Supplemental Digital Content is available in the text
Keywords: Meta-analysis, Osteonecrosis, Femoral head, Hip osteoarthritis, Joint preserving treatments, Transtrochanteric rotational osteotomy, Survival rate
Abstract
Background:
The clinical outcome of transtrochanteric rotational osteotomy (TRO) for osteonecrosis of the femoral head (ONFH) remains controversial, and the promising clinical results of several Japanese studies could not be reproduced in American and European studies. Trying to solve controversies on TRO for ONFH rising from apparently conflicting studies, a meta-analysis was conducted to assess the 5- and 10-year hip survival rates (with conversion to artificial joint replacement and radiographic failure as endpoints) after TRO.
Methods:
All eligible studies were searched in seven comprehensive databases including PubMed, Web of Science, Embase, Cochrane Library, VIP Database, China Knowledge Resource Integrated Database, and Wan Fang Database prior to June 2019. The outcomes evaluated were 5- and 10-year hip survival rates after TRO. The odds ratio and risk difference for the non-comparative binary data with the 95% confidence intervals (CIs) were calculated for each outcome. The included studies were assessed for methodologic bias and potential reasons for heterogeneity were explored.
Results:
Nineteen studies of TRO for ONFH were eligible for this meta-analysis according to inclusion criteria. Based on the previous report, two calculation methods (Methods 1 and 2) were adopted in this meta-analysis. Furthermore, we performed a sub-group analysis of the 5- and 10-year hip survival rates (Method 1) after TRO for ONFH: Asian sub-population and non-Asian sub-population. Taking conversion to artificial joint replacement as the endpoint, 5- and 10-year hip survival rates (Method 1) after TRO for ONFH in the Asian population were 0.86 (95% CI = 0.82–0.89) and 0.72 (95% CI = 0.65–0.78), respectively, and 5- and 10-year hip survival rates after TRO for ONFH in the non-Asian population were 0.55 (95% CI = 0.43–0.67) and 0.42 (95% CI = 0.28–0.55), respectively. The 5- and 10-year hip survival rates (Method 2) after TRO for ONFH were 0.90 (95% CI = 0.79–0.95) and 0.89 (95% CI = 0.81–0.94), respectively. Taking radiographic failure as the endpoint, 5- and 10-year hip survival rates after TRO for ONFH were 0.70 (95% CI = 0.64–0.76) and 0.53 (95% CI = 0.46–0.61), respectively.
Conclusions:
The 5- and 10-year hip survival rates after TRO for ONFH were satisfactory in the Asian population, and were acceptable in the non-Asian population despite high early failure rates.
Introduction
Osteonecrosis of the femoral head (ONFH) is a progressive disease characterized by the death of osteocytes due to a critical reduction in the blood supply of the femoral head.[1,2] Over 8 million patients were diagnosed with ONFH in China in 2017,[3,4] and more than 500,000 hip replacements are performed annually for ONFH patients in the United States.[5] Specifically, ONFH has become a challenge for young adults and active population due to the high incidence of collapse in the femoral head and severe hip pain and dysfunction, which often requires surgical intervention.
Total hip arthroplasty (THA) is the worldwide standard surgical procedure for patients with collapsed ONFH.[6] However, THA is usually associated with poor outcomes in young adults and active population with ONFH, with a high failure rate caused by prosthetic loosening and excessive wear of polyethylene inserts.[7–9] In this regard, hip-preserving surgeries, including non-vascularized or vascularized bone grafting,[10,11] core decompression,[12,13] osteotomy,[14,15] and stem-cell therapy,[16,17] are recommended for young patients with ONFH to postpone THA as long as possible.
Transtrochanteric rotational osteotomy (TRO), which has become one of the hip-preserving alternatives for ONFH, was developed by Sugioka in 1972.[18] The principle of TRO is to replace necrotic bone with healthy bone in weight-bearing area through anterior or posterior rotation after intertrochanteric osteotomy.[18] Therefore, TRO includes two alternative surgical procedures that are classified according to the direction of rotation: anterior rotation osteotomy (ARO) and posterior rotation osteotomy (PRO). In theory, the non-necrotic area is able to prevent further collapse of the femoral head by the presence of the smooth cartilage and normal sub-chondral bone. Previous studies have demonstrated the utility of TRO for different types of symptomatic ONFH with mild or moderate collapse, such as steroid-induced, alcohol-induced, post-traumatic, and idiopathic ONFH.[19–21]
However, the clinical outcome of TRO remains controversial because the promising results of several Japanese studies could not be confirmed by American and European studies.[22–24] On the contrary, TRO was still recommended as an effective joint-preserving surgery for ONFH by the Japanese Orthopaedic Association recently,[25] and a latest meta-analysis demonstrated that the clinical results of future THA were not affected by TRO.[26]
Therefore, we aimed to resolve these controversies by performing a meta-analysis to assess the efficiency of TRO in ONFH. The primary outcomes of interest were 5- and 10-year hip survival rates (with radiographic failure or conversion to THA or hemi-arthroplasty as the endpoint, respectively), as well as Merle d’Aubigne and Postel hip score[23] after TRO.
Methods
Literature search
Electronic search was performed independently by multiple investigators from the date of inception until June 2019. The following databases were used for literature review: PubMed, Web of Science, Embase, Cochrane Library, VIP Database, China Knowledge Resource Integrated Database, and Wan Fang Database. The following search terms were used: (1) “Osteotomy or Transtrochanteric Rotational Osteotomy or TRO or Sugioka's osteotomy”; and (2) “Osteonecrosis or Avascular necrosis or ON or AN and Femur head or Femoral head or FH.” References for the retrieved studies were also checked by the investigators, and duplicate studies were discarded after thorough evaluation.
Selection criteria
Full-text articles were selected according to the following inclusion criteria: (1) observational studies in English or Chinese, including randomized controlled trials (RCTs), case-control, nested case-control, and cohort studies; (2) patients with high confidence of ONFH diagnosis; (3) TRO (ARO or PRO) was used for the treatment ONFH based on the original technique described by Sugioka[18,19]; and (4) the presence of Kaplan-Meier survival curves or some original data in the full-text articles to calculate the 5- or 10-year hip survival rate after surgery, with conversion to THA, hemi-arthroplasty, or radiographic failure as the clinical endpoints.
The articles were excluded according to the following criteria: (1) case reports, reviews, editorials, letters to editors, animal experiments, or surgical techniques; (2) the studies which did not contain the hip survival rate after TRO; (3) the studies followed up for less than 5 years; and (4) the studies which were not for TRO based on the original technique described by Sugioka.
Data extraction
All data were mined using a pre-defined data extraction form that included the following information: (1) the surname of the first author; (2) the year of publication; (3) study methodology; (4) the number of patients; (5) the range of ages; (6) the follow-up time; (7) Kaplan-Meier survival curves hip of hip survival rate after TRO, with conversion to THA, hemi-arthroplasty or radiographic failure as the endpoints; (8) original data in the full-text articles that can be used to calculate the 5- or 10-year hip survival rate after TRO; and (9) the clinical outcomes at the end of the follow-up, including Merle d’Aubigne and Postel hip score (Excellent and good rate).
