Abstract
Objectives
The aims of this study were to examine (1) the concordance between income measured at the individual and area-based level and (2) the impact of using each measure of income on inequality estimates for three health indicators—the prevalence, respectively, of diabetes, smoking, and obesity.
Methods
Data for the health indicators and individual income among adults came from six cycles of the Canadian Community Health Survey (cycles 2003 through 2013). Area-based income was obtained by linking respondents’ residential postal codes to neighbourhood income quintiles derived from the 2006 Canadian census. Relative and absolute inequality between the lowest and highest income quintiles for each measure was assessed using rate ratios and rate differences, respectively.
Results
Concordance between the two income measures was poor in the overall sample (weighted Kappa estimates ranged from 0.19 to 0.21 for all years), and for the subset of participants reporting diabetes, smoking, or obesity. Despite the poor concordance, both individual and area-based income measures identified generally comparable levels of relative and absolute inequality in the rates of diabetes, smoking, and obesity over the 10-year study period.
Conclusion
The results of this study show that individual and area-based income measures categorize Canadians differently according to income quintile, yet both measures reveal striking income-related inequalities in rates of diabetes and smoking, and obesity among women. This suggests that either individual or area-level measures can be used to monitor income-related health inequalities in Canada; however, whenever possible, it is informative to consider both measures since they likely represent distinct social constructs.
Keywords: Income*, Health status disparities, Socio-economic factors, Diabetes mellitus, Obesity, Smoking
Résumé
Objectifs
Examiner (1) la concordance entre le revenu personnel et régional et (2) l’incidence de l’utilisation de chaque indicateur du revenu sur les estimations des inégalités pour trois indicateurs de la santé, soit la prévalence, respectivement, du diabète, du tabagisme et de l’obésité.
Méthode
Les données des indicateurs de la santé et du revenu personnel chez les adultes proviennent de six cycles (2003 à 2013) de l’Enquête sur la santé dans les collectivités canadiennes. Le revenu régional a été obtenu en maillant les codes postaux de résidence des répondants aux quintiles de revenu selon le quartier dérivés du Recensement du Canada de 2006. Les inégalités relatives et absolues entre les quintiles de revenu inférieur et supérieur pour chaque indicateur ont été évaluées par les rapports de taux et les différences de taux, respectivement.
Résultats
La concordance entre les deux indicateurs du revenu est faible dans l’échantillon global (le coefficient kappa pondéré est de 0,19 à 0,21 pour toutes les années) et pour le sous-ensemble de participants ayant fait état de diabète, de tabagisme ou d’obésité. Malgré cette faible concordance, les indicateurs du revenu personnel et régional révèlent des niveaux généralement comparables d’inégalités relatives et absolues dans les taux de diabète, de tabagisme et d’obésité sur les 10 ans de l’étude.
Conclusion
Les résultats de l’étude montrent que les indicateurs du revenu personnel et régional classent les Canadiens différemment selon le quintile de revenu, mais que les deux indicateurs révèlent des inégalités marquantes liées au revenu dans les taux de diabète et de tabagisme, et chez les femmes, dans les taux d’obésité. L’indicateur personnel ou l’indicateur régional peuvent donc l’un et l’autre être utilisés pour surveiller les inégalités de santé liées au revenu au Canada; dans la mesure du possible, il est toutefois instructif de les utiliser tous les deux, car ils représentent probablement des constructions sociales distinctes.
Mots-clés: Revenu*, Disparités de l’état de santé, Facteurs socioéconomiques, Diabète, Obésité, Tabagisme
Introduction
Income is a key component of socio-economic position and low income is among the most consistent predictors of poor health (Braveman et al. 2011; Public Health Agency of Canada 2008; Shavers 2007; Canadian Institute for Health Information 2016). In Canada, reducing health inequalities related to income and other social determinants of health is a core imperative of public health (Public Health Agency of Canada 2008). Measuring inequalities across population subgroups is an important first step in identifying differences that may be considered unfair or unjust and that can be acted on to improve health equity (Public Health Agency of Canada 2008). The monitoring of health inequalities between richer and poorer Canadians at the national, provincial, and municipal levels has generally shown that inequalities have either remained unchanged or widened over time (Canadian Institute for Health Information 2015; Martens et al. 2010; Agence de la Santé et des Services Sociaux de Montreal 2011; Toronto Public Health 2015). Continuing to monitor trends in health inequalities over time is critical to identifying whether progress is being made in improving health equity in Canada.
