Abstract
Angiogenesis induced by vascular endothelial growth factor A (VEGF-A) plays a critical role in tumor growth and metastasis. The study aimed to evaluate the expression of VEGF-A in gastric adenocarcinoma and investigate its correlations with tumor clinicopathological features and prognostic significance. VEGF-A expression was detected by immunohistochemistry on a tissue microarray containing 90 pairs of human gastric adenocarcinoma and paracancerous tissues. Levels of VEGF-A in gastric adenocarcinoma were significantly higher than those in paracancerous tissues (P=0.018). Furthermore, the result was coincident with that of human gastric adenocarcinoma xenografts in nude-mice (P<0.01). In addition, the VEGF-A expression was positive correlation with TNM stage (P=0.047), tumor size (P=0.028), positive lymph nodes (P=0.002) and lymphovascular invasion (P=0.001). Finally, Kaplan-Meier survival analysis showed that VEGF-A up-regulation indicated a poor prognosis for overall survival (P=0.039). In conclusions, VEGF-A may be used as a biomarker for evaluating both the biological behavior of tumor and the prognosis in patients with gastric adenocarcinoma.
Keywords: Vascular endothelial growth factor, gastric adenocarcinoma, prognosis, biomarker, overall survial
Introduction
Gastric cancer is the fifth most common cancer and the third leading cause of cancer-related deaths globally. An estimated 951,600 new gastric cancer cases and 723,100 deaths occurred in 2012 worldwide [1]. The incidence of gastric cancer is generally about twice as high in men as in women and varies tremendously throughout the world. The highest incidence countries are in Eastern Asia (particularly in Korea, Japan, and China) [2,3]. Gastric adenocarcinoma accounts for the vast majority of gastric cancer cases. Gastric adenocarcinoma clinically has no characteristic manifestations in early stage and further progress to weight loss, epigastric pain or discomfort, anorexia, vomiting and gastrointestinal bleeding. When these symptoms emerge, the cancer has often reached an advanced stage and may also have regional invasion or metastasis. Despite the development in diagnosis and treatment, advanced gastric adenocarcinoma carries a highly unfavorable prognosis, with a 5-year survival rate of about 20%-30% [4]. Therefore, identification of novel biomarkers to estimate prognosis early and correctly may provide useful information for clinical management.
Angiogenesis, the formation of new blood vessels from pre-existing vessels, plays an essential role in invasion and metastasis of various malignancies including gastric adenocarcinoma [5-7]. It is the result of an intricate balance between pro-angiogenic and anti-angiogenic factors. Of the numerous pro-angiogenic factors discovered thus far, vascular endothelial growth factor (VEGF) is one of the most important growth factors related to tumor angiogenesis [8]. The VEGF family is comprised of several secreted proteins, including VEGF-A, -B, -C, -D and placental growth factor [9]. Among them, VEGF-A is a dimeric glycoprotein which plays a significant role in promoting blood vessel dilation and permeability. And VEGF-A is considered to be the main and dominant inducer to the growth of new blood vessels. Recently, increasing evidences suggest up-regulation of VEGF-A in several malignant solid tumors tissues, as well as the elevation of circulating levels of VEGF-A in patients with cancer [10-15].
The impact of VEGF-A expression on prognosis has been demonstrated by meta-analysis in hepatocellular carcinoma [11] and pancreatic cancer [12]. Many studies have evaluated whether up-regulation of VEGF-A may be a prognostic factor for survival in patients with gastric cancer. However, the results of the studies are inconclusive and no consensus has been achieved [16]. In the present study, we detected the expression of VEGF-A in both human gastric adenocarcinoma tissues and in situ xenografts tissues of human gastric carcinoma cells in nude mice, as well as their corresponding paracancerous tissues, respectively. Additionally, we analyzed whether the expression of VEGF-A is correlated with tumor clinicopathological features and clinical outcome in patients with gastric adenocarcinoma.
Materials and methods
The animal experiment was approved by the Animal Use and Care Committee of Sichuan University and conducted according to the regulations.
Tissue microarray (TMA)
Gastric adenocarcinoma TMA implied in the present study was obtained from National Engineering Center for Biochip at Shanghai (Shanghai, China). TMA samples include a total of 90 gastric adenocarcinoma patients who had undergone a complete surgical resection of the gastric tumor between August 2008 and March 2009. Written informed consent forms for the tissue specimens were received from all participants, and the study was approved by the ethical committee of biobank center related hospitals. Detailed clinical and pathologic information of these 90 patients was collected (Table 1). All patients were followed up from the date of surgery until April 2014.
Table 1.
