Abstract
Objectives
We investigated associations between dieting and other health-compromising behaviours among adolescent girls, both cross-sectionally and longitudinally. The behaviours considered included smoking, binge drinking, and breakfast-skipping, and clusters of these.
Methods
Data for 3386 adolescent Ontario girls were drawn from COMPASS, a school-based study, which collects self-reported measures of weight, dieting, and other health-related factors. Multilevel logistic regression models were used to investigate relationships between dieting at baseline and smoking, binge drinking, and breakfast-skipping, as well as clusters of these behaviours at baseline and 2 years later.
Results
Baseline dieters were at an elevated risk of smoking and binge drinking (RR = 1.8 and 1.5, respectively) by follow-up compared to non-dieters. Further, dieting was associated with combinations of these behaviours, with the highest risks for smoking/breakfast-skipping (RR = 1.64) and smoking/binge drinking (RR = 1.55). Over one in two (58%) girls reported dieting at baseline and four in five baseline dieters reported dieting 2 years later. Seven in ten girls were dieting at one or both time points. Baseline dieters were more likely to engage in a greater number of risky behaviours, regardless of what the actual behaviours were.
Conclusion
Dieting is longitudinally associated with engagement in other risky behaviours among adolescent girls. These findings suggest that dieting may be an early risk factor for engagement in other risky behaviours and highlight the need for comprehensive prevention strategies to target shared underlying drivers. In addition, attention is needed to the potential for well-meaning weight-related initiatives to promote dieting.
Keywords: Adolescence, Dieting, Binge drinking, Smoking, Breakfast, Longitudinal
Résumé
Objectifs
Nous avons étudié les associations transversales et longitudinales entre le fait de suivre un régime et d’autres comportements compromettants pour la santé chez les adolescentes. Les comportements étudiés étaient le tabagisme, l’hyperalcoolisation rapide et la pratique de sauter le petit-déjeuner, ainsi que les grappes de ces comportements.
Méthode
Les données de 3386 adolescentes ontariennes ont été extraites de COMPASS, une étude en milieu scolaire qui recense les mesures autodéclarées du poids, du suivi d’un régime et d’autres facteurs liés à la santé. Des modèles de régression logistique multiniveaux ont servi à explorer les relations entre le suivi d’un régime au départ et le tabagisme, l’hyperalcoolisation rapide, la pratique de sauter le petit-déjeuner, et les grappes de ces comportements au départ et deux ans plus tard.
Résultats
Les filles qui suivaient un régime au départ couraient un risque plus élevé de tabagisme et d’hyperalcoolisation rapide (RT = 1,8 et 1,5, respectivement) deux ans plus tard que les filles qui ne suivaient pas de régime. De plus, le suivi d’un régime était associé aux combinaisons de ces comportements, les risques les plus élevés étant le tabagisme/la pratique de sauter le petit-déjeuner (RT = 1,64) et le tabagisme/l’hyperalcoolisation rapide (RT = 1,55). Plus d’une fille sur deux (58%) a déclaré suivre un régime au départ, et quatre filles sur cinq qui suivaient un régime au départ en suivaient toujours un deux ans plus tard. Sept filles sur dix suivaient un régime au départ, au suivi ou les deux. Les filles qui suivaient un régime au départ étaient susceptibles de se livrer à un plus grand nombre de comportements à risque, tous comportements confondus.
Conclusion
Suivre un régime est longitudinalement associé aux comportements à risque chez les adolescentes. Ces constatations indiquent que suivre un régime peut être un facteur de risque précoce de se livrer à d’autres comportements à risque, d’où la nécessité d’avoir des stratégies de prévention globales pour cibler les vecteurs communs sous-jacents. En outre, il faut envisager la possibilité que des initiatives bien intentionnées liées au poids incitent à se mettre au régime.
Mots-clés: Adolescence, régime alimentaire, hyperalcoolisation rapide, tabagisme, petit-déjeuner, étude longitudinale
Introduction
Though Canadian data are limited, existing evidence suggests that dieting to lose weight is an extremely common practice among adolescent girls (Woodruff et al. 2008; Findlay 2004). The propensity to engage in dieting is driven by multiple factors, including individual traits and societal standards related to body weight and shape, and is a highly gendered behaviour that differs significantly between adolescent boys and girls (Loth et al. 2014).
In a 2004 position statement, reaffirmed in 2016, the Canadian Pediatric Society discouraged dieting among this age group due to associated physical and psychological risks (Findlay 2004). These concerns persist, with cross-sectional and longitudinal research suggesting associations between dieting to lose weight and poor diet quality, poor academic performance, and increased risk of developing overweight and obesity and eating disorders (Woodruff et al. 2008; Findlay 2004; Golden et al. 2016). More recently, because of the associated risks, the American Academy of Pediatrics similarly discouraged dieting in adolescence (Golden et al. 2016).
