Abstract
Objective
To assess vaccine coverage for a cohort of children who have been in the care of the child welfare system compared to children in the general population.
Methods
This retrospective cohort study used population-based administrative health data for a 2008 birth cohort of children from Alberta, Canada. We assessed coverage at ages 2 (n = 44,206) and 7 (n = 42,241) for three vaccines with different administration schedules for children in care (at any period before the age of assessment) and those who had never been in care, comparing them using risk differences and relative risks (RRs). We similarly assessed coverage for children not in care who shared characteristics of children in care.
Results
At age two, vaccination coverage for children in care ranged from 54.3% to 81.4%, depending on vaccine. In comparison, coverage for those not in care ranged from 74.2% to 87.4%. At age seven, coverage for children in care ranged from 53.1% to 65.3%, compared to 76.6% to 83.4% for those not in care. For all vaccines at both ages, the risk for being under-vaccinated was higher for children in care (e.g., diphtheria, pertussis, tetanus, polio, Haemophilus influenzae type b at age 7: RR 2.01, 95% confidence interval [CI] (1.74–2.32). Even for children not in care who had characteristics similar to children in care, we found children in care had lower coverage.
Conclusion
Children in care have consistently lower vaccine coverage than children not in care. Policies and practices should promote optimal access to vaccination for these children.
Keywords: Vaccine, Immunization, Vaccination, Coverage, Child protective services, Child welfare
Résumé
Objectif
Déterminer la couverture vaccinale d’une cohorte bénéficiant de mesures de protection par rapport aux enfants de la population générale.
Méthodes
Il s’agit d’une étude de cohorte rétrospective qui se base sur les données administratives de santé pour diverses populations au sein d’une cohorte d’enfants de l’Alberta au Canada nés en 2008. Nous avons analysé la couverture pour trois vaccins à l’âge de deux ans (n = 44, 206) et de sept ans (n = 42, 241), sans égards au calendrier suivi, chez les enfants ayant fait l’objet de mesures de protection (à n’importe quel âge avant l’analyse) et chez ceux n’en ayant jamais bénéficié de manière à les comparer par les méthodes de différence de risques et de risques relatifs. Nous avons de la même façon analysé la couverture chez des enfants qui n’ont pas eu droit aux mesures de protection ayant des caractéristiques en commun avec les enfants qui y ont eu droit.
Résultats
La couverture vaccinale des enfants de deux ans bénéficiant de protection oscillait entre 54,3 % et 81,4 % selon le vaccin. En comparaison, pour les autres enfants du même âge, les résultats allaient de 74,2 % à 87,4 %. La couverture vaccinale des enfants de sept ans bénéficiant de protection oscillait quant à elle de 53,1 % à 65,3 %, par rapport à une fourchette de 76,6 % à 83,4 % pour les autres enfants du même âge. Pour tous les vaccins et aux deux âges, les risques de vaccination insuffisante étaient plus élevés pour les enfants ayant fait l’objet de mesures de protection (diphtérie, coqueluche, Haemophilus influenzae de type b à sept ans [risque relatif de 2,01 à intervalle de confiance de 95%, soit 1,74 à 2,32]). La couverture vaccinale était aussi plus élevée chez les enfants hors du réseau de protection ayant des caractéristiques en commun avec les enfants dans le réseau que chez ces derniers.
Conclusion
Les enfants bénéficiant de mesures de protection ont toujours une couverture vaccinale inférieure à celle des autres enfants. Des règles et pratiques devraient être mises en place pour optimiser l’accès de ces enfants aux vaccins.
Mots-clés: Vaccin, Immunisation, Vaccination, Couverture, Services de protection des enfants, Bien-être des enfants
Introduction
Children in care of the child welfare system receive supports and interventions from government and private agencies out of concern for their safety and family stability (Canadian Child Welfare Research Portal n.d.). In some cases, circumstances may necessitate that children be removed from the family home and placed in care (e.g., foster care, kinship care). These children, hereafter referred to as “children in care,” have higher health needs than children not in care yet are known to access preventive services less (American Academy of Pediatrics 2015). Possible barriers to accessing these services include poor collaboration and coordination between child service providers (Schneiderman and Villagrana 2010; Arora et al. 2014), high caseworker turnover (Ashton-Key and Jorge 2003), and neglect prior to being taken into care (Canadian Paediatric Society 2008).
