Abstract
Objectives
The objectives of this study were to: (1) report tuberculosis (TB) program performance for northern First Nations in the province of Manitoba; (2) present methods for TB program performance measurement using routinely collected surveillance data; and (3) advance dialogue on performance measurement of Canadian TB programs.
Methods
Data on a retrospective cohort of people diagnosed with TB in Manitoba between January 1, 2008 and December 31, 2010, and their contacts, were extracted from the Manitoba TB Registry. Performance measures based on US-CDC were analyzed. Adjusted probability ratios (aPR) and 95% confidence intervals (CIs) were reported with comparisons between on-/off-reserve First Nations, adjusted for age, sex, and treatment history.
Results
A cohort of n = 149 people diagnosed with TB and n = 3560 contacts were identified. Comparisons off-/on-reserve: Treatment completion (aPR = 1.03; 95% CI 0.995–1.07); early detection (aPR = 0.87; 95% CI 0.57–1.33); HIV testing and reporting (aPR = 0.42; 95% CI 0.21–0.83); pediatric TB (age < 15 years) (aPR = 1.20; 95% CI 0.47–3.06); retreatment for TB (aPR = 0.93; 95% CI 0.89–0.97); contact elicitation (aPR = 0.94; 95% CI 0.84–1.05); contact assessment (aPR = 0.69; 95% CI 0.50–0.94). Pediatric (ages < 15 years) TB incidence in northern Manitoba was 37.1 per 100,000/year.
Conclusion
TB program performance varies depending on residence in a reserve or non-reserve community. Action is urgently needed to address TB program performance in terms of contact investigation and HIV testing/reporting for First Nations off-reserve and to address high rates of pediatric TB in northern Manitoba. First Nations collaboration and models of care should be considered both on- and off-reserve to improve TB program performance.
Keywords: Tuberculosis; Manitoba; Health care quality, access, and evaluation; Indigenous population; First Nations; Performance measurement
Résumé
Objectifs
Les objectifs de cette étude étaient les suivants : 1) rendre compte des résultats du programme de lutte contre la tuberculose chez les Premières Nations du Nord du Manitoba; 2) présenter les méthodes de mesure des résultats du programme à l’aide des données de surveillance systématiquement recueillies; et 3) faire progresser le dialogue sur la mesure des résultats des programmes canadiens de lutte contre la tuberculose.
Méthode
Nous avons extrait du registre de la tuberculose du Manitoba une cohorte rétrospective des personnes qui avaient un diagnostic de tuberculose entre le 1er janvier 2008 et le 31 décembre 2010 et de leurs contacts. Les indicateurs de résultats, fondés sur ceux des CDC américains, ont été analysés. Les rapports de cotes ajustés (RCa) et les intervalles de confiance (IC) de 95 % sont présentés, avec des comparaisons entre les membres des Premières Nations dans les réserves et hors des réserves, et les données ajustées selon l’âge, le sexe et les antécédents thérapeutiques.
Résultats
N = 149 personnes ayant un diagnostic de tuberculose et n = 3560 contacts. Comparaisons dans les réserves/hors des réserves : achèvement du traitement (RCa = 1,03; IC de 95 % : 0,995–1,07); dépistage précoce (RCa = 0,87; IC de 95 % : 0,57–1,33); dépistage et déclaration du VIH (RCa = 0,42; IC de 95 % : 0,21–0,83); tuberculose infantile (< 15 ans) (RCa = 1,20; IC de 95 % : 0,47–3,06); retraitement contre la tuberculose (RCa = 0,93; IC de 95 % : 0,89–0,97); recherche des contacts (RCa = 0,94; IC de 95 % : 0,84–1,05); évaluation des contacts (RCa = 0,69; IC de 95 % : 0,50–0,94). Le taux de tuberculose infantile (< 15 ans) dans le Nord du Manitoba est de 37,1 pour 100,000/année.
Conclusion
Les résultats du programme de lutte contre la tuberculose varient selon que les communautés vivent dans les réserves ou hors des réserves. Des interventions urgentes sont nécessaires pour améliorer les résultats du programme en ce qui concerne la recherche des contacts et le dépistage et la déclaration du VIH chez les membres des Premières Nations hors des réserves, et pour réduire les taux élevés de tuberculose infantile dans le Nord du Manitoba. La collaboration et les modèles de soins des Premières Nations dans les réserves et hors des réserves devraient être envisagés pour améliorer les résultats du programme.
Mots-clés: Tuberculose; Manitoba; Qualité, accès, évaluation des soins de santé; Population indigène; Premières Nations; Mesure des résultats
Introduction
In Canada, tuberculosis (TB) remains a major public health concern with significantly higher incidence in Indigenous communities (Alvarez et al. 2014). In 2016, 333 (19%) of 1737 TB cases in Canada occurred among Canadian-born Indigenous peoples: 209 (63%) among First Nations, 114 (34%) among Inuit, and 10 (3%) among Métis, with incidence rates of 23.8, 170.1, and 2.1 per 100,000, respectively, compared to 0.6 per 100,000 for non-Indigenous Canadian-born (Vachon et al. 2018). Geographic variability has been observed among Canada’s Indigenous peoples. Among the Inuit, TB incidence is highest in the North (237.1 cases per 100,000 in 2014) and also varies across Inuit Nunangat (Inuit Homeland), which is the Inuit peoples’ traditional territories and which crosses provincial and territorial borders in northern Canada (Public Health Agency of Canada 2016). Among First Nations, TB incidence varies between those living on-reserve (34.1 per 100,000) and off-reserve (14.5 per 100,000) (Long et al. 2013). Some First Nations communities experience endemic TB, others experience periodic outbreaks, and some have very low TB incidence (Long et al. 2013). Determinants of disease in these communities include, but are not limited to, such factors as overcrowded and poorly ventilated housing, food insecurity, income disparity, access to and quality of health care services, racism and stigma, and prevalent comorbidities, including diabetes and renal failure (Alvarez et al. 2014).
