Abstract
The costs of obesity have been well studied, with estimates in Canada reaching $7.1 billion annually. These estimates fuel public and professional discourse about obesity as an “epidemic” with substantial economic and public health consequences. However, cost estimates for obesity thus far have neglected to consider a critical variable: weight bias (i.e., negative bias towards individuals based on their body weight). In this commentary, we propose that some costs currently attributed to obesity may be partly or fully attributable to weight bias. Taking a burden of illness approach, we show that data derived from a purposeful literature search, provided as proof of concept, support the notion that weight bias may be an important variable to consider when calculating obesity-related costs. We propose that future research on costs of obesity should consider weight bias, with goals of achieving more accurate cost attributions and identifying appropriate leverage points for interventions to improve well-being of the population.
Electronic supplementary material
The online version of this article (10.17269/s41997-018-0146-2) contains supplementary material, which is available to authorized users.
Keywords: Obesity, Costs and cost analysis, Body weight, Bias, Discrimination, Cost of illness
Résumé
Les coûts de l’obésité ont été bien étudiés, les estimations ayant atteint 7,1 milliards de dollars annuellement au Canada. Ces estimations alimentent le discours public et professionnel sur l’obésité en tant qu’épidémie ayant des coûts financiers ainsi que des conséquences graves sur la santé publique. Cependant, les estimations des coûts de l’obésité jusqu’à présent ont négligé de prendre en compte une variable déterminante : les préjugés contre les obèses (c’est-à-dire les attitudes et les croyances négatives envers les personnes obèses). Dans ce commentaire, nous soutenons que certains coûts actuellement attribués à l’obésité elle-même peuvent être plutôt attribués partiellement ou entièrement aux préjugés contre les obèses. Suivant l’approche proposée dans le document Le fardeau économique de la maladie au Canada (FEMC), nous avons effectué une recherche documentaire ciblée pour estimer les coûts financiers des préjugés contre les obèses. Servant de preuve de concept, les données obtenues soulignent la nécessité de prendre en compte les préjugés contre les obèses lors du calcul des coûts liés à l’obésité. Nous proposons que dorénavant les futures recherches sur les coûts de l’obésité devraient prendre en compte les préjugés contre les obèses afin d’attribuer les coûts plus précisément et d’identifier des points de levier pour les interventions dirigées à améliorer le bien-être de la population.
Mots-clés: Obésité, Coûts et analyse des coûts, Poids du corps, Biais, Discrimination, Coût de la maladie
Introduction
Obesity has been characterized as a public health “epidemic” with severe health consequences, including increased risks of cardiovascular disease, cancer, diabetes, and other serious ailments (PHAC/CIHI 2011). Accordingly, obesity is considered a formidable public health expense. The costs of obesity in Canada have been estimated at $4.6–$7.1 billion annually (PHAC/CIHI 2011).
The scientific literature on the costs of obesity has neglected the possible contribution of weight bias. Weight bias is defined as negative attitudes and behaviours (i.e., discrimination) against an individual based on their (usually heavier) body weight (Nutter et al. 2016). For example, research has consistently shown that individuals with large bodies are characterized as lazy and lacking willpower (Puhl and Heuer 2009). Weight bias is widespread and pervasive (Puhl and Brownell 2003).
We propose that some costs that have been attributed to obesity in existing burden of illness studies (e.g., delayed health care seeking to avoid biased doctors) may in fact reflect weight bias in addition to or instead of weight alone. This misattribution of costs, to the extent that it occurs, has two main implications: first, existing cost estimates of obesity may be inflated. Second, these estimates could improve intervention efforts focused on preventing or reducing obesity, resulting in missed intervention opportunities to improve practices and settings to include larger individuals. We aim to provide proof of concept that weight bias is an important but neglected consideration in cost of obesity estimates; we specifically identify putative costs that are unique to obesity and unique to weight bias, and that overlap the two.
Why weight bias matters in estimating costs of obesity
Body fat is feared and reviled by many segments of society (Nutter et al. 2016). For example, 25% of 4283 respondents in one study reported that they would rather be unable to have children than be obese. Respondents who weighed less were more likely to endorse such statements (Schwartz et al. 2006). Deeply-rooted, negative societal views on obesity manifest as weight bias and discrimination in various settings, including health care settings (Puhl and Heuer 2009) and the workplace (Carels et al. 2015). Being the target of weight bias has considerable detrimental effects. For example, individuals in large bodies who experience weight bias often also experience depression (Fettichand and Chen 2012) and eating disorders involving binge eating (Durso et al. 2012), which may further perpetuate obesity and its consequences (Vartanian and Novak 2011).
Weight bias may be understood through the lens of the social determinants of health, i.e., social factors such as gender, culture, and socio-economic status (SES) that influence health behaviours such as eating (O’Hara and Gregg 2006). Factors outside of one’s immediate control, including SES inequalities, tend to be associated with higher obesity rates (McLaren 2007). Therefore, in contrast to the prevailing view that individual choices (i.e., calories in/calories out) cause obesity, weight bias is a social justice issue that requires the consideration of complex societal factors that contribute to both obesity and weight bias, as well as their associated costs (Nutter et al. 2016; Fikkan and Rothblum 2012).