The co-occurrence of risky behaviours (Woodruff et al. 2008; Seo and Jiang 2009; Pirkle and Richter 2006; Larson et al. 2009; Crow et al. 2006) is emphasized as a target for comprehensive chronic disease prevention (Leatherdale 2015), highlighting the importance of investigating potential co-occurrences among dieting and other risky behaviours. For example, cross-sectional and longitudinal research carried out in the USA suggests links between dieting and other health-compromising behaviours, including smoking, binge drinking, and breakfast-skipping among adolescent girls (Seo and Jiang 2009; Pirkle and Richter 2006; Larson et al. 2009). In the context of the dieting literature, these three behaviours have been shown to independently follow dieting, but there is a gap in our understanding of how dieting may precede their co-occurrence. Our cross-sectional research among a large sample of Canadian girls demonstrated complex, and often contradictory, associations between weight management, weight perception, and each of these health-compromising behaviours; for example, girls who were smokers were more likely to try to gain weight, but more often perceived themselves as overweight compared to non-smokers (Raffoul et al, forthcoming). However, there has been a paucity of longitudinal research to explore whether dieting to lose weight predicts engagement in other risky behaviours, particularly in the last two decades and among Canadian youth. Such contextual evidence is needed to better inform early and effective comprehensive prevention efforts targeted at these behaviours; nearly 88% of first cigarette use occurs before the age of 18 (US Department of Health and Human Services 2012), adolescent binge drinking is a risk factor for the development of alcohol disorders in later life (DeWit et al. 2000), and breakfast-skipping may be an indicator of poor diet quality among adolescents (Storey et al. 2009). Adolescence is thus a key leverage point for preventing a potential cascade of health-compromising behaviours.
To address these gaps, we investigated associations between dieting and smoking, binge drinking, and breakfast-skipping, as well as clusters of these behaviours, both cross-sectionally and longitudinally, among girls who were in grades 9 and 10 at baseline.
Methods
Analyses were conducted using data from the COMPASS System, a prospective cohort study initiated in 2012 (Leatherdale et al. 2014). COMPASS includes a convenience sample of secondary schools in Ontario and Alberta, in which all students are eligible to participate, and employs active-information passive-consent procedures, whereby students are enrolled in the study unless actively withdrawn by a parent (Leatherdale et al. 2014). School- and student-level measures related to obesity/overweight status, dietary intake, binge drinking, tobacco, and associated health behaviours have been collected annually through in-class surveys, in Ontario since 2012 and in Alberta since 2013. Further details on COMPASS can be found elsewhere (Leatherdale et al. 2014). The study received ethics approval from the University of Waterloo Office of Research Ethics (#17264).
Data from years 1 (baseline, 2012) and 3 (follow-up, 2014) were utilized for these analyses, thus capturing girls attending schools in Ontario only. This study utilized only data from girls because of the noted gender differences in dieting among adolescents (Findlay 2004; Loth et al. 2014). Further, though similar research in boys is also of importance, measures to capture common behaviours, such as efforts to increase muscle mass, were not available. At baseline, 6232 girls in grades 9 and 10 completed the COMPASS survey. The sample analyzed here consisted of 3386 of these girls (55%) who had complete observations for the primary predictor (dieting) at baseline and outcome variables (risky behaviours) at follow-up.
Measures
Dieting to lose weight
Dieting to lose weight was based on responses to the question, “Which of the following are you trying to do about your weight?” Students could indicate whether they were trying to lose, gain, maintain weight, or not trying to do anything about their weight. As a proxy to determine dieting, this variable was dichotomized into trying to lose weight or not, and is subsequently referred to as dieting.
Health-compromising behaviours
Measures of health-compromising behaviours are consistent with previous research (Leatherdale 2015) and those used in national surveys (Leatherdale and Rynard 2013). Girls were categorized as current smokers if they indicated ever smoking 100 cigarettes and smoked one or more cigarettes in the past 30 days (Leatherdale and Rynard 2013). Binge drinking was defined as consuming five or more drinks of alcohol on one occasion. Girls were categorized as current binge drinkers if they engaged in this behaviour once a month or more (Leatherdale and Rynard 2013). Respondents were categorized as breakfast-skippers if they reported not eating breakfast two or more days a week. To account for the possibility that students who participate in school-based breakfast programs may consume breakfast more often during the school week than on weekends, preliminary analyses were undertaken and showed no significant difference between weekday and weekend breakfast consumption. Finally, variables were created for combinations of these variables (e.g., smoking and binge drinking) to enable determination of the prevalence of co-occurrence.
Additional measures
Girls self-reported their grade, ethnicity (categorized as white/non-white), and heights and weights (used to determine body mass index (BMI)). BMI was classified according to the World Health Organization’s categories of underweight, normal range, overweight, and obese (World Health Organization 2015) or missing; the latter category was included to account for the sizable proportion of girls (25.1%) who did not report their heights and/or weights.
Statistical analyses
The prevalence of each of the risky behaviours, as well as their co-occurrence, was estimated among dieting and non-dieting girls separately at baseline. Generalized logistic regression models were used to determine if rates of smoking, binge drinking, and breakfast-skipping were significantly different between dieting and non-dieting girls at baseline, controlling for grade, ethnicity, and BMI.
