Abstract
Objectives
This study aimed to assess functional health literacy levels among older adults living in subsidized housing in Hamilton, Ontario, and to assess the relationships between health literacy and other important health indicators, such as education level, age, ethnicity, body mass index (BMI), and self-reported health status.
Methods
Older adults (n = 237) living in subsidized housing buildings in Hamilton, ON, were assessed using the NVS-UK as a measure of functional health literacy in addition to a health indicator questionnaire through structured interview. Health literacy levels were analyzed using descriptive statistics and logistic regression to determine relationships between health literacy levels and other health indicators.
Results
Participants’ mean age was 73 years, 67% were female, 70% were not educated beyond high school, and 91% were white. Over 82% of participants had below adequate health literacy levels using the NVS-UK. Multivariable logistic regression revealed significant relationships between functional health literacy and BMI, education level, and pain and discomfort levels. No significant relationships were found between health literacy level and age group, anxiety and depression levels, CANRISK (Diabetes risk) score, gender, marital status, mobility issues, self-care issues, self-reported health status, or performance of usual activities.
Conclusions
As the population of older adults continues to grow, the appropriate resources must be available to both improve and support the health literacy level of the population. Future health research should gather information on the health literacy levels of target populations to ensure more equitable health service. This research provides a significant opportunity to better understand populations with health literacy barriers.
Keywords: Health literacy, Aged, Housing for the elderly, Seniors, Social housing, Socioeconomic status
Résumé
Objectifs
Évaluer les niveaux de littératie fonctionnelle en matière de santé chez des adultes âgés vivant dans des logements subventionnés à Hamilton, en Ontario, ainsi que les relations entre la littératie en santé et d’autres indicateurs de santé importants, comme le niveau d’instruction, l’âge, l’ethnicité, l’indice de masse corporelle (IMC) et l’état de santé autodéclaré.
Méthode
Des adultes âgés (n = 237) vivant dans des immeubles à logements subventionnés à Hamilton (Ontario) ont été évalués à l’aide de l’outil NVS-UK (Newest Vital Sign UK) pour mesurer leur littératie fonctionnelle en matière de santé et ont rempli un questionnaire d’indicateurs de santé lors d’entretiens dirigées. Leurs niveaux de littératie en santé ont été analysés par statistique descriptive et par régression logistique pour déterminer les relations entre les niveaux de littératie en santé et les autres indicateurs de santé.
Résultats
Les participants avaient 73 ans en moyenne, 67% étaient des femmes, 70% n’avaient qu’un diplôme d’études secondaires, et 91% étaient de race blanche. Plus de 82% avaient des niveaux de littératie en santé insuffisants selon le NVS-UK. L’analyse de régression logistique multivariée a mis au jour des relations significatives entre la littératie fonctionnelle en matière de santé et l’IMC, le niveau d’instruction et les niveaux de douleur et d’inconfort. Aucune relation significative n’a été observée entre les niveaux de littératie en santé et le groupe d’âge, les niveaux d’anxiété et de dépression, la note au questionnaire CANRISK (sur le risque de diabète), le sexe, l’état matrimonial, les problèmes de mobilité, les problèmes d’autosoins, l’état de santé autodéclaré ou l’accomplissement des tâches de la vie quotidienne.
Conclusions
Avec la croissance continue de la population adulte âgée, il faudra trouver des ressources appropriées pour améliorer et maintenir les niveaux de littératie en santé de la population. Les futures études de recherche en santé devraient recueillir des données sur les niveaux de littératie en santé de populations cibles pour améliorer l’équité de l’offre de services de santé. Notre étude offre une importante possibilité de mieux comprendre les populations confrontées à des obstacles sur le plan de la littératie en santé.
Mots-clés: Compétence informationnelle en santé, Sujet âgé, Résidences pour personnes âgées, Aînés, Logement social, Statut socioéconomique
Introduction
In Canada, health literacy is defined as, “the ability to access, comprehend, evaluate and communicate information as a way to promote, maintain, and improve health in a variety of settings across the life-course” (Canadian Council on Learning 2007a). According to the Canadian Council on Learning, health literacy is an integral component of the overall health of Canadians and approximately 60% of Canadian adults lack health literacy (Canadian Council on Learning 2007a). Among those above age 65, this figure increases to 88% (Canadian Council on Learning 2007b). Canadian older adults with limited health literacy in these abundant numbers can have devastating consequences for the health care system. Lower health literacy levels are related to negative health outcomes, such as inadequate diabetes control and substandard physical and mental health outcomes (Gazmararian et al. 2003; Kim et al. 2004; Rootman and Gordon-El-Bihbety 2008; Schillinger et al. 2003). Lower health literacy has also been associated with lower health-related quality of life in the general population of older adults (Wolf et al. 2005). Low health literacy can lead to increased health care system costs (Rootman and Gordon-El-Bihbety 2008). Since the prevalence of chronic disease increases with age (Statistics Canada 2006), the implications of Canadian older adults being health illiterate are serious. It suggests that the population faced with the majority of health issues may well have a reduced capacity to cope with them (Canadian Public Health Association 1998).
