Background:
Reduction mammaplasty was shown to ameliorate physical and psychological problems in adolescents suffering from macromastia. However, benefits of the Wise compared to the vertical incision pattern have not yet been established in this population. The aim of this study is to compare the outcomes of these 2 techniques in adolescents undergoing reduction mammaplasty.
Methods:
A retrospective study of adolescents undergoing breast reduction by a single surgeon between 2011 and 2017 was conducted. Wise and vertical reduction techniques were compared based on demographics, surgical outcomes, patient satisfaction, and aesthetic outcomes. Patient satisfaction was determined using the validated BREAST-Q survey, and aesthetic outcomes using the validated ABNSW system.
Results:
A total of 60 adolescents underwent reduction mammaplasty (Wise/inferior pedicle = 80.0%, Wise/superior medial pedicle = 1.7%, vertical/superior medial pedicle = 18.3%). Patients who reported preoperative pain (Wise = 95.9%, vertical = 72.7%, P = 0.039) were more likely to undergo Wise reduction. Patients with Wise reductions also were more likely to undergo bilateral reduction (Wise = 93.9%; vertical = 63.6%, P = 0.017). The major and minor complication rates were 1.7% (Wise = 2.0%, vertical = 0%, P = NS) and 23.3% (Wise = 20.4%, vertical = 36.4%, P = NS), respectively. Adolescents undergoing Wise incision demonstrated statistically significant improvement in NAC contour (Wise = 61%, vertical = 47%, P = 0.028) and overall aesthetic outcome (Wise = 25%, vertical = 17%, P = 0.008) with scarring not being a negative factor (Wise = −16%; vertical = −35%, P = 0.004). Patient satisfaction was comparable in both groups.
Conclusions:
Reduction mammaplasty is a safe, effective treatment for adolescent macromastia. The similarity in complication and satisfaction rates between Wise and vertical patterns suggests that both techniques can be safely performed in the adolescent population and allow for overall improvements in aesthetic outcomes.
INTRODUCTION
Adolescent macromastia is a common and often distressing issue affecting many females, which often leads to severe back and neck pain, posture abnormalities, and skin and soft tissue infections.1 Debilitating psychological effects such as development of eating disorders and low self-esteem are also reported by adolescents who suffer from macromastia.2 Reduction mammaplasty is a known alternative to alleviate many of these physical and psychological problems, and is frequently accomplished by use of either the Wise or vertical incision pattern.
Although outcomes of reduction mammaplasty have been well studied in adults3–7, only 3 studies to date have examined outcomes of breast reduction in the adolescent population.1,2,8 One of these studies examined patient satisfaction and was limited by small cohort size,8 and none examined aesthetic outcomes of the adolescents. Most importantly, none of these studies directly compared the outcomes of Wise versus vertical incision patterns. This study seeks to compare surgical, aesthetic, and patient satisfaction outcomes between 2 cohorts of adolescents who underwent reduction mammaplasty by either the Wise or vertical method. Ultimately, the goal of this comparison is to help determine characteristics of adolescents who would most benefit from breast reduction surgery and characterize the scope of advantages and disadvantages associated with both Wise and vertical patterns of breast reduction.
METHODS
Approval from the Institutional Review Board at the University of Pittsburgh was obtained. A retrospective cohort study was conducted of all adolescents who underwent reduction mammaplasty surgery between January 2011 and December 2017 performed by the senior author at the University of Pittsburgh Medical Center Children’s Hospital. Inclusion criteria were adolescent females requiring reduction mammaplasty; exclusion criteria were reduction mammaplasty using techniques other than Wise or vertical. The decision between Wise versus vertical incision pattern was made based on the breast size and degree of ptosis in the patient. The patients were then divided into 2 cohorts depending on the incision pattern performed.
Demographics
Variables examined included patient demographics (age, body mass index, co-morbidities), presenting symptoms, diagnosis (macromastia, asymmetry), and breast measurements (nipple to inframammary fold, sternal notch to nipple, bra size).
Surgical Outcomes
Intra and postoperative outcomes examined included reduction incision pattern (Wise, vertical) and pedicle type (inferior, superior medial), resected breast tissue weight and pathology, length of hospital stay, surgical complications, number of revisionary procedures, and follow-up. Major complications were defined as those requiring surgical revision, such as seromas, hematomas, nipple necrosis, or skin necrosis. Minor complications were defined as those that healed on their own without revision or required minor care in an ambulatory setting. These included delayed wound healing, wound dehiscence, scarring, or infection.
Patient Satisfaction
Patient satisfaction was evaluated postoperatively using the Satisfaction with Outcome module of the validated BREAST-Q reduction/mastopexy module Version 1.0.9,10 Patients were contacted by phone and administered 8 survey questions to assess their satisfaction with the procedure, the outcome, and the overall congruence with their expectations. Answers were graded using the BREAST-Q scale, which ranged from disagree to definitely agree. A total score from 0 to 100 was then calculated through the QScore scoring software, with higher scores indicating greater satisfaction.