Data from years 1 and 3 were linked for longitudinal analyses, following the same students from baseline to follow-up. A generalized estimating equation (GEE) modeling approach was used to allow for the observation of population-level averages among girls who were dieting or non-dieting, indifferent to how the grouped data were structured or clustered (Liang and Zeger 1986). Each of the longitudinal logistic regression models included dieting, grade, ethnicity, and BMI at baseline as independent variables, and one of smoking, binge drinking, breakfast-skipping, or combinations of these variables at follow-up as the dependent variable. In each of the models, participants who engaged in the outcome behaviour of interest at baseline (e.g., smokers at year 1) were excluded from the respective regression modeling (e.g., analysis examining relationship between dieting at year 1 and smoking at year 3). An additional longitudinal GEE regression, using the Poisson distribution, was conducted using the same covariates to investigate the prospective relationship between dieting and the number of behaviours girls engaged in, irrespective of the specific behaviours themselves.
All analyses were conducted using SAS, version 9.4 (SAS Institute, Cary, NC). An identifier indicating the school each girl attended was included in models to account for school-level clustering, identifying each repeated subject within their respective schools (Leatherdale et al. 2014).
Results
Nearly three quarters of the girls self-identified as white and over half were in grade 9 at baseline (Table 1). The majority reported heights and weights consistent with a ‘healthy weight’ (61.0%), followed by overweight (10.0%), obese (2.6%), and underweight (1.3%). One quarter did not report their heights and/or weights. Overall, 57.5% of girls reported dieting at baseline. Although baseline dieting was not associated with ethnicity or grade, it was significantly associated with BMI.
Table 1.
Bivariate associations between health-compromising behaviours, additional measures, and dieting status at baseline among Ontario adolescent girls in the COMPASS study (n = 3386), stratified by dieting status
| Dieting status | Chi-square (χ2) | ||||
|---|---|---|---|---|---|
| Parameter | N (%)a | Dieter (%)a | Non-dieter (%)a | ||
| Grade | 9 | 1850 (54.6) | 1051 (56.8) | 799 (43.2) | 3.41 |
| 10 | 1536 (45.4) | 897 (58.1) | 639 (41.9) | ||
| Ethnicity | White | 2487 (73.4) | 1426 (57.3) | 1061 (42.7) | 4.81 |
| Non-white | 887 (26.2) | 516 (58.2) | 371 (41.8) | ||
| BMI | Underweight | 45 (1.3) | 8 (17.8) | 37 (82.2) | 245.40** |
| Healthy weight | 2065 (61.0) | 1037 (50.2) | 1028 (49.8) | ||
| Overweight | 336 (10.0) | 296 (88.1) | 40 (11.9) | ||
| Obese | 89 (2.6) | 79 (88.8) | 10 (11.2) | ||
| Not stated | 851 (25.1) | 528 (62.0) | 323 (38.0) | ||
| Smoking | Yes | 116 (3.4) | 79 (68.1) | 37 (31.9) | 5.50* |
| No | 3270 (96.6) | 1869 (57.2) | 1401 (42.8) | ||
| Binge drinking | Yes | 372 (11.0) | 257 (69.1) | 115 (30.9) | 22.90** |
| No | 3008 (88.8) | 1687 (56.1) | 1321 (43.9) | ||
| Breakfast-skipping | Yes | 1731 (51.1) | 1105 (63.8) | 626 (36.2) | 58.71** |
| No | 1607 (47.5) | 815 (50.7) | 792 (49.3) | ||
*p value of < 0.05, **p value of < 0.001
aPercentages include all participants, and may not sum to 100% because of missing data
Associations among dieting and other risky behaviours at baseline
Accounting for the covariates, at baseline, dieting was not significantly associated with smoking, but girls with obesity were nearly three times more likely to be smokers than girls in the healthy BMI range (Table 2). Dieting girls were significantly more likely to engage in binge drinking and were at greater risk of frequently skipping breakfast than girls not dieting.
Table 2.
Adjusted relative risk estimates for health-compromising behaviours in relation to dieting and related measures at baseline among Ontario adolescent girls in the COMPASS study (n = 3386)
| Parameter | Adjusted relative riska (95% CI) | |||
|---|---|---|---|---|
| Smoking | Binge drinking | Breakfast-skipping | ||
| Dieting | No | 1.00 | 1.00 | 1.00 |
| Yes | 1.48 (0.97, 2.25) | 1.87 (1.55, 2.28)** | 1.61 (1.36, 1.89)** | |
| Grade | 9 | 1.00 | 1.00 | 1.00 |
| 10 | 1.02 (0.99, 1.05) | 1.04 (0.95, 1.13) | 0.97 (0.93, 1.02) | |
| Ethnicity | White | 1.00 | 1.00 | 1.00 |
| Non-white | 0.76 (0.44, 1.30) | 0.58 (0.41, 0.81)* | 1.04 (0.90, 1.22) | |
| BMI | Healthy weight | 1.00 | 1.00 | 1.00 |
| Underweight | 2.69 (0.83, 8.73) | 0.19 (0.03, 1.36) | 0.86 (0.49, 1.52) | |
| Overweight | 1.50 (0.92, 2.44) | 0.70 (0.47, 1.05) | 1.28 (1.00, 1.65) | |
| Obese | 2.98 (1.31, 6.81)* | 0.59 (0.29, 1.19) | 1.50 (1.02, 2.21)* | |
| Not stated | 1.21 (0.72, 8.73) | 0.65 (0.48, 0.88)* | 1.59 (1.30, 1.94)** | |
*p value of < 0.05, **p value of < 0.001
aRelative risk controlling for all other parameters in the table
At baseline, dieting was significantly associated with each cluster of behaviours (Fig. 1). Among girls who engaged in multiple behaviours, the proportion who reported dieting was consistently larger than the proportion who did not (e.g., the majority of girls who were current smokers and binge drinkers were also dieting). The co-occurrence of binge drinking and breakfast-skipping was most strongly associated with dieting (χ2 = 29.26, p < 0.001); three quarters of girls who engaged in this behaviour pattern were dieting.