Clinicopathological characteristics of 90 gastric adenocarcinoma cases
| Characteristics | Number of cases | Percentage (%) |
|---|---|---|
| Total | 90 | 100 |
| Average years | 62.1±12.3 | |
| <65 | 52 | 57.8 |
| ≥65 | 38 | 42.2 |
| Gender | ||
| Male | 53 | 58.9 |
| Female | 37 | 41.1 |
| Histologic grade | ||
| I~II | 21 | 23.3 |
| II~III | 69 | 76.7 |
| TNM stage | ||
| I | 9 | 10 |
| II | 27 | 30 |
| III | 50 | 55.6 |
| IV | 4 | 4.4 |
| Tumor size (cm) | 5.7±2.7 | |
| <5 cm | 35 | 38.9 |
| ≥5 cm | 55 | 61.1 |
| Lymphovascular Invasion | 29 | 32.2 |
| Positive lymph nodes | 67 | 74.4 |
| Distant metastasis | 4 | 4.4 |
Cell culture and treatments
Human gastric adenocarcinoma cell SGC7901 was obtained from the Type Culture Collection of the Chinese Academy of Sciences (Shanghai, China). Cells were cultured in RPMI-1640 (HyClone, Logan, UT, USA) supplemented with 10% fetal bovine serum (Gibco, Logan, UT, USA) and 100 U/ml penicillin, 100 U/ml streptomycin (HyClone, Logan, UT, USA) in a humidified atmosphere at 37°C with 5% CO2 in air. SGC7901 cells were trypsinized and resuspended in normal saline when cell density reached 80~90%.
Human gastric cancer xenografts
Ten healthy male BAL b/c nude mice, weighting 18-23 g, were obtained from the Experimental Animal Center of Sichuan University (Chengdu, China). The mice were kept under 12 hours’ light-dark cycles at a constant temperature and humidity with free access to chow and water. Briefly, 1 × 107 of SGC7901 cells were subcutaneously injected into the left flank of 2 nude mice. Tumors were aseptically dissected and mechanically minced after 4 weeks. A piece of tumor (~2 mm3) was transplanted under gastric serosa in each of the rest 8 nude mice and all mice were sacrificed under anesthesia after 4 weeks. Tumor tissues and corresponding paracancerous tissues were fixed in 4% neutral buffered paraformaldehyde for histopathologic and immunohistochemical examinations.
Immunohistochemistry (IHC) and scoring
For IHC, sections of TMA and gastric cancer xenografts were deparaffinized in xylene, rehydrated with graded ethanol dilutions. Antigen retrieval was performed at high temperature under high pressure in 10 mM sodium citrate buffer for 10 minutes. After blocking of endogenous peroxidase activity by H2O2, the sections were incubated with rabbit anti-VEGF-A (1:100, Santa Cruz Biotechnology, Santa Cruz, CA, USA) overnight at 4°C followed by incubation with horseradish peroxidase (HRP)-conjugated secondary antibody kits (ZSGB Bio, Beijing, China) for 30 minutes at room temperature. Finally, sections were stained with a solution of 3,3’-diaminobenzidine tetrahydrochloride and counterstained with hematoxylin. Negative control slides in which the primary antibodies were omitted were included in all assays.
Each slide was assessed independently by two pathologists who were blinded to clinical and pathologic information. The expression of VEGF-A in tissues was scored semi-quantitatively on the basis of positive percentage and intensity of stained preparation as described previously (staining index = positive × intensity score) [17]. The positive percentage of stained tumor cells was scored as: 0, no staining; 1, <20%; 2, 20-75%; 3, >75%. The intensity of stained tumor cells was graded on the following scale: 0, negative; 1, weak; 2, moderate; 3, strong staining. Based on the staining index, a final total score of 0-4 was considered to be low expression of VEGF-A, whereas a total score of 5-9 was defined as high expression.
Statistical analysis
All data were expressed as mean ± standard deviation and were analyzed by SPSS 13.0 software (SPSS, Chicago, IL, USA). Quantitative data were analyzed by using one-way ANOVA. The X2 test was applied to analyze the difference of clinicopathological parameters between low and high VEGF expression groups. Survival curves were evaluated by using the Kaplan-Meier method and compared by the log-rank test. A value of P<0.05 was considered significant.
Results
Patient characteristics
The clinicopathological characteristics of the patients enrolled in this study were summarized in Table 1. The TMA consisted of 90 patients with a diagnosis of gastric adenocarcinoma, among who included 53 males (58.9%) and 37 females (41.1%) with an average age of 62.1±12.3 years-old. In evaluating tumor histologic differentiation, 21 cases (23.3%) were in grade I~II, while the remaining 69 cases (76.7%) were in grade II~III. According to the TNM staging system, 9 (10%) cases were in stage I, 27 (30%) in stage II, 50 (55.6%) in stage III, and 4 (4.4%) in stage IV. The average tumor size was 5.7 cm, with 35 (38.9%) tumors <5 cm and 55 (61.1%) tumors ≥5 cm. Positive lymph nodes and distant metastasis were 67 (74.4%) and 4 (4.4%) of 90 patients, respectively. Lymphovascular invasion was observed in 29 cases (32.2%).
