Abstract
Objectives
To determine volumes and rates of multimorbidity in Ontario by age group, sex, material deprivation, and geography.
Methods
A cross-sectional population-based study was completed using linked provincial health administrative databases. Ontario residents were classified as having multimorbidity (3+ chronic conditions) or not, based on the presence of 17 chronic conditions. The volumes (number of residents) of multimorbidity were determined by age categories in addition to crude and age-sex standardized rates.
Results
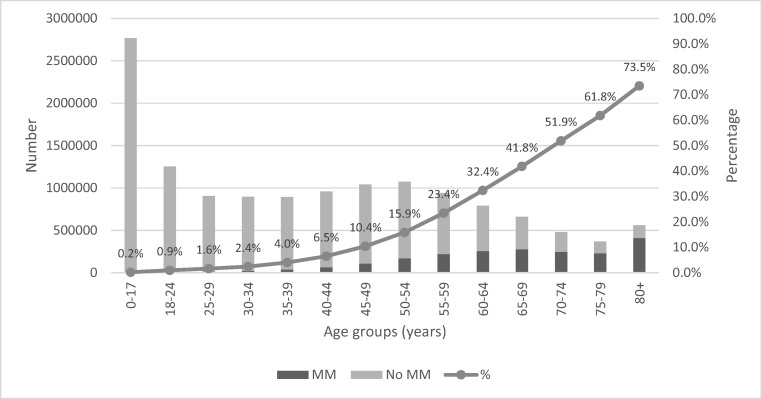
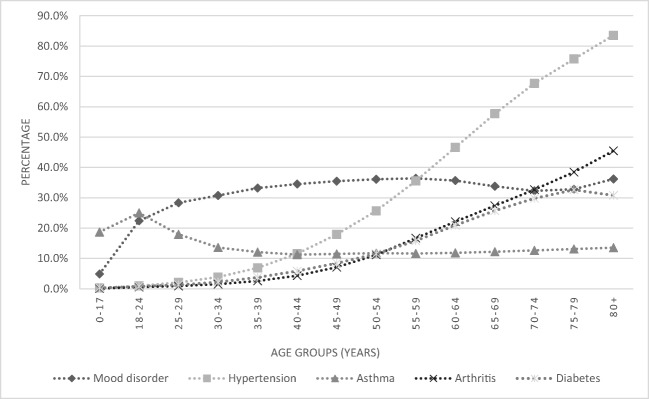
Among the 2013 Ontario population, 15.2% had multimorbidity. Multimorbidity rates increased across successively older age groups with lowest rates observed in youngest (0–17 years, 0.2%) and highest rates in the oldest (80+ years, 73.5%). The rate of multimorbidity increased gradually from ages 0 to 44 years, with a substantial and graded increase in the rates as the population aged. The top five chronic conditions, of the 17 examined, among those with multimorbidity were mood disorders, hypertensive disorders, asthma, arthritis, and diabetes.
Conclusion
Much of the common rhetoric around multimorbidity concerns the aging ‘grey tsunami’. This study demonstrated that the volume of multimorbidity is derived from adults beginning as young as age 35 years old. A focus only on the old underestimates the absolute burden of multimorbidity on the health care system. It can mask the association of material deprivation and geography with multimorbidity which can turn our attention away from two critical issues: (1) potential inequality in health and health care in Ontario and (2) preventing younger and middle-aged people from moving into the multimorbidity category.
Electronic supplementary material
The online version of this article (10.17269/s41997-018-0103-0) contains supplementary material, which is available to authorized users.
Keywords: Multimorbidity, Chronic conditions, Population health, Ontario
Résumé
Objectif
Déterminer les volumes et les taux de multimorbidité en Ontario selon le groupe d’âge, le sexe, la défavorisation matérielle et la géographie.
Méthode
Une étude populationnelle transversale a été exécutée en maillant des bases de données administratives de santé provinciales. Les résidents de l’Ontario ont été catégorisés comme ayant ou non des multimorbidités (3 états chroniques ou plus) en fonction de la présence de 17 états chroniques. Les volumes (nombre de résidents) de multimorbidité ont été déterminés par catégorie d’âge en plus des taux bruts et des taux standardisés pour l’âge et le sexe.
Résultats
Dans la population ontarienne de 2013, 15,2% des gens étaient atteints de multimorbidités. Les taux de multimorbidité augmentaient avec chaque groupe d’âge, les taux les plus faibles étant observés chez les plus jeunes (0-17 ans : 0,2%), et les taux les plus élevés, chez les plus âgés (80 ans et plus : 73,5%). Le taux de multimorbidité augmentait progressivement entre 0 et 44 ans, avec une hausse graduelle considérable dans les taux avec l’âge de la population. Sur les 17 états chroniques compris dans l’étude, les 5 états les plus courants chez les personnes atteintes de multimorbidités étaient les troubles de l’humeur, les troubles hypertensifs, l’asthme, l’arthrite et le diabète.
Conclusion
Le discours sur la multimorbidité s’articule principalement autour du « tsunami gris » du vieillissement. Notre étude démontre que le volume de multimorbidité comprend des adultes aussi jeunes que 35 ans. La restriction des études aux seules personnes âgées sous-estime le fardeau absolu de la multimorbidité sur le système de soins de santé. Elle peut masquer l’association entre la défavorisation matérielle ou la géographie et les multimorbidités, ce qui peut détourner notre attention de deux questions névralgiques : 1) les inégalités possibles sur le plan de la santé et des soins de santé en Ontario et 2) comment empêcher les jeunes et les personnes d’âge moyen de passer dans la catégorie des personnes atteintes de multimorbidités.