The impact of limited health literacy on individuals of lower socioeconomic status (SES) is even greater (Baur 2010). Older adults living in subsidized housing buildings generally have a lower SES, increased mortality rates, and a lower health-related quality of life (Bassuk et al. 2002; Huguet et al. 2008). This population of older adults are also high users of Emergency Medical Services (EMS), accounting for over a third of all EMS calls (Platts-Mills et al. 2010). Older adults with poor health literacy call EMS more frequently and are at higher risk for hospitalization (Berkman et al. 2011). Specifically, addressing the health literacy of older adults living in subsidized housing buildings could help reduce health inequities and improve health care utilization in this group (Murray et al. 2008). It is of note that the eligible age to reside in subsidized seniors’ housing ranges by municipality (e.g., 55 years in Niagara Region (Niagara Regional Housing 2003) and 59 years in the Greater Toronto Area (City of Toronto 2015)). In Hamilton, Ontario, where the current study was conducted, one resident must be 65 years or older, but their spouse may be younger (City of Hamilton n.d.). Accordingly, the Social Planning and Research Council of Hamilton purposefully included older adults, aged 55 years and older, in their report on vulnerable seniors in Hamilton (Social Planning and Research Council of Hamilton 2011) and housing authorities generally consider older adults in subsidized housing to be a population aged 55 years and over. However, beyond the resident’s age category and gender, very little demographic (e.g., education) or health-related information (e.g., quality of life, health literacy) is available for this specific hard-to-reach population.
The specific issues generated by Canadian older adults is one that our healthcare system has to face. The number of older adults Canada is anticipated to grow substantially in the next 20 years from 14.6% in 2012 to 24% in 2036 (Ontario Ministry of Finance 2016). In order to plan for the health care needs of this group, health literacy levels in this growing population must be evaluated since, to date, they have not been directly assessed. A three-level model of health literacy has been proposed: (1) basic/functional literacy, including skills for reading and writing that enable effective functioning related to health in everyday situations; (2) communicative/interactive literacy, including more advanced skills that enable active participation in activities that require extracting and understanding information from different sources, and applying new information to changing circumstances; and (3) critical literacy, including more advanced skills for critically analyzing information and using this information to exert greater control over life events and situations (Nutbeam 2000). Functional literacy, though the most limited level, tends to be that which is used in health-related settings involving information transfer. Deficits in functional literacy will result in patients who cannot understand and assimilate information from handouts about their chronic diseases (Mitchell and Begoray 2010). When functional literacy is inadequate, it is not possible to educate patients regarding their chronic health conditions (Williams et al. 1998). Communicative literacy involves the understanding of information and acting on that information, and critical literacy involves understanding how the information may be translated to other situations. Both of these are also the next steps to the interpretation of health information and therefore desirable in the subsidized housing population. Health promotion materials often assume a basic level of functional literacy, together with at least communicative literacy. Therefore, if health issues are to be addressed in the hard-to-reach and chronically ill population of older adults residing in subsidized housing, it is prudent to at least assess this population’s functional literacy, communicative literacy and possibly critical literacy as well.
Objectives
The objectives of this study were to (1) assess functional health literacy levels among older adults living in subsidized housing in Hamilton, Ontario, and (2) assess the relationship between functional health literacy and health indicators (such as body mass index (BMI) and self-reported health status), controlling for social determinants of health (e.g., education level, age, ethnicity).
Methods
Study setting and participants
Five subsidized seniors’ housing buildings in Hamilton, Ontario, were identified by the research team in collaboration with the Hamilton Paramedic Service and City Housing Hamilton. City Housing Hamilton provides rental units in these buildings at rates that are geared-to-income (typically 30% of total income), subsidized by government, to alleviate the burden of housing costs in low-income populations. Some buildings are designated specifically for older adults, requiring that all residents are 55 years and older and at least one resident of the unit is 65 years of age or older. Accordingly, the study population was defined as individuals aged 55 years or older, residing in City Housing Hamilton subsidized seniors’ buildings. The specific buildings selected were based on EMS call rates (number of calls/100 apartment units) in the 2 years prior to the survey period.
