Abstract
Ectopic thyroid tissue (ETT) was usually discovered in head and neck region, adrenal ETT was rare reported in literature. Here is a report of adrenal gland cyst with ETT in a 49-year old woman who was admitted to our hospital for health care. CT scan demonstrated a mass in left adrenal gland, and surgical resection was prepared. The mass was cystic, composed of normal adrenal and ectopic thyroid tissue, and was histologically benign. Immnunohistochemistry showed that the ETT was positive for TG and TTF-1, molecular examination indicated that ETT was without the molecular alterations associated with thyroid carcinoma (BRAF V600E, K-RAS). Further work-up did not show evidence of thyroid malignancy.
Keywords: Ectopic thyroid tissue, adrenal gland, immnunohistochemistry, gene mutation
Introduction
The thyroid gland develops embryologically from an evagination of the developing pharyngeal epithelium that descends from the foramen cecum at the base of the tongue to its normal position in the anterior neck. In the development of the thyroid gland, it can be remained in every stage of descending. This pattern of descent explains the occasional presence of ectopic thyroid tissue, most commonly located at the base of the tongue (lingual thyroid) or at other sites abnormally high in the neck.
Ectopic thyroid tissue (ETT) is reported in about 1 per 100,000-300,000 individuals and almost entirely results from thyroid abnormal embryologic at early stages [1]. Although most of ETT was found in the head and neck, few literatures were reported ETT was in mediastinum [2], heart [3], lung [4], abdomen [5], and adrenal gland.
We had checked the articles about adrenal ETT published in English, only 13 cases were reported until now. Here is the 14th case report of the adrenal ETT.
Case presentation
We had obtained consent from the patient for this case report. Here we discussed a 49-year-old woman with left adrenal gland occupation. The mass was incidentally discovered by ultrasonography (US) during a health care 11 days before. The patient was healthy in the past, without hypertension, hyperthyroidism and hypothyroidism. The functional thyroid parameters such as thyroid stimulating hormone (TSH), T3, T4 were within the normal levels.
The CT scan revealed there was an abnormal well-defined low density mass in the left adrenal glandregion, the max-sectional area is 20×18 mm, without any differences in the enhanced CT scan (Figure 1). The radiologist considered that it was adrenal adenoma. So the mass was surgical removed.
Figure 1.

CT Picture. Enhanced CT scan demonstrates a round, well circumscribed mass on the left side of the left adrenal gland (arrow).
Pathological findings
Gross examination showed an irregular gray tissue consisted of a potion of adrenal gland with cyst formation. The cyst wall wassmooth with 0.3 cm thick, without contents. Histological examination of the resected adrenal gland cyst demonstrated that the cyst wall was consist of fibrous tissue without an epithelial lining, and thyroid tissue was found in the cyst wall and the adherent adrenal gland regions.
Immunohistochemistry indicated ectopic thyroid tissue was positive for thyroglobulin (TG) and thyroid transcription factor-1 (TTF-1), negative for Galectin-3, HBME-1. BRAF V600E point mutation was also detected by immunohistochemistry (Figure 2). The immunostaining showed that ETT was negative for BRAF V600E.
Figure 2.
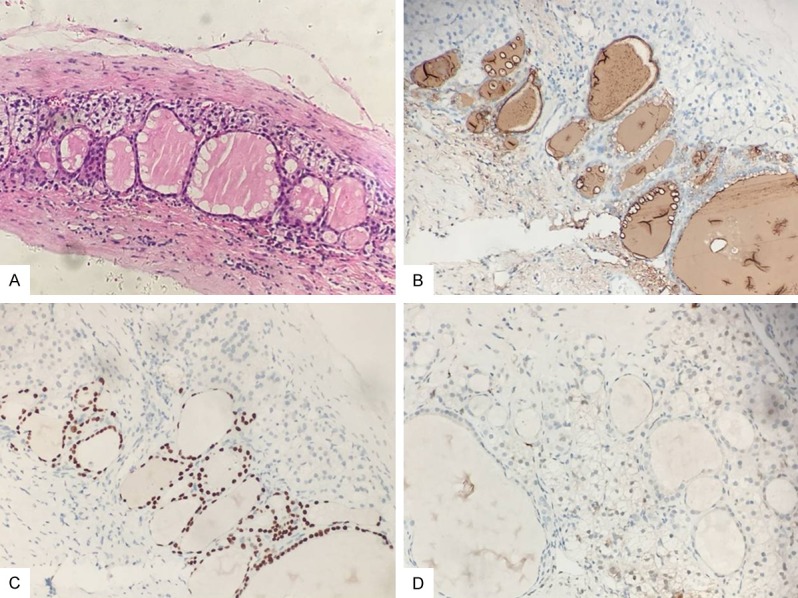
HE and Immunostain. A: The cyst wall is bordered by fibrous tissue with a single layer of epithelial celland includes few follicles occupied by colloid, intermingled with adrenal tissue (hematoxylin and eosin, 200×). B, C: TG and TTF-1 immunostain (brown chromogen) confirms the presence of ectopic thyroid tissue (200×). D: HMBE-1 was negative for the thyroid follicles (200×).