Data were extracted from survival curves and transformed for meta-analysis according to the method reported by Zhou et al.[27] Corresponding authors were contacted by email if the required information was not available in the included studies. Any disagreements between investigators were resolved by discussion with a third reviewer.
Assessment of risk of bias in the included studies
The methodologic quality of the included studies was assessed using the Newcastle-Ottawa Scale (NOS) for assessing risk of bias (ROB) in case-control and cohort studies[28] and using the Cochrane Collaboration for assessing ROB in RCTs.[29] Any discrepancy between studies was resolved through discussion.
Implementation of meta-analysis with non-comparative binary data
Of the included studies, 15 were cohort studies without control groups, and four were case-control studies with dissimilar control groups. Therefore, the data, including hip survival rate or excellent and good rate after TRO, provided in all the included studies were considered as non-comparative binary variables, and the effect indicator with their standard errors (SEs) were calculated using the two methods reported by Chen et al[30] using the following parameters: P, the hip survival rate or excellent and good rate after TRO; SE; X, the number of hip survival patients or excellent and good rate patients; and n, the total number of patients.
Method 1: when the total number of patients (n) was large enough and both n × P and n × (1 − P) are greater than 5, the following formula was used for calculation:
 |
The meta-analysis with the outcomes was conducted using RevMan software by using risk difference (RD) as the effect index and the Generic Inverse Variance was then selected to calculate the merged effect size.
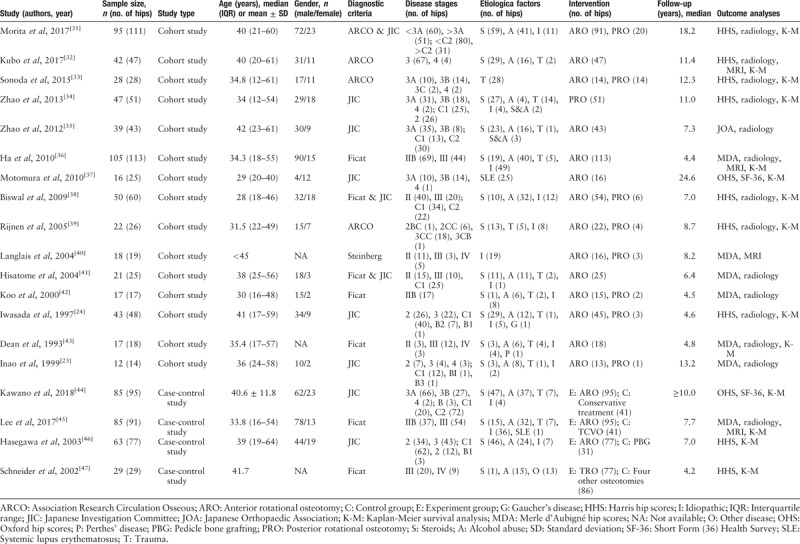
Method 2: when the numbers of hip survival patients or excellent and good patients (X) were 0 or both n × P and n × (1 − P) were less than or equal 5, the following formula was used for the calculation:
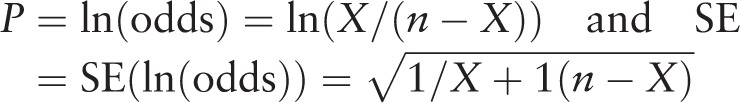 |
The meta-analysis with the outcomes was conducted using RevMan software using odds ratio (OR) as the effect index, and then generic inverse variance was selected to calculate the merged effect size. However, the final pooling rate (Pf) and its 95% confidence interval (CI) were further using the following formulas:
 |
Sensitivity analysis
Where appropriate, a sensitivity analysis was performed by excluding one study at a time to weigh up the relative influence of each individual study on the pooled effect size.
Statistical analysis
Statistical analysis was performed using the Review Manager software (RevMan 5.3, Cochrane Collaboration, London, UK). A statistical cutoff of significance for the overall estimates of effect was set at P < 0.05. The OR and RD for non-comparative binary data (hip survival rate after TRO, excellent, and good rate) with the 95% CIs for each outcome were calculated according to the method reported by Chen et al.[30] Heterogeneity among studies was assessed by I2 using the standard Chi-squared test, and a fixed effects model was used for meta-analysis when a study was identified as statistically homogeneous (P > 0.1 and I2 < 50%). On the contrary, a random-effects model was used for analysis, and the sources of heterogeneity were analyzed, when statistical heterogeneity among studies was identified (P < 0.1, I2 > 50%). The funnel plot was used to assess publication bias, which was identified by an asymmetry in the funnel plot.
Results
Search results
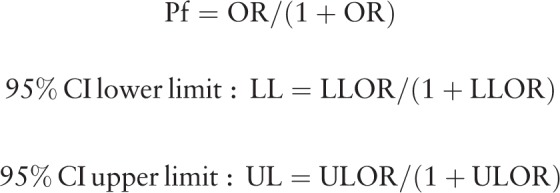
A total of 7045 studies were identified by the preliminary literature search, of which only 5466 duplicate articles were excluded. Of the retained 1579 studies, 1545 were excluded based on the inclusion, and exclusion criteria mentioned in the Methods section. Full-text review of the remaining 34 studies resulted in the selection of a final set of 19 English publications. No extra articles were eligible for inclusion from the references lists in the retained articles. The search and exclusion process are shown in Figure 1.
Figure 1.
Meta-analysis flow chart. CNKI: China national knowledge infrastructure; Embase: Excerpta Medica database; TRO: Transtrochanteric rotational osteotomy; VIP: VIP Database.
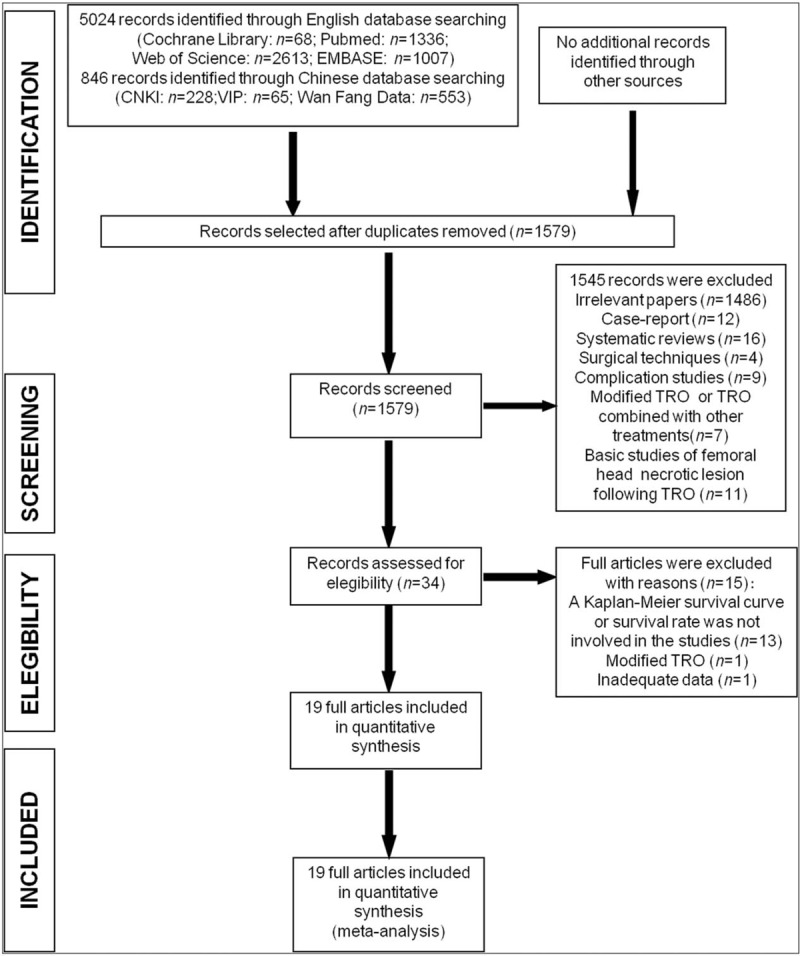
Characteristics of the included studies
Among the 19 selected studies, 4 were retrospective case-control studies and 15 were retrospective cohort studies [Table 1]. Eleven of the 19 included studies were conducted in Japan, 4 were conducted in Korea, and 4 were conducted in non-Asian countries including the United States, the Netherlands, Austria, and France [Table 1].