Vaccination is one preventive health service that is considered among the greatest public health interventions in the last century (Ehreth 2003). Yet, inequities in vaccine coverage leave some children at risk from vaccine preventable disease (Niederhauser and Stark 2005), as has been observed in Alberta, where children with young single mothers and in lower-income neighbourhoods are less likely to be fully immunized (Bell et al. 2015; MacDonald et al. 2016). Measurement of vaccine coverage is important when determining whether herd immunity has been achieved and as a performance indicator for programs and policies (Hill et al. 2003). This is particularly true for vulnerable populations, in order to identify disparities in preventive health service utilization and disease protection. With an estimated 62,428 Canadian children in care (as of 2013) (Jones et al. 2015), the Canadian Paediatric Society has identified the need to optimize policies and services for this at-risk population (Canadian Paediatric Society 2008). To date, there are no published Canadian studies assessing vaccination coverage among children in care.
The purpose of this study was to assess vaccine coverage (i.e., the proportion of the eligible population who have received a vaccine) of children who had spent time in care of the child welfare system. We also wanted to compare this coverage to two groups: (a) children in the general population and (b) children in the general population who share some of the characteristics of children in care (i.e., young maternal age and single marital status, large number of children in the home, and multiple household moves).
Methods
This retrospective cohort study used population-based data to assess vaccination status at age 2 and 7 years for a 2008 birth cohort of Canadian children. The study took place in the province of Alberta, population 4.25 million (Government of Alberta 2016), where a universal health care insurance plan provides routine recommended childhood and adolescent vaccinations free of charge. For children 2 months old up to preschool age, these are delivered at community health centres by public health nurses, according to the schedule set by the Alberta Ministry of Health (Government of Alberta 2017). The study population consisted of all children born in the province from January 1 to December 31, 2008 with two exceptions: First Nations children living on reserves, who receive their vaccinations through federally administered programs, and children in the border town of Lloydminster, who receive vaccination services from the province of Saskatchewan.
Three population-based data sources were deterministically linked using a unique lifetime identifier: the provincial Immunization and Adverse Reaction to Immunization (ImmARI) repository, Vital Statistics, and the Alberta Health Care Insurance Plan Central Stakeholder Registry (AHCIP/CSR). Vaccination status was obtained from ImmARI, which receives individual-level vaccination data for all publicly funded vaccines, except for First Nations children on reserves and Lloydminster residents. Vital Statistics provides data on every live birth in the province and was used to identify the birth cohort and characteristics of participants, including sex, maternal marital status, maternal age, and number of previous live births for the mother. AHCIP/CSR provides information on 99% of the provincial population, as it tracks enrolment in the provincial health care insurance plan (Bell et al. 2015); it was used to identify First Nations children, deaths, departures from the province, children in care, and postal codes.
“In care” status was determined by an indicator in the AHCIP/CSR database that is assigned when a child is taken into care and a new health care card is issued. For our analysis, a child was identified as being in care at age 2 if they were in care anytime between birth and age 2 years, and for age 7 if they were in care anytime between birth and 7 years. Currently available data did not allow identification of length of time spent in care, current care status, or type of care placement.
We assessed coverage at age 2 years for the following vaccines: diphtheria, pertussis, tetanus, polio, Haemophilus influenzae type b (DTaP-IPV-Hib); meningococcal conjugate (Men-C); and measles, mumps, rubella (MMR); and at age 7 years for DTaP-IPV and MMR. This allowed for comparison of coverage for vaccines with different schedules and varying numbers of recommended doses (four doses of DTaP-IPV-Hib by age 2, with an additional dose by age 7; three doses of Men-C by age 2; one dose of MMR by age 2, with an additional dose by age 7). Men-C was not assessed at age 7 as no additional doses are due after 2 years of age. Vaccine coverage was not assessed for varicella and pneumococcal vaccines, as the recommended schedule changed partway through the study period.
In a previous Alberta study, it was identified that characteristics of under-vaccinated children included young maternal age and single marital status, high number of previous live births, and multiple household moves (Bell et al. 2015). All of these characteristics contribute to what we will refer to as “competing demands” in a household and are similar to characteristics that are often seen in children in care (Potter et al. 2015). In our study, we aimed to determine whether vaccine coverage for children in care is different from that for children who are not in care; for the latter group, we considered both those with and those without competing demands. A child was considered to have competing demands if they came from a household with two or more of the following: (1) maternal age of 25 years or less, (2) single maternal marital status, (3) mother having four or more live births, and (4) two or more household moves by 2 years of age. The first three characteristics were assessed at time of birth of the child in the cohort. The cut points for each factor were based on natural break points in the data.