Aesthetic Outcomes
Aesthetic outcomes were evaluated using deidentified pre- and postoperative patient photographs. Aesthetic outcomes scoring was done using the validated ABNSW system created by the Japanese Breast Cancer Society, which assesses variables including (a)symmetry, (b)reast shape, (n)ipple deformation, (s)kin condition, and (w)ound scar.11 A panel of 2 independent, blinded medical students assessed and rated each variable on a scale ranging from zero to three, as specifically defined within the ABNSW scoring system, where higher scores imply better aesthetic outcomes.
Statistical Analysis
All data were recorded in a Microsoft Excel spreadsheet (Microsoft Corp., Redmond, Wash.) and analyzed using IBM SPSS for Windows Version 25.0 (IBM Corp., Armonk, N.Y.). Descriptive statistics were used to compare demographics and intra/postoperative variables that occurred in patients undergoing reduction with Wise versus vertical technique. These were recorded as percentages for categorical variables and means and SD for numerical variables. Categorical data was analyzed using Chi-square and Fisher’s exact tests. Means of groups were compared using t-test. Statistical significance was assumed for P-values < 0.05.
RESULTS
A total of 60 patients were reviewed, who underwent breast reduction with either the Wise (n = 49) or vertical pattern (n = 11).
Demographics
The mean age of patients undergoing reduction mammaplasty was 16.7 years (Wise = 16.7, vertical = 17.0, p = NS) and mean body mass index was 28.4 kg/m2 (Wise = 28.5, vertical = 27.3, p = NS). Comorbidities were similar in both groups and included patients who were overweight, obese, or smokers. Other demographics and patient characteristics are summarized in Table 1. Presenting symptoms associated with adolescent macromastia were similar between both groups. An exception was preoperative pain, which was reported by 95.9% of adolescents who underwent Wise reduction and 72.7 percent of adolescents who underwent vertical reduction (P = 0.039).
Table 1.
Patient Characteristics
| Overall | Wise | Vertical | P | |
|---|---|---|---|---|
| Total no. patients | 60 | 49 | 11 | — |
| Mean age ± SD, y | 16.7 ± 1.7 | 16.7 ± 1.8 | 17.0 ± 1.3 | NS |
| Mean BMI ± SD | 28.4 ± 4.2 | 28.5 ± 0.6 | 27.3 ± 2.6 | NS |
| Comorbidities, n (%) | ||||
| Obesity | 19 (31.7) | 18 (36.7) | 1 (9.1) | NS |
| Overweight | 27 (45.0) | 19 (38.8) | 8 (72.7) | NS |
| Smoking | 2 (3.3) | 2 (4.1) | 0 (0) | NS |
| Presenting symptoms, n (%) | ||||
| Pain | 55 (91.7) | 47 (95.9) | 8 (72.7) | 0.039 |
| Rash | 20 (33.3) | 17 (34.7) | 3 (27.3) | NS |
| Shoulder grooving | 16 (26.7) | 10 (20.4) | 6 (54.5) | NS |
| Asymmetry | 9 (15.0) | 5 (10.2) | 4 (36.4) | NS |
| Poor posture | 4 (6.7) | 3 (6.1) | 1 (9.1) | NS |
| Paresthesia | 2 (3.3) | 2 (4.1) | 0 (0) | NS |
| Sleep compromise | 2 (3.3) | 2 (4.1) | 0 (0) | NS |
BMI, body mass index; NS, not significant.
Most patients had diagnoses of macromastia (90%), with a large number also having diagnoses of asymmetry (48%). Patients with Wise pattern reductions were found to have a greater number of preoperative macromastia diagnoses (Wise = 95.9%, vertical = 63.6%, p = 0.008). Mean nipple to intramammary fold measurements were 12.4 ± 1.4 cm (right) and 11.7 ± 1.9 (left) while mean sternal notch to nipple measurements were 30.8 ± 3.7 (right) and 30.2 ± 4.1 (left). Patients undergoing Wise pattern incision were more likely to have a larger left nipple to intramammary fold measurement (Wise = 11.9 cm, vertical = 8.5 cm, P = 0.009). Preoperative cup sizes among both groups ranged from D to I, with the most frequent cup size being DD (Wise = 28.6%, vertical = 36.4%, p = NS). Preoperative measurements and diagnoses are summarized in Table 2.
Table 2.