All residents 55 years and older in the selected buildings were included as potential participants. Individuals who were residents in the building for less than 3 months were excluded. Participants were surveyed one-on-one by trained research staff and students through a structured, researcher-administered questionnaire in a common area in the building (e.g., wellness room). Convenience sampling was used to recruit participants as recruitment posters were posted in common areas of the building. Participants were given a $10.00 gift card upon survey completion. All surveys were conducted in English and participation was voluntary. Written consent was obtained from participants before beginning the survey. To ensure informed consent in this low literacy population, the consent form was written using Grade 6 lay language and the research staff reviewed the consent form with each participant. Individuals who were unable to consent were unable to participate in the survey. This research study was approved by the Hamilton Integrated Research Ethics Board (HiREB) (no. 14-210 and no. 14-645).
Measures
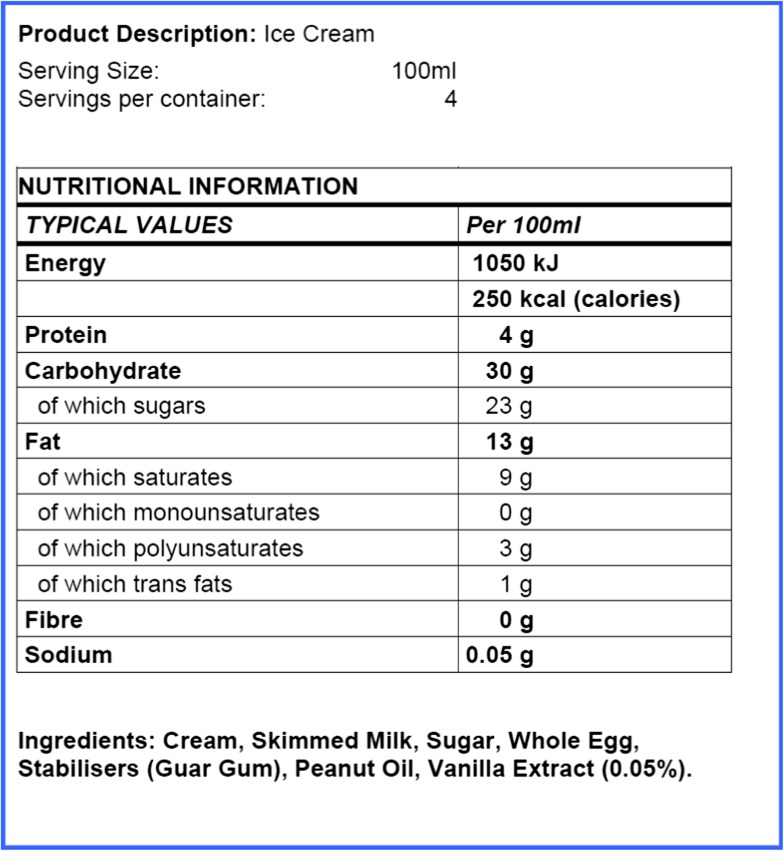
Functional health literacy was assessed using the Newest Vital Sign UK-validated version (NVS-UK) (Rowlands et al. 2013). The NVS-UK is a recognized and validated tool to assess health literacy (Rowlands et al. 2013) and is among the top three most widely used measures of health literacy (Shum et al. 2016). It is a validated predictor of health literacy that measures both literacy and numeracy skills (Rowlands et al. 2013). It is important to note that no single tool will assess all aspects of health literacy, but the NVS-UK does attempt to assess aspects of the “cognitive and social skills needed by individuals as they access, understand, and use information in ways that promote and maintain good health” but will not assign a specific reading or numeracy level (Rowlands et al. 2013). The NVS-UK consists of a Food Nutrition Label Showcard, a simplified food label similar to Canadian labels, with six associated questions (Appendix 1) (Weiss et al. 2005). NVS-UK scores can range from 0 to 6. Sensitivity and specificity of the NVS-UK instrument were analyzed using a receiver operating characteristic (ROC) curve (Rowlands et al. 2013). A score of 4–6 was predictive of adequate health literacy and a score of 0–3 of inadequate health literacy.
In addition to the health literacy assessment, all participants were asked a set of questions on demographics and other health-related items. The Health Awareness and Behaviour Tool (HABiT) is a reliable, multi-dimensional questionnaire developed for use with older adults in Canada (Agarwal and Angeles 2017). The HABiT questionnaire assesses multiple health-related topics, such as cardiovascular disease and diabetes knowledge, lifestyle risk factors, and quality of life. Questions included in the HABiT were obtained from validated sources, such as the Canadian Hypertension Education Program (CHEP), the Canadian Community Health Survey (CCHS), and the Canadian Diabetes Risk Questionnaire (CANRISK) (Hypertension Canada 2015; Statistics Canada 2016; Robinson et al. 2011).
Analysis
Data were analyzed using IBM SPSS Statistics version 17.0. Descriptive statistics were used to analyze survey respondents’ sociodemographics and health literacy scores. After examining correlations between variables, logistic regression was conducted to determine the relationships between health literacy (adequate versus below adequate), health indicators, and other social determinants of health (Table 2). The significance level was set at a p value < 0.05. The goodness of fit for the logistic regression model was determined using the Hosmer and Lemeshow test (Hosmer Jr et al. 2013).