Mots-clés: Morbidité associée, Maladies chroniques, Santé des populations, Ontario
Introduction
It has become commonplace to hear that Canada’s population is graying; the baby boomer generation has reached its senior years. This is a reasonable characterization of our changing population pyramid; Statistics Canada reports that, as of July 1, 2015, for the first time Canada has more citizens 65 years and older than children aged 0 to 14 years (Statistics Canada 2015). Along with this aging population comes an increase in the prevalence of people having multiple chronic conditions, referred to as multimorbidity. Media sources report, as the result of this demographic shift, enormous and increasing pressure is being placed on the Canadian health care system (CBC News 2012; The Globe and Mail 2015). The characterization in this messaging is we are facing a ‘grey tsunami’ (CBC 2014; The Star 2015) and we need to seek shelter from its onslaught. This myopic focus on the aging population tells only part of the story (Canadian Foundation for Healthcare Improvement 2011) and may blind us to other factors, such as material deprivation or geographic variation associated with multimorbidity, which may be important for policy makers responsible for the health and health care of their citizens.
It is true that in Canada and around the world, multimorbidity is increasing. Its prevalence is low until about age 40 years and steeply increases until plateauing at about 70 years (Fortin et al. 2012). We care about multimorbidity because it confers additional burden and disability in populations and health systems over and above that expected for the sum of individual conditions, including the receipt of fragmented care from numerous chronic condition-specific providers, increased risk of adverse polypharmacy outcomes, and higher health care utilization and costs (Boyd and Fortin 2010).
It is important to understand the prevalence and drivers of multimorbidity in order to ameliorate its effects, to plan and meet health care needs, to address potential inequalities, and ultimately to improve population health. A focus on multimorbidity is particularly relevant to public health; for example, those with multimorbidity may benefit from public health programming such as chronic disease self-management (Brady et al., 2015). A focus on multimorbidity is also relevant to primary health care policy and practice. With its focus on integrating care, much of the care and coordination for those with multimorbidity falls to primary care (Fortin et al. 2010).
The Ontario Ministry of Health and Long-Term Care (MOHLTC) in its 2015 Patients First: Action Plan for Health Care (Ontario MOHLTC 2015) has set as one priority ‘primary care providers are organized around the needs of our population…’. This population orientation necessitates a better understanding of the Ontario population with multimorbidity, beyond the message that our population is aging and consequently getting sicker. Therefore, the purpose of this study was to determine both the volume and rates of multimorbidity by age group in Ontario; and to examine rates by other characteristics, including sex, health care model, material deprivation, and geography.
Methods
This cross-sectional population-based study used linked provincial health administrative databases to classify Ontario residents according to whether or not they had multimorbidity and to compare demographic and geographic characteristics of those with and without multimorbidity. All residents of Ontario (2013 population approximately 13 million) obtain health care services from a government-administered single-payer insurance system. The datasets used in this study are listed under the variable descriptions that follow. Datasets were linked using unique, encoded identifiers and analyzed at the Institute for Clinical Evaluative Sciences (ICES). The study was approved by the research ethics board at Sunnybrook Health Sciences Centre (Toronto, Ontario, Canada); informed consent was not required. This report follows the RECORD (REporting of studies Conducted using Observational Routinely-collected health Data) statement (Benchimol et al. 2015).
Data sources and study population
This study included everyone between ages 0 and 105 years who were alive and eligible for health insurance in Ontario as of the July 1, 2013 index date according to the Ontario Registered Persons Database (RPDB), Ontario’s health care registry. Residents were further required to have a valid health insurance number, valid recorded age and sex, and to have had any contact with the Ontario health care system within the past 7 years (Kiran et al. 2015; Kiran et al. 2016). Demographic data and participant characteristics were also obtained from the RPDB.
Outcome—multimorbidity
Multimorbidity was defined as the presence of three or more of 17 chronic conditions (Fortin et al. 2012; Holzer et al. 2014). Only conditions for which there were validated definitions for use in health administrative data were included. These patient data were obtained either from predefined cohorts with common chronic conditions or, where such definitions were not available, using algorithms to identify people with those conditions.
The presence of a given chronic condition was based on either people’s presence in existing cohorts before the index date or by looking back at their health care utilization for 5 or 10 years (condition-dependent) and applying the specified algorithm. The algorithms and cohorts employ diagnostic codes from the International Classification of Diseases, 9th and 10th Revisions (ICD-9 and ICD-10), along with codes from the Ontario Health Insurance Plan (OHIP). These codes are recorded when people receive care and are found in health services delivery databases: Canadian Institute for Health Information Discharge Abstract Database (CIHI–DAD); Canadian Institute for Health Information Same Day Surgery Database (CIHI-SDS); National Ambulatory Care Reporting System (NACRS); Ontario Drug Benefit Claims (ODB); Ontario Health Insurance Plan Claims Database (OHIP); and Ontario Mental Health Reporting System (OMHRS).