Fig. 1.
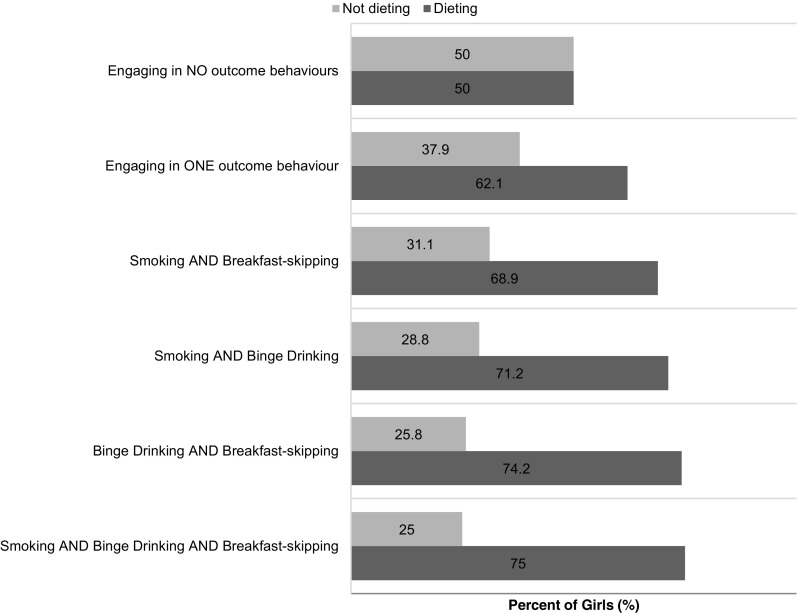
Prevalence of dieting among Ontario adolescent girls in the COMPASS study who were engaging in no, single, or multiple co-occurring health-compromising behaviours at baseline (n = 3386)
Dieting at baseline and other risky behaviours at follow-up
One in five (20.5%) girls who reported dieting at year 1 were not dieting at year 3, whereas three in ten (29.1%) who reported not dieting at year 1 were dieting in year 3. Almost three quarters (69.5%) were dieting in either or both year 1 and year 3. The prevalences of smoking, binge drinking, and breakfast-skipping at follow-up were 8.4%, 23.9%, and 53%, respectively. The prevalences of each cluster of behaviours also increased (data not shown).
Dieting at baseline was a significant predictor of each of smoking and binge drinking 2 years later (Table 3). Dieters were 1.76 times (95% CI [1.29 2.40], p < 0.001) more likely to be smokers and 1.48 times (95% CI [1.21 1.80], p < 0.001) more likely to report engaging in binge drinking 2 years later compared to non-dieters, controlling for grade, ethnicity, and BMI. There was no significant relationship between dieting at baseline and breakfast-skipping at follow-up (RR = 1.06, 95% CI [0.85, 1.33], p = 0.59).
Table 3.
Adjusted relative risk estimates for health-compromising behaviours at follow-up in relation to dieting and related measures at baseline among Ontario adolescent girls in the COMPASS study (n = 3386)
| Parameter | Adjusted relative riska (95% CI) | |||
|---|---|---|---|---|
| Smoking, year 3 (n = 3270) | Binge drinking, year 3 (n = 3014) | Breakfast-skipping, year 3 (n = 1655) | ||
| Dieting, year 1 | No | 1.00 | 1.00 | 1.00 |
| Yes | 1.76 (1.29, 2.40)** | 1.48 (1.21, 1.80)** | 1.06 (0.85, 1.33) | |
| Grade, year 1 | 9 | 1.00 | 1.00 | 1.00 |
| 10 | 0.79 (0.61, 1.02) | 1.00 (0.97, 1.03) | 1.03 (1.00, 1.06) | |
| Ethnicity, year 1 | White | 1.00 | 1.00 | 1.00 |
| Non-white | 0.92 (0.66, 1.28) | 0.80 (0.64, 0.99)* | 1.17 (0.92, 1.50) | |
| BMI, year 1 | Healthy weight | 1.00 | 1.00 | 1.00 |
| Underweight | 0.95 (0.23, 4.02) | 0.89 (0.39, 2.02) | 1.37 (0.60, 3.11) | |
| Overweight | 0.76 (0.45, 1.28) | 0.99 (0.73, 1.35) | 0.85 (0.56, 1.27) | |
| Obese | 0.86 (0.34, 2.19) | 0.60 (0.31, 1.15) | 1.01 (0.47, 2.16) | |
| Not stated | 1.14 (0.82, 1.58) | 0.85 (0.68, 1.06) | 1.11 (0.85, 1.45) | |
*p value of < 0.05, **p value of < 0.001
aRelative risk controlling for all other parameters in the table
Dieting at baseline and multiple risky behaviours at follow-up
Baseline dieters were significantly more likely than their non-dieting peers to engage in each combination of smoking, binge drinking, and breakfast-skipping at follow-up, as well as all three in combination (Table 4). Similarly, girls who dieted in year 1 were significantly more likely to engage in a greater number of health-compromising behaviours by year 3 than non-dieters (RR = 1.30, 95% CI 1.23–1.37, p < 0.0001), regardless of what the actual behaviours were. Girls who did not report their height and/or weight were at a slightly elevated risk of engaging in more behaviours than girls who reported weights and heights corresponding with a healthy weight (RR = 1.11, 95% CI [1.05–1.17], p < 0.01).