Table 2.
Logistic regression model for health literacy
| Variable | Odds ratio | 95% confidence interval | Significance | ||
|---|---|---|---|---|---|
| Upper | Lower | ||||
| Age | ≤ 64 | REF | .619 | ||
| 65–84 | .774 | .251 | 2.382 | .655 | |
| ≥ 85 | 1.760 | .254 | 12.212 | .567 | |
| Gender | Male | REF | |||
| Female | 1.267 | .406 | 3.953 | .683 | |
| Marital status | Married/common-law | REF | |||
| Single, divorced, separated, widowed | 1.102 | .195 | 6.217 | .912 | |
| Education level | College/university | REF | |||
| High school or less | .224 | .084 | .595 | .003 | |
| BMI | Underweight | 17.222 | 1.608 | 184.418 | .019 |
| Normal | REF | ||||
| Overweight/obese | 7.966 | 1.341 | 47.308 | .022 | |
| CANRISK score | Low/moderate risk | REF | |||
| High risk | 1.522 | .408 | 5.684 | .532 | |
| Self-reported health status | Good/very good/excellent | REF | |||
| Fair/poor | 1.764 | .611 | 5.090 | .294 | |
| Mobility issues | Absent | REF | |||
| Present | 1.354 | .386 | 4.745 | .636 | |
| Pain/discomfort | Absent | REF | |||
| Present | 4.300 | 1.053 | 17.552 | .042 | |
| Self-care issues | Absent | REF | |||
| Present | .336 | .081 | 1.390 | .132 | |
| Anxiety/depression | Absent | REF | |||
| Present | 1.921 | .730 | 5.054 | .186 | |
| Issues performing usual activities | Absent | REF | |||
| Present | .333 | .106 | 1.047 | .060 | |
| Constant | .016 | .006 | |||
| Hosmer and Lemeshow goodness of fit |
Chi-square = 6.615 Df = 8 Significance = .579 |
||||
*p values in italics are statistically significant at a 0.05 level
Results
Study population
A total of 237 participants (158 women, 79 men), aged 55 to 93 years (mean age = 71.31 years; standard deviation (SD) = 8.78), were assessed for health literacy (see Table 1 for respondent demographics). All participants resided in one of the five surveyed subsidized housing buildings in Hamilton, Ontario. The majority of participants were white (90.5%), educated to high school level or less (70.4%), and widowed, separated, divorced, or single (92.0%). This population also reported issues with pain or discomfort (75.2%), mobility (63.7%), anxiety or depression (47.5%), and difficulties performing usual activities (45.6%).
Table 1.
Overview of participant characteristics
| Participant profile | N = 237 |
| Mean age (SD) n = 232, 5 missing | 71.31 (8.78) |
| Female, n (%) | 158 (66.7) |
| Male, n (%) | 79 (33.3) |
| Education, n (%) | |
| Some high school or less | 102 (43.0) |
| High school diploma | 65 (27.4) |
| Some college or more | 30 (12.7) |
| College or university degree | 40 (16.9) |
|
Marital status, n (%) n = 236, 1 missing | |
| Married | 13 (5.5) |
| Living common-law | 6 (2.5) |
| Widowed | 62 (26.3) |
| Separated | 18 (7.6) |
| Divorced | 93 (39.4) |
| Single, never married | 44 (18.6) |
|
Ethnic group of biological mother, n (%) n = 233, 4 missing | |
| White | 211 (91.0) |
| Aboriginal | 2 (0.9) |
| Black (Afro-Caribbean) | 1 (03.9) |
| East Asian (Chinese, Vietnamese, Filipino, Korean, etc.) | 4 (1.7) |
| South Asian (East Indian, Pakistani, Sri Lankan, etc.) | 3 (1.3) |
| Other non-white (Latin American, Arab, West Arab) | 3 (1.3) |
|
Ethnic group of biological father, n (%) n = 234, 3 missing | |
| White | 211 (90.2) |
| Aboriginal | 2 (0.9) |
| Black (Afro-Caribbean) | 10 (4.3) |
| East Asian (Chinese, Vietnamese, Filipino, Korean, etc.) | 4 (1.7) |
| South Asian (East Indian, Pakistani, Sri Lankan, etc.) | 3 (1.3) |
| Other non-white (Latin American, Arab, West Arab) | 4 (1.7) |
| Health profile | |
|
Self-reported health status, n (%) n = 237, 0 missing | |
| Good/very good/excellent | 140 (68.8) |
| Fair/poor | 97 (32.2) |
|
Mobility issues, n (%) n = 237, 0 missing | |
| Absent | 86 (36.3) |
| Present | 151 (63.7) |
|
Pain/discomfort, n (%) n = 237, 0 missing | |
| Absent | 61 (25.7) |
| Present | 176 (75.2) |
|
Self-care issues, n (%) n = 237, 0 missing | |
| Absent | 190 (80.2) |
| Present | 47 (19.8) |