To measure income-related health inequalities, health indicators are compared across population groups defined by income categories. Income quintiles are frequently used categories of income and have been recommended by organizations like the World Health Organization for equity-oriented monitoring in the context of universal health care coverage (Hosseinpoor et al. 2014). Income quintiles can be defined using individual-level or aggregate area-based income data. While each approach has strengths and limitations, the choice of measure is often guided by data availability, with area-level income measures being the most widely available. In some cases (e.g., for indicators sourced from national surveys like the Canadian Community Health Survey), it is possible to disaggregate health indicators either by individual-level self-reported income, or by assigning census-based area-level income using respondents’ residential postal codes. As such, analysts are commonly faced with the choice of the most appropriate measure.
A number of authors have cautioned against using area-level indicators of socio-economic position as proxies of individual-level indicators due to poor concordance between them, particularly in rural areas and for certain health outcomes (Demissie et al. 2000; Sin et al. 2001; Finkelstein 2004; Hanley and Morgan 2008; Marra et al. 2011). Despite the poor concordance, a number of Canadian and international reports have shown that when individual or area-based income measures are used to assess inequalities in various health-related outcomes, both measures produce comparable estimates of inequality, suggesting that each income measure captures distinct constructs which may exert independent effects on health (Southern et al. 2005; Mustard et al. 1999; Krieger 1992; Locker and Ford 1996). In contrast, other reports have found individual-level income measures to yield stronger inequality estimates than area-level measures (Finkelstein 2004; Walker and Becker 2005; Pampalon et al. 2009; Narla et al. 2015; Geronimus and Bound 1998).
We conducted a study to examine the impact of using individual and area-based income measures on health inequality using large, nationally representative samples of Canadian adults spanning a 10-year period. In this study, individual-level household income was sourced from the Canadian Community Health Survey, and area-level household income was sourced from census data and was assigned through postal code linkage. These two approaches are commonly used in Canadian studies of health inequalities. Our first aim was to assess the level of concordance between individual- and area-level income in the overall sample, and in subsets of participants who reported any of three important public health indicators responsible for a major share of morbidity and premature mortality among Canadians (Institute for Health Metrics and Evaluations 2015): the prevalence of diabetes, smoking, or obesity. Our second aim was to determine whether the two income measures produce similar estimates of income-related inequality in these three health indicators. In order to test the robustness of findings to any temporal changes, all analyses were conducted using data spanning a 10-year period.
Methods
Study population
The Canadian Community Health Survey (CCHS) was used to define the study population and to derive health indicator rates and a measure of individual income. The CCHS is an ongoing population-based cross-sectional survey of community-dwelling Canadians aged 12 years or older, which is representative of over 97% of the target population (Statistics Canada 2016). This analysis was carried out for adult respondents (aged 18+ years) to six consecutive CCHS cycles: 2.1 (2003), 3.1 (2005), 2007/2008, 2009/2010, 2011/2012, and 2013. Because the CCHS does not calculate derived income variables for the territories (Statistics Canada 2011), only residents of provinces were included in our sample. Standard survey weights provided by Statistics Canada were applied in order to maintain population representativeness.
Income measures
Individual-level household income quintiles (i.e., five groups of approximately equal population size) were defined based on the “distribution of household income” derived variable (provincial level) available in the CCHS Master files. This variable represents a relative measure of individuals’ self-reported (before-tax) household income to the household income of all other respondents residing in the same province, adjusted for household and community size (Statistics Canada 2011). We excluded participants with missing or incomplete income information, which ranged from 15% of the full study sample in the 2003 cycle to 12% in 2013.
Area-level household income quintiles from the 2006 Canadian census were assigned using Statistics Canada’s Postal Code Conversion File Plus (PCCF+) Version 5J (Wilkins and Khan 2011) and residential postal codes reported in the CCHS to situate participants within a given dissemination area (DA) and to assign the corresponding area-level income quintile (Wilkins and Khan 2011). DAs are small, relatively stable geographical areas with an average population of 400–700 residents (Statistics Canada 2008). For PCCF+, community-specific income quintiles are derived by ranking DAs according to average household income, from lowest to highest, in each census metropolitan area (CMA), census agglomeration (CA), or provincial residual area not in any CMA or CA, and then dividing into approximate fifths (i.e., about 20% of DAs in each quintile). Average household income is adjusted for household size and sourced from a combination of self-reported census and tax file data (Statistics Canada 2006).
Statistical analysis
We generated a cross-tabulation of individual-level income quintiles by area-level income quintiles and calculated the percent total agreement between these two income measures. The degree of non-random concordance between individual- and area-level income quintiles was calculated using the weighted Kappa statistic, with Cicchetti-Allison linear weights used to take into account the degree of agreement. The weighted Kappa approach gives credit for complete and partial agreement, and is recommended for categorical data that follows an ordinal structure (Landis and Koch 1977).
We further examined income-related health inequalities for three health indicators sourced from self-reported information in the CCHS: diabetes diagnosed by health professional; smoking status (current cigarette use, daily, or occasional); and obesity based on self-reported information on height and weight (body mass index ≥ 30 kg/m2). The national prevalences of diabetes, smoking, and obesity, respectively, were calculated by income quintiles for all survey cycles and reported as percentages with 95% confidence intervals. These prevalence rates were age standardized based on the direct method using the 2011 Canadian census as the standard population.