Table 4.
Adjusted relative risk estimates for co-occurring health-compromising behaviours at follow-up in relation to dieting and related measures at baseline among Ontario adolescent girls in the COMPASS study (n = 3386)
| Parameter | Adjusted relative riska (95% CI) | ||||
|---|---|---|---|---|---|
| Smoking and binge drinking, year 3 (n = 3327) | Smoking and breakfast-skipping, year 3 (n = 3296) | Binge drinking and breakfast-skipping, year 3 (n = 3146) | Smoking and binge drinking and breakfast-skipping, year 3 (n = 3352) | ||
| Dieting, year 1 | No | 1.00 | 1.00 | 1.00 | 1.00 |
| Yes | 1.55 (1.08, 2.23)* | 1.64 (1.19, 2.26)* | 1.47 (1.18, 1.83)** | 1.51 (1.02, 2.21)* | |
| Grade, year 1 | 9 | 1.00 | 1.00 | 1.00 | 1.00 |
| 10 | 0.93 (0.70, 1.23) | 0.76 (0.58, 1.00) | 1.00 (0.96, 1.03) | 0.84 (0.61, 1.14) | |
| Ethnicity, year 1 | White | 1.00 | 1.00 | 1.00 | 1.00 |
| Non-white | 1.00 (0.69, 1.45) | 1.15 (0.83, 1.60) | 1.08 (0.86, 1.36) | 1.30 (0.89, 1.90) | |
| BMI, year 1 | Healthy weight | 1.00 | 1.00 | 1.00 | 1.00 |
| Underweight | 1.96 (0.59, 6.52) | 2.17 (0.84, 5.61) | 1.63 (0.72, 3.70) | 3.21 (1.11, 9.29) | |
| Overweight | 1.13 (0.66, 1.93) | 0.67 (0.40, 1.14) | 1.05 (0.74, 1.47) | 0.88 (0.48, 1.63) | |
| Obese | 0.96 (0.34, 2.73) | 0.65 (0.25, 1.65) | 1.19 (0.69, 2.04) | 1.10 (0.45, 2.70) | |
| Not stated | 1.15 (0.78, 1.69) | 1.10 (0.77, 1.56) | 0.88 (0.69, 1.13) | 1.04 (0.69, 1.59) | |
*p value of < 0.05, **p value of < 0.001
aRelative risk controlling for all other parameters in the table
Discussion
This study provides up-to-date insights into the pervasiveness of dieting among Canadian adolescent girls and the persistence of this behaviour over a 2-year period, as well as associations between dieting at baseline and other risky behaviours. One in two girls were dieting at baseline and 7 in 10 were dieting at either or both time points examined. The higher rates of dieting among girls in this study compared to other studies conducted in Ontario 6 to 7 years prior (Woodruff et al. 2008; Woodruff et al. 2010) are concerning, considering the range of potentially negative health- and academic-related consequences associated with the behaviour among this population (Woodruff et al. 2008; Findlay 2004). Further, dieting at baseline was longitudinally associated with smoking, binge drinking, and co-occurrences of risky behaviours.
This study’s findings replicate previous research on the prospective relationship between dieting and the highlighted behaviours. Research on smoking and dieting, using data collected in the 1990s, found that girls who dieted at baseline were up to 2.1 times more likely to be smokers by 1- and 2-year follow-ups than non-dieters (Austin and Gortmaker 2001). Decreasing prevalence of smoking (Health Canada 2014) may have contributed to the weaker relation between smoking and dieting observed in this study. We also found an increased risk of binge drinking among dieters, consistent with studies among American samples that estimate this risk at between 1.3 and 1.7 times (Field et al. 2002). Dieting at baseline was associated with breakfast-skipping at baseline (at which point, half of girls reported breakfast-skipping) but not at follow-up. It is possible that any temporal relationship between dieting and breakfast-skipping is initiated at an earlier age, for example, in elementary rather than high school. It is also noted that breakfast-skipping may not be conceptualized as a risky behaviour in the same way that smoking and binge drinking are, but evidence does suggest associations between not eating breakfast and poor diet quality among Canadian adolescents (Storey et al. 2009).