Preoperative Characteristics
| Overall | Wise | Vertical | P | |
|---|---|---|---|---|
| Total no. patients | 60 | 49 | 11 | — |
| Diagnosis, n (%) | ||||
| Macromastia | 54 (90.0) | 47 | 7 | 0.008 |
| Asymmetry | 29 (48.3) | 21 | 8 | NS |
| Nipple to IMF ± SD, cm | ||||
| Right | 12.4 ± 1.4 | 12.5 ± 1.4 | 11.0 ± 1.4 | NS |
| Left | 11.7 ± 1.9 | 11.9 ± 1.7 | 8.5 ± 0.7 | 0.009 |
| SN to nipple ± SD, cm | ||||
| Right | 30.8 ± 3.7 | 31.1 ± 3.7 | 28.9 ± 2.2 | NS |
| Left | 30.2 ± 4.1 | 30.6 ± 3.7 | 27.4 ± 4.2 | NS |
| Cup sizes, n (%) | ||||
| D | 6 (10.0) | 4 (8.2) | 2 (18.2) | NS |
| DD | 18 (30.0) | 14 (28.6) | 4 (36.4) | NS |
| DDD | 15 (25.0) | 14 (28.6) | 1 (9.1) | NS |
| DDDD | 1 (1.7) | 1 (2.0) | 0 (0.0) | NS |
| E | 1 (1.7) | 1 (2.0) | 0 (0.0) | NS |
| F | 4 (6.7) | 5 (10.2) | 0 (0.0) | NS |
| G | 7 (11.7) | 6 (12.2) | 1 (9.1) | NS |
| H | 1 (1.7) | 1 (2.0) | 0 (0.0) | NS |
| HHH | 1 (1.7) | 1 (2.0) | 0 (0.0) | NS |
| I | 2 (3.3) | 1 (2.0) | 1 (9.1) | NS |
IMF, inframammary fold; SN, sternal notch; NS, not significant.
Operative Details
Most patients underwent bilateral reduction (90%), with patients with Wise pattern reduction being more likely to undergo bilateral reduction compared with those with vertical patterns (Wise = 93.9%, vertical = 63.6%, P = 0.017). The inferior pedicle was favored for the Wise incision (inferior = 98%, superior medial = 2%) and the superior medial pedicle was favored for vertical incision pattern (inferior = 0%, superior medial = 100%). Mean mass of resected breast tissue was 508 g on the right side (Wise = 528.9 g, vertical = 390 g, P = NS) and 534 g on the left side (Wise=526.4 g, vertical=540.8 g, P = NS). Resected breast tissue pathology in both groups did not identify occult malignancy. The mean hospital stay post-surgery was found to be 1.3 ± 0.5 days. Patients undergoing Wise pattern reduction were found to have shorter length of hospital stay than their vertical reduction counterparts (Wise = 1.2 days, vertical = 1.6 days, P = 0.021). Mean time to follow-up for the total cohort was 6.3 months. Total number of procedures performed (which consisted of original breast reduction surgery as well as any revisionary surgeries) were found to be greater in the vertical group (Wise = 1.0 ± 0.0, vertical = 1.09 ± 0.3; P = 0.042). Operative details are summarized in Table 3.
Table 3.
Operative Details
| Overall | Wise | Vertical | P | |
|---|---|---|---|---|
| Total no. patients | 60 | 49 | 11 | — |
| Pedicle, n (%) | ||||
| Inferior | 48 (80.0) | 48 (98.0) | 0 (0.0) | NS |
| Superior medial | 12 (20.0) | 1 (2.0) | 11 (100.0) | NS |
| Operated side, n (%) | ||||
| Bilateral | 54 (90.0) | 46 (93.9) | 7 (63.6) | 0.017 |
| Right | 7 (11.7) | 3 (6.1) | 4 (36.4) | NS |
| Left | 0 (0.0) | 0 (0.0) | 0 (0.0) | NS |
| Contralateral mastopexy | 3 (5.0) | 1 (2.0) | 2 (18.2) | NS |
| Mean resected weight ± SD, g | ||||
| Right | 508.5 ± 318.0 | 528.9 ± 327.0 | 390.0 ± 257.6 | NS |
| Left | 533.8 ± 325.5 | 526.5 ± 341.4 | 540.9 ± 218.6 | NS |
| Length of stay ± SD, days | 1.3 ± 0.5 | 1.2 ± 0.3 | 1.6 ± 1.1 | 0.021 |
| Total mean no. procedures ± SD | 1.0 ± 0.0 | 1.09 ± 0.3 | 0.042 |
NS, not significant.
Surgical Outcomes
Surgical complications developed in 23% of patients (minor complications, 23%; major complications, 2%). Although a higher complication rate was observed with the vertical pattern (Wise = 20.4%, vertical = 36.4%), this was not statistically significant. Major complications were reported in only 1 patient (Wise = 2.0%, vertical = 0%, P = NS). No patients in either group suffered from complete nipple sensation loss. The greatest differences among minor complication rates were seen with wound dehiscence (Wise = 6.1%, vertical = 27.3%, P = NS) and delayed wound healing (Wise = 12.2%, vertical = 9.1%, P = NS). Both major and minor complications among 2 groups were found to be not statistically different (Table 4). Revisionary surgeries were documented in 2% of patients, with a 0% revision rate in Wise patients and 9.1% revision rate in vertical patients (P = NS).
Table 4.