|
Anxiety/depression, n (%) n = 236, 1 missing | |
| Absent | 124 (52.5) |
| Present | 112 (47.5) |
|
Issues performing usual activities, n (%) n = 237, 0 missing | |
| Absent | 129 (54.4) |
| Present | 108 (45.6) |
Health literacy scores
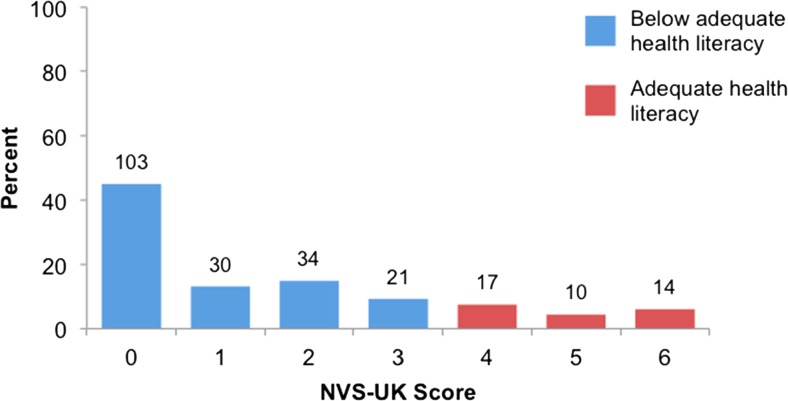
Of the 237 participants who completed the HABiT questionnaire, 229 (96.6%) completed the NVS-UK section. Of the 229 individuals who completed the NVS-UK, 188 (82.1%) had below adequate health literacy skills, whereas only 41 (17.9%) had adequate health literacy scores (see Fig. 1).
Fig. 1.
NVS-UK health literacy scores among study participants
Multivariable logistic regression was conducted using binary health literacy scores (adequate or below adequate) as the dependent variable to determine its association with other health-related variables. Through the regression analysis, significant relationships (p < 0.05) were found with BMI, education level, and pain and discomfort levels (see Table 2); the relationship was not significant with the other independent variables included in the model. The model was found to be a good fit (Hosmer and Lemeshow goodness of fit: chi-square 6.615, p = 0.579).
Participants who completed high school education or less had significantly lower odds of having adequate health literacy, compared to those who attended college or university (OR 0.224, 95% CI .084 to 0.595). The odds of having adequate health literacy was significantly higher in participants with a BMI in the underweight and overweight/obese BMI categories, compared to those who had a weight in the normal range of 18.5 to 24.9 kg/m2 (OR 17.222, 95% CI 1.608 to 184.418 and OR 7.966, 95% CI 1.341 to 47.308, respectively). Finally, participants reporting that they had pain or discomfort had significantly higher odds of having adequate health literacy, compared to those reporting no regular pain or discomfort (OR 4.300, 95% CI 1.053 to 17.552).
Discussion
More than 80% of older adult participants living in select subsidized housing buildings in Hamilton, Ontario, demonstrated below adequate functional health literacy levels as determined by the NVS-UK assessment tool. This is similar to the prevalence reported by the Canadian Council on Learning, which found that only one in eight adults (12%) over age 65 has adequate health literacy skills (Rootman and Gordon-El-Bihbety 2008). Consistent with previous research in older adults (Wister et al. 2010; Baker et al. 2000), below adequate health literacy in the study population was significantly associated with a lower education level. In this population, normal BMI and having no regular pain or discomfort were also found to be significantly associated with functional health literacy. Participant age group, gender, marital status, CANRISK (diabetes risk) score, mobility issues, self-care issues, anxiety and depression levels, performance of usual activities, or self-reported health status did not reveal any statistically significant relationships with health literacy.
Past literature has found that older adults with a BMI outside the normal range had lower health literacy (Geboers et al. 2016), conflicting with the results of the current study. In this population, we found that participants with a BMI outside of the normal range, whether above or below, had higher health literacy levels. This finding may be a result of those outside normal limits having had more attention drawn to their weight and possibly having more health education on reading food labels in an effort to correct this health risk. Having these dietary education interactions could positively impact their ability to correctly respond to the NVS-UK questions, which uses a food label assessment, and may confound the observed relationship. Therefore, caution should be used when interpreting these results and additional studies should investigate this relationship further with other health literacy tools.