Chi-square test was used to compare characteristics of children in care and those not in care. We calculated vaccination coverage for children in care and children not in care (both with and without competing demands). Relative risks (RRs) were used to determine the magnitude of the association between care status (in care versus not in care) and vaccine coverage. Moreover, we determined the risk difference of being fully vaccinated between children not in care and those in care. We also assessed and compared coverage after stratifying the “not in care” group by presence/absence of competing demands. Statistical analysis was conducted using SPSS 24.0 (IBM Corporation 2016). Ethics approval was obtained from the University of Alberta Human Research Ethics Board.
Results
Following exclusions (Fig. 1), there were 44,206 children in the 2-year-old cohort and 42,241 in the 7-year-old cohort. There were 292 (0.66%) children in care at any time during the study period, 129 at age 2 and 213 at age 7.
Fig. 1.
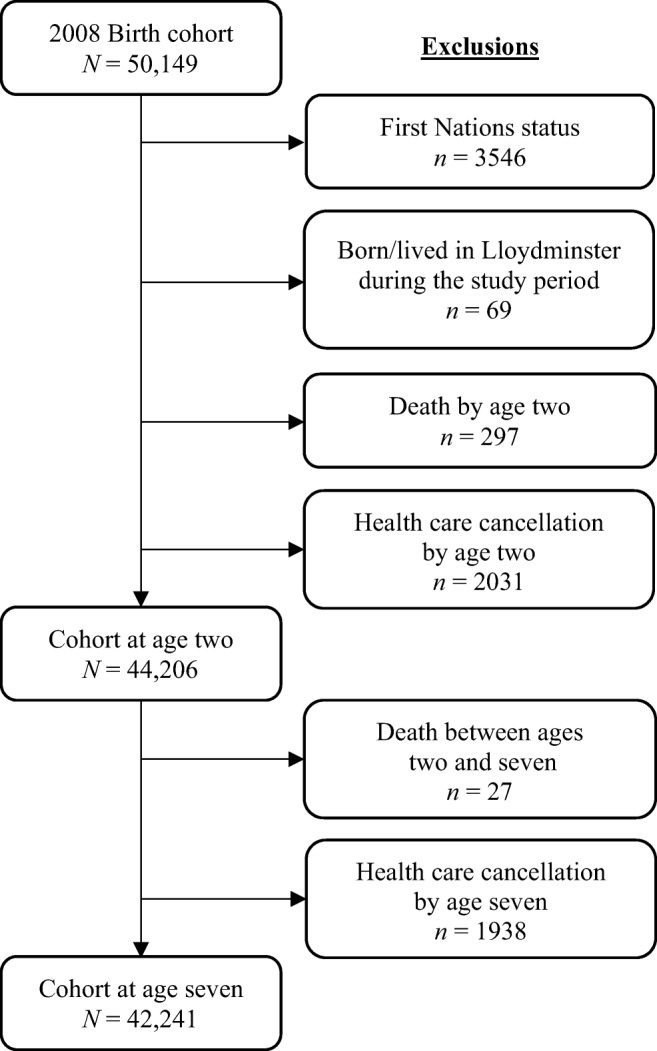
Cohort identification
Children in care versus children not in care
Table 1 presents the characteristics of children in care and children not in care. There were statistically significant differences for all characteristics, except sex of the child, between the two groups.
Table 1.
Characteristics of children in care and children not in care
| Characteristics | Children not in care (n = 43,914; 99.3%) No. (%) | Children in care (n = 292; 0.66%), No. (%) | p value for comparison |
|---|---|---|---|
| Sex of child | 0.953 | ||
| Male | 22,633 (51.5) | 151 (51.7) | |
| Female | 21,281 (48.5) | 141 (48.3) | |
| Maternal marital statusa | < 0.001 | ||
| Single | 10,909 (24.8) | 247 (84.6) | |
| Not single | 33,005 (75.2) | 45 (15.4) | |
| Maternal no. of live birthsa,b | < 0.001 | ||
| ≤ 3 | 40,591 (92.4) | 235 (80.5) | |
| ≥ 4 | 3323 (7.6) | 57 (19.5) | |
| Maternal agea | < 0.001 | ||
| ≤ 25 | 11,117 (25.3) | 182 (62.3) | |
| ≥ 26 | 32,797 (74.7) | 110 (37.7) | |
| No. of moves by age 2 | < 0.001 | ||
| ≤ 1 | 42,131 (95.9) | 203 (69.5) | |
| ≥ 2 | 1783 (4.1) | 89 (30.5) | |
| Total no. of competing demandsc,d | < 0.001 | ||
| 0 | 24,612 (56.0) | 14 (4.8) | |
| 1 | 12,358 (28.1) | 54 (18.5) | |
| 2 | 6075 (13.8) | 156 (53.4) | |
| 3 | 852 (1.9) | 63 (21.6) | |
| 4 | 17 (0.0) | 5 (1.7) |
No. number
aAt time of child’s birth
bIncludes index child
cCompeting demands are: single marital status, maternal age ≤ 25, ≥ 4 live births for mother, ≥2 household moves by age 2
dTotal percentage may not equal 100 due to rounding
Table 2 shows that at age 2, coverage for individual vaccines for children in care ranged from 54.3% for DTaP-IPV-Hib to 81.4% for MMR. At age 7, coverage was lower for these children, ranging from 53.1% for DTaP-IPV to 65.3% for MMR. Coverage decreased with increasing number of doses required.