Complication Rates
| Overall | Wise | Vertical | P | |
|---|---|---|---|---|
| Total no. patients | 60 | 49 | 11 | — |
| Surgical complications, n (%) | ||||
| Overall | 14 (23.3) | 10 (20.4) | 4 (36.4) | NS |
| Major | 1 (1.7) | 1 (2.0) | 0 (0.0) | NS |
| Minor | 14 (23.3) | 10 (20.4) | 4 (36.4) | NS |
| Delayed wound healing | 7 (11.7) | 6 (12.2) | 1 (9.1) | NS |
| Wound dehiscence | 6 (10.0) | 3 (6.1) | 3 (27.3) | NS |
| Fat necrosis | 2 (3.3) | 2 (4.1) | 0 (0.0) | NS |
| Scarring | 1 (1.7) | 1 (2.0) | 0 (0.0) | NS |
| Infection | 1 (1.7) | 0 (0.0) | 1 (9.1) | NS |
| Nipple necrosis | 1 (1.7) | 1 (2.0) | 0 (0.0) | NS |
| Skin necrosis | 0 (0.0) | 0 (0.0) | 0 (0.0) | NS |
| Nipple sensation loss | 0 (0.0) | 0 (0.0) | 0 (0.0) | NS |
| Hematoma | 0 (0.0) | 0 (0.0) | 0 (0.0) | NS |
| Seroma | 0 (0.0) | 0 (0.0) | 0 (0.0) | NS |
| Asymmetry/deformity | 0 (0.0) | 0 (0.0) | 0 (0.0) | NS |
| Revisions, n (%) | ||||
| No revisions | 59 (98.3) | 49 (100.0) | 10 (90.9) | NS |
| Secondary revision | 1 (1.7) | 0 (0.0) | 1 (9.1) | NS |
| Tertiary revision | 0 (0.0) | 0 (0.0) | 0 (0.0) | NS |
NS, not significant.
Patient Satisfaction
The total response rate was 72% (Wise = 69%, vertical = 82%), with a mean satisfaction score of 74%. Mean time to follow-up for patient satisfaction was 39.8 months. Patients undergoing Wise incision had higher satisfaction rates (77%) than those undergoing vertical incision (62%); however, this difference did not reach statistical significance. Patient satisfaction results are summarized in Table 5.
Table 5.
Patient Satisfaction
| Overall | Wise | Vertical | P | |
|---|---|---|---|---|
| Total no. patients | 43 | 34 | 9 | — |
| Satisfaction, % ± SD | 73.5 ± 23.4 | 76.6 ± 19.7 | 61.8 ± 33.0 | 0.2272 |
Aesthetic Outcomes
The majority of patients (70%) had their preoperative and postoperative photographs assessed (Wise = 63%, vertical = 100%). Patients were excluded from the analysis if their postoperative photographs were unavailable. Out of a total of three maximum points for each category, the overall preoperative mean for the group was 1.63 ± 0.33 points and the postoperative mean was 2.33 ± 0.30 points. Patients undergoing Wise reduction were noted to have less asymmetry both preoperatively (Wise = 1.89 points, vertical = 1.32 points, P = 0.047) and postoperatively (Wise = 2.55, vertical = 2.05, P = 0.008). Significant differences in postoperative photographs were also found for shape (Wise = 2.42, vertical = 2.05, P = 0.028), scar (Wise = 2.53, vertical = 1.95, P = 0.004), and overall score (Wise, 2.42; vertical, 2.07; P = 0.001). Comparison between preoperative and postoperative photographs showed overall aesthetic improvement in all categories except for scarring, with statistically significant improvement being noted in NAC contour (Wise, 61%; vertical, 47%; p = 0.028) and overall average (Wise, 25%; vertical, 17%; P = 0.008). Scarring compared with baseline preoperative pictures was significantly more in the vertical incision compared with the Wise incision (Wise = −16%, vertical = −35%, P = 0.004). Aesthetic outcomes results summarized in Table 6. Examples of preop and postop photographs are represented in Figures 1 and 2.
Table 6.
