeling them differently, or using the same label while positing different models. A comprehensive review of 28 studies revealed 29 different definitions of successful aging (Depp and Jeste 2006). A more recent systematic review of constructs of successful aging confirmed the heterogeneity present in 105 operational definitions retrieved and a tendency to emphasize physiological components (Cosco et al. 2013a).
The most used definition of successful aging further appears unachievable for the majority of older adults because it precludes having any chronic illness (Rowe and Kahn 1997). In their systematic review of studies done primarily in high income countries, Depp and Jeste concluded that only one third of older adults could be classified as aging successfully using a definition centered on the absence of disability (Depp and Jeste 2006). The authors of a study analyzing Canadian Community Health Survey data from 14,749 respondents aged 60 and over found that 17% were free of disease-related disability and that this percentage decreased steadily with advancing age, but that social engagement remained stable even as respondents became older (Weir et al. 2010). According to the United States Health and Retirement Study (HRS) involving approximately 1000 Americans, no more than 12% were free of major chronic conditions, physical disability, and cognitive impairment and were physically active and participating in social and productive activities (McLaughlin et al. 2010). This is by no means a problem specific to North America. A recent European study paints an equally bleak portrait using the above definition; a mean of 8.5% of older adults met criteria for successful aging (Hank 2011).
Current measures do not resonate with lay definitions and perceptions of what it means to age well, casting doubt on the relevance of research findings for health policies and practices. When asked, the perspective of older adults, themselves, is broader, less medical, and more positive than those of the aforementioned researchers, and not dependent upon absence of disability or chronic illness (Phelan et al. 2004). Montross and colleagues found, for example, that among 205 participants, self-rated successful aging scores were very high and linked with psychosocial components, such as independent living and positive adaptation to changes in health and lifestyle rather than with an absence of chronic illness and disability (Montross et al. 2006). Canadian authors focusing on men’s perspectives over time concur that we should broaden the biomedical notion of successful aging by integrating lay definitions (Tate et al. 2013). A systematic review comparing participants’ and researchers’ concepts of successful aging concluded that there is little overlap between the two, with qualitative studies emphasizing psychosocial aspects like attitude towards aging, while quantitative studies tend to focus on biomedical concepts (Cosco et al. 2014). Similarly, a meta-ethnography of qualitative research on the topic depicts the complexity of lay perspectives, highlighting no fewer than 12 interrelated psychosocial components ranging from independence to acceptance and adjustment (Cosco et al. 2013b).
There remains significant work to be done to incorporate older adults’ perspectives into population studies of aging well. The existence of many competing models also presents a significant obstacle to operationalizing research findings and developing health policies informed by empirical evidence. Moreover, there is, increasingly, a call for models of aging well that capture a range of outcomes rather than merely success or failure (Paul et al. 2015). To address these limitations and research gaps, the objective of this study is to develop a person-centered index of aging well in Canada by combining existing measures in line with older adults’ perceptions, and to examine the social determinants that are associated with this new concept of aging well. The research question guiding the qualitative portion of this investigation is: What does aging well mean to older adults in Canada? The results of the qualitative study guided the development of an index of aging well and the study of social determinants of aging well using epidemiological data in Canada. We aimed to develop an index that does not exclude older adults on the basis of having a chronic illness, that represents a range of outcomes instead of failure or success, and that incorporates additional psychosocial domains according to older adults’ perceptions.
The research objectives also draw on the development of person-centered medicine, which diverges from modern medicine’s reliance on defining well-being of the whole person by health of that person’s specific organ systems, rather than considering outcomes that may be more important to the persons being cared for (Mezzich et al. 2010). The movement aims at reorienting health care and policy, redefining patients as persons, abandoning an organ-centered vision that atomizes all, but particularly older adults into multiple pieces. The proponents of person-centered care consider that the subjective aspects of the person’s health situation are essential and not subordinate to the objective aspects of the disease.
Methods
This study adopts a mixed-methods research design, more specifically a convergent parallel design for data collection, and a sequential design for data analysis, whereby the results of the qualitative study guided the development of an index of aging well using existing individual measures (Creswell and Clark 2011).
Qualitative study design
A subset of 40 older adults was selected from the 2012 baseline sample of the International Mobility in Aging Study (IMIAS) at two Canadian sites (Saint-Hyacinthe and Kingston), using a stratified selection process to ensure a diversity of ages and education levels, and equal proportion by gender (Zunzunegui et al. 2015). The sample size was deemed the minimum necessary to be able to meaningfully examine participants’ perspectives across these groups across sites. Twenty semi-structured qualitative interviews were carried out at each site between November 2014 and April 2015 to explore participants’ perspectives on aging well. The interview guide is reported in the appendix. The methodology followed was that of a descriptive qualitative study, using inductive qualitative content analysis to explore the domains of aging well that older Canadian adults report (Sandelowski 2010; Hsieh and Shannon 2005). The interviews were transcribed verbatim, read closely, and then coded into specific domains by the first author. We developed recurrent themes that adequately covered the content of the interviews during the data analysis process, whereby by the last few interviews, there were no new themes emerging from our findings. Ethical approval for the study was obtained from the Institutional Review Board of the Research Centre of University of Montreal Hospital Centre (CRCHUM). IMIAS participants had consented to being contacted for future participation in research, such as this qualitative study following data collection in the original 2012 IMIAS study, and signed separate informed consent forms for the qualitative study.