Expression of VEGF-A in gastric adenocarcinoma tissues and corresponding paracancerous tissues
In TMA slide, the positive staining of VEGF-A was mainly located to the cytoplasm in both tumor and paracancerous tissues (Figure 1A). Base on the staining index described above, the expression of VEGF-A in gastric adenocarcinoma tissues was significantly higher in 53 cases, equivalent in 8 cases, and lower in 29 cases, compared with that in corresponding paracancerous tissues (Figure 1B). There was a significant difference in the expression of VEGF-A between human gastric adenocarcinoma tissues and paracancerous tissues (5.0±2.1 vs. 4.3±1.9; P=0.018, Figure 1C). Furthermore, the result was coincident with that of human gastric adenocarcinoma xenografts in node mice, which suggested that stronger expression of VEGF-A was observed in xenografts tissues, compared with that in paracancerous tissues (6.1±1.9 vs. 4.1±1.2; P<0.01, Figure 2). Overall, the levels of VEGF-A were higher in gastric adenocarcinoma tissues than those in paracancerous tissues.
Figure 1.
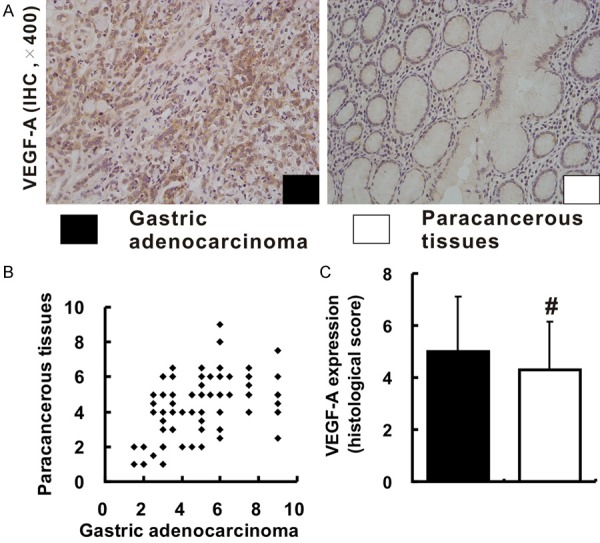
Expression of VEGF-A in human gastric adenocarcinoma tissues and paracancerous tissues. A. Shows the immunohistochemical staining of VEGF-A expression in human gastric adenocarcinoma tissues and paracancerous tissues (all images were taken at 400 × magnification). B and C. Reveal the differences in expression levels of VEGF-A in tumor tissues and paracancerous tissues based on the histological score.
Figure 2.
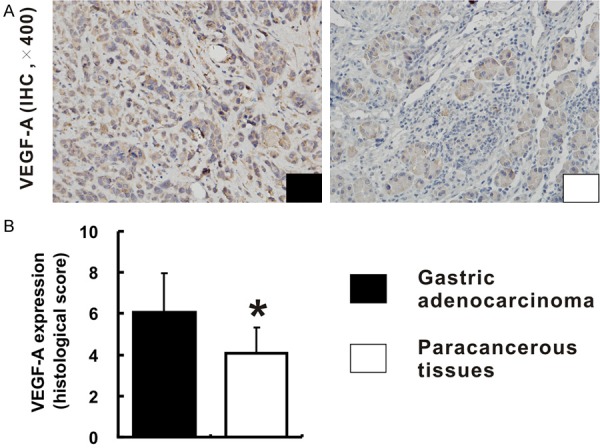
Expression of VEGF-A in human gastric adenocarcinoma xenografts tissues and paracancerous tissues. A. Shows the immunohistochemical staining of VEGF-A expression in human gastric adenocarcinoma xenografts tissues and paracancerous tissues in nude mice (400 × magnification). B. Reveals the differences in expression levels of VEGF-A in xenografts tissues and paracancerous tissues based on the histological score.