Aesthetic Outcomes
| Overall | Wise | Vertical | P | |
|---|---|---|---|---|
| Total no. patients | 43 | 31 | 11 | — |
| Preoperative ± SD | ||||
| Asymmetry | 1.8 ± 0.8 | 1.9 ± 0.7 | 1.3 ± 0.9 | 0.047 |
| Shape | 1.0 ± 0.6 | 1.1 ± 0.6 | 0.8 ± 0.8 | NS |
| NAC contour | 0.8 ± 0.6 | 0.8 ± 0.6 | 0.9 ± 0.5 | NS |
| Skin quality | 1.6 ± 0.7 | 1.6 ± 0.6 | 1.8 ± 0.9 | NS |
| Scarring | 3.0 ± 0.0 | 3.0 ± 0.0 | 3.0 ± 0.0 | NS |
| Overall | 1.6 ± 0.3 | 1.7 ± 0.3 | 1.6 ± 0.4 | NS |
| Postoperative ± SD | ||||
| Asymmetry | 2.4 ± 0.6 | 2.6 ± 0.4 | 2.1 ± 0.7 | 0.008 |
| Shape | 2.3 ± 0.5 | 2.4 ± 0.4 | 2.1 ± 0.7 | 0.028 |
| NAC contour | 2.5 ± 0.5 | 2.6 ± 0.4 | 2.3 ± 0.5 | NS |
| Skin quality | 2.0 ± 0.6 | 2.0 ± 0.6 | 2.0 ± 0.6 | NS |
| Scarring | 2.4 ± 0.6 | 2.5 ±0.5 | 2.0 ± 0.6 | 0.004 |
| Overall | 2.3 ± 0.3 | 2.4 ± 0.2 | 2.1 ± 0.3 | 0.001 |
| Total difference ± SD (%) | ||||
| Asymmetry | 0.7 ± 0.6 (22) | 0.7 ± 0.6 (24) | NS | |
| Shape | 1.3 ± 0.5 (44) | 1.2 ± 0.5 (41) | NS | |
| NAC contour | 1.8 ± 0.5 (61) | 1.4 ± 0.6 (47) | 0.028 | |
| Skin quality | 0.4 ± 0.5 (13) | 0.2± 0.5 (6) | NS | |
| Scarring | −0.5 ± 0.5 (−16) | −1.1 ± 0.6 (−35) | 0.004 | |
| Overall | 0.8 ± 0.3 (25) | 0.5 ± 0.3 (17) | 0.008 |
NS, not significant.
Fig. 1.
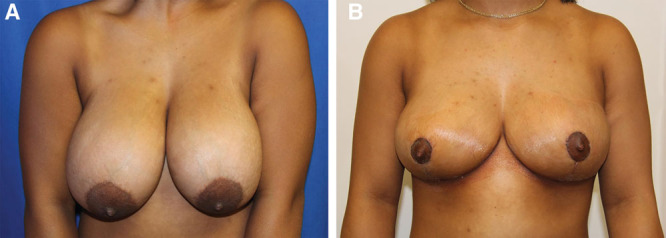
Wise Pattern Reduction. A 15-year-old woman presented with macromastia (A). She underwent a bilateral reduction mammaplasty removing 412.3 g on the right side and 338.8 g on the left side. Her result is shown (B) 1 month after reduction, with improvement in size and shape.
Fig. 2.
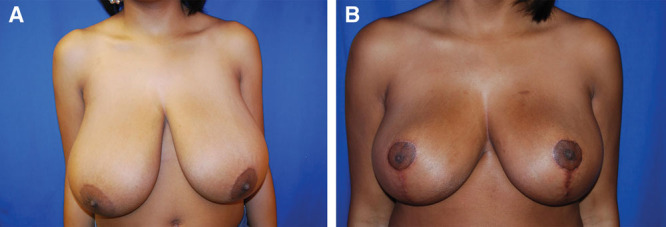
Vertical Pattern Reduction. An 18-year-old woman presented with macromastia (A). She underwent a bilateral reduction mammaplasty removing 885.4 g on the right side and 875.0 g on the left side. Her result is shown (B) 2 months after reduction, with improvement in size and symmetry.
DISCUSSION
Adolescent macromastia, a distressing condition caused by endocrine changes, childhood obesity, and juvenile (virginal) hypertrophy,1 is associated with innumerable physical and psychological ailments ranging from severe back/neck pain and breast tissue necrosis1 to body image distortions and social isolation.2,12 The first-line surgical treatment for symptomatic macromastia is reduction mammaplasty. Adolescents who have undergone bilateral reduction mammaplasty report resolution of pain, higher levels of extroversion, and greater emotional stability.3 Two of the most widely used techniques for this procedure include the Wise and the vertical reduction patterns.13 However, the outcomes of reduction mammaplasty in the adolescent population have been poorly studied2,8, despite reduction mammaplasty becoming increasingly common in young adults.14 Moreover, no studies have directly compared surgical, aesthetic, and patient satisfaction outcomes between Wise and vertical incision patterns in adolescents. Additionally, results in the adult population may not be directly applicable to the adolescent population given anatomical variations, such as greater density of breast parenchyma in younger women.15 This can influence what techniques offer optimal results specifically in the adolescent population.
Current literature has demonstrated complication rates in reduction mammaplasty to range from 7.1% to 53%.3 In the adolescent population, overall complication rates are similar, ranging from 10% to 55% with the most common complications being wound dehiscence and delayed wound healing, infection, seroma, hematoma, and skin/fat/nipple necrosis.1,2,8,16 Complications were comparable in our series and occurred in 23.3% of patients, with the most common being delayed wound healing (11.7%), wound dehiscence (10%), and fat necrosis (3.3%). Literature comparing Wise versus vertical techniques in the adult population has found no significant difference among rates of both major and minor complications between Wise versus vertical patterns.13,15,17,18 Similarly, we found that in the adolescent cohort, there was no significant difference in complication rates between patients undergoing reduction using either pattern and that they were similar to adult complications rates (Wise, 20.4% versus 8%–77.1%13,15,17,18; vertical, 36.4% versus 8%–66.7%13,15,17,18). Although some studies have found increased complications of wound dehiscence and wound healing with the Wise incision pattern due to the greater tension at the T junction19,20, our study found that the occurrence of these minor complications was similar in both groups of adolescents.