Table 1.
Characteristics of studies included in the meta-analysis.
Regarding discrepancy in methodologies, a meta-analysis was conducted separately for cohort studies and case-control studies.
Assessment of ROB and methodologic quality of the included studies
The methodologic quality of the included studies was assessed using the NOS. The details of NOS scores are shown in Supplementary Tables 1 and 2. The methodologic quality of the included studies was relatively stable. However, all included studies were retrospective case studies rather than RCTs, which may lead to selection bias, performance bias, and attrition bias.
Hip survival rate after TRO, with conversion to THA or hemi-arthroplasty as the endpoint
A meta-analysis was conducted on the 5- and 10-year hip survival rate after TRO with conversion to THA or hemi-arthroplasty as the endpoint.
Five-year hip survival rate after TRO
Among the articles that reported the 5-year hip survival rate after TRO, with conversion to THA or hemi-arthroplasty as the endpoint, seven cohort studies (395 hips)[24,31,36,38,39,40,43] were eligible for Method 1. Fixed effects model meta-analysis showed heterogeneity between studies (I2 = 79%, P < 0.0001) [Figure 2A]; thus, the sub-group analysis was adopted.
Figure 2.
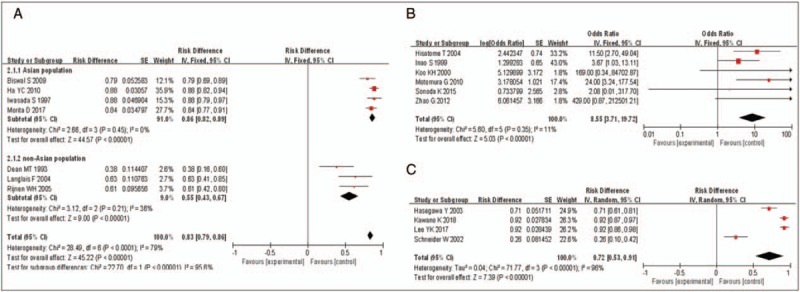
Forest plot showing hip survival rate 5 years after TRO. (A) Forest plot showing hip survival rate (with THA or hemi-arthroplasty as the endpoint) 5 years after TRO (cohort studies, Method 1). (B) Forest plot showing hip survival rate (with THA or hemi-arthroplasty as the endpoint) 5 years after TRO (cohort studies, Method 2). (C) Forest plot showing hip survival rate (with THA or hemi-arthroplasty as the endpoint) 5 years after TRO (case-control studies). CI: Confidence intervals; df: Degrees of freedom; IV: Inverse variance; SE: Standard error; THA: Total-hip arthroplasty; TRO: Transtrochanteric rotational osteotomy.
The population was divided into Asian and non-Asian sub-population due to discrepancy of reports between Asian and non-Asian countries methods. Among the included studies, four were performed on Asian population and three were performed on non-Asian population. In the Asian sub-population, fixed effects model meta-analysis (I2 = 0%, P = 0.45) showed that the hip survival rate in 5 years after TRO was 0.86 (95% CI 0.82–0.89, P < 0.00001) [Figure 2A]. On the contray, fixed effects model meta-analysis (I2 = 36%, P = 0.21) showed that the 5-year hip survival rate after TRO was 0.55 in the non-Asian sub-population (95% CI 0.43–0.67, P < 0.00001) [Figure 2A].
Among the articles that reported the hip survival rate for 5 years after TRO, with THA or hemi-arthroplasty as the endpoint, six cohort studies,[24,33,35,37,41,42] including 152 patients, were eligible for Method 2. Fixed effects model meta-analysis showed significant heterogeneity across studies (I2 = 11%, P = 0.35) [Figure 2B]; therefore, the fixed effects model was adopted. According to the formulas in Method 2, the final pooling of data showed that the 5-year hip survival rate after TRO, with THA or hemi-arthroplasty as the endpoint, was 0.90 (95% CI 0.79–0.95, P < 0.00001) [Figure 2B].
In addition, all the four case-control studies, including 292 patients,[44–47] were eligible for Method 1. Random effects model meta-analysis (I2 = 96%, P < 0.00001) showed that the 5-year hip survival rate after TRO, with THA or hemi-arthroplasty as the endpoint, was 0.72 (95% CI 0.53–0.91, P < 0.00001) [Figure 2C]. Sensitivity analysis showed that the heterogeneity was still significant after omitting the non-Asian study of Schneider et al.[47] These results suggest that the main effects of heterogeneity could be related to small sample size and discrepancy in control groups among studies.
Ten-year hip survival rate after TRO
Among the included studies that reported 10-year hip survival rate after TRO, with THA or hemi-arthroplasty as the endpoint, four cohort studies, including 204 patients[31,38–40] were eligible for Method 1. Fixed-effects model meta-analysis showed that the heterogeneity was significant across studies (I2 = 84%, P = 0.0004) [Figure 3A]; so, the sub-group analysis was adopted.
Figure 3.