Correlation between the VEGF-A expression and the clinicopathological features in gastric adenocarcinoma
Among 90 gastric adenocarcinoma patients, 41 (45.6%) cases were identified as low VEGF-A expression group, and 49 (54.4%) cases as high VEGF-A expression group. The relationships between the expression of VEGF-A and clinicopathological features were analyzed (Table 2). A significantly positive correlation was observed between VEGF-A expression and TNM stage (P=0.047, Figure 3 and Table 2). The rate of patients with TNM stage I~II was higher in low VEGF-A expression group (51.2%) than that in high VEGF-A expression group (30.6%). Whereas, the rate of patients with TNM stage III~IV was lower in low VEGF-A expression group than that in high VEGF-A expression group (48.8% vs. 69.4%). Besides, the expression of VEGF-A was significantly associated with tumor size (P=0.028). The rate of patients with tumor size ≥5 cm was lower in low VEGF-A expression group compared with that in high VEGF-A expression group (48.8% vs. 71.4%). Furthermore, high VEGF-A expression increased the risk of positive lymph nodes (P=0.002) and lymphovascular invasion (P=0.001). However, the results showed that there was no significant correlation between the expression of VEGF-A and other clinicopathological factors, including age, gender, histologic grade, and distant metastasis (P>0.05, Table 2).
Table 2.
Relationships between VEGF-A expression and clinicopathological characteristics in 90 gastric adenocarcinoma cases
| Characteristics | VEGF expression (%) | p value | |
|---|---|---|---|
|
| |||
| Low | High | ||
| Total | 41 | 49 | |
| Average years | 62.8±12.3 | 61.6±12.4 | |
| <65 | 22 (53.7) | 30 (61.2) | 0.469 |
| ≥65 | 19 (46.3) | 19 (38.8) | |
| Gender | |||
| Male | 24 (58.5) | 29 (59.2) | 0.95 |
| Female | 17 (41.5) | 20 (40.8) | |
| Histologic grade | |||
| I~II | 12 (29.3) | 9(18.4) | 0.223 |
| II~III | 29 (70.7) | 40 (81.6) | |
| TNM stage | |||
| I-II | 21 (51.2) | 15 (30.6) | 0.047 |
| III-IV | 20 (48.8) | 34 (69.4) | |
| Tumor size (cm) | 4.8±1.7 | 6.5±3.1 | |
| <5 cm | 21 (51.2) | 14 (28.6) | 0.028 |
| ≥5 cm | 20 (48.8) | 35 (71.4) | |
| Lymphovascular Invasion | 6 (14.6) | 23 (46.9) | 0.001 |
| Positive lymph nodes | 24 (58.5) | 43 (87.8) | 0.002 |
| Distant metastasis | 2 (4.9) | 2 (4.1) | 0.855 |
Figure 3.
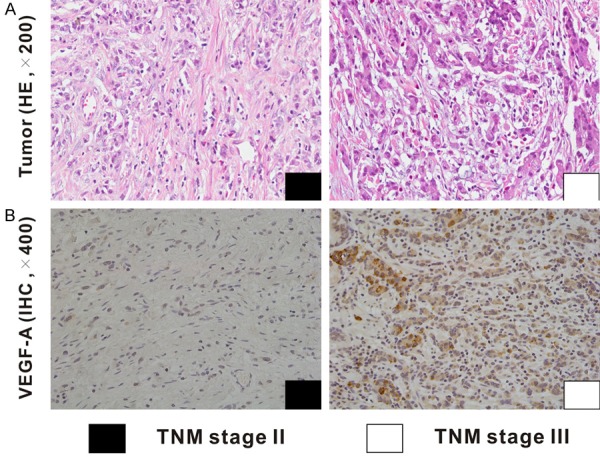
Correlation between the VEGF-A expression and the TNM stage in human gastric adenocarcinoma. Representing images for HE and IHC of VEGF-A in gastric adenocarcinoma patients with TNM stage II and III are shown.
Survival analysis
The survival analysis showed that the 5-years survival rate of patients was 36.7%. The median overall survival was 24 months. The median survival time was 53 months for low VEGF-A expression group and 21 months for high VEGF-A expression group. In addition, the 5-year survival rates were 54.1% and 24.5% in patients with low-expression and high-expression of VEGF-A, respectively. A significant association between VEGF-A expression and tumor prognosis in human gastric adenocarcinoma had been established. Patients with low expression levels of VEGF-A achieved better survival than patients with high expression levels of VEGF-A (P=0.039, Figure 4).
Figure 4.
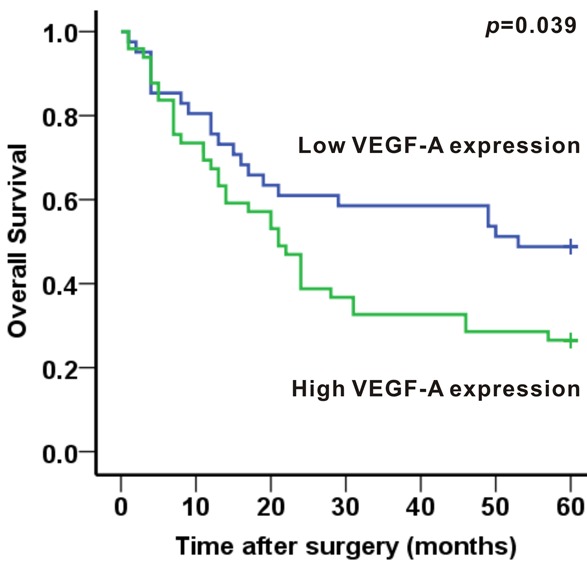
Association between VEGF-A expression and 5-year overall survival in human gastric adenocarcinoma. Patients with low expression levels of VEGF-A achieved better survival than patients with high expression levels of VEGF-A (P<0.05).