Table 2.
Proportion of children who received all recommended vaccine doses at ages 2 and 7 for children not in care and children in care, risk difference, and relative risk (RR) for not receiving all recommended vaccine doses, for children in care versus children not in care
| Children not in care No., % (95% CI) |
Children in care No., % (95% CI) |
Risk difference of having full number of vaccine dosesa % (95% CI) | RR of not having all vaccine dosesb RR (95% CI) |
|
|---|---|---|---|---|
| Age 2 | ||||
| n = 44,077 | n = 129 | |||
| DTaP-IPV-Hib (4 doses) | 32,724, 74.2% (73.8–74.7) | 70, 54.3% (45.7–62.9) | 20.0% (11.6–28.6) | 1.78 (1.47–2.14) |
| Men-C (3 doses) | 37,731, 85.6% (85.3–85.9) | 96, 74.4% (66.9–81.9) | 11.2% (4.4–19.4) | 1.78 (1.32–2.39) |
| MMR (1 dose) | 38,513, 87.4% (87.1–87.7) | 105, 81.4% (74.7–88.1) | 6.0% (0.2–13.6) | 1.47 (1.03–2.12) |
| Age 7 | ||||
| n = 42,028 | n = 213 | |||
| DTaP-IPV (5 doses) | 32,199, 76.6% (76.2–77.0) | 113, 53.1% (46.3–59.8) | 23.6% (17.0–30.3) | 2.01 (1.74–2.32) |
| MMR (2 doses) | 35,041, 83.4% (83.0–83.7) | 139, 65.3% (58.9–71.7) | 18.1% (12.0–24.7) | 2.09 (1.74–2.52) |
No. number, CI confidence interval, DTaP-IPV-Hib diphtheria, tetanus, pertussis, polio, Haemophilus influenzae tybe b, Men-C Meningococcal, MMR measles, mumps, rubella, DTaP-IPV diphtheria, tetanus, pertussis, polio, RR relative risk
aCalculated as risk of being vaccinated for children not in care minus children in care
bReference group = children not in care; Comparison group = children in care
At age 2, children in care were more likely to be under-vaccinated for all vaccines as compared to children not in care; for example, DTaP-IPV-Hib (RR 1.78, 95% CI: 1.47–2.14) and MMR (RR 1.47, 95% CI 1.03–2.12). At age 7, the RR for being under-vaccinated for DTaP-IPV vaccine was 2.01 (95% CI 1.74–2.32) for children in care as compared to children not in care. The risk of being under-vaccinated for children in care increased with age. For example, the association between being in care and being under-vaccinated for MMR was higher at age 7 (RR 2.09, 95% CI 1.74–2.52) than at age 2 (RR 1.47, 95% CI 1.03–2.12), although the 95% CIs for the RRs do overlap. The higher risk of under-vaccination for older children in care is also seen in the risk difference; at age 2, the risk difference in MMR coverage between children not in care versus those in care was 6.0% (95% CI 0.2–13.6%), whereas at age 7, the risk difference was 18% (95% CI 12.0–24.7%). Under-vaccination for DTaP-IPV showed a similar increase in its association with care at age 7 (RR 2.01, 95% CI 1.74–2.32) as compared to at age 2 (RR 1.78, 95% CI 1.47–2.14).
Children in care versus children not in care, with and without competing demands
Table 3 compares vaccine coverage between three groups: children in care, those not in care with competing demands (i.e., with many of the same characteristics as children in care), and those not in care without competing demands. At both ages 2 and 7, children not in care without competing demands had the highest coverage for all vaccines (e.g., 76.4% for DTaP-IPV-Hib at age 2), followed by children not in care with competing demands (63.1%). Children in care had the lowest coverage (54.3%).
Table 3.
