Abstract
Objectives
To assess the association between consumption of ultra-processed foods and obesity in the Canadian population.
Methods
Cross-sectional study including 19,363 adults aged 18 years or more from the 2004 Canadian Community Health Survey, cycle 2.2. Ultra-processed food intake was estimated using daily relative energy intake of ultra-processed food (% of total energy intake) from data obtained by 24-h food recalls. Obesity was assessed using body mass index (BMI ≥ 30 kg/m2). Univariate and multivariate linear regressions were performed to describe ultra-processed food consumption according to socio-economic and demographic variables, and multivariate logistic regression was performed to verify the association between ultra-processed food consumption and obesity, adjusting for potential confounders, including socio-demographic factors, physical activity, smoking, immigrant status, residential location, and measured vs self-reported weight and height.
Results
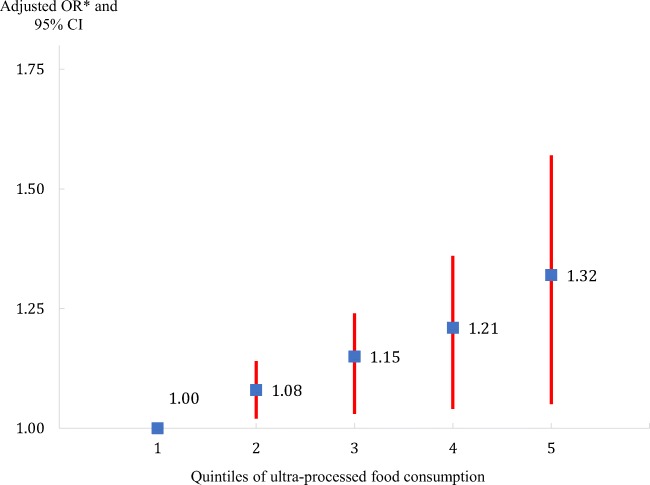
Ultra-processed foods make up almost half (45%) of the daily calories consumed by Canadian adults. Consumption of these foods is higher among men, younger adults, those with fewer years of formal education, smokers, those physically inactive, and Canadian-born individuals. Ultra-processed food consumption is positively associated with obesity. After adjusting for confounding factors, individuals in the highest quintile of ultra-processed food consumption were 32% more likely of having obesity compared to individuals in the first quintile (predicted OR = e0.005 × 56 = 1.32; 95% CI = 1.05–1.57).
Conclusion
Canadians would benefit from reducing consumption of ultra-processed foods and beverages and increasing consumption of freshly prepared dishes made from unprocessed or minimally processed foods.
Electronic supplementary material
The online version of this article (10.17269/s41997-018-0130-x) contains supplementary material, which is available to authorized users.
Keywords: Ultra-processed food, Food processing, Obesity, Diet quality
Résumé
Objectifs
Cette étude vise à évaluer l’association entre la consommation d’aliments ultra-transformés et l’obésité.
Méthodes
Étude transversale comprenant 19 363 adultes âgés de 18 ans ou plus qui ont participé à l’Enquête sur la santé dans les collectivités canadiennes, 2004, cycle 2.2. La consommation d’aliments ultra-transformés est estimée en utilisant l’apport énergétique relatif provenant des aliments ultra-transformés du rappel alimentaire de 24 heures. L’obésité est déterminée en utilisant l’indice de masse corporelle (IMC) ≥ 30 kg/m2. Les régressions linéaires univariée et multivariée ont été réalisées pour décrire la consommation d’aliments ultra-transformés selon différents groupes socioéconomiques et démographiques, et la régression logistique multivariée a été réalisée pour évaluer l’association entre la consommation de ces aliments et l’obésité, avec ajustement selon diverses variables de contrôle, incluant les facteurs sociodémographiques, l’activité physique, le tabagisme, le statut migratoire, la zone résidentielle et le type de mesure de l’IMC.
Résultats
Les aliments ultra-transformés sont largement consommés au Canada. La consommation de ces aliments est plus élevée chez les hommes, les jeunes adultes, les personnes avec moins d’années d’études, les fumeurs, les personnes physiquement inactives, et celles nées au Canada. La consommation d’aliments ultra-transformés est associée à l’obésité. Les individus du quintile supérieur de consommation d’aliments ultra-transformée ont 32 % plus de risque d’être obèses comparés aux individus du premier quintile (OR = e0.005 × 56 = 1,32; 95% CI = 1,05–1,57).
Conclusion
Les Canadiens pourraient bénéficier d’une réduction de la consommation de produits ultra-transformés et d’une augmentation de mets cuisinés sur place à base d’aliments peu ou pas transformés.
Mots-clés: Aliments ultra-transformés, Transformation alimentaire, Obésité, Qualité de l’alimentation
Introduction
In Canada, one in four adults (25%) is now obese, almost twice the prevalence observed in 1978 (PHAC 2011). Obesity prevalence has not changed much since 2004, and overall, there has been little or no improvement in population diet quality and health status over the last decades in Canada. One reason for that failure is that industrial food processing and its impact on the nature of food and on the state of human health has been overlooked and neglected in epidemiological and nutritional science, as well as in public policies and actions.
Food processing has allowed the development of very safe and convenient food products. However, with the goal of increasing shelf-life or reducing costs, the food industry uses methods such as hydrogenation, removal of water, addition of salt, sugars, fats, and additives, thus creating energy-dense and nutritionally imbalanced foods (Fardet 2016; Monteiro et al. 2017a). Of the few dietary assessment tools that differentiate food by its level of processing, the NOVA classification can be judged to be the most systematic and coherent (Moubarac et al. 2014).