The 17 conditions, chosen based on a research tool developed for the CIHR Community-Based Primary Health Care Signature Initiative (Fortin et al. 2017), were as follows: arthritis, asthma, cancer, congestive heart failure (CHF), chronic obstructive pulmonary disease (COPD), cardiovascular disease (CVD), dementia, diabetes, HIV, hypertension, inflammatory bowel disease (IBD), chronic kidney disease (CKD), chronic liver disease, mood disorder, osteoporosis, stroke/transient ischemic attack (TIA), and urinary incontinence. Further details describing definitions, administrative codes, and associated validation studies are detailed in Appendix A.
Independent variables
Sex, date of birth, and postal code were obtained from the RPDB. Age was calculated based on the index date, July 1, 2013. The type of health care model best describing where people received their primary care was captured and defined using the Client Agency Provider Enrolment (CAPE) database. Postal code was used to determine to which regional health authorities (Local Health Integration Network (LHIN)) people belonged. There are 14 LHINs in Ontario (Ontario LHINs 2014). The provincial government through the MOHLTC provides overall stewardship of Ontario’s health system, setting direction, strategic policy and system standards and delivering provincial programs and services (Ontario MOHLTC 2012). The LHINs are funded by the MOHLTC and ‘plan, coordinate and fund local health care services to improve access to health services and patient experience’ (Ontario MOHLTC 2017).
People were assigned to either an urban material deprivation quintile or to a rural location. Material deprivation is one of four indicators that are part of the Ontario Marginalization Index (Matheson et al. 2012). The material deprivation index was only applied to urban locations because it is considered reliable in urban settings where Census Dissemination Areas (CDAs) are small enough to allow for discrimination. In rural areas (defined as rural and small town communities of less than 10,000 persons), where CDAs can be geographically large, material deprivation can vary substantially within the CDA, making material deprivation quintiles unreliable (Wilkins 2004). People were classified as living in an urban or rural location using Canada Post’s Postal Code Conversion File Plus (PCCF+) (Statistics Canada 2013). Postal code located urban people within their CDA; they were assigned the material deprivation index of the CDA in which they lived. Based on this material deprivation index, people in urban areas were classified into material deprivation quintiles with 1 representing the least deprived and 5 representing the most deprived.
Analysis
People in the cohort were classified as having multimorbidity or not as determined by the presence of three or more of 17 chronic conditions examined; comparisons between the two groups were made based on mean age, sex, health care model, material deprivation/rural, and the 17 chronic conditions. Prevalence of multimorbidity was examined using volume (absolute numbers) and proportions (percentages) for the child age group from 0 to 17 years old, and then in 5-year age groups for adults from 18 to 80+ years. Further, the volume and proportion with each chronic condition among the age groups was determined. Prevalence of multimorbidity by material deprivation index and by LHIN was examined using volume and rates (annual proportions). In order to account for different age and sex composition across age, sex, material deprivation, and LHIN, crude rates and age-sex standardized rates using direct standardization to the 1991 Canadian population (Statistics Canada 2012) are reported. Confidence intervals of 95% were calculated around the standardized rates (Bains 2009).
Results
Multimorbidity cohort
The study identified a cohort of 13,581,191 people residing in Ontario on July 1, 2013.The presence of the 17 chronic conditions was obtained for the entire cohort. Among the Ontario population in 2013, 44% had no chronic conditions, 27.5% had one chronic condition, and 13.4% had two chronic conditions. The remaining 15.2% were classified as having multimorbidity, defined as three or more of the 17 examined chronic conditions (Table 1). Table 1 reports the characteristics of those with and without multimorbidity. People with multimorbidity were, on average, twice as old as people without multimorbidity. Males were less represented in the multimorbidity group; accounting for 43.4% of the multimorbidity cohort. While the majority of people in Ontario were enrolled in a primary health care model, participation was higher for those with multimorbidity (90.9% vs. 82.4%). The percentage of those with the least material deprivation was 5% lower for those with multimorbidity. The percentage of rural residents was lower for those without multimorbidity than for those with. There were large differences in the percentage of certain of the 17 chronic conditions between those with and without multimorbidity; for example, the percentage of people with multimorbidity who had hypertension was 77.5% compared to 10.9% for those without multimorbidity.
Table 1.