Discussion
Angiogenesis, which induced by VEGF and its receptor (VEGFR), plays a critical role in tumor growth and metastasis. VEGF-A, also referred to as VEGF, is the best characterized and the most frequently studied subtype of the VEGF family during the past decades [18]. Up-expression of VEGF-A has been observed in numerous solid tumor tissues [8], including gastric adenocarcinoma. Shi [19] conducted a retrospective study of 232 gastric adenocarcinoma tissues and 60 noncancerous tissues, which showed that compared with paired noncancerous tissues, expression of VEGF-A and microvessel density in carcinoma tissues were obviously increased. Yang [14] reported VEGF-A expression in gastric carcinoma tissues was significantly higher than that in normal gastric mucosal tissues with distance >5 cm from the tumor margin. Furthermore, recent researches [15,20] have suggested the VEGF-A levels in serum were significantly increased preoperatively in gastric cancer patients, compared with apparently healthy volunteers. In this study, we detected the expression of VEGF-A by IHC method in gastric adenocarcinoma tissues and paracancerous tissues in both TMA and nude-mice xenografts. According to the semi-quantitatively method, the levels of VEGF-A expression in adenocarcinoma tissues were higher than that in paracancerous tissues, indicating the correlation between VEGF-A expression and tumor biological behavior in gastric adenocarcinoma.
In the past few years, efforts have been made to investigate the correlation of VEGF-A expression with clinicopathological features in gastric adenocarcinoma. Yang [14] found expression rates for VEGF-A were significantly positively related to the TNM stage, tumor size, depth of invasion, lymph node metastasis and pathological stage. One study [21] showed VEGF-A positivity was much more prevalent for patients with vessel invasion, hepatic, and peritoneal metastasis. However, Liu’s study [22] suggested no correlation between VEGF-A expression and tumor size, T stage, or vascular invasion in patients with pN0 gastric carcinoma. In the present study, we examined 90 gastric adenocarcinoma samples for the expression of VEGF-A by IHC. In all, 41 (45.6%) cases showed low VEGF-A expression and 49 (54.4%) cases showed high VEGF-A expression. Further analyses revealed that VEGF-A expression was related to clinicopathological features of gastric adenocarcinoma including TNM stage, tumor size, positive lymph nodes and lymphovascular invasion. High expression of VEGF-A was accompanied by elevated TNM stage and tumor size, as well as increased the risk of lymphovascular invasion and positive lymph nodes. These results suggest that VEGF-A plays an essential role in tumor growth, regional invasion and lymphatic metastasis.
VEGF-A and its receptors regulate tumor biological behavior through angiogenesis pathway [23]. VEGF-A exerts its effects primarily through transmembrane tyrosine kinase receptors, VEGFR-1 and VEGFR-2. When binding to the extracellular domain of the receptor, a cascade of downstream proteins is activated after phosphorylation of the intracellular receptor tyrosine kinases. This process stimulates neovascularisation by promoting endothelial cell proliferation and migration. The newborn vessels can supply nutrition oxygen for tumors and discharge the metabolic wastes, which stimulate the growth of tumor and provide vascular pathway for tumor metastasis. The biological processes provide the reliable basis for the explanation of the relationship between VEGF-A expression and tumor size as well as vascular invasion and metastasis. The lack of correlation between VEGF-A expression and distant metastasis in this study may attribute to the limited distant metastasis cases (4 cases). Lymph node metastasis often represents the first step in the metastasis process of gastric carcinoma. The exact mechanism that VEGF-A promotes lymph node metastasis has still not been elucidated, but it’s conceivable that VEGF-A may induce angiogenesis in the lymph nodes, improve interstitial fluid pressure by increasing vascular permeability [24] and induce the synthesis of VEGF-C [25], which considered to be the driver for lymphangiogenesis. The characteristics of VEGF-A make it an ideal biomarker for evaluating the biological behavior in gastric adenocarcinoma.