Among the Canadian provinces, Manitoba has had the highest rate of TB for over a decade, ranging from 9.3 to 14.5 per 100,000 from 2004 to 2014 (Public Health Agency of Canada 2016). Within Manitoba, the City of Winnipeg and the Northern Health Region host approximately 90% of cases annually. Mobility between the two regions creates epidemiological links, as demonstrated by social network and molecular strain analysis (Al-Azem 2006; Blackwood et al. 2003). The incidence rates in specific Winnipeg neighbourhoods and among northern Manitoba First Nations were high in the 1990s, and the pattern has not changed significantly up to the present day (Blackwood et al. 2003; Olson 1999; Whitlock et al. 2012).
In the late 1980s and early 1990s, the United States (US) experienced a resurgence of TB which it was ill equipped to handle due to decades of budget cuts to TB programs. In 2000, the Institute of Medicine published Ending Neglect, which examined TB prevention and control in the US and made recommendations to strengthen TB control across the US. The CDC Response to Ending Neglect: The Elimination of Tuberculosis in the United States in 2002 provided a plan for TB elimination in the US (Centers for Disease Control and Prevention 2002). One component of this plan was ongoing and systematic evaluation of TB programs. While already in use within the US Centers for Disease Control and Prevention (US-CDC), the US-CDC published national TB program performance targets in 2009 based on a consultative process involving state and federal health authorities that began in 2006 (Hughes et al. 2010). Cooperative funding agreements with the US-CDC require that states report on performance of their TB programs and produce plans for improving performance towards national TB program objectives (Hughes et al. 2010). Accountability and transparency have been incorporated in their use by some states, such as Alaska, which publishes yearly performance data (State of Alaska 2017).
Canada has not implemented TB performance measures or targets nationally, and provincial TB programs are not required to report on performance or develop plans to improve performance as in the United States. Few studies have been published examining TB program performance in Canada (Basham et al. 2018; Jensen et al. 2012; Long et al. 2015). In 2012, the Pan-Canadian Public Health Network published an appendix of potential performance targets but these were never adopted nationally (Pan-Canadian Public Health Network 2012). In 2016, the federal government published a performance measurement framework for First Nations on-reserve TB programs (First Nations and Inuit Health Branch 2016). This framework, however, is merely a guidance document. It does not apply to TB activities for Indigenous individuals living off-reserve, nor for the general Canadian population, and it does not recommend public reporting of performance. Finally, a recent (2018) Chief Public Health Officer spotlight report on TB elimination in Canada, The Time is Now, did not mention any role for performance measurement in TB elimination, despite current guidance on TB program performance measurement as a valuable tool in the fight against TB (Heffernan and Long 2018; Tam 2018).
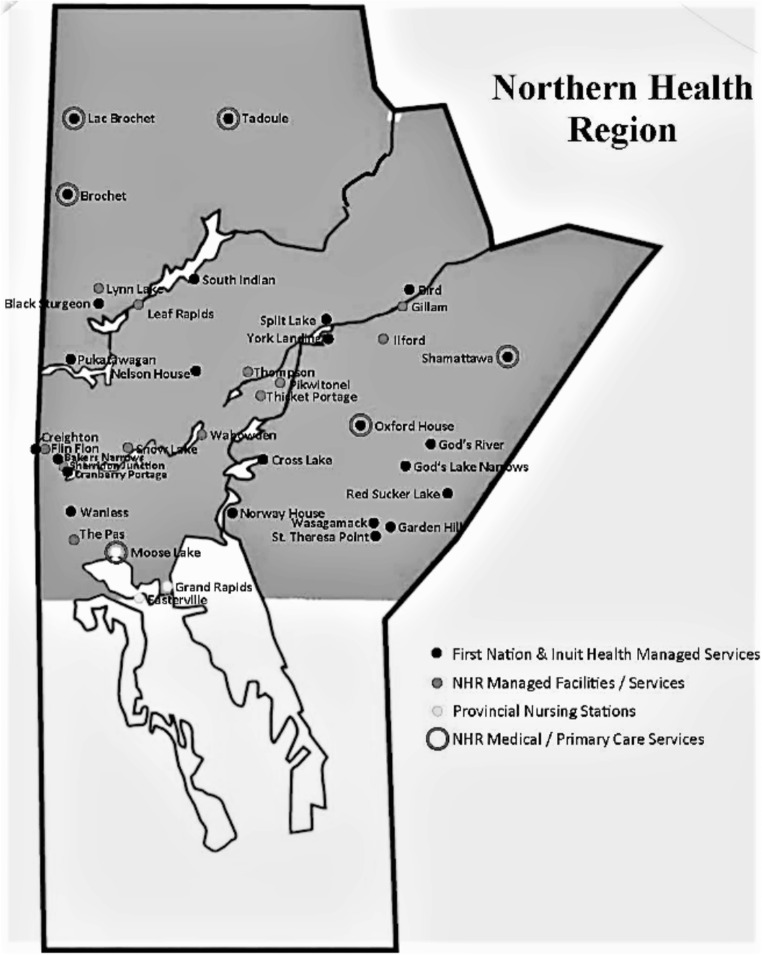
To address the ongoing elevated TB incidence within northern Manitoba First Nations, the Manitoba Keewatinowi Okimakanak (MKO), a Cree, Dené, and Oji-Cree political organization representing 27 First Nations communities in northern Manitoba, passed a resolution in 2010 calling for performance measurement of TB services within the MKO region. In response to this resolution, performance measurement analysis of the full Manitoba TB program was conducted based on performance measures developed by the US-CDC. This paper reports on our findings for the Northern Health Region of Manitoba (Fig. 1), which coincides with the MKO region, and discusses the role for performance measurement in Canadian TB programs.