Quantitative study design
An index capturing the domains reported by participants was created on the basis of the qualitative findings, i.e., representing the emerging themes deemed important by participants rather than an a priori model. The index was developed using data gathered in 2014 from all 670 Canadian participants in the IMIAS study, combining existing measures to better reflect lay conceptualizations of aging well in Canada. The IMIAS questionnaire was very comprehensive and contained a large number of measures of physical and psychosocial concepts to choose from to create an index that represents the domains of aging well deemed important by older adults. In previous research, low correlations were found between the domains of active aging, which precluded the use of latent measurement models (Belanger et al. 2017). Aging well is therefore better conceptualized as a composite index with relatively independent components, whereby a respondent could have mobility disability but have very satisfying social relations. The index was created as a continuous score from 0 to 100, building on the work of other scholars by following a weighting procedure similar to that developed by Cosco and colleagues (Cosco et al. 2015), but also including important additional psychosocial components according to the qualitative results obtained in the first part of this study. For each domain, we used established and clinically relevant cut-off values to differentiate between scores, or in the absence of such pre-existing cut-points, we differentiated between extreme scores (high, low), and others. The distribution of the index is represented with descriptive statistics and graphics, specifically a histogram with density estimate.
The health-related domains included an absence of disability in activities of daily living, an absence of mobility disability, an absence of pain, good self-rated health, and high cognitive function. The absence of disability in six activities of daily living (ADL) was assessed, namely walking across a room, dressing, bathing, eating, getting out of bed or of a chair, and going to the toilet. Previous research has shown that distinct groups emerge when examining the distribution of ADL disabilities, namely those with no disability in any activity, those with complete disability in one or more activities, and a middle group with the beginning of limitations in at least one activity (Béland 1995). A value of 100 was assigned to the first group, 0 to those with severe ADL disabilities, and 50 to those with minimal limitations. The same procedure was applied for mobility limitations, which comprises two items about the ability to walk 400 m and to climb a flight of stairs. As far as pain is concerned, respondents were asked if they were bothered by pain during the past month. Those who answered yes were asked where the pain was located out of 12 sites (back, hips, knees, legs, feet, hands, wrists, arms, shoulders, stomach, head, neck, or other location). We assigned a score of 100 for respondents reporting no pain, and following the work of Patel and colleagues (Patel et al. 2013), we deemed that the presence of pain at multiple sites (4 or more sites) was the worst possible outcome with a score of 0. Self-rated health was assessed with a standard question: “Would you rate your health as very good, good, fair, poor, or very poor?”. The answers were assigned progressively lower scores. We assessed cognitive function using the Leganes cognitive test, which has clinically significant cut-off points for dementia (total score of less than 22/32), mild cognitive impairment (more than 22/32 but less than 26/32) and normal cognitive function (26/32 and above) (de Yébenes et al. 2003).
The psychosocial domains retained were good mood, engagement in productive activities, good social relations, high life satisfaction, and high self-mastery. A standard scale was used for measuring depression, i.e., the Center for Epidemiological Studies Depression scale (CES-D). The scale contains 20 items about positive affect, negative affect, somatic complaints, and interpersonal relations, with a total maximum score of 60. A score above 20 was selected as the cut-off point indicating severe levels of depressive symptoms, and a score of 16 to 20 represents moderate depressive symptoms (Morin et al. 2011). Following many participants’ insistence about the importance of activities that make them feel useful, we integrated engagement in productive activities in the index. Any IMIAS respondent who worked (with or without remuneration), or often engaged in volunteering or caregiving, received a score of 100. Social relations were rated with one Likert-scale question about satisfaction with different types of social ties (friends, children, extended family, and spouse). Each respondent then obtained a total score, divided by the total number of social ties. We did not have standardized measures of life satisfaction in the IMIAS database, so we used two items from Wagnild’s resilience scale (Wagnild and Young 1993), namely “I feel proud that I have accomplished things in life”, and “My life has meaning”. Respondents needed a high rating on both items to be considered high on life satisfaction, and at least one low rating to be considered low. The seven items that constitute the Pearlin self-mastery scale were retained for the index (Pearlin and Schooler 1978). After reversing five negative items, respondents who agreed and agreed strongly on all seven items were considered to have high self-mastery (score of 100). The sum total of all the domains of aging well was finally divided by ten to obtain a total score on the index, with a maximum value of 100. The higher the score, the more someone ages well according to the domains included in the index.
We examined whether known determinants of positive aging were significantly associated with a higher score on the aging well index. We started from the WHO Active Aging Policy Framework, which identifies an exhaustive list of determinants that should be considered, namely behavioural, personal, physical, social, and economic determinants, as well as health and social services (World Health Organization 2002). Education was measured with the highest completed level of education among primary, secondary, and post-secondary. Income sufficiency was assessed as being insufficient, sufficient, or very sufficient. Home ownership was included as an additional measure of economic determinants. For health services, binary variables were added for having had access to a physician last time it was needed and having a regular physician. As part of health behaviours, alcohol consumption was measured with two variables, the first focusing on whether respondents drink alcohol regularly (more than 1–2 days a week), and the second whether or not there is binge drinking (more than 4 drinks per day). Tobacco was measured with a categorical variable that compared current smokers with past smokers and those who never smoked. Physical activity was measured as binary variables for walking at least 60 min per week and doing any leisure physical activity. Neighbourhood physical safety was assessed with this question: “Do you feel it is unsafe to walk around your neighbourhood?” and was reverse coded as a binary variable where respondents felt safe if they responded never or rarely feeling unsafe. Finally, victimization was measured by asking respondents three questions about whether they had been insulted or threatened, robbed, or attacked by a stranger in the past year. Any report of these incidents was coded as having been victimized. Bivariate and multivariate models were estimated for each of these determinants, and then for all of them together in a fully-adjusted model also controlling for age, gender, marital status, and site. For ease of interpretation, all variables were coded to try to predict higher scores on the aging well index.