The value of VEGF-A expression as an independent prognostic indicator has been evaluated by numerous studies [26-29]. However, these studies have shown conflicting and opposite results and no consensus has been reached. Recently, an extensive meta-analysis [16] has been published showing VEGF-A up-expression indicates a poor prognosis for overall survival and disease-free survival in patients with gastric carcinoma. In this study, we also confirmed a significant prognostic value of VEGF-A in gastric adenocarcinoma using a Kaplan-Meier survival analysis. Patients with low expression levels of VEGF-A achieved better survival than patients with high expression levels of VEGF-A. The current TNM staging system has some restrictions for the evaluation of the prognosis in gastric carcinoma patients with identical clinical or pathological stages may differ widely in their clinical evolution. Thus, detecting VEGF-A expression in gastric carcinoma tissues might be helpful for predicting patient prognosis. Inhibition of VEGF-A pathway can effectively suppress tumor angiogenesis in vitro and in vivo [30]. Monoclonal antibodies or receptor tyrosine kinase inhibitors with anti-VEGF-A activity are in clinical trials or are currently approved by the United States Food and Drug Administration. The above medicines have been prove to improved progression-free or overall survival in patients with metastatic colorectal cancer, metastatic breast cancer, and metastatic non-squamous non-small-cell lung cancer combined with chemotherapeutic drugs [31]. Several phase II [32,33] or III [34] clinical trials conducted to evaluate therapies targeting the VEGF-A pathway have shown benefits in certain patients with advanced gastric carcinoma from the addition of bevacizumab to chemotherapy. Nevertheless, further researches will be needed to identify eligible patients to receive therapies targeting the VEGF-A pathway and the ideal time window to initiate this target therapy.
For the questionable methods used in the single slide IHC and the staining quantitative analysis, it was suggested that the tissue expression of VEGF-A alone is not an independent prognostic marker for patients with gastric carcinoma [27]. In general, experiments of different batches may attribute to the differences in the staining degree even in the same slide. The inconclusive results may also come from subjective qualitative visual evaluation and differences experience of pathologists. To avoid disadvantages described above, gastric adenocarcinoma TMA was implied in the present study to ensure the synchronicity of the immunohistochemistry staining. Additionally, in order to minimize artificial factors, two experienced pathologists who were blinded to patient information assessed each slide independently by using a semi-quantitatively scoring system.
In conclusion, the present study showed that VEGF-A expression was significantly up-regulated in gastric adenocarcinoma tissues. Meanwhile, the expression of VEGF-A was intimately relevant to clinicopathological features including TNM stage, tumor size, positive lymph nodes and lymphovascular invasion. This study also indicated that the VEGF-A up-expression was significantly correlated with poor survival. Therefore, VEGF-A may be of use as a biomarker for evaluating both the biological behavior of tumor and the prognosis in patients with gastric adenocarcinoma.
Acknowledgements
This study is supported by the National Natural Science Foundation of China (81670551 and 81400637), the Chinesisch-Deutsches Zentrum fṻr Wissenschaftsfὅrderung (GZ1065) and the Science and Technology Support Program of Sichuan province (2016SZ0041).
Disclosure of conflict of interest
None.
References
- 1.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 2.Bertuccio P, Chatenoud L, Levi F, Praud D, Ferlay J, Negri E, Malvezzi M, La Vecchia C. Recent patterns in gastric cancer: a global overview. Int J Cancer. 2009;125:666–673. doi: 10.1002/ijc.24290. [DOI] [PubMed] [Google Scholar]
- 3.Rahman R, Asombang AW, Ibdah JA. Characteristics of gastric cancer in Asia. World J Gastroenterol. 2014;20:4483–4490. doi: 10.3748/wjg.v20.i16.4483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Fang WL, Huang KH, Chen JH, Lo SS, Hsieh MC, Shen KH, Li AF, Niu DM, Chiou SH, Wu CW. Comparison of the survival difference between AJCC 6th and 7th editions for gastric cancer patients. World J Surg. 2011;35:2723–2729. doi: 10.1007/s00268-011-1275-4. [DOI] [PubMed] [Google Scholar]