In contrast to previous research in older adults (Wolf et al. 2005), we found that self-reported health status and four of the five domains of health-related quality of life were not associated with functional health literacy in the study population. The only domain that had a significant relationship was the presence of pain or discomfort. Although there was sufficient heterogeneity in self-reported health status and all five quality of life domains, the insignificant results suggest that either the low SES of this entire study population or other factors that were controlled for in the analysis (e.g., education) attenuated the expected relationship between health literacy and quality of life. It is possible that these other factors (e.g., education) have a much stronger association with health literacy in this population, or it could mean that individuals in this study population, despite varying degrees of quality of life, are equally likely or equally less likely to seek out resources that would provide the opportunity to increase health literacy.
As noted above, pain or discomfort was the only quality of life domain found to be significantly associated with adequate health literacy in this context. In the limited studies available on this specific domain, pain and discomfort was not associated with health literacy (Briggs et al. 2010; Devraj et al. 2013), but we hypothesize that in this population (low income, low education), those with pain or discomfort may be more likely to seek out medical attention and therefore have more health education.
We found no significant relationship between participant age group and functional health literacy. Research suggests that adults over age 65 have lower health literacy compared to their younger counterparts (Canadian Council on Learning 2007a; Canadian Council on Learning 2007b); however, this is comparing the full spectrum of adults (16 years and older), while the current study only included those 55 years and older. The findings of the current study suggest that, in a subsidized housing context, there is no significant difference in functional health literacy between those who are 55–64 years old and those in older age categories.
A higher CANRISK score was hypothesized to predict below adequate health literacy. The relationship between health literacy and diabetes has been documented in the literature as lower health literacy is more prevalent among individuals with diabetes (Schillinger et al. 2002). This is likely a result of decreased knowledge about diabetes risk factors (Williams et al. 1998; Schillinger et al. 2002). The study findings suggest that individuals with a lower health literacy also have poorer glycemic control and therefore have a higher burden of diabetes-related problems (Schillinger et al. 2002). However, this study found no significant association between functional health literacy and having a high risk of diabetes. Further research with individuals who already have diabetes in this population is needed to better understand their health literacy and its impact on glycemic control and other diabetes-related health concerns.
Overall, there is no significant difference in the health literacy scores of men and women, which has been supported in previous literature (Rootman and Gordon-El-Bihbety 2008). The link between marital status and health literacy is also not significant. A prior study among older adults found no significant difference in health literacy levels for those living alone (Geboers et al. 2016).
Strengths and limitations
This study has targeted a vulnerable, hard-to-reach population with a demographic profile that differs substantially from the general older adult population. The characteristics of these individuals (living alone, limited education, low income) are underrepresented in health research and it required substantial resources to capture this novel data. Although the findings of this study cannot be generalized to the broader population of older adults, it provides unique insight and may be generalizable to other subsidized seniors’ buildings in other communities.
Convenience sampling was deemed necessary to access this understudied population. The study started with a random sampling design, knocking on the doors of pre-defined unit numbers; however, we determined that this was not feasible. Many residents were not willing to open their doors to an unknown individual, even with identification and notice that we would be in the building. While two of the five buildings were randomly sampled, it required a substantial amount of time and there were a lot of non-responders, requiring the list of random units to be expanded in order to achieve the desired sample size. By continuing to expand the list of random numbers until we reached enough individuals willing to answer their door, it most likely led to a biased sample akin to convenience sampling. Therefore, it was decided to survey the remaining three buildings using convenience sampling. This experience highlights one of the reasons why this population is understudied and the importance of our first look into this vulnerable population.
While convenience sampling was used, our sample is still relatively representative of the larger population of interest based on demographic information provided by City Housing Hamilton for these five seniors’ buildings. For example, 67.7% of respondents were 65 years and older, compared to 66.8% of all residents, and 92.2% of respondents were living alone, compared to 92.0% of all residents. Our sample did have more female representation (66.7% of respondents versus 56.8% of all residents). These limitations should be considered when interpreting the study results and when designing future research studies with this population.
Conclusion
As the population of older adults in Canada grows, attention must be focused on strategies to assist these individuals in achieving desirable health outcomes. The study population was of lower SES and had generally low levels of formal education; this population is also more likely to have chronic health problems and therefore will face more barriers due to the inadequate functional health literacy observed. Further research is needed to understand the observed relationships for functional literacy with BMI and quality of life, given their contrast to previous research with the general population of older adults. Specifically, assessing functional health literacy with other tools, assessing other types of health literacy in this population (i.e., communicative and critical literacy), and using qualitative methods to gain more insight into these associations could improve our understanding of these dynamics. Gathering information on the health literacy levels of this population is the first step in providing more equitable health services, understanding that health literacy barriers can be a hindrance to properly managing health-related conditions (e.g., diabetes). This can be addressed through targeted health literacy education within this population as well as ensuring that health information and related materials (e.g., chronic disease management) are delivered in a manner appropriate for individuals with limited health literacy.