Fig. 1.
Map of Northern Health Region, Manitoba, Canada, depicting the study area and indicating First Nations and non-First Nations communities as well as federal and provincial health service providers
Methods
Study population and data source
We identified a retrospective cohort of people diagnosed with TB in Manitoba between January 1, 2008 and December 31, 2010, and reported to the Manitoba TB Registry, as well as individual contacts identified through contact investigation. The TB Registry is the database of all TB cases in the province. Reporting of TB cases is mandatory, and the provincial program for TB diagnosis and care is centralized. Previous research with this database suggests that the reporting and capture of all provincial cases is likely complete, although individual data points within each file may be missing because of incomplete reporting (Lix et al. 2018). The total follow-up period of the cohort was until December 31, 2012 to determine treatment completion, HIV testing/reporting, and contact investigation outcomes.
Performance measures
US-CDC National TB Program Objectives and Performance Targets for 2015 were adapted to the Manitoba TB situation and data available for the study (Table 1). Performance measures were defined at the individual level using binary variables (0: definition not met; 1: definition met) based on fields in the Manitoba TB Registry. The sum of individuals meeting each performance measure’s definition was divided by the number of cohort members included in the denominator for that performance measure. For example, the proportion of infectious pulmonary TB cases diagnosed early (Early Detection) used the number of pulmonary TB cases among the cohort as the denominator.
Table 1.
Performance measurement framework: cross-referenced with selected sources
| Performance measures used in the current study | Canadian Tuberculosis Standards, 6th edition | United States TB Program Performance Targets (2015) | Guidance for TB Prevention and Control Programs in Canada – Appendix IVa |
|---|---|---|---|
| Treatment completion/cure | 90% | 93% | ≥ 90% |
| Early detection of pulmonary cases (smear-negative at diagnosis) | No | No | No |
| Retreatment cases | < 3% of cases treated within 2 years of treatment ending | < 3% cases/year | ≤ 3% of cases treated within 2 years of treatment ending |
| HIV testing/reporting | 90% | 88.7% | > 90% |
| Pediatric cases | No | < 0.4 cases/100,000 for children 0–5 years | No |
| Contacts elicited (PTB cases only) | Implied; no specific target set | 100% of AFB smear-positive | 100% of infectious cases |
| Contacts assessed (contacts of PTB cases only) | Implied; no specific target set | 93% of AFB smear-positive | 100% of infectious cases |
aThe Pan-Canadian Public Health Network “Guidance for TB Prevention and Control Programs in Canada” performance measurements are used in Health Canada’s Monitoring and Performance Framework for Tuberculosis Programs for First Nations On-Reserve
AFB, acid fast bacilli; HIV, human immunodeficiency virus; PTB, pulmonary tuberculosis
The analysis reported here was one part of a multipart analysis that established performance baselines for Manitoba as a whole and specific geographic (Winnipeg Health Region and Northern Health Region) and population origin groups (First Nations, non-Canadian-born, and Canadian-born non-First Nations), with an aim to inform numerical targets for these measures.
The incidence rate of pediatric TB was calculated using Census 2011 age-specific population count of children age < 15 years in the Northern Health Region of Manitoba as the denominator. Because 3 years of cases were used, the denominator was multiplied by three, to provide an average annual incidence rate estimate for January 1, 2008 to December 31, 2010.
Early detection was defined as culture-positive pulmonary cases that were smear-negative at diagnosis. During the study period (2008–2012), the standard of diagnosis and care in Manitoba was derived from the 6th edition of the Canadian Tuberculosis Standards, which advised at least three sputum collections from suspected pulmonary cases, and also provided guidelines regarding use of induced sputum and bronchoscopy (Public Health Agency of Canada 2007).