- 5.Carmeliet P, Jain RK. Molecular mechanisms and clinical applications of angiogenesis. Nature. 2011;473:298–307. doi: 10.1038/nature10144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ilson DH. Angiogenesis in gastric cancer: hitting the target? Lancet. 2014;383:4–6. doi: 10.1016/S0140-6736(13)61892-9. [DOI] [PubMed] [Google Scholar]
- 7.Javle M, Smyth EC, Chau I. Ramucirumab: successfully targeting angiogenesis in gastric cancer. Clin Cancer Res. 2014;20:5875–5881. doi: 10.1158/1078-0432.CCR-14-1071. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Ferrara N, Gerber HP, LeCouter J. The biology of VEGF and its receptors. Nat Med. 2003;9:669–676. doi: 10.1038/nm0603-669. [DOI] [PubMed] [Google Scholar]
- 9.Holmes DI, Zachary I. The vascular endothelial growth factor (VEGF) family: angiogenic factors in health and disease. Genome Biol. 2005;6:209. doi: 10.1186/gb-2005-6-2-209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Dvorak HF. Vascular permeability factor/vascular endothelial growth factor: a critical cytokine in tumor angiogenesis and a potential target for diagnosis and therapy. J. Clin. Oncol. 2002;20:4368–4380. doi: 10.1200/JCO.2002.10.088. [DOI] [PubMed] [Google Scholar]
- 11.Schoenleber SJ, Kurtz DM, Talwalkar JA, Roberts LR, Gores GJ. Prognostic role of vascular endothelial growth factor in hepatocellular carcinoma: systematic review and meta-analysis. Br J Cancer. 2009;100:1385–1392. doi: 10.1038/sj.bjc.6605017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Smith RA, Tang J, Tudur-Smith C, Neoptolemos JP, Ghaneh P. Meta-analysis of immunohistochemical prognostic markers in resected pancreatic cancer. Br J Cancer. 2011;104:1440–1451. doi: 10.1038/bjc.2011.110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wang X, Chen X, Fang J, Yang C. Overexpression of both VEGF-A and VEGF-C in gastric cancer correlates with prognosis, and silencing of both is effective to inhibit cancer growth. Int J Clin Exp Pathol. 2013;6:586–597. [PMC free article] [PubMed] [Google Scholar]
- 14.Yang S, Zhao Z, Wu R, Lu H, Zhang X, Huan C, Wang C, Wu X, Guan G. Expression and biological relationship of vascular endothelial growth factor-A and matrix metalloproteinase-9 in gastric carcinoma. J Int Med Res. 2011;39:2076–2085. doi: 10.1177/147323001103900603. [DOI] [PubMed] [Google Scholar]
- 15.Halmaciu I, Gurzu S, Dobreanu M, Suciu BA, Brinzaniuc K. [Preliminary results regarding vascular endothelial growth factor (VEGF-A) levels in the serum of gastric cancer patients] . Rev Med Chir Soc Med Nat Iasi. 2012;116:446–451. [PubMed] [Google Scholar]
- 16.Ji YN, Wang Q, Li Y, Wang Z. Prognostic value of vascular endothelial growth factor a expression in gastric cancer: a meta-analysis. Tumour Biol. 2014;35:2787–2793. doi: 10.1007/s13277-013-1371-1. [DOI] [PubMed] [Google Scholar]
- 17.Ohuchida K, Mizumoto K, Ishikawa N, Fujii K, Konomi H, Nagai E, Yamaguchi K, Tsuneyoshi M, Tanaka M. The role of S100A6 in pancreatic cancer development and its clinical implication as a diagnostic marker and therapeutic target. Clin Cancer Res. 2005;11:7785–7793. doi: 10.1158/1078-0432.CCR-05-0714. [DOI] [PubMed] [Google Scholar]
- 18.Otrock ZK, Makarem JA, Shamseddine AI. Vascular endothelial growth factor family of ligands and receptors: review. Blood Cells Mol Dis. 2007;38:258–268. doi: 10.1016/j.bcmd.2006.12.003. [DOI] [PubMed] [Google Scholar]
- 19.Shi H, Xu JM, Hu NZ, Xie HJ. Prognostic significance of expression of cyclooxygenase-2 and vascular endothelial growth factor in human gastric carcinoma. World J Gastroenterol. 2003;9:1421–1426. doi: 10.3748/wjg.v9.i7.1421. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Al-Moundhri MS, Al-Shukaili A, Al-Nabhani M, Al-Bahrani B, Burney IA, Rizivi A, Ganguly SS. Measurement of circulating levels of VEGF-A, -C, and -D and their receptors, VEGFR-1 and -2 in gastric adenocarcinoma. World J Gastroenterol. 2008;14:3879–3883. doi: 10.3748/wjg.14.3879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Yang Q, Ye ZY, Zhang JX, Tao HQ, Li SG, Zhao ZS. Expression of matrix metalloproteinase-9 mRNA and vascular endothelial growth factor protein in gastric carcinoma and its relationship to its pathological features and prognosis. Anat Rec (Hoboken) 2010;293:2012–2019. doi: 10.1002/ar.21071. [DOI] [PubMed] [Google Scholar]