Acknowledgements
We would like to acknowledge the help and support of the City of Hamilton Housing Department.
Appendix 1
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflicts of interest.
References
- Agarwal G, Angeles R (2017) Development and validation of the Health Awareness and Behaviour Tool (HABiT). Trillium Primary Health Care Research Day. Wednesday, June 1st 2017. Metro Toronto Convention Centre.
- Baker DW, Gazmararian JA, Sudano J, Patterson M. The association between age and health literacy among elderly persons. The Journals of Gerontology Series B: Psychological Sciences and Social Sciences. 2000;55(6):S368–S374. doi: 10.1093/geronb/55.6.S368. [DOI] [PubMed] [Google Scholar]
- Bassuk SS, Berkman LF, Amick BC. Socioeconomic status and mortality among the elderly: Findings from four US communities. American Journal of Epidemiology. 2002;155(6):520–533. doi: 10.1093/aje/155.6.520. [DOI] [PubMed] [Google Scholar]
- Baur C. (2010). The national action plan to improve health literacy. Washington D.C.: US Department of Health and Human Services, Office of Disease Prevention and Health Promotion.
- Berkman ND, Sheridan SL, Donahue KE, Halpern DJ, Crotty K. Low health literacy and health outcomes: An updated systematic review. Annals of Internal Medicine. 2011;155(2):97–107. doi: 10.7326/0003-4819-155-2-201107190-00005. [DOI] [PubMed] [Google Scholar]
- Briggs AM, Jordan JE, Buchbinder R, Burnett AF, O’Sullivan PB, Chua JY, Osborne RH, Straker LM. Health literacy and beliefs among a community cohort with and without chronic low back pain. Pain. 2010;150(2):275–283. doi: 10.1016/j.pain.2010.04.031. [DOI] [PubMed] [Google Scholar]
- Canadian Council on Learning . Health literacy in Canada: Initial results from the International Adult Literacy and Skills Survey. Ottawa: Canadian Council on Learning; 2007. [Google Scholar]
- Canadian Council on Learning . State of learning in Canada: No time for complacency. Ottawa: Canadian Council on Learning; 2007. [Google Scholar]
- Canadian Public Health Association. (1998). Working with low-literacy seniors: practical strategies for health providers. Ottawa: National Literacy and Health Program. Available at: http://www.cpha.ca/uploads/portals/h-l/l-l-seniors_e.pdf. Accessed Dec 2016.
- City of Hamilton. (n.d.). Building selection form. Hamilton: CityHousing Hamilton Available at: http://www.cityhousinghamilton.com/userfiles/file/LookingForHousing/BuildingSelectionForm_Revised.pdf. Accessed 1 Nov 2017.
- City of Toronto . Rent-Geared-To-Income (RG) Administration Manual, Chapter 8: Filling Vacancies and Allocating RGI Assistance. Toronto: City of Toronto Shelter, Support and Housing Administration; 2015. [Google Scholar]
- Devraj R, Herndon CM, Griffin J. Pain awareness and medication knowledge: A health literacy evaluation. Journal of Pain & Palliative Care Pharmacotherapy. 2013;27(1):19–27. doi: 10.3109/15360288.2012.751955. [DOI] [PubMed] [Google Scholar]
- Gazmararian JA, Williams MV, Peel J, Baker DW. Health literacy and knowledge of chronic disease. Patient Education and Counseling. 2003;51(3):267–275. doi: 10.1016/S0738-3991(02)00239-2. [DOI] [PubMed] [Google Scholar]
- Geboers B, Reijneveld SA, Jansen CJ, de Winter AF. Health literacy is associated with health behaviors and social factors among older adults: Results from the LifeLines Cohort Study. Journal of Health Communication. 2016;21:45–53. doi: 10.1080/10810730.2016.1201174. [DOI] [PubMed] [Google Scholar]
- Hosmer Jr DW, Lemeshow S, Sturdivant RX. (2013). Applied logistic regression, chapter 2 (pp. 35–47). Hoboken: John Wiley & Sons.
- Huguet N, Kaplan MS, Feeny D. Socioeconomic status and health-related quality of life among elderly people: Results from the Joint Canada/United States Survey of Health. Social science and medicine. 2008;66(4):803–810. doi: 10.1016/j.socscimed.2007.11.011. [DOI] [PubMed] [Google Scholar]
- Hypertension Canada. (2015). Hypertension Canada CHEP Guidelines 2015. Available at http://guidelines.hypertension.ca/. Accessed Dec 2016.