Results
Qualitative study: aging well from the perspective of Canadian older adults
As can be seen in Table 1, the 40 IMIAS participants who were invited to take part in the qualitative study are comparable across the two study sites. The subsample is also similar to Canadian IMIAS participants, with few respondents reporting insufficient income, and a majority having some chronic illnesses (Zunzunegui et al. 2015). Table 2 contains excerpts representing each of the ten domains aligned with successful aging that were identified at the two research sites. An absence of disability in activities of daily living and an absence of disability in mobility were important domains mentioned at both sites. Descriptions of aging well included having independence, being able to do things for oneself and to go where one pleases. Participants recounted anecdotes about relatives who grew dependent on others and were unable to age well. More than the presence of chronic illnesses, pain was named by many as a deterrent to pursuing activities and doing things deemed to be important to aging well, with its impact varying with severity of the pain itself. Generally, being in good health was mentioned as the first aspect of aging well. The final domain of physical health that emerged from the qualitative content analysis was high cognitive function. Loss of memory or cognitive ability was clearly a concern for participants. Their perspective on aging well encompassed maintaining cognitive function until old age.
Table 1.
Sample characteristics of qualitative study participants in 2012
| Variables | Total | Kingston | Saint-Hyacinthe | |||
|---|---|---|---|---|---|---|
| n | % | n | % | n | % | |
| Age | ||||||
| 64–69 | 22 | 55 | 12 | 60 | 10 | 50 |
| 70–75 | 18 | 45 | 8 | 40 | 10 | 50 |
| Sex | ||||||
| Men | 20 | 50 | 10 | 50 | 10 | 50 |
| Women | 20 | 50 | 10 | 50 | 10 | 50 |
| Marital status | ||||||
| Single | 4 | 10 | 2 | 10 | 2 | 10 |
| Married | 22 | 55 | 11 | 55 | 11 | 55 |
| Widowed | 6 | 15 | 3 | 15 | 3 | 15 |
| Divorced | 8 | 20 | 4 | 20 | 4 | 20 |
| Education | ||||||
| Primary | 8 | 20 | 4 | 20 | 4 | 20 |
| Secondary | 11 | 27.5 | 5 | 25 | 6 | 30 |
| Post-secondary | 21 | 52.5 | 11 | 55 | 10 | 50 |
| Income sufficiency | ||||||
| Very sufficient | 16 | 40 | 10 | 50 | 6 | 30 |
| Barely sufficient | 22 | 55 | 9 | 45 | 13 | 65 |
| Insufficient | 2 | 5 | 1 | 5 | 1 | 5 |
| Chronic diseases* | ||||||
| No (0–1) | 12 | 30.8 | 5 | 26.3 | 7 | 35 |
| Yes (2+) | 27 | 69.2 | 14 | 73.7 | 13 | 65 |
*Chronic diseases: hypertension, diabetes, cancer, lung disease, heart disease, stroke, arthritis
Table 2.
Results of the qualitative content analysis
| Domains | Excerpts in Saint-Hyacinthe | Excerpts in Kingston |
|---|---|---|
| Absence of ADL disability | [Aging well] It’s keeping your physical autonomy, not being dependent on others. (SH064) | For me to age successfully and to have quality of life, that’s really important because my mother in law really suffered a lot in her last years since she was bedridden, she could not do anything, she was living with us, and looking back on it… “oh my god, what an existence!” (K120) |
| Absence of mobility disability | Aging well, it means to be able to… well I hope that it never happens, but we never know… being able to move around and to continue your activities. (SH388) | Oh I think the most important thing is I often say… you know, when you mention “rheumatoid arthritis”, people often say “oh gee that’s too bad, you poor thing” I say “hey, as long as I can walk, I am happy” that’s the way I feel, you know. […] As long as I am mobile, I am happy. (K409) |
| Good health | Aging well is not having health problems like I do at the moment. If I go out I always have to think about bringing what I need [to deal with urinary incontinence]. (SH284) | I have got lung problems, so I find that I have to stop and get my breath and that’s annoying. […] And I think my eye condition [macular degeneration] really limits me. (K038) |
| Absence of pain | When I try to lift something, my elbow hurts. That’s because I fell this summer and my elbow got the worst of it. Since then, as soon as I make any effort, the pain comes back. (SH006) | I have got a bad back and right now my shoulder is bothering me because I fell. I fell down the stairs outside a month ago now. […]It’s better today, but I had a hell of a day yesterday with it. Just pain all the time. (K143) |
| High cognitive function | That’s something about aging that scares me, to become dependent at some point… we often talk about Alzheimer and senility, about aging problems that lead to you becoming dependent. That scares me; it’s the part that concerns me the most. (SH201) | So you asked me the question of what it means to age well, it means to be able to do intellectual things, which have been part of my make up and continue to be that way, and so to have my faculties. (K115) |
| Good mood | [Aging well] is to be in good health, good mood, sharp mind, knowing to socialize with others, exchanging, sharing. And also taking time to relax and enjoy oneself, but also to be of service and having leisure time. (SH056) | I got really down this fall because I turned 70… in October. That was a downer because to me it’s, you know, the beginning of the end. I mean it sounds old. And at the same time three of my friends were diagnosed with cancer. […] Anyway… so I got really down with that. (K051) |
| Engagement in productive activities | The most important for me is still work, it’s still that. […] Yes, work still occupies a great place, very great place. (SH172) |
I: Would you say that’s the most important activity to you? P: Volunteering? Absolutely. That is my social outlet, my creative outlet, everything. (K183) |