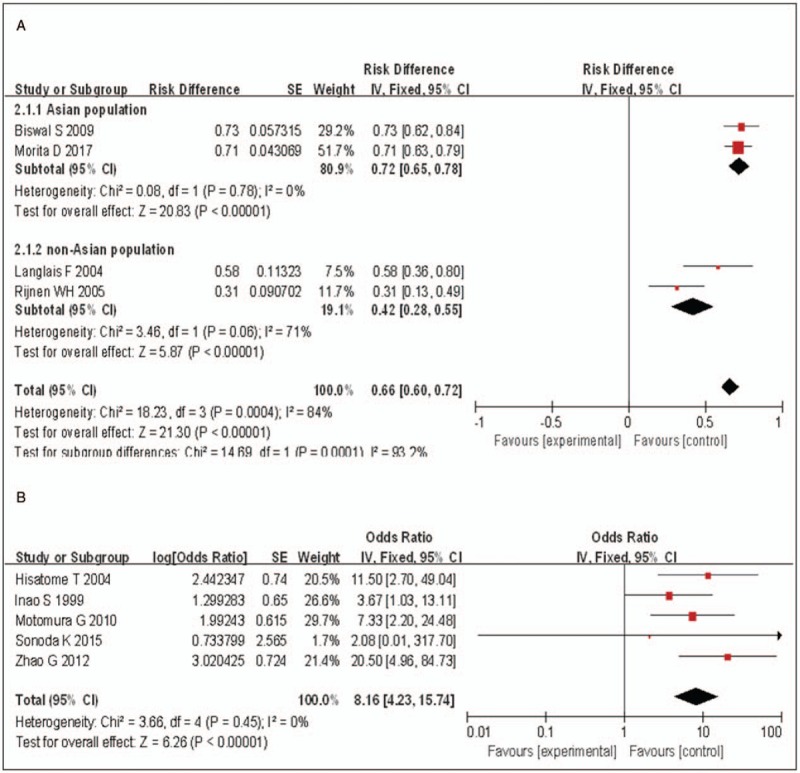
Forest plot showing hip survival rate 10 years after TRO. (A) Forest plot showing hip survival rate (with THA or hemi-arthroplasty as the endpoint) 10 years after TRO (cohort studies, Method 1). (B) Forest plot showing hip survival rate (with THA or hemi-arthroplasty as the endpoint) 10 years after TRO (cohort studies, Method 2). CI: Confidence interval; df: Degrees of freedom; IV: Inverse variance; SE: Standard error; THA: Total-hip arthroplasty; TRO: Transtrochanteric rotational osteotomy.
The population was divided into Asian and non-Asian sub-population. Among the included studies, two were performed on Asian population and two were from non-Asian population. For the Asian sub-population, fixed-effects model meta-analysis (I2 = 0%, P = 0.78) showed that the 10-year hip survival rate after TRO, with THA or hemi-arthroplasty as the endpoint, was 0.72 (95% CI 0.65–0.78, P < 0.00001) [Figure 3A]. For the non-Asian sub-population, fixed-effects model meta-analysis (I2 = 71%, P = 0.06) showed that the 10-year hip survival rate after TRO, with THA or hemi-arthroplasty as the endpoint, was 0.42 (95% CI 0.28–0.55, P < 0.00001) [Figure 3A].
Among the included articles that reported the 10-year hip survival rate after TRO, with THA or hemi-arthroplasty as the endpoint, five cohort studies,[24,33,35,37,41] including 135 patients, was eligible for Method 2. Fixed-effects model meta-analysis showed non-significant heterogeneity across samples (I2 = 0%, P = 0.45) [Figure 3B]; so, the fixed-effects model was adopted. According to the formulas in Method 2, the final pooling of data showed that the 10-year hip survival rate after TRO, with THA or hemi-arthroplasty as the endpoint, was 0.89 (95% CI 0.81–0.94, P < 0.00001).
Hip survival rate after TRO, with radiographic failure as the endpoint
A meta-analysis was then performed to determine the 5- and 10-year hip survival rates after TRO with radiographic failure as the endpoint. Radiographic failure was defined as secondary collapse of the femoral head or osteoarthritic change, including osteophyte formation and joint space narrowing.
Five-year hip survival rate after TRO
Among the studies that reported the 5-year hip survival rate after TRO, with radiographic failure as the endpoint, three cohort studies (206 patients)[24,31,32] were eligible for the Method 1. Fixed-effects model meta-analysis (I2 = 8%, P = 0.34) showed that the 5-year hip survival rate after TRO, with radiographic failure as the endpoint, was 0.70 (95% CI 0.64–0.76, P < 0.00001) [Figure 4A].
Figure 4.
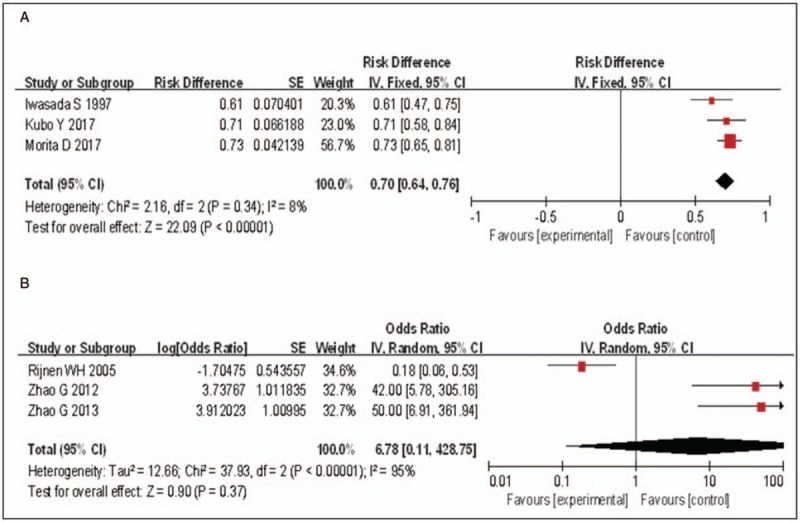
Forest plot showing hip survival rate (with radiographic failure as the endpoint) 5 years after TRO. (A) Forest plot showing hip survival rate (with radiographic failure as the endpoint) 5 years after TRO (cohort studies, Method 1). (B) Forest plot showing hip survival rate (with radiographic failure as the endpoint) 5 years after TRO (cohort studies, Method 2). CI: Confidence intervals; df: Degrees of freedom; IV: Inverse variance; SE: Standard error; TRO: Transtrochanteric rotational osteotomy.
Similarly, three studies,[34,35,39] including 120 patients, that had reported the 5-year hip survival rate after TRO, with radiographic failure as the endpoint, were eligible for the Method 2. Fixed-effects model meta-analysis showed significant that heterogeneity across studies (I2 = 95%, P < 0.00001) [Figure 4B]; thus, the random-effects model was adopted. Despite that sensitivity analysis showed that the heterogeneity originated from the results of Rijnen et al,[39] the other two studies were also performed by the same team.[34,35] Regarding the probability of results bias, we decided to abandon pooling the data.
Ten-year hip survival rate after TRO
Among the included studies that reported the 10-year hip survival rate after TRO, with radiographic failure as the endpoint, only two cohort studies (158 patients)[31,32] were eligible for Method 1. Fixed-effects model meta-analysis (I2 = 40%, P = 0.20) showed that the 10-year hip survival rate after TRO was 0.53 (95% CI 0.46–0.61, P < 0.00001) [Figure 5A], with radiographic failure as the endpoint.
Figure 5.