For each CCHS cycle, income-related inequality between the lowest and highest income quintiles for each health indicator was assessed using the Rate Ratio (RR), a relative measure of inequality, and the Rate Difference (RD), an absolute measure of inequality. The calculation of RRs and RDs did not include adjustment for any other variables. Corresponding 95% confidence intervals were calculated for each measure.
Analyses were conducted for both sexes combined and were also disaggregated by sex. However, in this paper we present sex-specific results only when patterns differed significantly by sex. Estimates were considered to be statistically significantly different from one another when their corresponding 95% confidence intervals did not overlap. All analyses were conducted using SAS (version 9.3), Cary, NC.
Results
As shown in Table 1, the concordance between measures of individual and area-based income in 2013 was poor, as indicated by a weighted Kappa statistic of 0.1999; 95% CI 0.1996–0.2001. Overall, only 27.4% of Canadians were in “perfect agreement” according to individual and area-based income measures, with higher levels of agreement observed in the lowest (Q1) and highest (Q5) income quintiles. Another 35.9% of Canadians were within 1 quintile of the “perfect agreement” diagonal.
Table 1.
Weighted counts and percent total agreement between individual-level and area-level income quintiles among Canadians, 2013 Canadian Community Health Survey
| Area-level income quintiles | Individual-level income quintiles | ||||||
|---|---|---|---|---|---|---|---|
| Q1—lowest income | Q2 | Q3 | Q4 | Q5—highest income | Total n | % of total | |
| Q1-lowest income | 1,508,700 | 1,118,151 | 869,801 | 553,731 | 506,408 | 4,556,790 | |
| 6.3 | 4.7 | 3.6 | 2.3 | 2.1 | 18.9 | ||
| Q2 | 1,055,029 | 1,059,007 | 992,206 | 977,464 | 763,772 | 4,847,479 | |
| 4.4 | 4.4 | 4.1 | 4.1 | 3.2 | 20.1 | ||
| Q3 | 776,129 | 979,807 | 1,049,326 | 1,108,992 | 1,039,245 | 4,953,500 | |
| 3.2 | 4.1 | 4.4 | 4.6 | 4.3 | 20.6 | ||
| Q4 | 582,503 | 853,231 | 972,429 | 1,200,249 | 1,248,881 | 4,857,293 | |
| 2.4 | 3.5 | 4.0 | 5.0 | 5.2 | 20.2 | ||
| Q5-highest income | 455,595 | 551,162 | 914,879 | 1,165,319 | 1,767,419 | 4,854,375 | |
| 1.9 | 2.3 | 3.8 | 4.8 | 7.3 | 20.2 | ||
| Total n | 4,377,956 | 4,561,358 | 4,798,642 | 5,005,755 | 5,325,725 | 24,070,000 | |
| % of total | 18.2 | 19.0 | 19.9 | 20.8 | 22.1 | 100.0 | |
| Kappa (95% CI) | 0.1999 (0.1996–0.2001) | ||||||
Italicized values denote the weighted count and percentage of Canadians who were in “perfect agreement” (i.e. categorized to be in the same income quintile using individual-level and area-level income measures)
Poor agreement between individual and area-based income measures was consistent across all survey cycles (Kappas ranged from 0.1919 in 2005 to 0.2144 in 2007). Agreement was also poor when the sample was restricted to subgroups who reported diabetes, smoking, and obesity (data not shown).
Diabetes
Figure 1 displays the percentage of adults reporting diabetes in survey cycles 2003 through 2013 according to individual-level income quintiles (panel A) and area-level income quintiles (panel B), as well as the corresponding estimates of relative and absolute inequality. Both measures of income showed increases in diabetes prevalence over time within all income quintiles.
Fig. 1.