| Good social relations | To be actively seeing people, meeting people, not always be enclosed in your house and talk to no one. […] I have good contact with my children as well, we talk regularly on the phone and they come see us, we go. Our network of family is… close. (SH127) | Being with family. Yeah, that’s the most important. […] We had five kids, fairly close together, pretty close together and they grew up together and done all kinds of things together, traveled and done this and done that and everything else. The family is the big thing. We just love being together. (K294) |
| High life satisfaction | At least in my life, we have been married for 49 years my husband and me, and there’s never been problems between us. I am not saying that we always agree on everything, no one does for their whole life. Overall, we are very happy. We have a beautiful life, compared to a lot of people, yes. (SH 127) | It’s kind of spooky to think of that, because this is really… a really nice existence, when I look at all the really neat things in my life, like the wife I was married to and the kid we had – we only had the one… her life, what we have here, all of this is paid for and my pensions are pretty good. (K120) |
| High self-mastery | If we were not able to travel at all, we’d be bored a little, but we expect it anyways. It would bother us quite a bit, but myself that’s how I am, once it’s over, it’s over. I do not ruminate, I accept the past. When I look back, I see the good sides, and I forget the bad ones. (SH321) | I hope I can still keep going, I am going to try anyway. Just do not let little things like aches and that sort of thing stop you. Just keep going as well as you can. (K006) |
Psychosocial domains also were perceived as essential for successful aging. Good mood was discussed by many participants, especially those who had experienced challenging periods of depression or who had a difficult time navigating life changes accompanying the aging process. Participants acknowledged that having a positive affect or disposition, or at least not being unhappy, was essential to aging well. The importance of engagement in productive activities was, perhaps surprisingly, present in many of the participants’ comments. Nearly all mentioned either working, volunteering, or taking care of others as most important to them. Participants identified a wide variety of productive activities not currently captured in formal surveys, such as tending gardens to grow food, sewing and knitting for family members, or actively managing investments portfolios. Having good social relations and maintaining regular social contact were important aspects as well. While the absence of some social ties did not seem to preoccupy participants unless they were recently bereaved, having good quality relations with at least one person or group was important. Enjoying one’s life (life satisfaction) was also mentioned regularly, referring to both contentment with the sum of one’s life achievements, and well-being and happiness with current level of activities and relationships. The final domain identified was self-mastery, that is, both a general positive attitude towards aging and one’s ability to adapt and continue on with meaningful activities despite aging.
In addition, participants’ narratives offer insight for the conceptualization of the domains of aging well as being distinct from their determinants. While income sufficiency was discussed at length in the data, it was presented as instrumental to pursuing other activities rather than as intrinsic to aging well. One participant mentioned the link between financial resources and stress: “Of course there’s the financial aspect. By that I mean having enough money to avoid the stress of that” (participant SH 177). Another identified income sufficiency as limiting the pursuit of activities, “I suppose finances is the only thing that really affects what we do. You know? You’d like to go to the theater more, you know… you start paying $85 a person, well, forget about it, you know, that kind of thing. So basically just finance” (participant K 366). Similarly, the safety of the physical environment where participants lived enabled them to go out and enjoy their favorite activities and was not a limiting issue (participant K 256). In closing, the themes identified in the data represent the domains of aging well that were most important from the perspective of participating Canadian older adults and that we then included in the development of a person-centered index of aging well.
Quantitative results: aging well distribution and associated social determinants
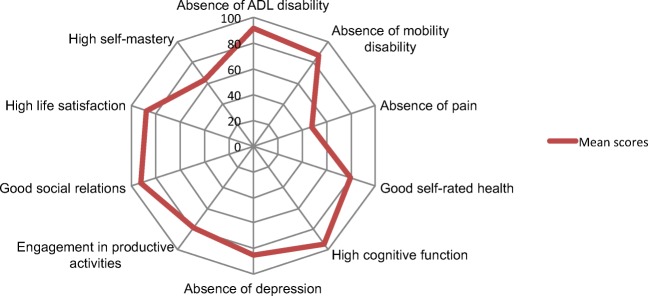
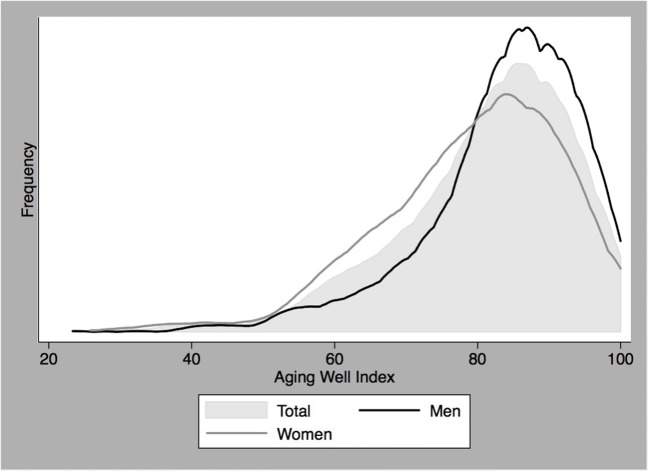
Table 3 lists the measures included in the original aging well index to represent participants’ perspectives, with the detailed cut-off points used to assign scores to different values, as well as the calculation of the total score. The mean score on the aging well index across domains was 81 (SD, 13) among Canadian older adults. As seen in Fig. 1, there is very little disability in activities of daily living in our sample, while 69.2% of the sample has 2 or more chronic conditions. As can be seen in Fig. 2, men had a statistically significant higher mean score on the index of aging well than women, with mean scores of 83 (SD, 12) and 79 (SD, 13) respectively. Figure 1 displays the mean scores for the specific domains of aging well. These scores indicate aspects of the health and psychosocial well-being that deserve improvement according to older adults themselves, particularly pain management and self-mastery in the case of the IMIAS Canadian sample.