Characteristics of Ontario population by multimorbidity status (column %)
| Multimorbidity | |||
|---|---|---|---|
| No | Yes | All | |
| Total | N = 11,514,013 | N = 2,067,178 | N = 13,581,191 |
| 84.8% | 15.2% | ||
| Age (mean (SD)) | 34.9 (20.5) | 66.1 (14.7) | 39.6 (22.7) |
| Sex (male) | 5,766,465 (50.1%) | 897,645 (43.4%) | 6,664,110 (49.1%) |
| Health care model (enrolment model) | 9,489,981 (82.4%) | 1,878,143 (90.9%) | 11,368,124 (83.7%) |
| Material deprivation quintilesa | |||
| 1 | 2,686,447 (23.3%) | 384,502 (18.6%) | 3,070,949 (22.6%) |
| 2 | 2,044,318 (17.8%) | 348,591 (16.9%) | 2,392,909 (17.6%) |
| 3 | 1,842,131 (16.0%) | 336,951 (16.3%) | 2,179,082 (16.0%) |
| 4 | 1,692,356 (14.7%) | 335,109 (16.2%) | 2,027,465 (14.9%) |
| 5 | 1,889,011 (16.4%) | 384,299 (18.6%) | 2,273,310 (16.7%) |
| Rural | 1,209,310 (10.5%) | 250,018 (12.1%) | 1,459,328 (10.7%) |
| Missing | 150,440 (1.3%) | 27,708 (1.3%) | 178,148 (1.3%) |
| Chronic conditions | |||
| Arthritis | 434,700 (3.8%) | 921,257 (44.6%) | 1,355,957 (10.0%) |
| Asthma | 1,477,358 (12.8%) | 568,241 (27.5%) | 2,045,599 (15.1%) |
| Cancer | 324,338 (2.8%) | 579,017 (28.0%) | 903,355 (6.7%) |
| CHF | 13,181 (0.1%) | 224,523 (10.9%) | 237,704 (1.8%) |
| COPD | 216,977 (1.9%) | 602,014 (29.1%) | 818,991 (6.0%) |
| CVD | 131,206 (1.1%) | 570,652 (27.6%) | 701,858 (5.2%) |
| Dementia | 16,150 (0.1%) | 137,665 (6.7%) | 153,815 (1.1%) |
| Diabetes | 448,212 (3.9%) | 821,056 (39.7%) | 1,269,268 (9.3%) |
| HIV | 9972 (0.1%) | 7212 (0.3%) | 17,184 (0.1%) |
| Hypertension | 1,258,109 (10.9%) | 1,602,543 (77.5%) | 2,860,652 (21.1%) |
| IBD | 42,922 (0.4%) | 38,301 (1.9%) | 81,223 (0.6%) |
| Kidney disease, chronic | 21,959 (0.2%) | 173,455 (8.4%) | 195,414 (1.4%) |
| Liver disease, chronic | 135,903 (1.2%) | 142,571 (6.9%) | 278,474 (2.1%) |
| Mood disorder | 2,430,479 (21.1%) | 1,227,209 (59.4%) | 3,657,688 (26.9%) |
| Osteoporosis | 118,319 (1.0%) | 253,855 (12.3%) | 372,174 (2.7%) |
| Stroke/TIA | 30,062 (0.3%) | 169,453 (8.2%) | 199,515 (1.5%) |
| Urinary incontinence | 247,502 (2.1%) | 349,416 (16.9%) | 596,918 (4.4%) |
COPD chronic obstructive pulmonary disease, TIA transient ischemic attack
aPlace of residence is broken down by material deprivation for urban residents but not for rural residents. The material deprivation index is valid only within urban populations (Wilkins 2004)
Sex and age, and multimorbidity
Table 2 reports the crude and standardized rates of multimorbidity by sex and age. Multimorbidity rates increased across age groups with the lowest rates observed in the youngest age group (0–17 years, 0.2%) and the highest rates observed in the oldest (80+ years, 73.5%). Crude and sex standardized rates did not vary, suggesting rates were similar for males and females.
Table 2.
Age-sex crude and standardized (using 1991 population) rates of multimorbidity
| Crude rate (%) | Age-sex standardized rate (%) [95% CI] | |
|---|---|---|
| Overall | 15.2 | 11.5 [11.5–11.5] |
| Sexa | ||
| Female | 16.9 | 12.2 [12.2–12.2] |
| Male | 13.5 | 10.8 [10.7–10.8] |
| Age categorya | ||
| 0 to 17 years | 0.2 | 0.2 [0.2–0.2] |
| 18–24 years | 0.9 | 0.9 [0.9–0.9] |
| 25–29 years | 1.6 | 1.6 [1.6–1.6] |
| 30–34 years | 2.4 | 2.4 [2.4–2.4] |
| 35–39 years | 4.0 | 4.0 [4.0–4.0] |
| 40–44 years | 6.5 | 6.5 [6.4–6.5] |
| 45–49 years | 10.4 | 10.4 [10.4–10.5] |
| 50–54 years | 15.9 | 15.9 [15.8–15.9] |
| 55–59 years | 23.4 | 23.4 [23.3–23.5] |
| 60–64 years | 32.4 | 32.3 [32.2–32.4] |
| 65–69 years | 41.8 | 41.8 [41.6–41.9] |
| 70–74 years | 51.9 | 51.8 [51.6–52.0] |
| 75–79 years | 61.8 | 61.8 [61.5–62.0] |
| 80+ years | 73.5 | 73.5 [73.3–73.7] |
| Material deprivationb | ||
| 1—least deprived | 12.5 | 10.3 [10.2–10.3] |
| 2 | 14.6 | 11.0 [10.9–11.0] |
| 3 | 15.5 | 11.5 [11.4–11.5] |
| 4 | 16.5 | 12.1 [12.1–12.1] |
| 5—most deprived | 16.9 | 13.5 [13.5–13.6] |
| Rural | 17.0 | 11.0 [11.0–11.1] |
| Missing | 16.6 | 12.3 [12.1–12.5] |
| LHINs | ||
| LHIN 1 Erie St. Clair | 18.8 | 13.4 [13.3–13.5] |
| LHIN 2 South West | 15.4 | 10.7 [10.7–10.8] |