Proportion of children who received all recommended vaccine doses at ages 2 and 7, for children not in care (with and without competing demands) and children in care
| Children not in care | Children in care | ||
|---|---|---|---|
| No competing demandsa | Competing demands | ||
| No., % (95% CI) | No., % (95% CI) | No., % (95% CI) | |
| Age 2 | |||
| n = 37,010 | n = 7067 | n = 129 | |
| DTaP-IPV-Hib (4 doses) | 28,265, 76.4% (75.9–76.8) | 4459, 63.1% (62.0–64.2) | 70, 54.3% (45.7–62.9) |
| Men-C (3 doses) | 32,099, 86.7% (86.4–87.1) | 5632, 79.7% (78.8–80.6) | 96, 74.4% (66.9–81.9) |
| MMR (1 dose) | 32,671, 88.3% (87.9–88.6) | 5842, 82.7% (81.8–83.5) | 105, 81.4% (74.7–88.1) |
| Age 7 | |||
| n = 35,542 | n = 6486 | n = 213 | |
| DTaP-IPV (5 doses) | 27,934, 78.6% (78.2–79.0) | 4265, 65.8% (64.6–66.9) | 113, 53.1% (46.3–59.8) |
| MMR (2 doses) | 30,146, 84.8% (84.4–85.2) | 4895, 75.5% (74.4–76.5) | 139, 65.3% (58.9–71.7) |
No. number, CI confidence interval, DTaP-IPV-Hib diphtheria, tetanus, pertussis, polio, Haemophilus influenzae tybe b, Men-C Meningococcal, MMR measles, mumps, rubella, DTaP-IPV diphtheria, tetanus, pertussis, polio
aCompeting demands are single marital status, maternal age ≤ 25, ≥ 4 live births for mother, ≥ 2 household moves by age 2
For all vaccines in both age groups, the RR for under-vaccination was highest for children in care (as compared to those not in care without competing demands), superseding that of children not in care with competing demands (see Table 4). For example, at age 7, compared to children not in care without competing demands, the RR for being under-vaccinated for DTaP-IPV was 2.19 (95% CI 1.90–2.53) for children in care, whereas for children not in care with competing demands, it was 1.60 (95% CI 1.54–1.66).
Table 4.
Relative risk (RR) for not receiving all recommended vaccine doses at ages 2 and 7, for children not in care (with and without competing demands) and children in care
| Children not in care | Children in care | ||
|---|---|---|---|
| No competing demandsa | Competing demands | ||
| RR of not having all vaccine doses RR (95% CI) |
RR of not having all vaccine doses RR (95% CI) |
||
| Age 2 | |||
| DTaP-IPV-Hib (4 doses) | reference | 1.56 (1.51–1.62) | 1.94 (1.60–2.34) |
| Men-C (3 doses) | reference | 1.53 (1.45–1.61) | 1.93 (1.44–2.59) |
| MMR (1 dose) | reference | 1.48 (1.40–1.57) | 1.59 (1.11–2.28) |
| Age 7 | |||
| DTaP-IPV (5 doses) | reference | 1.60 (1.54–1.66) | 2.19 (1.90–2.53) |
| MMR (2 doses) | reference | 1.62 (1.54–1.70) | 2.29 (1.90–2.76) |
No. number, CI confidence interval, DTaP-IPV-Hib diphtheria, tetanus, pertussis, polio, Haemophilus influenzae tybe b, Men-C Meningococcal, MMR measles, mumps, rubella, DTaP-IPV diphtheria, tetanus, pertussis, polio, RR relative risk
aCompeting demands are single marital status, maternal age ≤ 25, ≥ 4 live births for mother, ≥ 2 household moves by age two
Discussion
This is the first Canadian study to assess the vaccine coverage of children in care (Hermann et al. 2017). We found that children in care consistently had lower vaccine coverage than children who had never been in care.
Our findings reflect the majority of the published literature from the United States (Hansen et al. 2004; Henderson et al. 2006), the United Kingdom (Ashton-Key and Jorge 2003), Italy (Ferrara et al. 2016), Australia (Arora et al. 2014), and Sweden (Kohler et al. 2015). For instance, one population-based USA study identified that children in foster care were less likely to initiate vaccination by 3 months than other children receiving Medicaid (Henderson et al. 2006). Another study from the US, based on retrospective medical record review, found that 41.9% of children in foster care were delayed in vaccination as compared to 15.3% of children not in foster care in the Medicaid program (Hansen et al. 2004). In contrast, a small number of studies found adequate or higher vaccination among children in care (Jaudes et al. 2012; Stein et al. 2014). A national study from the US found over 96% of children in care were fully vaccinated (Stein et al. 2014). However, that study used self and caregiver report for vaccination status, a method that can overestimate vaccine coverage (Miles et al. 2013). Another study identified that children in care had higher vaccine coverage than the general population, but the authors credited the higher rates to the implementation of an expanded medical home model for children in care (Jaudes et al. 2012).