According to NOVA, food processing is defined as all physical, biological, and chemical methods and techniques that occur after foods are separated from nature and before they are consumed or used in the preparation of dishes and meals (Monteiro et al. 2017a). Based on this definition, all foods are classified into: (1) unprocessed and minimally processed foods, such as fresh fruits and vegetables, packaged grains or flour, pasta, pasteurized milk, and chilled or frozen meat; (2) processed culinary ingredients, such as sugar, honey, salt, and butter; (3) processed foods, such as fruits in syrup and vegetables in brine; and (4) ultra-processed foods (Monteiro et al. 2017a). Particularly important for this study, ultra-processed foods are formulations of many ingredients, mostly of exclusive industrial use that result from a sequence of industrial processes (hence, ultra-processed) (Monteiro et al. 2017a). Examples are breakfast cereals, soft drinks and packaged fruit juices and drinks, packaged sweet or savory snacks, flavoured yogurts, instant dishes, reconstituted meat products such as sausages and nuggets, and most types of fast foods (Monteiro et al. 2017a).
Globally, ecological studies show that ultra-processed foods are dominating food supplies (PAHO 2015; Monteiro et al. 2017b). World sales of these foods increased by almost 45% between the years 2000 and 2013 (PAHO 2015). After the United States, Canada has the second highest annual sales of ultra-processed foods in the world; on average, Canadians bought approximately 230 k per person of ultra-processed foods in 2013 (PAHO 2015). Analyses of 2004 and 2015 national food consumption data reveal that almost half of Canadian daily calories come from ultra-processed foods (Moubarac 2017; Moubarac et al. 2016).
Studies have consistently shown that as the intake of ultra-processed food increases, overall quality of diets deteriorates and becomes more obesogenic (Moubarac et al. 2016; Louzada et al. 2017; Steele et al. 2017). Diets based on these foods are energy-dense, high in free and added sugars, saturated and trans fats, and depleted in most micronutrients and other bioactive compounds, fibre, and protein (Moubarac et al. 2016; Louzada et al. 2017; Steele et al. 2017; Steele and Monteiro 2017). Consumption of ultra-processed foods have also been associated with diet-related chronic diseases. Longitudinal studies in Spain show that ultra-processed food consumption increases the risk of overweight, obesity, and hypertension (Mendonça et al. 2016a, b). In France, a cohort study shows that consumption of ultra-processed foods increases the risk of some types of cancer (Fiolet et al. 2018). Cross-sectional studies have linked ultra-processed food consumption with obesity (Louzada et al. 2015; Juul et al. 2018), the metabolic syndrome (Lavigne-Robichaud et al. 2017; Tavares et al. 2012; Nasreddine et al. 2018), and dyslipidemias (Rauber et al. 2015).
Based on this research, the contribution of ultra-processed food to overall dietary intake has been proposed as an indicator of overall diet quality (PAHO 2015; Vandevijvere et al. 2013). In 2016, the Standing Senate Committee on Social Affairs, Science, and Technology of Canada highlighted the need to update Canada’s Food Guide to address food processing and suggested the use of NOVA (Ogilvie and Eggleton 2016). Similar recommendations were made by the Heart and Stroke Foundation of Canada (Moubarac 2017). Despite that, to date, there are no nationwide studies performed in Canada linking consumption of ultra-processed food with diet-related chronic diseases. The objective of this study is to examine the association between consumption of ultra-processed foods and obesity in the Canadian population.
Methods
Study context and design
We used data from the 2004–2005 Canadian Community Health Survey (CCHS, cycle 2.2, nutrition focus) conducted by Statistics Canada (Health Canada 2006). With an overall response rate of 77%, the survey studied approximately 35,000 individuals (Health Canada 2006). The sampling strategy was a multistage stratified cluster used to ensure representativeness of the Canadian population (Health Canada 2006). Dwellings were the sampling unit, and subsequently, one person from each dwelling was randomly selected to participate in the complete survey (Health Canada 2006).
The questionnaire used in the interviews contained two components: (1) general health and (2) 24-h food recalls that provided data on all food and beverages consumed in the previous 24 h of the interview day (Health Canada 2006). Interviews were computer-assisted, and the 24-h food recall data collection was performed using the Automated Multiple-Pass Method, a system used to maximize respondents’ recall of foods eaten (Health Canada 2006).
Trained interviewers collected height and weight values of respondents by using a high-quality calibrated digital balance (ProFit UC-321 made by Lifesource) and a measuring tape attached to the wall (Gorber et al. 2008). A subsample (10%) of respondents aged 18 years or more was asked to self-report their weight and height before being measured (Health Canada 2006). Due to several reasons (refusal, problems with equipment), around 37% of the survey’s respondents were not measured, but most of them (85%) agreed to self-report their weight and height (Health Canada 2006).
Study population
For this study, we retained all participants aged 18 years or above (n = 21,160). We excluded pregnant and breastfeeding women (n = 257), respondents with an invalid 24-h food recall, and those who reported not having consumed any calories on the previous day of the survey (n = 44).
We also excluded respondents with neither measured nor self-reported values of weight and height (n = 927). Compared to individuals with this information, individuals with no values were more likely to be women (60.8% vs 49.4%), less likely to be between 18 and 34 years (19.2% vs 28.7%), more likely to be classified in the upper-income category (32.8% vs 23.5%) and to not state their income (18.1% vs 9.1%).
In order to control for misreporting in the 24-h food recall, we used equations by the Institute of Medicine to estimate energy requirement of each individual. These equations are based on sex, age, and level of physical activity and are not available for underweight individuals. Thus, individuals with very low body weight (BMI < 18.5 kg/m2) (after adjustment of reported values) were excluded (n = 375), as were those with missing information on physical activity (n = 5).
Further, individuals with missing values for any other covariate used in our analyses were removed (n = 132), with the exception of the income variable. A total of 2043 adults did not state their income. In order to avoid excluding these individuals, we created a category “not stated” for this variable. We observed no significant difference in mean ultra-processed food consumption and mean BMI between individuals with complete vs incomplete data. A total of 19,363 participants were retained for our analyses.