A comparison of aesthetic outcomes between the 2 techniques has yielded mixed results in the literature. Although the Wise technique has consistently demonstrated reliable results in management of glandular excess and nipple position21, proponents of the vertical technique advocate that it better preserves breast upper-pole fullness and is associated with a lower inframammary scar burden, lower boxy-shape, and a lower rate of postoperative pseudoptosis.13,21–23 Certain studies have corroborated this by demonstrating better scar aesthetic outcome using vertical pattern in the adult population.17,23,24 However, objective parameters of skin quality, asymmetry, shape, and NAC contour have not been widely evaluated within the literature and have never been compared between Wise and vertical patterns in the adolescent population.1,2,8,25 In our cohort, both Wise and vertical groups showed improvements in all aesthetic outcomes, other than scarring. The deterioration in scarring is to be expected because the preoperative photographs had no scars since they had not undergone a reduction mammaplasty yet. Significant postoperative results included less asymmetry, better shape, less scarring, and higher overall total aesthetic score in Wise pattern patients. Statistically significant improvements between the preoperative and postoperative aesthetic outcomes comparing the 2 techniques included less scarring (Wise = −16%, vertical = −35%, P = 0.004) and greater improvement in NAC contour (Wise = 61%, vertical = 47%, P = 0.028) in the Wise pattern compared with the vertical pattern. Patients undergoing Wise pattern incision also showed significantly greater overall aesthetic improvement than their vertical incision counterparts (Wise = 25%, vertical = 17%, P = 0.008). Although certain studies have demonstrated more optimal maintenance of postoperative breast shape using the vertical incision,13,26 our study indicated better shape preservation with the Wise incision. As Bouwer et al suggests, this may be because the vertical incision pattern relies on pillars of breast tissue that can easily descend after surgery.27 As studies demonstrate, this can result in earlier postoperative bottoming out with the vertical incision, despite longer follow-up times showing eventual better preserved breast projection in the vertical incision.27 Likewise, though the literature traditionally points out Wise as leaving unsightly inframammary scars,13,21–23 our study noted less scarring with the Wise pattern. Our takeaway from this is that when deciding what pattern to use in the adolescent population, it is not necessary to completely rebuff Wise pattern due to its reputation of scarring. In fact, studies have demonstrated that by adjusting certain factors such as tension at the T-point junction, Wise pattern can also result in a minimal scarring rates.19,28 Other studies have alluded to the fact that rather than incision pattern, certain subtleties of the reduction mammaplasty procedure in general determine the level of skin tension on closure.29 These subtleties can include seemingly minor details such as marking by landmark instead of measurement and maintaining thick skin flaps for vascularity; however, they have been shown to greatly influence the outcomes of whichever incision pattern is used, and can explain some of the variation behind trends associated with use of the Wise and vertical patterns.29 With this in mind, we support that surgeon’s preference and comfort with technique are integral to attaining optimal aesthetic results. These factors should be weighed just as heavily as the prevailing literature on aesthetic outcomes when deciding which incision pattern to pursue in the adolescent population.
Patient satisfaction following adolescent reduction mammaplasty is consistently high.2,8,16,30 Lee et al8 reported 82% of patients were satisfied and would recommend the same procedure to a teenage friend, while Xue et al2 reported post-procedure satisfaction as high as 97% using self-reported patient measures. Our study found a similarly high overall satisfaction (74%) using the BREAST-Q questionnaire. Comparing Wise and vertical techniques in the adult population, studies from Cruz-Korchin et al found no significant difference in patient satisfaction between the two.17 Similarly, our study of adolescent counterparts also found no significant difference between the 2 methods in terms of overall patient satisfaction. A significant source of stress during adolescence is caused by perception of oneself and interpersonal relationships.31 It is not surprising that reduction mammaplasty is consistently associated with significant improvements in self body-image and participation in social activities2 leading to such high satisfaction rates in adolescents.
Numerous studies have demonstrated both the physical and psychosocial benefits of reduction mammaplasty in the adolescent population.25,32–34 Our study builds upon these data by quantifying the degree of improvement in aesthetics and quality of life within this population. Characteristics of adolescents that benefit from this procedure are those who present with significant physical or emotional distress. For the adolescents in our study, this meant back/shoulder/chest/neck pain (92%), rash (33%), shoulder grooving (27%), and asymmetry (15%). Psychological characteristics of adolescents who would benefit from this procedure include those with marked social and emotional impairment due to extreme embarrassment, inability to participate in desired activities/sports, unwanted attention from boys, dysfunctional eating behaviors, and problems finding properly fitting clothes.2 The improvement of these physical and emotional factors was confirmed in our study by a significant increase in satisfaction. In fact, 91% of patients stated they either “definitely agreed” or “somewhat agreed” that having surgery changed their lives for the better, with 88% stating they would do it over again if in the same situation again. Advantages of Wise pattern in our study included overall improved aesthetic outcomes, shorter hospital stays, and fewer total number of procedures for adolescent patients. Although studies in the adult population have noted certain aesthetic advantages with use of the vertical pattern,13,20–23 our study noted more disadvantages including less improvement in NAC contour. As both Wise and vertical incision patterns produced similar rates of complications and patient satisfaction in our study, surgeon’s preference and level of comfort with the procedure remains the leading indication for choosing between Wise versus vertical incision pattern.