Vaccine coverage when stratified by presence or absence of competing demands
The literature indicates that children with competing demands and children in care are both at greater risk for incomplete vaccination (Bell et al. 2015; Ferrara et al. 2016; Kohler et al. 2015). In addition, children in care have been identified as coming from households with competing demands (Potter et al. 2015). This was found to be true in our study, as 95.2% (278/292) of children in care had one or more competing demands. To determine whether these competing demands were solely responsible for the lower vaccination coverage among children in care, we compared vaccine coverage of children in care to children not in care who had competing demands. For all vaccines and age groups, the risk of being under-vaccinated was higher for children in care than for children not in care who had competing demands. Thus, it appears that competing demands may partially, but not completely, explain the lower vaccine coverage for children in care.
Factors affecting vaccination among children in care
We identified two patterns in vaccine coverage among children in care that suggest influential factors. First, the higher the number of vaccine doses that were required to be fully immunized, the lower the vaccine coverage. For instance, at age 2, coverage for DTaP-IPV-Hib (four doses required) was 54.3%, compared to 81.4% coverage for MMR (one dose required). One possible explanation for this pattern (which has been observed to a lesser extent among children not in care) may be difficulties in foster caregivers attending medical appointments (Schneiderman et al. 2016) or pre-existing incomplete vaccination status when the child entered care. If several appointments are required to complete a multi-dose vaccine series, there may be a greater likelihood of an appointment not being attended. The literature suggests that lack of awareness of required vaccinations and current contact information by both social services and health service providers means that vaccination may be seen as someone else’s responsibility, thus affecting interagency co-ordination (Hunter et al. 2008). In addition to circumstances while in care, children may experience medical neglect prior to entering care (Canadian Paediatric Society 2008) and require several catch-up vaccines upon entry into care.
Second, consistent with previous studies (Hill et al. 2003; Croft 2009), we found that vaccine coverage of children in care decreased with age. For example, coverage for the age-appropriate doses of MMR was 81.4% at age 2 and 65.3% at age 7. The literature suggests that a lack of coordination and information sharing between health and social services, as well as discontinuity of care, may lead to gaps in service provision for children in care. This may result in subpar delivery of immunization services and/or poor record-keeping of vaccinations administered, leading to lower vaccine coverage that becomes exaggerated over time (Hunter et al. 2008; Croft 2009; Rodrigues 2004).
An additional issue is that anecdotal reports from clinicians in our study setting noted that the lower coverage we observed in children in care may partially be explained by difficulties in obtaining informed consent to proceed with vaccination for children in care. Depending on the type of child welfare intervention, the foster carer may not have authority to provide informed consent and the biological parent or the court-appointed guardian may need to be contacted before proceeding with vaccination.
Strengths and limitations
Our study used vaccination data from a provincial administrative dataset that accounts for virtually all childhood vaccines given within the province. However, despite using data from an annual birth cohort, the relatively small numbers in each group prohibited us from controlling for potentially confounding factors in our analysis. The necessity to exclude First Nations children from our study (due to lack of data on vaccines administered on reserves) is also a limitation given that Indigenous children comprise 70% of children in care in the province (Government of Alberta Human Services 2017). Since First Nations children are thought to have lower vaccination coverage than their non-First Nations counterparts (Government of Canada 2016), it is likely that vaccine coverage for First Nations children in care is even lower.
Another issue was that the AHCIP/CSR did not indicate duration of time a child was in care, current care status, or type of placement. Therefore, we were unable to differentiate between vaccine coverage before, during, and after the child welfare intervention. This limits the understanding of the causes of low vaccination coverage, as it may be a result of conditions in the family home prior to entering care, a gap in the social service and health provision for these children once they enter care, or both. In addition, the AHCIP/CSR database only identified children in care who were issued a new health care card, who may differ systematically in some way from those who did not. Despite these limitations, this study is the first in Canada to examine vaccination of children in care, and thus serves as an indicator that further work in this field is critical to better understand this phenomenon.
Recommendations
Having identified a signal that current practices are not adequately servicing this at-risk population, we propose that future work focus on (1) improved measurement of vaccine coverage in this population and (2) better understanding of barriers to service delivery. Both of these will require collaboration and data sharing among various departments and levels of government, as well as community partners.