Obesity indicator
We grouped BMI (kg/m2) into three categories: normal weight (18.5 ≤ BMI < 25.0), overweight (25.0 ≤ BMI < 30.0), and obese (BMI ≥ 30.0) (Health Canada 2006). BMI was calculated from measured values of weight (kg) and height (m) (BMI = weight[kg]/height[m]2) (Health Canada 2006). In the absence of measured height and weight, we used adjusted self-reported values. Self-reported values are subject to potential bias since there is a tendency to underestimate weight and overestimate height (Gorber et al. 2008). In a subsample of individuals with both measured and self-reported values (n = 1035), we performed linear regressions to generate correction equations (Gorber et al. 2008). We fitted separate models for BMI, weight, and height, and analyses were done for men and women separately. Supplementary Table 1 shows the final equations.
Ultra-processed food consumption
We used information from one 24-h food recall in order to estimate daily relative energy intake of ultra-processed foods (% of total energy intake as a continuous variable). Food items were classified into the four NOVA groups: unprocessed and minimally processed foods; processed culinary ingredients; processed foods; and ultra-processed foods. More details of this procedure have been published elsewhere (Moubarac et al. 2016). For detailed information about each NOVA food group, see Supplementary Table 2.
To handle potential systematic misreporting to which self-reported food intake is often subjected, we followed procedures described elsewhere (Garriguet 2008; Jessri et al. 2016). Briefly, we compared the reported energy intake (EI) with the estimated energy requirement (EER) of respondents to identify plausible and implausible reporters (under- or over-reporters). We calculated an EI:EER ratio for each subject and used cutoff points proposed by Jessri and colleagues to identify implausible reporters (Jessri et al. 2016). Individuals whose EI:EER ratio was below 0.70 were classified as under-reporters, and individuals whose ratio was above 1.42 were classified as over-reporters (Jessri et al. 2016).
Other variables
Four socio-demographic characteristics were included in our analyses: sex (men:women); age (grouped as 18–34; 35–44; 45–64; 65+ for the descriptive analyses); education (highest level of formal education completed by the respondent, dichotomized as less than post-secondary graduation; post-secondary graduation); and income adequacy (based on total household income and the number of persons per household and divided into lowest; lower-middle; upper-middle; highest; not stated, see Supplementary Table 3 for more information) (Statistics Canada 2008).
Two lifestyle variables were considered: physical activity index (PAI, grouped as inactive if 1.5 kcal/kg/day or active if ≥ 1.5 kcal/kg/day) and smoking status (non-smoker or smoker). Cultural background was expressed by immigrant status (non-immigrant or immigrant). Residential zone (rural or urban) was determined by Statistics Canada according to the number of dwellings in the region of residence (Health Canada 2006).
Statistical analyses
For the descriptive analysis, we first calculated the relative consumption (% of total daily energy intake) of each NOVA food group and subgroup and the mean relative intake of ultra-processed foods (% of total energy from ultra-processed foods). Second, we estimated the mean relative consumption of ultra-processed foods by the respondents’ characteristics and performed bivariate and multivariate linear regressions to assess differences in consumption across groups. In this analysis, relative consumption of ultra-processed foods (% of total energy intake, continuous) was the outcome. A hierarchical procedure was used to allow specifying a fixed sequential order of entry of the explanatory variables in the multivariate model. The blocks were as follows: (1) socio-demographic (sex, age, education, income level); (2) lifestyle (physical activity, smoking status); (3) culture (immigrant status); (4) environment (zone of residence); and (5) reporting group (plausible reporter, under-reporter, over-reporter) + measurement type (height and weight measured; height and weight self-reported; one value measured, and the other self-reported). The p value and standardized linear regression coefficients are presented. We assessed normality of variables graphically using histograms.
Finally, we calculated mean BMI across quintiles of ultra-processed food consumption and performed a multivariate logistic regression to separate the specific association between ultra-processed food consumption and obesity from the effects of other predictor variables. Here, obesity status (non-obese, BMI < 30 kg/m2/obese, BMI ≥ 30 kg/m2) is the outcome variable, and relative intake of ultra-processed foods (continuous) is the independent variable. Results are reported in a ten-percentage point increase (instead of a one-percentage point increase) by dividing the variable relative consumption of ultra-processed foods by ten. Likewise, we predicted the odds ratio of obesity at the mean ultra-processed food consumption observed at each quintile of ultra-processed foods. We used the following expression: OR1,i = , where i = 2, 3, 4, 5; and and are the mean ultra-processed food consumption in the respective quintiles of ultra-processed food consumption.
We performed exploratory analyses with overweight status as the outcome variable (non-overweight, BMI < 25 kg/m2/overweight, BMI ≥ 25 kg/m2).
The entry of covariates in the logistic regression models followed the same hierarchical procedure as described earlier.
Because total energy intake (kcal/day, continuous) and consumption of fruits and vegetables (total number of times per day respondents eat fruits and vegetables, continuous) may be plausible mediators of the association between ultra-processed food consumption and obesity but may also be a confounder, we performed sensitivity analysis controlling for these two variables. They were both added last to the model as a block called “dietary characteristics.”
Multiplicative interactions between the exposure variable and all covariates were tested by adding multiplicative terms in the logistic regression model.
All analyses were weighted (WTSD_M) and bootstrapped (BRR method) and performed using SAS version 9.4. Alpha is set at the 0.05 level.
Results
The mean age of the participants was 45.99 years (SE, 0.13), and the mean BMI was 26.98 kg/m2 (SE, 0.04). The average daily consumption of fruits and vegetables was 4.21 times a day (SE, 0.01). Canadians aged 18 years or over consumed on average 2047.36 kcal/day (SE, 6.92), 45.10% of which came from ultra-processed foods (939.65 kcal/day), 41.58% from unprocessed or minimally processed foods (832.48 kcal/day), 7.09% from processed foods (148.11 kcal/day), and 6.23% from culinary ingredients (131.51 kcal/day). The distribution of total daily energy intake according to NOVA groups and subgroups is presented in Table 1.
Table 1.