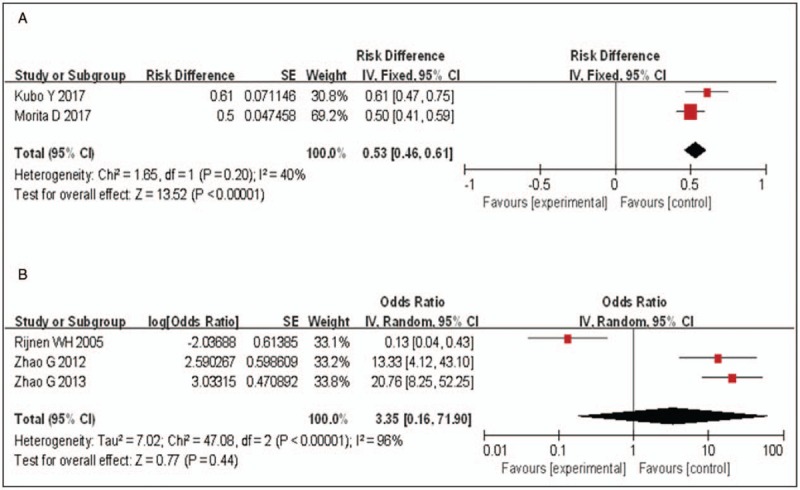
Forest plot showing hip survival rate (with radiographic failure as the endpoint) 10 years after TRO. (A) Forest plot showing hip survival rate (with radiographic failure as the endpoint) 10 years after TRO (cohort studies, Method 1). (B) Forest plot showing hip survival rate (with radiographic failure as the endpoint) 10 years after TRO (cohort studies, Method 2). CI: Confidence intervals; df: Degrees of freedom; IV: Inverse variance; SE: Standard error; TRO: Transtrochanteric rotational osteotomy.
On the contrary, three cohort studies (120 patients)[34,35,39] were eligible for the Method 2, which had reported the 10-year hip survival rate after TRO, with radiographic failure as the endpoint. Fixed effects model meta-analysis showed significant heterogeneity across studies (I2 = 96%, P < 0.00001) [Figure 5B]; so, the random-effects model was adopted. Although sensitivity analysis showed that the heterogeneity originated from the study performed by Rijnen et al,[39] the other two articles were also performed by the same team.[34,35] Regarding the probability of results bias, we decided to abandon pooling the data.
Hip survival rate after TRO and Merle d’Aubigne and Postel hip score
A meta-analysis was conducted to evaluate hip survival rate in patients with excellent and good Merle d’Aubigne and Postel hip scores after TRO. The Merle d’Aubigne and Postel hip score allocates up to 6 points each for pain, mobility and walking ability. Our meta-analysis included patients with excellent (17 or 18 points), good (15 or 16 points), fair (13 or 14 points), and poor (≤12 points) scores.
Among the studies that reported excellent and good scores after TRO at the last follow-up, four cohort studies (171 patients)[23,36,40,41] were eligible for Method 1. Fixed-effects model meta-analysis (I2 = 83%, P = 0.0006) showed that the hip survival rate for excellent and good (Merle d’Aubigne and Postel hip score) at the last follow-up after TRO was 0.66 (95% CI 0.47–0.86, P < 0.00001) [Figure 6].
Figure 6.
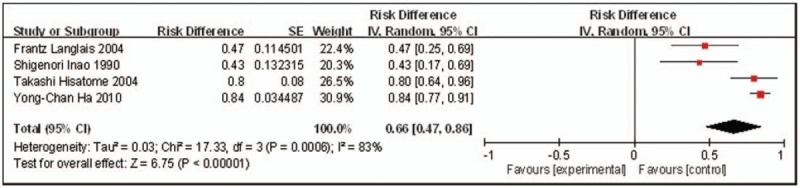
Forest plot showing excellent and good rate after TRO (Merle d’Aubigné hip scores) at the last follow-up (cohort studies, Method 1). CI: Confidence intervals; df: Degrees of freedom; IV: Inverse variance; SE: Standard error; TRO: Transtrochanteric rotational osteotomy.
Discussion
TRO was developed in 1973 by Sugioka[18] as a surgical treatment to relieve the pain, improve the joint function and prevent the progressive collapse of femoral head after osteonecrosis. TRO was divided into two alternative surgical procedures according to the different direction of rotation: ARO and PRO. Decision of ARO or PRO is generally made depending on the location of the necrotic area that is defined using preoperative lateral radiograph of the hip. ARO is usually recommended when the necrotic area in the femoral head is located toward the anterior part of the weight-bearing surface, while PRO is recommended when the necrotic area is located more toward the cranial or posterior part of the weight-bearing surface.[19,20]
In theory, necrotic bone is removed by TRO from the weight-bearing area and is replaced with normal bone that can prevent further collapse of the femoral head. Several reports in Japan and Korea have reported favorable long-term clinical effects of TRO on ONFH by preserving the collapsed femoral head for a longer time.[20–22,24,31,37] In addition, several histologic studies have described new bone or normal bony architecture covering dead trabeculae as a result of fibrous tissue proliferation in the dead trabeculae after TRO, which was accompanied with vascular ingrowth and “creeping substitution” appearance.[48,49]
However, studies from the western countries have reported high failure rates after TRO in the early post-operative period. Indeed, Dean et al[43] reported only 17% satisfactory results of TRO for hips with ONFH during a mean follow-up of 5 years, while 83% of hips showed further collapse of the femoral head. On the contrary, Schneider et al[47] reported a 5-year hip survival probability of 0.26 after Sugioka's osteotomy, and 0.15 after 10 years, which was also associated with a high incidence of complications (55.2%). In addition, Rijnen et al[39] showed that the radiologic survival rate after TRO was only 54% after 1 year. Therefore, multiple studies did not recommend TRO due to the high failure rate. Nevertheless, TRO was recently recommended as an effective joint-preserving surgery for ONFH by the Japanese Orthopaedic Association,[25] and a meta-analysis have recently demonstrated that the clinical outcomes of THA were not affected by TRO.[26]
The inconsistency in the outcomes of TRO could be related to differences in various factors, such as the selection criteria of patients, ethnicity, body mass index of patients, blood supply to the femoral head, pre-operative stage of the necrosis, the extent of necrosis, the method of fixation, the surgical technique, and the post-operative management.[36,50] While the TRO signs reported by Sugioka included relatively widespread necrotic lesions, clinical outcomes of TRO were better in patients with stage II disease than in those with stage III disease.[51] In addition, the incidence of non-union had been decreased by the replacement of the traditional cancellous bone screw fixation with more rigid fixation devices, such as the plate and screw system.[52–54] Furthermore, operative impairment of blood supply to the femoral head and the post-operative intact ratio could be associated with the progressive collapse after TRO. In addition, good intra-operative care should be taken during osteotomy to avoid the impairment of medial femoral circumflex artery, and a post-operative intact ratio should be more than 34% to achieve favorable outcomes.[51,55] Interestingly, the non-Asian countries study by Langlais et al[40] has reported that 47% of patients with ONFH showed favorable outcomes within 10 years after TRO, which underscores the importance of the above factors, especially in Caucasians.
In this regard, we have conducted a meta-analysis to assess the 5- and 10-year hip survival rates after TRO in an attempt to solve the controversies on applying TRO for ONFH treatment that have been raised by the inconsistent results from different studies.