| LHIN 3 Waterloo Wellington | 11.6 | 9.5 [9.4–9.5] |
| LHIN 4 Hamilton Niagara Haldimand Brant | 16.9 | 11.7 [11.76–11.8] |
| LHIN 5 Central West | 13.2 | 12.2 [12.1–12.2] |
| LHIN 6 Mississauga Halton | 13.0 | 11.0 [10.9–11.1] |
| LHIN 7 Toronto Central | 14.2 | 11.5 [11.4–11.5] |
| LHIN 8 Central | 14.1 | 11.1 [11.1–11.2] |
| LHIN 9 Central East | 16.7 | 12.4 [12.4–12.5] |
| LHIN 10 South East | 18.1 | 11.7 [11.7–11.8] |
| LHIN 11 Champlain | 14.7 | 11.0 [10.9–11.0] |
| LHIN 12 North Simcoe Muskoka | 17.1 | 11.9 [11.8–12.0] |
| LHIN 13 North East | 18.5 | 12.4 [12.3–12.4] |
| LHIN 14 North West | 14.3 | 10.4 [10.3–10.6] |
aRates for males and females standardized for age; Rates for age categories standardized by sex; standardized rates based on the 1991 Canadian population
bPlace of residence is broken down by material deprivation for urban residents but not for rural residents. The material deprivation index is valid only within urban populations (Wilkins 2004)
Figure 1 describes the Ontario population with multimorbidity, reporting the volume (number of residents) of multimorbidity and percentage of people in each age group with multimorbidity. For childhood 0 to 17 years of age, of almost 3 million children, 5040 (0.2%) had multimorbidity. In the adult age groups, percentages with multimorbidity were higher at each successively older age group. In the oldest, 80+ years, 73.5% had multimorbidity, accounting for 410,099 individuals. While those 80+ years had the largest rate, the volumes and rates increased at a much earlier age. The rate of multimorbidity increased gradually from ages 0 to 44 years, with a substantial and graded increase in the rates as the population aged. Cumulatively, between ages 35 and 79 years, 1.6 million people had multimorbidity, while 0.4 million people aged 80+ years were living with multimorbidity.
Fig. 1.
Ontario population with multimorbidity: volume (number) and percentage by age group
Material deprivation and multimorbidity
Table 2 reports the crude rates and age-sex standardized rates of multimorbidity by urban material deprivation quintiles and by rural location. When age-sex standardized rates of multimorbidity were compared across levels of material deprivation, the rates increased with each quintile from 10.3% for those in the least deprived group to 13.5% for those most deprived. For people living in a rural location, the crude rural rate of 16.99% was as high as the crude 5th quintile of material deprivation; however, the age-sex standardized rate of multimorbidity was 11.03%, which would be between the 2nd and 3rd quintiles.
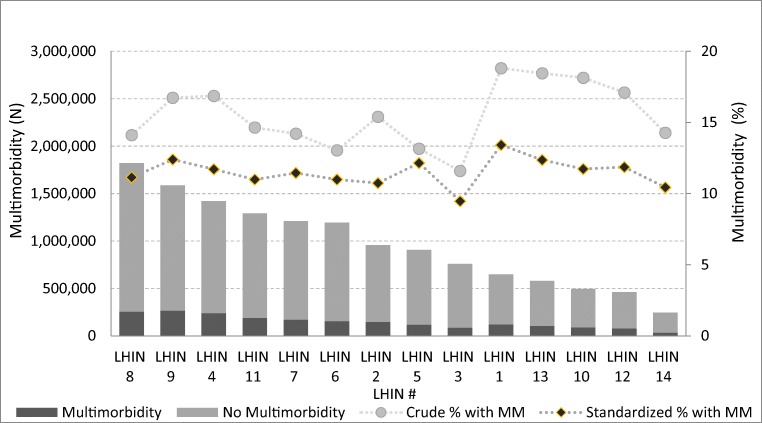
Region and multimorbidity
Table 2 reports the crude rates and age-sex standardized rates of multimorbidity by geographic distribution. Figure 2 reports multimorbidity graphically for each of the 14 LHINs in Ontario. The bars provide the volumes of people with multimorbidity within each LHIN. The lines depict yearly rate of multimorbidity (crude and age-sex standardized) which can be compared across LHINs. The age-sex standardized rate of multimorbidity ranged from 9.5% in the Waterloo-Wellington LHIN to 13.4% in the Erie-St. Clair LHIN.
Fig. 2.
Ontario population with multimorbidity: volume (N) and annual ratea by LHINb. aStandardized rates based on the 1991 Canadian population. bOrdered by LHIN from highest to lowest population
Individual chronic conditions and multimorbidity
Figure 3 provides the prevalence (percentages) of the top five chronic conditions (mood disorder, hypertensive disorders, asthma, arthritis, and diabetes) by age group for those people with multimorbidity. Appendix B provides the prevalence of each of the 17 chronic conditions by broad age groups for the Ontario population. Mood disorder persisted as one of the top five conditions in each age group. Among the adult age groups, diabetes and hypertension were in the top five conditions. For children, asthma was second in prevalence to mood disorder and the volumes of the other three top conditions were low.
Fig. 3.