Similar to what was observed for smoking and binge drinking individually, the prevalence rates for clusters of all behaviours increased from baseline to follow-up, with the rates of some clusters (smoking/breakfast-skipping) growing more than others (binge drinking/breakfast-skipping), although the relative risks in relation to dieting status at baseline were all fairly similar. The proportion of girls dieting among each cluster of behaviours was consistently greater than the proportion of girls who were not, with the exception of girls engaging in none of the other behaviours, among whom the prevalences of dieting and not dieting were equal. The patterns observed suggest that dieting to lose weight was not clustered with each of these behaviours because it happens to occur so often among this population, but because it occurred more frequently as girls engaged in more health-compromising, risky behaviours. Girls who dieted at baseline were also more likely to engage in a greater number of risky behaviours than non-dieters, regardless of what the actual behaviours were.
The most transparent explanation for why dieting may be associated with and predict the onset of engaging in multiple risky behaviours, particularly smoking and breakfast-skipping, is that girls practice these other behaviours to assist in weight loss. Evidence suggests that girls who perceive smoking as an effective tool for weight loss are more likely to smoke than girls who do not (Seo and Jiang 2009) and that meal-skipping may also be used to encourage weight loss (Larson et al. 2009); however, binge drinking has not been conclusively shown to serve as a tool for weight loss among this population but does cluster with the other behaviours. The theory of dietary restraint, which details that greater restriction of food and beverage intake results in a greater desire and/or need to consume more at a later time (Polivy and Herman 1985), has been applied to weight management and binge drinking; a study using cross-sectional data from COMPASS found that, among girls, breakfast-skipping was associated with both binge drinking and with dieting to lose weight (Patte and Leatherdale 2016). The theorized mechanism by which girls may be restricting intake to serve the purposes of weight loss and binge drinking without worry of calories fits with prior literature on trading-off of health behaviours among youth (Giles and Brennan 2014). In other words, youth may engage in a more healthful behaviour (e.g., exercise) to offset the harmful consequences of another behaviour (e.g., smoking). Further research to encompass a broader range of health-promoting and health-comproming behaviours may build an understanding of such trade-offs and their implications for health over the short and long term.
The propensity to engage in multiple health-compromising behaviours is likely to be mediated by an ever-changing system that encapsulates factors at every level, including family dynamics, the school setting, and governmental policy (Hale and Viner 2012). Given this inherent complexity, researchers are increasingly turning to systems science approaches to better understand clustering of risky behaviours in adolescence and inform comprehensive policy and program interventions to promote health (Johnston et al. 2014). The recognition that all factors in the “system” are interrelated and dependent on one another may aid in further conceptualizing how and why these behaviours cluster, as well as temporal relationships. As such, systems theories can help to better inform strategies to address factors that might be viewed as early warnings of vulnerability to other risky behaviours. Further, systems approaches may be helpful in highlighting faulty paradigms underlying policies and interventions promoting weight loss to achieve health (Penney and Kirk 2015). For example, obesity-related interventions may promote the belief that girls need to lose weight intentionally, possibly reinforcing other behaviours, such as smoking, to obtain the perceived appetite-suppressing effect of tobacco. By better understanding such feedback loops, researchers can better predict and mitigate unintended consequences and policy resistance (Johnston et al. 2014).
In the current study, the proportion of girls who reported dieting was almost equivalent to the proportion reporting heights and weights corresponding with a healthy weight. This finding appears consistent with previous literature demonstrating high prevalence of dieting among girls regardless of self-reported weight status (Crow et al. 2006). The extent of discord between dieting and weight status may be misestimated, however, since many of the girls in the sample may have underreported their weight, as is common among this population (Arbour-Nicitopoulos et al. 2010). Further, one quarter of the sample did not report their height and/or weight; these girls are likely heterogeneous in several facets, but previous research suggests that their non-response may be motivated (Arbour-Nicitopoulos et al. 2010). Rate of dieting among this subset of girls was higher than among girls in the healthy weight category, which may suggest that their non-response was driven by greater perceptions of being affected by overweight.
The findings of this study should be interpreted in light of several additional considerations. Despite the limitation of intermittently missing data (at year 2) among a portion of the girls in the sample, which is common in longitudinal research, GEE models are robust in their modeling of incomplete data (Liang and Zeger 1986) because they do not impose a variance structure on the data and can account for variance outside of pre-determined covariates. Nonetheless, complete data were available for just over half of girls from year 1 who were eligible to participate in year 3. We cannot ascertain the true reasons underlying participant dropout, which may include switching schools, absenteeism, or having a spare class period. Among the girls who were not available to participate in year 3, the data from year 1 suggest that they had higher rates of dieting (60.2%), smoking (10.2%), binge drinking (17.9%), frequent breakfast-skipping (60.0%), and clusters of the behaviours at baseline than the girls included in this study. Thus, our results likely underestimate the associations between dieting and other behaviours.