Statistical analysis
Log-binomial and robust Poisson regression were used to determine the probability of achieving a performance measure’s definition (0: no [reference]; 1: yes). The probability ratio (PR) of achieving a performance measure was calculated using PROC GENMOD to implement a generalized linear model (GLM) with generalized estimating equations (GEE). The GEE extension was used to account for clustering of the contact investigation outcomes within cases, based on case characteristics rather than contact characteristics, but was employed for analyses involving only cases as well for consistency. The PR has the same calculation and interpretation as a risk ratio (RR), although the concept of risk was not appropriate in the context of this study so we opted for “probability” instead (Zou and Donner 2011). The models estimate the probability of the performance measurement definition being met for First Nations people living on-reserve compared to off-reserve. The PR for off-/on-reserve was adjusted (aPR) for age group (0–18 years, 19–35 years, 36–55 years, 56 years+), sex (male, female), and treatment history (1st time treated, 2+ times treated). However, the model of pediatric TB did not adjust for age or treatment history and the model for retreatment did not adjust for treatment history (the response variable). All data analyses were conducted in SAS 9.2 (SAS Institute Inc., Cary, NC). An alpha = 0.05 level was set for determining statistical significance with 95% confidence intervals (95% CI) representing estimate precision.
Ethics
Study ethical approval was provided by the University of Manitoba Health Research Ethics Board (HREB), the Assembly of Manitoba Chiefs – Health Information and Research Governance Committee (HIRGC), and the Manitoba Health Information and Privacy Committee (HIPC). A data access request was made to Manitoba Health Public Health Surveillance Unit, and after completion of a Researcher Agreement, data were transferred from Manitoba Health to the University of Manitoba Centre for Global Public Health (CGPH) Applied Public Health Evaluation and Research Unit where analyses were conducted. Study results were reviewed by the HIRGC and HIPC, prior to submission for publication, to ensure privacy and respect for First Nations participants.
Results
Cohort characteristics
A total of 149 First Nations people diagnosed with TB (31 clinical; 118 microbiological) in the Northern Health Region of Manitoba, between January 1, 2008 and December 31, 2010, were included in the analysis (Table 2). Males formed a majority of cases. Half of First Nations people diagnosed with TB in northern Manitoba were age ≤ 35 years. Ninety-seven cases were pulmonary. Of the total number of cases, 118 were culture positive with the remaining being clinically diagnosed. Among the pulmonary cases with positive culture, 72 were smear-negative, with the remaining being smear-positive. In total, there were 3560 contacts identified in northern Manitoba.
Table 2.
TB patient characteristics: northern Manitoba First Nations, 2008–2010
| Characteristic | n (%) |
|---|---|
| Sex (Male) | 87 (58.4) |
| Age 0–18 years | 33 (22.1) |
| Age 19–35 years | 43 (28.9) |
| Age 36–55 years | 58 (38.9) |
| Age 56 years+ | 15 (10.1) |
| Microbiological diagnosis (C+) | 118 (79.2) |
| Pulmonary disease (C+) | 97 (65.1) |
C+, culture positive
Performance measures
Table 3 presents results for seven performance measures analyzed for northern Manitoba First Nations. In terms of treatment for active TB, a slightly (6%) higher probability of completion was observed for First Nations living off-reserve in the crude analysis model (PR = 1.06; 95% CI 1.02–1.10, p < 0.05). In the adjusted model, this finding became non-significant (aPR = 1.03; 95% CI 0.995–1.07).
Table 3.
TB program performance measures among northern Manitoba First Nations, 2008–2012: comparisons off-reserve vs. on-reserve
| Performance measure | n (%)a | Crude PR (95% CI)b | Adjusted PR (95% CI)b |
|---|---|---|---|
| Treatment completion | 145 (94.8) | 1.06 (1.02, 1.10)* | 1.03 (0.995,1.07) |
| Early detection | 72 (71.3) | 0.87 (0.58, 1.32) | 0.87 (0.57, 1.33) |
| HIV testing and reporting | 95 (62.1) | 0.44 (0.22, 0.87)* | 0.42 (0.21, 0.83)* |
| Pediatric TB (age < 15 years) | 24 (15.7) | 1.29 (0.49, 3.39) | 1.20 (0.47, 3.06) |
| Retreatment for TB | 9 (5.9) | 0.94 (0.90, 0.97)* | 0.93 (0.89, 0.97)* |
| Contact elicitation (among cases of infectious pulmonary TB) | 100 (99.0) | 0.93 (0.80, 1.07) | 0.94 (0.84, 1.05) |
| Contact assessment (among contacts of infectious pulmonary TB) | 3163 (88.9) | 0.69 (0.51, 0.95)* | 0.69 (0.50, 0.94)* |
CI, confidence interval, PR, probability ratio
aNorthern Health Region values overall
bProbability ratio (PR) off-reserve (numerator) vs. on-reserve (denominator). Analyses of off- vs. on-reserve performance measures for treatment completion, early detection, HIV testing/reporting, contact elicitation, and contact assessment are each adjusted for age, sex, and retreatment status while analysis of pediatric TB was adjusted for sex, and analysis of retreatment was adjusted for age and sex. Values of PR < 1.0 mean lower probability of the performance measure definition being met off-reserve compared to on-reserve. Values with PR ~ 1.0 show no difference between on- and off-reserve performance
*p < 0.05, **p < 0.01, ***p < 0.001
There was no significant difference in the probability of pulmonary TB cases being smear-negative at diagnosis (early detection indicator) between First Nations living off-reserve and on-reserve (aPR = 0.87; 95% CI 0.57–1.33).