A total of 19 studies on the use of TRO for ONFH treatment were eligible for our meta-analysis according to inclusion criteria. Two calculation methods, Methods 1 and 2, were adopted in this meta-analysis.[30] In addition, sub-group analysis was performed to evaluate the 5- and 10-year hip survival rates (Method 1) after TRO in ONFH patients: Asian sub-population and non-Asian sub-population. By setting the conversion to THA or hemi-arthroplasty as the endpoint, the current meta-analysis showed a higher 5- and 10-year hip survival rates after TRO for ONFH patients in the Asian population, compared with the non-Asian population, regardless the method of calculation used. In comparison, although 5-year hip survival rate after TRO was not satisfactory in non-Asian population, the 10-year outcome was relatively tolerable. Moreover, despite the limited literature, the 5- and 10-year hip survival rates of pooled TRO in ONFH patients were 0.70 and 0.53, respectively, when choosing radiographic failure as the endpoint.
Except for two results, heterogeneity was low in this meta-analysis. One of the two results was from the analysis in four case-control studies on the 5-year hip survival rate after TRO with THA or hemi-arthroplasty as the endpoint. Sensitivity analysis showed that the heterogeneity remained significant after omitting the result of the non-Asian study by Schneider et al.[47] We speculated that the important factors of heterogeneity could be related to the small sample size and to discrepancies in the control groups. The other result was from the analysis of the 5-year hip survival rate after TRO with radiographic failure as the endpoint. Although sensitivity analysis showed that the heterogeneity was originated from the results of Rijnen et al,[39] another two studies were performed by the same authors.[34,35] Regarding the probability of results bias, we decided to abandon pooling the data of the above two results. In addition, we have also conducted a meta-analysis on the excellent and good Merle d’Aubigne and Postel hip scores rates after TRO; however, the heterogeneity was significant. We therefore speculated that the important factors of heterogeneity could be related to the difference in follow-up time. Therefore, we should be cautious in interpreting the pooled results.
Finally, certain limitations in this meta-analysis that may affect the validity of our results should not be ignored. First, the quality of the included studies is not optimal due to the lack of RCTs on TRO, which prevented us from reaching a robust conclusion. Second, we have only included English and Chinese literatures without considering the effect of other studies with different languages on the current results of this meta-analysis, which might cause some sort of bias in the results. Third, the sources of clinical heterogeneity were not considered, including age, body mass index, pre-operative stage and extent of necrosis, the method of fixation, the surgical technique, and the post-operative management. Fourth, the number of patients included in this meta-analysis was relatively small due to the limited number of studies included, which can weaken the statistical analysis validity. Finally, we were unable to detect potential publication bias by funnel plots due to the limited number of included studies.
In conclusion, given the data collected, our findings demonstrate that the 5- and 10-year hip survival rates in ONFH patients after TRO were satisfactory in the Asian population and were relatively acceptable in the non-Asian population despite high early failure rates. Therefore, TRO could be an effective hip-preserving alternative for young patients or active population with symptomatic ONFH when patients are appropriately selected, the surgical procedure is accurately performed, and adequate post-operative rehabilitation is provided. Nevertheless, RCTs with larger sample sizes and that include the different races of Asian and non-Asian population are needed to confirm these results.
Funding
This work was supported by grants from the National Natural Science Foundation of China (No. 81802151); Shandong Province Natural Science Foundation (No. ZR2016HQ05, No. ZR2017BH089, and No. ZR2019MH012); China Postdoctoral Science Foundation (No. 2018M642616); and Qingdao Applied Foundational Research Youth Project (No. 19-6-2-55-cg)
Conflicts of interest
None.
Supplementary Material
Footnotes
How to cite this article: Xu YX, Ren YZ, Zhao ZP, Wang YZ, Wang T, Li T. Hip survival rate in the patients with avascular necrosis of femoral head after transtrochanteric rotational osteotomy: a systematic review and meta-analysis. Chin Med J 2019;132:2960–2971. doi: 10.1097/CM9.0000000000000562
References
- 1.Feng Y, Yang SH, Xiao BJ, Xu WH, Ye SN, Xia T, et al. Decreased in the number and function of circulation endothelial progenitor cells in patients with avascular necrosis of the femoral head. Bone 2010; 46:32–40.. doi: 10.1016/j.bone.2009.09.001. [DOI] [PubMed] [Google Scholar]
- 2.Kamiya N, Yamaguchi R, Aruwajoye O, Adapala NS, Kim HK. Development of a mouse model of ischemic osteonecrosis. Clin Orthop Relat Res 2015; 473:1486–1498.. doi: 10.1007/s11999-015-4172-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Pascart T, Falgayrac G, Migaud H, Quinchon JF, Norberciak L, Budzik JF, et al. Region specific Raman spectroscopy analysis of the femoral head reveals that trabecular bone is unlikely to contribute to non-traumatic osteonecrosis. Sci Rep 2017; 7:97.doi: 10.1038/s41598-017-00162-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zhao DW, Yu M, Hu K, Wang W, Yang L, Wang BJ, et al. Prevalence of nontraumatic osteonecrosis of the femoral head and its associated risk factors in the Chinese population: results from a nationally representative survey. Chin Med J 2015; 128:2843–2850.. doi: 10.4103/0366-6999.168017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mankin HJ. Nontraumatic necrosis of bone (osteonecrosis). N Engl J Med 1992; 326:1473–1479.. doi: 10.1056/NEJM199205283262206. [DOI] [PubMed] [Google Scholar]
- 6.Mont MA, Hungerford DS. Non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Am 1995; 77:459–474.. doi: 10.2106/00004623-199503000-00018. [DOI] [PubMed] [Google Scholar]
- 7.Gardeniers JWM. Treatment of osteonecrosis by joint replacement. Hip Int 1998; 8:159–166.. doi: 10.1177/112070009800800306. [Google Scholar]