- Kim S, Love F, Quistberg DA, Shea JA. Association of health literacy with self-management behavior in patients with diabetes. Diabetes Care. 2004;27(12):2980–2982. doi: 10.2337/diacare.27.12.2980. [DOI] [PubMed] [Google Scholar]
- Mitchell B, Begoray, DL. (2010). Electronic personal health records that promote self-management in chronic illness. The Online Journal of Issues in Nursing, 15(3). 10.3912/OJIN.Vol15No03PPT01
- Murray S, Hagey J, Willms D, Shillington R, Desjardins R. Health literacy in Canada: A healthy understanding. Ottawa: Canadian Council on Learning; 2008. [Google Scholar]
- Niagara Regional Housing . NRH Notice 03-20: Age Requirement for Senior Mandated Housing. Thorold: Niagara Regional Housing; 2003. [Google Scholar]
- Nutbeam D. Health literacy as a public health goal: A challenge for contemporary health education and communication strategies into the 21st century. Health Promotion International. 2000;15(3):259–267. doi: 10.1093/heapro/15.3.259. [DOI] [Google Scholar]
- Ontario Ministry of Finance . Ontario population projections update 2015–2041. Ottawa: Ontario Ministry of Finance; 2016. [Google Scholar]
- Platts-Mills TF, Leacock B, Cabanas JG, Shofer FS, McLean SA. Emergency medical services use by the elderly: Analysis of a statewide database. Prehospital Emergency Care. 2010;14(3):329–333. doi: 10.3109/10903127.2010.481759. [DOI] [PubMed] [Google Scholar]
- Robinson CA, Agarwal G, Nerenberg K. Validating the CANRISK prognostic model for assessing diabetes risk in Canada's multi-ethnic population. Chronic diseases and injuries in Canada. 2011;32(1):19–31. [PubMed] [Google Scholar]
- Rootman I, Gordon-El-Bihbety D. A vision for a health literate Canada. Ottawa, ON: Canadian Public Health Association; 2008. [Google Scholar]
- Rowlands G, Khazaezadeh N, Oteng-Ntim E, Seed P, Barr S, Weiss BD. Development and validation of a measure of health literacy in the UK: The newest vital sign. BMC Public Health. 2013;13(1):116. doi: 10.1186/1471-2458-13-116. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schillinger D, Grumbach K, Piette J, et al. Association of health literacy with diabetes outcomes. Journal of the American Medical Association. 2002;288:475–482. doi: 10.1001/jama.288.4.475. [DOI] [PubMed] [Google Scholar]
- Schillinger D, Piette J, Grumbach K, Wang F, Wilson C, Daher C, Leong-Grotz K, Castro C, Bindman AB. Closing the loop: Physician communication with diabetic patients who have low health literacy. Archives of Internal Medicine. 2003;163(1):83–90. doi: 10.1001/archinte.163.1.83. [DOI] [PubMed] [Google Scholar]
- Shum J, Poureslami I, Doyle-Waters MM, FitzGerald JM. The application of health literacy measurement tools (collective or individual domains) in assessing chronic disease management: A systematic review protocol. Systematic Reviews. 2016;5:97. doi: 10.1186/s13643-016-0267-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Social Planning and Research Council of Hamilton . A profile of vulnerable seniors in Hamilton. Hamilton: The Social Planning and Research Council of Hamilton; 2011. [Google Scholar]
- Statistics Canada. (2006). A portrait of seniors in Canada: Introduction. Available at http://www.statcan.gc.ca/pub/89-519-x/89-519-x2006001-eng.htm. Accessed Dec 2016.
- Statistics Canada. (2016). Canadian Community Health Survey: Array. Available at http://www.statcan.gc.ca/eng/survey/household/3226. Accessed Dec 2016.
- Weiss BD, Mays MZ, Martz W, Castro KM, DeWalt DA, Pignone MP, Mockbee J, Hale FA. Quick assessment of literacy in primary care: The newest vital sign. Annals of Family Medicine. 2005;3(6):514–522. doi: 10.1370/afm.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Williams MV, Baker DW, Parker RM, Nurss JR. Relationship of functional health literacy to patients' knowledge of their chronic disease: A study of patients with hypertension and diabetes. Archives of Internal Medicine. 1998;158(2):166–172. doi: 10.1001/archinte.158.2.166. [DOI] [PubMed] [Google Scholar]
- Wister AV, Malloy-Weir LJ, Rootman I, Desjardins R. Lifelong educational practices and resources in enabling health literacy among older adults. Journal of Aging and Health. 2010;22(6):827–854. doi: 10.1177/0898264310373502. [DOI] [PubMed] [Google Scholar]
- Wolf MS, Gazmararian JA, Baker DW. Health literacy and functional health status among older adults. Archives of Internal Medicine. 2005;165(17):1946–1952. doi: 10.1001/archinte.165.17.1946. [DOI] [PubMed] [Google Scholar]