Data were collected using self-report measures, with misreporting and misclassification possible. Further, the complexity of dieting, including its duration, associated methods, and severity (Findlay 2004), cannot be fully observed using a single item. This measure, then, could only be used as a proxy to identify girls intentionally trying to lose weight. Additionally, although there are other potential covariates that may have been relevant to include in the regression analyses (i.e., negative home environment), our inclusion of grade, race/ethnicity, and BMI as covariates was limited by the availability of data from the surveys. COMPASS does not represent a nationally representative sample, which limits the generalizability of the study’s findings to Canadian girls. However, the rates of engagement in risky behaviours of COMPASS respondents have been shown to be consistent with data from nationally representative surveys (Leatherdale 2015). Other Canadian studies estimate that about 6% of adolescent girls are current smokers (Health Canada 2014), one quarter have engaged in binge drinking in the previous month (Leatherdale and Rynard 2013), and previous research conducted among southern Ontarian girls found that nearly a quarter of girls reported skipping breakfast on a single 24-h recall and nutrition behaviour questionnaire (Woodruff et al. 2008; Woodruff et al. 2010). Finally, the COMPASS student questionnaire asks participants whether they identify as male or female, terms used to identify sex rather than gender, and so this study may unintentionally include participants whose self-identified sex is female but gender identity is not girl/woman.
In sum, dieting is pervasive, persistent, and linked to other risky behaviours among adolescent girls. These findings are concerning given the dominant focus on obesity prevention and the promotion of healthy weights in public health and school-based health promotion initiatives (Institute of Medicine 2012). Obesity prevention policies and programming that do not recognize the complexity of factors involved and that focus narrowly on weight and weight loss may unintentionally promote dieting (Ramos 2015) and, in turn, result in an increased risk of engaging in other health-compromising behaviours. These potential unintentional consequences may occur across BMI categories, presenting risks to those at healthy weights and affected by overweight. In a clinical setting, these findings may heed warning to physicians or practitioners advising weight loss, to anticipate the other behaviours that girls may possibly engage in. This study has provided insights into how dieting co-occurs with and predicts the onset of other risky behaviours, providing a stepping stone for system approaches to further conceptualize how these and other risky behaviours connect with one another and the underlying factors. Framing these issues using a system complexity lens has the potential to identify targets for comprehensive prevention programs and policies to improve overall health among youth.
Acknowledgements
Dr. Jess Haines of the University of Guelph provided valuable feedback on data analysis and interpretation. Amanda Raffoul was funded by a Queen Elizabeth II Graduate Scholarship in Science and Technology. Scott Leatherdale is a Chair in Applied Public Health Research funded by the Public Health Agency of Canada (PHAC) in partnership with Canadian Institutes of Health Research (CIHR). At the time that the analyses were conducted, Sharon Kirkpatrick was funded by a Capacity Development Award from the Canadian Cancer Society Research Institute (702855). The COMPASS study was supported by a bridge grant from the CIHR Institute of Nutrition, Metabolism, and Diabetes (INMD) through the “Obesity—Interventions to Prevent or Treat” priority funding award (OOP-110788; awarded to S. Leatherdale) and an operating grant from the CIHR Institute of Population and Public Health (IPPH) (MOP-114875; awarded to S. Leatherdale).
Compliance with ethical standards
Conflict of interest
The authors declare that they have no conflict of interest.
References
- Arbour-Nicitopoulos KP, Faulkner GE, Leatherdale ST. Learning from non-reported data: interpreting missing body mass index values in young children. Measurement in Physical Education and Exercise Science. 2010;14(4):241–251. doi: 10.1080/1091367X.2010.520243. [DOI] [Google Scholar]
- Austin SB, Gortmaker SL. Dieting and smoking initiation in early adolescent girls and boys: a prospective study. American Journal of Public Health. 2001;91(3):446–450. doi: 10.2105/AJPH.91.3.446. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crow S, Eisenberg ME, Story M, Neumark-Sztainer D. Psychosocial and behavioral correlates of dieting among overweight and non-overweight adolescents. The Journal of Adolescent Health. 2006;38(5):569–574. doi: 10.1016/j.jadohealth.2005.05.019. [DOI] [PubMed] [Google Scholar]
- DeWit DJ, Adlaf EM, Offord DR, Ogborne AC. Age at first alcohol use: a risk factor for the development of alcohol disorders. The American Journal of Psychiatry. 2000;157(5):745–750. doi: 10.1176/appi.ajp.157.5.745. [DOI] [PubMed] [Google Scholar]
- Field AE, Austin SB, Frazier AL, Gillman MW, Camargo CA, Jr, Colditz GA. Smoking, getting drunk, and engaging in bulimic behaviors: in which order are the behaviors adopted? Journal of the American Academy of Child and Adolescent Psychiatry. 2002;41(7):846–853. doi: 10.1097/00004583-200207000-00018. [DOI] [PubMed] [Google Scholar]
- Findlay S. Dieting in adolescence. Paediatrics & Child Health. 2004;9(7):487–491. doi: 10.1093/pch/9.7.487. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Giles EL, Brennan M. Between healthy food, alcohol and physical activity behaviours. BMC Public Health. 2014;14(1):1231. doi: 10.1186/1471-2458-14-1231. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Golden NH, Schneider M, Wood C. Preventing obesity and eating disorders in adolescents. Pediatrics. 2016;138(3):e20161649. doi: 10.1542/peds.2016-1649. [DOI] [PubMed] [Google Scholar]
- Hale DR, Viner RM. Policy responses to multiple risk behaviours in adolescents. Journal of Public Health (Oxford, England) 2012;34(Suppl. 1):i11–i19. doi: 10.1093/pubmed/fdr112. [DOI] [PubMed] [Google Scholar]
- Health Canada. (2014). Youth Smoking Survey: Table 2. Smoking status, by sex and grouped grades, Canada, 2012–2013. http://healthycanadians.gc.ca/publications/healthy-living-vie-saine/youth-smoking-survey-tables-2012-2013-tableaux-enquete-jeunes-tabagisme/index-eng.php. Published 2014.