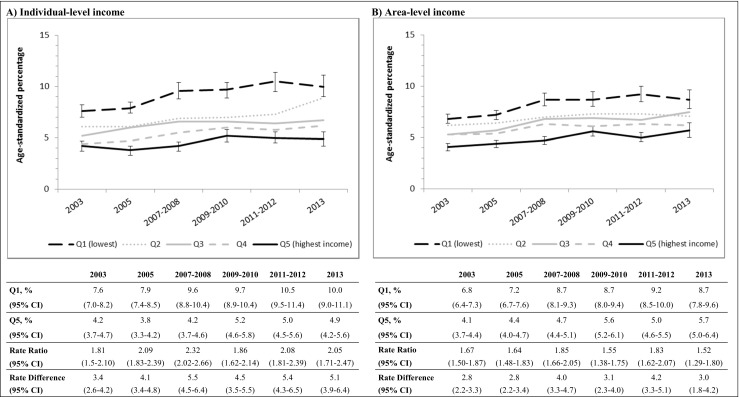
Trends in diabetes prevalence between 2003 and 2013, by individual-level and area-level income quintiles, and corresponding estimates of relative inequality (rate ratio) and absolute inequality (rate difference). Note: all estimates are age standardized
Income-related inequality for diabetes was present on the relative and absolute scales (i.e., according to the RR and RD, respectively) for both income measures and all survey cycles (Fig. 1, panels A and B). For example, in 2013, Canadians in the lowest quintile of individual-level income had a 2-fold higher prevalence of diabetes (panel A: RR = 2.05; 95% CI 1.71–2.47) compared to those in the highest income quintile, and 1.5-times higher prevalence according to area-level income (panel B: RR = 1.52; 95% CI 1.29–1.80). This translated to an absolute difference (i.e., RD) of 5.1 percentage points between the lowest and highest income quintiles measured using individual-level income (panel B: 95% CI 3.9–6.4), and a difference of 3.0 percentage points according to area-level income (panel B: 95% CI 1.8–4.2). There were no significant differences between estimates of relative and absolute inequality based on individual-level vs. area-level income.
Smoking
Temporal trends in the prevalence of daily or occasional smoking were similar for individual-level and area-level income measures and showed a slight decrease in prevalence over time in the highest income quintiles only (Fig. 2, panels A and B). Similar to patterns documented for diabetes prevalence, income-related inequality in smoking was observed on both the relative and absolute scales for all survey cycles and for both income measures, with substantially higher rates of smoking in the lowest vs. the highest income quintiles.
Fig. 2.
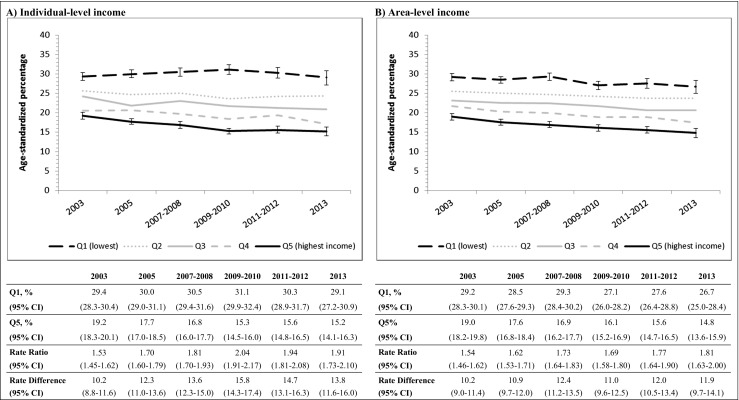
Trends in smoking prevalence between 2003 and 2013, by individual-level and area-level income quintiles, and corresponding estimates of relative inequality (rate ratio) and absolute inequality (rate difference). Note: all estimates are age standardized
Obesity
Patterns in the prevalence of obesity according to income differed by sex and are therefore shown separately for men and women (Figs. 3 and 4). Among men (Fig. 3), the prevalence of obesity within different income quintiles over time was similar for the individual- and area-level income measures (e.g., in 2013, obesity prevalence in Q1 was 18.8% for individual-level income [panel A] and 18.2% for area-level income [panel B]). Measures of relative and absolute income-related inequality showed some differences for individual- and area-level incomes. For example, RRs comparing levels of obesity between men in the lowest vs. highest individual-level income quintiles showed virtually no difference (i.e., RRs were at or near the null value of 1.0) for nearly all study cycles (Fig. 3, panel A). However, analogous RRs based on area-level income quintiles showed significantly higher levels of obesity among men in the lowest-income neighbourhoods for the 2003, 2005, and 2006–2007 cycles (Fig. 3, panel B).
Fig. 3.