Limitations of our study include small sample size in vertical incision pattern population (n = 11), variable follow-up times, missing data, and retrospective design of study which may be subject to recall bias of respondents. Future directions of this study include assessing prevalence and quantifying improvement of specific psychological/psychiatric symptoms (depression, anxiety, body image), as well as stratifying outcomes by risk factors (such as body mass index) to assess for confounding factors. Long-term follow-up to assess impact on lactation and changes in breast morphology with age is another source of future analysis.
To conclude, our study shows that relatively low complication rates, along with high rates of patient satisfaction and improvement in aesthetic outcomes, make reduction mammaplasty a well-tolerated and life-improving procedure in adolescents suffering from macromastia. There was no statistical difference in complication or satisfaction rates between both the Wise and vertical reduction patterns; this lack of disparity implies that other factors, including patient preference and surgeon’s comfort in performing the respective procedure, should guide therapeutic decision-making.
ACKNOWLEDGMENT
Approval from the Institutional Review Board at the University of Pittsburgh was obtained prior to conducting this study.
Footnotes
Published online 31 December 2019.
Presented at the 64th Annual Scientific Meeting of the Ivy Society, April 21 2018, Hershey, Pennsylvania; and 61st Annual Meeting of the Ohio Valley Society of Plastic Surgeons, June 1-2 2018, Cleveland, Ohio.
Disclosure: The authors have no financial interest to declare in relation to the content of this article.
REFERENCES
- 1.Koltz PF, Myers RP, Shaw RB, et al. Adolescent breast reduction: indications, techniques, and outcomes. Plast Reconstr Surg. 2011;127:158e–159e. [DOI] [PubMed] [Google Scholar]
- 2.Xue AS, Wolfswinkel EM, Weathers WM, et al. Breast reduction in adolescents: indication, timing, and a review of the literature. J Pediatr Adolesc Gynecol. 2013;26:228–233. [DOI] [PubMed] [Google Scholar]
- 3.Cunningham BL, Gear AJ, Kerrigan CL, et al. Analysis of breast reduction complications derived from the BRAVO study. Plast Reconstr Surg. 2005;115:1597–1604. [DOI] [PubMed] [Google Scholar]
- 4.Chao JD, Memmel HC, Redding JF, et al. Reduction mammaplasty is a functional operation, improving quality of life in symptomatic women: a prospective, single-center breast reduction outcome study. Plast Reconstr Surg. 2002;110:1644–1652; discussion 1653. [DOI] [PubMed] [Google Scholar]
- 5.Spector JA, Karp NS. Reduction mammaplasty: a significant improvement at any size. Plast Reconstr Surg. 2007;120:845–850. [DOI] [PubMed] [Google Scholar]
- 6.Kerrigan CL, Collins ED, Kim HM, et al. Reduction mammaplasty: defining medical necessity. Med Decis Making. 2002;22:208–217. [DOI] [PubMed] [Google Scholar]
- 7.Spector JA, Singh SP, Karp NS. Outcomes after breast reduction: does size really matter? Ann Plast Surg. 2008;60:505–509. [DOI] [PubMed] [Google Scholar]
- 8.Lee MC, Lehman JA, Jr, Tantri MD, et al. Bilateral reduction mammoplasty in an adolescent population: adolescent bilateral reduction mammoplasty. J Craniofac Surg. 2003;14:691–695. [DOI] [PubMed] [Google Scholar]
- 9.Pusic AL, Klassen AF, Scott AM, et al. Development of a new patient-reported outcome measure for breast surgery: the BREAST-Q. Plast Reconstr Surg. 2009;124:345–353. [DOI] [PubMed] [Google Scholar]
- 10.Pusic AL, Klassen A, Cano S. BREAST-Q Reduction/Mastopexy. 2012. qportfolio.org/score-breast-q-reduction-mastopexy/. Accessed April 1, 2019. [Google Scholar]
- 11.Yamashita K. Cosmetic Assessment. J Japan Soc Endoscop Surg. 2004;10:165–170. [Google Scholar]
- 12.Losee JE, Serletti JM, Kreipe RE, et al. Reduction mammaplasty in patients with bulimia nervosa. Ann Plast Surg. 1997;39:443–446. [DOI] [PubMed] [Google Scholar]
- 13.Ogunleye AA, Leroux O, Morrison N, et al. Complications after reduction mammaplasty: a comparison of wise pattern/inferior pedicle and vertical scar/superomedial pedicle. Ann Plast Surg. 2017;79:13–16. [DOI] [PubMed] [Google Scholar]