Sixty-three percent of First Nations people diagnosed with TB in northern Manitoba had an HIV test result recorded in the Manitoba TB Registry. First Nations people diagnosed with TB who lived off-reserve had a 58% lower probability of having an HIV test result recorded in the Manitoba TB Registry (95% CI 17–79%).
Out of a total population (First Nations and non-First Nations) of 70,090 people living in the Northern Health Region of Manitoba, 30.7% of whom were age < 15 years (Statistics Canada 2013), there were 24 First Nations pediatric TB cases in a 3-year period, yielding an estimated annual incidence rate of 37.1 per 100,000 population. There was a statistically significant higher probability that a First Nations female diagnosed with TB was age < 15 years compared to a First Nations male diagnosed with TB in the unadjusted model (PR = 2.34; 95% CI 1.09–5.00, p < 0.05), which remained significant when adjusted for on-/off-reserve residence (aPR = 2.85; 95% CI 1.09–4.96, p < 0.05).
Retreatment (a history of being treated for TB in Manitoba) was 7% lower among northern First Nations people diagnosed with TB living off-reserve compared to those living on-reserve (95% CI 3–11%, p < 0.05), after adjusting for age and sex. Younger northern First Nations people diagnosed with TB (ages 19–35 years and 36–55 years) were less likely to have a history of TB treatment compared to older cases (ages 36–55 years and 56 years+, respectively).
Among northern Manitoba First Nations, contacts were elicited (named) in the investigation of 77% of people diagnosed with TB (all forms), and 99% of people diagnosed with infectious (culture positive) pulmonary TB. There was no significant difference between those living off-reserve compared to on-reserve in terms of contact elicitation among people diagnosed with either all forms of TB or infectious pulmonary TB. However, contact assessment (medical evaluation for TB or LTBI) was complete for 92% of contacts of people diagnosed with infectious pulmonary TB living on-reserve and only 59% of those living off-reserve. After adjusting for age, sex, and treatment history, the probability of contact assessment being complete for contacts of people diagnosed with infectious pulmonary TB living off-reserve was 31% lower (95% CI 6–50%, p < 0.05) than contacts of people diagnosed with infectious pulmonary TB living on-reserve.
Discussion
In Canada, responsibility for the provision of health care for First Nations people who have status under the Indian Act, and who live in a reserve community, lies with the federal government. The quality of care provided has been a concern since the signing of the treaties that provide the basis for the state’s obligation with regard to the health of First Nations peoples (Bryce 1922). Assessment of the quality of health care requires data not only about inputs, processes, and outputs on the part of the state and care providers, but also outcomes (Smith et al. 2009). First Nations peoples have been asking for performance measures of the health programs provided by the federal government for many years (Assembly of First Nations 2006). It is a matter of transparency and accountability.
Without performance measures, how can First Nations peoples and health care providers know which TB program efforts are effective, which are not, and which require further evaluation? HIV testing in TB patients is a case in point. Canadian TB standards recommend HIV testing in all persons diagnosed with TB. In Manitoba, this is particularly important because the province has higher rates of HIV as well as TB among First Nations peoples, and those with newly diagnosed HIV are more likely to present with advanced disease compared to non-First Nations people (Becker et al. 2013; Manitoba HIV Program 2017; Plitt et al. 2009). The coinciding elevated incidence of TB and HIV in Manitoba’s First Nations peoples points to an urgent public health problem that demands effective action guided by data-based evidence.
It is not clear whether the lack of reported HIV data in the Manitoba provincial TB database reflects a failure to do HIV testing or a failure to report the result. Either way, this points to a serious program failure. Manitoba currently has a policy requiring active counselling and informed consent for HIV testing, while other provinces such as Alberta have an “opt-out” policy in which HIV testing is performed as part of routine TB care unless the patients actively refuse. By 2004, Alberta had achieved virtually complete HIV testing with results reporting for people diagnosed with TB. Their use of an “opt-out” model of HIV testing among people diagnosed with TB has been credited with sharp increase in HIV testing and results reporting (Long et al. 2014). If HIV testing of TB patients is incomplete in Manitoba, the program should look more closely at the processes of testing. Are patients being offered testing? Are there barriers to consent generated by mistrust or fear? Is confidentiality a concern? If testing is done but results are not being reported to the Manitoba TB Registry, then protocols should be established to collect HIV test results for all people diagnosed with TB in Manitoba, for example, through cross-population of Manitoba TB Registry data with data from the Manitoba HIV Program, and vice versa.
The high pediatric TB rate calculated in this study (37.1 per 100,000 people age < 15 years) in northern Manitoba is far beyond the pediatric TB rate in Manitoba as a whole (5.0 per 100,000 people age 5–14 years in 2014) and nationally (0.8 per 100,000 people aged 4–15 years in 2014) (Public Health Agency of Canada 2016). Our pediatric TB rate is qualitatively different than that calculated by Dhawan et al., who found an unadjusted pediatric TB rate among Alberta Registered First Nations of 7.46 per 100,000 person-years among children age < 15 years (Dhawan et al. 2018). Differences in the study populations, Alberta overall in Dhawan et al., and northern Manitoba in our study, explain this difference. Northern Manitoba has a far higher TB incidence rate than Alberta overall or Manitoba overall, and therefore, we should also expect to find a higher pediatric TB rate in northern Manitoba compared to either Alberta overall or Manitoba overall, as we did. Pediatric TB is an indicator of ongoing transmission within Indigenous communities and serves as a call for action (Long et al. 2004).