Distribution of total daily energy intake according to NOVA food groups and subgroups. Canadian adults ≥ 18 years (n = 19,363), 2004
| NOVA food groups and subgroups | % of energy intake mean (SE) |
|---|---|
| Unprocessed or minimally processed foods | 41.58 (0.14) |
| Meat and poultry | 9.74 (0.08) |
| Grains and flours | 7.53 (0.07) |
| Milk and plain yogurt | 5.21 (0.05) |
| Fruits and fruit juices | 5.26 (0.05) |
| Pasta | 3.13 (0.05) |
| Roots and tubers | 3.13 (0.04) |
| Vegetables | 2.44 (0.02) |
| Eggs | 1.83 (0.03) |
| Nuts | 1.01 (0.03) |
| Fish | 0.92 (0.03) |
| Legumes | 0.49 (0.02) |
| Othera | 0.90 (0.02) |
| Culinary ingredients | 6.23 (0.05) |
| Sugarsb | 2.80 (0.03) |
| Plant oils | 2.17 (0.03) |
| Animal fats | 1.00 (0.02) |
| Otherc | 0.26 (0.01) |
| Processed foods | 7.09 (0.07) |
| Cheese | 3.44 (0.05) |
| Canned or preserved foodsd | 2.44 (0.03) |
| Othere | 1.21 (0.04) |
| Ultra-processed foods | 45.10 (0.14) |
| Industrial packaged breads | 8.31 (0.06) |
| Confectionary | 6.82 (0.07) |
| Soft drinks, sweetened fruit juices, and drinks | 6.73 (0.06) |
| Fast food dishesf | 5.07 (0.10) |
| Sauces and spreads | 4.61 (0.05) |
| Margarine | 3.94 (0.04) |
| Sweetened breakfast cereals | 2.67 (0.04) |
| Chips, crackers, and other salty snacks | 2.36 (0.04) |
| Reconstituted meat productsg | 2.00 (0.04) |
| Sweetened milk-based productsh | 0.43 (0.02) |
| Other ultra-processed foodsi | 2.00 (0.04) |
| Total | 100.00 |
Data source: Statistics Canada, CCHS 2.2, Nutrition (Statistics Canada 2008)
aSea foods, spices and herbs, yeast, coffee, tea, un-disaggregated home-made dishes
bWhite and brown sugar, iced sugar, molasses, honey, and maple syrup
cVinegar, coconut milk, unsweetened cocoa powder, cornstarch
dFruits, vegetables, or pulses preserved in oil, salt or sugar; cured, smoked, or pickled meat and fish
eSalted, sweetened or oil-roasted nuts or seeds, almond paste, prepared tofu, condensed milk, peanut butter, pita breads, bannock, and dumpling
fHamburgers, hot dogs, fries, pizzas, sandwiches, and other products bought in fast food outlets
gSausages, luncheon meats, meat spreads, bacon, corned beef, beef jerky, fish sticks, and simulated meats
hIce cream, chocolate milk, flavoured yogurt, milkshakes, and malted milk
iCanned soups, baby products, canned mixed dishes, cheese products, frozen and prepared french fries and onion rings, fish or seafood imitations, meal replacements, sweeteners, protein shake powder, egg substitutes, coffee whitener, veggie slice, sausages, vanilla extract, malt extract, whey protein, added calcium, and soy protein
The distribution of specific respondent characteristics, the mean daily share of ultra-processed foods (% of total daily energy), and the results of bivariate analyses are presented in Table 2. Results from the multivariate linear regression models are shown in Table 3. In the final model, the variables significantly associated with ultra-processed food consumption were sex, age, education, physical activity, smoking status, immigrant status, and reporting group (under-reporter category). The strongest predictor was immigrant status (standardized β = − 0.22) and age (standardized β = − 0.14).
Table 2.
Dietary share of ultra-processed food according to characteristics of respondents. Canadian adults ≥ 18 years (n = 19,363), 2004
| Variables | Distribution (%) | % of energy intake from ultra-processed foods mean (SE) |
|---|---|---|
| Sex | ||
| Men | 50.94 | 45.98 (0.40)- |
| Women | 49.06 | 44.18 (0.38)* |
| Age | ||
| 18 to 34 years | 28.43 | 50.24 (0.55)- |
| 35 to 44 years | 20.60 | 43.90 (0.77)* |
| 45 to 64 years | 34.95 | 42.62 (0.46)* |
| 65 years or more | 16.02 | 41.90 (0.42)* |
| P for trend | < 0.001 | |
| Education | ||
| < post-secondary graduation | 19.36 | 46.52 (0.55)- |
| Post-secondary graduation | 80.64 | 44.75 (0.32)* |
| Income | ||
| Lowest | 8.14 | 44.45 (0.98)- |
| Lower-Middle | 18.59 | 45.01 (0.66)- |
| Upper-Middle | 32.86 | 45.01 (0.49)- |
| Highest | 31.63 | 44.79 (0.51)- |
| Not stated | 8.77 | 45.11 (0.91) |
| P for trend | 0.928 | |
| Physical activity | ||
| Inactive | 56.81 | 45.62 (0.38)- |
| Active | 43.19 | 44.40 (0.42)* |
| Smoking status | ||
| Non-smoker | 75.06 | 43.74 (0.31)- |
| Smoker | 24.94 | 49.19 (0.60)* |
| Immigration status | ||
| Non-immigrant | 76.41 | 47.77 (0.29)- |
| Immigrant | 23.59 | 36.44 (0.65)* |
| Residential area | ||
| Rural | 17.60 | 47.52 (0.52)- |
| Urban | 82.40 | 44.58 (0.32)* |
| Weight status | ||
| Normal weight | 40.17 | 44.33 (0.45)- |
| Overweight | 37.59 | 44.87 (0.45)- |
| Obese | 22.24 | 46.88 (0.58)* |
| P for trend | 0.001 | |
| Reporting group | ||
| Plausible reporter | 57.87 | 45.91 (0.35)- |
| Under-reporter | 31.09 | 43.92 (0.57)* |
| Over-reporter | 11.04 | 44.15 (0.81)- |
| P for trend | 0.003 | |
| Measurement type | ||
| Height and weight measured | 60.55 | 45.41 (0.37) |
| Height and weight self-reported | 34.10 | 44.35 (0.50) |
| One value measured and the other self-reported | 5.34 | 46.26 (1.32) |
| P for trend | 0.456 | |
Data source: Statistics Canada, CCHS 2.2, Nutrition (Statistics Canada 2008)
*p < 0.05 based on bivariate linear regressions (the category of reference is the first listed)
Table 3.