Table 3.
Aging well items and index calculation
| Domain | Survey Questions IMIAS | Responses | Values | Calculation |
|---|---|---|---|---|
| (A) Absence of disability in activities of daily living |
Walking across room Dressing Bathing Eating Getting out of bed or chair Going to the toilet |
No difficulty in any ADL | 100 | A |
| A little difficulty in at least 1 ADL | 50 | |||
| A lot of difficulty in at least 1 ADL | 0 | |||
| (B) Absence of mobility disability (Nagi) |
Climbing a flight of stairs Walking 400 m |
No difficulty in any | 100 | B |
| A little difficulty in at least 1 | 50 | |||
| A lot of difficulty/unable in at least 1 | 0 | |||
| (C) Absence of pain |
Bothered by pain in last month Number of sites |
No pain | 100 | C |
| 1 to 3 sites | 50 | |||
| 4 and more sites | 0 | |||
| (D) Good self-rated health | Would you say that your health is ... | Very good | 100 | D |
| Good | 75 | |||
| Fair | 50 | |||
| Poor | 25 | |||
| Very poor | 0 | |||
| (E) High cognitive function | Leganes Cognitive Test (0–32) | No deficit > 26 | 100 | E |
| Mild impairment > 22 ≤ 26 | 50 | |||
| Dementia ≤ 22 | 0 | |||
| (F) Absence of depression | Center for Epidemiological Studies Depression (CES-D) (0–60) | No depression < 8 | 100 | F |
| Mild depressive symptoms 8–15 | 66 | |||
| Moderate depressive symptoms 16–20 | 33 | |||
| Severe depressive symptoms > 20 | 0 | |||
| (G) Engagement in productive activities | Work/volunteering or caregiving | Working/volunteering or caregiving often | 100 | G |
| Volunteering or caregiving once in a while | 50 | |||
| Not working/never or almost never | 0 | |||
| (H) Good social relations | Satisfactory relation with friends, partner, children, family | Very satisfied/satisfied | 100 | H = (total/number of ties) |
| Moderately satisfied | 50 | |||
| Not very/not at all satisfied | 0 | |||
| (I) High life satisfaction |
I feel proud that I have accomplished things in life. My life has meaning. |
Agree/strongly agree both | 100 | I |
| Others | 50 | |||
| Disagree in any of the two | 0 | |||
| (J) High self-mastery | Pearlin 7-item self-mastery scale | Agree/strongly agree on all | 100 | J |
| Others | 50 | |||
| Disagree on at least one | 0 | |||
| Overall score | Aging well index | A + B + C + D + E + F + G + H + I + J/10 | ||
Fig. 1.
Mean scores on aging well domains in Canada
Fig. 2.
Distribution of aging well in Canada
As reported in Table 4, there were significant positive bivariate associations between aging well scores and being younger, male, and married, having a post-secondary diploma, sufficient or very sufficient income, and owning one’s home. Health services were not significantly associated with better scores. Health behaviours, particularly not smoking and doing leisure physical activity, were related with higher scores. Finally, feeling safe in one’s neighbourhood was also positively related with aging well. In the fully adjusted model, male gender, income sufficiency, home ownership, leisure time physical activity, and neighbourhood safety all remained significantly associated with aging well. The large coefficients for income sufficiency are particularly notable, with those reporting sufficient and very sufficient incomes scoring 11.50 and 13.67 points higher than those with insufficient income, everything else held equal.
Table 4.
Social determinants of aging well index at Canadian IMIAS sites (n = 645)
| Variables | Bivariate regression | Multivariate regression | ||
|---|---|---|---|---|
| Coefficients | 95% CI | Coefficients | 95% CI | |
| Age | ||||
| 66–71 | 2.13* | .11, 4.15 | 1.01 | − .91, 2.93 |
| 72–77 | ref | ref | ||
| Gender | ||||
| Men | 4.30*** | 2.34, 6.25 | 2.27* | .24, 4.31 |
| Women | ref | ref | ||
| Marital status | ||||
| Single | ref | ref | ||
| Married | 4.96* | .45, 9.46 | 1.39 | − 3.19, 5.96 |
| Widowed | − .55 | − 5.73, 4.62 | − 1.13 | − 6.22, 3.96 |
| Divorced | − 3.032 | − 8.10, 2.04 | − 1.08 | − 6.04, 3.88 |
| Education | ||||
| Primary | ref | ref | ||
| Secondary | 3.34 | − 2.25, 8.93 | − 1.33 | − 6.92, 4.25 |
| Post-secondary | 6.52* | 1.25, 11.78 | − 1.06 | − 6.60, 4.47 |
| Income sufficiency | ||||
| Insufficient | ref | ref | ||
| Sufficient | 15.27*** | 10.86, 19.67 | 11.50*** | 6.87, 16.12 |
| Very sufficient | 18.86*** | 14.57, 23.15 | 13.67*** | 9.05, 18.30 |
| House ownership | ||||
| Not an owner | ref | ref | ||
| Owner | 7.16*** | 4.96, 9.37 | 2.61* | .15, 5.07 |
| Study site | ||||
| Kingston | ref | ref | ||
| St-Hyacinthe | − .33 | − 2.31, 1.65 | 1.57 | − .51, 3.65 |
| Access to healthcare | ||||
| No | ref | ref | ||
| Yes | 3.12 | − 2.93, 9.18 | .87 | − 4.82, 6.57 |
| Regular MD | ||||
| No | ref | ref | ||
| Yes | .62 | − 5.61, 6.86 | .72 | − 5.11, 6.56 |
| Alcohol > 1–2 days/week | ||||
| No | ref | ref | ||
| Yes | − 3.51 | − 5.51, − 1.51 | − .72 | − 2.72, 1.28 |
| Binge > 4 drinks per day | ||||
| No | ref | ref | ||
| Yes | 2.89 | − 3.96, 9.74 | − .32 | − 7.18, 6.53 |
| Walking 60 min/week | ||||
| No | ref | ref | ||
| Yes | 1.87 | − .87, 4.60 | 1.17 | − 1.44, 3.78 |
| Leisure physical activity | ||||
| No | ref | ref | ||
| Yes | 5.28*** | 3.20, 7.37 | 3.57** | 1.51, 5.62 |
| Smoking | ||||
| Current | ref | ref | ||