More females than males were noted among northern Manitoba children with TB who were less than 15 years of age. In a previous study of the entire population of Manitoba, the adjusted probability ratio that a female compared to male person diagnosed with TB was a child age < 15 years was 1.66 (95% CI 0.95–2.88) (Basham et al. 2018). When considering only First Nations, the adjusted PR was 1.88 (95% CI 1.02–3.35). Among northern Manitoba First Nations, the adjusted PR was 2.32 (95% CI 1.09–4.96). This difference may reflect social behaviour, such as more time spent indoors, that may place female children at greater TB risk. A recent study in the neighbouring province of Saskatchewan found that a significantly lower proportion of female than male children living on-reserve met the Canadian Society for Exercise and Physiology Physical Activity Standard (Lemstra et al. 2013). It is unclear whether these female children, compared to males, spend a greater proportion of their time indoors, and it is also unclear whether increased indoor time in these communities may be a risk factor for TB exposure and disease. Regardless, the data suggest that the Manitoba TB program should renew its focus on the prompt diagnosis and care of adults with active TB who may live or spend time in households or other spaces with children, along with rapid identification and treatment of infected children.
Among the pulmonary cases in which respiratory cultures were sent and were positive, the proportion of smear-positive cases was relatively low (28.7%). This may indicate early diagnosis of infectious TB, but we are unable to rule out the possibility that the results reflect suboptimal microbiologic investigation. The Manitoba TB Registry only records positive cultures so we do not know how many microbiologic specimens were sent from patients. It is apparent that the analysis of performance measures requires both specimen denominator as well as numerator data.
Contact assessment was complete for a high proportion of contacts on-reserve but was significantly lower off-reserve, indicating challenges for provincial and/or regional public health services’ ability to locate and successfully engage with people in contact with those diagnosed with infectious pulmonary TB. On-reserve, single health centres (Nursing Stations) run all health programs, and smaller communities make it more likely that contacts can be located. Off-reserve, there are more providers, housing options, and potentially greater mobility, possibly making it more difficult to locate contacts (Eisenbeis et al. 2016). Regardless of why, the result of lower contact assessment is that people who are latently infected with TB are not identified or treated until disease activation, which further propagates TB, putting vulnerable people (e.g., children) at risk. Increased resources are needed to locate, evaluate, and provide preventive treatment to people in contact with people diagnosed with infectious pulmonary TB living off-reserve in northern Manitoba. This will help reduce incidence and protect vulnerable people from contact with infectious TB. The large number of contacts per case among First Nations in Manitoba, particularly in northern Manitoba, makes this a resource-intensive task but one that also has large potential for improved public health. In addition to TB prevention, increased public health resources for TB contact tracing and treatment may lead to greater engagement of people at risk for TB with the health system and may lead to identifying and meeting previously unmet health needs among the First Nations population.
Collaborative, respectful, relationships with communities affected by TB are essential to the success of TB programs, particularly among Indigenous peoples, given the history of TB in Canada (Alvarez et al. 2014). Performance measurement can be a collaborative effort that opens programs to transparency and accountability with key populations. In Manitoba, this project was initiated by resolution of MKO First Nations and facilitated involvement of First Nations in program performance measurement and analysis.
Several limitations related to TB registry data are noted. First, we were not able to analyze all measures initially planned, particularly around LTBI diagnosis and treatment, due to lack of data. Second, we did not have definitions for some variables provided, including resides_on_reserve, a variable indicating “yes” or “no”. We took this to mean permanent residence, given that the proportion on-reserve in the study sample mirrored the First Nations population distribution on- and off-reserve. We also note that almost a decade has passed since the cohort enrollment period. However, the incidence of TB in northern Manitoba remains high with no evidence of abatement. First Nations communities continue to look for full partnership in TB programs in their communities, with analysis and publication of data in a manner that provides transparency and accountability (Lix et al. 2018). This paper can be viewed as a case study of TB program performance using TB surveillance data with First Nations oversight.
Conclusion
Notable differences were found in TB program performance among First Nations people living on- and off-reserve in northern Manitoba, demonstrating poorer program performance off-reserve in the areas of contact assessment and HIV testing/reporting. No significant difference in performance on-/off-reserve was found in treatment completion for all forms of TB, early detection of infectious pulmonary TB, contact elicitation, or probability of cases being age < 15 years. A slightly lower retreatment rate was found off-reserve compared to on-reserve.
Performance measurement is a valuable tool for understanding the strengths and weaknesses of TB programs. For First Nations people in high TB burden communities, performance measurement is required in order to understand what is working and what is not working in current TB programs, and to hold those programs to a standard of transparency and accountability that will lead to needed change. The impetus for this study was a resolution on the part of MKO, a First Nations political organization, that was seeking answers to the health crisis of epidemic and endemic TB in their region. The adoption of national TB performance measures and targets, with publication of results (transparency) and clear processes of accountability, will assist the Canadian government and the public they serve, to improve their programs. For Canada, the goal to eliminate TB will require the provision of adequate resources and implementation of trusting partnerships with the Indigenous peoples who experience a high burden of TB morbidity and mortality. This, in turn, cannot be achieved without reliable shared (available) data.