Results from multivariate linear regression models on determinants of ultra-processed food consumption, standardized linear regression coefficients (β and p values). Canadian adults ≥ 18 years (n = 19,363), 2004
| Variables | Model 1 | Model 2 | Model 3 | Model 4 | Model 5 | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| Socio-demographic (R2 = 0.03) | Lifestyle (R2 = 0.04) | Culture (R2 = 0.09) | Environment (R2 = 0.09) | Reporting + measurement (R2 = 0.09) | ||||||
| β | p value | β | p value | β | p value | β | p value | β | p value | |
| Sex | ||||||||||
| Men | – | – | – | – | – | – | – | – | – | – |
| Women | − 0.04 | 0.007 | − 0.03 | 0.026 | − 0.04 | 0.004 | − 0.04 | 0.005 | − 0.04 | 0.004 |
| Age | ||||||||||
| Continuous | − 0.16 | < 0.001 | − 0.15 | < 0.001 | − 0.14 | < 0.001 | − 0.14 | < 0.001 | − 0.14 | < 0.001 |
| Education | ||||||||||
| < post-secondary graduation | – | – | – | – | – | – | – | – | – | – |
| Post-secondary graduation | − 0.08 | < 0.001 | − 0.07 | < 0.001 | − 0.06 | < 0.001 | − 0.06 | < 0.001 | − 0.06 | < 0.001 |
| Income | ||||||||||
| Lowest | – | – | – | – | – | – | – | – | – | – |
| Lower-middle | 0.02 | 0.495 | 0.02 | 0.378 | 0.02 | 0.267 | 0.02 | 0.277 | 0.02 | 0.313 |
| Upper-middle | 0.03 | 0.219 | 0.04 | 0.104 | 0.02 | 0.337 | 0.02 | 0.346 | 0.02 | 0.376 |
| Highest | 0.01 | 0.689 | 0.03 | 0.325 | − 0.01 | 0.848 | − 0.01 | 0.850 | − 0.01 | 0.822 |
| Not stated | 0.02 | 0.418 | 0.02 | 0.237 | 0.02 | 0.314 | 0.02 | 0.318 | 0.02 | 0.285 |
| Physical activity | ||||||||||
| Inactive | – | – | – | – | – | – | – | – | ||
| Active | – | – | − 0.04 | 0.006 | − 0.04 | 0.006 | − 0.04 | 0.006 | ||
| Smoking status | ||||||||||
| Non-smoker | – | – | – | – | – | – | – | – | ||
| Smoker | – | – | 0.07 | < 0.001 | 0.07 | < 0.001 | 0.07 | < 0.001 | ||
| Immigrant status | ||||||||||
| Non-immigrant | – | – | – | – | – | – | – | – | – | – |
| Immigrant | – | – | – | – | − 0.23 | < 0.001 | − 0.22 | < 0.001 | − 0.22 | < 0.001 |
| Residential area | ||||||||||
| Rural | – | – | – | – | – | – | – | – | – | – |
| Urban | – | – | – | – | – | – | − 0.01 | 0.213 | − 0.01 | 0.298 |
| Reporting group | ||||||||||
| Plausible reporter | – | – | – | – | – | – | – | – | – | – |
| Under-reporter | – | – | – | – | – | – | – | – | − 0.03 | 0.023 |
| Over-reporter | – | – | – | – | – | – | – | – | − 0.02 | 0.084 |
| Measurement type | ||||||||||
| Both values measured | – | – | – | – | – | – | – | – | – | – |
| Both values reported | – | – | – | – | – | – | – | – | − 0.02 | 0.166 |
| One value measured and the other self-reported | – | – | – | – | – | – | – | – | − 0.00 | 0.957 |
Data source: Statistics Canada, CCHS 2.2, Nutrition (Statistics Canada 2008)
The mean dietary share of ultra-processed food to total energy intake across quintiles of ultra-processed food consumption was 20.08% in the first quintile, 36.11% in the second, 46.67% in the third, 57.66% in the fourth, and 75.95% in the last quintile (p for trend < 0.001). Across quintiles of ultra-processed food consumption, the mean BMI in the first quintile was 26.55 kg/m2 (SE, 0.17), 27.02 kg/m2 (SE, 0.17) in the second, 26.84 kg/m2 (SE, 0.14) in the third, 27.31 kg/m2 (SE, 0.16) in the fourth, and 27.35 kg/m2 (SE, 0.20) in the last quintile (p for trend < 0.001).
Results of the multivariate logistic models between ultra-processed food consumption and obesity/overweight are presented in Table 4. No significant multiplicative interaction was found between the exposure variable and covariates (data not shown).
Table 4.