- 14.Larson K, Gosain AK. Cosmetic surgery in the adolescent patient. Plast Reconstr Surg. 2012;129:135e–141e. [DOI] [PubMed] [Google Scholar]
- 15.Antony AK, Yegiyants SS, Danielson KK, et al. A matched cohort study of superomedial pedicle vertical scar breast reduction (100 breasts) and traditional inferior pedicle wise-pattern reduction (100 breasts): an outcomes study over 3 years. Plast Reconstr Surg. 2013;132:1068–1076. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Webb ML, Cerrato F, Rosen H, et al. The effect of obesity on early outcomes in adolescents undergoing reduction mammaplasty. Ann Plast Surg. 2012;68:257–260. [DOI] [PubMed] [Google Scholar]
- 17.Cruz-Korchin N, Korchin L. Vertical versus wise pattern breast reduction: patient satisfaction, revision rates, and complications. Plast Reconstr Surg. 2003;112:1573–1578; discussion 1579. [DOI] [PubMed] [Google Scholar]
- 18.Kreithen J, Caffee H, Rosenberg J, et al. A comparison of the lejour and wise pattern methods of breast reduction. Ann Plast Surg. 2005;54:236–241; discussion 241. [PubMed] [Google Scholar]
- 19.Khalil HH, Malahias M, Shetty G. Triangular lipodermal flaps in wise pattern reduction mammoplasty (superomedial pedicle): A novel technique to reduce T-junction necrosis. Plast Surg (Oakv). 2016;24:191–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hudson DA, Moodley S. Breast reduction: decreasing complications and improving long-term aesthetic results with parenchymal sutures. Plast Reconstr Surg Glob Open. 2017;5:e1470. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Spear SL, Howard MA. Evolution of the vertical reduction mammaplasty. Plast Reconstr Surg. 2003;112:855–868; quiz 869. [DOI] [PubMed] [Google Scholar]
- 22.Chen CM, White C, Warren SM, et al. Simplifying the vertical reduction mammaplasty. Plast Reconstr Surg. 2004;113:162–172; discussion 173. [DOI] [PubMed] [Google Scholar]
- 23.Hall-Findlay EJ. A simplified vertical reduction mammaplasty: shortening the learning curve. Plast Reconstr Surg. 1999;104:748–759; discussion 760. [PubMed] [Google Scholar]
- 24.Ferreira MC. Evaluation of results in aesthetic plastic surgery: preliminary observations on mammaplasty. Plast Reconstr Surg. 2000;106:1630–1635; discussion 1636. [DOI] [PubMed] [Google Scholar]
- 25.Sharma KS, Lim P, Baines R, et al. Reduction mammaplasty in adolescents: a review of the indications, timing, and outcomes in a regional plastic surgery unit. Eur J Plast Surg. 2014;37:661–666. [Google Scholar]
- 26.Swanson E. Comparison of vertical and inverted-T mammaplasties using photographic measurements. Plast Reconstr Surg Glob Open. 2013;1:e89. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Bouwer LR, van der Biezen JJ, Spronk CA, et al. Vertical scar versus the inverted-T scar reduction mammaplasty: a 10-year follow-up. J Plast Reconstr Aesthet Surg. 2012;65:1298–1304. [DOI] [PubMed] [Google Scholar]
- 28.Chao JW, Taylor EM, Rohde CH. Reducing wound healing complications of wise pattern breast reduction with the inverted “V” modification. J Plast Reconstr Aesthet Surg. 2014;67:421–422. [DOI] [PubMed] [Google Scholar]
- 29.McCulley SJ, Schaverien MV. Superior and superomedial pedicle wise-pattern reduction mammaplasty: maximizing cosmesis and minimizing complications. Ann Plast Surg. 2009;63:128–134. [DOI] [PubMed] [Google Scholar]
- 30.McMahan JD, Wolfe JA, Cromer BA, et al. Lasting success in teenage reduction mammaplasty. Ann Plast Surg. 1995;35:227–231. [DOI] [PubMed] [Google Scholar]
- 31.Bester G. Stress experienced by adolescents in school: the importance of personality and interpersonal relationships. J Child Adolescent Mental Health. 20191–13. [DOI] [PubMed] [Google Scholar]
- 32.Nuzzi LC, et al. The effect of reduction mammaplasty on quality of life in adolescents with macromastia. Pediatrics. 2017;140. [DOI] [PubMed] [Google Scholar]
- 33.Cerrato F, Webb ML, Rosen H, et al. The impact of macromastia on adolescents: a cross-sectional study. Pediatrics. 2012;130:e339–e346. [DOI] [PubMed] [Google Scholar]
- 34.Miller BJ, Morris SF, Sigurdson LL, et al. Prospective study of outcomes after reduction mammaplasty. Plast Reconstr Surg. 2005;115:1025–1031; discussion 1032. [DOI] [PubMed] [Google Scholar]