Costs of weight bias: proof of concept that weight bias should be included in estimates of costs of obesity
We first examined relevant literature on weight bias and costs of obesity with which we were familiar. Next, we conducted a purposive literature search using three general search engines (Scopus, Google Scholar, and Summon) to identify a list of potential costs. Costs, or burden, associated with an illness can be considered from two perspectives: direct vs. indirect, and individual vs. societal (i.e., costs that consider and extend beyond health care; Byford et al. 2000). We sought to identify any study published after 2000 that quantified a putative cost of obesity or weight bias. Qualitative studies were excluded due to our primary emphasis on cost quantification. Due to the paucity of weight bias literature in Canada, we also examined literature from countries with cultures similar to Canada’s (USA, Australia, UK).
We summarize below results of our purposive literature review on the costs of obesity. We itemize putative costs of weight bias in terms of domain (health care, social, and economic) and setting (health care, interpersonal relationships, education, and employment). Finally, we explore the overlap between the two sets of costs. It is this last step that permits us to identify costs that have been attributed to obesity that may be re-attributed, in full or in part, to weight bias, and thus provide proof of concept.
Approach to identifying costs
Health economists debate the different economic approaches for considering health-related costs. A burden of illness approach involves estimating or quantifying the magnitude or extent of costs associated with a particular problem (Jefferson et al. 2000). In contrast, a cost-effectiveness approach goes a step further and estimates or compares the relative value of different interventions to address the problem (Byford et al. 2000). We have adopted a burden of illness approach, which is appropriate when (1) the burden is not known, and (2) there is a need to raise awareness or provide a basis for advocacy. Both characteristics are true for weight bias in the context of costs of obesity.
Costs attributed to obesity
Aside from direct (e.g., diabetes) and indirect (e.g., reduced quality of life) health costs associated with obesity, obesity costs in published studies fall into two additional categories: (1) workplace (e.g., absenteeism), and (2) general societal costs (e.g., increased medical expenditure). See Appendix 1 (supplementary online material) for details.
Putative costs of weight bias
Through our literature review, we identified seven putative costs of weight bias in three categories: (1) health (i.e., delayed health treatment-seeking behaviours, medical treatment contingent on weight loss, detrimental physical and mental health outcomes), (2) societal (i.e., lower education attainment, interpersonal problems), and (3) workplace (i.e., workplace discrimination). See Appendix 2 (supplementary online materials) for details.
Overlapping costs
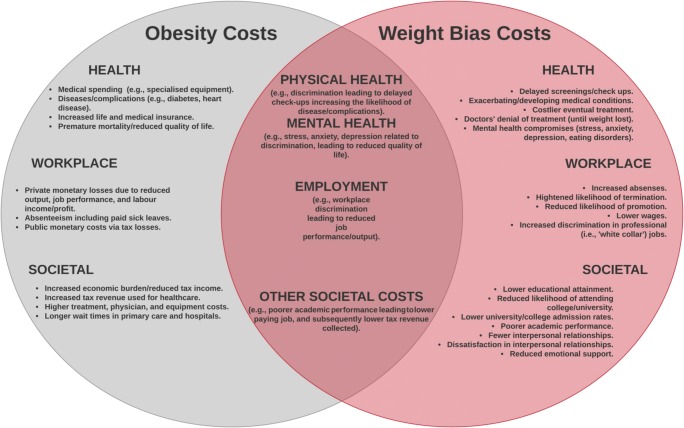
Figure 1 illustrates the costs (direct and indirect) that overlap between obesity and weight bias. Drawing from Appendices 1 and 2 (supplementary online material), four major areas of potential overlap between obesity and weight bias costs were identified: (1) employment (e.g., lack of promotions), (2) physical health (e.g., reduced physical activity), (3) mental health (e.g., depression and binge eating), and (4) other societal costs (e.g., diminished interpersonal relationships). These overlapping areas represent issues relating to weight bias that are currently included in estimates of cost of obesity in Canada (e.g., Moffatt et al. 2011), and support our overall assertion that weight bias is an important, yet missing, component of obesity cost estimates.
Fig. 1.
Obesity and weight bias costs, including areas of overlap
Conclusions and implications
Because of the significant and deeply rooted bias towards obesity in our society that manifests as weight bias and discriminatory behaviour (Nutter et al. 2016; Carels et al. 2015), it is incomplete to estimate costs of obesity without considering weight bias. Accordingly, we explored whether some of the costs of obesity could be partially attributed to weight bias, and in turn whether the costs of weight bias might represent a viable avenue for further scholarly inquiry.
We identified and presented initial support for our idea. Specifically, four areas of costs attributed to obesity overlap with and could be partially attributed to the effects of weight bias. Thus, preliminary evidence suggests that weight bias does contribute to costs previously attributed to obesity. Importantly, consideration of the role of weight bias vis-à-vis costs of obesity was nearly absent in the cost of obesity studies we reviewed, highlighting a gap in the literature. We suggest that this area requires further inquiry.