To identify KRAS (exon 2 and exon 3) gene mutation, DNA was extracted from formalin-fixed paraffin-embedded material from the ETT.
Real-time quantitative PCR indicated that there was no KRAS (exon 2 and exon 3) mutation in the ectopic thyroid tissue (Figure 3).
Figure 3.
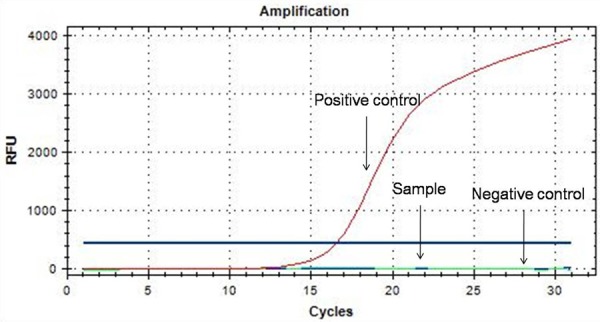
Real-time RT-PCR showed that there was no mutation in K-Ras gene (exon 2 and exon 3).
Discussion
The thyroid anlage appears in the embryo as a midline structure at the site corresponding to the foramen cecum of the adult tonge. From here, it decends as a component of the thyroglossal duct along the midline to reach its final position in the mid neck. ETT could be found in any site along the line of thyroid descending. The midline region, especially the head and neck, is the most common localization [6].
Although few cases were reported in the literature for ETT in adrenal glands and cervical, the mechanism of the ectopic thyroid beneath the diaphragm has been poorly revealed [6]. The most important differential diagnosis of this case was the metastasis of a cystic papillary thyroid carcinoma. Some researchers also considered that thyroid carcinoma could be metastasis to adrenal gland or ETT malignant transformation [7-9].
In this case, the ETT was made up of round or oval follicles that vary considerably in size. The follicles were lined by a single layer of follicular cells with flat shape. Immunohistochemistry showed that ETT was positive for TG and TTF-1, negative for Galectin-3 and HBME-1. The results were consistent with the literature reports [10,11].
Jeon M had reported that BRAF V600E or RAS mutations were observed in almost all the thyroid carcinoma [12]. In this case, neither BRAF V600E point mutation nor KRAS (exon 2 and exon 3) mutation was detected in ETT. So we considered that ETT was normal thyroid tissue, not the thyroid carcinoma metastasis. Moreover, the thyroid glands of the patient were also examined by ultrasonography without abnormal.
Gian Piero Casadei analyzed 10 cases of adrenal ETT were reported in English literatures from 1996-2014. The age of the patients with adrenal ETT was range from 32 to 67 years old. Seven cases of adrenal ETT were discovered incidentally, and most of patients had no endocrine abnormalities. Eight cases of adrenal ETT were cystic, containing colloid-like material [13]. This case was a 49-year old woman with adrenal ETT discovered suddenly by health care. The adrenal ETT was cystic, unilocular. The clinical and pathological manifestations were consistent with reports in literatures.
CT and MRI were considered to be the accurate methods to locate and diagnose the adrenal cysts [14]. In this case, CT scan showed an abnormal well-defined low density mass in the left adrenal gland region, without any differences in the enhanced CT. The radiologist considered that it was adrenal adenoma. Although the endocrine examination within normal, surgical resection was prepared.
We considered that CT-guided fine needle aspiration cytology (FNAC) could be used to diagnosis of ectopic thyroid. FNAC was the most useful method for distinguishing the benign or malignant lesions in adrenal [15]. However, FNAC results may be misleading or non-diagnostic sometimes, especially for cystic masses.So the patient in this case was prepared for surgical resection. Six months later, the postoperative CT revealed no recurrence in the left adrenal gland. And the blood test demonstrated TSH, T3, T4 were also within the normal levels.
In conclusion, a 49-year old woman with adrenal gland ETT, blood detection was within normal. Pathological examination showed a cystic lesion, composed of normal adrenal and ectopic thyroid tissue, without BRAF V600E and K-RAS (exon 2 and exon 3) mutation. Further work-up did not exhibit evidence of thyroid malignancy.
Acknowledgements
This work was supported by the Natural Science Foundation of Shandong Province (No. ZR2013HQ018, No. ZR2016HL29), Science and Technology Development Project of Yantai City (No. 2013ZH098).
Disclosure of conflict of interest
None.