| Former | − 2.51* | − 4.55, − .46 | − 1.07 | − 5.00, 2.86 |
| Never | − 5.85** | − 10.02, − 1.67 | 1.45 | − 2.59, 5.50 |
| Safe neighbourhood | ||||
| No | ref | ref | ||
| Yes | 7.33*** | 4.18, 10.49 | 3.47* | .31, 6.63 |
| Victimization history | ||||
| Yes | ref | ref | ||
| No | 3.83 | − .25, 7.91 | 1.81 | − 2.02, 5.65 |
* p < 0.05, ** p < 0.01, *** p < 0.001
Discussion
The aim of this paper was to develop a person-centered index of aging well in Canada by combining existing measures into an original composite index that better captures lay perspectives, and to examine its social determinants. Our findings are in line with previous work on lay perspectives which concluded that positive aging is multidimensional and is composed of health, social and psychological domains (Bowling 2007). The main contributions of lay perspectives in this analysis were an emphasis on symptomatic conditions like pain, the inclusion of additional psychosocial domains like self-mastery, and the differentiation between domains and determinants, all of which guided the development of the index in the quantitative research design. The index developed encompasses standard health components from previous definitions of successful or active aging (Rowe and Kahn 1997; Fernández-Ballesteros et al. 2013), while excluding chronic conditions and adding symptomatic and psychosocial dimensions that matter from the perspective of older adults. While our sample of participants had a large number of chronic conditions, they were largely asymptomatic and reported good self-rated health and functional status. The inclusion of symptomatic conditions such as pain and functional disabilities rather than only the presence of chronic diseases reflects the perspectives of participants regarding conditions that interfered with their quality of life. In addition, their narratives support the inclusion of financial resources and safe environments as determinants rather than intrinsic domains of aging well.
To develop the index, we built on previous work contributing to the creation of continuous scores by Cosco and colleagues (Cosco et al. 2015), which included engagement, personal resources, cognitive function, activities of daily living, and instrumental activities of daily living. Our qualitative findings confirm the relevance of this previous work but also show the importance of dimensions that were not captured before, including mood, pain, social support, and self-mastery. By exploring Canadian older adults’ perceptions, we offer a more complete, person-centered, and nuanced index than versions that focus either on functional abilities or medical and biomedical conditions (Cosco et al. 2015; Rowe and Kahn 2015). Unlike a recent meta-ethnography that found as many as 12 psychosocial domains (Cosco et al. 2013b), we regrouped participants’ perspectives into 10 main health and psychosocial domains overall. We strived to achieve balance between an exhaustive index capturing lay perspectives, and the development of a concise composite index relying on standardized measures. As far as the weighting of the scores and calculation of the index is concerned, unless there were clinically significant cut-off points demonstrated in previous research, we followed general principles distinguishing between groups that have good outcomes, poor outcomes, and other respondents. While the qualitative portion highlights important domains to be considered as part of the index, comparison between studies is enhanced when standardized measures of these domains are adopted, bearing in mind the potential measurement equivalence between different measurement tools and respecting the integrity of previously validated scales. The index proposed also yields a concept of aging well that does not involve a cut-off point to label older adults as successful or not. We share the opinion of other researchers in the field that a binary outcome does not capture the nuances of individual trajectories when it comes to positive aging (Paul et al. 2015).
It is difficult to compare determinants of positive aging across different studies because authors include different domains as part of the concept itself and as determinants. Nevertheless, demographic (age and gender), socio-economic (education, occupation, and income), behavioural (smoking habit, alcohol consumption, and exercise), and environmental (security and accessibility) factors constitute recognized determinants of various concepts of positive aging (Depp and Jeste 2006; World Health Organization 2002). The validation of composite models is challenging because they do not lend themselves to factor analysis. The fact that the composite measure of aging well proposed was significantly associated with determinants proposed by the WHO lends credibility to the index. In this context, respondents who had financial security were overall much more likely to score highly on the aging well index, which means that they were more likely to have good physical and mental health, high physical and cognitive function, to be free of pain, as well as to be productive, socially engaged, and to have a positive attitude about their ability to age well.