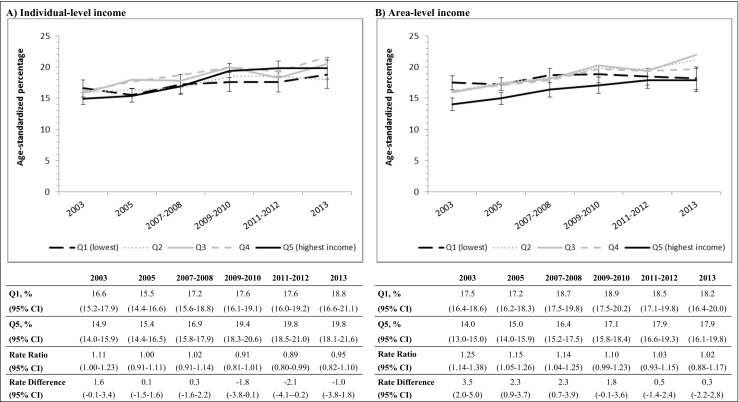
Trends in obesity prevalence among men between 2003 and 2013, by individual-level and area-level income quintiles, and corresponding estimates of relative inequality (rate ratio) and absolute inequality (rate difference). Note: all estimates are age standardized
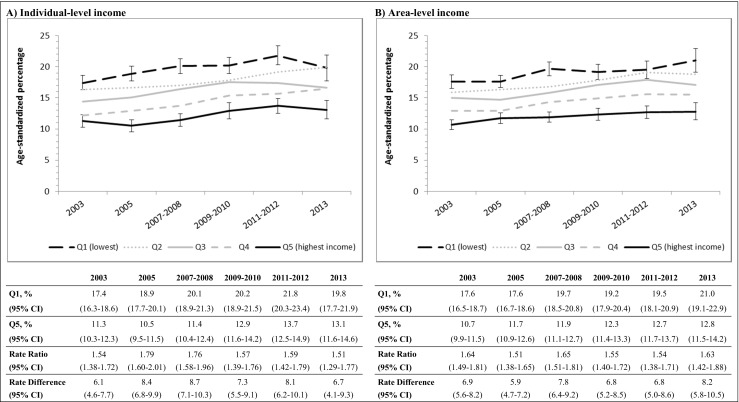
Fig. 4.
Trends in obesity prevalence among women between 2003 and 2013, by individual-level and area-level income quintiles, and corresponding estimates of relative inequality (rate ratio) and absolute inequality (rate difference). Note: all estimates are age standardized
Among women (Fig. 4), there were similar trends in obesity prevalence across quintiles of each income measure. In contrast to men, income-related inequality among women was present for measures of both individual- and area-level income according to relative and absolute measures of inequality, with RR and RD estimates of similar magnitude. For example, in 2013, obesity prevalence among women in Q1 vs. Q5 was 1.5-times higher according to individual-level income (Fig. 4, panel A: RR = 1.51, 95% CI 1.29–1.77) and 1.6-times higher according to area-level income (Fig. 4, panel B: RR = 1.63, 95% CI 1.42–1.88). This translated to 6.7 percentage points higher in terms of absolute inequality when using individual-level income (panel A: 95% CI 4.1–9.3) and 8.2 percentage points higher when using area-level income quintiles (panel B: 95% CI 5.8–10.5).
Discussion
In this study, we examined measures of self-reported individual income and census-based area-level income, which represent the most commonly used approaches for assessing income-related health inequalities in Canada. To investigate the concordance between these two measures of income, we used nationally representative cross-sectional samples of adults residing in ten Canadian provinces between 2003 and 2013. We further examined income-related inequalities in the prevalence of three important public health indicators—diabetes, smoking, and obesity—according to each of the two income measures. Our results showed that the concordance between these measures of individual and area-based income was poor both in the overall sample and in subgroup analyses of the three health indicators. Despite the low levels of agreement, both income measures revealed similar patterns of income-related inequality in the prevalence of diabetes, smoking, and obesity over the 10-year study period. We documented higher rates of each health indicator within both the lower individual-level and lower area-level income quintiles, which persisted over time. An exception to this pattern was obesity prevalence among men where rates showed little variation according to individual-level income, but were slightly higher among men residing in the lowest-income areas (vs. the highest-income areas) for several survey cycles.
Our finding of poor agreement between measures of individual and area-based income is consistent with results of a number of Canadian studies which compared agreement between different socio-economic measures at the individual and area levels (Demissie et al. 2000; Sin et al. 2001; Hanley and Morgan 2008; Marra et al. 2011; Southern et al. 2005; Mustard et al. 1999). This pattern of poor agreement is likely driven by the reality that area-level measures of income represent a range of incomes that exist within households living in a particular area. The heterogeneity of individual incomes in a given area can be substantial in remote and rural regions due to the imprecise nature of postal codes. Rural postal codes cover large geographical areas that are less homogenous in terms of the socio-economic composition of its residents than areas covered by urban postal codes (Pampalon et al. 2010; Wilkins 2004). Additionally, individual income measured from cross-sectional surveys may not accurately represent prior income. For example, low post-retirement incomes reported by older adults may not accurately represent higher incomes prior to retirement and higher levels of accumulated wealth.