Association between ultra-processed food consumption and obesity and overweight outcomes. Results from the multivariate logistic regression models. Canadian adults ≥ 18 years (n = 19,363), 2004
| Outcome | Models | Odds ratioa | 95% confidence interval | |
|---|---|---|---|---|
| Obesity (BMI ≥ 30 kg/m2) | Model 1 | Crudeb | 1.06 | 1.03–1.11 |
| Model 2 | Socio-demographicc | 1.07 | 1.05–1.12 | |
| Model 3 | Lifestyled | 1.07 | 1.04–1.12 | |
| Model 4 | Culturee | 1.05 | 1.02–1.10 | |
| Model 5 | Environmentf | 1.05 | 1.02–1.10 | |
| Model 6 | Reporting group + measurement typeg | 1.05 | 1.02–1.10 | |
| Overweight (BMI ≥ 25 kg/m2) | Model 1 | Crudeb | 1.03 | 1.02–1.09 |
| Model 2 | Socio-demographicc | 1.05 | 1.04–1.11 | |
| Model 3 | Lifestyled | 1.05 | 1.04–1.11 | |
| Model 4 | Culturee | 1.04 | 1.02–1.09 | |
| Model 5 | Environmentf | 1.04 | 1.02–1.09 | |
| Model 6 | Reporting group + measurement typeg | 1.03 | 1.02–1.09 | |
Data source: Statistics Canada, CCHS 2.2, Nutrition (Statistics Canada 2008)
aOdds ratio of a 10% increase in relative intake of ultra-processed foods (% of total energy intake)
bModel 1: crude
cModel 2: Model 1 + socio-demographic characteristics (sex, age, education and income)
dModel 3: Model 2 + lifestyle habits (physical activity and smoking status)
eModel 4: Model 3 + cultural background (immigrant status)
fModel 5: Model 4 + environment (residential area)
gModel 6: Model 5 + reporting group + measurement type (reporting group: under-reporter, plausible reporter, over-reporter; measurement type: height and weight measured, height and weight reported, one value measured and the other self-reported).
In the final model—after adjusting for sex, age, education, income, physical activity, smoking status, immigrant status, zone of residence, reporting group, and measurement type—a ten-percentage point increase in the relative energy intake from ultra-processed foods increased the likelihood of obesity by 5% (OR = 1.05, 95% CI = 1.01–1.08). Likewise, the odds of obesity at the mean ultra-processed food consumption observed in the highest quintile (average intake of ultra-processed food, 76% of total energy intake) was 32% higher (OR = e0.005 × 56 = 1.32; 95% CI = 1.05–1.57) than the odds at the mean of the lowest quintile (average intake, 20%). Figure 1 shows the predicted adjusted OR of being obese across quintiles of ultra-processed food consumption.
Fig. 1.
Predicted adjusted OR of obesity at mean ultra-processed food consumption observed across quintiles of ultra-processed food consumption. Canadian adults ≥ 18 years (n = 19,363), 2004. Asterisk indicates adjustment for age, sex, income, education, physical activity, smoking, immigrant status, residential area, reporting group, and measurement type. The mean dietary share of ultra-processed foods is 20.08% in the first quintile of ultra-processed food consumption, 36.11% in the second, 46.67% in the third, 57.66% in the fourth, and 75.95% in the last quintile. Data source: Statistics Canada, CCHS 2.2, Nutrition (Statistics Canada 2008)
For overweight, a ten-percentage point increase in the relative energy intake from ultra-processed foods increased the likelihood of overweight by 3% (OR = 1.03, 95% CI = 1.01–1.07).
The strength of the association between ultra-processed food consumption and obesity/overweight did not significantly change whether or not total energy intake and fruit and vegetable consumption were presented in the model (Supplementary Table 4).
Discussion
We found that ultra-processed foods are largely consumed in Canada. Consumption of these foods is higher among men, younger adults, smokers, and those who are physically inactive, Canadian born or who have fewer years of formal education. Our findings show that consumption of ultra-processed foods is associated with obesity.
In other high-income countries, adult men tend to consume more ultra-processed foods than adult women, and consumption of ultra-processed foods decreases with age (Louzada et al. 2015; Mendonça et al. 2016b). In Canada, elderly adults, and especially women, are the most likely to only eat food prepared at home, and the least likely to eat at fast food outlets (Garriguet 2007). In addition, culinary skills were customarily passed to women who were often responsible for household meal preparation (Flagg et al. 2014). It is known that home cooking is associated with better diet quality (Wolfson and Bleich 2015) and decreased ultra-processed food consumption in the United Kingdom (Lam and Adams 2017). This might partially explain differences in consumption across sex and age groups.
In our study, respondents with higher levels of formal education consumed less ultra-processed foods. Although education and nutrition knowledge do not always result in healthy eating habits, they are prerequisites for making better food choices in a food environment where a multitude of healthy and unhealthy food options are available (McEntee 2009). Unhealthy lifestyle habits like smoking and being physical inactive are associated with increased consumption of ultra-processed foods. Individuals who adopt healthy lifestyle habits might be more concerned about their health and diet and might be less likely to consume ultra-processed foods.
Immigrants consume significantly less ultra-processed foods than native-born Canadians. Although acculturation commonly occurs after long periods in the host country, certain immigrant groups in Canada tend to maintain some traditional dietary habits which are believed to be healthier than typical Western diets (Sanou et al. 2014). Maintenance of traditional food cultures that emphasize traditional home-cooked meals and eating together as a family may protect against ultra-processed food consumption.
Our findings support the existing literature suggesting an association between consuming ultra-processed foods and obesity (Mendonça et al. 2016b; Louzada et al. 2015; Juul et al. 2018). We found that individuals whose diets are based on ultra-processed foods are 32% more likely of having obesity than individuals whose diets are not based on ultra-processed foods. In Spain, a prospective study found that individuals in the highest quartile of ultra-processed food consumption had a risk 26% higher of developing overweight or obesity compared to individuals in the first quartile (Mendonça et al. 2016b). In the US, a cross-sectional study showed that consuming ≥ 74.2% vs ≤ 36.5% of total energy from ultra-processed food was associated with 48%, 53%, and 62% higher odds of overweight, obesity, and abdominal obesity, respectively (Juul et al. 2018).
Limitations
Because of the cross-sectional design, the results of our study could be affected by reverse causality, that is, the obesity status could influence the consumption of ultra-processed foods. In this case, the likely effect would be a dilution of the true association between ultra-processed foods and obesity since some obese people could be trying to have a healthier diet. Although the association between consumption of ultra-processed foods and obesity was adjusted for several potential confounders, such as demographic and socio-economic variables and physical activity, as in any observational study, the results of our study are subject to residual confounding.