To better identify subgroups most at risk of under-vaccination, data linkage with multiple government ministries (e.g., health, social/children’s services) will be necessary. This would enable comprehensive identification of all children in care, a larger dataset to allow for control of confounding factors, and determination of coverage variability by such factors as time in care and type of care setting. A critical focus would be vaccination coverage for First Nations children in care, as they are a large and distinct segment of this population.
Additional qualitative research could help elucidate the barriers and supports to vaccination for children in care. An examination of existing policies is warranted, but policies alone are not effective in improving vaccine coverage of children in care. As found previously (Ashton-Key and Jorge 2003), providing information to social services on children’s vaccination needs does not in itself improve vaccine coverage. This study and others (Jaudes et al. 2012; Hunter et al. 2008) suggest that improved coverage may be achieved through coordinated and integrated care between social services and health departments. Research is also needed to explore the perspectives of children, guardians, health providers, and child intervention staff regarding perceived barriers and proposed strategies to improve immunization service delivery.
Conclusion
Our study suggests that children who have been in care of the government have lower vaccine coverage compared to children who have never been in care. Using a population-based administrative database, this disparity was found true for DTaP-IPV-Hib, Men-C, and MMR vaccines. Children in care were also more likely to have lower vaccine coverage than children not in care with competing demands. Given the challenges already faced by children in care, it is imperative that these vulnerable children have full access to preventive health services. Further research could help us to understand the causes of low vaccine coverage, effective interventions to improve coverage, and strategies to improve interagency collaboration.
Acknowledgements
With thanks to Bruce McDonald for his support with data linkage. This article arose from the Master of Nursing thesis project of J. Hermann. Thus, an early version of this manuscript is posted on an online university thesis repository: Hermann J. Immunization coverage of Albertan children in care of the government. University of Alberta Education & Research Archive. https://era.library.ualberta.ca/items/5827fcfb-fda3-4eec-82aa-7b382188fde5).
Compliance with ethical standards
Ethics approval was obtained from the University of Alberta Human Research Ethics Board.
Conflict of interest
The authors declare that they have no conflict of interest.
References
- American Academy of Pediatrics. (2015). Council on Foster Care, Adoption, and Kinship Care, Committee on Early Childhood and C on A. Technical report: health care issues for children and adolescents in foster care and kinship care. Pediatrics, 136(4). 10.1542/peds.2015-2656.
- Arora, N., Kaltner, M., & Williams, J. (2014). Health needs of regional Australian children in out-of-home care., 50, 782–786. 10.1111/jpc.12637. [DOI] [PubMed]
- Ashton-Key M, Jorge E. Does providing social services with information and advice on immunisation status of “looked after children” improve uptake? Archives of Disease in Childhood. 2003;88:299–301. doi: 10.1136/adc.88.4.299. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bell CA, Simmonds KA, MacDonald SE. Exploring the heterogeneity among partially vaccinated children in a population-based cohort. Vaccine. 2015;33(36):4572–4578. doi: 10.1016/j.vaccine.2015.07.004. [DOI] [PubMed] [Google Scholar]
- Canadian Child Welfare Research Portal. (n.d.) Frequently Asked Questions (FAQs). http://cwrp.ca/faqs. Accessed September 7, 2016.
- Canadian Paediatric Society Special considerations for the health supervision of children and youth in foster care. Paediatrics & Child Health. 2008;13(2):129–136. doi: 10.1093/pch/13.2.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Croft G. Implementation of health recommendations after initial statutory health assessment. Adoption and Fostering. 2009;33(2):76–81. doi: 10.1177/030857590903300212. [DOI] [Google Scholar]
- Ehreth J. The global value of vaccination. Vaccine. 2003;21(7–8):596–600. doi: 10.1016/S0264-410X(02)00623-0. [DOI] [PubMed] [Google Scholar]
- Ferrara P, Fabrizio GC, Romani L, et al. Immunisation status of children in foster homes: the first Italian data. Minerva Pediatrica. 2016;68(1):36–39. [PubMed] [Google Scholar]
- Government of Alberta. (2016). Population. http://economicdashboard.alberta.ca/Population. Accessed February 18, 2018.
- Government of Alberta. (2017). Routine Immunization Schedule. http://www.health.alberta.ca/health-info/imm-routine-schedule.html. Accessed February 18, 2018.