Top five chronic conditions among those with multimorbidity in Ontario by percentage
Discussion
This paper examined the notion that the problem of multimorbidity rests with the aging Ontario population. This study quantified multimorbidity in the Ontario health care system by providing the numbers of people with multimorbidity by age group and quantified the relative prevalence as rates in percentages of people with multimorbidity by age group. As expected, prevalence increased across age groups and was the highest among people 80 years and older. These findings were consistent with other studies that found an association between age and rates of multimorbidity (Violan et al. 2014; Koné Pefoyo et al. 2015). Less often seen in the literature is an examination of the volume of multimorbidity by age. This study demonstrated that, in terms of the absolute numbers of people, the volume of multimorbidity is derived from adults beginning as young as age 35 years, a finding consistent with one Scottish study where the absolute numbers of people with multimorbidity was higher for those under the ages of 65 years (Barnett et al., 2012). Advanced age itself is therefore not the sole driver of volume of multimorbidity.
A focus only on advanced age prevents us from appreciating the causes and solutions to multimorbidity among people in the middle years require urgent attention. For example, it would be a worthwhile endeavor to focus serious efforts on preventing the 96% of those 35–39 years without multimorbidity from moving into the multimorbidity category as they age. While not all disease can be prevented, much of multimorbidity is derived from conditions that can be prevented or at least ameliorated through healthy lifestyle choices such as good diet and physical activity, including the top five conditions identified in this study. For example, by ages 50 to 54 years, one quarter of Ontario residents has hypertension. This number is approximately 10% higher in each successive age group. Diabetes is just as dramatic with the percentage almost tripling from 11.5% at ages 50 to 54 to 30.8% at ages 80+ years. Hypertension and diabetes are examples of conditions where efforts to prevent people in their middle years from accumulating these additional chronic conditions could have a substantial impact on population health.
Currently, our health care system focuses primarily on treating single conditions (Boyd and Fortin 2010). Given the volume of people with multimorbidity across adulthood, a reassessment of management toward multimorbidity and better coordination among specialty care may be beneficial.
There was variation in the prevalence of multimorbidity across material deprivation in Ontario. The prevalence of multimorbidity was highest for the most materially deprived and lowest for the least, with a difference of 3.2% between the two. The relationship found between material deprivation and multimorbidity was supported by a systematic review across 12 countries that found a relationship between socio-economic status and multimorbidity (Violan et al. 2014) and an Ontario study that found an association between deprivation and mental health in immigrants (Durbin et al. 2015). While the difference is small, it is of concern, given it represents a large number of residents. Despite access to universal health care, marginalized people continue to experience poorer health, suggesting an important avenue for intervention, regardless of age. It is important to consider the interaction of age group with location. The crude rate of multimorbidity for rural Ontarians is 17.0%, higher than any other urban group. However, the age-sex standardized rate is only 11.0%, comparable to the standardized rate for the least deprived urban group. This indicates that the volume of multimorbidity is, in part, a reflection of the older population found in rural areas.
There was variation in the proportion of people with multimorbidity across Ontario’s 14 LHINs with a difference of 7.2% between the LHINs with the lowest and highest crude rates of multimorbidity. These differences persisted, albeit lessened (3.9%), after accounting for age-sex differences between the LHINs, suggesting that where you live in the province is independently associated with poorer health. As with material deprivation, percentage differences are small but this translates to large numbers of residents. This is clearly a multi-dimensional problem requiring systems-level solutions that might include attending to the socio-economic and physical environment (Fung et al., 2007) as well as the health care system (Hall et al. 2017). The rate of multimorbidity was 12.4% in the North East LHIN but only 10.4% in the North West LHIN. Both LHINs are geographically remote and might be expected to have similar rates of multimorbidity; however, the lower rate in the northwest likely reflects that we used Ontario health services utilization to define the presence of the 17 chronic conditions. Because of a scarcity of services in the northwest, people often access services in nearby Manitoba or through nursing stations or federally funded services. Data on these services are not available through Ontario health administrative data. Therefore, the reduced rates were likely a reflection of how we captured the conditions. While this geography is particular to Ontario, the findings have relevance to other jurisdictions wishing to consider variation of multimorbidity with geography such as variation in regional health authorities, urban and rural locations, and geographically remote populations.
The strength of this paper lays in its ability to use health administrative data to characterize multimorbidity for the entire population of Ontario. Using age and sex standardization allows comparisons to be made across different urban material deprivation quintiles/rurality and across geographic regions, over and above what might be expected because of different age and sex variation within these units of analysis. This study also focused on both absolute and relative numbers of multimorbidity by age, a finding less often seen in the literature, but which is of public health importance. An additional contribution of this current study was the reporting of multimorbidity rates across the geography of Ontario, a consideration not seen in other studies of multimorbidity patterns.
A limitation of this paper is that only 17 chronic conditions were available to be included. As well, these conditions were defined through people’s contact with the health care system which depends on accessing care and on appropriate diagnostic codes being recorded. If anything, this suggests that estimates of multimorbidity are conservative. That multimorbidity was defined as a count of conditions is another limitation; there was no assessment of illness severity. Capturing multimorbidity using a count is consistent with the literature (van den Akker et al. 2001) and reflects data that are readily available; however, the effect of variability in severity cannot be assessed from this study. This was a cross-sectional study that did not follow the same people as they age. Therefore, one has to consider a cohort effect where, for example, the low prevalence in the middle years may be a reflection of this cohort. Smoking rates have decreased and obesity rates have risen in recent decades. It is difficult to predict how these and other forces on health may affect the rates of multimorbidity in future cohorts. If current cohorts become less healthy as they age, it will be even more important to ensure that our conversations around multimorbidity centre on more than just the inevitability of aging.