Compliance with ethical standards
Disclaimer
The results and conclusions are those of the authors and no official endorsement by Manitoba Health, or other data providers, is intended or should be inferred.
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- Al-Azem A. A. (2006). Social Network analysis in tuberculosis control among the aboriginal population of Manitoba. [University of Manitoba Ph.D. Dissertation]. Winnipeg: University of Manitoba.
- Alvarez, G. G., Orr, P., Wobeser, W. L., Cook, V., & Long, R. (2014). Tuberculosis prevention and care in First Nations, Inuit and Métis Peoples. In G. G. Alvarez et al. (Eds.), Canadian Tuberculosis Standards, 7th Ed. (pp. 345–362). Ottawa: Public Health Agency of Canada.
- Assembly of First Nations . The Development of a First Nations Health Reporting Framework. Ottawa: Assembly of First Nations, Health & Social Secretariat; 2006. [Google Scholar]
- Basham, C. A., Elias, B., Fanning, A., Cook, C., & Orr, P. H. (2018). A performance measures analysis of a Canadian provincial tuberculosis (TB) program: Manitoba, 2008-2012. International Journal of Tuberculosis and Lung Disease, 22(4), 437–443. [DOI] [PubMed]
- Becker Marissa L, Thompson Laura H, Pindera Carla, Bridger Natalie, Lopez Carmen, Keynan Yoav, Bullard Jared, Van Caseele Paul, Kasper Ken. Feasibility and Success of Hiv Point-of-Care Testing in an Emergency Department in an Urban Canadian Setting. Canadian Journal of Infectious Diseases and Medical Microbiology. 2013;24(1):27–31. doi: 10.1155/2013/164797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Blackwood, K. S., Al-Azem, A. A., Elliott, L. J., Hershfield, E. S., & Kabani, A. M. (2003). Conventional and molecular epidemiology of tuberculosis in Manitoba. BMC Infect Dis, 3, 18-28. [DOI] [PMC free article] [PubMed]
- Bryce PH. The story of a national crime: being a record of the health conditions of the Indians of Canada from 1904 to 1921. 1. Ottawa: James Hope & Sons, Ltd.; 1922. [Google Scholar]
- Centers for Disease Control and Prevention (2002). CDC’s Response to Ending Neglect: The Elimination of Tuberculosis in the United States. Atlanta, Ga: US Department of Health & Human Services.
- Dhawan Vivek, Bown Jennifer, Lau Angela, Langlois-Klassen Deanne, Kunimoto Dennis, Bhargava Ravi, Chui Linda, Collin Simon M., Long Richard. Towards the elimination of paediatric tuberculosis in high-income, immigrant-receiving countries: a 25-year conventional and molecular epidemiological case study. ERJ Open Research. 2018;4(2):00131–2017. doi: 10.1183/23120541.00131-2017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eisenbeis Lisa, Gao Zhiwei, Heffernan Courtney, Yacoub Wadieh, Long Richard, Verma Geetika. Contact investigation outcomes of Canadian-born adults with tuberculosis in Indigenous and non-Indigenous populations in Alberta. Canadian Journal of Public Health. 2016;107(1):e106–e111. doi: 10.17269/cjph.107.5255. [DOI] [PMC free article] [PubMed] [Google Scholar]
- First Nations and Inuit Health Branch. (2016). Health Canada’s Monitoring and Performance Framework for Tuberculosis Programs for First Nations On-Reserve. Ottawa: Government of Canada. (http://www.healthycanadians.gc.ca/publications/science-research-sciences-recherches/first-nations-tuberculosis-monitoring-framework-cadre-surveillance-tuberculose-premieres-nations/index-eng.php). Accessed 24 Feb 2018.
- Heffernan Courtney, Long Richard. Would program performance indicators and a nationally coordinated response accelerate the elimination of tuberculosis in Canada? Canadian Journal of Public Health. 2018;110(1):31–35. doi: 10.17269/s41997-018-0106-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hughes, S., Young, K., Jereb, J., Pratt, R., Navin, T., Ijaz, K., Khan, A. (2010). Monitoring tuberculosis programs --- National Tuberculosis Indicator Project, United States, 2002-2008. Morb Mortal Wkly Rep, 59(10), 295–298. [PubMed]
- Jensen M., Lau A., Langlois-Klassen D., Boffa J., Manfreda J., Long R. A population-based study of tuberculosis epidemiology and innovative service delivery in Canada. The International Journal of Tuberculosis and Lung Disease. 2012;16(1):43–49. doi: 10.5588/ijtld.11.0374. [DOI] [PubMed] [Google Scholar]
- Lemstra, M., Rogers, M., Thompson, A., & Moraros, J. (2013). Prevalence and correlates of physical activity within on-reserve first nations youth. J Phys Act Health, 10(3), 430–436. [DOI] [PubMed]
- Lix, L.M., Plourde, P. J., Larcombe, L., Kinew, K.A., Basham, C. A., Derksen, S., Srisakuldee, W., Schultz, J., McCulloch, S. (2018). Exploring Tuberculosis Treatment, Management, and Prevention in Manitoba’s Administrative Health Data. Winnipeg: Manitoba Centre for Health Policy.