Despite the low levels of agreement between income measured at the individual and area levels, we observed generally consistent patterns of income-related inequality over the 10-year study period using each measure of income for prevalence rates of diabetes, smoking, and obesity. Our findings are in line with results based on a number of smaller samples which similarly observed that both individual and area-based measures of socio-economic position were associated with inequality in various health outcomes, including life expectancy, health-related quality of life, and disability (Southern et al. 2005; Walker and Becker 2005; Pampalon et al. 2009). For example, Southern et al. showed that despite poor levels of agreement between measures of individual and area-based income among a cohort of cardiac patients in Alberta, both measures were positively and independently associated with rates of survival and quality of life (Southern et al. 2005). Taken together, such findings suggest that individual and area-based income measures may represent distinct underlying social constructs (Southern et al. 2005; Geronimus and Bound 1998; Diez Roux 2001). Studies that include both individual- and area-level income measures in models predicting variations in rates of health-related outcomes commonly find each measure to exert an independent effect (Narla et al. 2015; Pampalon et al. 2010; Yip et al. 2002; Meijer et al. 2012). Individual-level income may represent access to material goods and services necessary for achieving a healthier lifestyle (e.g., ability to purchase high-quality foods, gym memberships, and to go on regular vacations) (Shavers 2007; Humphries and Van Doorslaer 2000; Braveman et al. 2005). Area-based income, on the other hand, may reflect social characteristics of neighbourhoods (e.g., social norms and contagion processes related to smoking, diet, and levels of physical activity), as well as access to services and resources that promote and support healthy behaviours (e.g., accessibility of food retail outlets and physical activity resources) (Diez Roux 2001; Braveman et al. 2005). Living in a socially marginalized area may in itself represent a source of chronic stress, which has been linked to the development of chronic conditions like diabetes and to the adoption of health-compromising behaviours (Diez Roux 2001; Raphael et al. 2008; Robinette et al. 2016).
Several previous studies which compared the impact of using different measures of income on associations with health outcomes concluded that area-based income measures produce weaker associations compared to individual-level measures (Finkelstein 2004; Walker and Becker 2005; Pampalon et al. 2009; Narla et al. 2015; Geronimus and Bound 1998). In contrast to these reports, our estimates of relative and absolute inequality in the prevalence of three health indicators were generally of similar direction and magnitude for both individual and area-based measures of income, which is similar to findings of a number of Canadian and US-based studies (Southern et al. 2005; Mustard et al. 1999; Krieger 1992; Locker and Ford 1996). In fact, for obesity prevalence among men, our area-based income measure identified greater variations in prevalence compared to its individual-level counterpart. Collectively, these findings suggest that measures of income derived at the individual and area levels can produce comparable results when attempting to identify variations in health outcomes.
As such, our findings demonstrate merit in both measures of income at the individual and small area levels. To gain a more nuanced understanding of social inequalities in health, we recommend that where possible, researchers incorporate both individual- and area-level indicators of income in future analyses. In reality, the choice of measure is often constrained by data availability, and each measure has inherent strengths and limitations. Individual-level income is the most precise source of personal-level income data but is often unavailable within many routinely collected datasets, such as medical and administrative records. When available, self-reported individual-level income commonly involves a large proportion of missing data due to the sensitivity of this information (Shavers 2007). Importantly, missing data are often non-randomly distributed along socio-demographic lines, which can represent an important source of bias, particularly when the proportion of missing values is large (Potter et al. 2005). Additionally, individual-level income fails to take into account other assets that increase wealth, and is more affected by annual fluctuations in earned income (Shavers 2007). Area-based income measures, on the other hand, can indicate the combined effects of wealth and earned income, are less influenced by earning fluctuations, and are usually much more complete (i.e., have fewer missing values). As shown in this and other studies, area-based income is a poor proxy for individual-level income. Despite this, we showed that area-based income identified sizeable variations in several population health outcomes that were consistent with individual-level income measures. This finding highlights the continued usefulness of area-based income indicators (alongside individual-level measures, where possible) for monitoring health inequalities across geographic regions and over time.
Our study has several limitations. Our use of cross-sectional survey data precludes any causal inferences regarding the association of income and diabetes, smoking, and obesity. Without an understanding of the direction of associations and their underlying mechanisms, the ability to inform the design of effective policies or programs to reduce inequalities is limited. Our study is also limited by the use of self-reported individual-level data for health status and income. The accuracy of respondents’ self-reported information could not be verified, and so the possibility of reporting bias cannot be ruled out. Additionally, the capacity to disentangle contextual effects of neighbourhood characteristics from individual-level attributes would require a multilevel study design and other neighbourhood-level variables which were unavailable to us, and represents an important avenue for future study.
Nonetheless, our study also has a number of strengths. To our knowledge, our study is the first to investigate the effects of different income measures on estimates of inequality in the prevalence of diabetes, smoking, and obesity using Canadian data. Another notable strength is our use of large, nationally representative samples of Canadian adults. We also conducted analyses covering a 10-year period to ensure that our findings were robust to changes over time.
Conclusion
Despite poor concordance between income measured at the individual level and at the area level, both measures identified comparable levels of inequality in three important health indicators over the 10-year study period. This suggests that individual- and area-level income measures may represent distinct underlying constructs, each of which impacts health. Collectively, our findings suggest that either individual or area-level measures can be used to monitor income-related inequalities in health; however, wherever possible, future efforts could aim to incorporate both individual- and area-level measures of income, since they represent distinct social constructs.