References
- 1.Noussios G, Anagnostis P, Goulis DG, Lappas D, Natsis K. Ectopic thyroid tissue: anatomical, clinical, and surgical implications of a rare entity. Eur J Endocrinol. 2011;165:375–82. doi: 10.1530/EJE-11-0461. [DOI] [PubMed] [Google Scholar]
- 2.Abdel Aal M, Scheer F, Andresen R. Ectopic mediastinal thyroid tissue with a normally located thyroid gland. Iran J Radiol. 2015;12:e7054. doi: 10.5812/iranjradiol.7054. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Rabus MB, Poçi N, Yılmaz F, Yerlikhan O, Aktemur T, Arslan A, Ozturk S, Oztek I, Balkanay M. Right ventricular mass: intracardiac ectopic thyroid tissue: a case report. Echocardiography. 2015;32:178–80. doi: 10.1111/echo.12741. [DOI] [PubMed] [Google Scholar]
- 4.Ko HH, Cho SW, Lee HS, Kim HS, Nam ES, Cho SJ. Ectopic intrapulmonary thyroid: a case report. Korean J Thorac Cardiovasc Surg. 2013;46:237–9. doi: 10.5090/kjtcs.2013.46.3.237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Kutz M, Vila JJ, Urman JM, Garaigorta M, Guinduláin E, Tarifa A, Gómez ML. Ectopic retroperitoneal thyroid gland. Gastroenterol Hepatol. 2012;35:400–3. doi: 10.1016/j.gastrohep.2012.03.013. [DOI] [PubMed] [Google Scholar]
- 6.Santangelo G, Pellino G, De Falco N, Colella G, D’Amato S, Maglione MG, De Luca R, Canonico S, De Falco M. Prevalence, diagnosis and management of ectopic thyroid glands. Int J Surg. 2016;28(Suppl 1):S1–6. doi: 10.1016/j.ijsu.2015.12.043. [DOI] [PubMed] [Google Scholar]
- 7.Ginzburg S, Reddy M, Veloski C, Sigurdson E, Ridge JA, Azrilevich M, Kutikov A. Papillary thyroid carcinoma metastases presenting as ipsilateral adrenal mass and renal cyst. Urol Case Rep. 2015;3:221–2. doi: 10.1016/j.eucr.2015.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Farina E, Monari F, Tallini G, Repaci A, Mazzarotto R, Giunchi F, Panzacchi R, Cammelli S, Padula GD, Deodato F, Pasquali R, Fanti S, Fiorentino M, Morganti AG. Unusual thyroid carcinoma metastases: a case series and literature review. Endocr Pathol. 2016;27:55–64. doi: 10.1007/s12022-015-9410-7. [DOI] [PubMed] [Google Scholar]
- 9.Lianos G, Bali C, Tatsis V, Anastasiadi Z, Lianou E, Papathanasiou V, Messinis T. Ectopic thyroid carcinoma. Case report. G Chir. 2013;34:114–6. [PMC free article] [PubMed] [Google Scholar]
- 10.Ma H, Xu S, Yan J, Zhang C, Qin S, Wang X, Li N. The value of tumor markers in the diagnosis of papillary thyroid carcinoma alone and in combination. Pol J Pathol. 2014;65:202–9. doi: 10.5114/pjp.2014.45782. [DOI] [PubMed] [Google Scholar]
- 11.Bohinc BN, Parker JC, Hope WW, Kotwall C, Turner J, Cheng W, Lloyd RV. Micropapillary thyroid carcinoma and concomitant ectopic thyroid tissue in the adrenal gland: metastasis or metaplasia? Thyroid. 2011;21:1033–8. doi: 10.1089/thy.2010.0390. [DOI] [PubMed] [Google Scholar]
- 12.Jeon M, Chun SM, Kim D, Kwon H, Jang EK, Kim TY, Kim WB, Shong Y, Jang SJ, Song DE, Kim WG. Genomic alterations of anaplastic thyroid carcinoma detected by targeted massive parallel sequencing in a BRAF V600E mutation-prevalent area. Thyroid. 2016;26:683–90. doi: 10.1089/thy.2015.0506. [DOI] [PubMed] [Google Scholar]
- 13.Casadei GP, Bertarelli C, Giorgini E, Cremonini N, de Biase D, Tallini G. Ectopic thyroid tissue in the adrenal gland: report of a case. Int J Surg Pathol. 2015;23:170–175. doi: 10.1177/1066896914541001. [DOI] [PubMed] [Google Scholar]
- 14.Allen BC, Francis IR. Adrenal imaging and intervention. Radiol Clin North Am. 2015;53:1021–35. doi: 10.1016/j.rcl.2015.05.004. [DOI] [PubMed] [Google Scholar]
- 15.Rana C, Krishnani N, Kumari N. Spectrum of adrenal lesions on fine needle aspiration cytology. Indian J Pathol Microbiol. 2012;55:461–466. doi: 10.4103/0377-4929.107781. [DOI] [PubMed] [Google Scholar]