From a clinical viewpoint and as stated by Friedman et al., shifting the focus of attention from health-related conditions to those of a positive aging may aid clinicians in prioritizing interventions aimed at the promotion of aging well (Friedman et al. 2015). Health care providers in charge of taking care of older adults have well-established guidelines for chronic diseases; however, when it comes to treating the older adult as a whole, there is no clear guidance. This aging well index can help frame a systematic approach to the older adult as a person rather than to a particular disease or collection of chronic diseases that are often already being managed (Cesari et al. 2016). Moreover, aging well can be viewed on a spectrum of health with frailty at the other extreme, a state where the individual is already vulnerable to a number of low-impact stressors, and requires medical intervention. The aging well concept is therefore useful for prevention among the majority of older adults who are not frail. The index finally represents a valuable global, person-centered outcome that could be examined over time, as health and social policies shape the living conditions of older adults.
This work has many strengths, including a mixed-methods design drawn from the same population of older adults at two Canadian sites. There were limitations, however, given the convergent data collection process, i.e., survey questions could not be modified to accommodate for findings of the qualitative data analysis. The pain indicator available in the survey data did not include a measure of severity. Future work could perfect these specific measures and the weighing of the index for these domains. In addition, the qualitative data showed the variety of productive activities that could be considered and that have to date not been captured in larger surveys. There was also limited variation in access to health services because IMIAS respondents were recruited from patient lists at primary care practices. Finally, the study samples were relatively young older adults (65–74 years old), and come from two smaller cities (Kingston, Saint-Hyacinthe), neither of which have large immigrant populations in the age group of interest. Given a much more diverse population in larger urban centres and in the coming cohorts of Canadian older adults, increasing the cultural and ethnic diversity of research on this topic is an important direction for future research. Conducting further research with seniors age 75 and over would further inform the weighing of the different domains to better represent the perceptions of older adults who are potentially living with disability when it comes to aging well.
In conclusion, the new index that was developed highlights important aspects of health and psychosocial well-being according to older adults, which are often overlooked as part of researcher-driven research on positive aging. Moreover, the results also highlight modifiable social determinants that could guide social and health policy action to maximize the opportunities for aging well in this population. Since human aging is a global phenomenon, future research should examine person-centered constructs of aging well across different populations in the world and assess the uniqueness and universal validity of different domains and concepts. The use of procedures to explore the psychometric properties of the index would also be recommended, as would analyses that can identify different profiles of aging well in the population according to the domains suggested.
Electronic supplementary material
(DOCX 112 kb)
Acknowledgements
The authors would like to thank the research participants. The first author received a postdoctoral fellowship from the Quebec Research Fund- Health (FRQ-S) to conduct this work. The qualitative study expenses were supported by a new initiative grant from the Public Health Research Institute of University of Montreal (IRSPUM). The IMIAS study was supported by an emerging team grant from the Canadian Institutes of Health Research (AAM-108751).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Emmanuelle Bélanger, Phone: (401) 863-9924, Email: emmanuelle_belanger@brown.edu.
Mario Ulises Pérez-Zepeda, Email: ulises.perez@salud.gob.mx.
Roberto Carlos Castrejón-Pérez, Email: rc.castrejon.perez@gmail.com.
Tamer Ahmed, Email: tia@queensu.ca.
Grégory Moullec, Email: gregory.moullec@umontreal.ca.
Susan P. Phillips, Email: phillip@queensu.ca
Maria Victoria Zunzunegui, Email: maria.victoria.zunzunegui@umontreal.ca.
References
- Béland F. El perfil de las incapacidades funcionales en las personas mayores. Revista multidisciplinar de gerontología. 1995;5(4):232–244. [Google Scholar]
- Belanger E, Ahmed T, Filiatrault J, Yu H-T, Zunzunegui MV. An empirical comparison of different models of active aging in Canada: The International Mobility in Aging Study. Gerontologist. 2017;57(2):197–205. doi: 10.1093/geront/gnv126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bowling A. Aspirations for older age in the 21ST century: what is successful aging? International Journal of Aging & Human Development. 2007;64(3):263–297. doi: 10.2190/L0K1-87W4-9R01-7127. [DOI] [PubMed] [Google Scholar]
- Cesari M, Marzetti E, Thiem U, Pérez-Zepeda MU, Abellan Van Kan G, Landi F, et al. The geriatric management of frailty as paradigm of “the end of the disease era”. European Journal of Internal Medicine. 2016;31:11–14. doi: 10.1016/j.ejim.2016.03.005. [DOI] [PubMed] [Google Scholar]
- Cosco TD, Prina AM, Perales J, Stephan BCM, Brayne C. Operational definitions of successful aging: a systematic review. International Psychogeriatrics. 2013;26(03):373–381. doi: 10.1017/S1041610213002287. [DOI] [PubMed] [Google Scholar]