At the time of this study, the most recent data available in Canada with detailed information on food intake and weight and height measurements was the 2004 CCHS 2.2. Our results may not reflect current Canadian dietary habits. However, recent analyses show that ultra-processed food consumption remained relatively stable between the years 2004 and 2015 (Moubarac 2017), and it is unlikely that the association between ultra-processed food consumption and obesity has changed during this period.
For 37% of the survey respondents, measured values of weight and height were not available. For these cases, we used self-reported values that were corrected to account for potential reporting bias. Still, nearly 3% of respondents in the 2004 CCHS 2.2 had neither measured nor self-reported values of height and weight, and they were excluded from analysis.
Self-reported food intake is often subject to misreporting. To address this, we adjusted our models for reporting group. Still, if obese people should be more prone to under-report ultra-processed food consumption, this could result in attenuation or even inverse associations between ultra-processed food consumption and obesity.
Ultra-processed food consumption was most probably underestimated. Mixed dishes, such as lasagna, were already broken down into ingredients in the dataset, and some ultra-processed dishes not consumed in a fast food setting (such as a frozen lasagna consumed at home) might have been treated as culinary preparations instead of ultra-processed foods (Moubarac et al. 2016).
Another limitation concerns day-to-day variation linked to 24-h dietary recalls. If the diet on the recall day does not represent the participant’s usual diet, this could lead to spurious associations between ultra-processed food consumption and obesity.
Conclusion
Our study supports existing evidence on the association between ultra-processed food consumption and obesity. Clear identification of the risks associated with a high consumption of ultra-processed foods should become part of the public discourse, and Canadians must be encouraged to favour fresh, minimally processed foods. A whole-of-society approach with several strategies should be employed to make the healthy choice the easier choice for Canadians. These include a ban on the advertising of ultra-processed food and beverages to children, taxation of ultra-processed products, and implementation of effective tax levers to encourage consumption of healthy foods. Starting early with children and introducing food preparation skills into school curricula will go a long way toward the popularization of home and artisanal food preparation. Finally, future dietary guidelines for the Canadian population should take food processing into account.
Electronic supplementary material
(DOCX 30 kb)
Compliance with ethical standards
This study complies with current research ethics standards and was approved by the Health Research Ethics Board of the University of Montreal (17-017-CERES-D). Data access was granted by Statistics Canada, under contract (no. 13-SSH-MTL-3475) and data were analyzed at the Québec interUniversity Centre for Social Statistics in Montreal.
Contributor Information
Milena Nardocci, Email: milena.nardocci.fusco@umontreal.ca.
Bernard-Simon Leclerc, Email: bs.leclerc@umontreal.ca.
Maria-Laura Louzada, Email: maria.laura.louzada@gmail.com.
Carlos Augusto Monteiro, Email: carlosam@usp.br.
Malek Batal, Email: malek.batal@umontreal.ca.
Jean-Claude Moubarac, Phone: +1 (514) 343-6111, Email: jc.moubarac@umontreal.ca.
References
- Fardet A. Minimally processed foods are more satiating and less hyperglycemic than ultra-processed foods: A preliminary study with 98 ready-to-eat foods. Food & Function. 2016;7(5):2338–2346. doi: 10.1039/C6FO00107F. [DOI] [PubMed] [Google Scholar]
- Fiolet T, Srour B, Sellem L, et al. Consumption of ultra-processed foods and cancer risk: Results from NutriNet-Santé prospective cohort. BMJ. 2018;360:k322. doi: 10.1136/bmj.k322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flagg LA, Sen B, Kilgore M, et al. The influence of gender, age, education and household size on meal preparation and food shopping responsibilities. Public Health Nutrition. 2014;17(9):2061–2070. doi: 10.1017/S1368980013002267. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Garriguet D. Canadians’ eating habits. Health Reports. 2007;18(2):17–32. [PubMed] [Google Scholar]
- Garriguet D. Impact of identifying plausible respondents on the under-reporting of energy intake in the Canadian Community Health Survey. Health Reports. 2008;19(4):47–55. [PubMed] [Google Scholar]
- Gorber SC, Shields M, Tremblay MS, et al. The feasibility of establishing correction factors to adjust self-reported estimates of obesity. Health Reports. 2008;19(3):71–82. [PubMed] [Google Scholar]
- Health Canada (2006). Canadian Community Health Survey, Cycle 2.2, Nutrition (2004): A guide to accessing and interpreting the data. Accessed 16 Nov 2016. Available at: http://www.hc-sc.gc.ca/fn-an/surveill/nutrition/commun/cchs_guide_escc-eng.php. Accessed 16 Nov 2016.