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Agence de la Santé et des Services Sociaux de Montreal. 2011 report of the director of public health. Social inequalities in health in Montreal: Progress to date. Montreal, QC; 2011.
- Braveman PA, Cubbin C, Egerter S, et al. Socioeconomic status in health research: one size does not fit all. J Am Med Assoc. 2005;294(22):2879–2888. doi: 10.1001/jama.294.22.2879. [DOI] [PubMed] [Google Scholar]
- Braveman P, Egerter S, Williams DR. The social determinants of health: coming of age. Annu Rev Public Health. 2011;32:381–398. doi: 10.1146/annurev-publhealth-031210-101218. [DOI] [PubMed] [Google Scholar]
- Canadian Institute for Health Information . Trends in income-related health inequalities in Canada. Ottawa, ON: CIHI; 2015. [Google Scholar]
- Canadian Institute for Health Information . Pan-Canadian dialogue to advance the measurement of equity in health care. Ottawa, ON: CIHI; 2016. [Google Scholar]
- Demissie K, Hanley JA, Menzies D, Joseph L, Ernst P. Agreement in measuring socio-economic status: area-based versus individual measures. Chronic Dis Can. 2000;21(1):1–7. [PubMed] [Google Scholar]
- Diez Roux AV. Investigating neighborhood and area effects on health. Am J Public Health. 2001;91(11):1783–1789. doi: 10.2105/AJPH.91.11.1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Finkelstein MM. Ecologic proxies for household income: how well do they work for the analysis of health and health care utilization? Canadian Journal of Public Health. 2004;95(2):90–94. doi: 10.1007/BF03405773. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Geronimus AT, Bound J. Use of census-based aggregate variables to proxy for socioeconomic group: evidence from national samples. Am J Epidemiol. 1998;148(5):475–486. doi: 10.1093/oxfordjournals.aje.a009673. [DOI] [PubMed] [Google Scholar]
- Hanley, G. E., & Morgan, S. (2008). On the validity of area-based income measures to proxy household income. BMC Health Serv Res, 8. 10.1186/1472-6963-8-79. [DOI] [PMC free article] [PubMed]
- Hosseinpoor Ahmad Reza, Bergen Nicole, Koller Theadora, Prasad Amit, Schlotheuber Anne, Valentine Nicole, Lynch John, Vega Jeanette. Equity-Oriented Monitoring in the Context of Universal Health Coverage. PLoS Medicine. 2014;11(9):e1001727. doi: 10.1371/journal.pmed.1001727. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Humphries KH, Van Doorslaer E. Income-related health inequality in Canada. Soc Sci Med. 2000;50(5):663–671. doi: 10.1016/S0277-9536(99)00319-6. [DOI] [PubMed] [Google Scholar]
- Institute for Health Metrics and Evaluations. Global burden of disease study (GBD), country profiles: Canada. Available at: http://www.healthdata.org/canada. Updated 2015. Accessed November 30, 2016.
- Krieger N. Overcoming the absence of socioeconomic data in medical records: validation and application of a census-based methodology. Am J Public Health. 1992;82(5):703–710. doi: 10.2105/AJPH.82.5.703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics. 1977;33(1):159–174. doi: 10.2307/2529310. [DOI] [PubMed] [Google Scholar]
- Locker D, Ford J. Using area-based measures of socioeconomic status in dental health services research. J Public Health Dent. 1996;56(2):69–75. doi: 10.1111/j.1752-7325.1996.tb02399.x. [DOI] [PubMed] [Google Scholar]
- Marra, C. A., Lynd, L. D., Harvard, S. S., & Grubisic, M. (2011). Agreement between aggregate and individual-level measures of income and education: a comparison across three patient groups. BMC Health Serv Res, 11. 10.1186/1472-6963-11-69. [DOI] [PMC free article] [PubMed]
- Martens PJ, Brownell M, Au W, et al. Health inequalities in Manitoba: is the socioeconomic gap widening or narrowing over time? Winnipeg, MB: Manitoba Centre for Health Policy; 2010. [Google Scholar]
- Meijer M, Röhl J, Bloomfield K, Grittner U. Do neighborhoods affect individual mortality? A systematic review and meta-analysis of multilevel studies. Soc Sci Med. 2012;74(8):1204–1212. doi: 10.1016/j.socscimed.2011.11.034. [DOI] [PubMed] [Google Scholar]
- Mustard CA, Derksen S, Berthelot J, Wolfson M. Assessing ecologic proxies for household income: a comparison of household and neighbourhood level income measures in the study of population health status. Health and Place. 1999;5(2):157–171. doi: 10.1016/S1353-8292(99)00008-8. [DOI] [PubMed] [Google Scholar]
- Narla NP, Pardo-Crespo MR, Beebe TJ, et al. Concordance between individual vs. area-level socioeconomic measures in an urban setting. J Health Care Poor Underserved. 2015;26(4):1157–1172. doi: 10.1353/hpu.2015.0122. [DOI] [PubMed] [Google Scholar]
- Pampalon R, Hamel D, Gamache P. A comparison of individual and area-based socio-economic data for monitoring social inequalities in health. Health Reports / Statistics Canada. 2009;20(4):85–94. [PubMed] [Google Scholar]
- Pampalon R, Hamel D, Gamache P. Health inequalities in urban and rural Canada: comparing inequalities in survival according to an individual and area-based deprivation index. Health and Place. 2010;16(2):416–420. doi: 10.1016/j.healthplace.2009.11.012. [DOI] [PubMed] [Google Scholar]
- Potter BK, Speechley KN, Gutmanis IA, Campbell MK, Koval JJ, Manuel DA. Comparison of measures of socioeconomic status for adolescents in a Canadian national health survey. Chronic Dis Can. 2005;26(2–3):80–89. [PubMed] [Google Scholar]
- Public Health Agency of Canada. The chief public health officer’s report on the state of public health in Canada: addressing health inequalities. PHAC: Ottawa, ON; 2008.