To the extent that costs of obesity are misattributed due to failure to account for weight bias, there are important implications for public health and policy. First, the support identified for different types of costs associated with weight bias (e.g., education, workplace, health care) can contribute to providing more accurate cost estimates. Second, this work can be used to inform interventions to improve well-being, rather than focusing solely on reducing weight.
Reducing weight bias could indirectly impact the current obesity costs on the public health system by reducing delayed medical treatment and improving well-being (e.g., reducing depression associated with weight bias; Fettichand and Chen 2012; Durso et al. 2012). However, evaluating delayed treatment-seeking due to weight bias is challenging, as multiple physical and mental health issues could contribute to doctor avoidance above and beyond weight bias.
Future directions
Building on our proof of concept, future research could (1) attempt to assign dollar costs to weight bias and (2) mobilize mixed-methods research in a variety of settings (school, work, etc.) to enrich the context of this line of inquiry. Ultimately, this area of research would benefit from a cost-benefit or cost-effectiveness study as a long-term goal, to help inform useful interventions and public policies to reduce weight bias and improve population well-being.
Electronic supplementary material
(DOCX 26 kb)
Acknowledgements
Lindsay McLaren is supported by an Applied Public Health Chair funded by CIHR (Institute of Population and Public Health and Institute of Musculoskeletal Health and Arthritis), the Public Health Agency of Canada, and Alberta Innovates Health Solutions.
References
- Byford S, Torgerson DJ, Raftery J. Economic note: cost of illness studies. BMJ. 2000;320(7245):1335. doi: 10.1136/bmj.320.7245.1335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Carels RA, Rossi J, Borushok J, et al. Changes in weight bias and perceived employability following weight loss and gain. Obes Surg. 2015;25(3):568–570. doi: 10.1007/s11695-014-1522-5. [DOI] [PubMed] [Google Scholar]
- Durso LE, Latner JD, Whiteetal MA. Internalized weight bias in obese patients with binge eating disorder: associations with eating disturbances and psychological functioning. Int J Eat Disord. 2012;45(3):423–427. doi: 10.1002/eat.20933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fettichand KC, Chen EY. Coping with obesity stigma affects depressed mood in African-American and white candidates for bariatric surgery. Obesity. 2012;20(5):1118–1121. doi: 10.1038/oby.2012.12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fikkan JL, Rothblum ED. Is fat a feminist issue? Exploring the gendered nature of weight bias. Sex Roles. 2012;66(9–10):575–592. doi: 10.1007/s11199-011-0022-5. [DOI] [Google Scholar]
- Jefferson T, Demicheli V, Mugford M. Cost-of-illness studies, elementary economic evaluation in health care. 2. London: BMJ Publishing Group; 2000. [Google Scholar]
- McLaren L. Socioeconomic status and obesity. Epidemiol Rev. 2007;29:9–48. doi: 10.1093/epirev/mxm001. [DOI] [PubMed] [Google Scholar]
- Moffatt E, Shack LG, Petz GJ, et al. The cost of obesity and overweight in 2005: a case study of Alberta. Canada Canadian Journal of Public Health. 2011;102(2):144–148. doi: 10.1007/BF03404164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nutter, S., Russell-Mayhew, S., Alberga, A. S., et al. (2016). Positioning of weight bias: moving towards social justice. J Obes, 1–10. [DOI] [PMC free article] [PubMed]
- O’Hara L, Gregg J. The war on obesity: a social determinant of health. Health Promotion Journal of Australia. 2006;17(3):260–263. doi: 10.1071/HE06260. [DOI] [PubMed] [Google Scholar]
- PHAC/CIHI. (2011). Obesity in Canada: a joint report from the Public Health Agency of Canada (PHAC) and the Canadian Institute for Health Information (CIHI). PHAC/CIHI.. https://www.canada.ca/content/dam/phac-aspc/migration/phac-aspc/hp-ps/hl-mvs/oic-oac/assets/pdf/oic-oac-eng.pdf. Accessed 3 September 2018.
- Puhl RM, Brownell KD. Psychosocial origins of obesity stigma: toward changing a powerful and pervasive bias. Obes Rev. 2003;4(4):213–227. doi: 10.1046/j.1467-789X.2003.00122.x. [DOI] [PubMed] [Google Scholar]
- Puhl RM, Heuer CA. The stigma of obesity: a review and update. Obesity. 2009;17(5):941–964. doi: 10.1038/oby.2008.636. [DOI] [PubMed] [Google Scholar]
- Schwartz MB, Vartanian LR, Nosek BA, Brownell KD. The influence of one’s own body weight on implicit and explicit anti-fat bias. Obesity. 2006;14(3):440–447. doi: 10.1038/oby.2006.58. [DOI] [PubMed] [Google Scholar]
- Vartanian LR, Novak SA. Internalized societal attitudes moderate the impact of weight stigma on avoidance of exercise. Obesity. 2011;19(4):757–762. doi: 10.1038/oby.2010.234. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 26 kb)