- 22.Liu YF, Guo S, Zhao R, Chen YG, Wang XQ, Xu KS. Correlation of vascular endothelial growth factor expression with tumor recurrence and poor prognosis in patients with pN0 gastric cancer. World J Surg. 2012;36:109–117. doi: 10.1007/s00268-011-1192-6. [DOI] [PubMed] [Google Scholar]
- 23.Abdel-Rahman O. Targeting vascular endothelial growth factor (VEGF) pathway in gastric cancer: preclinical and clinical aspects. Crit Rev Oncol Hematol. 2015;93:18–27. doi: 10.1016/j.critrevonc.2014.05.012. [DOI] [PubMed] [Google Scholar]
- 24.Kondo K, Kaneko T, Baba M, Konno H. VEGF-C and VEGF-A synergistically enhance lymph node metastasis of gastric cancer. Biol Pharm Bull. 2007;30:633–637. doi: 10.1248/bpb.30.633. [DOI] [PubMed] [Google Scholar]
- 25.Ding S, Li C, Lin S, Han Y, Yang Y, Zhang Y, Li L, Zhou L, Kumar S. Distinct roles of VEGF-A and VEGF-C in tumour metastasis of gastric carcinoma. Oncol Rep. 2007;17:369–375. [PubMed] [Google Scholar]
- 26.Vidal O, Soriano-Izquierdo A, Pera M, Elizalde JI, Palacin A, Castells A, Pique JM, Volant A, Metges JP. Positive VEGF immunostaining independently predicts poor prognosis in curatively resected gastric cancer patients: results of a study assessing a panel of angiogenic markers. J Gastrointest Surg. 2008;12:1005–1014. doi: 10.1007/s11605-007-0336-3. [DOI] [PubMed] [Google Scholar]
- 27.Lee SJ, Kim JG, Sohn SK, Chae YS, Moon JH, Kim SN, Bae HI, Chung HY, Yu W. No association of vascular endothelial growth factor-A (VEGF-A) and VEGF-C expression with survival in patients with gastric cancer. Cancer Res Treat. 2009;41:218–223. doi: 10.4143/crt.2009.41.4.218. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Suzuki S, Dobashi Y, Hatakeyama Y, Tajiri R, Fujimura T, Heldin CH, Ooi A. Clinicopathological significance of platelet-derived growth factor (PDGF)-B and vascular endothelial growth factor-A expression, PDGF receptor-beta phosphorylation, and microvessel density in gastric cancer. BMC Cancer. 2010;10:659. doi: 10.1186/1471-2407-10-659. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Lastraioli E, Boni L, Romoli MR, Crescioli S, Taddei A, Beghelli S, Tomezzoli A, Vindigni C, Saragoni L, Messerini L, Bernini M, Bencini L, Giommoni E, Freschi G, Di Costanzo F, Scarpa A, Morgagni P, Farsi M, Roviello F, De Manzoni G, Bechi P, Arcangeli A Gruppo Italiano di Ricerca Cancro Gastrico (GIRCG) VEGF-A clinical significance in gastric cancers: immunohistochemical analysis of a wide Italian cohort. Eur J Surg Oncol. 2014;40:1291–1298. doi: 10.1016/j.ejso.2014.03.028. [DOI] [PubMed] [Google Scholar]
- 30.Jain RK. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science. 2005;307:58–62. doi: 10.1126/science.1104819. [DOI] [PubMed] [Google Scholar]
- 31.Lyseng-Williamson KA, Robinson DM. Spotlight on bevacizumab in advanced colorectal cancer, breast cancer, and non-small cell lung cancer. Bio Drugs. 2006;20:193–195. doi: 10.2165/00063030-200620030-00007. [DOI] [PubMed] [Google Scholar]
- 32.Shah MA, Jhawer M, Ilson DH, Lefkowitz RA, Robinson E, Capanu M, Kelsen DP. Phase II study of modified docetaxel, cisplatin, and fluorouracil with bevacizumab in patients with metastatic gastroesophageal adenocarcinoma. J. Clin. Oncol. 2011;29:868–874. doi: 10.1200/JCO.2010.32.0770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.El-Rayes BF, Zalupski M, Bekai-Saab T, Heilbrun LK, Hammad N, Patel B, Urba S, Shields AF, Vaishampayan U, Dawson S, Almhanna K, Smith D, Philip PA. A phase II study of bevacizumab, oxaliplatin, and docetaxel in locally advanced and metastatic gastric and gastroesophageal junction cancers. Ann Oncol. 2010;21:1999–2004. doi: 10.1093/annonc/mdq065. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Ohtsu A, Shah MA, Van Cutsem E, Rha SY, Sawaki A, Park SR, Lim HY, Yamada Y, Wu J, Langer B, Starnawski M, Kang YK. Bevacizumab in combination with chemotherapy as firstline therapy in advanced gastric cancer: a randomized, double-blind, placebo-controlled phase III study. J. Clin. Oncol. 2011;29:3968–3976. doi: 10.1200/JCO.2011.36.2236. [DOI] [PubMed] [Google Scholar]