- Raphael D, Anstice S, Raine K, McGannon KR, Rizvi SK, Yu V. The social determinants of the incidence and management of type 2 diabetes mellitus: are we prepared to rethink our questions and redirect our research activities? Giornale Italiano di Diabetologia e Metabolismo. 2008;28(3):154–161. [Google Scholar]
- Robinette JW, Charles ST, Almeida DM, Gruenewald TL. Neighborhood features and physiological risk: an examination of allostatic load. Health and Place. 2016;41:110–118. doi: 10.1016/j.healthplace.2016.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shavers VL. Measurement of socioeconomic status in health disparities research. J Natl Med Assoc. 2007;99(9):1013–1023. [PMC free article] [PubMed] [Google Scholar]
- Sin DD, Svenson LW, Man SFP. Do area-based markers of poverty accurately measure personal poverty? Canadian Journal of Public Health. 2001;92(3):184–187. doi: 10.1007/BF03404301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Southern DA, McLaren L, Hawe P, Knudtson ML, Ghali WA. Individual-level and neighborhood-level income measures: agreement and association with outcomes in a cardiac disease cohort. Med Care. 2005;43(11):1116–1122. doi: 10.1097/01.mlr.0000182517.57235.6d. [DOI] [PubMed] [Google Scholar]
- Statistica Canada (2006). Income and earnings reference guide, 2006 census. Catalogue no. 97–563-GWE2006003. Available at: http://www12.statcan.gc.ca/census-recensement/2006/ref/rp-guides/income-revenu-eng.cfm. Accessed May 6, 2017.
- Statistics Canada. 2006 Census Dictionary. Available at: www.statcan.gc.ca. Updated 2008. Accessed January 2, 2016.
- Statistics Canada . Annual component, 2009–2010 derived variable (DV) specification. Otattawa, ON: Statistics Canada; 2011. [Google Scholar]
- Statistics Canada. Canadian Community Health Survey—Annual Component (CCHS). Available at: http://www23.statcan.gc.ca/imdb/p2SV.pl?Function=getSurvey&SDDS=3226. Updated (2016). Accessed November 30, 2016.
- Toronto Public Health . The unequal city 2015: income and health inequalities in Toronto. Toronto, ON: Toronto Public Health; 2015. [Google Scholar]
- Walker AE, Becker NG. Health inequalities across socio-economic groups: comparing geographic-area-based and individual-based indicators. Public Health. 2005;119(12):1097–1104. doi: 10.1016/j.puhe.2005.02.008. [DOI] [PubMed] [Google Scholar]
- Wilkins R. Neighbourhood income quintiles derived from Canadian postal codes are apt to be misclassified in rural but not urban areas (working paper). Statistics Canada. Available at: https://www.researchgate.net/publication/301488517_Neighbourhood_income_quintiles_derived_from_Canadian_postal_codes_are_apt_to_be_misclassified_in_rural_but_not_urban_areas. Updated (2004). Accessed November 30, 2016.
- Wilkins R, Khan S. PCCF+ version 5J* user’s guide. Ottawa, ON: Statistics Canada; 2011. [Google Scholar]
- Yip AM, Kephart G, Veugelers PJ. Individual and neighbourhood determinants of health care utilization: implications for health policy and resource allocation. Canadian Journal of Public Health. 2002;93(4):303–307. doi: 10.1007/BF03405022. [DOI] [PMC free article] [PubMed] [Google Scholar]