Much of the common rhetoric around multimorbidity concerns the aging ‘grey tsunami’. This is an over-simplification which disregards the important fact that currently the very old are a much smaller percentage of the overall population than are younger age groups. A focus only on the very old underestimates the absolute volume of multimorbidity on the health care system. It can turn our attention away from critical issues such as how to prevent younger people from moving into the multimorbidity category. It masks the association of material deprivation and geography with multimorbidity, an association which reflects the inequality in opportunity for all Ontarians to be healthy and may reflect inequality in access to health care services. A planned future study will determine whether there is variability in health care utilization for people with and without multimorbidity, once again examining not only by age but also by urban material deprivation/rurality and by LHIN region.
Electronic supplementary material
(DOCX 17 kb)
(DOCX 17 kb)
Funding
This study was supported by the ICES Western site through participation in the ICES Western Faculty Scholar’s Program. Support for Dr. Bridget Ryan’s participation in the ICES Western Faculty Scholars Program came from the Department of Family Medicine, Schulich School of Medicine and Dentistry, Western University. Dr. Ryan was also funded by the Canadian Institutes of Health Research Community-based Primary Health Care Innovation Team, Patient-centred Innovations for Persons with Multimorbidity.
ICES is funded by an annual grant from the Ontario Ministry of Health and Long-Term Care. Core funding for ICES Western is provided by the Academic Medical Organization of Southwestern Ontario, the Schulich School of Medicine & Dentistry, Western University and the Lawson Health Research Institute.
Compliance with ethical standards
This study was approved by the institutional review board at Sunnybrook Health Sciences Centre, Toronto, Canada.
Conflict of interest
The authors declare that they have no conflicts of interest.
Disclaimer
This project was conducted at the Institute for Clinical Evaluative Sciences (ICES) Western Site. These datasets were linked using unique encoded identifiers and analyzed at the Institute for Clinical Evaluative Sciences (ICES). The data were analyzed by Britney Allen, MSc (Biostatistician at ICES Western). Parts of this material are based on data and information compiled and provided by the Canadian Institute for Health Information (CIHI). However, the analyses, conclusions, opinions, and statements expressed herein are those of the authors, and not necessarily those of CIHI or the other funding sources. No endorsement by CIHI or the other funding sources is intended or should be inferred.
Contributor Information
Bridget L. Ryan, Phone: 519-661-2111, Email: bryan@uwo.ca
Krista Bray Jenkyn, Email: kbrayjenkyn@ices.on.ca.
Salimah Z. Shariff, Email: Salimah.Shariff@ices.on.ca
Britney Allen, Email: Britney.allen@ices.on.ca.
Richard H. Glazier, Email: Rick.glazier@ices.on.ca
Merrick Zwarenstein, Email: Merrick.zwarenstein@ices.on.ca.
Martin Fortin, Email: Martin.Fortin@usherbrooke.ca.
Moira Stewart, Email: moira@uwo.ca.
References
- Bains N. (2009). Standardization of rates. Report from the Association of Public Health Epidemiologists in Ontario (APHEO) through the Core Indicators for Public Health in Ontario Project.
- Barnett K, Mercer SW, Norbury M, Watt G, Wyke S, Guthrie B. Epidemiology of multimorbidity and implications for health care, research, and medical education: a cross-sectional study. Lancet. 2012;380:37–43. doi: 10.1016/S0140-6736(12)60240-2. [DOI] [PubMed] [Google Scholar]
- Benchimol EI, Smeeth L, Guttmann A, Harron K, Moher D, Petersen I, et al. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) statement. PLoS Med. 2015;12(10):e1001885. doi: 10.1371/journal.pmed.1001885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Boyd CM, Fortin M. Future of multimorbidity research: how should understanding of multimorbidity inform health system design? Public Health Review. 2010;32:451–474. doi: 10.1007/BF03391611. [DOI] [Google Scholar]
- Brady TJ, Anderson LA, Kobau R. Chronic disease self-management support: public health perspectives. Front Public Health. 2015;2(Article 234):1–5. doi: 10.3389/fpubh.2014.00234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Canadian Foundation for Healthcare Improvement. (2011). Myth: the aging populations is to blame for uncontrollable healthcare costs. Mythbusters: using evidence to debunk common misconceptions in Canadian Healthcare. February 2011. Retrieved June 23, 2017. http://www.cfhi-fcass.ca/sf-docs/default-source/mythbusters/Myth_AgingPopulation_EN_FINAL.pdf?sfvrsn=0
- CBC News. (2012). Baby boomers’ health demands will pose challenges. May 29, 2012. Retrieved Jun 23, 2017. http://www.cbc.ca/news/health/baby-boomers-health-demands-will-pose-challenges-1.1151890.
- CBC News (2014). June 11, 2014. Retrieved Jun 23, 2017. https://www.theglobeandmail.com/opinion/our-hospitals-are-not-ready-forthegreytsunami/article19113784/.