- Cosco TD, Prina AM, Perales J, Stephan BCM, Brayne C. Lay perspectives of successful ageing: a systematic review and meta-ethnography. BMJ Open. 2013;3(6):e002710. doi: 10.1136/bmjopen-2013-002710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cosco TD, Matthew Prina A, Perales J, Stephan B, Brayne C. Whose“ successful ageing?”: Lay-and researcher-driven conceptualisations of ageing well. Eur J Psychiatry. 2014;28(2):124–130. doi: 10.4321/S0213-61632014000200006. [DOI] [Google Scholar]
- Cosco TD, Stephan BCM, Brayne C. Validation of an a priori, index model of successful aging in a population-based cohort study: the successful aging index. Int Psychogeriatr. 2015;27(12):1971–1977. doi: 10.1017/S1041610215000708. [DOI] [PubMed] [Google Scholar]
- Creswell JW, Clark VLP. Designing and conducting mixed methods research. Thousand Oaks, CA: Sage Publications Ltd.; 2011. [Google Scholar]
- Depp CA, Jeste DV. Definitions and predictors of successful aging: a comprehensive review of larger quantitative studies. The American Journal of Geriatric Psychiatry. 2006;14(1):6–20. doi: 10.1097/01.JGP.0000192501.03069.bc. [DOI] [PubMed] [Google Scholar]
- Fernández-Ballesteros, R., Robine, J.M., Walker, A., Kalache, A. (2013). Active aging: a global goal. Curr Gerontol Geriatr Res 2013, 298012. [DOI] [PMC free article] [PubMed]
- Friedman SM, Shah K, Hall WJ. Failing to focus on healthy aging: a frailty of our discipline? Journal of the American Geriatrics Society. 2015;63(7):1459–1462. doi: 10.1111/jgs.13512. [DOI] [PubMed] [Google Scholar]
- Hank K. How “successful” do older Europeans age? Findings from SHARE. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences. 2011;66(2):230–236. doi: 10.1093/geronb/gbq089. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hsieh H-F, Shannon SE. Three approaches to qualitative content analysis. Qualitative Health Research. 2005;15(9):1277–1288. doi: 10.1177/1049732305276687. [DOI] [PubMed] [Google Scholar]
- McLaughlin SJ, Connell CM, Heeringa SG, Li LW, Roberts JS. Successful aging in the United States: prevalence estimates from a national sample of older adults. The Journals of Gerontology Series B Psychological. 2010;65B(2):216–226. doi: 10.1093/geronb/gbp101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mezzich J, Snaedal J, van Weel C, Heath I. Toward person-centered medicine: from disease to patient to person. The Mount Sinai Journal of Medicine. 2010;77(3):304–306. doi: 10.1002/msj.20187. [DOI] [PubMed] [Google Scholar]
- Montross LP, Depp C, Daly J, Reichstadt J, Golshan S, Moore D, et al. Correlates of self-rated successful aging among community-dwelling older adults. The American Journal of Geriatric Psychiatry. 2006;14(1):43–51. doi: 10.1097/01.JGP.0000192489.43179.31. [DOI] [PubMed] [Google Scholar]
- Morin AJS, Moullec G, Maïano C, Layet L, Just JL, Ninot G. Psychometric properties of the Center for Epidemiologic Studies Depression Scale (CES-D) in French clinical and nonclinical adults. Revue d'Épidémiologie et de Santé Publique. 2011;59(5):327–340. doi: 10.1016/j.respe.2011.03.061. [DOI] [PubMed] [Google Scholar]
- Patel KV, Guralnik JM, Dansie EJ, Turk DC. Prevalence and impact of pain among older adults in the United States: findings from the 2011 National Health and Aging Trends Study. Pain. 2013;154(12):2649–2657. doi: 10.1016/j.pain.2013.07.029. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Paul C, Teixeira L, Ribeiro O. Positive aging beyond “success”: towards a more inclusive perspective of high level functioning in old age. Educational Gerontology. 2015;41(12):930–941. doi: 10.1080/03601277.2015.1071590. [DOI] [Google Scholar]
- Pearlin LI, Schooler C. The structure of coping. Journal of Health and Social Behavior. 1978;19(1):2–21. doi: 10.2307/2136319. [DOI] [PubMed] [Google Scholar]
- Phelan EA, Anderson LA, LaCroix AZ, Larson EB. Older adults“ views of ‘successful aging’—how do they compare with researchers” definitions? Journal of the American Geriatrics Society. 2004;52(2):211–216. doi: 10.1111/j.1532-5415.2004.52056.x. [DOI] [PubMed] [Google Scholar]
- Rowe JW, Kahn RL. Successful aging. Gerontologist. 1997;37(4):433–440. doi: 10.1093/geront/37.4.433. [DOI] [PubMed] [Google Scholar]
- Rowe JW, Kahn RL. Successful aging 2.0: conceptual expansions for the 21st century. The Journals of Gerontology Series B. 2015;70(4):593–596. doi: 10.1093/geronb/gbv025. [DOI] [PubMed] [Google Scholar]
- Sandelowski M. What’s in a name? Qualitative description revisited. Research in Nursing & Health. 2010;33(1):77–84. doi: 10.1002/nur.20362. [DOI] [PubMed] [Google Scholar]
- Tate RB, Swift AU, Bayomi DJ. Older men's lay definitions of successful aging over time: the Manitoba follow-up study. International Journal of Aging & Human Development. 2013;76(4):297–322. doi: 10.2190/AG.76.4.b. [DOI] [PubMed] [Google Scholar]
- Wagnild GM, Young HM. Development and psychometric evaluation of the resilience scale. Journal of Nursing Measurement. 1993;1(2):165–178. [PubMed] [Google Scholar]
- Weir PL, Meisner BA, Baker J. Successful aging across the years: does one model fit everyone? Journal of Health Psychology. 2010;15(5):680–687. doi: 10.1177/1359105309353648. [DOI] [PubMed] [Google Scholar]
- World Health Organization. Active ageing: a policy framework. 2002. Available at: http://whqlibdoc.who.int/hq/2002/who_nmh_nph_02.8.pdf. Accessed May 2017. [PubMed]
- de Yébenes MG, Otero A, Zunzunegui MV. Validation of a screening test for cognitive function in elderly populations with a low level of education. International Journal of Geriatric Psychiatry. 2003;18:925–936. doi: 10.1002/gps.947. [DOI] [PubMed] [Google Scholar]
- Zunzunegui MV, Alvarado BE, Guerra R, Gómez JF, Ylli A, Guralnik JM, et al. The mobility gap between older men and women: the embodiment of gender. Archives of Gerontology and Geriatrics. 2015;61(2):140–148. doi: 10.1016/j.archger.2015.06.005. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 112 kb)