- Institute of Medicine. (2012). Accelerating progress in obesity prevention. Washington, D.C.: National Academies Press; . doi:10.17226/13275. [DOI] [PMC free article] [PubMed]
- Johnston LM, Matteson CL, Finegood DT. Systems science and obesity policy: a novel framework for analyzing and rethinking population-level planning. American Journal of Public Health. 2014;104(7):1270–1278. doi: 10.2105/AJPH.2014.301884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Larson NI, Neumark-Sztainer D, Story M. Weight control behaviors and dietary intake among adolescents and young adults: longitudinal findings from project EAT. Journal of the American Dietetic Association. 2009;109(11):1869–1877. doi: 10.1016/j.jada.2009.08.016. [DOI] [PubMed] [Google Scholar]
- Leatherdale ST. An examination of the co-occurrence of modifiable risk factors associated with chronic disease among youth in the COMPASS study. Cancer Causes & Control. 2015;26(4):519–528. doi: 10.1007/s10552-015-0529-0. [DOI] [PubMed] [Google Scholar]
- Leatherdale ST, Rynard VA. Cross-sectional examination of modifiable risk factors for chronic disease among a nationally representative sample of youth: are Canadian students graduating high school with a failing grade for health? BMC Public Health. 2013;13(1):569. doi: 10.1186/1471-2458-13-569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leatherdale ST, Brown KS, Carson V, et al. The COMPASS study: a longitudinal hierarchical research platform for evaluating natural experiments related to changes in school-level programs, policies and built environment resources. BMC Public Health. 2014;14(1):331. doi: 10.1186/1471-2458-14-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liang KY, Zeger SL. Longitudinal data analysis using generalized linear models. Biometrika. 1986;73(1):13–22. doi: 10.1093/biomet/73.1.13. [DOI] [Google Scholar]
- Loth KA, Maclehose R, Bucchianeri M, Crow S, Neumark-Sztainer D. Predictors of dieting and disordered eating behaviors from adolescence to young adulthood. The Journal of Adolescent Health. 2014;55(5):705–712. doi: 10.1016/j.jadohealth.2014.04.016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patte, K. A., & Leatherdale, S. T. (2016). A cross-sectional analysis examining the association between dieting behaviours and alcohol use among secondary school students in the COMPASS study. Journal of Public Health (Oxford, England), 1–9. 10.1093/pubmed/fdw034. [DOI] [PMC free article] [PubMed]
- Penney TL, Kirk SFL. The health at every size paradigm and obesity: missing empirical evidence may help push the reframing obesity debate forward. American Journal of Public Health. 2015;105(5):e38–e42. doi: 10.2105/AJPH.2015.302552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pirkle EC, Richter L. Personality, attitudinal and behavioral risk profiles of young female binge drinkers and smokers. The Journal of Adolescent Health. 2006;38(1):44–54. doi: 10.1016/j.jadohealth.2004.09.012. [DOI] [PubMed] [Google Scholar]
- Polivy J, Herman CP. Dieting and binging. A causal analysis. The American Psychologist. 1985;40(2):193–201. doi: 10.1037/0003-066X.40.2.193. [DOI] [PubMed] [Google Scholar]
- Ramos SX. The ineffectiveness and unintended consequences of the public health war on obesity. Canadian Journal of Public Health. 2015;106(2):e79–e81. doi: 10.17269/cjph.106.4757. [DOI] [PubMed] [Google Scholar]
- Seo DC, Jiang N. Associations between smoking and extreme dieting among adolescents. Journal of Youth and Adolescence. 2009;38(10):1364–1373. doi: 10.1007/s10964-009-9421-0. [DOI] [PubMed] [Google Scholar]
- Storey K, Hanning R, Lambraki I, Driezen P, Fraser S, McCargar L. Determinants of diet quality among Canadian adolescents. Canadian Journal of Dietetic Practice and Research. 2009;70(2):58–65. doi: 10.3148/70.2.2009.58. [DOI] [PubMed] [Google Scholar]
- U.S. Department of Health and Human Services. (2012). Preventing Tobacco Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health.
- Woodruff SJ, Hanning RM, Lambraki I, Storey KE, McCargar L. Healthy eating index-C is compromised among adolescents with body weight concerns, weight loss dieting, and meal skipping. Body Image. 2008;5(4):404–408. doi: 10.1016/j.bodyim.2008.04.006. [DOI] [PubMed] [Google Scholar]
- Woodruff SJ, Hanning RM, McGoldrick K, Brown KS. Healthy eating index-C is positively associated with family dinner frequency among students in grades 6–8 from southern Ontario, Canada. European Journal of Clinical Nutrition. 2010;64(5):454–460. doi: 10.1038/ejcn.2010.14. [DOI] [PubMed] [Google Scholar]
- World Health Organization. (2015). Global database on body mass index: BMI classification. http://apps.who.int/bmi/index.jsp?introPage=intro_3.html. Published 2015. Accessed May 10, 2017.