- Government of Alberta Human Services. (2017). Child Intervention Information and Statistics Summary 2017 / 18 Third Quarter (December) Update. 2017;(December). http://www.humanservices.alberta.ca/documents/child-intervention-info-stats-summary-2017-18-q3.pdf. Accessed February 18, 2018.
- Government of Canada. (2016). Regional communicable disease control report, First Nations and Inuit Health Branch—Alberta Region (internal report).
- Hansen RL, Lakhani Mawjee F, Barton K, Metcalf MB, Joye NR. Comparing the health status of low-income children in and out of foster care. Child Welfare. 2004;83:367–380. [PubMed] [Google Scholar]
- Henderson JW, Arbor SA, Broich SL, Mohr Peterson J, Hutchinson JE. Immunization initiation among infants in the Oregon health plan. Research and Practice. 2006;96(5):800–802. doi: 10.2105/AJPH.2005.068742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hermann JS, Featherstone RM, Russell ML, MacDonald SE. Immunisation coverage of children in the child welfare system: a systematic review protocol. BMJ Open. 2017;7(4):e014625. doi: 10.1136/bmjopen-2016-014625. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill CM, Mather M, Goddard J, Mather M. Cross sectional survey of meningococcal C immunisation in children looked after by local authorities and those living at home. BMJ. 2003;326:364–365. doi: 10.1136/bmj.326.7385.364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hunter D, Mccartney G, Fleming S, Guy F. Improving the health of looked after children in Scotland 1. Using a specialist nursing service to improve the health care of children in residential accommodation. Adoption and Fostering. 2008;32(4):51–57. doi: 10.1177/030857590803200407. [DOI] [Google Scholar]
- IBM Corporation. (2016). IBM SPSS statistics for windows.
- Jaudes PK, Champagne V, Harden A, Masterson J, Bilaver LA. Expanded medical home model works for children in foster care. Child Welfare. 2012;91(1):9–34. [PubMed] [Google Scholar]
- Jones, A., Sinha, V., & Trocmé. N. (2015). Children and youth in out-of-home care in the Canadian provinces. http://cwrp.ca/sites/default/files/publications/en/167e.pdf. Accessed September 7, 2016.
- Kohler M, Emmelin M, Hjern A, Rosvall M. Children in family foster care have greater health risks and less involvement in child health services. Acta Paediatrica. 2015;104:508–513. doi: 10.1111/apa.12901. [DOI] [PubMed] [Google Scholar]
- MacDonald SE, Bell CA, Simmonds KA. Coverage and determinants of uptake for privately funded rotavirus vaccine in a Canadian birth cohort, 2008-2013. The Pediatric Infectious Disease Journal. 2016;35(6):e177–e179. doi: 10.1097/INF.0000000000001125. [DOI] [PubMed] [Google Scholar]
- Miles M, Ryman TK, Dietz V, Zell E, Luman ET. Validity of vaccination cards and parental recall to estimate vaccination coverage: a systematic review of the literature. Vaccine. 2013;31(12):1560–1568. doi: 10.1016/j.vaccine.2012.10.089. [DOI] [PubMed] [Google Scholar]
- Niederhauser VP, Stark M. Narrowing the gap in childhood immunization disparities. Pediatric Nursing. 2005;31(5):387–388. [PubMed] [Google Scholar]
- Potter D, Nasserie T, Tonmyr L. A review of recent analyses of the Canadian incidence study of reported child abuse and neglect (CIS) Health Promotion and Chronic Disease Prevention in Canada. 2015;35(8–9):119–129. doi: 10.24095/hpcdp.35.8/9.02. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rodrigues VC. Health of children looked after by the local authorities. Public Health. 2004;118:370–376. doi: 10.1016/j.puhe.2003.10.009. [DOI] [PubMed] [Google Scholar]
- Schneiderman JU, Villagrana M. Meeting children’s mental and physical health needs in child welfare: the importance of caregivers. Social Work in Health Care. 2010;49(2):91–108. doi: 10.1080/00981380903158037. [DOI] [PubMed] [Google Scholar]
- Schneiderman, J. U., Kennedy, A. K., & Sayegh, C. S. (2016). Qualitative study of foster caregivers’ views on adherence to pediatric appointments. Journal of Pediatric Health Care, 1–7. 10.1016/j.pedhc.2016.05.001. [DOI] [PMC free article] [PubMed]
- Stein REK, Hurlburt MS, Heneghan AM, et al. Health status and type of out-of-home placement: Informal kinship care in an investigated sample. Academic Pediatrics. 2014;14(6):559–564. doi: 10.1016/j.acap.2014.04.002. [DOI] [PMC free article] [PubMed] [Google Scholar]