- Durbin A, Moineddin R, Lin E, Steele LS, Glazer RH. Examining the relationship between neighbourhood deprivation and mental health service use of immigrants in Ontario, Canada: a cross-sectional study. BMJ Open. 2015;5:e006690. doi: 10.1136/bmjopen-2014-006690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin M, Hudon C, Haggerty J, Akker M, Almirall J. Prevalence estimates of multimorbidity: a comparative study of two sources. BMC Health Services Research. 2010;10(1):111. doi: 10.1186/1472-6963-10-111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin M, et al. A systematic review of prevalence studies on multimorbidity: toward a more uniform methodology. Annals of Family Medicine. 2012;10:142–151. doi: 10.1370/afm.1337. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fortin M, Almirall J, Nicholson K. Development of a research tool to document self-reported chronic conditions in primary care. Journal of Comorbidity. 2017;7(1):117–123. doi: 10.15256/joc.2017.7.122. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fung KY, Luginaah IN, Gorey KM. Impact of air pollution on hospital admissions in southwestern Ontario, Canada: generating hypotheses in sentinel high-exposure places. Environ Health. 2007;6:18. doi: 10.1186/1476-069X-6-18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hall RE, Khan F, Levi J, Ma H, Fang J, Martin C, et al. (2017). Ontario and LHIN 2015/16 stroke report cards and progress reports: Setting the bar higher. Toronto, ON: Institute for Clinical Evaluative Sciences
- Holzer BM, Siebenhuener K, Bopp M, Minder CE. (2014). Overcoming cut-off restrictions in multimorbidity prevalence estimates. BMC Public Health, 14: 780. http://www.biomedcentral.com/1471-2458/14/780. [DOI] [PMC free article] [PubMed]
- Kiran T, Kopp A, Moineddin R, Glazier RH. Longitudinal evaluation of physician payment reform and team-based care for chronic disease management and prevention. CMAJ. 2015;187(17):E494–E502. doi: 10.1503/cmaj.150579. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kiran T, Kopp A, Glazier RH. Those left behind from voluntary medical home reforms in Ontario, Canada. Annals of Family Medicine. 2016;14(6):517–525. doi: 10.1370/afm.2000. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Koné Pefoyo AJ, Bronskill SE, Gruneir A, Calzavara A, Thavorn K, Petrosyan Y, et al. The increasing burden and complexity of multimorbidity. BMC Public Health. 2015;15:415. doi: 10.1186/s12889-015-1733-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Matheson FI, Dunn JR, Smith KLW, Moineddin R, Glazier RH. Development of the Canadian Marginalization Index: a new tool for the study of inequality. Canadian Journal of Public Health. 2012;103(Suppl. 2):S12–S16. doi: 10.1007/BF03403823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ontario Local Health Integration Network. (2014). Ontario’s LHINs. © Queen’s Printer for Ontario. Retrieved June 23, 2017. http://www.lhins.on.ca/
- Ontario Ministry of Health and Long Term Care. (2012). Legislation: Local Health System Integration Act, 2006. © Queen’s Printer for Ontario. Retrieved June 23, 2017. http://www.health.gov.on.ca/en/common/legislation/lhins/default.aspx
- Ontario Ministry of Health and Long-Term Care. (2015). Putting patients first: action plan for health care. http://www.health.gov.on.ca/en/ms/ecfa/healthy_change/. Retrieved November 16, 2015.
- Ontario Ministry of Health and Long Term Care. (2017). Data Catalogue: Legislation: Local Health Integration Network (LHIN) Offices. © Queen’s Printer for Ontario Added January 17, 2017. Retrieved June 23, 2017. https://www.ontario.ca/data/local-health-integration-network-office-lhin-locations
- Statistics Canada. (2013). Postal CodeOMConversion File (PCCF). Statistics Canada Catalogue no. 92-154-X.
- Statistics Canada. (2015). The Daily: Canada’s population estimates: age and sex, July 1, 2015. Updated September 29, 2015. Retrieved July 7, 2017. http://www.statcan.gc.ca/daily-quotidien/150929/dq150929b-eng.htm
- Statistics Canada. (2012). The Canadian population in 2011: age and sex. Catalogue no. 98-311-X2011001. Statistics Canada.
- The Globe and Mail (2015) Canada’s health-care system braces for hike in costs with influx of seniors. November 8, 2015. Retrieved June 23, 2017. https://www.theglobeandmail.com/globe-investor/retirement/canadas-health-care-system-braces-for-hike-in-costs-with-influx-of-seniors/article27169986/
- The Star (2015). Get moving on prepaing for ‘grey tsunami’: Editorial. February 2, 2015. Retrieved June 23, 2017. https://www.thestar.com/opinion/editorials/2015/02/02/get-moving-on-preparing-for-greytsunami-editorial.html.
- van den Akker M, Buntinx F, Roos S, Knottnerus JA. Problems in determining occurrence rates of multimorbidity. Journal of Clinical Epidemiology. 2001;54(7):675–679. doi: 10.1016/S0895-4356(00)00358-9. [DOI] [PubMed] [Google Scholar]
- Violan C, Foguet-Boreu Q, Flores-Meteo G, Salisbury C, Blom J, Freitag M, et al. Prevalence, determinants and patterns of multimorbidity in primary care: a systematic review of observational studies. PLoS One. 2014;9(7):e102149. doi: 10.1371/journal.pone.0102149. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilkins R. (2004). Neighbourhood income quintiles derived from Canadian postal codes are apt to be misclassified in rural but not urban areas. working paper. Statistics Canada.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 17 kb)
(DOCX 17 kb)