- 8.Radl R, Hungerford M, Materna W, Rehak P, Windhager R. High failure rate and stem migration of an uncemented femoral component in patients with femoral head osteonecrosis than in patients with osteoarthrosis. Acta Orthop 2005; 76:49–55.. doi: 10.1080/00016470510030319. [DOI] [PubMed] [Google Scholar]
- 9.Hartley WT, McAuley JP, Culpepper WJ, Engh CA, Jr, Engh CA., Sr Osteonecrosis of the femoral head treated with cementless total hip arthroplasty. J Bone Joint Surg Am 2000; 82:1408–1413.. doi: 10.2106/00004623-200010000-00006. [DOI] [PubMed] [Google Scholar]
- 10.Eisenschenk A, Lautenbach M, Schwetlick G, Weber U. Treatment of femoral head necrosis with vascularized iliac crest transplants. Clin Orthop Relat Res 2001; 386:100–105.. doi: 10.1097/00003086-200105000-00013. [DOI] [PubMed] [Google Scholar]
- 11.Judet H, Gilbert A. Long-term results of free vascularized fibular grafting for femoral head necrosis. Clin Orthop Relat Res 2001; 386:114–119.. doi: 10.1097/00003086-200105000-00015. [DOI] [PubMed] [Google Scholar]
- 12.Mukisi-Mukaza M, Manicom O, Alexis C, Bashoun K, Donkerwolcke M, Burny F, et al. Treatment of sickle cell disease's hip necrosis by core decompression: a prospective case-control study. Orthop Traumatol Surg Res 2009; 95:498–504.. doi: 10.1016/j.otsr.2009.07.009. [DOI] [PubMed] [Google Scholar]
- 13.Rajagopal M, Balch Samora J, Ellis TJ. Efficacy of core decompression as treatment for osteonecrosis of the hip: a systematic review. Hip Int 2012; 22:489–493.. doi: 10.5301/HIP.2012.9748. [DOI] [PubMed] [Google Scholar]
- 14.Mont MA, Fairbank AC, Krackow KA, Hungerford DS, et al. Corrective osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Am 1996; 78:1032–1038.. doi: 10.2106/00004623-199607000-00007. [DOI] [PubMed] [Google Scholar]
- 15.Sakano S, Hasegawa Y, Torii Y, Kawasaki M, Ishiguro N. Curved intertrochanteric varus osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br 2004; 86:359–365.. doi: 10.1302/0301-620x.86b3.14383. [DOI] [PubMed] [Google Scholar]
- 16.Hernigou P, Flouzat-Lachaniette CH, Delambre J, Poignard A, Allain J, Chevallier N, et al. Osteonecrosis repair with bone marrow cell therapies: state of the clinical art. Bone 2015; 70:102–109.. doi: 10.1016/j.bone.2014.04.034. [DOI] [PubMed] [Google Scholar]
- 17.Lau RL, Perruccio AV, Evans HM, Mahomed SR, Mahomed NN, Gandhi R, et al. Stem cell therapy for the treatment of early stage avascular necrosis of the femoral head: a systematic review. BMC Musculoskelet Disord 2014; 15:156.doi: 10.1186/1471-2474-15-156. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sugioka Y. Transtrochanteric anterior rotational osteotomy for the femoral head in the treatment of osteonecrosis affecting the hip: a new osteotomy operation. Clin Orthop Relat Res 1978; 130:191–201.. [PubMed] [Google Scholar]
- 19.Sugioka Y, Katsuki I, Hotokebuchi T. Transtrochanteric rotational osteotomy of the femoral head for the treatment of osteonecrosis. Follow-up statistics. Clin Orthop Relat Res 1982; 169:115–126.. [PubMed] [Google Scholar]
- 20.Ikemura S, Yamamoto T, Nakashima Y, Mawatari T, Motomura G, Iwamoto Y. Transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head in patients 20 years or younger. J Pediatr Orthop 2009; 29:219–223.. doi: 10.1097/BPO.0b013e31819bc746. [DOI] [PubMed] [Google Scholar]
- 21.Atsumi T, Muraki M, Yoshihara S, Kajihara T. Posterior rotational osteotomy for the treatment of femoral head osteonecrosis. Arch Orthop Trauma Surg 1999; 119:388–393.. doi: 10.1007/s004020050435. [DOI] [PubMed] [Google Scholar]
- 22.Belal MA, Reichelt A. Clinical results of rotational osteotomy for treatment of avascular necrosis of the femoral head. Arch Orthop Trauma Surg 1996; 115:80–84.. doi: 10.1007/bf00573446. [DOI] [PubMed] [Google Scholar]
- 23.Inao S, Ando M, Gotoh E, Matsuno T. Minimum 10-year results of Sugioka's osteotomy for femoral head osteonecrosis. Clin Orthop Relat Res 1999; 368:141–148.. [PubMed] [Google Scholar]
- 24.Iwasada S, Hasegawa Y, Iwase T, Kitamura S, Iwata H. Transtrochanteric rotational osteotomy for osteonecrosis of the femoral head 43 patients followed for at least 3 years. Arch Orthop Trauma Surg 1997; 116:447–453.. doi: 10.1007/bf00387576. [DOI] [PubMed] [Google Scholar]
- 25.Kubo T, Ueshima K, Saito M, Ishida M, Arai Y, Fujiwara H. Clinical and basic research on steroid-induced osteonecrosis of the femoral head in Japan. J Orthop Sci 2016; 21:407–413.. doi: 10.1016/j.jos.2016.03.008. [DOI] [PubMed] [Google Scholar]
- 26.Shigemura T, Yamamoto Y, Murata Y, Sato T, Tsuchiya R, Mizuki N, et al. Total hip arthroplasty after failed transtrochanteric rotational osteotomy for osteonecrosis of the femoral head: a systematic review and meta-analysis. Orthop Traumatol Surg Res 2018; 104:1163–1170.. doi: 10.1016/j.otsr.2018.06.019. [DOI] [PubMed] [Google Scholar]
- 27.Zhou ZR, Zhang TS, Li B. Extracting and transforming of appropriate data of Meta-analysis in survival curve (in Chinese). Chin J Evid Based Cardiovasc Med 2014; 6:243–247.. doi: 10.3969/j.1674-4055.2014.03.02. [Google Scholar]
- 28.Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010; 25:603–605.. doi: 10.1007/s10654-010-9491-z. [DOI] [PubMed] [Google Scholar]
- 29. Higgins JP, Green S. Cochrane Handbook for Systematic Reviews of Interventions Version 5.1.0. London: The Cochrane Collaboration, 2011. [Google Scholar]
- 30.Chen YH, Du L, Geng XY, Liu GJ. Implement meta-analysis with non-comparative binary data in RevMan software (in Chinese). Chin J Evid Based Med 2014; 14:889–896.. doi: 10.7507/1672-2531.20140147. [Google Scholar]
- 31.Morita D, Hasegawa Y, Okura T, Osawa Y, Ishiguro N. Long-term outcomes of transtrochanteric rotational osteotomy for non-traumatic osteonecrosis of the femoral head. Bone Joint J 2017; 99-B:175–183.. doi: 10.1302/0301-620X.99B2.BJJ-2016-0417.R2. [DOI] [PubMed] [Google Scholar]
- 32.Kubo Y, Motomura G, Ikemura S, Sonoda K, Yamamoto T, Nakashima Y. Factors influencing progressive collapse of the transposed necrotic lesion after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. Orthop Traumatol Surg Res 2017; 103:217–222.. doi: 10.1016/j.otsr.2016.10.019. [DOI] [PubMed] [Google Scholar]