- Jessri M, Lou WY, L’Abbé MR. Evaluation of different methods to handle misreporting in obesity research: Evidence from the Canadian national nutrition survey. The British Journal of Nutrition. 2016;115(1):147–159. doi: 10.1017/S0007114515004237. [DOI] [PubMed] [Google Scholar]
- Juul F, Martinez-Steele E, Parekh N, et al. Ultra-processed food consumption and excess weight among US adults. The British Journal of Nutrition. 2018;120(1):90–100. doi: 10.1017/S0007114518001046. [DOI] [PubMed] [Google Scholar]
- Lam MCL, Adams J. Association between home food preparation skills and behaviour, and consumption of ultra-processed foods: Cross-sectional analysis of the UK National Diet and nutrition survey (2008–2009) International Journal of Behavioral Nutrition and Physical Activity. 2017;14(1):68. doi: 10.1186/s12966-017-0524-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lavigne-Robichaud, M., Moubarac, J.-C., Lantagne-Lopez, S., et al. (2017). Diet quality indices in relation to metabolic syndrome in an indigenous Cree (Eeyouch) population in northern Québec, Canada. Public Health Nutrition, 21(1), 172–180. [DOI] [PMC free article] [PubMed]
- Louzada MLC, Baraldi LG, Steele EM, et al. Consumption of ultra-processed foods and obesity in Brazilian adolescents and adults. Preventive Medicine. 2015;81:9–15. doi: 10.1016/j.ypmed.2015.07.018. [DOI] [PubMed] [Google Scholar]
- Louzada, M. L. d. C., Ricardo, C. Z., Steele, E. M., et al. (2017). The share of ultra-processed foods determines the overall nutritional quality of diets in Brazil. Public Health Nutrition, 21(1), 94–102. [DOI] [PMC free article] [PubMed]
- McEntee J. Highlighting food inadequacies: Does the food desert metaphor help this cause? British Food Journal. 2009;111(4):349–363. doi: 10.1108/00070700910951498. [DOI] [Google Scholar]
- Mendonça, R. D., Lopes, A. C. S., Pimenta, A. M., et al. (2016a). Ultra-processed food consumption and the incidence of hypertension in a Mediterranean cohort: The Seguimiento Universidad de Navarra Project. American Journal of Hypertension, 30(4), 358–366. [DOI] [PubMed]
- Mendonça, R. D., Pimenta, A. M., Gea, A., et al. (2016b). Ultraprocessed food consumption and risk of overweight and obesity: the University of Navarra Follow-Up (SUN) cohort study. The American Journal of Clinical Nutrition, 104(5), 1433–1440. [DOI] [PubMed]
- Monteiro, C. A., Cannon, G., Moubarac, J.-C., et al. (2017a). The UN decade of nutrition, the NOVA food classification and the trouble with ultra-processing. Public Health Nutrition, 21(1), 5–17. [DOI] [PMC free article] [PubMed]
- Monteiro, C. A., Moubarac, J.-C., Levy, R. B., et al. (2017b). Household availability of ultra-processed foods and obesity in nineteen European countries. Public Health Nutrition, 21(1), 18–26. [DOI] [PMC free article] [PubMed]
- Moubarac JC (2017). Ultra-processed foods in Canada: consumption, impact on diet quality and policy implications. Montréal: TRANSNUT, University of Montreal. Available at: http://www.heartandstroke.ca/-/media/pdf-files/canada/media-centre/hs-report-upp-moubarac-dec-5-2017.ashx.
- Moubarac J-C, Parra DC, Cannon G, et al. Food classification systems based on food processing: Significance and implications for policies and actions: A systematic literature review and assessment. Current Obesity Reports. 2014;3(2):256–272. doi: 10.1007/s13679-014-0092-0. [DOI] [PubMed] [Google Scholar]
- Moubarac, J.-C., Batal, M., Louzada, M. L., et al. (2016). Consumption of ultra-processed foods predicts diet quality in Canada. Appetite, 108, 512–520. [DOI] [PubMed]
- Nasreddine L, Tamim H, Itani L, et al. A minimally processed dietary pattern is associated with lower odds of metabolic syndrome among Lebanese adults. Public Health Nutrition. 2018;21(1):160–171. doi: 10.1017/S1368980017002130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogilvie, K.K., Eggleton, A. (2016). Obesity in Canada. A whole-of-society approach for a healthier Canada. Report of the standing senate committee on social affairs, science and technology. Standing senate committee on social affairs, Science and Technology. Available at: www.senate-senat.ca/social.asp.
- PAHO . Ultra-processed food and drink products in Latin America: trends, impact on obesity, policy implications. Washington D.C.: Pan American Health Organization; 2015. [Google Scholar]
- PHAC. (2011). Obesity in Canada - healthy living - Public Health Agency of Canada. Public Health Agency of Canada. Available at: http://www.phac-aspc.gc.ca/hp-ps/hl-mvs/oic-oac/index-eng.php. Accessed 10 Aug 2016.
- Rauber F, Campagnolo PDB, Hoffman DJ, et al. Consumption of ultra-processed food products and its effects on children’s lipid profiles: A longitudinal study. Nutrition, Metabolism, and Cardiovascular Diseases. 2015;25(1):116–122. doi: 10.1016/j.numecd.2014.08.001. [DOI] [PubMed] [Google Scholar]
- Sanou D, O’Reilly E, Ngnie-Teta I, et al. Acculturation and nutritional health of immigrants in Canada: A scoping review. Journal of Immigrant and Minority Health. 2014;16(1):24–34. doi: 10.1007/s10903-013-9823-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Statistics Canada (2008). Canadian Community Health Survey (CCHS) Cycle 2.2, 2004. Nutrition - General Health (including vitamins & mineral supplements) & 24-hour dietary recall, Master and Shared files - Derived variables documentation. Available at: http://www23.statcan.gc.ca/imdb-bmdi/pub/document/5049_D24_T9_V1-eng.pdf.
- Steele, E. M., & Monteiro, C. A. (2017). Association between dietary share of ultra-processed foods and urinary concentrations of phytoestrogens in the US. Nutrients, 9(3). 10.3390/nu9030209. [DOI] [PMC free article] [PubMed]
- Steele EM, Popkin BM, Swinburn B, et al. The share of ultra-processed foods and the overall nutritional quality of diets in the US: Evidence from a nationally representative cross-sectional study. Population Health Metrics. 2017;15(1):6. doi: 10.1186/s12963-017-0119-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tavares LF, Fonseca SC, Garcia Rosa ML, et al. Relationship between ultra-processed foods and metabolic syndrome in adolescents from a Brazilian Family Doctor Program. Public Health Nutrition. 2012;15(1):82–87. doi: 10.1017/S1368980011001571. [DOI] [PubMed] [Google Scholar]
- Vandevijvere S, Monteiro CA, Krebs-Smith SM, et al. Monitoring and benchmarking population diet quality globally: A step-wise approach. Obesity Reviews. 2013;14(Suppl 1):135–149. doi: 10.1111/obr.12082. [DOI] [PubMed] [Google Scholar]
- Wolfson JA, Bleich SN. Is cooking at home associated with better diet quality or weight-loss intention? Public Health Nutrition. 2015;18(8):1397–1406. doi: 10.1017/S1368980014001943. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(DOCX 30 kb)