- Long Richard, Hoeppner Vernon, Orr Pamela, Ainslie Martha, King Malcolm, Abonyi Sylvia, Mayan Maria, Kunimoto Dennis, Langlois-Klassen Deanne, Heffernan Courtney, Lau Angela, Menzies Dick. Marked Disparity in the Epidemiology of Tuberculosis among Aboriginal Peoples on the Canadian Prairies: the Challenges and Opportunities. Canadian Respiratory Journal. 2013;20(4):223–230. doi: 10.1155/2013/429496. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long, R., Whittaker, D., Russell, K., Kunimoto, D., & Reid, R. (2004). Pediatric tuberculosis in Alberta First Nations. Canadian Journal of Public Health, 95(4), 249–255. [DOI] [PMC free article] [PubMed]
- Long Richard, Niruban Selvanayagam, Heffernan Courtney, Cooper Ryan, Fisher Dina, Ahmed Rabia, Egedahl Mary Lou, Fur Rhonda. A 10-Year Population Based Study of ‘Opt-Out’ HIV Testing of Tuberculosis Patients in Alberta, Canada: National Implications. PLoS ONE. 2014;9(6):e98993. doi: 10.1371/journal.pone.0098993. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Long, R., Heffernan, C., Gao, Z., Egedahl, M. L., & Talbot, J. (2015). Do ‘Virtual’ and ‘Outpatient’ public health tuberculosis clinics perform equally well? A program-wide evaluation in Alberta, Canada. PLoS ONE, 10(12), e0144784. [DOI] [PMC free article] [PubMed]
- Manitoba HIV Program. (2017). Manitoba HIV Program Update 2016. Winnipeg: Nine Circles Community Health Centre.
- Olson, L. (1999). A Comparative Study on the Incidence of Tuberculosis Among Status Indians and Other Selected Groups in Manitoba, Canada. [University of Manitoba M.Sc. Thesis]. Winnipeg: University of Manitoba.
- Pan-Canadian Public Health Network. (2012). Guidance for tuberculosis prevention and control programs in Canada (1st ed.). Ottawa: Government of Canada (http://www.phn-rsp.ca/pubs/gtbpcp-oppctbc/pdf/Guidance-for-Tuberculosis-Prevention-eng.pdf). Accessed 10 June 2018.
- Plitt Sabrina S., Mihalicz Dana, Singh Ameeta E., Jayaraman Gayatri, Houston Stan, Lee Bonita E. Time to Testing and Accessing Care among a Population of Newly Diagnosed Patients with HIV with a High Proportion of Canadian Aboriginals, 1998–2003. AIDS Patient Care and STDs. 2009;23(2):93–99. doi: 10.1089/apc.2007.0238. [DOI] [PubMed] [Google Scholar]
- Public Health Agency of Canada. (2007). Canadian tuberculosis standards. In R. Long & E. Ellis (Eds.), Canadian Tuberculosis Standards (6th ed.). Ottawa: Public Health Agency of Canada and Canadian Lung Association (http://www.lung.ca/cts-sct/pdf/tbstand07_e.pdf). Accessed 8 Aug 2018.
- Public Health Agency of Canada. (2016). Tuberculosis in Canada 2014 – Pre-Release. Ottawa: Minister of Public Works and Government Services Canada.
- Smith PC, Mossialos C, Papanicolas I, Leatherman S. Introduction. In: Smith PC, Mossialos C, Papanicolas I, Leatherman S, editors. Performance Measurement in health system improvement: experience, challenges, prospects. New York: Cambridge University Press; 2009. pp. 3–24. [Google Scholar]
- State of Alaska. (2017). Tuberculosis in Alaska: 2016 Annual Report. Anchorage: Department of Health and Social Services, Division of Public Health, Section of Epidemiology.
- Statistics Canada. (2013). Northern regional health authority (2013 health region), Manitoba and Manitoba (Table). Health profile. Catalogue No. 82-228-XWE. (December 2013):1–23. Ottawa: Government of Canada.
- Tam, T. (2018). The Time is Now: Chief Public Health Officer Spotlight on Eliminating Tuberculosis in Canada. Ottawa: Government of Canada.
- Vachon J, Gallant V, Siu W. Tuberculosis in Canada, 2016. Canadian Communicable Disease Report. 2018;44(6):75–81. doi: 10.14745/ccdr.v44i34a01. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whitlock, M., Shaw, S., Nowicki, D., Mahmud, S. (2012). The epidemiology of active tuberculosis disease in the Winnipeg health region. Winnipeg: Winnipeg Regional Health Authority (http://www.wrha.mb.ca/community/publichealth/files/services/surveillance/TuberculosisReport.pdf). Accessed 30 Oct 2012.
- Zou GY, Donner Allan. Extension of the modified Poisson regression model to prospective studies with correlated binary data. Statistical Methods in Medical Research. 2011;22(6):661–670. doi: 10.1177/0962280211427759. [DOI] [PubMed] [Google Scholar]