- 33.Sonoda K, Yamamoto T, Motomura G, Nakashima Y, Yamaguchi R, Iwamoto Y. Outcome of transtrochanteric rotational osteotomy for posttraumatic osteonecrosis of the femoral head with a mean follow-up of 12.3 years. Arch Orthop Trauma Surg 2015; 135:1257–1263.. doi: 10.1007/s00402-015-2282-y. [DOI] [PubMed] [Google Scholar]
- 34.Zhao G, Yamamoto T, Motomura G, Iwasaki K, Yamaguchi R, Ikemura S, et al. Radiological outcome analyses of transtrochanteric posterior rotational osteotomy for osteonecrosis of the femoral head at a mean follow-up of 11 years. J Orthop Sci 2013; 18:277–283.. doi: 10.1007/s00776-012-0347-0. [DOI] [PubMed] [Google Scholar]
- 35.Zhao G, Yamamoto T, Ikemura S, Motomura G, Iwasaki K, Yamaguchi R, et al. Clinico-radiological factors affecting the joint space narrowing after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. J Orthop Sci 2012; 17:390–396.. doi: 10.1007/s00776-012-0238-4. [DOI] [PubMed] [Google Scholar]
- 36.Ha YC, Kim HJ, Kim SY, Kim KC, Lee YK, Koo KH. Effects of age and body mass index on the results of transtrochanteric rotational osteotomy for femoral head osteonecrosis. J Bone Joint Surg Am 2010; 92:314–321.. doi: 10.2106/JBJS.H.01020. [DOI] [PubMed] [Google Scholar]
- 37.Motomura G, Yamamoto T, Suenaga K, Nakashima Y, Mawatari T, Ikemura S, et al. Long-term outcome of transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head in patients with systemic lupus erythematosus. Lupus 2010; 19:860–865.. doi: 10.1177/0961203310361896. [DOI] [PubMed] [Google Scholar]
- 38.Biswal S, Hazra S, Yun HH, Hur CY, Shon WY. Transtrochanteric rotational osteotomy for nontraumatic osteonecrosis of the femoral head in young adults. Clin Orthop Relat Res 2009; 467:1529–1537.. doi: 10.1007/s11999-008-0696-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Rijnen WH, Gardeniers JW, Westrek BL, Buma P, Schreurs BW. Sugioka's osteotomy for femoral-head necrosis in young Caucasians. Int Orthop 2005; 29:140–144.. doi: 10.1007/s00264-005-0639-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Langlais F, Fourastier J, Gédouin JE, Ropars M, Lambotte JC, Thomazeau H. Can rotation osteotomy remain effective for more than ten years? Orthop Clin N Am 2004; 35:345–351.. doi: 10.1016/j.ocl.2004.03.001. [DOI] [PubMed] [Google Scholar]
- 41.Hisatome T, Yasunaga Y, Takahashi K, Ochi M. Progressive collapse of transposed necrotic area after transtrochanteric rotational osteotomy for osteonecrosis of the femoral head induces osteoarthritic change: mid-term results of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. Arch Orthop Trauma Surg 2004; 124:77–81.. doi: 10.1007/s00402-003-0610-0. [DOI] [PubMed] [Google Scholar]
- 42.Koo KH, Song HR, Yang JW, Yang P, Kim JR, Kim YM. Trochanteric rotational osteotomy for osteonecrosis of the femoral head: the use of MRI in the selection of patients. J Bone Joint Surg 2000; 83-B:83–89.. doi: 10.1302/0301-620x.83b1.10914. [DOI] [PubMed] [Google Scholar]
- 43.Dean MT, Cabanel ME. Transtrochanteric anterior rotational osteotomy for avascular necrosis of the femoral head: long-term results. J Bone Joint Surg 1993; 75-B:597–601.. [DOI] [PubMed] [Google Scholar]
- 44.Kawano K, Motomura G, Ikemura S, Kubo Y, Fukushi J, Hamai S, et al. Long-term hip survival and factors influencing patient-reported outcomes after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head: a minimum 10-year follow-up case series. Mod Rheumatol 2018; 17:1–7.. doi: 10.1080/14397595.2018.1558917. [DOI] [PubMed] [Google Scholar]
- 45.Lee YK, Park CH, Ha YC, Kim DY, Lyu SH, Koo KH. Comparison of surgical parameters and results between curved varus osteotomy and rotational osteotomy for osteonecrosis of the femoral head. Clin Orthop Surg 2017; 9:160–168.. doi: 10.4055/cios.2017.9.2.160. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Hasegawa Y, Sakano S, Iwase T, Iwasada S, Torii S, Iwata H. Pedicle bone grafting versus transtrochanteric rotational osteotomy for avascular necrosis of the femoral head. J Bone Joint Surg 2003; 85-B:191–198.. doi: 10.1302/0301-620x.85b2.13190. [DOI] [PubMed] [Google Scholar]
- 47.Schneider W, Aigner N, Pinggera O, Knahr K. Intertrochanteric osteotomy for avascular necrosis of the head of the femur. Survival probability of two different methods. J Bone Joint Surg Br 2002; 84:817–824.. doi: 10.1302/0301-620x.84b6.12837. [DOI] [PubMed] [Google Scholar]
- 48.Yamamoto T, Ikemura S, Iwamoto Y, Sugioka Y. The repair process of osteonecrosis after a transtrochanteric rotational osteotomy. Clin Orthop Relat Res 2010; 468:3186–3191.. doi: 10.1007/s11999-010-1384-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Yasunaga Y, Hisatome T, Ikuta Y, Nakamura S. A histological study of the necrotic area after transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br 2001; 83:167–170.. doi: 10.1302/0301-620x.83b2.11503. [DOI] [PubMed] [Google Scholar]
- 50.Onodera S, Majima T, Abe Y, Ito H, Matsuno T, Minami A. Transtrochanteric rotational osteotomy for osteonecrosis of the femoral head: relation between radiographic features and secondary collapse. J Orthop Sci 2005; 10:367–373.. doi: 10.1007/s00776-005-0906-8. [DOI] [PubMed] [Google Scholar]
- 51.Sugioka Y, Hotokebuchi T, Tsutsui H. Transtrochanteric anterior rotational osteotomy for idiopathic and steroid-induced necrosis of the femoral head. Indications and long-term results. Clin Orthop Relat Res 1992; 277:111–120.. [PubMed] [Google Scholar]
- 52.Sugano N, Takaoka K, Ohzono K, Matsui M, Saito M, Saito S. Rotational osteotomy for non-traumatic avascular necrosis of the femoral head. J Bone Joint Surg Br 1992; 74:734–739.. [DOI] [PubMed] [Google Scholar]
- 53.Ikemura S, Yamamoto T, Jingushi S, Nakashima Y, Mawatari T, Iwamoto Y. Use of a screw and plate system for a transtrochanteric anterior rotational osteotomy for osteonecrosis of the femoral head. J Orthop Sci 2007; 12:260–264.. doi: 10.1007/s00776-007-1123-4. [DOI] [PubMed] [Google Scholar]
- 54.Chen WP, Tai CL, Shih CH, Hsieh PH, Leou MC, Lee MS. Selection of fixation devices in proximal femur rotational osteotomy: clinical complications and finite element analysis. Clin Biomech 2004; 19:255–262.. doi: 10.1016/j.clinbiomech.2003.12.003. [DOI] [PubMed] [Google Scholar]
- 55.Miyanishi K, Noguchi Y, Yamamoto T, Irisa T, Suenaga E, Jingushi S, et al. Prediction of the outcome of transtrochanteric rotational osteotomy for osteonecrosis of the femoral head. J Bone Joint Surg Br 2000; 82:512–516.. doi: 10.1302/0301-620x.82b4.10065. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


